Abstract
Background: Unstable intra-articular proximal interphalangeal (PIP) joint fracture-dislocations present a difficult problem that requires congruous joint reduction and stable internal fixation or distraction. Though fractures with limited articular involvement may be treated successfully with less invasive procedures, fracture-dislocations with a volar shear component may benefit from joint reduction with subchondral support for maintenance of stability. The purpose of this article is to describe a volar transverse plate and screw technique and report the short-term postoperative results. Methods: Seventeen patients with volar shear PIP dorsal fracture-dislocations were treated with transverse plate and screw constructs at an average of 21 days (range, 2-52) after injury. Information on postoperative stability, range of motion at PIP and distal interphalangeal (DIP) joints, and radiographic outcomes and complications were retrospectively collected. Results: At a mean of 7.3 months post-operation (range, 1.5-24), there were no recurrent dislocations and an average PIP arc of 77.4° and DIP arc of 61.5°. Sixteen of 17 patients had radiographically concentric joints, with 1 patient showing slight radiographic dorsal subluxation not apparent clinically. Two of 17 patients (11.8%) had revision surgery for tenolysis and removal of hardware to improve range of motion at 4 and 9 months post-operation. Conclusions: In the setting of PIP dorsal fracture-dislocations with volar shear component >40% of the articular surface, the Seatbelt procedure allows for concentric joint and articular surface reduction with subchondral support for maintenance of stability. This volar transverse plating technique allows for highly functional range of motion without PIP dorsal subluxation clinically in the setting of comminution and delayed presentation.
Keywords: proximal interphalangeal joint, PIP fracture-dislocation, PIP volar shear fracture, range of motion, PIP volar lip fracture
Introduction
Unstable proximal interphalangeal (PIP) joint fracture-dislocation treatment remains problematic for hand surgeons with stiffness, persistent subluxation, and degenerative changes occurring if not treated properly.12 The preponderance of literature supports anatomic PIP joint reduction,12 but there is no consensus as to which technique achieves the best results. Surgical techniques must balance anatomic reduction with minimal soft tissue disruption, while preventing redislocation in a joint that is prone to both stiffness and instability. Cadaveric models studying the biomechanical stability of these injuries demonstrated that when there was loss of 40% of the volar base of the middle phalanx, there was consistent subluxation of the PIP joint.10 These injuries often involve a greater component of articular surface than initially appreciated due to the comminution seen with the volar shear pattern of fracture-dislocation.1
Many techniques have been described for treatment of unstable PIP volar lip fractures. These include dorsal block pinning, dynamic external fixation, volar plate arthroplasty, and hemi-hamate arthroplasty (HHA). A variety of exposures and implants have been utilized to treat this injury pattern. The number of described techniques is representative of both the variability of these injuries and the difficulty in successfully treating these fracture patterns. In this case series, we review our experience with open reduction and internal fixation through a volar “shotgun” approach with transverse plating, termed the “seatbelt procedure” in patients with > 40% articular involvement and clinical or radiographic dorsal subluxation.
In this case series, we describe a technique that allows for fracture reduction, articular congruity, minimization of irritation from prominent hardware and prevention of dorsal dislocation in the setting of repairable base of the middle phalanx fracture-dislocations. To our knowledge, this technique has not been previously described or reported.
Materials and Methods
A retrospective, institutional review board–approved chart review was performed on patients who had undergone open reduction internal fixation (ORIF) with volar, transverse plating for unstable PIP fracture-dislocations at 2 institutions by 4 fellowship-trained hand surgeons over a 7-year period. All patients with a Current Procedural Terminology (CPT) code 26785 (open treatment of phalangeal joint dislocation) or 26746 (open treatment of interphalangeal fracture) were included based on an institutional query search tool, and charts were reviewed for use of this technique in the operative report.
Inclusion criteria for this study comprised isolated volar shear PIP dorsal fracture-dislocations with both clinical signs of instability and persistent dorsal “V” sign on lateral radiographs despite attempts at reduction (Figure 1). Exclusion criteria included multiple PIP fracture-dislocations of the same hand, concomitant dorsal comminution requiring additional fixation, other concomitant fractures of the ipsilateral hand, and follow-up less than 6 weeks. This left 17 patients to be included in this study: 12 males and 5 females.
Figure 1.
(a) Posteroanterior and (b) lateral radiographs of ring finger. Unstable proximal interphalangeal joint fracture-dislocation with volar shear component of middle phalanx. Upon evaluation in the operating room, the articular involvement was >45%.
Using electronic medical records, we elicited demographic data regarding age, sex, mechanism of injury, occupation, and hand dominance. Operative notes were reviewed regarding specifics of surgical technique and implanted hardware. Preoperative and postoperative functional, clinical, and radiographic data were reviewed, including range of motion (ROM) and clinical stability from clinic and occupational therapy assessments. These data were collected at the 2-week postoperative visit and at intervals until the patient’s most recent follow-up. Final follow-up was determined by the patient’s progress with occupational therapy and if further improvement was anticipated. A shared decision was then made between the physician and patient.
The primary outcome was postoperative ROM at PIP and distal interphalangeal (DIP) joints. Secondary outcomes were complications, including dislocation or subluxation.
Operative Technique
Patients underwent a volar approach, Bruner or oblique-midlateral-oblique “trapdoor,” to the PIP joint. A window was created in the flexor tendon sheath between A2 and A4 and was reflected to reveal the underlying flexor tendons. The tendons were retracted to expose the volar plate. The volar plate was released distally and one or both collateral ligaments were released proximally or distally to hyperextend and “shotgun” the PIP joint. This allowed for evaluation and congruous reduction of the articular surface (Figure 2). The percentage of articular involvement was assessed. Upon intraoperative evaluation, the intra-articular surface of all our patients involved more than 40% of the articular surface, often more radial than ulnar, resulting in underestimation of articular involvement on lateral radiographs. A dental pick was used for reducing impacted articular surface. Based on surgeon preference, demineralized bone matrix was used to help maintain reduction in the setting of comminution. Visual inspection confirmed the presence of an intact dorsal cortex. A pre- or intraoperatively contoured 3-hole transverse plate was fashioned by cutting off the vertical portion of a “T” plate. Small Kirschner-wires (K-wires) (0.028 or 0.035 inch) were occasionally used for maintenance of reduction while 3 nonlocking screws (either 1.3 or 1.5 mm) were placed for fracture fixation, volar to dorsal through the plate. The finger was then reduced and ranged to test fixation and stability under fluoroscopy. The collateral ligaments were not routinely repaired.
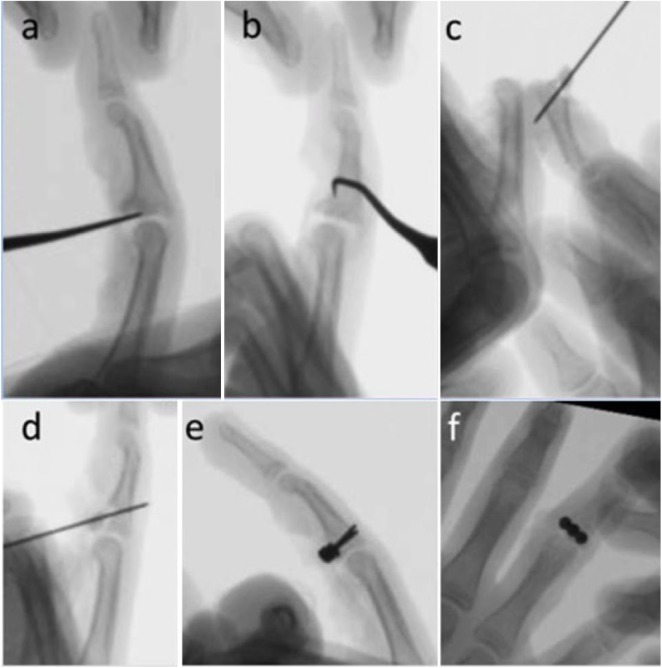
Figure 2.
Intraoperative fluoroscopy. (a) Dental pick is used to reduce impacted articular fragments and (b) free any formation of consolidated tissue. (c) The joint is “shotgunned” open exposing the joint allowing for (d) Kirschner-wire to reduce the fracture. (e) Lateral and (f) posteroanterior fluoroscopy of 3-hole plate with 3 nonlocking screws achieving concentric reduction of joint.
The soft tissue volar plate was then placed over the plate-screw construct for soft tissue coverage, preventing irritation of the flexor tendons. In 3 cases, a single ulnar slip of the flexor digitorum superficialis was cut proximally and sutured to the radial portion of the volar plate. This supplied additional soft tissue coverage of the metal plate construct and also acts as a stabilizer to the middle phalanx from dorsal subluxation. After wound closure, patients were placed in a 30° dorsal blocking splint or ulnar gutter splint for immobilization until first occupational therapy visit.
Postoperative Follow-up
Patients remained in their splint until seen by occupational therapy at a mean of 7 days (range, 3-15) postoperatively, at which time they were place on an early motion protocol. Clinic visits were at 2 and 6 weeks with regular subsequent follow-up based on clinical and radiographic progress (Figure 3). At clinic visits, radiographs were obtained as well as notes documenting ROM, clinical subluxation, and complications including sensory deficits and infection (Figure 4).
Figure 3.
(a) Posteroanterior, (b) oblique, and (c) lateral plain films of the volar transverse plate with 3 screws resulting in stable fixation of middle phalanx and concentric reduction of the joint.
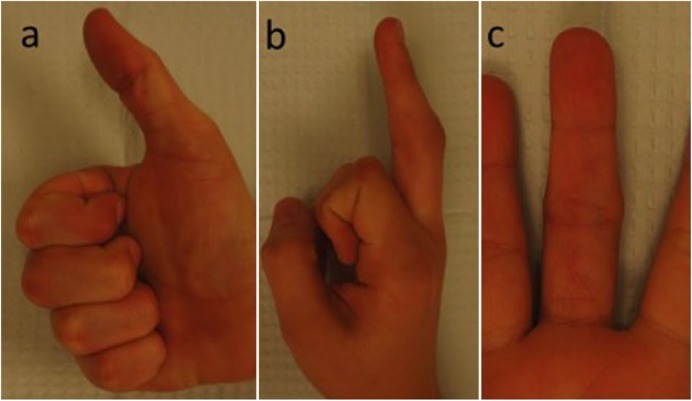
Figure 4.
Clinical photos at 6 weeks post-procedure showing (a) flexion to distal palmar crease, (b) functional extension, and (c) healed Bruner incision.
Results
Patients
Seventeen patients with an average age of 36.8 years (range, 13-78) met inclusion criteria. The average time from injury to surgery was 21.6 days (range, 2-52). Ten of 17 patients (59%) injured their dominant hand, and 10 of 17 injured their ring finger compared with 4 long finger, 2 small finger, and 1 index finger. In 11 of 17 patients (65%), the injury occurred while playing sports, while the majority of remaining injuries were due to a fall on outstretched hand. There were no other concomitant soft tissue injuries at the time of PIP injury, and concomitant ipsilateral hand fractures were excluded. There were no significant or relevant comorbidities in this cohort.
Intraoperative Findings
Intraoperatively, the articular surface of the middle phalanx was assessed, showing a mean of 51.3% (range, 45-65%) PIP articular involvement. It was noted that percentage of articular involvement is often greater than what was seen on lateral radiographs due to comminution and oblique orientation of fracture. In one of the cases, the tip of a drill had broken off within the bone. The decision was made to not risk the morbidity required for removal, and it was left in place. There were no other intraoperative complications.
Outcomes
Final follow-up was on average 7.3 months (range, 1.5-24.4) post-procedure. There was no clinical dorsal instability in our cohort. One patient demonstrated radiographic evidence of slight dorsal subluxation, which was not evident clinically.
The average PIP total arc of motion was 77.4° (range, 25-120°; SD, 21°). Average extension was 12.3° (0-60°; SD, 17°) and average flexion was 89.7° (70-120°; SD, 13°). Thirteen of 17 patients had an arc of motion greater than 70°, with 1 patient having limited ROM (25°). This patient presented for surgery 50 days after initial injury and was significantly older than our average patient (78.6 years old compared to mean 36.8). The average DIP arc of motion was 61.5° (0-95°; SD, 30°) and the average metacarpophalangeal arc of motion was 95° (86-110°; SD, 8°). The same patient with 25° PIP arc of motion had a fixed DIP joint at 15° with no arc of motion. She was noted to have significant pain at presentation and limited engagement with occupational therapy appointments.
Complications
At most recent follow-up, 1 patient had radiographic evidence of slight dorsal subluxation, which was not evident clinically. This patient’s PIP arc of motion was 65°, and he had no functional complaints and did not require further surgery. Two patients (11.8%) have undergone revision surgery for removal of hardware and tenolysis, one at over 9 months post-operation and one at 4 months post-operation. At 3 months following the removal of hardware and tenolysis, 1 patient improved PIP arc from 70° to 90° and DIP arc remained at 40°. The other patient improved PIP arc from 45° to 70° and DIP of 10° to 65°. One patient had slight distal numbness at the tip of his finger, which resolved at 5 months post-operation. There were no superficial or deep infections, and no antibiotics given for infection. There were no postoperative dislocations, catching or triggering at time of follow-up.
Discussion
Volar shear fractures of the middle phalanx in PIP fracture-dislocations pose a difficult problem for the hand surgeon and can result in poor outcomes if not properly treated. The PIP joint has the greatest arc of motion (120°) of the 3 phalangeal joints and is predisposed to stiffness with injury.2 Surgical techniques must balance anatomic reduction with minimal soft tissue disruption while preventing redislocation in a joint that is prone to both stiffness and instability. Perhaps due to the difficulty of achieving these goals of treatment, there are many techniques described5,6,8,9,13,14,17 without clear consensus on a uniformly successful procedure for these variable injuries.
The 3 treatment principles originally described by Kiefhaber and Stern in treating PIP fracture-dislocations are: (1) restoration of both joint and articular congruity; (2) rigid but nonlimiting fixation; and (3) early ROM.12 The Seatbelt procedure satisfies all of these conditions. The subchondral screws within the plate construct act as a raft for the subchondral bone and the transverse plate can buttress even comminuted fractures previously felt irreparable. Even in cases were there did not appear to be >40% articular involvement on lateral radiographs, intraoperative evaluation routinely showed more articular involvement than anticipated. The oblique orientation of the articular surface fracture was often more radial and ulnar, resulting in underestimation of articular involvement on lateral radiographs.
In our study, the patients underwent surgery at an average of 21 days post-injury, with 6 patients undergoing the procedure 30 days or more after their injury. As a tertiary referral center, delayed presentations for these injuries are common. Given the delayed presentation of our cohort, articular approximation and joint congruity becomes difficult without open exposure to the fracture site. Our results show satisfactory results when used for PIP fracture-dislocations in both the acute and subacute setting.
While dorsal block splint and pinning have produced good results with minimal soft tissue trauma for volar lip fragments involving 40% of the articular surface or less, there are limitations. These techniques rely on closed reduction of the joint in setting of vertical shear displacement and require a period of immobilization of at least 4 weeks to avoid dislocation or recurrent subluxation, due to lack of union at time of wire removal.1,14,16 Their use is contingent upon acceptable joint concentricity and fragment alignment with closed traction.11 Moreover, immobilization of more than 3 weeks can result in permanent loss of motion.2
Dynamic traction has produced good results, especially in the setting of comminuted pilon fractures. A study by Ruland et al15 reported an 88° PIP arc and 60° DIP arc at a mean 16-month follow-up for 34 patients with a mix of PIP fracture-dislocations and pilon fractures. Similar constructs by Ellis et al7 of 14 patients showed 88° PIP arc after 26 months; however, only 8 patients had follow-up and 5 patients showed small step off or development of radiographic arthritis.
Previous studies examining ORIF have shown good results but noted limitations in either the dorsal approach or in managing comminution. In a study by Aladin et al,1 it was noticed that the dorsal approach for more comminuted fractures did not allow for satisfactory volar purchase, which required cerclage wiring, resulting in PIP arc of 48° in 5 patients. Deitch et al4 studied ORIF with interfragmentary screws with or without − K-wires through volar and/or dorsal approach and found 3 of 33 (11%) postoperative dislocations due to loss of fixation. In addition, they comment on extensor tendon adhesions resulting in DIP extensor lag.
Our current technique aims to address these limitations by using a volar hardware construct, which acts as a buttress for the volar fracture components, especially in the setting of comminution. Moreover, the authors find that dorsal cortical bone at insertion of the central slip on the middle phalanx has great purchase for screw fixation, and soft tissue irritation is rare, as there is no superficial tendon excursion at this level. The volar approach also decreases extensor tendon irritation and subsequent adhesions, with the possible advantage of decreasing extensor lag.
Cheah et al3 studied volar mini-plating of 13 patients using a vertical plate or hook plate constructs to buttress the volar fragments. In this cohort, the degree of articular involvement ranged from 30% to 70% (average, 44%). At 25-month follow-up, there was a 75° PIP and 65° DIP arc of motion. However, 4 of 13 (30.8%) required plate and screw removal.
In the case of irreparable PIP fracture-dislocation in which the comminution is too great, HHA has been reported with good results. Williams et al17 describe 13 patients, 12 with follow-up, at 16 months who had a PIP arc of motion of 85° and a 60° DIP arc. There were 2 patients (16.7%) with recurrent subluxation. Yang et al18 reported 11 patients treated with HHA with 38-month follow-up, who showed an active ROM of the DIP and PIP joint of 80.4° and 85.4°, respectively. While HHA has demonstrated its value as a salvage technique, we have shown that a volar construct can provide good outcomes even in a subacute setting and should be considered for PIP fracture-dislocations regardless of chronicity and comminution.
There were limitations to our study. The retrospective nature of the study has potential biases and weaknesses inherently associated with this study design. Despite good early outcomes, the follow-up is relatively short, compared with other studies. As this technique places importance on concentric reduction of the joint, it would potentially be beneficial to show maintenance of concentricity over an extended period. Our study also included patients treated by 4 separate board-certified surgeons. Postoperative treatment protocols differed among surgeons.
In the setting of PIP dorsal fracture-dislocations with volar shear component >40% of the articular surface, the seatbelt procedure allows for concentric joint and articular surface reduction with subchondral support for maintenance of stability. This volar transverse plating technique allows for highly functional ROM without PIP dorsal subluxation clinically in the setting of comminution and delayed presentation.
Footnotes
Authors’ Note: All authors have seen and approved the manuscript and have contributed significantly to the article. In this description of a novel surgical technique, we have 4 attending surgeons from 2 institutions who have contributed cases and insight for the article and 3 resident authors who have contributed significantly in data collection and writing of the manuscript.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: No experiments on animals were performed for this study. No experimental procedures were performed on any human subject for this study.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Aladin A, Davis TR. Dorsal fracture-dislocation of the proximal interphalangeal joint: a comparative study of percutaneous Kirschner wire fixation versus open reduction and internal fixation. J Hand Surg Br. 2005;30(2):120-128. [DOI] [PubMed] [Google Scholar]
- 2. Blazar PE, Steinberg DR. Fractures of the proximal interphalangeal joint. J Am Acad Orthop Surg. 2000;8(6):383-390. [DOI] [PubMed] [Google Scholar]
- 3. Cheah AE, Tan DM, Chong AK, et al. Volar plating for unstable proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2012;37(1):28-33. [DOI] [PubMed] [Google Scholar]
- 4. Deitch MA, Kiefhaber TR, Comisar BR, et al. Dorsal fracture dislocations of the proximal interphalangeal joint: surgical complications and long-term results. J Hand Surg Am. 1999;24(5):914-923. [DOI] [PubMed] [Google Scholar]
- 5. De Smet L, Boone P. Treatment of fracture-dislocation of the proximal interphalangeal joint using the Suzuki external fixator. J Orthop Trauma. 2002;16(9):668-671. [DOI] [PubMed] [Google Scholar]
- 6. Dionysian E, Eaton RG. The long-term outcome of volar plate arthroplasty of the proximal interphalangeal joint. J Hand Surg Am. 2000;25(3):429-437. [DOI] [PubMed] [Google Scholar]
- 7. Ellis SJ, Cheng R, Prokopis P, et al. Treatment of proximal interphalangeal dorsal fracture-dislocation injuries with dynamic external fixation: a pins and rubber band system. J Hand Surg Am. 2007;32(8):1242-1250. [DOI] [PubMed] [Google Scholar]
- 8. Hamer DW, Quinton DN. Dorsal fracture subluxation of the distal interphalangeal joint of the finger and the interphalangeal joint of the thumb treated by extension block splintage. J Hand Surg Br. 1992;17(5):591-594. [DOI] [PubMed] [Google Scholar]
- 9. Hamilton SC, Stern PJ, Fassler PR, et al. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2006;31(8):1349-1354. [DOI] [PubMed] [Google Scholar]
- 10. Hastings H, II, Carroll C., IV Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin. 1988;4(3):503-527. [PubMed] [Google Scholar]
- 11. Keramidas E, Solomos M, Page RE, et al. The Suzuki frame for complex intra-articular fractures of the proximal interphalangeal joint of the fingers. Ann Plast Surg. 2007;58(5):484-488. [DOI] [PubMed] [Google Scholar]
- 12. Kiefhaber TR, Stern PJ. Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am. 1998;23(3):368-380. [DOI] [PubMed] [Google Scholar]
- 13. Krakauer JD, Stern PJ. Hinged device for fractures involving the proximal interphalangeal joint. Clin Orthop Relat Res. 1996(327):29-37. [DOI] [PubMed] [Google Scholar]
- 14. Newington DP, Davis TR, Barton NJ. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: a 16-year follow up. J Hand Surg Br. 2001;26(6):537-540. [DOI] [PubMed] [Google Scholar]
- 15. Ruland RT, Hogan CJ, Cannon DL, et al. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am. 2008;33(1):19-25. [DOI] [PubMed] [Google Scholar]
- 16. Waris E, Mattila S, Sillat T, et al. Extension block pinning for unstable proximal interphalangeal joint dorsal fracture dislocations. J Hand Surg Am. 2016;41(2):196-202. [DOI] [PubMed] [Google Scholar]
- 17. Williams RM, Kiefhaber TR, Sommerkamp TG, et al. Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am. 2003;28(5):856-865. [DOI] [PubMed] [Google Scholar]
- 18. Yang DS, Lee SK, Kim KJ, et al. Modified hemihamate arthroplasty technique for treatment of acute proximal interphalangeal joint fracture-dislocations. Ann Plast Surg. 2014;72(4):411-416. [DOI] [PubMed] [Google Scholar]