Abstract
Background
Traditional medicine serves as a form of primary health care for more than 80% of African populations. Currently, there is no research documenting if and how African migrant communities engage with their traditional health practices and beliefs after they resettle in Western countries. The aim of this study was to examine African migrant women’s experiences and perspectives about traditional and complementary medicine use in relation to their maternal health and wellbeing in Australia.
Methods
We conducted a mixed method study between December 2016 and October 2017. Questionnaires were completed by 319 women and 15 in-depth interviews were conducted among African migrant women residing across the Sydney metropolitan area, Australia. Survey data were analysed using SPSS (version 23) and logistic regression model was used to test associations. Qualitative data were analysed thematically using NVivo 11 software to identify themes and conceptual categories in the participants’ responses. The study was informed by Andersen’s Socio-behavioural model of health service utilisation.
Results
The findings indicated that use of traditional and complementary medicine was high and continued to be well used following African women’s resettlement in Australia. The survey found that 232 (72.7%) women use some form of traditional and complementary medicine for maternal health and wellbeing purposes. Most women (179, 77.2%) reported that maintaining their maternal health and wellbeing was the most common reason for use. The interview findings indicated that access to traditional medicine included making requests from relatives and friends who travelled to Africa looking for a similar medicinal plant in Australia and preparing home remedies with advice from family members and healers back in Africa. Age ≥ 35 years (OR, 16.5; 95%CI, 6.58–41.5; p < 0.001), lower education (OR, 24; 95%CI, 8.18–71.1; p < 0.001), parity (OR, 7.3; 95%CI, 1.22–42.81; p = 0.029), and lower income (OR, 2.7; 95%CI, 1.23–5.83; p = 0.013) were strong predictors of traditional medicine use.
Conclusion
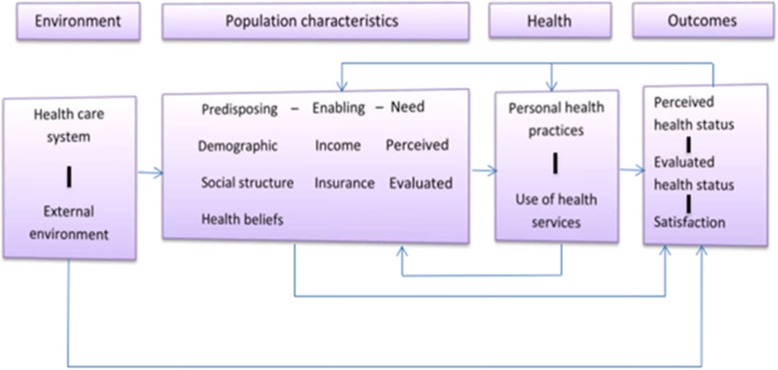
Use of traditional and complementary medicine among African migrant women in Sydney remained high following resettlement in Australia. As noted in Andersen’s sociobehavioural model of health service utilisation, specific predisposing and enabling factors including age, education and income were associated with use of traditional and complementary medicine.
Keywords: Traditional medicine, Complementary and alternative medicine, Maternal wellbeing, African migrant women, Australia
Background
Australia has a growing and diverse African community [1]. The 2011 census data showed that there were close to 340,000 people of African descent living in Australia [1]. This number increased to around 390,000 African migrants in the 2016 Census. While the vast majority of Africans come to Australia as skilled migrants there is also a significant increase in arrivals from refugee countries such Ethiopia, Eritrea, Democratic Republic of Congo and Somalia [1]. In general, the state of New South Wales (NSW) has the largest number of permanent settler arrivals with 30% of the national total between 2006 and 2011 and approximately 40% of all humanitarian entrants [2, 3]. According to the 2016 census there were 86,410 African migrants.
Traditional medicine plays a crucial role for 70–90% of the African population as a primary health care option [4]. The practice of traditional medicine in Africa is a method of healing founded on its own concept of indigenous knowledge systems that developed over a long period of time within various societies [4]. Being practiced for countless generations well before the introduction of Western medical care, traditional medicine is culturally valued and accepted by most African communities [5–7]. Studies have shown that women in Africa extensively depend on cultural health practices for their maternal health and wellbeing [8, 9].
Australia has universal healthcare, including maternal services, with a public health insurance system, Medicare. Medicare provides treatment free of charge in public hospitals and subsidies the cost of out-of hospital treatment. The out-of-hospital treatment component of Medicare provides a rebate benefit for services, based on a proportion of a schedule of fees covering each type of service [10]. Although, conventional maternal healthcare is accessible in Australia, it is not clear if the widespread use of traditional medicine in Africa also continues following re-location in Australia among African migrant women [8]. As such, the present study examines the use of traditional and complementary medicine for maternal health and wellbeing among African migrant women in Australia. More specifically, the study seeks to determine the type of traditional and complementary medicine use, reasons and sources for use, and socio-demographic predictors of use of these therapies. Findings from this study will provide the opportunity to increase the knowledge and awareness of health professionals about the cultural health practices and beliefs of African migrant women in Australia. This will facilitate provision of culturally sensitive and responsive health services when caring for African migrant women by taking into account their cultural health practices and beliefs.
As defined by the World Health Organization [11], traditional medicine in this study refers to “the sum total of the knowledge, skills and practices based on the theories, beliefs and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health, as well as in the prevention, diagnosis, improvement or treatment of physical and mental illnesses”. Similarly, this study adopted the National Centre for Complementary and Integrative Medicine (NCCIM) definition for complementary and alternative medicine which states” group of diverse medical and health care systems, practices, and products that are not generally considered part of conventional medicine” [12].
Theoretical framework
To understand factors that motivate the use of traditional and complementary medicine among African migrants, the Andersen’s sociobehavioural model of health service utilization was used [13]. It posits that health service utilisation depends on three core components which include: predisposing characteristics, enabling resources, and need factors. This theoretical framework also effectively integrates different factors which may influence the use of traditional and complementary medicine (Fig. 1). For instance, predisposing factors such as socio-demographic characteristics (e.g. age, gender, and education), knowledge, perceptions and attitudes, and race/ethnicity have been indicated to influence traditional and complementary medicine use [14–16]. Likewise, enabling factors such as income, insurance, access to and cost of conventional care have been shown to determine the use of traditional and complementary medicine [17, 18]. The need factors have also been consistently found to influence traditional and complementary medicine use based on previous studies [19, 20]. While human behaviors are complex, this model provides a comprehensive framework to describe health behaviors leading to utilization of traditional and complementary therapies.
Fig. 1.
Core components of health seeking behaviour (Andersen, 1995, p. 8)
Methods
Study design
A sequential explanatory mixed method study was undertaken from December 2016 to October 2017. Creswell and Creswell state that “explanatory sequential mixed methods is one in which the researcher first conducts quantitative research, analyzes the results and then builds on the results to explain them in more detail with qualitative research” [21]. This type of design is popular in fields with a strong quantitative orientation in which the initial quantitative results need to be explained further with the qualitative data [21]. In this study, data was collected sequentially with the survey results informing the development of the individual interview protocol. The survey examined the pattern of maternal traditional and complementary medicine use by African migrant women and the qualitative phase explored women’s experiences and perspectives about traditional and complementary medicine use in relation to their maternal health and wellbeing.
Study participants
African migrant women residing across the Sydney metropolitan area were invited to participate in this study. Inclusion criteria were: born in Africa, aged ≥18 years, speak English, and had been a resident in Australia for at least 12 months. In addition, women were required to satisfy at least one of the following criteria: planning a pregnancy, attempted to conceive, have ever been pregnant, or had children. Women who were in Australia on short term work or holiday visas were excluded. In addition, women who nominated their willingness during the survey to participate in the interviews were purposively selected based on their experience of using traditional and complementary medicine for maternal health and wellbeing.
A verbal informed consent was obtained from all women who participated in the study. As the data collection involved online and telephone approaches, obtaining written consent was not possible. Ethical approval was received from Western Sydney University Human Research Ethics Committee (ref: H1196).
Sampling strategy
A homogenous convenience sample of 319 Black African migrant women were included in the survey. According to Jager et al., (2017) one way to minimize the disadvantages of nonprobability sampling (lack of clearer generalisability) is through the strategic use of homogenous convenience samples (e.g. Black or White, male or females). Using this approach, the target population (not just the sample studied) was a specific sociodemographic subgroup.
When survey participants completed the questionnaires, they were invited to voluntarily nominate their willingness to be contacted for individual interviews. In addition to the inclusion criteria outlined under the survey, interview participants were selected purposively based on their experience of traditional and complementary medicine use for maternal health and wellbeing. Fifteen eligible women were interviewed. After 13 interviews, no new themes emerged which indicated saturation was achieved. In qualitative interviews, saturation occurs when no new or relevant data seems to emerge regarding the research objectives [22].
Study promotion and recruitment procedures
The study was promoted through community consultations and networking with community associations, multicultural organisations, churches, and business firms which were affiliated with the African communities in Sydney. The study was advertised through posters and flyers displayed in prominent places including; shopping centers, train and bus stations, entertainment places, University and College campuses, restaurants, cafes, and African hair salons. For women expressing interest in the study a link to the online survey was sent through email, text messages and social media (Facebook, WhatsApp, and Viber). Optionally, paper-based questionnaires were hand delivered to individuals attending the organisations. Questionnaires were returned to the researchers using reply-paid and addressed envelopes.
Data collection and measures
Surveys
Survey data were collected by using self-completed questionnaires (supplementary file 1). In addition, some participants completed an investigator administered questionnaires through face-to-face and over the phone [23]. Currently there are no standardised survey tools suitable to assess the use of traditional medicine among African migrant communities in Western countries. Therefore, the present study was based on a new survey tool developed by the authors from a comprehensive literature review. A researcher who develops a new measure should establish that it has “face validity” as a minimum requirement and that the new measure apparently reflects the content of the concept in question [24]. As an essentially intuitive process, the face validity of this study was ensured by using a mixed methods sequential explanatory design which allowed triangulation of quantitative and qualitative data on the same topic. The use of a mixed methods approach assured validating the survey findings through semi-structured in-depth interviews [25]. In addition, a pilot test performed before the main study ensured the face validity of the survey questionnaire.
The survey explored socio-demographic characteristics including age, marital status, pregnancy and birth, income, education and employment status, religion, and country of origin were collected using both open and closed questions. The survey also explored patterns of traditional and complementary medicine use in Australia relating to maternal health and wellbeing. Women were asked about the traditional and complementary health practices they used in Australia. A list of common traditional health practices was provided along with open-ended questions to facilitate participant recall. The survey also include question on specific maternal health related reasons for use of traditional medicine from preconception through to pregnancy and postnatal periods. A pilot test of the survey was undertaken to examine face validity. The pilot was carried out among eight African-born women. Following the pilot study, several modifications were made including revising terms to improve the readability of the questionnaire.
Interviews
The development of the interview guide was informed by the preliminary analysis of the survey data to women’s experience of using traditional and complementary medicine for maternal health and wellbeing. Data for the interviews was collected using a digital audio-recorder and notes were taken by the researcher during and immediately following the interview. Interviews lasted between 40 and 80 min. All audio-recorded interviews were transcribed in full. The first interview was transcribed by the researcher and subsequent audio-recorded interviews were transcribed verbatim by a transcription company (https://www.pacifictranscription.com.au/). The interview explored in more detail women’s experiences and perceptions of using traditional medicine during preconception, pregnancy, and/or postnatal periods (supplementary file 2). Interview results were presented by way of pseudonyms.
Data analysis
Survey data was checked for consistency, coded appropriately, and entered into SPSS software package version 23. Descriptive analysis using frequencies and proportions was conducted to describe the sample characteristics and distribution of variables. The relationship between traditional medicine use and independent factors was examined using binary logistic regression model. For all significance tests a p-value of 0.05 or less and a 95% confidence interval were used. Bivariate logistic analysis was initially conducted with potential predictor variables to establish their association with use of traditional medicine. Following the bivariate analysis, multivariate logistic regression analysis was conducted to control for possible confounding variables and to compute the adjusted odds ratios (OR) for the explanatory variable. All variables with a p-value of less or equal to 0.25 were selected and entered simultaneously into a logistic regression model because the traditional level of 0.05 can fail to identify important variables [26]. A stepwise backward elimination method was employed to eventually produce the most parsimonious model. In backward elimination method, variables with greater p-value were sequentially eliminated until all variables in the model were p < 0.05 [27].
Qualitative data were analysed thematically using NVivo 11 software program [28] to identify themes, conceptual categories, commonalities and differences in the participants’ responses. The analysis was started by listening to the recoded audio and reading and re-reading the transcripts several times [29]. This process of familiarisation or immersion into the data helped the researcher to reflect on the entirety of the data and better understand and interpret the women’s views about traditional medicine. The next step was generating codes and using NVivo 11 to produce a concise matrix of key emerging ideas. Finally, a coding summary and report was produced with the sub-themes that make meaningful contributions to answering the research questions. The first author conducted the data analysis and generated the summary codes. The second and third authors reviewed the interview transcripts, the coding summary and provided feedback for revisions to coding framework which were then incorporated into the qualitative data analysis by the first author. Names have been changed to protect the identity of women.
Results
A total 634 survey questionnaires were distributed and 348 (54.9%) surveys were returned (205 online and 143 paper-based). Twenty-nine questionnaires (25 online and 4 paper-based) had significant missing data due to unanswered questions and were disregarded. A total of 319 completed survey questionnaires were analysed.
A sub-sample of 15 women who nominated their interest during the survey completed one-to-one interviews. Eleven interviews took place over the phone and four were undertaken face-to-face. After 13 interviews, no new themes emerged which indicated that saturation was achieved.
Socio-demographics of participants
Forty-three nations in Africa were represented in this study. One hundred and thirty-one women (41.1%) were aged between 25 and 34 years (Table 1). Two hundred and forty two (75.8%) of the participants were currently employed. The majority of women (208, 65.2%) reported annual household income of less than 50,000 (AUD$). Many of the women were married (203, 63.6%). Overall, 235 (73.7%) and 225 (70.5%) participants had been pregnant at least once and had at least one child respectively.
Table 1.
Demographic characteristics of survey participants
| Characteristics | N (%) | |
|---|---|---|
| Age | 18–24 years | 25 (7.8) |
| 25–34 years | 131 (41.1) | |
| 35–44 years | 115 (36.1) | |
| 45–54 years | 34 (10.7) | |
| 55 or older | 14 (4.1) | |
| Annual household income (AUS$) | 0–24,000 | 96 (30.1) |
| 25,000-49,999 | 112 (35.1) | |
| 50.000–74,999 | 65 (20.4) | |
| 75,000-99,999 | 25 (7.8) | |
| 100,000 or above | 21 (6.6) | |
| Marital status | Married or living together | 203 (63.6) |
| Single | 82 (25.7) | |
| Divorce/Separated/widowed | 34 (10.7) | |
| Gravidity | Never been pregnant | 84 (26.3) |
| Has been pregnant at least once | 235 (73.7) | |
| Parity | No children | 94 (29.5) |
| Have at least one child | 225 (70.5) | |
| Education status | Less than high school | 6 (1.9) |
| High School graduate | 33 (10.3) | |
| Certificate or diploma level | 127 (39.8) | |
| University degree | 117 (36.7) | |
| Postgraduate degree | 36 (11.3) | |
| Employment status | Unemployed | 27 (8.5) |
| Full time | 99 (31) | |
| part time | 143 (44.8) | |
| self employed | 25 (7.9) | |
| other | 25 (7.8) | |
| Religion | African Traditional | 14 (4.4) |
| Christian | 203 (63.6) | |
| Muslim | 97 (30.4) | |
| Others | 5 (1.6) | |
Women in the interview also had diverse backgrounds from different regions in Africa, such as Nigeria, Cameroon, and Sierra Leone, in West Africa; Ethiopia, and Tanzania in East Africa; Rwanda and Gabon in Central Africa; Sudan in Northern Africa; and Zimbabwe in Southern Africa (Table 2). The majority of participants had arrived to Australia on Family Visas.
Table 2.
Characteristics of interview participants
| S. no | Name | Education | Age at arrival in Australia | Length of time in Australia, in year | Number of children | Religion | Visa type on entry | English proficiency (Self rated) |
|---|---|---|---|---|---|---|---|---|
| 1 | Fiona | Secondary school | 38 | 21 | 3 | Christian | Humanitarian /Refugee | Good |
| 2 | Zena | University degree | 30 | 32 | 3 | Catholic | Humanitarian /Refugee | Excellent |
| 3 | Soy | Postgraduate degree | 38 | 8 | 3 | African traditional | Skilled/work | Good |
| 4 | Sim | University degree | 22 | 11 | 2 | Christian | Family/partner | Good |
| 5 | Anna | University degree | 32 | 10 | 1 | Christian | Humanitarian /Refugee | Excellent |
| 6 | Tia | Postgraduate degree | 26 | 2 | 2 | Christian | Student | Good |
| 7 | Mary | Diploma | 18 | 30 | 4 | Christian | Humanitarian /Refugee | Excellent |
| 8 | Eva | University degree | 26 | 2 | 1 | Christian | Student | Fluent |
| 9 | Saly | University degree | 26 | 22 | 2 | Christian | Family/partner | Excellent |
| 10 | Hiva | University degree | 19 | 11 | 1 | Christian | Family/partner | Excellent |
| 11 | Ney | Postgraduate degree | 10 | 20 | 0 | Christian | Family/partner | Fluent |
| 12 | Mire | University degree | 23 | 2 | 0 | Christian | Skilled/work | Good |
| 13 | Lita | Certificate | 32 | 3 | 2 | Christian | Family/partner | Excellent |
| 14 | Jay | Postgraduate degree | 10 | 16 | 0 | Christian | Student | Good |
| 15 | Ema | University degree | 20 | 5 | 2 | Muslim | Family/partner | Good |
Patterns of traditional and complementary medicine use
Use of traditional or complementary medicines was high with 232 (72.7%) women using some form of traditional or complementary medicine (Table 3). The most frequently used traditional or complementary medicine products and services were herbal medicine (163, 61.7%), prayer for health (146, 55.3%), vitamins (88, 33.3%), massage (87, 33%), and faith healer services (81, 30.9%).
Table 3.
Common forms of traditional and complementary medicines used by African migrant women
| Types of traditional or complementary medicine used | n (%) |
|---|---|
| Any type of complementary or traditional medicine | 232 (72.7) |
| Herbal medicine | 163 (61.7) |
| Prayer for health | 146 (55.3) |
| Vitamins | 88 (33.3) |
| Massage | 87 (33.0) |
| Faith healer | 81 (30.9) |
| Traditional Chinese Medicine | 72 (27.3) |
| Chiropractic | 30 (11.4) |
| minerals | 25 (9.5) |
| Antioxidants | 21 (8.0) |
| Yoga | 18 (6.8) |
| Meditation | 23 (8.7) |
| Diet therapy | 19 (7.2%) |
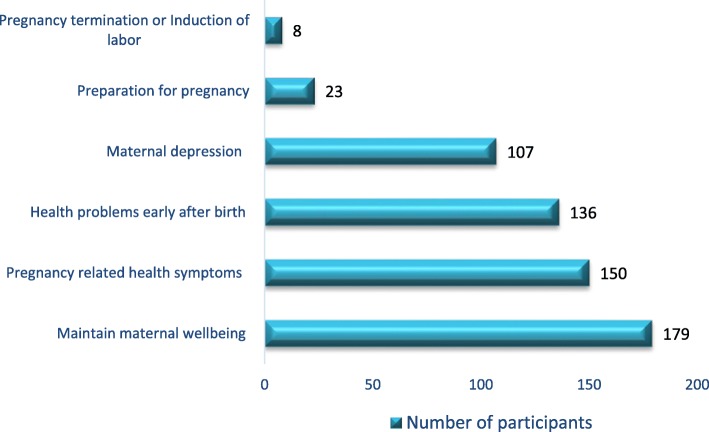
Reasons for use of traditional or complementary medicine
The majority of women identified maintaining their wellbeing was the most common reason for using traditional or complementary medicine prior to conception, during pregnancy and the postnatal period (179, 77.2%). The other common reasons reported by the participants were pregnancy related symptoms (150, 64.7%) (Fig. 2).
Fig. 2.
Maternal health related reasons for use of traditional and complementary medicine among African migrant women
Interview participants confirmed these survey findings. In one interview, for example, Ema commented, “I have used various traditional medicines, depending on the circumstance. Not necessarily because I am sick, but also as a prevention strategy and for wellbeing.” For some participants, using these practices was perceived as a balancing mechanism to the modern-day lifestyle in which more unhealthy foods were consumed with less physical exercise.
The modern lifestyle here is like no exercise, junk foods and all artificial products. So I am more conscious with which health choice I should make this time. My African knowledge about this traditional medicine helps me a lot (Ema).
Another reason for using traditional and complementary medicine related to specific maternal health conditions. For instance, many participants indicated that they used different forms of traditional medicine to prevent and treat nausea and vomiting in the first trimester of their pregnancy. According to Tia,
I normally used homemade remedies like I put some honey with my tea; and especially when I was pregnant I was using lemon with water, because during first trimester pregnancy, you know, there is nausea and vomiting (Tia).
Ema also mentioned, “I used herbal stuffs during my pregnancy because I have sort of nausea and vomiting.” The use of traditional and complementary medicine was also indicated for losing weight during pregnancy. Hiva, a mother of two stated, “I do use herbal things like herbal tea. Herbal tea and also other herbal products that make you lose weight during pregnancy.”
During the postnatal period, use of traditional medicine was reported for a number of specific reasons. For instance, respondents indicated that traditional medicine was believed to restore a woman’s pre-pregnancy body shape and strength after giving birth.
It's well known that when a woman has a baby, she needs to go through this process [hot water bath using herbal fragrances] to get back her body in the sense of mobility, flexibility, prevent the soreness and disease (Soy).
According to Sim, “soon after giving birth, it [traditional medicine] was believed it would help me to get stronger and be able to get back to normal shape.” Ema explained, “after giving birth I was not strong for a long time and that’s why I was depending on traditional medicine.” Women also reported that they used herbal medicine for increasing breast milk production. For example, Ema said, “that food cooked with herbs was good for me to produce more milk.”
Some participants reported that they used traditional and complementary medicine to help them prepare for pregnancy or to enhance the chance of conception.
Even before my pregnancy I used these herbs, but I don't remember the name, but my mum recommends me to increase the chance of fertility. Because I have a delayed pregnancy for three or four years after marriage. So I always took herbs with food that my mother cooks. She also has some special foods mixed with different herbs and spices that she gives me to become pregnant (Ema).
Sources of information about traditional medicine
To provide more insight into who provided the information and how it influenced use of traditional and complementary medicine, the participants were asked during the interviews about accessing their culture specific traditional therapies and the process of knowledge acquisition related to traditional medicine in their respective cultures. In response, many women discussed that the information or knowledge about traditional medicine was handed down through their families to maintain good health and to treat illnesses.
For example, Ney stated that her main source of knowledge about traditional medicine was from her close family members.
I grew up with somebody [her mother] who is very much who looks outside of western medicine. Through my mum's influence I always seek alternative ways of looking after my health. I've always sought to use certain herbal soups, or probiotics (Ney).
The knowledge or information about use of traditional medicine for maternal health purposes was also learnt from mothers or grandmothers. In her comment on how she learned about traditional medicine from her mother, Sim remarked:
It's like, when I got pregnant, when I gave birth, my mum told me, oh this will help you to get this or that- so I think that's how it gets passed on. She probably got it from her mum and her mum got it from her mum. So, I'd probably say the same thing to my daughter. I think it was passed on This is how I had traditional medicine and it helped me. So probably maybe generation to generation I think (Sim).
For some participants, traditional medicine was accepted because of their families prior practice or use. The most important thing in this case was not the effectiveness, but rather the belief and trust the family held towards traditional medicine.
I just have, you know, there are times we say traditional medicines are just believing. So I have been used to drinking this bitter root they call bamba in my language, so we've been used to drinking it in the morning. My mother used to soak it. Sometimes she boils it and then give it to us. I don't really go, we don't really go to any other traditional healers or whatever it is. We just believe in drinking that thing that my mother gives me (Fiona).
Anna recalled how she was excited when her husband told her that the traditional medicine which she used to use it in Africa was also available in Australia. “So when I came here, it was just - when my husband told me about he found this tree here, it was just a continuation. I just drink.” Some participants also reported that their African friends were an important source of information about traditional or complementary medicine in Australia.
I have a lot of friends who are just very much in this alternative way of living, sort of modern day hippies, and then somebody said, oh try this, try this. It's your root so why don't you just try and release whatever it is that you're hanging on. Look, I don't know if it worked or not. I don't know if it was the placebo, but I just remember that I took her advice and I tried different traditional medicine (Ney).
I can get the information from my friends here, from relatives, even sometimes I call my mum back home to tell me what to use for such and such problems and she will teach me how to prepare that [traditional medicine] (Ema).
A participant indicated that she accesses specific herbal products sent directly from Africa or through sharing from friends and relatives.
Well I have a habit of asking my mother to send me some plant medicine powder that she got from local healers. Whenever, some friends go back to Africa for a holiday, I will ask them to bring that for me. Sometimes I also ask relatives and friends to share with me if they have one, usually these African herbal medicines good for many illnesses but I don’t remember the name of the plant (Mire).
Socio-demographic predictors of traditional and complementary medicine use
A multivariate logistic regression analysis was undertaken to determine the predictive factors of traditional and complementary medicine use (Table 4). Older women (≥ 35 years) were 16.5 times more likely to use these practices for maternal wellbeing than women aged < 35 years (p < 0.001). Women with lower income and educational level were 2.7 and 24.0 times more likely to use traditional and complementary medicine for their maternal wellbeing compared to those with higher income (p = 0.013) and educational status (p < 0.001) respectively. Primiparous women were 7.3 times more likely to use these practices for maternal wellbeing compared to nulliparous women (p = 0.029).
Table 4.
Sociodemographic predictors of traditional and complementary medicine use for maternal wellbeing among African migrant women after resettlement in Australia
| Factors | Total (n = 319) |
Use of traditional and complementary medicine for maternal wellbeing | OR | 95%CI | P-value | ||
|---|---|---|---|---|---|---|---|
| Yes (n = 232) | No (n = 87) | ||||||
| Age | < 35 years | 156 (48.9%) | 77 (33.2%) | 79 (90.8%) | - | - | - |
| ≥ 35 years | 163 (51.1%) | 155 (68.8%) | 8 (9.2%) | 16.5 | 6.58–41.51 | < 0.001 | |
| Household income (AUS$) | < 50,000 | 208 (65.2%) | 175 (75.4%) | 33 (37.9%) | 2.7 | 1.23–5.83 | 0.013 |
| ≥50,000 | 111 (34.8%) | 57 (24.6%) | 54 (62.1%) | - | - | - | |
| Marital status | Single or separated | 116 (36.4%) | 71(30.6%) | 45(51.7%) | - | - | - |
| Married | 203 (63.6%) | 161 (69.4) | 42 (48.3%) | ||||
| Gravidity | Never been pregnant | 84 (26.3%) | 47 (20.3%) | 37 (42.5%) | - | - | - |
| Has been pregnant at least once | 235 (73.7%) | 185 (79.7%) | 50 (57.5%) | ||||
| Parity | No children | 94 (29.5%) | 49 (21.1%) | 45 (51.7%) | 1 | - | - |
| Have at least one child | 225 (70.5%) | 183 (78.9%) | 42 (48.3%) | 7.3 | 1.22–42.81 | 0.029 | |
| Education status | Certificate or below | 166 (52%) | 161 (69.4%) | 5 (5.7%) | 24.1 | 8.18–71.1 | < 0.001 |
| Diploma or above | 153 (48%) | 71 (30.6%) | 82 (94.3%) | - | - | - | |
Discussion
Currently, research on African migrants’ traditional health practices and how this may influence their health-seeking behaviour in Western countries is limited. This is the first mixed methods study which generated a comprehensive understanding of the cultural health practices and beliefs of African migrant women in Australia. Triangulation largely resulted in consistency across the survey and interview findings and increased the trustworthiness and validity of the conclusion form this study.
The findings indicated that use of traditional and complementary medicine among African migrant women was high and continued use following migration. Being practiced for countless generations even well before the introduction of Western medical care, traditional medicine is highly valued and culturally accepted by most African communities [5–7]. As such, the findings in this study might be a reflection that African migrant women in Australia continue their cultural health practices because of their health and illness beliefs, cultural acceptance, and concept of holistic health related to traditional medicine.
This study’s findings demonstrated that herbal medicine was the most common form of traditional medicine used by African migrant women. Respondents indicated that the knowledge and experience of gathering and preparation of herbal medicines was a common practice in their families in Africa. The result of this study may suggest the pre-migration experience of African women played a significant role in continuing use of herbal medicine in Australia.
Our study found that spiritual healing (prayer for health purposes with or without consulting faith healers) were commonly utilised by African migrant women. Previous studies also identified that the practice of prayer for health was common among migrant African communities [30–33]. Brown et al., (2007) found that prayer was the most common traditional health practice among African Americans compared to other minority groups [33]. A study reviewing the influence of spiritual beliefs and practices on the treatment preferences of African Americans indicated that spirituality is an important part of African-American culture and spiritual beliefs are important in understanding and coping with illness and provided a framework within which treatment decisions are made [31]. In another study, African Americans held beliefs that consider prayer as the most important part of their health care and influences their medication decisions [34]. In addition, African Americans were more likely to believe that the power of spirituality and prayer promotes healing and treatment of active health complaints than other minority groups [35–39]. Similarly, the present study findings have shown that prayer was used not only for religious purposes but also as part of maintaining the general wellbeing and treatment of specific maternal health complaints.
This study also found that that African migrant women report the use of complementary therapies which were not common in Africa but are widely used in the Australian population. Use of these modalities included vitamin/minerals, massage, and chiropractic, and traditional Chinese medicine. As such, the present finding may suggest that African migrant women are open to explore and experience complementary therapies outside of their culturally specific health practices. Perhaps, this might also be an attempt to substitute their cultural health practices that they were unable to easily access in Australia. Study findings indicated that services from traditional birth attendants, bone setters, and diviners were common practices women utilised while they were in Africa but least mentioned after their resettlement to Australia. On the other hand, this finding may indicate that African migrant women also hold similar views with Australia complementary medicine users. For example, some of these views including the perception of complementary medicine as holistic, preventive, safe and that complementary medicine practitioners are more supportive towards their health compared to other health professionals were also identified among the general Australian population [40].
Many women in the study identified that maintenance of their maternal wellbeing was the most common reason for use of traditional and complementary medicine. This study also found that treatment of specific maternal health complaints during antenatal and postnatal periods were also a common reason for use of traditional medicine. Previous studies also revealed that African women who have health complaints during pregnancy or after birth were more proactive about their health and were accessing a broader range of traditional and complementary therapies [8, 41]. This use could start from the preparation phase for pregnancy through to the antenatal and postnatal periods. Some women reported that the use of traditional and complementary medicine was associated with the perception that it increases immunity. Similarly, traditional medicine was often perceived as a better preventive strategy and regarded as more natural, safe, and/or having at least equal efficacy when compared with medical prescriptions for maternal wellbeing among African women in Africa [42, 43]. As such, the present finding may suggest that previous perceptions among African migrant women were important to continued us of traditional medicine because they believed that it has a medicinal value which was important to protect their general wellbeing.
The present study identified that African migrant women use various approaches to access their cultural traditional medicines in Australia. These sources included sharing from relatives and friends who recently traveled to Africa and brought back some traditional medicines, looking for a similar medicinal plant in Australia, and preparing home remedies with advices from family members and healers back in Africa. This finding was similar to research with other migrant groups which highlighted that migrant communities may depend on family members and traditional healers who came from their own country of origin to access their cultural health practices. Mexican migrants in US rely heavily on transnational networks to meet their health care needs [44]. According to the study, through their close family recommendations, Mexican migrants were able to address their health care needs in a way that is culturally appropriate to them by involving family, friends, other migrants, parcel services, long distance calling booths, and ethnic shops to access culture specific traditional medicine. However, participants in the present study identified that across many African migrant communities in Australia there were no traditional practitioners (except faith healers) who were themselves African migrants.
As noted in the Anderson’s sociobehaviour model of health service utilisation, specific predisposing and enabling factors including age, education and income were associated with use of traditional and complementary medicine. Our analysis found that lower educational level was significantly correlated with increased traditional and complementary medicine use for maternal health and wellbeing. Similar to this finding, other studies have also reported that African women who use traditional medicine were more likely to be less educated [45, 46]. Increased use of traditional medicine among the less educated group in this study could be partly explained by the fact that lower education may limit African women’s knowledge about available healthcare options in Australia. Additionally, African migrant women with less educational level may also have lower health literacy about the Western medical care and thus embrace their traditional beliefs and practices as first line of maternal health care in Australia.
Low income was also strongly associated with use of traditional medicine for maternal health and wellbeing among the African migrant women. Previous study findings indicated that women with low income may experience limited autonomy as compared to their male counterparts (on whom they may be dependent) who may be responsible for making decisions concerning women’s health care choices and wellbeing [47, 48]. Our analysis also shows that older age (≥ 35 years) and having children were associated with an increased use of traditional medicine for maternal wellbeing and is consistent with previous studies [41, 49–51]. This could be possibly due to the fact that these women may have spent more time in Africa and thus had pre-migration experiences of using traditional medicine.
Implications
The findings from this study can be used to increase the knowledge of healthcare professionals about the African migrant women’s cultural health practices. This in turn will facilitate provision of culturally sensitive and responsive health services when caring for African migrant women by taking into account their cultural health practices. Further research exploring specific traditional and complementary medicine modalities such as herbal medicines will have implications for users and health professionals with respect to information on safety, effectiveness, and appropriate utilisation of these products. Studies examining health beliefs of African migrant women and how traditional health practices and beliefs may influence utilisation of Western medical care are needed.
Strengths and limitations
There are many key strengths inherent in this study. This study which generated a comprehensive understanding of the cultural health practices and beliefs of African migrant women in Sydney. As such it filled an important knowledge gap in the literature. A key methodological strength of the study was the use of a mixed methods approach in bringing together the different strengths of the quantitative and qualitative methods and then validating the survey findings through semi-structured in-depth interviews through data triangulation.
A key limitation was the use of nonprobability sampling strategy which may affect generalisability of the findings. Random sampling was not possible for this study because of the unknown sampling frame of African migrant women population who can meet the selection criteria. However, efforts were made to try and approximate random sampling by eliminating as many biases as possible. Some of such efforts were: 1) the use of homogenous convenience sampling strategy instead of conventional convenience sampling, 2) a fairly large sample for a relatively small population size of African migrant women in Australia, and 3) recruitment of participants across multiple venues including community organisations, market places, religious institutions, colleges and Universities, entertainment places, event and gathering sites, and train and bus stations. In addition, taking the sample only from the geographic area of the Sydney metropolitan area may also limit the generalisability of the findings.
Conclusion
In summary, our finding indicated that use of traditional and complementary medicine is high among the African migrant women. African migrant women use traditional and complementary medicine for health maintenance and treatments of specific health conditions at various points from preconception through to the postnatal period.
Supplementary information
Acknowledgements
The authors would like to acknowledge multicultural organisations and community associations working with African communities across Sydney who aided in the recruitment of participants. The authors would also like to acknowledge African-born women who provided their time and voices to this research.
Abbreviations
- CAM
Complementary and alternative medicine
- NICM
National Institute of Complementary Medicine
- SPSS
Statistical package for social sciences
- WHO
World Health Organization
Authors’ contributions
ZS conceived and designed the study with continuous support from TD and CAS. ZS collected the data. All authors involved in data analysis and interpretation. ZS drafted the manuscript. TD and CAS read and revised the manuscript. All authors have read and approved the submission.
Funding
ZS was supported by Western Sydney University Postgraduate Research Award and Tuition Fee Waiver Scholarship to study a PhD program.
Availability of data and materials
The supporting materials used in this study are contained within the article.
Ethics approval and consent to participate
Ethical approval was received from Western Sydney University Human Research Ethics Committee (ref: H1196). Informed consent was obtained from all individual participants included in the study.
Consent for publication
All participants gave consent for direct quotes from their interviews to be published in this manuscript.
Competing interests
ZS and CAS declared that as a medical research institute, NICM Health Research Institute receives research grants and donations from foundations, universities, government agencies and industry. Sponsors and donors provide untied and tied funding for work to advance the vision and mission of the Institute. TD declared that she has no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zewdneh Shewamene, Email: zeedshow@gmail.com.
Tinashe Dune, Email: T.Dune@westernsydney.edu.au.
Caroline A. Smith, Email: caroline.smith@westernsydney.edu.au
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12906-020-2852-6.
References
- 1.The Federation of Ethnic Communities’ Councils of Australia. Shared Experience and Learning from African Communities in Australia [http://fecca.org.au/wp-content/uploads/2017/08/Issue-46.pdf. [Accessed 15 July 2018].
- 2.Immigration in the past 5 years – focus on NSW. [http://blog.id.com.au/2011/population/australian-demographic-trends/immigration-nsw/. [Accessed 23 June 2016].
- 3.Department of Immigration and Boarder Protection. Annual performance statements. Canberra; 2017. https://www.finance.gov.au/sites/default/files/rmg-134-annual-performance-statements-for-commonwealth-entities_0.pdf. Accessed 5 Feb 2019
- 4.Antwi-Baffour SS, Bello AI, Adjei DN, Mahmood SA, Ayeh-Kumi PF. The place of traditional medicine in the African society: the science, acceptance and support. Am J Health Res. 2014;2(2):49–54. doi: 10.11648/j.ajhr.20140202.13. [DOI] [Google Scholar]
- 5.Mahomoodally MF. Traditional medicines in Africa: an appraisal of ten potent African medicinal plants. Evid Based Complement Alternat Med. 2013;2013:617459. doi: 10.1155/2013/617459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nelms LW, Gorski J. The role of the African traditional healer in women's health. J Transcult Nurs. 2006;17(2):184–189. doi: 10.1177/1043659605285411. [DOI] [PubMed] [Google Scholar]
- 7.Abdullahi A. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med. 2011;8(5 Suppl):115–123. doi: 10.4314/ajtcam.v8i5S.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shewamene Z, Dune T, Smith CA. The use of traditional medicine in maternity care among African women in Africa and the diaspora: a systematic review. BMC Complement Altern Med. 2017;17(1):382. doi: 10.1186/s12906-017-1886-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmed SM, Nordeng H, Sundby J, Aragaw YA, de Boer HJ. The use of medicinal plants by pregnant women in Africa: a systematic review. J Ethnopharmacol. 2018;244:297–313. doi: 10.1016/j.jep.2018.05.032. [DOI] [PubMed] [Google Scholar]
- 10.Callander EJ, Fox H. What are the costs associated with child and maternal healthcare within Australia? A study protocol for the use of data linkage to identify health service use, and health system and patient costs. BMJ Open. 2018;8(2):e017816. doi: 10.1136/bmjopen-2017-017816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization . General guidelines for methodologies on research and evaluation of traditional medicine. Geneva: World Health Organization; 2000. [Google Scholar]
- 12.National Centre for Complementary and Integrative Medicine (NCCIM) https://nccih.nih.gov/health/integrative-health#hed1 Access date: 5 Jan 2020.
- 13.Andersen RM. Behavioral Model of Families’ Use of Health Services. Research Series No. 25. Chicago: Center for Health Administration Studies, University of Chicago; 1968. [Google Scholar]
- 14.Lee YS, Lee IS, Kim SY, Lee H, Park HJ, Lee H, Kim SH, Chae Y. Identification of determinants of the utilisation of acupuncture treatment using Andersen's behavioural model. Acupunct Med. 2015;33(2):129–135. doi: 10.1136/acupmed-2014-010661. [DOI] [PubMed] [Google Scholar]
- 15.Yussman SM, Ryan SA, Auinger P, Weitzman M. Visits to complementary and alternative medicine providers by children and adolescents in the United States. Ambul Pediatr. 2004;4(5):429–435. doi: 10.1367/A03-091R1.1. [DOI] [PubMed] [Google Scholar]
- 16.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328(4):246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 17.Hall HG, Griffiths DL, McKenna LG. The use of complementary and alternative medicine by pregnant women: a literature review. Midwifery. 2011;27(6):817–824. doi: 10.1016/j.midw.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Frawley J, Adams J, Sibbritt D, Steel A, Broom A, Gallois C. Prevalence and determinants of complementary and alternative medicine use during pregnancy: results from a nationally representative sample of Australian pregnant women. Aust N Z J Obstet Gynaecol. 2013;53(4):347–352. doi: 10.1111/ajo.12056. [DOI] [PubMed] [Google Scholar]
- 19.Sirois FM, Gick ML. An investigation of the health beliefs and motivations of complementary medicine clients. Soc Sci Med. 2002;55(6):1025–1037. doi: 10.1016/S0277-9536(01)00229-5. [DOI] [PubMed] [Google Scholar]
- 20.Sirois FM, Purc-Stephenson RJ. Consumer decision factors for initial and long-term use of complementary and alternative medicine. Complement Health Pract Rev. 2008;13(1):3–19. doi: 10.1177/1533210107310824. [DOI] [Google Scholar]
- 21.Creswell JW, Creswell JD. Research design: qualitative, quantitative, and mixed methods approaches: Thousand Oaks: Sage publications; 2017.
- 22.Strauss A, Corbin J. Basics of qualitative research: procedures and techniques for developing grounded theory. Thousand Oaks: Sage; 1998. [Google Scholar]
- 23.de Leeuw E, Hox J. Mixing data collection methods: Lessons from social survey research. In: Bergman, M.M. (ed.) Advances in mixed methods research: theories and applications. Thousand Oaks: Sage; p. 138-149.
- 24.Bryman A. Integrating quantitative and qualitative research: how is it done? Qual Res. 2006;6(1):97–113. doi: 10.1177/1468794106058877. [DOI] [Google Scholar]
- 25.Punch KF, Oancea A. Introduction to research methods in education. Thousand Oaks: Sage; 2014.
- 26.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3(1):17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Austin PC, Tu JV. Automated variable selection methods for logistic regression produced unstable models for predicting acute myocardial infarction mortality. J Clin Epidemiol. 2004;57(11):1138–1146. doi: 10.1016/j.jclinepi.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 28.Bazeley P, Jackson K. Qualitative data analysis with NVivo. Thousand Oaks: Sage Publications Limited; 2013.
- 29.Flick U. The SAGE handbook of qualitative data analysis. Thousand Oaks: SAGE; 2013.
- 30.Mandizadza EJ, Chidarikire S. A phenomenological study into the role of spirituality and religiousness in the mental health of people with Cancer in Zimbabwe. J Spirit Mental Health. 2016;18(2):145–161. doi: 10.1080/19349637.2015.1100972. [DOI] [Google Scholar]
- 31.Johnson KS, Elbert-Avila KI, Tulsky JA. The influence of spiritual beliefs and practices on the treatment preferences of African Americans: a review of the literature. J Am Geriatr Soc. 2005;53(4):711–719. doi: 10.1111/j.1532-5415.2005.53224.x. [DOI] [PubMed] [Google Scholar]
- 32.Truter I. African traditional healers: cultural and religious beliefs intertwined in a holistic way. South Afr Pharma J. 2007;74(8):56–60.
- 33.Brown CM, Barner JC, Richards KM, Bohman TM. Patterns of complementary and alternative medicine use in African Americans. J Altern Complement Med. 2007;13(7):751–758. doi: 10.1089/acm.2006.6392. [DOI] [PubMed] [Google Scholar]
- 34.Meredith KL, Jeffe DB, Mundy LM, Fraser VJ. Sources influencing patients in their HIV medication decisions. Health Educ Behav. 2001;28(1):40–50. doi: 10.1177/109019810102800105. [DOI] [PubMed] [Google Scholar]
- 35.Mansfield CJ, Mitchell J, King DE. The doctor as God’s mechanic? Beliefs in the southeastern United States. Soc Sci Med. 2002;54(3):399–409. doi: 10.1016/S0277-9536(01)00038-7. [DOI] [PubMed] [Google Scholar]
- 36.Bearon LB, Koenig HG. Religious cognitions and use of prayer in health and illness. The Gerontologist. 1990;30(2):249–253. doi: 10.1093/geront/30.2.249. [DOI] [PubMed] [Google Scholar]
- 37.Mathews HF, Lannin DR, Mitchell JP. Coming to terms with advanced breast cancer: black women’s narratives from eastern North Carolina. Soc Sci Med. 1994;38(6):789–800. doi: 10.1016/0277-9536(94)90151-1. [DOI] [PubMed] [Google Scholar]
- 38.Potts RG. Spirituality and the experience of cancer in an African-American community: implications for psychosocial oncology. J Psychosoc Oncol. 1996;14(1):1–19. doi: 10.1300/J077v14n01_01. [DOI] [Google Scholar]
- 39.Wilson-Ford V. Health-protective behaviors of rural black elderly women. Health Soc Work. 1992;17(1):28–36. doi: 10.1093/hsw/17.1.28. [DOI] [PubMed] [Google Scholar]
- 40.Reid R, Steel A, Wardle J, Trubody A, Adams J. Complementary medicine use by the Australian population: a critical mixed studies systematic review of utilisation, perceptions and factors associated with use. BMC Complement Altern Med. 2016;16(1):176. doi: 10.1186/s12906-016-1143-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kaadaaga HF, Ajeani J, Ononge S, Alele PE, Nakasujja N, Manabe YC, Kakaire O. Prevalence and factors associated with use of herbal medicine among women attending an infertility clinic in Uganda. BMC Complement Altern Med. 2014;14:27. doi: 10.1186/1472-6882-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duru CB, Uwakwe KA, Chinomnso NC, Mbachi II, Diwe KC, Agunwa CC, Iwu AC, Merenu IA. Socio-demographic determinants of herbal medicine use in pregnancy among Nigerian women attending clinics in a tertiary Hospital in Imo State, south-east, Nigeria. Am J Med Stud. 2016;4(1):1–10. [Google Scholar]
- 43.Mureyi DD, Monera TG, Maponga CC. Prevalence and patterns of prenatal use of traditional medicine among women at selected Harare clinics: a cross-sectional study. BMC Complement Altern Med. 2012;12:164. doi: 10.1186/1472-6882-12-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.González-Vázquez T, Pelcastre-Villafuerte BE, Taboada A. Surviving the distance: the transnational utilization of traditional medicine among Oaxacan migrants in the US. J Immigr Minor Health. 2016;18(5):1190–1198. doi: 10.1007/s10903-015-0245-6. [DOI] [PubMed] [Google Scholar]
- 45.Mothupi MC. Use of herbal medicine during pregnancy among women with access to public healthcare in Nairobi, Kenya: a cross-sectional survey. BMC Complement Altern Med. 2014;14:432. doi: 10.1186/1472-6882-14-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sarmiento Iván, Zuluaga Germán, Andersson Neil. Traditional medicine used in childbirth and for childhood diarrhoea in Nigeria's Cross River State: interviews with traditional practitioners and a statewide cross-sectional study. BMJ Open. 2016;6(4):e010417. doi: 10.1136/bmjopen-2015-010417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Osamor PE, Grady C. Women’s autonomy in health care decision-making in developing countries: a synthesis of the literature. Int J Womens Health. 2016;8:191–202. doi: 10.2147/IJWH.S105483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ngomane S, Mulaudzi FM. Indigenous beliefs and practices that influence the delayed attendance of antenatal clinics by women in the Bohlabelo district in Limpopo, South Africa. Midwifery. 2012;28(1):30–38. doi: 10.1016/j.midw.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 49.Bayisa B, Tatiparthi R, Mulisa E. Use of herbal medicine among pregnant women on antenatal care at Nekemte hospital, Western Ethiopia. Jundishapur J Nat Pharm Prod. 2014;9(4):e17368. doi: 10.17795/jjnpp-17368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bell RA, Suerken C, Quandt SA, Grzywacz JG, Lang W, Arcury TA. Prayer for health among US adults: the 2002 National Health Interview Survey. Complement Health Pract Rev. 2005;10(3):175–188. doi: 10.1177/1533210105285445. [DOI] [Google Scholar]
- 51.Birdee GS, Kemper KJ, Rothman R, Gardiner P. Use of complementary and alternative medicine during pregnancy and the postpartum period: an analysis of the National Health Interview Survey. J Womens Health. 2014;23(10):824–829. doi: 10.1089/jwh.2013.4568. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The supporting materials used in this study are contained within the article.