Abstract
Background
The Dutch-Flemish PROMIS® Upper Extremity (DF-PROMIS-UE) V2.0 item bank was recently developed using Item Response Theory (IRT). Unknown for this bank are: (1) if it is legitimate to calculate IRT-based scores for short forms and Computerized Adaptive Tests (CATs), which requires that the items meet the assumptions of and fit the IRT-model (Graded Response Model [GRM]);(2) if it is legitimate to compare (sub) groups of patients using this measure, which requires measurement invariance; and (3) the precision of the estimated patients’ scores for patients with different levels of functioning and compared to legacy measures. Aims were to evaluate (1) the assumptions of and fit to the GRM, (2) measurement invariance and (3) (comparative) precision of the DF-PROMIS-UE v2.0.
Methods
Cross-sectional data were collected in Dutch patients with upper extremity disorders. Assessed were IRT-assumptions (unidimensionality [bi-factor analysis], local independence [residual correlations], monotonicity [coefficient H]), GRM item fit, measurement invariance (absence of Differential Item Functioning [DIF] due to age, gender, center, duration, and location of complaints) and precision (standard error of IRT-based scores across levels of functioning). To study measurement invariance for language [Dutch vs. English], additional US data were used. Legacy instruments were the Disability of the Arm, Shoulder and Hand (DASH), the QuickDASH and the Michigan Hand Questionnaire (MHQ).
Results
In total 521 Dutch (mean age ± SD = 51 ± 17 years, 49% female) and 246 US patients (mean age ± SD = 48 ± 14 years, 69% female) participated. The DF-PROMIS-UE v2.0 item bank was sufficiently unidimensional (Omega-H = 0.80, Explained Common Variance = 0.68), had negligible local dependence (four out of 1035 correlations > 0.20), good monotonicity (H = 0.63), good GRM fit (no misfitting items) and demonstrated sufficient measurement invariance. Precise estimates (Standard Error < 3.2) were obtained for most patients (7-item short form, 88.5%; standard CAT, 91.3%; and, fixed 7-item CAT, 87.6%).
The DASH displayed better reliability than the DF-PROMIS-UE short form and standard CAT, the QuickDASH displayed comparable reliability. The MHQ-ADL displayed better reliability than the DF-PROMIS-UE short form and standard CAT for T-scores between 28 and 50. For patients with low function, the DF-PROMIS-UE measures performed better.
Conclusions
The DF-PROMIS-UE v2.0 item bank showed sufficient psychometric properties in Dutch patients with UE disorders.
Keywords: Dutch-Flemish PROMIS, Upper extremity, Item response theory, Measurement invariance, Reliability
Background
Upper extremity (UE) disorders impact health care, society and the lifes of patients. For instance in the field of orthopaedic and trauma surgery, UE disorders account for a large proportion of attendances to the Emergency Department with highest incidences in young patients and elderly females [1]. Total annual costs for all acute and chronic UE disorders are reported to be 290 million euro, of which wrist fractures are the most expensive injuries (83 million euro) due to high incidence, whereas upper arm fractures are most expensive per case (4440 euro) [1]. In addition, these disorders cause considerable losses in working days and productivity [2]. The disability caused by UE disorders significantly reduces physical, mental, and social health [2].
Patient-reported outcome measures (PROMs), consisting of validated questionnaires, are increasingly used in daily clinical practice to assess the impact of acute and chronic UE disorders on the lifes of patients. In the past, outcomes following these disorders were objectified using clinical measurements such as grip strength, range of motion, and radiological parameters. Nowadays the patient perspective on these outcomes is becoming more important. This may include the impact on physical health (e.g., physical functioning, pain intensity and interference), mental health (e.g., depression), and social health (e.g., ability to participate in social roles and activities).
The use of PROMs in daily clinical practice and for research purposes is not without problems. Many different PROMs have been developed and are being used in patients with UE disorders, including the Disability of the Arm, Shoulder and Hand (DASH) questionnaire [3], the QuickDASH [4], the Patient-Rated Wrist Evaluation (PRWE) [5], and the Michigan Hand Questionnaire (MHQ) [6]. Variation exists in their psychometric properties [7–10]. In addition, completing PROMs is time consuming for patients. Finally, the interpretation of the PROM scores is hampered by the variability of conditions the PROMs are applied to [8] and varies between them.
The Patient-Reported Outcomes Measurement Information System (PROMIS®) might offer a solution for some of the problems related to the use of traditional PROMs. The National Institutes of Health PROMIS® initiative has developed a new assessment system for measuring patient-reported health. The goal was to improve measurement quality and comparability of PROMs and reduce patients’ burden. Item banks were developed and validated for measuring specific symptoms and health status domains [11, 12]. An item bank is a universal (non-disease specific) applicable set of items (questions) with responses (answers) that all measure the same domain (construct or concept) [13]. The items of a bank are calibrated on a scale, using a modern psychometric technique, called Item Response Theory (IRT) modelling. In this way, people and items are located on the same scale (ruler or metric) according to their “difficulty”. For PROMIS, the score is expressed as a T-score, which is a standardized score, with 50 currently representing the average score of the US general population, with a standard deviation of 10. IRT-based item banks enable the use of short forms (fixed subsets of items from the item bank) and Computerized Adaptive Testing (CAT). CAT uses an algorithm that selects the most informative items from the item bank, based on the individual’s response to previously administered items. In this way, high measurement precision can be obtained with low respondent burden [11, 14].
PROMIS included an item bank that measures UE-related physical functioning and this bank has recently been updated, from v1.2 to v2.0, to measure a wider range of upper extremity functioning and showed higher precision when used in patients with UE disorders [15]. The v2.0 item bank was translated into Dutch-Flemish (DF-PROMIS-UE v2.0) and some of the psychometric properties of this bank have been studied in patients with UE disorders from a general [16] and an academic hospital [17]. Evidence was found for the following psychometric properties: internal consistency [17], structural validity [17], construct validity [16, 17] and cross-cultural validity [16]. In addition, absence of floor and ceiling effects in the full bank and the 7-item short form was shown [16].
Some other important psychometric properties of the DF-PROMIS-UE v2.0 item bank still need to be evaluated. Unknown for the DF-PROMIS-UE v2.0 bank are: (1) if it is legitimate to calculate IRT-based scores for short forms and Computerizes Adaptive Tests (CATs), which requires that the items meet the assumptions of and fit to the IRT-model (in this case the Graded Response Model [GRM]);(2) if it is legitimate to compare (sub) groups of patients using the measure at issue, which requires measurement invariance; and (3) the precision of the estimated patients’ scores for patients with different levels of functioning and compared to legacy measures. Therefore, the aims of this study were to evaluate (1) the assumptions of and fit to the GRM, (2) measurement invariance and (3) (comparative) precision of the DF-PROMIS-UE v2.0 item bank in patients with UE disorders in comparison to legacy instruments Disability of Arm Shoulder and Hand (DASH) questionnaire, QuickDASH and Michigan Hand Questionnaire (MHQ).
Methods
Participants
Patients visiting the outpatient department of trauma surgery at a level 1 traumacenter or the outpatient department of orthopaedic surgery at a level 2 traumacenter, between February 2018 and August 2018, were invited to participate. Patients were eligible if they were 18 years or older, had an UE disorder, were able to read Dutch and provided informed consent. Because we deemed a sample of at least 500 patients mandatory for item parameter estimation, data of studies performed by van Bruggen et al. [17] and Haan et al. [16] were pooled [18]. To study measurement invariance for language, we used additional data of US patients from an online panel, aged 18 years or older, who endorsed having some difficulty due to UE pain or function [15].
Measures
Besides demographic and disease specific questions, the questionnaire included the full DF-PROMIS-UE v2.0 item bank. In addition, the questionnaire contained 3 disease-specific legacy instruments: the DASH, the QuickDASH and the MHQ (Table 1).
Table 1.
Legacy instruments
| DASH |
30 items (addressed to disabilities and symptoms in musculoskeletal disorders of the upper limbs). Timeframe: during the last week. |
|
Six different 5-point Likert response scales: • No difficulty/Mild difficulty/Moderate difficulty/Severe difficulty/Unable • Not at all/Slightly/Moderately/Quite a bit/Extremely • Not limited at all/Slightly limited/Moderately limited/Very limited/Unable • None/Mild/Moderate/Severe/Extreme • No difficulty/Mild difficulty/Moderate difficulty/Severe difficulty/So much difficulty that I can’t sleep • Strongly disagree/Disagree/Neither agree or disagree/Agree/Strongly agree. | |
| Higher scores imply more disability: 0 (no disability) to 100 (most severe disability). | |
| QuickDASH |
11 items (addressed to disabilities and symptoms in musculoskeletal disorders of the upper limbs). Timeframe: during the last week. |
|
Two different 11-point response scales: • Pain: 0 (no pain) to 10 (unbearable pain) • Function: 0 (no disability) to 10 (most disability) | |
| Higher scores imply more disability: 0 (no disability) to 100 (most severe disability). | |
| MHQ-ADL | 7 items (addressed to activities of daily living). Timeframe: during the last week. |
|
One 5-point Likert response scale: • Not difficult at all/A little difficult/Somewhat difficult/Moderately difficult/Very difficult. | |
| Higher scores imply less disability: 0 (Very difficult to do) to 100 (not difficult to do at all). |
Abbreviations in alphabetic order: DASH Disability of Arm, Shoulder and Hand, MHQ-ADL Michigan Hand Questionnaire-Activities of Daily Living subscale
The DF-PROMIS-UE v2.0 item bank contains 46 items addressing upper extremity function. There are two different 5-point Likert response scales: 1) Unable to do/With much difficulty/With some difficulty/With a little difficulty/Without any difficulty; 2) Cannot do/Quite a lot/Somewhat/Very little/Not at all. There is no timeframe for the items, but current status is inferred. Higher scores indicate better function. A 7-item short form was developed. In addition, the item bank can be used as CAT. The total score of the DF-PROMIS-UE v2.0 item bank, short form or CAT is not a sum or total score, but a weighted score, based on the underlying IRT-model, taking the difficulty of the items into account. All scores are expressed as a T-score, which is a standardized score, with 50 currently representing the average score of the US general population, with a standard deviation of 10, and higher scores indicate more of the domain at issue, in this case better UE-related physical functioning.
The DASH questionnaire contains 30 items, specifically addressed to physical function and symptoms in musculoskeletal disorders of the upper extremity (Table 1) [3]. Both the original English DASH and the official Dutch translation were found to have sufficient psychometric properties [19–21].
The QuickDASH is an 11-item shortened version of the DASH (Table 1). Using conceptual methods these 11 items were selected from the total DASH questionnaire based on the criteria: 1) number of items with > 40% in one response category, 2) Cronbach’s alpha > 0.90 and 3) highest correlation with the 30-item DASH and with other markers of physical function and severity of problem. The QuickDASH has sufficient psychometric properties [4].
The MHQ is a hand-specific instrument that measures several domains and is applicable to patients with conditions of, or injury to, the hand and wrist (Table 1) [6]. The MHQ contains six distinct subscales. In this study, we used the MHQ subscale Activities of Daily Living (MHQ-ADL), which assesses difficulty in performing daily activities for the right hand (5 items), for the left hand (5 items) and both hands (7 items). We used the 7 items referring to both hands because this corresponds most with the generic PROMIS items. The psychometric properties of the MHQ score were found to be sufficient [6, 22–26].
Procedures
The study was approved by the local medical ethics committees of the participating hospitals. Consenting patients were requested to complete all 46 items of the DF-PROMIS-UE v2.0 item bank through an online survey or, only if preferred, using a paper version of the questionnaire. In addition, patients completed general questions regarding age, gender, education and ethnicity. Also questions regarding type of injury and duration of complaints were included. In addition, the DASH, which encompasses the QuickDASH, and the MHQ were completed.
Statistical analysis
IRT-model assumptions and fit
The psychometric analyses were conducted using the original PROMIS analysis plan [14]. For an item bank it is important to know if it is legitimate to calculate IRT-based scores for short forms and CATs. This requires, firstly, that the items meet the assumptions of an IRT-model and, secondly, fit to the IRT-model at issue. An IRT-model requires that the following four assumptions are met: unidimensionality, local independence, monotonicity and measurement invariance [14, 27].
Studying the first IRT-assumption, unidimensionality, addresses the research question whether the items assessed one construct, in this case UE-related physical function. Unidimensionality was evaluated using multiple methods:
Confirmatory Factor Analyses (CFA). The CFA was conducted on the polychoric correlation matrix with Weighted Least Squares with Mean and Variance adjustment (WLSMV) estimation, using the R package LAVAAN (version 0.5–23.1097) [28]. Fit of the unidimensional model was evaluated using the following parameters: Chi-square, df, p-value, Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Means Square Error of Approximation (RMSEA) with 90% CI and Standardized Root Mean Residual (SRMR) [28]. We reported scaled fit indices, which are considered more exact than unscaled indices. Sufficient evidence for unidimensionality and thus adequate model fit was considered if CFI > 0.95, TLI > 0.95, RMSEA < 0.06 and a SRMR < 0.08 [14, 27, 29].
Exploratory Factor Analysis (EFA). EFA was carried out on the polychoric correlation matrix with WLSMV estimation procedures using the R package Psych (version 1.7.5) [18]. Unidimensionality was considered sufficient when the first factor accounts for at least 20% of the variability and when the ratio of the variance explained by the first to the second factor is greater than 4 [14].
Exploratory bi-factor analysis was performed when CFA showed a poor model fit. Bi-factor analysis evaluates, when multidimensionality is present, the impact of multidimensionality. Exploratory bi-factor analysis was conducted using the R package Psych (version 1.7.5). Criteria were: omega H and Explained Common Variance (ECV). Coefficient omega H > 0.80 [30] and ECV > 0.60 [31] indicates that the risk of biased parameters, when fitting multidimensionality data into a unidimensional model, is low.
When suspicion for lack of unidimensionality was present, an additional forced two-factor analysis EFA with Varimax rotation was performed in SPSS (version 26).
Evaluating the second IRT-assumption, local independence, addresses the research question whether the items are only related to the construct (the dominant factor) being measured and not to other constructs (any other factors). This implies that, after controlling for the dominant factor, there should be no significant covariance between item responses. Local independence was evaluated by examining the residual correlation matrix resulting from the single factor CFA. A value of 0.20 above the average residual correlation was taken as a critical value for local dependence [32].
Studying the third IRT-assumption, monotonicity, addresses the research question whether the probability of an affirmative response to the items increases with increasing levels of the underlying construct. This implies, e.g., in case the item responses “Unable to do/With much difficulty/With some difficulty/With a little difficulty/Without any difficulty”, that the probability of endorsing a higher item response category, e.g., choosing “Without any difficulty” instead of “With a little difficulty”, should increase with increasing levels of the underlying construct, in this case the UE-related physical functioning. Monotonicity was evaluated by fitting a non-parametric IRT model, using Mokken scaling in the R package Mokken (version 2.8.4) [33, 34]. We evaluated the fit of the model by calculating the scalability coefficient H per item and for the total scale. We considered monotonicity acceptable if the scalability coefficients for the items were ≥ 0.30 and for the total scale ≥0.50 [33].
Evaluating the fourth IRT-assumption, measurement invariance, addresses the research question whether it is legitimate to compare (sub) groups of patients using the measure at issue. Item parameters should be equivalent between (sub) groups, e.g., age or gender groups, implying that there should be absence of Differential Item Functioning (DIF). DIF analyses are used to examine if people from different (sub) groups, e.g. males versus females, with the same level of the construct, e.g. the same level of UE-related physical functioning, have different probabilities of giving a certain response to an item [14, 35, 36]. Uniform DIF exists when the DIF is consistent, with the same magnitude of DIF across the entire range of the construct [14, 35, 36]. In this case the item location parameters differ between the (sub)groups. Non-uniform DIF exists when the magnitude or direction of DIF differs across the construct. In this case the item discrimination parameters differ between the (sub)groups. DIF was evaluated with use of the R package Lordif (version 0.3–3), using ordinal logistic regression models with a McFadden’s pseudo R2 change of 2% as critical value [14, 37, 38]. DIF was evaluated for age (median split: < 53 years versus ≥53 years), gender, duration of complaints (< 6 months versus ≥6 months), center (level 1 versus level 2 traumacenter) and primary location of complaints (hand/wrist versus arm/shoulder). Regarding location of complaints, patients were able to report on multiple areas. For the DIF analysis regarding location of complaints we used patients who reported either pain in shoulder/arm or hand/wrist only. Measurement invariance for language is a key aspect of cross-cultural validity and was addressed by a DIF analysis for language (Dutch-Flemish versus American-English). In the US dataset some response categories had insufficient responses for analysis and these categories had to be collapsed. In order to compare our population with the US population, scores on the response categories “without much difficulty” and “unable to do” were therefore collapsed for 8 items (PFA43r1, PFB16r1, PFB19r1, PFB20r1, PFB21r1, PFB23r1, PFB31r1, and PFB37r1). For item PFB15r1 the response categories ‘with some difficulty’, ‘without much difficulty’ and ‘unable to do’ were collapsed, according to the US PROMIS convention [39]. The impact of DIF on total scores was examined by plotting the differences between the initial theta and theta corrected for DIF.
After evaluation of the IRT-assumptions, the IRT-model at issue, in this case the logistic Graded Response Model (GRM) which is an IRT-model for ordinal data, was fit to the item response data. The GRM model yields two item types of parameter estimates: the item thresholds and the item slope [35]. Item threshold parameters locate item response categories along the scale (i.e. the construct of interest) [35]. The item slope parameter refers to the discriminative ability of the items, with higher slope values indicating a stronger relationship to the construct of interest [35]. For items with five response categories, four item thresholds were estimated. To assess the fit of the GRM we used the R-package Mirt (version 3.3.2) [40]. To assess the degree to which possible misfit affects the IRT-model, a generalization of Orlando and Thissen’s S-X2 for polytomous data was used [41]. These statistics compare the observed and expected response frequencies under the estimated IRT model and quantifies the differences between the observed and expected response frequencies. Items with a S-X2p-value ≤0.001 demonstrate poor fit [14, 42].
Precision
Measurement precision (reliability) is conceptualized within IRT as “‘information”. In the context of IRT the measurement precision can differ across levels of the measured construct (θ = Theta). The relationship between information (I) and standard error (SE) is defined by the formula.
SE (θ) = 1/√I(θ), where SE is the standard error of the estimated θ, I is information and θ is the estimated level of the construct. For each patient, we calculated four T-scores: one based on all items of the item bank, one based on the standard 7-item short form, and two based on CAT simulations. In the first simulated CAT we used the standard PROMIS CAT stopping rules. The standard CAT stops if a SE of 3 on the T-score metric is reached, comparable to a reliability slightly higher than 0.90, or a maximum of 12 items has been administered. The recommended minimum of four items was not used because this could not be specified in the R-package at issue. In the second simulated CAT we administered a fixed number of seven items to compare the reliability of this CAT with the 7-item short form. In all simulations the starting item was the item with the highest information value for the average level of functioning in our study population (theta = 0) (http://www.healthmeasures.net/score-and-interpret/calculate-scores). All PROMIS T-scores were calculated using the US item parameters (http://www.healthmeasures.net/score-and-interpret/calculate-scores). We used the R-package catR (version 3.12) and expected a posteriori (EAP) estimations for the CAT simulations [18]. The SEs across T-scores for the entire item banks were plotted, for the standard 7-item short form, and for the two different CAT simulations. In addition, the distribution of T-scores in our population was plotted. This enabled us to relate the reliability of the item bank to the distribution of T-scores in this population.
To compare the precision of the DF-PROMIS-UE v2.0 item bank to the precision of the DASH, QuickDASH and the MHQ-ADL (comparative precision), we also fitted a GRM on these three legacy instruments. The scoring of the DASH and QuickDASH was reversed resulting in higher scores indicated better functioning, comparable to PROMIS. We plotted the Standard Errors (SEs) of the T-scores of the DASH, QuickDASH and MHQ-ADL in addition to the SEs of the T-scores of the DF-PROMIS-UE v2.0 short form and standard CAT.
In addition, relative efficiency was quantified per patient for each measure as Information ((1/SE)2) divided by the number of items administered. Relative efficiency among the instruments was calculated as the mean efficiency of the PROMIS measures divided by the mean efficiency of the legacy measures. If the mean relative efficiency is larger than 1, the PROMIS measure is on average more efficient (more information per item) than the legacy instrument, but if it is less than 1, the legacy instrument is on average more efficient.
Results
Of the 828 invited eligible patients, 624 (75%) (405 of 524 level 1 center and 218 of 304 level 2 center) provided informed consent. Of these 624 consenting patients, 103 (all level 1) did not complete the questionnaire, even after two reminders by email. Of the remaining 521 (303 level 1 center and 218 level 2 center, total response rate 63%) patients, 515 fully completed the DF-PROMIS-UE v2.0 item bank. Most analyses were performed on 521 patients. The CAT simulations were performed on the 515 cases with complete DF-PROMIS-UE response data. The DIF analyses for location of complaints were based on 337 patients (268 patients who reported complaints in shoulder/arm only and 68 patients who reported complaints in the hand/wrist only).
Demographic and clinical characteristics
Demographic and clinical characteristics of the Dutch and US samples are summarized in Table 2. The mean age of the Dutch population was 51 years (SD 17) and 253 (49%) were female.
Table 2.
Demographic and clinical characteristics of the Dutch and US samples
| Dutch sample (n = 521) | US sample (n = 246) | |||
|---|---|---|---|---|
| Level 1 center (n = 303) | Level 2 center (n = 218) | Total (n = 521) | ||
| Age, mean (SD) | 50 (17) | 53 (15) | 51 (17) | 48 (14) |
| Gender, n (%) | ||||
| Male | 159 (53) | 109 (50) | 268 (51) | 76 (31) |
| Female | 144 (47) | 109 (50) | 253 (49) | 170 (69) |
| Country of birth, n (%) | ||||
| Netherlands | 276 (91) | 161 (65) | 437 (86) | |
| Other | 27 (9) | 44 (20) | 71 (14) | |
| Missing | 0 (0) | 13 (15) | 0 (0) | |
| Social status, n (%) | ||||
| Single | 110 (36) | 69 (32) | 179 (34) | |
| Married/living together | 155 (51) | 127 (58) | 282 (54) | |
| Living apart together | 15 (5) | 4 (2) | 19 (4) | |
| Living with parents | 16 (5) | 6 (3) | 22 (4) | |
| Other | 7 (3) | 12 (5) | 19 (4) | |
| Educational level, n (%) | ||||
| < high school degree | 34 (11) | 40 (18) | 74 (15) | 6 (2) |
| High school degree | 99 (33) | 75 (33) | 174 (33) | 53 (22) |
| Some college | 16 (5) | 14 (6) | 30 (6) | 81 (33) |
| College degree | 122 (40) | 72 (33) | 194 (37) | 80 (32) |
| Advanced degree | 32 (11) | 17 (8) | 49 (9) | 26 (11) |
| Employment status, n (%) | ||||
| Full time | 141 (47) | 84 (39) | 217 (43) | |
| Part time | 55 (18) | 40 (18) | 93 (18) | |
| Student | 20 (7) | 5 (2) | 25 (5) | |
| Unpaid/volunteer/household | 13 (4) | 18 (8) | 31 (6) | |
| Retired | 49 (16) | 40 (18) | 88 (17) | |
| Unemployed | 6 (2) | 10 (5) | 14 (3) | |
| Other | 19 (6) | 21 (10) | 40 (8) | |
| Duration of complaints, n (%) | ||||
| < 1 month | 135 (45) | 22 (10) | 157 (30) | |
| 1–3 months | 39 (13) | 22 (10) | 61 (12) | |
| 3–6 months | 42 (14) | 30 (14) | 72 (14) | |
| < 6 months (DIF) | 216 (72) | 74 (34) | 290 (56) | |
| 6–12 months | 20 (7) | 36 (17) | 56 (11) | |
| 1–2 years | 8 (3) | 46 (21) | 54 (10) | |
| 2–5 years | 2 (1) | 31 (14) | 33 (6) | |
| 5 years | 1 (0) | 31 (14) | 32 (6) | |
| ≥ 6 months (DIF) | 31 (11) | 144 (66) | 175 (33) | |
| Unknown/missing | 56 (19) | 0 (0) | 56 (11) | |
| Location of paina, n (%) | ||||
| Shoulder(s) | 137 (45) | 190 (87) | 318 (63) | |
| Arm(s) | 125 (41) | 142 (65) | 259 (51) | |
| Shoulder/arm (DIF)b | 132 (44) | 136 (62) | 268 (80) | |
| Hand(s) | 105 (35) | 59 (27) | 161 (32) | |
| Finger(s) | 64 (21) | 49 (22) | 112 (22) | |
| Hand/wrist (DIF)b | 62 (21) | 7 (3) | 69 (20) | |
| DF-PROMIS-UE v2.0, mean (SD) T-scores | 34.7 (3.6) | 33.4 (9.1) | 33.9 (8.9) | 36.5 (7.0) |
| DASH, mean (SD) T-scores | 35.6 (22.1) | 36.5 (21.0) | 35.9 (21.6) | |
| QuickDASH, mean (SD) T-scores | 36.8 (22.1) | 38.1 (21.8) | 37.3 (22.0) | |
| MHQ-ADL, mean (SD) T-scores | 61.4 (31.0) | 74.5 (25.6) | 66.7 (29.6) | |
Abbreviations in alphabetic order: DASH Disability of Arm, Shoulder and Hand, DF-PROMIS-UE v2.0 Dutch-Flemish translated version of the PROMIS Upper Extremity v2.0 item bank, DIF Differential item functioning, MHQ-ADL Michigan Hand Questionnaire-Activities of Daily Living subscale, n Number, SD Standard deviation, % Percentage
aMultiple answers were allowed, bFor the DIF analysis regarding location of complaints only patients who reported either pain in shoulder/arm or hand/wrist were included
IRT-model assumptions and fit
The results of the psychometric analyses are summarized in Tables 3 and 4.
Table 3.
Results with respect to the IRT-model assumptions of the DF-PROMIS-UE v2.0 bank
| Analyses | Outcome | Result |
|---|---|---|
| IRT assumptions and model fit | ||
| Confirmatory Factor Analysis of one-factor model | Chi square | 5964.333 |
| df | 989 | |
| p-value | 0.000 | |
| Scaled CFI | 0.93 | |
| Scaled TLI | 0.93 | |
| Scaled RMSEA (90% CI) | 0.099 (0.097–0.101) | |
| Scaled SRMR | 0.09 | |
| Exploratory Factor Analysis | Eigenvalue first factor | 30.1 |
| Eigenvalue second factor | 2.8 | |
| Ratio | 10.7 | |
| Exploratory bi-factor analysis | ECV | 0.68 |
| Omega-H | 0.80 | |
| Local Dependency | Residual correlation > 0.17 | 4 item pairs locally dependent (3.3%) |
| Monotonicity | Scalability coefficient H | 0.63 |
| Scalability coefficients Hi | Range 0.55–0.70 | |
Abbreviations in alphabetic order: CFI Comparative Fit Index, ECV Explained Common Variance, RMSEA Root Means Square Error of Approximation, SRMR Standardized root mean residual, TLI Tucker-Lewis Index
Table 4.
Result with respect to the monotonicity assumption and GRM-model fit at the item level, GRM-model item parameters, and measurement invariance of the DF-PROMIS-UE v2.0 bank
| Item | Monotonicity | GRM-model fit | GRM-model Item parameters | Measurement invariance | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ID | Item stem | Scalability coefficient Hi | S-X2 p-value |
a | b1 | b2 | b3 | b4 | Gender | Center | Duration of complaints | Location of complaints | Language | |||||
| UF | R2 | UF | R2 | UF | R2 | UF | R2 | UF | R2 | |||||||||
| PFA14r1ab | Are you able to carry a heavy object (over 10 pounds/5 kg)? | 0.591 | 0.181 | 1.862 | −0.613 | −0.227 | 0.415 | 1.054 | ||||||||||
| PFA16r1 | Are you able to dress yourself, including tying shoelaces and buttoning your clothes? | 0.639 | 0.021 | 2.780 | −1.757 | −1.097 | − 0.397 | 0.444 | ||||||||||
| PFA17 | Are you able to reach into a high cupboard? | 0.550 | 0.677 | 1.670 | − 1.156 | −0.587 | −0.046 | 0.657 | UD | 0.118 | ||||||||
| PFA18 | Are you able to use a hammer to pound a nail? | 0.656 | 0.451 | 3.027 | −0.768 | −0.421 | − 0.059 | 0.361 | ||||||||||
| PFA20 | Are you able to cut your food using eating utensils? | 0.642 | 0.003 | 3.028 | −1.553 | −0.985 | −0.376 | 0.172 | UD | 0.032 | ||||||||
| PFA28 | Are you able to open a can with a hand can opener? | 0.679 | 0.063 | 3.404 | −0.738 | −0.431 | − 0.111 | 0.463 | UD | 0.027 | ||||||||
| PFA29r1 | Are you able to pull heavy objects (10 pounds/5 kg) towards yourself? | 0.629 | 0.363 | 2.266 | −1.068 | −0.534 | −0.066 | 0.771 | ||||||||||
| PFA34ab | Are you able to wash your back? | 0.604 | 0.353 | 1.989 | −0.906 | − 0.343 | 0.249 | 1.077 | UD | 0.028 | ||||||||
| PFA35 | Are you able to open and close a zipper? | 0.606 | 0.247 | 2.572 | −2.203 | −1.347 | −0.704 | 0.099 | ||||||||||
| PFA36ab | Are you able to put on and take off a coat or jacket? | 0.579 | 0.408 | 1.968 | −2.736 | −1.438 | −0.495 | 0.604 | UD | 0.043 | ||||||||
| PFA38 | Are you able to dry your back with a towel? | 0.622 | 0.596 | 2.378 | −1.488 | −0.923 | −0.181 | 0.682 | UD | 0.028 | ||||||||
| PFA40 | Are you able to turn a key in a lock? | 0.611 | 0.729 | 2.545 | −1.992 | −1.446 | −0.922 | −0.342 | ||||||||||
| PFA43r1 | Are you able to write with a pen or pencil? | 0.592 | 0.242 | 2.345 | −1.857 | −1.371 | −0.843 | −0.401 | ||||||||||
| PFA44 | Are you able to put on a shirt or blouse? | 0.606 | 0.4822 | 2.222 | −2.361 | −1.439 | −0.624 | 0.473 | ||||||||||
| PFA48 | Are you able to peel fruit? | 0.634 | 0.149 | 2.983 | −1.187 | −0.877 | − 0.491 | 0.058 | UD | 0.050 | UD | 0.027 | ||||||
| PFA50 | Are you able to brush your teeth? | 0.612 | 0.211 | 2.310 | −2.416 | −2.001 | −1.292 | −0.614 | ||||||||||
| PFA54 | Are you able to button your shirt? | 0.630 | 0.140 | 2.783 | −1.871 | −1.330 | −0.730 | 0.084 | UD | 0.023 | UD | 0.020 | UD | 0.023 | ||||
| PFB11 | Are you able to wash dishes, pots, and utensils by hand while standing at a sink? | 0.638 | 0.251 | 2.928 | −1.421 | −0.825 | −0.375 | 0.303 | ||||||||||
| PFB13ab | Are you able to carry a shopping bag or briefcase? | 0.593 | 0.010 | 1.926 | −1.262 | −0.808 | −0.126 | 0.580 | UD | 0.027 | ||||||||
| PFB15r1 | Are you able to change the bulb in a table lamp? | 0.641 | 0.768 | 3.067 | −1.280 | −1.012 | −0.571 | −0.001 | ||||||||||
| PFB16r1 | Are you able to press with your index finger (for example ringing a doorbell)? | 0.596 | 0.071 | 2.165 | −2.651 | −2.110 | −1.510 | −0.950 | UD | 0.025 | ||||||||
| PFB18 | Are you able to shave your face or apply makeup? | 0.645 | 0.377 | 3.073 | −1.810 | − 1.411 | − 0.841 | − 0.101 | ||||||||||
| PFB19r1 | Are you able to squeeze a new tube of toothpaste? | 0.663 | 0.518 | 3.177 | −2.142 | −1.667 | −1.055 | −0.410 | ||||||||||
| PFB20r1 | Are you able to cut a piece of paper with scissors? | 0.651 | 0.071 | 3.313 | −1.624 | −1.229 | −0.844 | − 0.310 | UD | 0.021 | ||||||||
| PFB21r1 | Are you able to pick up coins from a table top? | 0.603 | 0.013 | 2.164 | −2.350 | −1.916 | −1.389 | −0.677 | UD | 0.043 | ||||||||
| PFB22 | Are you able to hold a plate full of food? | 0.662 | 0.489 | 2.965 | −1.488 | − 1.153 | −0.639 | 0.103 | ||||||||||
| PFB23r1b | Are you able to poor liquid from a bottle into a glass? | 0.661 | 0.002 | 3.046 | −1.692 | −1.373 | −0.798 | −0.151 | ||||||||||
| PFB25 | Are you able to push open a door after turning the knob? | 0.593 | 0.257 | 2.157 | −2.353 | −1.524 | −0.966 | − 0.182 | ||||||||||
| PFB26 | Are you able to shampoo your hair? | 0.644 | 0.331 | 2.907 | −1.470 | −1.009 | − 0.496 | 0.287 | ||||||||||
| PFB27 | Are you able to tie a knot or a bow? | 0.640 | 0.015 | 3.027 | −1.429 | −0.959 | −0.570 | 0.042 | UD | 0.056 | UD | 0.031 | ||||||
| PFB28r1a | Are you able to lift 10 pounds (5 kg) above your shoulder? | 0.639 | 0.081 | 2.040 | −0.198 | 0.224 | 0.670 | 1.350 | UD | 0.062 | ||||||||
| PFB30 | Are you able to open a new milk carton? | 0.675 | 0.035 | 3.590 | −1.449 | −0.990 | −0.520 | 0.100 | ||||||||||
| PFB31r1 | Are you able to open car doors? | 0.654 | 0.181 | 2.906 | −1.773 | −1.330 | −0.798 | −0.181 | ||||||||||
| PFB33 | Are you able to remove something from your back pocket? | 0.577 | 0.478 | 2.045 | −1.626 | −1.104 | −0.576 | 0.209 | ||||||||||
| PFB34ab | Are you able to change a light bulb overhead? | 0.638 | 0.311 | 2.357 | −0.717 | −0.357 | 0.079 | 0.824 | UD | 0.052 | ||||||||
| PFB36 | Are you able to put on a pullover sweater? | 0.595 | 0.475 | 2.061 | −2.009 | −1.148 | −0.265 | 0.618 | UD | 0.058 | ||||||||
| PFB37r1 | Are you able to reach and get down a 5 pound (2 kg) object from above your head? | 0.660 | 0.724 | 3.125 | −1.980 | − 1.547 | −0.978 | 0.348 | ||||||||||
| PFB39r1 | Are you able to reach and get down a 5 pound (2 kg) object from above your head? | 0.626 | 0.605 | 2.218 | −0.886 | −0.533 | − 0.055 | 0.705 | UD | 0.022 | UD | 0.030 | ||||||
| PFB41 | Are you able to trim your fingernails? | 0.586 | 0.595 | 2.352 | −1.487 | −1.091 | −0.547 | 0.001 | UD | 0.038 | ||||||||
| PFB56r1 | Are you able to lift one pound (0.5 kg) to shoulder level without bending your elbow? | 0.563 | 0.250 | 1.816 | −1.004 | −0.604 | −0.191 | 0.508 | UD | 0.041 | ||||||||
| PFC43 | Are you able to use your hands, suchs as for turning faucets, using kitchen gadgets, or sewing? | 0.619 | 0.045 | 2.853 | −1.755 | −1.243 | −0.713 | −0.069 | UD | 0.232 | UD | 0.024 | ||||||
| PFC49 | Are you able to water a house plant? | 0.662 | 0.016 | 3.091 | −1.807 | −1.431 | −1.056 | −0.463 | UD | 0.028 | UD | 0.022 | ||||||
| PFM2b | Are you able to lift a heavy painting or picture to hang on your wall above eye-level? | 0.684 | 0.720 | 2.786 | −0.431 | −0.083 | 0.377 | 1.208 | NUD | 0.021 | ||||||||
| PFM16ab | Are you able to pass a 20-pound (10 kg) turkey or ham to other people at the table? | 0.697 | 0.275 | 2.698 | −0.212 | 0.176 | 0.677 | 1.469 | ||||||||||
| PFM18b | Are you able to continuously swing a baseball bat or tennis racket back and forth for 5 min? | 0.624 | 0.131 | 1.941 | −0.339 | 0.091 | 0.553 | 1.239 | UD | 0.028 | ||||||||
| PFC8 | Does your health now limit you in opening a previously opened jar? | 0.617 | 0.203 | 2.460 | −1.903 | 0.999 | −0.365 | 0.391 | ||||||||||
Abbreviations in alphabetical order: ID Identification, GRM Graded Response Model, NUD Non-Uniform DIF, ID, UD Uniform DIF, UF Uniformity
a items included in the 7a short form
b items selected as one of the first three items in the CAT
Unidimensionality
The results indicated unidimensionality, although not all criteria for unidimensionality were met (Table 3). The CFA results showed some lack of unidimensionality. The EFA and the bi-factor analysis supported unidimensionality. The forced two-factor analyses showed some evidence for a 2-factor model, including one factor consisting of items referring to using the shoulder or lifting heavy objects (eigenvalue 26.1) and one factor consisting of items referring to fine tactile function (eigenvalue 3.3) (Appendix 1).
Local dependence
Thirty-seven percent of the residual correlations were positive. The average residual correlation was − 0.033, so the critical value 0.20 above the mean would be 0.17 [32]. Four residual correlations (out of 1035 correlations, 0.004%) were larger than 0.17, suggesting local dependence: PFA14r1 (‘Are you able to carry a heavy object (over 10 pounds /5 kg)?’) had a residual correlation of 0.214 with PFA29r1 (‘Are you able to pull heavy objects (10 pounds/ 5 kg) towards yourself?’), PFA36 (‘Are you able to put on and take off a coat or jacket?’) had a residual correlation of 0.221 with PFA44 (‘Are you able to put on a shirt or blouse?’), a residual correlation of 0.184 with PFB36 (‘Are you able to put on a pullover sweater?’) and a residual correlation of 0.173 with PFA34 (‘Are you able to wash your back?’) respectively. An additional 32 item pairs had negative residual correlations > − 0.20, suggesting multidimensionality.
Monotonicity
The scalability coefficients Hi of the items ranged from 0.55 (PFA17 ‘Are you able to reach into a cupboard?’) to 0.70 (PFM16 ‘Are you able to pass a 20-pound (10kg) turkey or ham to other people at the table?’) for the individual items (Table 4). The Mokken scalability coefficient H for the entire item bank was 0.63. Therefore, the DF-PROMIS-UE v2.0 items sufficiently met the monotonicity assumption.
Measurement invariance
No DIF was found for age, one item was flagged for DIF regarding gender, 7 items were flagged for DIF regarding center, three items were flagged for DIF regarding duration of complaints, and 15 items were flagged for DIF regarding location of complaints (Table 4). The combined impact of the DIF items on total scores was negligible for all DIF variables (as an example, Appendix 2 shows the differences between the initial theta and theta corrected for DIF for location of complaints; 75% of these differences were roughly between − 0.075 and 0.06 theta points). When analyzing DIF for language, one item was flagged for non-uniform DIF and three items were flagged for uniform DIF (Table 4). The impact of DIF for language on the total score was negligible providing evidence for cross-cultural validity (Table 4).
GRM fit
There were no misfitting items (Table 4). On the Dutch metric, the item thresholds ranged from − 2.7 (PFA36 ‘Are you able to put on and take off a coat or jacket?’) to 1.5 (PFM16 ‘Are you able to pass a 20-pound (10kg) turkey or ham to other people at the table?’) (min/max of all thresholds). The item discrimination parameters ranged from 1.7 to 3.6. The item with lowest discriminative ability was PFA17 (‘Are you able to reach into a cupboard?’) and PFB30 (‘Are you able to open a new milk carton?’) was the item with highest discriminative ability.
Precision
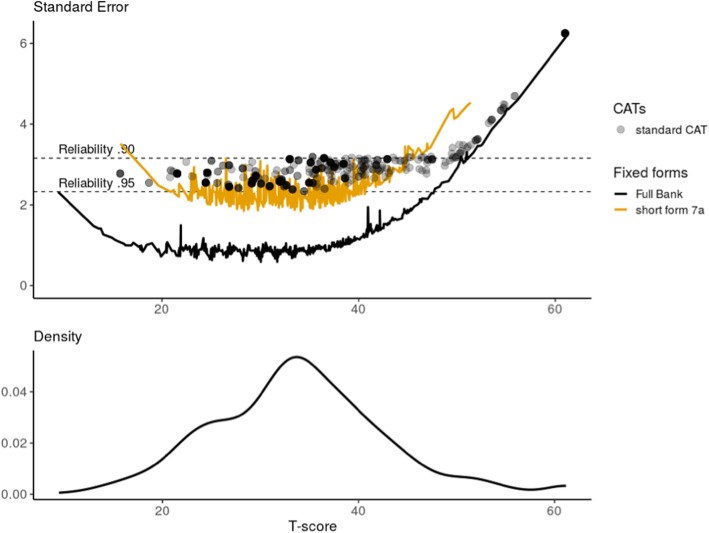
The three items with the highest information at θ = 0 (average of this Dutch sample) were PFB30 (“Are you able to open a new milk carton?”), PFA28 (“Are you able to open a can with a hand can opener?”) and PFA18 (“Are you able to use a hammer to pound a nail?”). Figure 1 shows the standard errors across T-scores for the full item bank, the standard 7-item short form and the two simulated CATs as well as the distribution of scores in the patient population based on the US item parameters. A theta could reliably be estimated (> 0.90) for 498/521 (95.6%) of the patients based on the full item bank and for all patients in the clinical range (T-score < 50). A theta could reliably be estimated for 460/521 (88.3%) of the patients based on the 7-item short form, and for all but five patients with T-scores lower than 45. Using the standard CAT, a reliability of > 0.90 was obtained for 469/515 (91.1%) of the patients and for all except three patients with a T-score < 50. The average number of items administered was 4.7 and 83.3% of the patients needed less than 7 items to get a reliable score. For the fixed 7-item CAT, a reliability of > 0.90 was obtained for 450/515 (87.4%) of the patients and for all patients with a T-score < 47.
Fig. 1.
Reliability of the DF-PROMIS-UE v2.0 when using different applications (full item bank, 7-item short form and simulated standard CAT. Shading represents many of the same scores. The density plot represents the distribution of T-scores in the study sample
Comparative precision
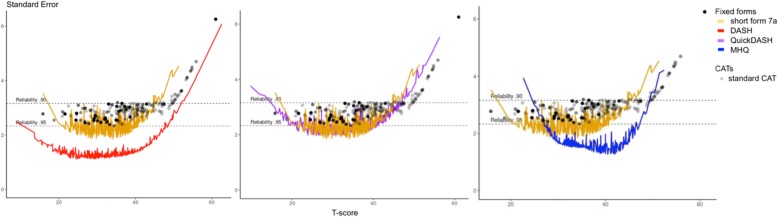
The DASH showed some lack of unidimensionality (CFI 0.91, TLI 0.90, RMSEA 0.13, SRMR 0.08) but all items fitted a GRM model. The QuickDASH also showed some lack of unidimensionality (CFI 0.94, TLI 0.92, RMSEA 0.15, SRMR 0.08) but all items fitted a GRM model. The MHQ-ADL showed better unidimensionality, although the RMSEA was higher than the criterion (CFI 0.99, TLI 0.99, RMSEA 0.13, SRMR 0.03) and all items fitted the GRM model. Figure 2 shows the reliability of the Dutch-Flemish DF-PROMIS-UE v2.0 short form and standard CAT versus the DASH, QuickDASH and MHQ-ADL. The 30-item DASH displayed better reliability than the DF-PROMIS-UE 7-item short form and standard CAT (Fig. 2a). The 11-item QuickDASH showed comparable reliability to the DF-PROMIS-UE CAT and short form (Fig. 2b). The 7-item MHQ-ADL displayed better reliability than the DF-PROMIS-UE 7-item short form and standard CAT for T-scores between T-scores of about 28 to 50, but for patients with low function the DF-PROMIS-UE v2.0 7-item short form and standard CAT performed better (Fig. 2c).
Fig. 2.
a-c Reliability of the CAT of the DF-PROMIS-UE v2.0 and the short form 7a, DASH, QuickDASH and MHQ
Relative efficiency
The DF-PROMIS-UE 7-item short form is on average more efficient than the full item bank. The DF-PROMIS-UE CAT is on average more efficient than the DF-PROMIS-UE full bank and 7-item short form and more efficient than the DASH, quickDASH and MHQ (Table 5). The DF-PROMIS-UE 7-item short form and full item bank are on average more efficient than the DASH and QuickDASH, but less efficient than the MHQ (Table 5).
Table 5.
Mean relative efficiency of PROMIS measures versus legacy instruments
| DF-PROMIS-UE full bank (46 items) | DF-PROMIS-UE 7-item short form (7 items) | DF-PROMIS-UE standard CAT (average 4.7 items) | |
|---|---|---|---|
| DF-PROMIS-UE full bank (46 items) | 1.37 | 1.54 | |
| DF-PROMIS-UE 7-item short form (7 items) | 1.30 | ||
| DASH (30 items) | 1.30 | 1.50 | 1.82 |
| QuickDASH (11 items) | 1.42 | 1.58 | 1.96 |
| MHQ (7 items) | 0.79 | 0.95 | 1.12 |
DASH Disability of Arm, Shoulder and Hand, DF-PROMIS-UE v2.0 Dutch-Flemish translated version of the PROMIS Upper Extremity v2.0 item bank, MHQ-ADL Michigan Hand Questionnaire-Activities of Daily Living subscale
Discussion
We validated the DF-PROMIS-UE v2.0 item bank in a Dutch population with upper extremity disorders. Together with two recent publications from our research group, this study provides the first complete foreign language validation of this item bank [16, 17]. Although we found some problems with the unidimensionality and the measurement invariance assumptions of the IRT model, a good IRT model fit and a high reliability across a wide range of the construct for the DF-PROMIS-UE v2.0 item bank were found.
With regard to unidimensionality, CFI and TLI values (0.93 and 0.93) were near the minimum criteria of 0.95, RMSEA was higher than the maximum criterion of 0.06 (0.10) and SRMR was slightly higher than the maximum criterion of 0.08 (0.09). A few studies reported on the validation of the PROMIS-UE v1.2 item bank, but none described the CFI, TLI, RMSEA, or SRMR values [39, 43–46]. A high RMSEA has been reported for many other PROMIS item banks [47–50]. It has been suggested that traditional cutoffs and standards for CFA fit statistics, are not suitable to establish unidimensionality of item banks measuring health concepts and bi-factor analysis has been suggested to examine whether a scale is sufficiently unidimensional [27, 51]. The bi-factor analysis results suggested sufficient unidimensionality of the DF-PROMIS-UE v2.0 item bank, which supports the use of IRT. However, a forced two-factor exploratory factor analyses showed that a 2-factor model, including one factor consisting of items referring to fine tactile function and one factor consisting of items referring to using the shoulder or lifting heavy objects could also be considered, although several items loaded on both factors.
Four item pairs had residual correlations above the critical value of 0.17. This local dependence is probably mainly due to redundancy-dependency (high degree of overlap within the content of the items), which we consider irrelevant to the measurement of upper extremity. However, items of pair PFA14r1 and PFA29r1 were both administered in the CAT in 14% of cases (in this order) and items of pair PFA36 and PFA44 were both administered in the CAT in 5.5% of cases (in this order). Moreover, PFA34 and PFA36 are both included in the standard short form 7a. Future studies should examine whether these results are consistent across studies and whether the CAT or short form would perform better if one ofor more of these local dependent items would be excluded. An additional 32 item pairs had negative residual correlations > − 0.20, suggesting multidimensionality. Most of these item pairs consisted of one item referring to fine tactile function and one item referring to using the shoulder or lifting heavy objects.
With respect to measurement invariance, we found no evidence for DIF due to age, but some items were flagged for DIF for gender, center, duration of complaints, and language. However, the impact of DIF on T-scores was considered negligible. Our study results therefore indicate that is legitimate to compare these groups when applying the DF-PROMIS-UE v2.0 item bank. However, for the items flagged for DIF regarding location of complaints, five out of the seven items included in the short form and five out of the nine items that were selected as one of the first three items in the CAT showed uniform DIF for location of complaints. Overall, the DIF results all seem to be related to a difference in performance between items regarding fine tactile function versus items regarding lifting heavy objects, which is in accordance with the forced two-factor EFA results. For example, all DIF results for location of complaint indicated that among patients with the same overall level of UE functioning, patients with only hand/wrist injuries indicated more problems with activities that involve fine tactile functioning and patients with only shoulder problems indicated more problems with activities involving heavy lifting tasks, reaching above shoulder level or behind the back. It is known that grip strength is merely a reflection of overall muscle strength and condition of a chain of muscles in the upper limb and at longterm follow-up is not severely impacted by hand or wrist injury [52–54]. In contrast, range of motion is significantly impacted by hand and wrist injuries and influences fine tactile functioning [53–55]. Therefore, we hypothesize that arm/shoulder problems impact heavy lifting activity, but to a lesser extent fine tactile functioning. In our previous study eight items were flagged DIF for language in the level 2 center patients [16], while in this study only four items were flagged for language DIF. This might be due to the slightly different study population of the level 1 center, including more patients with hand problems. More research in other populations with different distribution of injuries of the upper extremity should be performed to investigate possible multidimensionality and the impact of DIF for location of complaints on short form and CAT scores.
When studying measurement invariance for language (cross-cultural validity), we found 3 items with DIF. None of these DIF items are included in the standard 7a short form. Item PFM2 was selected as second item in the standard CAT in 15.9% of the patients, but the R2 change is small (0.0212) so the impact also should be small. Crins et al. examined language DIF of the PROMIS Physical Function v1.2 in a study in chronic pain patients. They found four items with language DIF, of which one item (PFB13 ‘Are you able to carry a shopping bag or briefcase?’) is also included in the PROMIS-UE v2.0 item bank. This item was not flagged for language DIF in our study. In contrast to our study, Crins et al. did not find DIF for any of the items flagged for DIF in our study that were also included in the PROMIS Physical Function v1.2 item bank [49]. It has been suggested that such differences can occur because most available DIF methods can detect whether there is DIF but cannot identify the exact DIF items due to parameter identification issues [56]. Our study and the study of Crins et al., found minimal impact of language DIF on T-scores, which suggests that the original US item parameters can be used for calculating the T-scores of the DF-PROMIS-UE v2.0 bank.
We found high reliability of simulated standard CAT T-scores with a reliability of > 0.90 (which has been considered a minimum requirement for use of PROMs in individual patients [57]) in 91.7% of the patients and in all patients within the clinical range, with on average only 4.7 items. The short form 7a had a reliability of > 0.90 in 88.5% of the patients. The short form was slightly more reliable than the standard CAT in the middle of the scale for T-scores between 18 and 45 but performed less than the CAT in patients with low function (range of T-score in the study population was 11–61). Both the standard CAT and the short form had sufficient reliability but the CAT required less items. The DASH displayed better reliability than the DF-PROMIS-UE v2.0 standard CAT and 7-item short form, while the QuickDASH displayed comparable reliability. However, the DASH requires 30 items, which may be considered too much for use in daily clinical practice. The MHQ-ADL is less reliable than the DF-PROMIS-UE v2.0 measures in patients with low functioning. Future studies should examine whether it is possible to further improve the standard CAT by choosing another starting item. Currently, item PFM16 is being used (‘Are you able to pass a 20-pound (10 kg) turkey or ham to other people at the table?’), but this item is less informative (ranked 14) in the Dutch sample and was flagged for language DIF in the level 2 traumacenter [16].
For adequate interpretation, a PROM has to be validated in the language in which it will be used, as we have done for the DF-PROMIS-UE v2.0. Van Eck et al. have performed validation of the DASH-Dutch Language Version and showed that it also measures a unidimensional trait [19]. Iordens et al. performed validation of the Dutch translated version of the QuickDASH [58]. Unfortunately, to our knowledge, the MHQ has not been validated in the Dutch language. This might hamper the interpretability of the outcome presented in this study with respect to the MHQ. On the other hand, our own study provides evidence for the adequate unidimensionality and reliability of the MHQ-ADL.
When reporting on outcomes of UE disorders in literature, extensive core sets including functional outcomes and PROMs have been suggested to improve comparability of studies [59, 60]. However, for clinical practice, a more practical ‘lean’ core set is advisable including a PROM with low burden for the patient and clinician. An advantage of the incorporating the DF-PROMIS-UE v2.0 in this ‘lean’ core set is that it has high correlation with other PROMs reporting on UE disorders, it decreases burden for patients and clinicians and it will allow clinicians to speak a ‘common language’ with regard to outcome reporting [61, 62]. However, the PROM should be able to detect clinical relevant change as expressed in the Minimal Important Change (MIC). De Vet et al. defined MIC as ‘the smallest change in construct to be measured which patients perceive as important’ [63]. The MIC threshold is very important in daily practice, where clinicians can compare at a patients’ individual level the current and previous values of outcome measures of interest. The MIC has been estimated for the DASH, QuickDASH, and MHQ [58, 64, 65]. However, for the PROMIS-UE v2.0 a MIC has not been established. Future research regarding test-retest reliability, smallest detectable change, and MICs is mandatory to be able to interpret outcome as reported with the DF-PROMIS-UE v2.0 in clinical practice.
Conclusions
The DF-PROMIS-UE v2.0 item bank showed sufficient psychometric properties in a Dutch population with injuries of the upper extremity. This item bank is now ready for use as CAT in research and clinical practice and will be made available through the Dutch-Flemish Assessment Center (http://www.dutchflemishpromis.nl). However, more research on possible multidimensionality and impact of DIF for location of complaints on short form and CAT scores is recommended. Furthermore, test-retest reliability, responsiveness, and MICs need to be assessed in future studies. DF-PROMIS-UE v2.0 CATs allow reliable and valid measurement of outcome following musculoskeletal disorders of the upper extremity in an efficient and user-friendly way with limited administration time.
Acknowledgements
We thank prof. dr. M. Boers for his effort for the graphics.
Abbreviations
- CAT
Computerized Adaptive Testing
- CFA
Confirmatory factor analysis
- CFI
Comparative Fit Index
- DASH
Disability of Arm, Shoulder and Hand
- DF-PROMIS-UE v2.0
Dutch-Flemish translation of the Patient-Reported Outcomes Measurement Information System Physical Functioning – Upper Extremity version 2.0
- DIF
Differential Item Functioning
- EAP
Expected a posteriori
- ECV
Explained Common Variance
- EFA
Exploratory Factor Analysis
- GRM
Graded Response Model
- IRT
Item Response Theory
- MHQ-ADL
Michigan Hand Questionnaire subscale Activities of Daily Living
- PROM
Patient Reported Outcome Measure
- PROMIS
Patient-Reported Outcomes Measurement Information System
- PRWE
Patient Reported Wrist Evaluation
- RMSEA
Root Means Square Error of Approximation
- SD
Standard deviation
- SE
Standard error
- SRMR
Standardized Root Mean Residual
- TLI
Tucker-Lewis Index
- UE
Upper extremity
- US
United States
- WLSMV
Weighted Least Squares with Mean and Variance adjustment
Appendix 1
Table 6.
Forced two-factor EFA
| Item ID | Item stem | Rotated factor loadings | |
|---|---|---|---|
| factor 1 | factor 2 | ||
| PFA14r1 | Are you able to carry a heavy object (over 10 pounds/5 kg)? | 0.275 | 0.724 |
| PFA16r1 | Are you able to dress yourself, including tying shoelaces and buttoning your clothes? | 0.604 | 0.511 |
| PFA17 | Are you able to reach into a high cupboard? | 0.208 | 0.791 |
| PFA18 | Are you able to use a hammer to pound a nail? | 0.583 | 0.541 |
| PFA20 | Are you able to cut your food using eating utensils? | 0.802 | 0.300 |
| PFA28 | Are you able to open a can with a hand can opener? | 0.706 | 0.442 |
| PFA29r1 | Are you able to pull heavy objects (10 pounds/5 kg) towards yourself? | 0.383 | 0.734 |
| PFA34 | Are you able to wash your back? | 0.340 | 0.700 |
| PFA35 | Are you able to open and close a zipper? | 0.704 | 0.331 |
| PFA36 | Are you able to put on and take off a coat or jacket? | 0.444 | 0.574 |
| PFA38 | Are you able to dry your back with a towel? | 0.486 | 0.615 |
| PFA40 | Are you able to turn a key in a lock? | 0.683 | 0.330 |
| PFA43r1 | Are you able to write with a pen or pencil? | 0.738 | 0.235 |
| PFA44 | Are you able to put on a shirt or blouse? | 0.541 | 0.516 |
| PFA48 | Are you able to peel fruit? | 0.828 | 0.250 |
| PFA50 | Are you able to brush your teeth? | 0.646 | 0.304 |
| PFA54 | Are you able to button your shirt? | 0.781 | 0.287 |
| PFB11 | Are you able to wash dishes, pots, and utensils by hand while standing at a sink? | 0.747 | 0.356 |
| PFB13 | Are you able to carry a shopping bag or briefcase? | 0.405 | 0.660 |
| PFB15r1 | Are you able to change the bulb in a table lamp? | 0.696 | 0.409 |
| PFB16r1 | Are you able to press with your index finger (for example ringing a doorbell)? | 0.582 | 0.271 |
| PFB18 | Are you able to shave your face or apply makeup? | 0.709 | 0.380 |
| PFB19r1 | Are you able to squeeze a new tube of toothpaste? | 0.788 | 0.271 |
| PFB20r1 | Are you able to cut a piece of paper with scissors? | 0.823 | 0.243 |
| PFB21r1 | Are you able to pick up coins from a table top? | 0.732 | 0.169 |
| PFB22 | Are you able to hold a plate full of food? | 0.667 | 0.476 |
| PFB23r1 | Are you able to poor liquid from a bottle into a glass? | 0.675 | 0.449 |
| PFB25 | Are you able to push open a door after turning the knob? | 0.548 | 0.469 |
| PFB26 | Are you able to shampoo your hair? | 0.617 | 0.514 |
| PFB27 | Are you able to tie a knot or a bow? | 0.813 | 0.280 |
| PFB28r1 | Are you able to lift 10 pounds (5 kg) above your shoulder? | 0.133 | 0.870 |
| PFB30 | Are you able to open a new milk carton? | 0.777 | 0.383 |
| PFB31r1 | Are you able to open car doors? | 0.639 | 0.475 |
| PFB33 | Are you able to remove something from your back pocket? | 0.484 | 0.544 |
| PFB34 | Are you able to change a light bulb overhead? | 0.361 | 0.744 |
| PFB36 | Are you able to put on a pullover sweater? | 0.413 | 0.645 |
| PFB37r1 | Are you able to reach and get down a 5 pound (2 kg) object from above your head? | 0.722 | 0.353 |
| PFB39r1 | Are you able to reach and get down a 5 pound (2 kg) object from above your head? | 0.288 | 0.830 |
| PFB41 | Are you able to trim your fingernails? | 0.754 | 0.245 |
| PFB56r1 | Are you able to lift one pound (0.5 kg) to shoulder level without bending your elbow? | 0.274 | 0.740 |
| PFC43 | Are you able to use your hands, suchs as for turning faucets, using kitchen gadgets, or sewing? | 0.769 | 0.278 |
| PFC49 | Are you able to water a house plant? | 0.639 | 0.424 |
| PFM2 | Are you able to lift a heavy painting or picture to hang on your wall above eye-level? | 0.369 | 0.749 |
| PFM16 | Are you able to pass a 20-pound (10 kg) turkey or ham to other people at the table? | 0.305 | 0.756 |
| PFM18 | Are you able to continuously swing a baseball bat or tennis racket back and forth for 5 min? | 0.236 | 0.765 |
| PFC8 | Does your health now limit you in opening a previously opened jar? | 0.620 | 0.457 |
Appendix 2
Fig. 3.
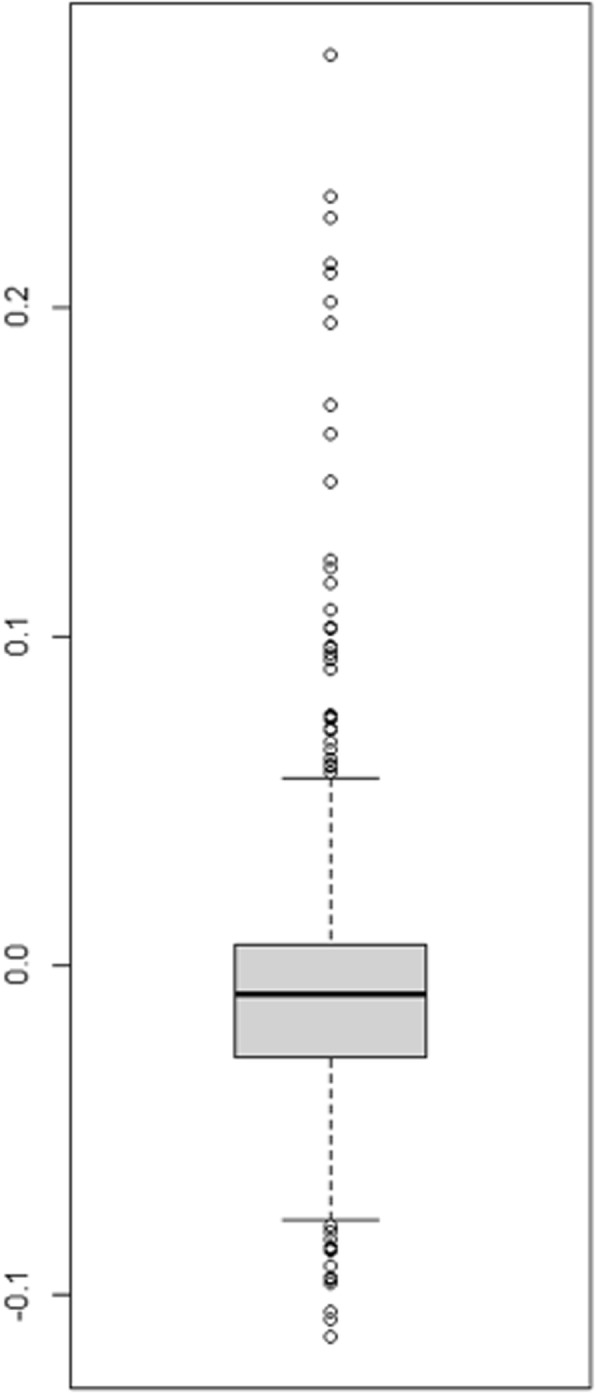
Differences between the initial theta and theta corrected for DIF for location of complaints. The box shows the interquartile range, representing the middle 50% of the differences
Authors’ contributions
CL was responsible for the data management and wrote the manuscript. SB and EH performed the data collection. DD supported with data collection. KE and VS translated the 4 new items. AK shared the data of the US patient group and contributed to the data analyses. LR and CT designed the study. LR contributed to writing the manuscript. CT performed all statistical analyses and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Funding
No funding sources are applicable.
Availability of data and materials
The Dutch-Flemish dataset used and analyzed during the current study are available from the corresponding author on reasonable request. The US dataset is publicly available on the HealthMeasures Dataverse 10.7910/DVN/IHNIRH.
Ethics approval and consent to participate
Medical ethical approval was waivered by the local Medical Ethics Committee of the Amsterdam University Medical Center [reference number 2018.259], because this study was observational and only requested answering validated questionnaires from the participants. In addition, the study was performed in compliance with the principles outlined in the Declaration of Helsinki on ethical principles for medical research involving human subjects [66]. Verbal consent was obtained from all participants and registered in the electronic patient file. Following consent, patients visited an online platform where a digital consent was recorded, before answering questions regarding demographic information and the PROMs.
Consent for publication
All presented data in this study cannot be traced to individual patients and do not compromise anonymity. Therefore consent for publication is not applicable.
Competing interests
CBT is president of the PROMIS Health Organization, a charitable foundation that aims to advance the science of health outcomes assessment through the use of PROMIS. CBT and LDR are coordinators of the Dutch-Flemish PROMIS National Center. AK is one of the developers of the US PROMIS-UE v2.0 item bank. The other authors declare they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Polinder S, Iordens GI, Panneman MJ, Eygendaal D, Patka P, Den Hartog D, et al. Trends in incidence and costs of injuries to the shoulder, arm and wrist in The Netherlands between 1986 and 2008. BMC Public Health. 2013;13:531. doi: 10.1186/1471-2458-13-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hou WH, Chi CC, Lo HL, Chou YY, Kuo KN, Chuang HY. Vocational rehabilitation for enhancing return-to-work in workers with traumatic upper limb injuries. Cochrane Database Syst Rev. 2017;12:CD010002. doi: 10.1002/14651858.CD010002.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy CA, Beaton DE, Smith P, Van Eerd D, Tang K, Inrig T, et al. Measurement properties of the QuickDASH (disabilities of the arm, shoulder and hand) outcome measure and cross-cultural adaptations of the QuickDASH: a systematic review. Qual Life Res. 2013;22(9):2509–2547. doi: 10.1007/s11136-013-0362-4. [DOI] [PubMed] [Google Scholar]
- 5.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan hand outcomes questionnaire. J Hand Surg Am. 1998;23(4):575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 7.Hong I, Bonilha HS. Psychometric properties of upper extremity outcome measures validated by Rasch analysis: a systematic review. Int J Rehabil Res. 2017;40(1):1–10. doi: 10.1097/MRR.0000000000000202. [DOI] [PubMed] [Google Scholar]
- 8.Thoomes-de Graaf M, Scholten-Peeters GG, Schellingerhout JM, Bourne AM, Buchbinder R, Koehorst M, et al. Evaluation of measurement properties of self-administered PROMs aimed at patients with non-specific shoulder pain and “activity limitations”: a systematic review. Qual Life Res. 2016;25(9):2141–2160. doi: 10.1007/s11136-016-1277-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt S, Ferrer M, Gonzalez M, Gonzalez N, Valderas JM, Alonso J, et al. Evaluation of shoulder-specific patient-reported outcome measures: a systematic and standardized comparison of available evidence. J Shoulder Elb Surg. 2014;23(3):434–444. doi: 10.1016/j.jse.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 10.Resnik L, Borgia M, Silver B, Cancio J. Systematic review of measures of impairment and activity limitation for persons with upper limb trauma and amputation. Arch Phys Med Rehabil. 2017;98(9):1863–1892.e14. doi: 10.1016/j.apmr.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 11.Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The patient-reported outcomes measurement information system (PROMIS): progress of an NIH roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riley WT, Rothrock N, Bruce B, Christodolou C, Cook K, Hahn EA, et al. Patient-reported outcomes measurement information system (PROMIS) domain names and definitions revisions: further evaluation of content validity in IRT-derived item banks. Qual Life Res. 2010;19(9):1311–1321. doi: 10.1007/s11136-010-9694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reeve BB, Hays RD, Bjorner JB, Cook KF, Crane PK, Teresi JA, et al. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the patient-reported outcomes measurement information system (PROMIS) Med Care. 2007;45(5 Suppl 1):S22–S31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- 15.Kaat AJ, Buckenmaier CT, 3rd, Cook KF, Rothrock NE, Schalet BD, Gershon RC, et al. The expansion and validation of a new upper extremity item bank for the patient-reported outcomes measurement information system(R) (PROMIS) J Patient Rep Outcomes. 2019;3(1):69. doi: 10.1186/s41687-019-0158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haan EA, Terwee CB, Van Wier MF, Willigenburg NW, Van Deurzen DFP, Pisters MF, et al. Translation, cross-cultural and construct validity of the Dutch-Flemish PROMIS(R) upper extremity item bank v2.0. Qual Life Res. 2020. 10.1007/s11136-019-02388-2. [DOI] [PubMed]
- 17.van Bruggen SGJ, Lameijer CM, Terwee CB. Structural validity and construct validity of the Dutch-Flemish PROMIS((R)) physical function-upper extremity version 2.0 item bank in Dutch patients with upper extremity injuries. Disabil Rehabil. 2019:1–9. 10.1080/09638288.2019.1651908. [DOI] [PubMed]
- 18.Magis D. Random generation of response patterns under computerized adaptive testing with the R package catR. J Stat Softw. 2012;48:1–31. doi: 10.18637/jss.v048.i08. [DOI] [Google Scholar]
- 19.Van Eck ME, Lameijer CM, El Moumni M. Structural validity of the Dutch version of the disability of arm, shoulder and hand questionnaire (DASH-DLV) in adult patients with hand and wrist injuries. BMC Musculoskelet Disord. 2018;19(1):207. doi: 10.1186/s12891-018-2114-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Veehof MM, Sleegers EJ, van Veldhoven NH, Schuurman AH, van Meeteren NL. Psychometric qualities of the Dutch language version of the disabilities of the arm, shoulder, and hand questionnaire (DASH-DLV) J Hand Ther. 2002;15(4):347–354. doi: 10.1016/S0894-1130(02)80006-0. [DOI] [PubMed] [Google Scholar]
- 21.Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop. 2008;32(1):1–6. doi: 10.1007/s00264-007-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chung BT, Morris SF. Reliability and internal validity of the Michigan hand questionnaire. Ann Plast Surg. 2014;73(4):385–389. doi: 10.1097/SAP.0b013e31827fb3db. [DOI] [PubMed] [Google Scholar]
- 23.Chung BT, Morris SF. Confirmatory factor analysis of the Michigan hand questionnaire. Ann Plast Surg. 2015;74(2):176–181. doi: 10.1097/SAP.0b013e3182956659. [DOI] [PubMed] [Google Scholar]
- 24.McMillan CR, Binhammer PA. Which outcome measure is the best? Evaluating responsiveness of the disabilities of the arm, shoulder, and hand questionnaire, the Michigan hand questionnaire and the patient-specific functional scale following hand and wrist surgery. Hand (N Y) 2009;4(3):311–318. doi: 10.1007/s11552-009-9167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.London DA, Stepan JG, Calfee RP. Determining the Michigan hand outcomes questionnaire minimal clinically important difference by means of three methods. Plast Reconstr Surg. 2014;133(3):616–625. doi: 10.1097/PRS.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 26.Maia MV, de Moraes VY, Dos Santos JB, Faloppa F, Belloti JC. Minimal important difference after hand surgery: a prospective assessment for DASH, MHQ, and SF-12. SICOT J. 2016;2:32. doi: 10.1051/sicotj/2016027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cook KF, Kallen MA, Amtmann D. Having a fit: impact of number of items and distribution of data on traditional criteria for assessing IRT's unidimensionality assumption. Qual Life Res. 2009;18(4):447–460. doi: 10.1007/s11136-009-9464-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48:1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- 29.Hu L, Bentler PM. Structural equation modelling. 6. 1999. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives; pp. 1–55. [Google Scholar]
- 30.Rodriguez A, Reise SP, Haviland MG. Applying bifactor statistical indices in the evaluation of psychological measures. J Pers Assess. 2016;98(3):223–237. doi: 10.1080/00223891.2015.1089249. [DOI] [PubMed] [Google Scholar]
- 31.Reise SP, Bonifay WE, Haviland MG. Scoring and modeling psychological measures in the presence of multidimensionality. J Pers Assess. 2013;95(2):129–140. doi: 10.1080/00223891.2012.725437. [DOI] [PubMed] [Google Scholar]
- 32.Christensen KB, Makransky G, Horton M. Critical values for Yen’s Q3: identification of local dependence in the Rasch model using residual correlations. Appl Psychol Meas. 2017;41(3):178–194. doi: 10.1177/0146621616677520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mokken RJ. Theory and procedure of scale analysis: with applications in political research. the Hague: Mouton; 1971. [Google Scholar]
- 34.Van der Ark L. Journal of statitistical software. 20. 2007. Mokken scale analysis in R; pp. 1–19. [Google Scholar]
- 35.Embretson SE, Reise SP. Item response theory for psychologists. Mahwah: Lawrence Erlbaum; 2000.
- 36.Holland P, Wainer H. Differential item functioning. Hillsdale: Lawrence Erlbaum Associates; 1993.
- 37.Choi SW, Gibbons LE, Crane PK. lordif: an R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and Monte Carlo simulations. J Stat Softw. 2011;39(8):1–30. doi: 10.18637/jss.v039.i08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crane PK, Gibbons LE, Jolley L, van Belle G. Differential item functioning analysis with ordinal logistic regression techniques. DIFdetect and difwithpar. Med Care. 2006;44(11 Suppl 3):S115–S123. doi: 10.1097/01.mlr.0000245183.28384.ed. [DOI] [PubMed] [Google Scholar]
- 39.Rose M, Bjorner JB, Gandek B, Bruce B, Fries JF, Ware JE., Jr The PROMIS physical function item bank was calibrated to a standardized metric and shown to improve measurement efficiency. J Clin Epidemiol. 2014;67(5):516–526. doi: 10.1016/j.jclinepi.2013.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chalmers P. A multidimensional item response theory package for the R environment. J Stat Softw. 2012;48:1–29. doi: 10.18637/jss.v048.i06. [DOI] [Google Scholar]
- 41.Orlando M, Thissen D. Further investigation of the performance of S-X2: an item fit index for use with dichotomous item response theory models. Appl Psychol Meas. 2003;27:289–298. doi: 10.1177/0146621603027004004. [DOI] [Google Scholar]
- 42.McKinley R, Mills C. A comparison of several goodness-of-fit statistics. Appl Psych Meas. 1985;9:49–57. doi: 10.1177/014662168500900105. [DOI] [Google Scholar]
- 43.Kaat AJ, Rothrock NE, Vrahas MS, O'Toole RV, Buono SK, Zerhusen T, Jr, et al. Longitudinal validation of the PROMIS physical function item bank in upper extremity trauma. J Orthop Trauma. 2017;31(10):e321–e326. doi: 10.1097/BOT.0000000000000924. [DOI] [PubMed] [Google Scholar]
- 44.Beckmann JT, Hung M, Voss MW, Crum AB, Bounsanga J, Tyser AR. Evaluation of the patient-reported outcomes measurement information system upper extremity computer adaptive test. J Hand Surg Am. 2016;41(7):739–744.e4. doi: 10.1016/j.jhsa.2016.04.025. [DOI] [PubMed] [Google Scholar]
- 45.Hung Man, Voss Maren W., Bounsanga Jerry, Crum Anthony B., Tyser Andrew R. Examination of the PROMIS upper extremity item bank. Journal of Hand Therapy. 2017;30(4):485–490. doi: 10.1016/j.jht.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tyser AR, Beckmann J, Franklin JD, Cheng C, Hon SD, Wang A, et al. Evaluation of the PROMIS physical function computer adaptive test in the upper extremity. J Hand Surg Am. 2014;39(10):2047–2051.e4. doi: 10.1016/j.jhsa.2014.06.130. [DOI] [PubMed] [Google Scholar]
- 47.Crins MH, Roorda LD, Smits N, de Vet HC, Westhovens R, Cella D, et al. Calibration and validation of the Dutch-Flemish PROMIS pain interference item bank in patients with chronic pain. PLoS One. 2015;10(7):e0134094. doi: 10.1371/journal.pone.0134094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crins MH, Roorda LD, Smits N, de Vet HC, Westhovens R, Cella D, et al. Calibration of the Dutch-Flemish PROMIS pain behavior item bank in patients with chronic pain. Eur J Pain. 2016;20(2):284–296. doi: 10.1002/ejp.727. [DOI] [PubMed] [Google Scholar]
- 49.Crins MHP, Terwee CB, Klausch T, Smits N, de Vet HCW, Westhovens R, et al. The Dutch-Flemish PROMIS physical function item bank exhibited strong psychometric properties in patients with chronic pain. J Clin Epidemiol. 2017;87:47–58. doi: 10.1016/j.jclinepi.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 50.Flens G, Smits N, Terwee CB, Dekker J, Huijbrechts I, de Beurs E. Development of a computer adaptive test for depression based on the Dutch-Flemish version of the PROMIS item Bank. Eval Health Prof. 2017;40(1):79–105. doi: 10.1177/0163278716684168. [DOI] [PubMed] [Google Scholar]
- 51.Reise SP, Scheines R, Widman KF, Havilan MG. Multidimensionality and structural coefficients bias in structural equation modeling a bifactor perspective. Educ Psychol Meas. 2013;73:5–26. doi: 10.1177/0013164412449831. [DOI] [Google Scholar]
- 52.Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A, Jr, Orlandini A, et al. Prognostic value of grip strength: findings from the prospective urban rural epidemiology (PURE) study. Lancet. 2015;386(9990):266–273. doi: 10.1016/S0140-6736(14)62000-6. [DOI] [PubMed] [Google Scholar]
- 53.Lameijer CM, Ten Duis HJ, Vroling D, Hartlief MT, El Moumni M, van der Sluis CK. Prevalence of posttraumatic arthritis following distal radius fractures in non-osteoporotic patients and the association with radiological measurements, clinician and patient-reported outcomes. Arch Orthop Trauma Surg. 2018;138(12):1699–1712. doi: 10.1007/s00402-018-3046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lameijer CM, Niezen CK, El Moumni M, van der Sluis CK. Pain, impaired functioning, poor satisfaction and diminished health status eight years following perilunate (fracture) dislocations. Disabil Rehabil. 2018;19:1–8. doi: 10.1080/09638288.2018.1512165. [DOI] [PubMed] [Google Scholar]
- 55.Lameijer C. M., ten Duis H. J., Dusseldorp I. van, Dijkstra P. U., van der Sluis C. K. Prevalence of posttraumatic arthritis and the association with outcome measures following distal radius fractures in non-osteoporotic patients: a systematic review. Archives of Orthopaedic and Trauma Surgery. 2017;137(11):1499–1513. doi: 10.1007/s00402-017-2765-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bechger TM, Maris G. A statistical test for differential item pair functioning. Psychometrika. 2015;80(2):317–340. doi: 10.1007/s11336-014-9408-y. [DOI] [PubMed] [Google Scholar]
- 57.Streiner DL, Norman GR. Health measurement scales. A practical guide to their development and use. New York: Oxford University Press; 2008. [Google Scholar]
- 58.Iordens GIT, Den Hartog D, Tuinebreijer WE, Eygendaal D, Schep NWL, Verhofstad MHJ, et al. Minimal important change and other measurement properties of the Oxford elbow score and the quick disabilities of the arm, shoulder, and hand in patients with a simple elbow dislocation; validation study alongside the multicenter FuncSiE trial. PLoS One. 2017;12(9):e0182557. doi: 10.1371/journal.pone.0182557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goldhahn J, Beaton D, Ladd A, Macdermid J, Hoang-Kim A. Recommendation for measuring clinical outcome in distal radius fractures. Osteoporosis Int. 2012;23:S341. doi: 10.1007/s00402-013-1767-9. [DOI] [PubMed] [Google Scholar]
- 60.Waljee JF, Ladd A, MacDermid JC, Rozental TD, Wolfe SW. Distal radius outcomes consortium. A unified approach to outcomes assessment for distal radius fractures. J Hand Surg Am. 2016;41(4):565–573. doi: 10.1016/j.jhsa.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 61.Makhni EC, Meadows M, Hamamoto JT, Higgins JD, Romeo AA, Verma NN. Patient reported outcomes measurement information system (PROMIS) in the upper extremity: the future of outcomes reporting? J Shoulder Elb Surg. 2017;26(2):352–357. doi: 10.1016/j.jse.2016.09.054. [DOI] [PubMed] [Google Scholar]
- 62.van Bruggen SGJ, Lameijer CM, Terwee CB. Structural validity and construct validity of the Dutch-Flemish PROMIS physical function - upper extremity version 2.0 item bank in Dutch patients with upper extremity injuries. 2019. [DOI] [PubMed] [Google Scholar]
- 63.de Vet HCW, Knol DL, Terwee CB, Mokkink LB. Measurement in medicine. Cambridge: Cambridge University Press; 2011. [Google Scholar]
- 64.Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH) J Orthop Sports Phys Ther. 2014;44(1):30–39. doi: 10.2519/jospt.2014.4893. [DOI] [PubMed] [Google Scholar]
- 65.Shauver MJ, Chung KC. The minimal clinically important difference of the Michigan hand outcomes questionnaire. J Hand Surg Am. 2009;34(3):509–514. doi: 10.1016/j.jhsa.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Nurs Ethics. 2002;9(1):105–109. doi: 10.1191/0969733002ne486xx. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The Dutch-Flemish dataset used and analyzed during the current study are available from the corresponding author on reasonable request. The US dataset is publicly available on the HealthMeasures Dataverse 10.7910/DVN/IHNIRH.