Abstract
Background: Carpal tunnel syndrome (CTS) is one of the most common compressive neuropathies and affects a large amount of individuals. We investigated the direct and indirect cost to society of operative versus nonoperative management of CTS. Methods: A Monte Carlo simulation model was used to estimate the lifetime direct and indirect costs associated with nonoperative and operative treatment of CTS, and its utility to patients. Results: Operative treatment of CTS had a lower total cost and a higher utility when compared with nonoperative treatment. Conclusions: CTS surgery is clearly a cost-effective treatment strategy that should be included in the societal perspective regarding evolving costs and savings associated with health care.
Keywords: carpal tunnel syndrome, carpal tunnel release, health care, Monte Carlo simulation, cost-effective, patient care, patient utility
Introduction
Carpal tunnel syndrome (CTS) is the most common upper extremity compressive neuropathy. It has a prevalence of approximately 3% in the general population and nearly 8% in the working population.1-3 Outcomes of CTS can improve with nonoperative and operative treatment, yet the number of operatively treated CTS patients continues to increase. From 1996 to 2006, the annual number of carpal tunnel releases (CTRs) that were performed had increased by 38% (from 360 000 to 577 000).4
Workdays missed due to CTS result in monetary loss to both the patient and the economy.5 Based on the Bureau of Labor Statistics, in 2015, patients with CTS missed 28 days of work. For comparison, 28 days is slightly less than a fracture and nearly 1 week more than an amputation.6 It is becoming exceedingly important to optimize patient outcomes and simultaneously minimize health care costs and lessen the economic burden a disease state places on society from missed work. There are previous studies that evaluate the cost-effectiveness between open and endoscopic CTR7,8 and simultaneous bilateral and staged bilateral CTR,9 as well as operative and nonoperative management.10 However, to our knowledge, there is no study that has evaluated the direct and indirect cost to society of operative versus nonoperative treatment of CTS. The purpose of this study was to estimate the value of CTR from a societal perspective. It is our hypothesis that operative treatment of CTS has more societal and economic value than nonoperative treatment.
Materials and Methods
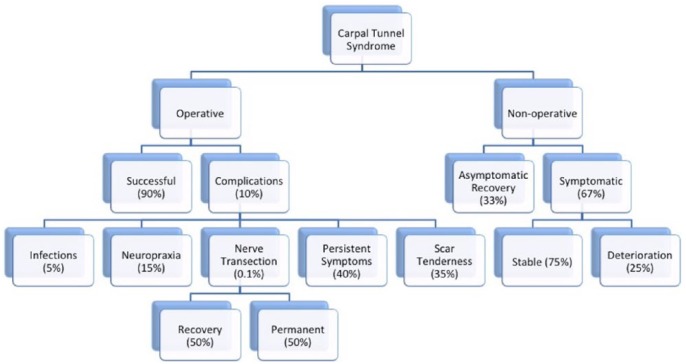
We constructed a Monte Carlo simulation model to estimate the lifetime direct and indirect costs associated with nonoperative and operative treatment of CTS. The Monte Carlo method is a technique that relies on repeated random sampling to generate numerical data. This method is used often in probability theory and completed using computer algorithms that rely on repeated random sampling, allowing the randomness to solve for outcomes. The outcomes and probabilities for CTS interventions stated in Figure 1 were obtained from general literature review and senior author expert opinion when data were not available. The model and analysis were performed using a general decision analysis software package (TreeAge Pro Suite 2016; TreeAge Software, Williamstown, MA). Our Monte Carlo simulations consisted of 100 000 individual trials for both cost and utility.
Figure 1.
Monte Carlo decision-making tree.
We first created a decision tree with 2 primary treatment paths: operative and nonoperative (Figure 1).
Simulations that were randomly selected for the operative arm (open CTR) either had a successful surgery or had a complication. The complications consisted of infection, neuropraxia, nerve transection, persistent symptoms, and scar tenderness. Simulations that led down the nonoperative arm had asymptomatic recovery or continued to be symptomatic. Those that remained symptomatic transitioned to those that remained stable and symptomatic and those that had deterioration of their symptoms. All individuals were assumed to live 38 years (from age 45 to 83) based on census data.
Cost
Direct costs include all medical costs for nonoperative and operative treatment of CTS. Direct costs of treatment of CTS were taken from the work of Pomerance and Zurakowski.10 For operative treatment, which included an open CTR, they calculated the average cost per patient of operatively treated CTS using reimbursement data from the doctor’s office, anesthesia, therapist fees, testing, surgery, and surgical facility. Similarly, for nonoperative treatment, the average cost per patient was calculated using reimbursement data from the doctor’s office, therapist fees, testing, and splinting.10
Indirect costs include lost wages due to inability to work, lower earnings, or missed work. Cost for missed work was based on Median US Salary in 2010 of US $41 673 per year. The amount of missed work calculated did not include time away from work for doctor’s appointments, day of surgery, and recovery. Direct and indirect costs were incorporated into the Monte Carlo simulation model to estimate the impact of CTS surgery on a patient’s lifetime.
Utility
Utility is an individual’s preferences for specific health outcomes. Estimating the utility of a treatment helps determine its effect on the quality of life of a patient. Quality-of-life measurements incorporate physical and social functioning, as well as psychological well-being.8,10,11 Utilities specific to carpal tunnel patients were taken from previously produced work by Chung et al and used for this analysis (Table 1). A 10 represented perfect health, and 0 represented death. The utility is presented as an average for a given year of an individual’s life, with a healthy individual’s utility having a score of 7.8.
Table 1.
Carpal Tunnel Syndrome Outcomes and Utility.
| Type of outcome | Utility ± SD | Time | Utility ± SD (remainder of life) |
|---|---|---|---|
| Successful surgery | 7.8 ± 1.4 | Life | |
| Asymptomatic/recover: nonoperative treatment | 7.8 ± 1.4 | Life | |
| Symptomatic and stable | 7.0 ± 1.7 | Life | |
| Symptomatic and deteriorate | 5.1 ± 1.8 | Life | |
| Infection | 7.5 ± 1.8 | 3 wk | 7.8 ± 1.4 |
| Neuropraxia | 7.0 ± 1.7 | 3 mo | 7.8 ± 1.4 |
| Nerve transection with recovery | 5.1 ± 1.8 | 9 mo | 7.8 ± 1.4 |
| Nerve transaction—permanent | 5.1 ± 1.8 | Life | |
| Persistent symptoms | 7.0 ± 1.7 | Life | |
| Scar tenderness | 6.9 ± 1.7 | 6 mo | 7.8 ± 1.4 |
Results
Operative treatment of CTS had a lower total cost and a higher utility when compared with nonoperative treatment (Table 2).
Table 2.
Carpal Tunnel Syndrome Cost and Utility.
| Operative | Nonoperative | |
|---|---|---|
| Mean cost | US $3536.59 ± US $7155.66 | US $95 735.65 ± US $92 841.14 |
| Mean utility | 7.8 ± 1.42 | 7.1 ± 1.79 |
The mean total cost of operative treatment of CTS was US $3536.59 ± US $7155.66, with a mean utility of 7.8 ± 1.42. The cost of successful operative treatment of CTS, which occurs 90% of the time, was US $3068.00. The mean total cost of nonoperative treatment was US $95 735.65 ± US $92 841.14, with a mean utility of 7.1 ± 1.79. In the nonoperative treatment arm, 33% of cases become asymptomatic/recover. Based on the data of Pomerance and Zurakowski, the cost of this is US $2322.00.10 The remaining 67% of the nonoperative treatment arm continue to have symptoms and either remain stable or deteriorate. In 75% of cases, the symptoms remain stable, and the cost per year is US $3846.72. This accounts for 2 days per month of missed work. In 25% of the symptomatic nonoperative treatment group, the condition deteriorates and results in a US $41 673.00 per year cost. The graph in Figure 2 summarizes the cost of successful operative and all 3 possible nonoperative treatment options.
Figure 2.
Successful operative and nonoperative treatment cost.
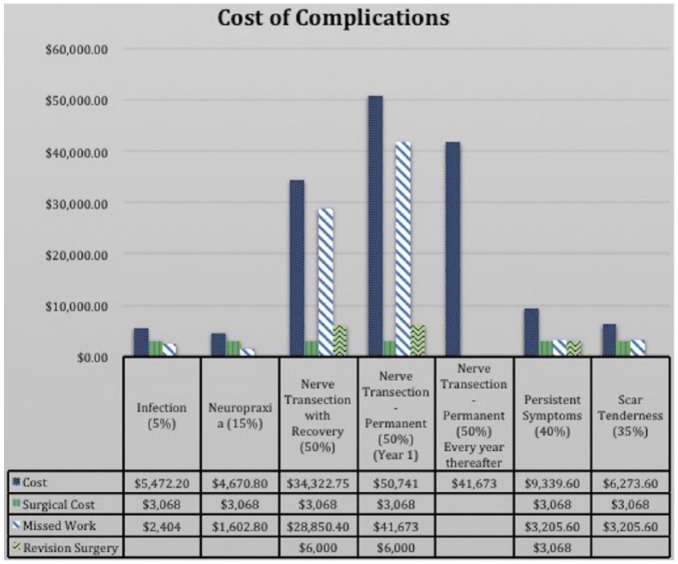
A complication occurred in 10% of cases. Infection accounts for 5% of the total complications (0.5% rate over all outcomes) and costs US $5472.20 (US $3068.00 for the initial open CTR and US $2404.00 for missing 3 weeks of work to deal with the infection). After these 3 weeks, they are presumed to be cured and go back to normal life. Neuropraxia accounts for 15% of the complications (1.5% overall rate) and costs US $4670.80 (surgical cost of US $3068.00 and US $1602.80 for 10 days of missed work to recover from the neuropraxia symptoms). Nerve transection is a rare complication and accounts for 0.1% of the complications (0.01% overall rate). When it recovers, it costs US $37 918.40 (surgical cost of US $3068.00, revision surgery with nerve repair of US $6000.00, and cost of 180 days of missed work totaling US $28 850.40). When the nerve transection does not recover, the first year’s cost after this complication totals US $50 741.00 (surgical cost of US $3068.00, revision surgery with nerve repair of US $6000.00, and cost of 260 days of missed work [1 work year] totaling US $41 673.00). The cost per year thereafter is US $41 673.00 until the retirement age of 65. Persistent symptoms following open CTR accounts for 40% of the complications (4% overall rate). The total cost is US $9341.60, and this includes the original surgery (US $3068.00), a revision surgery (re-release; US $3068.00), plus 1 work month of missed work (US $3205.60). Finally, scar tenderness accounts for 35% of complications (3.5% overall rate), and the total cost is US $6273.60 (surgical cost of US $3068.00 and 1 month of missed work [20 days] totaling US $3205.60). The breakdown of the cost of these complications is summarized in Figure 3.
Figure 3.
Cost of unsuccessful complications.
Discussion
CTS can be successfully treated operatively and nonoperatively. However, the long-term successfulness of nonoperative treatment does not have robust evidence to support this option, and symptom deterioration over time has also been confirmed.12-14 Operative treatment has been proven to be the most cost-effective treatment in previous studies by Pomerance and Zurakowski10 and Korthals-de Bos et al.15 These studies evaluated the cost-effectiveness of operative versus nonoperative treatment and found surgery to be the preferred treatment for CTS.10,15 A recent systematic review and meta-analysis that looked at 9 randomized controlled trials and 4 observational studies confirmed that operative treatment of CTS has better efficacy and safety over nonoperative management.16
Similar cost-effectiveness models have been carried out for rotator cuff tears and end-stage knee osteoarthritis, specifically for societal cost of operative versus nonoperative management. Both studies demonstrate a significant societal savings when these diagnoses are treated operatively.11,17 Surgical treatment for CTS had a much smaller cost and a higher utility when compared with conservative treatment. We specifically used higher costs for complications and longer time spent off from work in our Monte Carlo simulation model that would cause an error toward an overestimation of the overall operative cost. Despite this, our model still resulted in a relatively substantial cost differential between operative and nonoperative treatment. For this cost gap to be narrowed, a nerve transection rate of nearly 11% would have to be used during the simulation.
This study does have limitations. To allow the Monte Carlo simulation model to run appropriately, the analysis was based on certain estimations on costs, utility, and surgical outcomes; however, using data from previously accepted cost-effectiveness studies minimized this. We also used a Monte Carlo simulation model in which there are no recurrent cycles and no possibility of an early death. Each simulation progressed through the decision tree without factoring in the probability of: (1) adequate resolution of symptoms after revision CTR; (2) recurrent symptoms after a period of being symptom-free; or (3) an early death. Instead of a Monte Carlo model, a Markov model was used in similar studies that evaluated societal cost of rotator cuff tears and end-stage osteoarthritis.11 A Markov model can be particularly helpful when there is a recurrent problem within the population that a patient can continually cycle through, such as repeat symptomatic rotator cuff tears in the same patient after an arthroscopic repair. Markov models can also be helpful when attempting to adjust for the possibility of an early death at any stage in the decision tree.
The estimates of indirect costs of CTS primarily accounted for missed work due to complications and symptom persistence. It did not account for work missed for doctor’s appointments, postoperative care, therapy sessions, or additional prescriptions. Nor did this account for other return-to-work factors such as occupation and productivity, patient comorbidities, anxiety, and patient expectation.18
The utility values used were taken from the work of Chung et al. While these have been used in previous cost-effectiveness studies, they may not fully represent the national mean of these values.
Conclusions
Operative treatment of CTS has a significantly lower mean cost and higher mean utility than nonoperative treatment of CTS. While this is not to say that everyone with CTS should undergo operative treatment, it is clearly a cost-effective treatment strategy that should be included in the societal perspective of the evolving costs and savings in health care.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Because this article did not contain studies with human subjects, no informed consent was obtained.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Atroshi I, Englund M, Turkiewicz A, et al. Incidence of physician-diagnosed carpal tunnel syndrome in the general population. Arch Intern Med. 2011;171(10):943-944. [DOI] [PubMed] [Google Scholar]
- 2. Atroshi I, Gummesson C, Johnsson R, et al. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282(2):153-158. [DOI] [PubMed] [Google Scholar]
- 3. Dale AM, Harris-Adamson C, Rempel D, et al. Prevalence and incidence of carpal tunnel syndrome in US working populations: pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39(5):495-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fajardo M, Kim SH, Szabo RM. Incidence of carpal tunnel release: trends and implications within the United States ambulatory care setting. J Hand Surg Am. 2012;37(8):1599-1605. [DOI] [PubMed] [Google Scholar]
- 5. Foley M, Silverstein B, Polissar N. The economic burden of carpal tunnel syndrome: long-term earnings of CTS claimants in Washington State. Am J Ind Med. 2007;50(3):155-172. [DOI] [PubMed] [Google Scholar]
- 6. US Bureau of Labor Statistics. Nonfatal occupational injuries and illnesses requiring days away from work, 2015. Washington, DC: US Department of Labor; 2015. https://www.bls.gov/news.release/pdf/osh2.pdf. Accessed October 22, 2018. [Google Scholar]
- 7. Thoma A, Wong WH, Sprague S, et al. A cost-utility analysis of open and endoscopic carpal tunnel release. Can J Plast Surg. 2006;14(1):15-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chung KC, Walters MR, Greenfield ML, et al. Endoscopic versus open carpal tunnel release: a cost-effectiveness analysis. Plast Reconstr Surg. 1998;102:1089-1099. [DOI] [PubMed] [Google Scholar]
- 9. Park KW, Boyer MI, Gelberman RH, et al. Simultaneous bilateral versus staged bilateral carpal tunnel release: a cost-effectiveness analysis. J Am Acad Orthop Surg. 2016;24:796-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pomerance J, Zurakowski DI. The cost-effectiveness of nonsurgical versus surgical treatment for carpal tunnel syndrome. J Hand Surg. 2009;34:1193-1200. [DOI] [PubMed] [Google Scholar]
- 11. Mather RC, Koenig L, Acevedo D, et al. The societal and economic value of rotator cuff repair. J Bone Joint Surg Am. 2013;95:1993-2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gerritsen AA, de Krom MC, Struijs MA, et al. Conservative treatment options for carpal tunnel syndrome: a systematic review of randomised controlled trials. J Neurol. 2002;249:272-280. [DOI] [PubMed] [Google Scholar]
- 13. Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(2):CD001554. [DOI] [PubMed] [Google Scholar]
- 14. O’Connor D, Marshall S, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003;(1):CD003219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Korthals-de Bos IB, Gerritsen AA, van Tulder MW, et al. Surgery is more cost-effective than splinting for carpal tunnel syndrome in the Netherlands: results of an economic evaluation alongside a randomized controlled trial. BMC Musculoskelet Disord. 2006;7:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ren Y-M, Wang X-S, Wei Z-J. Efficacy, safety, and cost of surgical versus nonsurgical treatment for carpal tunnel syndrome: a systematic review and meta-analysis. Medicine. 2016;95(40):e4857. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17. Ruiz D, Jr, Koenig L, Dall TM, et al. The direct and indirect costs to society of treatment for end-stage knee osteoarthritis. J Bone Joint Surg Am. 2013;95:1473-1480. [DOI] [PubMed] [Google Scholar]
- 18. Elfar JC, Foad MB, Foad SL, et al. A cost analysis of staged and simultaneous bilateral carpal tunnel release. Hand. 2012;7(3):327-332. [DOI] [PMC free article] [PubMed] [Google Scholar]