Abstract
Aim:
Cardiac arrest in the intensive care unit (ICU-CA) is a common and highly morbid event. We investigated the preventability of ICU-CAs and identified targets for future intervention.
Methods:
This was a prospective, observational study of ICU-CAs at a tertiary care center in the United States. For each arrest, the clinical team was surveyed regarding arrest preventability. An expert, multi-disciplinary team of physicians and nurses also reviewed each arrest. Arrests were scored 0 (not at all preventable) to 5 (completely preventable). Arrests were considered ‘unlikely but potentially preventable’ or ‘potentially preventable’ if at least 50% of reviewers assigned a score of ≥1 or ≥3 respectively. Themes of preventability were assessed for each arrest.
Results:
43 patients experienced an ICU-CA and were included. A total of 14 (32.6%) and 13 (30.2%) arrests were identified as unlikely but potentially preventable by the expert panel and survey respondents respectively, and an additional 11 (25.6%) and 10 (23.3%) arrests were identified as potentially preventable. Timing of response to clinical deterioration, missed/incorrect diagnosis, timing of acidemia correction, timing of escalation to a more senior clinician, and timing of intubation were the most commonly cited contributors to potential preventability. Additional themes identified included the administration of anxiolytics/narcotics for agitation later identified to be due to clinical deterioration and misalignment between team and patient/family perceptions of prognosis and goals-of-care.
Conclusions:
ICU-CAs may have preventable elements. Themes of preventability were identified and addressing these themes through data-driven quality improvement initiatives could potentially reduce CA incidence in critically-ill patients.
Keywords: Heart arrest, Cardiopulmonary resuscitation, Critical care, Intensive care unit quality improvement
Introduction
In-hospital cardiac arrest (IHCA) is a common occurrence in the United States with an annual incidence of over 290,000 cases per year.1,2 The incidence of IHCA has been increasing over the past decade. Unfortunately, survival to hospital discharge following IHCA remains low and survivors are commonly discharged with significant neurologic dysfunction.3 More than half of IHCAs occur in intensive care units (ICU), where outcomes are generally worse than those on monitored (i.e. telemetry) inpatient wards.4 Despite the substantial and increasing disease burden of ICU cardiac arrest (ICU-CA), there is little published data regarding their causes and preventability.5
Patients in the ICU are closely monitored, with a care structure that typically includes a low nurse-patient ratio, continuous cardiac and hemodynamic monitoring, and the immediate availability of the physician team. The close monitoring of patients in the ICU environment, however, may falsely reassure staff that patient safety is optimized, and thus contribute to a culture in which cardiac arrests that occur in the ICU are seen as inevitable and therefore not preventable.6 Additionally, tools used to prevent adverse events on inpatient wards are impractical in the ICU because these are often based on standardized vital sign abnormalities and may not be applicable to the abnormal physiological parameters frequently encountered in the ICU. As ICU-CA incidence increases, with only modest concomitant improvements in arrest outcomes, there is an acute need to explore possible preventability in ICU-CA and derive data-driven tools to assist clinicians tasked in averting them.
In the present study, we hypothesize that many ICU-CAs have preventable elements. Further, we identify common themes of preventability that can be used to develop tools for ICU-CA prevention.
Materials and methods
Study design, setting, and population
This was a prospective observational study conducted at a single tertiary care center in an urban setting. The study site includes 77 ICU beds divided into medical, surgical, neurologic, cardiac, trauma and cardiac surgery units, with one mixed medical/surgical unit. All ICUs are managed by trained intensivists with the exception of the cardiac care unit, which is managed by cardiologists (some of whom carry certification in critical care medicine). Patients in surgical ICUs are comanaged between the intensivist and surgical teams. Boarding patients (e.g. a patient on a medical ICU service but physically in a surgical ICU bed due to lack of beds in the medical ICU) were counted as being in the ICU in which they were physically located. The study was conducted between August 2017 and May 2018.
All patients who experienced an ICU-CA and received chest compressions of any duration were included. Only the index ICU arrest was reviewed. Patients who experienced an arrest within one hour of arrival to the ICU were excluded a priori to data analysis so as to limit analyzed cardiac arrest events to those potentially modifiable with changes to ICU care.
The study was reviewed and approved by the Beth Israel Deaconess Medical Center (BIDMC) Committee on Clinical Investigation (Institutional Review Board).
Case review — expert panel
A multi-disciplinary panel of critical care physicians (n = 7) and nurses (n = 3) (“expert panel”) was assembled. The composition of the expert panel included representatives of Pulmonary/Critical Care, Anesthesia/Critical Care, Cardiology, and Emergency Medicine. Members of the panel were selected to ensure a mix of representation from various medical specialties in addition to including individuals who serve on the site’s Resuscitation Committee and/or have substantial experience in IHCA research and quality improvement.
Prior to the start of the study, the expert panel independently reviewed 17 randomly selected cases of ICU-CA occurring between February and December 2016. Following independent review of these retrospective cases, the expert panel met to discuss ratings given to each arrest and build consensus around the case review process. During this process, common themes of preventability began to emerge and a list of contributing factors was finalized for use during the study. A case review tool was built to capture the appropriate data elements.
The expert panel was then tasked with independently reviewing each ICU-CA occurring during the study period. Each arrest was assessed on a scale ranging from 0 (not at all preventable) to 5 (completely preventable) had earlier or different action been taken in in the ICU (see Fig. 1). Members of the expert panel then selected from a list of predefined potential contributing factors to preventability. The predefined contributors were selected based on expert consensus of the panel. In addition, a comment section allowed for expert panel members to add preventability themes not present in the predefined list.
Fig. 1 −.
Preventability scale.
After independently completing all reviews, the expert panel met on a monthly basis to discuss all ICU-CAs reviewed in the preceding month. After discussion of each arrest, panel members were allowed to modify their preventability score so as to provide for more accurate ratings in the event of missed or clarified data regarding the ICU-CAs. In addition, new themes of preventability were identified during case discussion.
Provider surveys
A survey was developed to assess the perceptions of front-line clinical providers caring for patients who experience ICU-CA. The survey was developed in an iterative process and piloted among members of the expert panel. The survey instrument can be found in Supplemental Figure S1.
The survey was distributed electronically via REDCap electronic data capture tools hosted at the study site.7 Surveys were sent to the clinical team members (attending physician, trainees, advanced practice clinicians [APCs, i.e. nurse practitioners and physician assistants], and bedside nurses) caring for patients in the period immediately preceding the cardiac arrest. Surveys were generally sent within 48 -h of the arrest and included two weekly reminders if needed. As with the expert panel review, survey respondents were asked to assess the preventability of the cardiac arrest. In contrast to the expert panel, predefined categories of preventability were not offered and potential contributing factors to the arrest were elicited solely in free text form to avoid bias from the investigators. The free-text responses were later categorized by the author group into thematic categories.
Statistical analysis
A combination of quantitative and qualitative methodologies was used to assess the data. Descriptive statistics are reported with means with standard deviations or medians with interquartile ranges. Comparisons were made with t-tests, Wilcoxon rank sum tests, or Fisher’s exact tests as appropriate. Agreement amongst the expert panel was assessed using Fleiss’s Kappa. ICU-CAs were classified as ‘not preventable’ if less than half of raters selected a score ≥1, as ‘unlikely but potentially preventable’ if at least half of raters selected a score ≥1, and ‘potentially preventable’ if at least half of all raters selected a score ≥3.
The frequencies of predefined preventability themes, as well as new themes identified during review, were tabulated for comparison. Free text themes were categorized by two members of the expert panel into one of the a priori identified thematic categories or into unique categories if no a priori theme was appropriate. Discrepancies between reviewers were resolved through case discussion. Preventability themes are reported only for those arrests identified as at least unlikely but potentially preventable.
Results
A total of 48 patients suffered an ICU-CA during the study period, out of a total of 5062 patients admitted to the ICU. Of these, 5 patients arrested within one hour of ICU admission and were excluded from further analysis. Of the remaining 43 patients, the median age was 69 (IQR: 58–77) and 34.9% were female. There were 5062 ICU admissions during the study period. Complete details of patient demographics, arrest characteristics, and outcomes can be found in Table 1.
Table 1 −.
Cohort characteristics.
| Variable | Complete cohort (n = 43) | Potentially preventablea (n = 11) | Unlikely or not preventable (n = 32) | p-Value |
|---|---|---|---|---|
| Demographics | ||||
| Age (median, IQR) | 69.0 (58–77) | 69.0 (60–78) | 69.0 (58–77) | 0.66 |
| Gender (%female) | 34.9 | 9.1 | 43.8 | 0.07 |
| Race (%white) | 51.2 | 54.6 | 50.0 | >0.99 |
| Vasopressor | 62.8 | 63.6 | 62.5 | >0.99 |
| Invasive mechanical ventilation | 55.8 | 36.4 | 62.5 | 0.17 |
| Arrest characteristics | ||||
| Location n(%) | 0.92 | |||
| Cardiac care unit 8 beds | 10 (23.3) | 2 (18.2) | 8 (25.0) | |
| Cardiac surgery 15 beds | 2 (4.7) | 0 (0) | 2 (6.3) | |
| Medical ICUb 28 beds | 18 (41.9) | 5 (45.5) | 13 (40.6) | |
| Neurologic ICU 8 beds | 1 (2.3) | 0(0) | 1 (3.1) | |
| Surgical ICU 8 beds | 8 (18.6) | 2 (18.2) | 6 (18.8) | |
| Trauma surgical ICU 10 beds | 4 (9.3) | 2 (18.2) | 2 (6.3) | |
| Initial rhythm (shockable %) | 28.6 | 9.1 | 35.5 | 0.21 |
| Time of day (Daytimec %) | 39.5 | 36.4 | 40.6 | >0.99 |
| Duration of resuscitative efforts (minutes, median, IQR) | 12 (4–27) | 14 (8–15) | 12 (4–32) | 0.69 |
| Time from ICU admission until arrest (hours, median, IQR) | 50.0 (9.5–156.7) | 9.5 (1.8–50.1) | 69.5 (16.2–252.5) | 0.01 |
| Outcomes | ||||
| Return of spontaneous circulation (ROSC) achieved | 62.8 | 54.6 | 65.6 | 0.72 |
| Survival to hospital discharge | 23.3 | 36.4 | 18.8 | 0.25 |
As determined by a preventability score of ≥ 3 by at least half of expert reviewers.
Includes both the medical ICU and a mixed medical/surgical ICU that is occupied primarily be medical ICU patients.
Daytime defined as the hours from 0700 until 1859.
Expert review results
A median of 7 (IQR 6–8) reviewers evaluated each arrest. Overall, 14 (32.6%) arrests were identified as unlikely but potentially preventable (i.e. most ratings ≥1) and an additional 11 (25.6%) arrests were identified as potentially preventable (i.e. most ratings ≥3). There was fair agreement amongst reviewers regarding which arrests were potentially vs. less likely preventable (percent agreement = 74.7%, κ = 0.34, p < 0.0001).8
The most commonly selected (by at least one reviewer) predefined contributors to preventability in cases classified as at least unlikely but potentially preventable included: ‘delayed response to clinical deterioration (72.0%),’ ‘missed or incorrect diagnosis (52.0%),’ ‘acute condition not escalated appropriately by trainee physician (48.0%),’ ‘delayed correction of acidemia (48.0%),’ and ‘delayed intubation for respiratory failure (40%)’. The most commonly reported theme of preventability identified during panel case review (outside of the categories identified a priori) was anxiolytics/narcotics given for agitation ultimately related to clinical deterioration, which was identified in 5 (20.0%) arrests. See Fig. 2 for complete details.
Fig. 2 −.
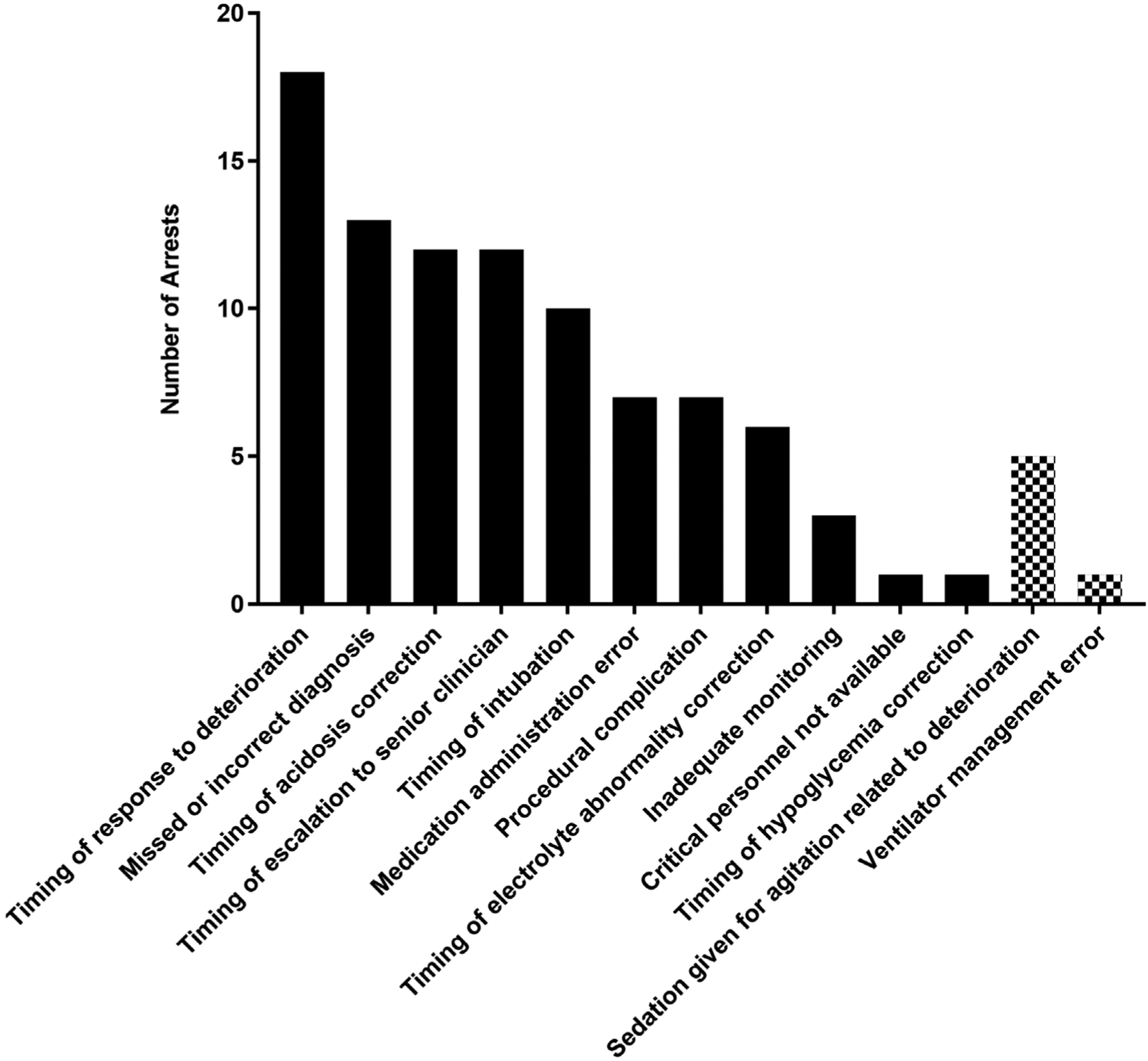
Themes of preventability as determined by the expert panel.
The number of arrests in which at least one expert review identified the contributor to arrest preventability. Only contributors identified in at least one arrest are included in this graph to allow for readability. Solid color bars represent a priori defined contributors and speckled bars represent novel contributors identified during expert review of the cases. Only ICU-CAs identified as at least ‘unlikely but potentially’ preventable are included.
Survey results
A total of 165 clinician surveys were sent with a median of 4 surveys per cardiac arrest. The overall response rate was 60.6%, with 28/43 (65.1%) attending physicians, 39/78 (50.0%) trainee physicians and APCs, and 33/44 (75.0%) of registered nurses responding.
In sum, 13 (30.2%) arrests were identified as unlikely but potentially preventable by at least half of the survey respondents for each case and 10 (23.3%) were identified as potentially preventable. ‘Delayed intubation for respiratory failure’ was the most commonly identified contributor to ICU-CA among those deemed at least unlikely but potentially preventable, occurring in 7 (30.4%) ICU-CAs. ‘Missed or incorrect diagnosis’ was identified in 4 (17.4%) arrests and ‘delayed response to clinical deterioration’ was identified in 3 (13.0%) arrests. Notably, a misalignment in team and patient/family goals of care or inadequate discussion of goals of care was identified in 4 (17.4%) arrests rated as at least ‘unlikely but potentially preventable.’
When asked ‘Did you observe/were you informed of any clinical changes preceding the cardiac arrest?,’ at least one survey respondent answered in the affirmative in 37/43 (86.1%) cases. Trainee physicians/APCs and nurses were each more likely to respond that they were aware of clinical changes prior to the ICU-CA as compared to attending physicians (71.7% vs. 73.5% vs. 44.4% respectively, p = 0.04). When asked ‘To the best of your memory, was the attending physician alerted to clinical decompensation prior to the cardiac arrest?” all survey respondents answered ‘yes’ in 16 (37.2%) cases and ‘no’ in 7 (16.3%) cases. In the remaining cases, there were mixed responses or some respondents were unsure.
Combined expert panel review and survey data
There was a strong, positive correlation between the median preventability scores for each arrest as determined by the expert panel and survey respondents (ρ = 0.60, p <0.001). Overall, 6 (14.0%) potentially preventable by both the expert panel and the survey respondents. Five (11.6%) ICU-CAs were identified as being potentially preventable by the expert panel but unlikely or not preventable by the survey respondents, and 4 (9.3%) were identified as being potentially preventable by the survey respondents only.
Discussion
In the present study, many ICU-CAs were identified by an expert panel and front-line providers to have had some opportunity for preventative action in the ICU, and a substantial proportion (>20%) were found to be potentially preventable had earlier or different action been taken in the ICU. In addition, a number of recurrent themes were identified in those ICU-CAs deemed to be potentially preventable including, ‘delayed response to clinical deterioration’ and ‘delayed intubation for respiratory failure’ among others. Some additional notable and modifiable practices that may contribute to preventable ICU-CAs included the administration of anxiolytics/narcotics in response to agitation related to unrecognized clinical decompensation and ambiguity or uncertainty regarding goals of care and whether the documented code status was considered appropriate for a given patient.
IHCA is a relatively common event with an increasing incidence in the United States.9 Despite improvements in resuscitation and post-arrest practices, IHCA outcomes remain poor with only a minority of IHCA victims surviving to hospital discharge.3 IHCA events also expose caregivers of victims to high levels of stress10 and may place other hospitalized patients at increased risk of clinical deterioration by diverting attention and other resources.11 As such, preventing unexpected death on the hospital ward has been a focus of numerous research and quality improvement efforts. These efforts have included (1) identifying patients at higher risk of decompensation, (2) expanded availability of physiologic monitoring, and (3) the development of rapid response systems to expedite the management of deteriorating patients.12 While these interventions have variably been shown to reduce unexpected death on hospital wards,12,13 research into the preventability of ICU-CAs has been far more limited.
In one prior retrospective cohort study at a tertiary care center in the United States, 104 IHCAs occurring over a 12 month period were identified.14 Of these, 30 occurred in an ICU setting with the remainder occurring on hospital wards. After review, the authors categorized 3 (10%) ICU-CAs as potentially preventable as compared to 21.6% of arrests occurring on hospital wards. Of those potentially preventable ICU-CAs, two were attributed to a failure to follow hospital guidelines/policies and one was attributed to delay in clinical care. Notably, the three preventable ICU-CAs were being managed on the cardiology, neurosurgery, and transplant surgery services with none on a primary intensivist service. Additionally, the authors only identified events for which a ‘code’ was called, thus some arrests that occurred in the ICU setting for which no ‘code’ was called may have been missed. In a second retrospective cohort review of IHCAs occurring over a one-year period in a United Kingdom hospital, 15 of 37 (40.5%) arrests in the critical care setting and 63 of 81 (77.8%) arrests in the non-critical care setting were identified as potentially preventable.15 While that study did not break out reasons for preventable arrest between critical care and non-critical care areas, the most common precipitants of potentially preventable arrests were inadequate response to new laboratory findings, delay by nursing in informing physicians, and delay by physicians in responding. Differences in rates of cardiac arrest preventability between the above two studies likely stems from differences in how preventability was defined and interpreted. Specifically, the former study defined preventability based on a stricter set of criteria whereas the latter study required only ‘suboptimal’ practice linked to the event.
Delays in the acute management of deteriorating patients were the most common contributors to preventability in the present study. In particular, delay in response to clinical deterioration, delay in acidosis correction, and delay in intubation were identified as contributors in a number of ICU-CAs. In review of these cases, intubation was often deferred as the patient was perceived to have adequate oxygenation/ventilation despite rapidly declining hemodynamic status and/or worsening metabolic acidosis. Earlier intubation of these patients, before they lose the ability to compensate for their physiologic derangement, may prevent some ICU-CAs. The expert review panel additionally identified a number of instances in which patient agitation or anxiety was treated with narcotics or anxiolytics alone, while the symptoms were in fact an early indicator of other clinical decompensation and may have been related to air hunger/hypoxemia. This observation suggests that patients with new agitation/anxiety in the ICU should be assessed for signs of hemodynamic instability or organ dysfunction prior to (or at least in conjunction with) the administration of anxiolytics or narcotics, although certainly these medications are sometimes necessary for patient comfort and safety.
Finally, it is worth highlighting that discordance between a patient’s documented goals-of-care and the perception of the appropriateness of those goals by the treating team may sometimes play a role in preventable ICU-CA. Patients in whom the goals-of-care are not well defined but appear to be moving towards a decision to forgo cardiopulmonary resuscitation may be in a dangerous grey zone, where providers may delay aggressive or invasive therapies while discussions are ongoing and thereby increase the likelihood of cardiac arrest necessitating resuscitation. Although in many of these cases, forgoing aggressive interventions may be in the patient’s best interest, the misalignment in goals-of-care may need to be addressed by earlier conversations about prognosis and feasible goals between clinicians, patients, and families so as to avoid a situation in which intubation is delayed but cardiopulmonary resuscitation is provided after an arrest.
In this cohort of ICU-CAs, bedside nurses and trainee physicians/APCs were equally likely to report awareness of a patient’s clinical decompensation prior to ICU-CA. Attending physicians, in contrast, were significantly less likely to report being aware of that decompensation. In review of these cases, the expert panel found that failure to alert the attending physician to patient decompensation contributed to some of the delays in care escalation described in the preceding paragraph, highlighting one area where team communication may be improved. It is additionally notable that preventable arrests were more likely to occur early in a patient’s ICU course—when patients are acutely ill and less well known to clinical teams. We speculate that timely communication and response to clinical deterioration may be the most impactful when applied during this critical period.
The strengths of this study include its prospective design and the incorporation of both expert review and front-line clinician experience into the preventability assessment for ICU-CA. The prospective nature of the study ensured complete capture of all ICU-CA’s occurring during the study period and allowed expert reviewers to assess data in real-time without reliance on archived data sources (which often lose some granularity in the archiving process). Drawing on the combined experience of independent expert reviewers and front-line clinical providers (including trainee and attending physicians, APCs, and nurses) allowed the investigators to obtain a more complete understanding of the events surrounding each ICU-CA.
This study also had a number of limitations. First, the agreement amongst expert reviewers regarding ICU-CA preventability was only ‘fair’, which speaks to the difficulty and subjectivity of assessing cardiac arrest preventability. Notably, other studies assessing cardiac arrest or death preventability in critically ill populations have also struggled with below optimal rates of agreement amongst reviewers.16,17 Experts were also generally not involved in the direct care of the ICU-CA patients and nuances of clinical decision making may have been missed. An additional limitation is that the number of survey respondents varied across ICU-CAs, with some surveys having only a single respondent. Further, we included only cases in this study where ICU-CA occurred. There may be a number of cases in which the same themes (e.g. delayed intubation) would be identified but without a consequent ICU-CA. Finally, the single-center design of this study limits generalizability to other hospital systems.
Overall, our results highlight that many ICU-CAs have potentially preventable elements and that recurring themes of preventability can be identified. These results run counter to the paradigm that critically ill patients are closely monitored and therefore ICU-CAs are generally not preventable. We have begun work to address these themes of preventability through an educational initiative and an ICU based clinical trigger-and-decision aid program. Future work should assess the generalizability of the themes identified in this study at other institutions and explore ways to reduce the incidence of preventable ICU-CA across other centers.
Conclusions
Cardiac arrests which occur in the ICU, despite intensive monitoring and staffing, may have elements of potential preventability. Consideration of these themes may help identify opportunities for interventions to avoid cardiac arrest.
Supplementary Material
Funding sources
The overall project was funded by a grant from the Controlled Risk Insurance Company (CRICO). Dr. Moskowitz and Dr. Berg are additionally funded through NIH grants K23GM128005-1 and K23 HL128814-03, respectively. Dr. Grossestreuer receives support from Harvard Catalyst I The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541) and financial contributions from Harvard University and its affiliated academic healthcare centers. Dr. Donnino is funded by grant 1R01HL36705-1 and 1K24HL127101-01.
Footnotes
Disclosures
None
Conflicts of interest
The authors have no conflicts of interest to report.
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.resuscitation.2019.09.003.
REFERENCES
- 1.Go AS, Mozaffarian D, Roger VL, et al. Executive summary: heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 2013;127:143–52. [DOI] [PubMed] [Google Scholar]
- 2.Andersen LW, Holmberg MJ, Berg KM, et al. In-hospital cardiac arrest: a review. JAMA 2019;321:1200–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Girotra S, Nallamothu BK, Spertus JA, et al. Trends in survival after in-hospital cardiac arrest. N Engl J Med 2012;367:1912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perman SM, Stanton E, Soar J, et al. Location of in-hospital cardiac arrest in the United States-variability in event rate and outcomes. J Am Heart Assoc 2016. 5:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Efendijev I, Nurmi J, Castrén M, et al. Incidence and outcome from adult cardiac arrest occurring in the intensive care unit: a systematic review of the literature. Resuscitation 2014;85:472–9. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong RA, Kane C, Oglesby F, et al. The incidence of cardiac arrest in the intensive care unit: a systematic review and meta-analysis. J Intensive Care Soc 2018. 20: 175114371877471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- 9.Holmberg Mathias J, Catherine R, Chan Paul S, et al. Abstract 23: incidence of adult in-hospital cardiac arrest in the United States. Circulation 2018;138:A23 [Cited 2019 Feb 26] Available from: 10.1161/circ.138.suppl_2.23. [DOI] [Google Scholar]
- 10.Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med 2013;368:1008–18. [DOI] [PubMed] [Google Scholar]
- 11.Volchenboum SL, Mayampurath A, Göksu-Gürsoy G, et al. Association between in-hospital critical illness events and outcomes in patients on the same ward. JAMA 2016;316:2674–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan PS, Jain R, Nallmothu BK, et al. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med 2010;170:18–26. [DOI] [PubMed] [Google Scholar]
- 13.Howell MD, Ngo L, Folcarelli P, et al. Sustained effectiveness of a primary-team-based rapid response system. Crit Care Med 2012;40:2562–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galhotra S, DeVita MA, Simmons RL, et al. Mature rapid response system and potentially avoidable cardiopulmonary arrests in hospital. Qual Saf Health Care 2007;16:260–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation 2002;54:115–23. [DOI] [PubMed] [Google Scholar]
- 16.Rhee C, Jones TM, Hamad Y, et al. Prevalence, underlying causes, and preventability of sepsis-associated mortality in US acute care hospitals. JAMA Netw Open 2019;2:e187571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parshuram CS, Dryden-Palmer K, Farrell C, et al. Effect of a pediatric early warning system on all-cause mortality in hospitalized pediatric patients: the EPOCH randomized clinical trial. JAMA 2018;319:1002–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


