Depression during childbearing is a major public health concern.1–3 The Agency for Healthcare Research and Quality estimated that 14.5% of women develop depressive episodes during pregnancy and a similar percentage develop depression in the first 3 months following birth.4 The agency commented that the “specifics of the course of a depressive illness with onset during the perinatal period, including the severe physiologic and psychological challenges unique to this period that complicate the identification and management of perinatal depression, seem to suggest that this topic would have a substantial degree of high-quality research. We were surprised by the paucity of research in this area.”4(p90)
Multiple challenges exist with respect to advancing knowledge in the field of perinatal mental health. In the DSM-IV,5 postpartum onset includes the qualifier for a new episode of major depressive disorder (or manic or mixed episode of bipolar disorder or brief psychotic disorder) that begins within 4 weeks of birth. However, from a public health standpoint, women and their newborns suffer regardless of when the episode begins. Intervention for prevalent rather than incident cases will have the greatest impact on public health.
Although a striking 1 of 7 women experience postpartum depression, higher rates have been reported among vulnerable populations, including mothers of preterm infants6 and adolescents, who have rarely been included in studies of perinatal mental health.7 One third of all births in America occur to women enrolled in Medicaid,8 and birth rates are higher in minority than in white women. Several investigators have reported elevated rates of depression among low-income women.9–11 Increased rates of depression are consistent with risk factors for psychiatric illness (high life stress and low social support), which impede access to adequate care.
The majority of studies in perinatal mental health have focused on depression to the relative exclusion of other disorders. A broader scope of perinatal mental illnesses (including comorbidities) is equally if not more appropriate for intervention. A comprehensive conceptualization of perinatal mental health caseness is needed to inform public health screening and treatment development efforts.
The rates of multiple psychiatric disorders (requiring hospitalization or outpatient care) were elevated in primiparae in a large-scale epidemiologic study.2 The overall risk for any psychiatric episode after birth (compared to nonpostpartum women) was elevated for the first 3 months postpartum. However, the disease-specific increased risk for major depression was elevated for 5 months; for bipolar disorder, 2 months; for schizophrenia, 1 month; and for adjustment disorders, 2 months.2 Greater knowledge of strategies to effectively identify and intervene with women of childbearing age (and their families) across a variety of mental disorders is urgently needed.
A consistent finding in epidemiologic studies is the female predominance of most mood disorders, anxiety disorders, and eating disorders, which are maximally prevalent during the childbearing years.12 Women have about twice the risk not only for depression but also for panic disorder, phobias, and generalized anxiety disorder. These disorders commonly precede the onset of depression and comprise important comorbidities.
For example, Mazzeo et al.13 investigated associations among eating disorders and depression during pregnancy and postpartum in a population-based sample. Both binge-eating disorder and bulimia nervosa were positively associated with developing postpartum depression, even when lifetime major depression was controlled.13 National estimates of substance use disorders indicate elevated use associated with major depression (19%) and mania (28%) (odds ratio = 2.5 and 3.9, respectively) compared to adults without mood disorders.14
In this issue of the Journal, the work of Vesga-López et al. and Borri et al. adds to our knowledge about the frequency of and disability associated with Axis 1 disorders and comorbidities in childbearing-aged women. Kim et al. remind us that the psychiatric disorder with the greatest propensity for episode onset postbirth is bipolar disorder (risk of first-time hospital admission postpartum days 0 to 30 = 23.33, 95% CI = 11.52 to 47.24, according to the findings of Munk-Olsen et al.2). Perinatal episodes of bipolar disorder are often undiagnosed or misdiagnosed,15 factors that increase the risk for tragic family consequences.16
These observations support the importance of viewing an episode of illness (and a diagnosis) obtained at one point in time such as during the childbearing period within the framework of the woman’s lifetime health.17 Case characterization becomes an expanded construct. The case is not only a woman with depression, but a woman with depression plus an array of health asset and risk factors that shape intervention approaches and their outcomes. Examples are an individual’s psychiatric and medical comorbidities, health knowledge and education, financial resources, social support, access to psychiatric services, and health plan membership. Such factors serve to contextualize a given case, which creates the opportunity for greater specificity and personalization of interventions, with the promise of improved outcomes.
An advantage of focusing intervention on the perinatal period is that expectant couples and family members are often motivated to make significant changes in health behaviors, such as decreasing cigarette smoking and alcohol use.18,19 Childbearing provides an opportunity for building upon a natural interest in investing in the welfare of offspring by embracing positive health behaviors. Moreover, successful interventions have the potential to both reduce maternal disability and mitigate negative effects on the development of the children and family.
On the other hand, childbearing creates special needs for postpartum women and their families. The low motivation and energy associated with postpartum disorders, plus the physical demands of delivery and caring for the newborn, interfere with the woman’s ability to seek help.20 The tendency of women to prioritize the needs of others is especially strong for women with a new baby. Interpersonal disputes with her partner and disruptions in social relationships also inhibit the woman’s ability to seek assistance.21
The literature on perinatal mental disorders is consistent with other data that demonstrate low recognition and treatment rates.22,23 Women with mental illness identified by primary care practitioners rarely accept referrals or obtain care in psychiatric settings. Additionally, screening and provider education alone have little effect on practice.24 Pincus et al.25 described a conceptual framework for designing depression interventions driven by consideration of the “6 Ps” (patient, provider, practice, plan, purchaser, population). This model was adapted by our team for perinatal disorders (Figure 1). Strategies to address mental disorders during childbearing must include focused efforts to encourage patients toward selfmanagement with family support, to assist clinicians with evidence-based decision making regarding treatment, and to enhance delivery systems to ensure access to treatment.
Figure 1.
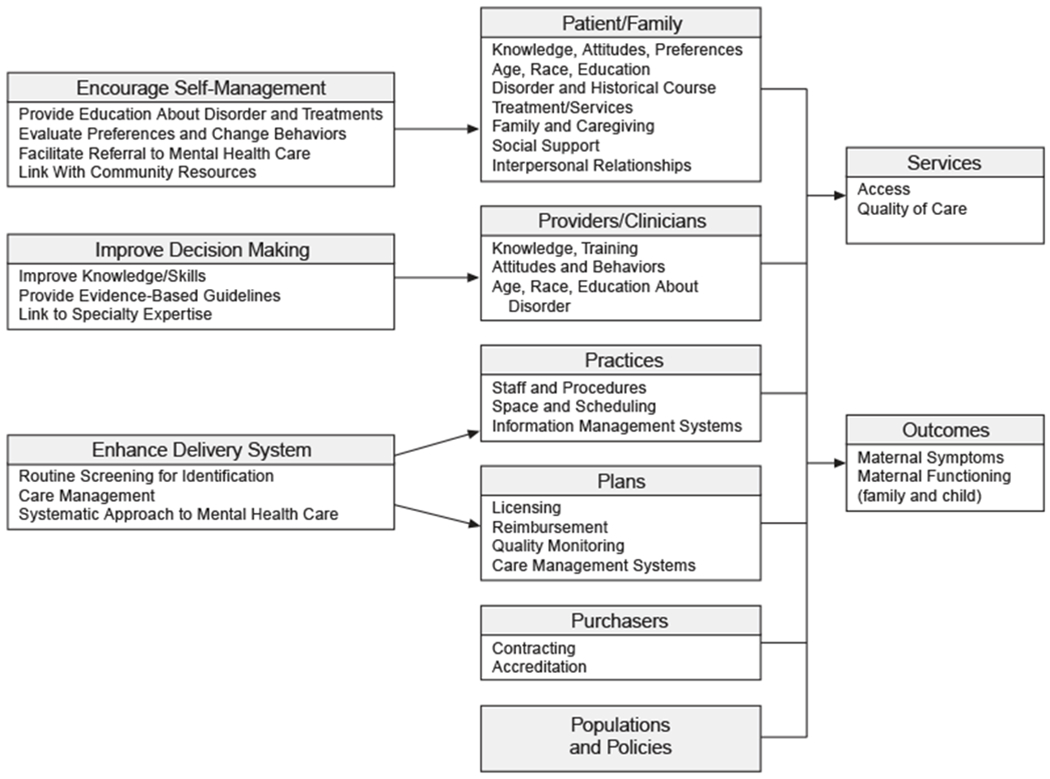
Model for Designing Interventions for Perinatal Psychiatric Disordersa
aBased on Pincus et al.25
Practice issues also impact the care of perinatal women with mental illness. Mental health services must address the disparate health care settings used by new mothers and their unique barriers to care. The fragmentation of health care for women makes identifying a point of responsibility difficult. Obstetrician/gynecologists typically evaluate women at 4 to 6 weeks following delivery, but their ability and motivation to provide ongoing care is limited. They receive limited training in the diagnosis and treatment of psychiatric disorders26 and report greater lack of knowledge and skills compared to other physicians. These physicians are not typically reimbursed for psychiatric treatment.27
Pediatricians have consistent contact with new mothers, but very few identify or treat mothers with mental illness. In addition, practice considerations (private interview space, visit schedules, staffing, and availability of systems for monitoring and follow-up) are prohibitive. Collaborative care, a structured approach based on chronic disease management principles and nonmedical specialists working with the primary care physician and a mental health professional, is a potential solution.28,29 Collaborative care models that incorporate the issues faced by childbearing women and their families hold promise for accessible and effective interventions.22
Challenges at the health plan level frequently involve no or insufficient reimbursement (or other incentives) for the treatment of psychiatric illnesses by primary care professionals (including obstetrician/gynecologists). The separation of mental health from general health services can create a barrier to collaboration between mental health and primary care professionals.27 System-level (rather than physician-level) interventions offer a practical strategy for intervention because systems (such as health plans) have the volume and infrastructure capacity to implant care management models for perinatal disorders that can meet the needs of women across providers.
Psychiatric episodes are the most common medical complications of childbearing. Although perinatal psychiatric disorders have received increasing political attention in the United States, substantial health services and policy investment must follow. Enhanced efforts to develop and implement effective programs to identify women and provide interventions will require coordination of multiple administrative levels within the health care system. The promise is substantial improvement in the health and lives of mothers and their families. Addressing mental illness in childbearing women, an opportune stage of development for intervention, is a long overdue investment in the health of the next generation of Americans.
1606 Gender Differences in Generalized Anxiety Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC).
1617 Axis I Psychopathology and Functional Impairment at the Third Month of Pregnancy: Results From the Perinatal Depression-Research and Screening Unit (PND-ReScU) Study.
1625 A Closer Look at Depression in Mothers Who Kill Their Children: Is It Unipolar or Bipolar Depression?
Contributor Information
Katherine L. Wisner, Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania
Sarah Hudson Scholle, National Committee for Quality Assurance, Washington, D.C.
Bradley Stein, University of Pittsburgh School of Medicine, Community Care Behavioral Health, RAND Corporation, Pittsburgh, Pennsylvania
REFERENCES
- 1.US Department of Health and Human Services: Healthy People 2010. Understanding and Improving Health and Objectives for Improving Health. 2nd ed. Washington, DC: US Government Printing Office; 2000 [Google Scholar]
- 2.Munk-Olsen T, Laursen T, Pederson C, et al. New parents and mental disorders: a population-based register study. JAMA 2006;296(21):2582–2589 [DOI] [PubMed] [Google Scholar]
- 3.Wisner K, Chambers C, Sit D. Postpartum depression a major public health problem. JAMA 2006. December;296(21):2616–2618 [DOI] [PubMed] [Google Scholar]
- 4.Gaynes BN, Gavin N, Meltzer-Brody S, et al. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes. Evidence Report/Technology Assessment: No 119. AHRQ publication 05-E006-1. Rockville, Md: Agency for Healthcare Research and Quality; 2005. Available at: http://www.ahrq.gov/clinic/epcsums/peridepsum.htm Accessed 8-13-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- 6.Logsdon MC, Davis DW, Birkimer JC, et al. Predictors of depression in mothers of pre-term infants. J Social Behav Personality 1997;12:73–88 [Google Scholar]
- 7.Troutman B, Cutrona C. Nonpsychotic postpartum depression among adolescents. J Abnorm Psychol 1990;99:69–78 [DOI] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Centers for Disease Control and Prevention Vital Statistics of the United States, 1999. Vol 1, Natality. Hyattsville, Md: Centers for Disease Control and Prevention; 2001 [Google Scholar]
- 9.Scholle SH, Kelleher K. Preferences for depression advice among low-income women. Matern Child Health J 2003. June;7(2):95–102 [DOI] [PubMed] [Google Scholar]
- 10.Hobfoll SE, Ritter C, Lavin J, et al. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol 1995. June;63(3):445–453 [DOI] [PubMed] [Google Scholar]
- 11.Miranda J, Azocar F, Komaromy M, et al. Unmet mental health needs of women in public-sector gynecologic clinics. Am J Obstet Gynecol 1998. February;178(2):212–217 [DOI] [PubMed] [Google Scholar]
- 12.Grant B, Weissman M. Gender and the Prevalence of Psychiatric Disorders In: Narrow W, First M, Sirovatka P, et al. , eds. Age and Gender Considerations in Psychiatric Diagnosis: A Research Agenda for DSM-V. Arlington, Va: American Psychiatric Association; 2007:31–45 [Google Scholar]
- 13.Mazzeo SE, Slof-Op’t Landt MC, Jones I, et al. Associations among postpartum depression, eating disorders, and perfectionism in a population-based sample of adult women. Int J Eat Disord 2006;39(3):202–211 [DOI] [PubMed] [Google Scholar]
- 14.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004;61(8):807–816 [DOI] [PubMed] [Google Scholar]
- 15.Wisner KL, Peindl KS, Hanusa BH. Psychiatric episodes in women with young children. J Affect Disord 1995;34(1):1–11 [DOI] [PubMed] [Google Scholar]
- 16.Spinelli MG. Infanticide: contrasting views. Arch Womens Ment Health 2005. May;8(1):15–24 [DOI] [PubMed] [Google Scholar]
- 17.Misra DP, Guyer B, Allston A. Integrated perinatal health framework: a multiple determinants model with a life span approach. Am J Prev Med 2003. July;25(1):65–75 [DOI] [PubMed] [Google Scholar]
- 18.Mullen PD. How can more smoking suspension during pregnancy become lifelong abstinence? lessons learned about predictors, interventions, and gaps in our accumulated knowledge. Nicotine Tob Res 2004. April;6(suppl 2):S217–S238 [DOI] [PubMed] [Google Scholar]
- 19.Wisner KL, Sit DKY, Reynolds SK, et al. Psychiatric Disorders In: Gabbe SG, Neibyl JR, Simpson JL, eds. Obstetrics: Normal & Problem Pregnancies. 5th ed. Philadelphia, Pa: Churchill-Livingstone Elsevier;2007:1249–1288 [Google Scholar]
- 20.Holden JM. Postnatal depression: its nature, effects, and identification using the Edinburgh Postnatal Depression scale. Birth 1991;18(4):211–221 [DOI] [PubMed] [Google Scholar]
- 21.O’Hara MW, Stuart S, Gorman LL, et al. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 2000. November;57(11):1039–1045 [DOI] [PubMed] [Google Scholar]
- 22.Georgiopoulos AM, Bryan TL, Wollan P, et al. Routine screening for postpartum depression. J Fam Pract 2001;50(2):117–122 [PubMed] [Google Scholar]
- 23.Bryan TL, Georgiopoulos AM, Harms RW, et al. Incidence of postpartum depression in Olmsted County, Minnesota: a population-based, retrospective study. J Reprod Med 1999. April;44(4):351–358 [PubMed] [Google Scholar]
- 24.Katon W, Gonzales J. A review of randomized trials of psychiatric consultation-liaison studies in primary care. Psychosomatics 1994;35(3):268–278 [DOI] [PubMed] [Google Scholar]
- 25.Pincus H, Pechura C, Elinson L, et al. Depression in primary care: linking clinical and system strategies. Gen Hosp Psychiatry 2001;23:311–318 [DOI] [PubMed] [Google Scholar]
- 26.Schmidt LA, Greenberg BD, Holzman GB, et al. Treatment of depression by obstetrician-gynecologists: a survey study. Obstetrics Gynecol 1997. Aug;90(2):296–300 [DOI] [PubMed] [Google Scholar]
- 27.Williams JW Jr, Rost K, Dietrich AJ, et al. Primary care physicians’ approach to depressive disorders: effects of physician specialty and practice structure. Arch Fam Med 1999;8(1):58–67 [DOI] [PubMed] [Google Scholar]
- 28.Gilbody S, Bower P, Fletcher J, et al. Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Arch Internal Med 2006. November;166(21):2314–2321 [DOI] [PubMed] [Google Scholar]
- 29.Katon WJ, Unutzer J. Pebbles in a pond: NIMH grants stimulate improvements in primary care treatment of depression. Gen Hosp Psychiatry 2006;28(3):185–188 [DOI] [PubMed] [Google Scholar]


