Abstract
Background
Cognitive behavioural therapy (CBT) is an evidence‐based treatment for anxiety disorders. Many people have difficulty accessing treatment, due to a variety of obstacles. Researchers have therefore explored the possibility of using the Internet to deliver CBT; it is important to ensure the decision to promote such treatment is grounded in high quality evidence.
Objectives
To assess the effects of therapist‐supported Internet CBT (ICBT) on remission of anxiety disorder diagnosis and reduction of anxiety symptoms in adults as compared to waiting list control, unguided CBT, or face‐to‐face CBT. Effects of treatment on quality of life and patient satisfaction with the intervention were also assessed.
Search methods
We searched the Cochrane Depression, Anxiety and Neurosis Review Group Specialised Register (CCDANCTR) to 16 March 2015. The CCDANCTR includes relevant randomised controlled trials from MEDLINE, EMBASE, PsycINFO and CENTRAL. We also searched online clinical trial registries and reference lists of included studies. We contacted authors to locate additional trials.
Selection criteria
Each identified study was independently assessed for inclusion by two authors. To be included, studies had to be randomised controlled trials of therapist‐supported ICBT compared to a waiting list, attention, information, or online discussion group; unguided CBT (that is, self‐help); or face‐to‐face CBT. We included studies that treated adults with an anxiety disorder (panic disorder, agoraphobia, social phobia, post‐traumatic stress disorder, acute stress disorder, generalized anxiety disorder, obsessive compulsive disorder, and specific phobia) defined according to the Diagnostic and Statistical Manual of Mental Disorders III, III‐R, IV, IV‐TR or the International Classification of Disesases 9 or 10.
Data collection and analysis
Two authors independently assessed the risk of bias of included studies and judged overall study quality. We used data from intention‐to‐treat analyses wherever possible. We assessed treatment effect for the dichotomous outcome of clinically important improvement in anxiety using a risk ratio (RR) with 95% confidence interval (CI). For disorder‐specific and general anxiety symptom measures and quality of life we assessed continuous scores using standardized mean differences (SMD). We examined statistical heterogeneity using the I2 statistic.
Main results
We screened 1736 citations and selected 38 studies (3214 participants) for inclusion. The studies examined social phobia (11 trials), panic disorder with or without agoraphobia (8 trials), generalized anxiety disorder (5 trials), post‐traumatic stress disorder (2 trials), obsessive compulsive disorder (2 trials), and specific phobia (2 trials). Eight remaining studies included a range of anxiety disorder diagnoses. Studies were conducted in Sweden (18 trials), Australia (14 trials), Switzerland (3 trials), the Netherlands (2 trials), and the USA (1 trial) and investigated a variety of ICBT protocols. Three primary comparisons were identified, therapist‐supported ICBT versus waiting list control, therapist‐supported versus unguided ICBT, and therapist‐supported ICBT versus face‐to‐face CBT.
Low quality evidence from 11 studies (866 participants) contributed to a pooled risk ratio (RR) of 3.75 (95% CI 2.51 to 5.60; I2 = 50%) for clinically important improvement in anxiety at post‐treatment, favouring therapist‐supported ICBT over a waiting list, attention, information, or online discussion group only. The SMD for disorder‐specific symptoms at post‐treatment (28 studies, 2147 participants; SMD ‐1.06, 95% CI ‐1.29 to ‐0.82; I2 = 83%) and general anxiety symptoms at post‐treatment (19 studies, 1496 participants; SMD ‐0.75, 95% CI ‐0.98 to ‐0.52; I2 = 78%) favoured therapist‐supported ICBT; the quality of the evidence for both outcomes was low.
One study compared unguided CBT to therapist‐supported ICBT for clinically important improvement in anxiety at post‐treatment, showing no difference in outcome between treatments (54 participants; very low quality evidence). At post‐treatment there were no clear differences between unguided CBT and therapist‐supported ICBT for disorder‐specific anxiety symptoms (5 studies, 312 participants; SMD ‐0.22, 95% CI ‐0.56 to 0.13; I2 = 58%; very low quality evidence) or general anxiety symptoms (2 studies, 138 participants; SMD 0.28, 95% CI ‐2.21 to 2.78; I2 = 0%; very low quality evidence).
Compared to face‐to‐face CBT, therapist‐supported ICBT showed no significant differences in clinically important improvement in anxiety at post‐treatment (4 studies, 365 participants; RR 1.09, 95% CI 0.89 to 1.34; I2 = 0%; low quality evidence). There were also no clear differences between face‐to‐face and therapist supported ICBT for disorder‐specific anxiety symptoms at post‐treatment (7 studies, 450 participants; SMD 0.06, 95% CI ‐0.25 to 0.37; I2 = 60%; low quality evidence) or general anxiety symptoms at post‐treatment (5 studies, 317 participants; SMD 0.17, 95% CI ‐0.35 to 0.69; I2 = 78%; low quality evidence).
Overall, risk of bias in included studies was low or unclear for most domains. However, due to the nature of psychosocial intervention trials, blinding of participants and personnel, and outcome assessment tended to have a high risk of bias. Heterogeneity across a number of the meta‐analyses was substantial, some was explained by type of anxiety disorder or may be meta‐analytic measurement artefact due to combining many assessment measures. Adverse events were rarely reported.
Authors' conclusions
Therapist‐supported ICBT appears to be an efficacious treatment for anxiety in adults. The evidence comparing therapist‐supported ICBT to waiting list, attention, information, or online discussion group only control was low to moderate quality, the evidence comparing therapist‐supported ICBT to unguided ICBT was very low quality, and comparisons of therapist‐supported ICBT to face‐to‐face CBT were low quality. Further research is needed to better define and measure any potential harms resulting from treatment. These findings suggest that therapist‐supported ICBT is more efficacious than a waiting list, attention, information, or online discussion group only control, and that there may not be a significant difference in outcome between unguided CBT and therapist‐supported ICBT; however, this latter finding must be interpreted with caution due to imprecision. The evidence suggests that therapist‐supported ICBT may not be significantly different from face‐to‐face CBT in reducing anxiety. Future research should explore heterogeneity among studies which is reducing the quality of the evidence body, involve equivalence trials comparing ICBT and face‐to‐face CBT, examine the importance of the role of the therapist in ICBT, and include effectiveness trials of ICBT in real‐world settings. A timely update to this review is needed given the fast pace of this area of research.
Plain language summary
Internet‐based cognitive behavioural therapy with therapist support for anxiety in adults: a review of the evidence
Who may be interested in this review?
People who suffer from anxiety and their families.
General Practitioners.
Professionals working in psychological therapy services.
Developers of Internet‐based therapies for mental health problems.
Why is this review important?
Many adults suffer from anxiety disorders, which have a significant impact on their everyday lives. Anxiety disorders often result in high healthcare costs and high costs to society due to absence from work and reduced quality of life. Research has shown that cognitive behavioural therapy (CBT) is an effective treatment which helps to reduce anxiety. However, many people are not able to access face‐to‐face CBT due to long waiting lists, lack of available time for appointments, transportation problems, and limited numbers of qualified therapists.
Internet‐based CBT (ICBT) provides a possible solution to overcome many of the barriers to accessing face‐to‐face therapy. Therapists can provide support to patients who are accessing Internet‐based therapy by telephone or e‐mail. It is hoped that this will provide a way of increasing access to CBT, particularly for people who live in rural areas. It is not yet known whether ICBT with therapist support is effective in reducing symptoms of anxiety.
What questions does this review aim to answer?
This review aims to summarise current research to find out whether ICBT with therapist support is an effective treatment for anxiety.
The review aims to answer the following questions:
‐ is ICBT with therapist support more effective than no treatment (waiting list)?
‐ how effective is ICBT with therapist support compared with face‐to‐face CBT?
‐ how effective is ICBT with therapist support compared with unguided CBT (self‐help with no therapist input)?
‐ what is the quality of current research on ICBT with therapist support for anxiety?
Which studies were included in the review?
Databases were searched to find all high quality studies of ICBT with therapist support for anxiety published until March 2015. To be included in the review, studies had to be randomised controlled trials involving adults over 18 years with a main diagnosis of an anxiety disorder; 38 studies with a total of 3214 participants were included in the review.
What does the evidence from the review tell us?
ICBT with therapist support was significantly more effective than no treatment (waiting list) at improving anxiety and reducing symptoms. The quality of the evidence was low to moderate.
There was no significant difference in the effectiveness of ICBT with therapist support and unguided CBT, though the quality of the evidence was very low. Patient satisfaction was generally reported to be higher with therapist‐supported ICBT, however patient satisfaction was not formally assessed.
ICBT with therapist support may not differ in effectiveness as compared to face‐to‐face CBT. The quality of the evidence was low.
There was a low risk of bias in the included studies, except for blinding of participants, personnel, and outcome assessment. Adverse events were rarely reported in the studies.
Summary of findings
Background
Description of the condition
Individuals with anxiety disorders experience excessive anxiety (fear or worry) which is disproportionate to actual threat or danger and significantly interferes with normal daily functioning. Anxiety disorders can include a range of physical (for example, trembling, tense muscles, rapid breathing), cognitive (for example, worries, difficulty concentrating), emotional (for example, distress, negative affect, irritability), and behavioural (for example, difficulty sleeping, hyperarousal) symptoms. Often those with anxiety disorders develop maladaptive strategies to lessen anxiety, such as avoidance (Health Canada 2002; Wilson 2006) or substance use (Stewart 2008). Studies from Canada (Statistics Canada 2004), the USA (Kessler 2005a), Australia (Slade 2007), Nigeria (Gureje 2006), and Europe (ESEMeD/MHEDEA 2000 Investigators 2004) suggest that 6% to 18% of adults experience an anxiety disorder every year. Moreover, rates of remission within one year are low, that is, from 33% to 42% across specific anxiety disorders (Robins 1991).
There are many types of anxiety disorders, including panic disorder (PD), agoraphobia, social phobia, post‐traumatic stress disorder (PTSD), acute stress disorder, generalized anxiety disorder (GAD), obsessive compulsive disorder (OCD), and specific phobia. These are diagnosed according to criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM IV‐R) (APA 2000) or the International Classification of Diseases (ICD 10) (WHO 1999). Anxiety disorders often co‐occur with each other (Kessler 2005a) as well as with mood disorders (Fava 2000) and substance abuse or dependence (Stewart 2008). They tend to have an early onset (Kessler 2005b) and chronic course (Bruce 2005). Anxiety disorders also have a major economic impact; for instance, costs of direct treatment, unnecessary medical treatment, and work absences or lost productivity amount to more than USD 40 billion per year in the United States (DuPont 1996; Greenberg 1999). Studies have shown significantly higher annual per capita medical costs for primary care patients with social phobia than for those with no mental health diagnosis (GBP 11,952 and EUR 2957 respectively) (Acarturk 2009); primary care patients with PD versus those with a chronic somatic condition (EUR 10,269 versus EUR 3019) (Batelaan 2007); and primary care patients with GAD as compared to those without GAD (USD 2375 versus USD 1448) (Revicki 2012).
Description of the intervention
Accumulating research supports the efficacy of CBT in the treatment of anxiety disorders (Bisson 2007; Hunot 2007; Norton 2007; Stewart 2009) and anxiety symptoms (Deacon 2004). As its name suggests, CBT includes both cognitive as well as behavioural interventions or techniques. It has no one 'founder' and now exists in many different forms. Its roots, however, lie largely in the work of Aaron Beck (Beck 1979). While pharmacotherapy (most commonly, benzodiazepines or selective serotonin reuptake inhibitors) has been shown to be effective in the treatment of anxiety disorders, meta‐analyses and review articles suggest that CBT is as effective in the acute phase of anxiety and may be more effective than pharmacotherapy or a combination of both treatments in the long term (Westra 1998; Otto 2000; Otto 2005; Pull 2007). Moreover, some anxiety medications pose significant risk for addiction (McNaughton 2008) or serious side effects, or both (Buffett‐Jerrot 2002; Choy 2007).
Unfortunately, certain barriers (for example, time constraints, transportation problems, stigma, long waiting lists, a lack of sufficiently qualified clinicians) continue to limit access to CBT (Alvidrez 1999; Young 2001; Mohr 2006). Many of these barriers are particularly relevant for those living in rural communities (Yuen 1996; Rost 2002; Hauenstein 2006). National surveys in Canada (Statistics Canada 2004) and the US (Kessler 2004) suggested that less than one third (only 32% and 20%, respectively) of those with a current psychiatric disorder received some form of treatment in the past year. In a Canadian sample, only 11% of individuals with an anxiety disorder had received treatment (Ohayon 2000). Increasingly, efforts are being made to improve access to CBT on a large scale, particularly for those groups who are most at risk due to lack of services (for example, the UK‐based National Health Service 'Improving Access to Psychological Therapies' (IAPT) programme launched in 2006) (Department of Health 2008). A distance delivery approach wherein CBT is delivered over the Internet with a therapist providing support by telephone or e‐mail is one way to minimize treatment barriers and increase access to care while still delivering empirically‐supported treatment. Such an approach could increase access to mental health professionals for those in rural areas, facilitate treatment for those of limited mobility, and increase patient confidentiality (that is, by engaging in treatment from home clients do not 'risk' being seen at mental health clinics) and privacy (for example, a degree of visual anonymity). The widespread availability of the Internet makes this type of intervention feasible and worth consideration. Recent systematic reviews of computer‐ and Internet‐based treatment for mental health problems suggest largely that these types of treatment are more effective than a waiting list control and equally effective as face‐to‐face psychotherapy in treating anxiety and depression symptoms (Spek 2007; Bee 2008; Cuijpers 2009; Reger 2009; Cuijpers 2010).
How the intervention might work
Therapist‐supported ICBT should work to treat anxiety in the same manner as conventional face‐to‐face CBT. The underlying principles of CBT posit that psychopathology, or emotional disturbances, are the result of cognitive distortions and maladaptive behaviour. Whereas there are hypotheses about the relative importance of cognitive and behavioural techniques, as well as suggestions that the strong collaborative working relationship between the therapist and client are key to the success of CBT, the exact mechanisms of action in CBT are not yet well understood (Olatunji 2010). It is thought that disorder‐specific symptoms develop as a result of a particular pattern of dysfunctional cognitions in combination with a specific set of behaviours that serve to exacerbate these dysfunctional cognitions further (Beck 2005). As such, CBT works to improve symptoms by treating these maladaptive cognitions and behaviours.
In essence, cognitive techniques and behaviour modification strategies are used to identify, evaluate, and challenge underlying maladaptive thoughts and beliefs. As an example, it is thought that catastrophic thoughts about the outcomes of experiencing arousal‐related physiological sensations, as well as inaccurate predictions about the probability of these dangerous outcomes, and avoidance of situations that may induce these sensations contribute to the development and maintenance of PD (Clark 1986; Barlow 1988). Accordingly, CBT for panic uses cognitive restructuring techniques to teach individuals to identify and challenge their maladaptive cognitions and beliefs. This is combined with the use of gradual, repeated exposure to feared sensations to help individuals revise their perceptions of threat and reduce their fear of these arousal‐related physiological sensations (Landon 2004). A similar description of the CBT model could be provided for the other anxiety disorders (for example, social phobia) (Heimberg 2002). Whereas the underlying cognitive and behavioural principles are evident in the CBT interventions for each of the anxiety disorders, current forms of CBT also target core components of a particular disorder and, as such, specific models of CBT now exist for each disorder, which modify and adapt CBT principles to fit disorder‐specific symptoms (for example, specific phobia (Ost 1997); OCD (Salkovskis 1985; Foa 2010); PD (Clark 1986; Casey 2004); social phobia (Heimberg 2002); GAD (Dugas 2007); PTSD (Ehlers 2000).
ICBT therapists would be expected to draw on these models in the same manner as face‐to‐face CBT therapists. Typically, ICBT involves the client following a written treatment program available on the Internet in conjunction with receiving therapist support, either via telephone calls, texts, or e‐mail (Andersson 2006). The intervention involves content that mimics that of face‐to‐face CBT, therapist‐client contact (albeit through non‐traditional means), and the client engaging in further 'homework' outside of the session. As such, we anticipated that ICBT will work in the same way and as well as traditional face‐to‐face CBT.
Why it is important to do this review
Recently, research into ICBT has elicited considerable interest from within the scientific and clinical communities. With advances in modern communication technologies and their widespread availability, this type of treatment is quickly becoming a more realistic option. These advances have come at a time when long waiting lists and a lack of treatment availability stand in stark contrast to the growing emphasis on the importance of mental health and provision of evidence‐based treatments. A desire to pursue Internet treatment as a viable option to increase access to treatment is growing. The importance of ensuring that the decision to promote such treatment is grounded firmly in high quality evidence is therefore paramount.
The present review asked whether therapist‐supported ICBT is efficacious in treating anxiety, and if it is as efficacious as face‐to‐face CBT. Past meta‐analyses have reviewed the efficacy of ICBT for anxiety symptoms (Spek 2007). A number of reviews that have included ICBT have looked more broadly, however, at health problems in general (Barak 2008; Bee 2008) or all computer‐based interventions (Cuijpers 2009; Reger 2009; Andrews 2010). Moreover, many of these reviews have not focused on the role of therapist involvement (for example, Cuijpers 2009; Reger 2009; Andrews 2010). Ultimately, as the field of ICBT is growing quickly, an updated review on therapist‐supported ICBT is needed. The findings of this review will be helpful in guiding the path of future research in this field away from continued replication of established findings and toward addressing gaps in the literature and considering the next steps in ICBT implementation.
There is a Cochrane Review on media‐delivered CBT and behavioural therapy (BT) (self‐help) for anxiety disorders (Mayo‐Wilson 2013). Mayo‐Wilson's review answers questions about the efficacy of delivering CBT to clients in non‐traditional formats, including via the Internet. In the protocol of their review, Mayo‐Wilson specified that they would not include studies with therapist contact. With a post‐protocol change, they revised their review to include studies that involved therapist contact with the qualifier that the interventions must be able to be delivered stand‐alone without therapist contact. With this in mind, the focus of their review remains largely on self‐help therapies in which therapist involvement is not necessary and treatment is largely client‐driven. Mayo‐Wilson did not conduct analyses separating out those interventions with and without therapist contact. As such, a meta‐analysis with a particular emphasis on the efficacy of therapist‐supported ICBT is needed, particularly as at this point there remains conflicting evidence of the comparable efficacy of self‐help and therapist‐supported interventions (for example, Spek 2007; Titov 2008c; Berger 2011). The present review considered the specific efficacy of therapist‐supported ICBT in comparison to each of a waiting list control (that is, no treatment), traditional face‐to‐face CBT, and self‐help interventions and as such will fill a gap in the literature and answer current calls for research in this area (Reger 2009). The protocol for the present review can be found in the Cochrane Library (Olthuis 2011).
Objectives
To assess the effects of therapist‐supported ICBT on remission of anxiety disorder diagnosis and reduction of anxiety symptoms in adults as compared to waiting list control, unguided CBT, or face‐to‐face CBT. Effects of treatment on quality of life and patient satisfaction with the intervention were also assessed.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel group randomised controlled trials (RCTs), cross‐over, and cluster randomised trials.
Types of participants
Participant characteristics
We included studies of adults (over 18 years of age; no upper limit).
Diagnosis
Participants with a primary diagnosis of an anxiety disorder according to the DSM‐III (APA 1980), DSM‐III‐R (APA 1987), DSM‐IV (APA 1994), DSM‐IV‐TR (APA 2000), ICD‐9 (WHO 1979) or ICD‐10 (WHO 1999) diagnostic criteria.
We included studies that focused on or adequately reported subgroup information for any of the following anxiety disorders: panic disorder (PD) with or without agoraphobia, agoraphobia without a history of panic, social phobia (social anxiety disorder), post‐traumatic stress disorder (PTSD), acute stress disorder, obsessive compulsive disorder (OCD), specific phobia, generalized anxiety disorder (GAD), and anxiety disorder not otherwise specified. Included studies used diagnoses determined using a validated diagnostic instrument, for example, the Structured Clinical Interview for DSM‐IV‐TR Axis I Disorders (SCID‐I) (First 2002).
Setting
We included studies in which treatment entailed participants engaging in the treatment from their homes and therapists located at primary care settings, university laboratories, community mental health clinics, or private practice clinics. Participants could be treatment‐seeking community members responding to media advertisements for study participation or they could be referred to the study by a health professional.
Co‐morbidities
We included studies of participants with co‐morbid diagnoses (for example, major depressive disorder, substance abuse) only if they had been diagnosed with a primary anxiety disorder. We did not include studies of participants reporting anxiety symptoms that did not meet criteria for an anxiety disorder (for example, participants with a clinical presentation of major depressive disorder who reported subthreshold anxiety symptoms or participants scoring high on measures of anxiety symptoms but who were not assessed for a DSM diagnosis).
Types of interventions
Experimental interventions
Cognitive behavioural therapies
We included studies that investigated the efficacy of a therapist‐supported Internet cognitive behavioural therapy (CBT), behavioural therapy (BT), or cognitive therapy (CT) intervention for anxiety, defined as the following.
BT interventions must have been designed to change the behaviours that result from maladaptive anxiety‐related cognitions (we included interventions including, but not limited to, exposure, desensitization, and behavioural experiments).
CT must have been focused on elements of cognitive restructuring of irrational or maladaptive anxiety‐related cognitions.
CBT interventions consisted of some combination of the elements of CT and BT.
Whereas psychoeducation often is an important part of CBT, we did not consider psychoeducation alone to be a sufficient CBT intervention unless it included some of the other treatment components described here.
Internet interventions
To be considered an Internet intervention, CBT must have been delivered over the Internet through the use of web pages or e‐mail, or both. Crucially, Internet interventions must have included therapist support but this interaction could not be face‐to‐face. However, we included interventions that involved an initial face‐to‐face intake or interview session or an initial session to orient clients to the Internet delivery method or to engage in treatment planning, or a combination of these. Thus, therapist support must have occurred via e‐mail or the telephone, or both. Including only interventions that could be delivered entirely by distance methods reflected a primary motive for conducting this review, to find ways to increase access to treatment for those who may not be able to visit provider centres. While it was possible that Internet‐based interventions that provided some support in a face‐to‐face setting could be just as effectively restructured to be delivered completely by distance, it was more rigorous to include only studies that provided evidence specifically on the efficacy of Internet CBT delivered completely via distance methods. We did not select interventions based on their length, or the number or duration of sessions.
Comparator interventions
Waiting list, attention, information, or online discussion group only control condition (no intervention for participants beyond weekly status monitoring by research personnel or accessing online non‐treatment related disease information or discussion groups)
Unguided CBT (i.e., self‐help CBT with no therapist support)
Conventional face‐to‐face CBT interventions (including individual or group CBT delivered in a traditional face‐to‐face format)
Types of outcome measures
Primary outcomes
Efficacy of therapist‐supported ICBT in leading to clinically important improvement in anxiety as determined by a diagnostic interview, for example, the SCID‐I (First 2002) or the Anxiety Disorders Interview Schedule (ADIS‐IV) (DiNardo 1994) or a defined cut‐off on a validated scale, for example, the Yale Brown Obsessive Compulsive Scale (YBOCS) (Goodman 1989). In case the Clinical Global Impression scale change or improvement items (CGI) (Guy 1976) were used, we employed a score of 1 = 'very much' or 2 = 'much improved' to indicate clinically important improvement.
Efficacy of therapist‐supported ICBT in leading to reduction in anxiety symptom severity measured by scores on a validated, observer‐rated instrument, for example, the Hamilton Anxiety Rating Scale (Hamilton 1959), or a validated self‐report measure of: (a) disorder‐specific symptoms, for example, the Social Phobia Scale (SPS) (Mattick 1998), and (b) anxiety symptoms in general, for example, the Beck Anxiety Inventory (BAI) (Beck 1991).
Secondary outcomes
Quality of life as assessed by either measures of quality of life, for example, the Quality of Life Inventory (QOLI) (Frisch 1992), or measures of disability, for example the Sheehan Disability Scales (SDS) (Leon 1997) as increasing disability entails decreased quality of life. While research suggests that quality of life and disability are distinct but somewhat overlapping constructs (Hambrick 2003), quality of life measures have not often been conceptually or operationally distinguished from measures of disability, resulting in considerable overlap amongst indices of quality of life and disability (Mogotsi 2000). With this in mind, we anticipated an overlapping conceptualization of these two constructs in the included studies and included both types of measures within the meta‐analysis in order to capture all possible information about treatment outcome related to quality of life.
Participant satisfaction with the intervention. Participant satisfaction tends to be measured uniquely across different studies using a mix of qualitative and quantitative indices. In anticipation of this, we evaluated participants' satisfaction with the intervention of interest as compared to the comparator interventions in a qualitative manner.
Adverse events, in whatever manner reported by study authors.
Timing of outcome assessment
We performed separate analyses based on different periods of assessment: immediately post‐treatment and at one follow‐up period at least six months post‐treatment but not more than one year. When studies reported more than one follow‐up assessment point, we used the longest follow‐up period so as to provide the best estimate of the long‐term outcomes of the intervention.
Hierarchy of outcome measures
For primary outcomes, separate meta‐analyses were conducted for the two outcomes. The clinically important improvement in anxiety outcome measures were selected according to the following hierarchy, based on availability in a particular study: (1) diagnostic interview, (2) cut‐off on a validated scale, (3) CGI scores. For reduction in anxiety symptom severity, the outcomes of available observer‐rated and self‐report measures were statistically combined and a mean score was created across the measures within a particular study. Measures of variance for this mean score were created by combining standard deviations across studies according to the method described by Borenstein 2009. This method requires that the correlation between two measures be known; as such, in the case that this correlation was not known, the measures with better psychometric properties were included in the analysis.
For secondary outcomes, quality of life outcome measures were treated in the same way as anxiety symptom severity measures. Due to the qualitative nature of the other secondary outcome, participant satisfaction with the intervention, a hierarchy of outcome measures was not required.
Search methods for identification of studies
We used several methods to identify both published and unpublished studies for possible inclusion in this review (see below). We did not restrict studies to those reported in any particular language; however, we conducted searches in English and initiated contact with authors in English.
Electronic searches
The Cochrane, Depression, Anxiety and Neurosis Review Group's Specialised Register (CCDANCTR)
The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintains two clinical trials registers at their editorial base in Bristol, UK, a references register and a studies‐based register. The CCDANCTR‐References Register contains over 39,500 reports of RCTs in depression, anxiety, and neurosis. Approximately 60% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register and records are linked between the two registers through the use of unique Study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Co‐ordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950 to date), EMBASE (1974 to date) and PsycINFO (1967 to date); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), and review‐specific searches of additional databases. Reports of trials are also sourced from international trial registers via the World Health Organisation (WHO International Clinical Trials Registry Platform (ICTRP), ClinicalTrials.gov, drug companies, and the handsearching of key journals, conference proceedings, and other (non‐Cochrane) systematic reviews and meta‐analyses.
Details of CCDAN's generic search strategies can be found on the Group‘s website (http://cmd.cochrane.org/), or available on request from the Trials Search Co‐ordinator (email: tsc@ccdan.org).
To date, three searches have been run for this review. Two for the first published version (with searches to 12 April 2013 and 25 September 2014, Appendix 1) and the latest search to 16 March 2015 (listed below). All findings have now been fully incorporated into the meta‐analyses.
1. CCDANCTR‐Studies and CCDANCTR References:
The CCDANCTR was searched all years to 16 March 2015 using the following (amended) search strategy and results de‐duplicated against those retrieved previously (using the Cochrane Register of Studies (CRS) software).
#1 (anxiety or *phobi* or PTSD or post‐trauma* or “post trauma*” or posttrauma* or (stress and disorder*) or panic or OCD or obsess* or compulsi* or GAD):ti,ab,kw #2 (therap* or train*):ti,ab #3 (acceptance* or assertive* or brief* or commitment* or exposure or group or implosive or “problem solving” or problem‐solving or "solution focused" or solution‐focused or schema):ti,ab,kw #4 (psychotherap* or *CBT* or cognitive or behavio* or “contingency management” or “functional analys*” or mindfulness* or “mind training” or psychoeducat* or relaxation or “role play*”):ti,ab,kw,ky,mh,mc,emt #5 ((#2 and #3) or #4) #6 (computer* or distance* or remote or tele* or Internet* or web* or WWW or phone or mobile or e‐mail* or email* or online* or on‐line or videoconferenc* or video‐conferenc* or "chat room*" or "instant messaging" or iCBT):ti,ab,kw #7 (#1 and #5 and #6) #8 (internet* or online or web*):ti #9 (anxi* or *phobi* or panic or GAD or "general* anxiety" or OCD or obsess* or PTSD or *trauma* or "stress disorder*"):ti #10 (assisted or administer* or administr* or coach* or guided or guidance or *therapist* or ((telephone or email) next (support or assist*))):ti,ab #11 (#8 and #9 and #10) #12 (#7 or #11)
2. International Trial Registries
Trial registries were searched (to 16 March 2015) to identify unpublished and/or ongoing studies. These included ClinicalTrials.gov and the WHO International Clinical Trials Registry Portal (ICTRP).
Searching other resources
Reference lists
We examined the reference lists of previous related meta‐analyses (Spek 2007; Bee 2008; Cuijpers 2009; Reger 2009; Andrews 2010; Cuijpers 2010) and of articles selected for inclusion in the present review.
Personal contacts and correspondence
We contacted experts in the field, including principal authors of RCTs in the field of ICBT for anxiety, via e‐mail and asked them if they were aware of any further studies which meet the present review’s inclusion criteria.
Unpublished studies
In order to search for unpublished studies, we searched international trial registries including via the WHO ICTRP (http://apps.who.int/trialsearch/) and ClinicalTrials.gov (www.clinicaltrials.gov) to March 2015.
Data collection and analysis
Selection of studies
In collaboration with the CCDAN Trials Search Co‐ordinator, one review author (JVO) conducted searches of electronic databases and reference lists and contacted authors in order to locate potential trials to be included in the review. Two review authors (JVO and KMB) independently assessed the titles and abstracts of the resulting lists of studies for relevance. We then obtained full articles for potentially relevant abstracts. Both review authors independently assessed the identified trials to determine eligibility as outlined in Criteria for considering studies for this review. We collated and compared assessments. In the case of disagreement with respect to trial eligibility, we made the final decision by discussion and consensus, if necessary with the involvement of another member of the review group (MCW or SHS, or both).
Data extraction and management
We independently extracted data from the included studies regarding methodology and treatment outcomes, and recorded the data using a data extraction spreadsheet designed by one of the review authors (JVO). If the included trials did not provide complete information (for example, details of dropout, group means and standard deviations), we contacted the primary investigator by e‐mail to attempt to obtain unreported data to permit an intention‐to‐treat (ITT) analysis. We contacted other investigators as needed.
Two review authors (JVO and KMB) independently extracted the following data from each trial report:
description of trial, including primary researcher and year of publication;
characteristics of trial methodology, including the diagnostic criteria employed, participant inclusion and exclusion criteria, the screening instrument(s) used, the inclusion or exclusion of co‐morbidity, the receipt of other interventions simultaneously, and the number of centres involved;
characteristics of participants, including age, gender, primary diagnosis, any co‐morbid diagnoses, and duration of primary symptoms;
characteristics of the intervention (for both the experimental and comparator interventions), including intervention classification (i.e., CBT, BT, CT), content and components (e.g., psychoeducation, relaxation training, exposure, cognitive restructuring), method of delivery of therapist support (e.g., telephone, e‐mail), duration, amount of therapist and experimenter contact, and number of participants randomised to each intervention; and
outcome measures employed, as listed in Types of outcome measures, as well as the dropout rates for participants in each treatment condition and whether the data reflected intention‐to‐treat (ITT) analyses with last observation carried forward (LOCF) or another method.
We subsequently recorded data in RevMan 5.3 data tables (RevMan 2014).
Main planned comparisons
We planned to compare each of the outcomes of interest, at post‐treatment and 6 to 12 month follow‐up, for each of the following comparisons:
therapist‐supported ICBT versus waiting list, attention, information, or online discussion group only control,
therapist‐supported ICBT versus unguided CBT, and
therapist‐supported ICBT versus face‐to‐face CBT.
Assessment of risk of bias in included studies
We assessed the risk of bias in each included study using the Cochrane Collaboration’s 'risk of bias' tool (Higgins 2011a). We assessed the following six areas for risk of bias.
Sequence generation: was the allocation sequence of participants adequately randomised?
Allocation concealment: was the allocation sequence adequately concealed from participants as well as those involved in the enrolment and assignment of participants?
Blinding: were participants, study personnel, and those assessing outcomes kept unaware of participants’ allocation to a study condition throughout the course of the investigation?
Incomplete outcome data: were there incomplete data for the main or secondary outcomes (e.g., due to attrition)? Were incomplete data adequately addressed?
Selective reporting: was the study free of suggestions of selective reporting of outcomes (e.g., reporting of a subset of outcomes on the basis of the results)?
Other potential threats to bias: was the study free of any other problems (e.g., early stopping, baseline imbalance, cross‐over trials) that could have introduced bias?
We did not assess risk of bias related to therapist experience and qualifications. Evidence in the field as to the impact of therapist experience on treatment outcomes remains mixed (for example, Hahlweg 2001; Andersson 2012; Norton 2014), as such, it would be inappropriate to impose bias on a study based on a characteristic we are unsure would actually introduce bias. In addition, we did not assess risk of bias related to therapist allegiance. This was because: (a) all studies investigated CBT, and (b) it would have been impossible to know if researchers were allied with a particular type of delivery method.
Two review authors (JVO and KMB) independently assessed risk of bias for each included study. We resolved disagreements by consensus and discussion with a third review author (MCW or SHS) where necessary. If further information about a particular trial was required to assess its risk of bias, we contacted the primary investigator of the relevant study. We created 'risk of bias' tables describing the information outlined above, as reported in each study. These tables also include a judgement on the risk of bias, made by the review authors for each of the six areas, based on the following three categories: (1) low risk of bias, (2) high risk of bias, and (3) unclear or unknown risk of bias.
Measures of treatment effect
Dichotomous outcomes
We analysed our only dichotomous outcome, clinically important improvement in anxiety (yes or no) (as measured by no longer meeting diagnostic criteria on a diagnostic interview, no longer meeting a designated cut‐off on a validated scale, or meeting the criteria for very much or much improved on the CGI) using risk ratios (RRs) and 95% confidence intervals (CIs) within studies.
Continuous outcomes
As most studies that were selected for inclusion used different measures to assess sufficiently similar constructs, we compared continuous outcomes (that is, general and disorder‐specific anxiety symptoms, quality of life) by calculating the standardized mean difference (SMD) and its 95% CI. However, when all of the studies within a meta‐analysis used the same measure to assess an outcome (for example, if all studies within a meta‐analysis used the BAI to assess general anxiety symptoms), we compared continuous outcomes by calculating the mean difference (MD) to facilitate the interpretation of the clinical relevance of the findings.
Most included studies used more than one measure to assess each of the continuous outcomes. Thus, a mean score was created across the measures included within each study. Measures of variance for this mean score were created by combining standard deviations across studies according to the method described by Borenstein 2009. This method requires that the correlation between two measures be known; as such, on the rare occasion when this correlation was not known and could not be identified in prior literature the measure in question was excluded from analyses. This occurred in five instances (Klein 2006, Richards 2006, and Kiropoulos 2008 for the Body Vigilance Scale; Andersson 2009 and Andersson 2013 for the Fear Survey Schedule III). A sixth study simply included too many measures to be meaningfully combined (Berger 2014) and so the Brief Symptom Index was used as a proxy to index disorder‐specific symptoms.
To combine measures of quality of life and disability into one outcome, we reversed the scores of the disability measures (that is, by subtracting mean scores from the measure total scores) to align them with the quality of life measures.
Endpoint versus change data
We anticipated that we might encounter some studies that reported analyses based on changes from baseline and other studies that reported analyses based on final values. We planned to present the two types of analysis results in separate subgroups to avoid confusion for readers and, where appropriate, to combine both types of scores in the final results. Despite these plans, none of the included studies reported change data so we used endpoint data in all meta‐analyses.
Skewed data
We dealt with skewed data according to the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a) and Higgins 2008. In order to conduct the final analysis, transformed or untransformed data had to be obtained for all studies because log‐transformed and untransformed data cannot be combined in meta‐analyses (Higgins 2011a). In the case that a limited number of studies included in one meta‐analysis presented log‐transformed data, we back‐transformed these data and included untransformed data in the meta‐analysis. We then conducted a sensitivity analysis excluding any studies that presented transformed data.
Unit of analysis issues
Parallel group randomised controlled trials (RCTs)
In some parallel group RCTs, participants randomly assigned to a waiting list, attention, information, or online discussion group only control were permitted to pursue the active treatment after their period on the waiting list was complete. To analyse dichotomous and continuous data for these trials, we only included data from participants before they crossed over to their second treatment condition; in other words, only data from the original comparison (waiting list, attention, information, or online discussion group only control versus therapist‐supported ICBT) was used in the meta‐analyses.
Cross‐over trials
When included studies were cross‐over trials, we planned to include only data from the first phase of the trial.
Cluster randomised trials
When cluster randomised trials had accounted for clustering within their analyses (through the use of multilevel modelling or general estimating equations, for example) we planned to include data directly in the meta‐analyses. For studies that failed to appropriately account for clustering, we planned to impute the data based on the number of clusters reported in each intervention group, the size of each cluster, summary statistics, and an estimate of intracluster correlation. We also planned to exclude cluster trials with a high risk of bias (that is, where clustering was not accounted for in analyses) from sensitivity analyses.
Multiple intervention arms
When multiple intervention arms met our inclusion criteria, we planned to combine eligible groups to create a pair‐wise comparison following the procedure outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We planned to conduct sensitivity analyses excluding any studies with multiple intervention arms that did not report all intervention comparisons.
Dealing with missing data
We used data from ITT analyses whenever they were reported by study authors. In 21 studies, authors employed a LOCF method to address missing data with the assumption that participants who were missing data following randomisation (that is, dropouts) did not respond to treatment. Of the remaining studies, two studies used multiple imputation methods to create ITT data (Kok 2012; van Ballegooijen 2013). Seven studies used a mixed effects models approach in an ITT approach to deal with missing data (Bergstrom 2010; Berger 2011; Hedman 2011; Paxling 2011; Andersson 2012a; Andersson 2012b; Silfvernagel 2012). Two studies did not include ITT data (Andersson 2009; Andersson 2013). One study did not report whether they used ITT data (Greist 2012).
Because included studies did not report individual participant data, if authors did not provide ITT analyses in their manuscript we contacted the primary investigator by e‐mail to attempt to obtain unreported data to permit an ITT analysis. When we did not receive responses from study authors we simply included their reported, non‐ITT, continuous outcome data in the analysis. This was the case for two studies (Andersson 2009; Andersson 2013). For dichotomous outcomes, we were able to impute ITT data by assuming that participants who had dropped out did not meet the target event (that is, clinically important improvement in anxiety). We conducted sensitivity analyses excluding studies for which ITT data were not available (either from the published manuscript or from study authors) to determine the extent to which missing data influenced effect sizes.
If included trials did not provide complete information (that is, group means, standard deviations, and sample size), we contacted the primary investigator by e‐mail to attempt to obtain unreported data. We contacted other study investigators as needed. The only sources for outcome data were the original published report or author correspondence. If standard deviations were not available from the authors, we planned to calculate these using other data reported in the article, including t‐values, CIs, and standard errors. If that was not possible, we planned to impute standard deviations from other investigations using similar measures and populations.
Assessment of heterogeneity
We tested the extent of statistical heterogeneity in meta‐analyses using the I2 statistic (Higgins 2002), which calculates the percentage of variability due to heterogeneity rather than chance. According to the guidelines outlined in the Cochrane Handbook for Systematic Reviews of Interventions, I2 values may be interpreted as follows:
0% to 40% might not be important;
30% to 60% may represent moderate heterogeneity;
50% to 90% may represent substantial heterogeneity; and
75% to 100% represents considerable heterogeneity (Higgins 2011a).
We interpreted the importance of these I2 values in consideration of the magnitude and direction of effects and the strength of evidence for heterogeneity (as indexed by the P value from the Chi2 test). If there was evidence of heterogeneity, we first re‐checked the data for accuracy. We considered sources of heterogeneity according to the pre‐specified subgroup and sensitivity analyses listed in Subgroup analysis and investigation of heterogeneity.
Assessment of reporting biases
Where there were sufficient numbers of trials to make such a plot meaningful (that is, at least 10 included studies (Higgins 2011a)) we constructed funnel plots to determine the possible influence of publication bias. We planned to enhance funnel plots with contour lines delineating areas of statistical significance (as suggested by Peters 2008) to assist in the differentiation of asymmetry due to publication bias or other causes.
Data synthesis
We combined data using an inverse‐variance random‐effects model due to expected variation in the characteristics of the interventions investigated and participant populations. We combined dichotomous outcome measures by computing a pooled risk ratio (RR) and 95% CI. We combined continuous outcomes when means and standard deviations were available. When sufficiently similar continuous outcomes were measured differently across studies we calculated an overall standardized mean difference (SMD) and 95% CI. However, as indicated previously, when outcomes were measured similarly across studies we used a mean difference method. We used the RevMan 5.3 software for data synthesis.
Subgroup analysis and investigation of heterogeneity
We conducted subgroup analyses but interpreted these with caution due to the risk of false positive conclusions. We planned to perform the following subgroup analyses:
gender of participants;
type of anxiety disorder (i.e., PD with or without agoraphobia, agoraphobia without a history of panic, social phobia (social anxiety disorder), PTSD, acute stress disorder, OCD, specific phobia, GAD, and anxiety disorder not otherwise specified);
amount of therapist contact, designated as low (90 min or less), medium (91 to 299 min), or high (300 min or more);
type of CBT (i.e., BT, CT, or CBT); and
research group (i.e., the laboratory from which the study was generated).
We were not able to conduct a subgroup analysis based on gender of participants as none of the included studies distinguished outcomes based on this participant variable. We also were not able to conduct a subgroup analysis based on type of CBT. Only three studies (Andersson 2009; Kok 2012; Andersson 2013) had a stronger focus on BT, as compared to CT or CBT; and no studies examined a CT‐only intervention. For the final subgroup analysis by research group, seven research groups were identified: a group each in Sweden, Switzerland, and the USA; and two distinct groups in Australia and the Netherlands.
Sensitivity analysis
We conducted sensitivity analyses to determine the extent to which observed pooled effect sizes depend on the quality of the design characteristics of studies. We planned to conduct the following sensitivity analyses:
exclusion of studies with a designation of high risk of bias for one or more of the categories as outlined in Assessment of risk of bias in included studies;
exclusion of cluster randomised trials where clustering was not appropriately accounted for in analysis;
exclusion of studies with multiple intervention arms with selective reporting of intervention comparisons;
exclusion of studies with a somewhat more active waiting list control condition (i.e., attention, information, or online discussion group only control)
exclusion of studies with imputed standard deviations for continuous outcomes;
exclusion of studies with back transformed data for continuous outcomes;
exclusion of studies not reporting: (a) dichotomous, and (b) continuous outcomes according to the ITT principle;
exclusion of studies with continuous outcomes analysed using LOCF; and
assuming treatment dropouts were responders for dichotomous outcomes.
Summary of findings
Summary of findings tables were created to present the main findings of the review. We imported meta‐analytic data from RevMan into GRADEprofiler version 3.6 to create summary of findings tables for each of the three most clinically relevant comparisons: ICBT with therapist support versus waiting list control, ICBT with therapist support versus unguided ICBT, and ICBT with therapist support versus face‐to‐face CBT. The summary of findings tables present meta‐analytic outcomes for each of the continuous and dichotomous outcomes at post‐treatment and summarize the number of studies and participants included in each analysis. In addition, GRADEprofiler allowed us to rate the quality of the evidence for each outcome for each comparison considering: (a) risk of bias, (b) inconsistency, (c) indirectness, (d) imprecision, and (e) publication bias.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies
Results of the search
We screened a total of 1736 citations and selected 38 studies with 3214 participants for inclusion.
In detail, searches of the CCDANCTR (all years to 16 March 2015) retrieved a total of 1265 records, including manuscripts in peer‐reviewed journals, conference abstracts, and clinical trial registrations. Secondary search methodologies ‐ including searching the reference lists of eligible studies, contacting experts in the field and conducting additional searches of trial registries ‐ identified a further 471 records. After de‐duplication and following a brief screening of the titles and abstracts, 244 full‐text articles were retrieved for a more detailed evaluation of eligibility.
The PRISMA flow diagram shown in Figure 1 outlines the study selection process and broad reasons for exclusion. Studies were excluded if: (a) participants did not meet diagnostic criteria for an anxiety disorder, as assessed by study authors (population), (b) the intervention of interest was not ICBT, did not involve a therapist, or included too much face‐to‐face therapist contact (intervention), (c) the comparator was not appropriate given our selection criteria (comparator), (d) the trial was not randomised or did not use adequate diagnostic measures (methods), or (e) the trial was ongoing (ongoing). After consolidating references into studies, 38 were eligible for inclusion in the meta‐analyses.
1.
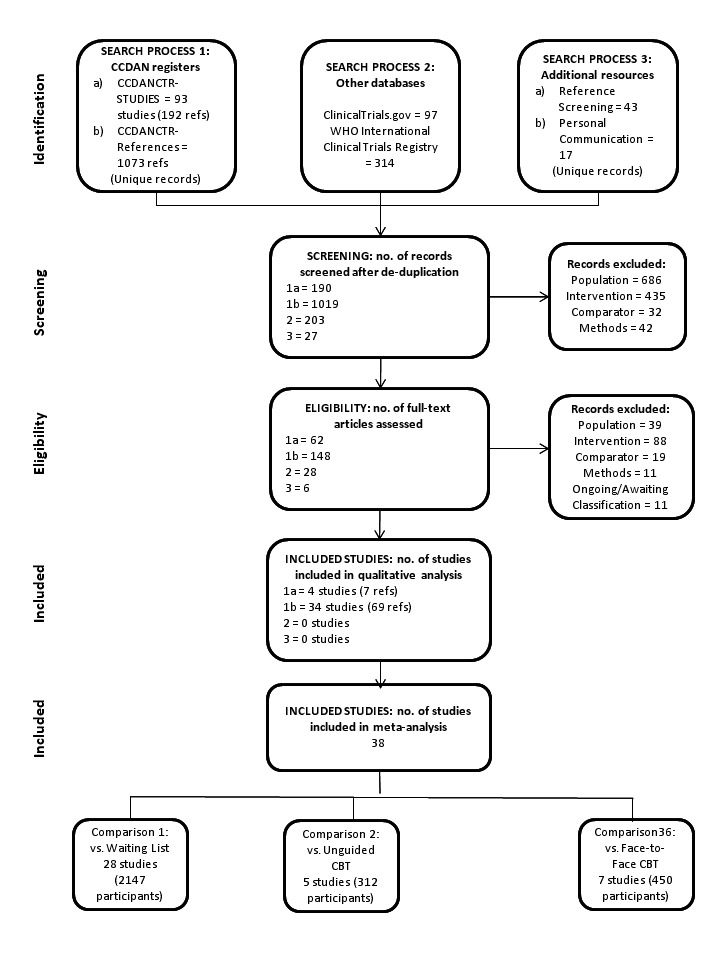
PRISMA diagram of the search process.
E‐mail correspondence for supplemental data was exchanged with Dr Tomas Furmark (Furmark 2009a; Furmark 2009b), Dr Per Carlbring (Carlbring 2001; Carlbring 2006; Carlbring 2007; Carlbring 2011), Dr Nickolai Titov (Titov 2008a; Titov 2008b; Titov 2008c; Titov 2009; Titov 2010; Titov 2011), Dr Britt Klein (Klein 2006; Richards 2006; Kiropoulos 2008), Dr Wouter van Ballegooijen (van Ballegooijen 2013), Dr. Thomas Berger (Berger 2014), and Dr. Jill Newby (Newby 2013).
Included studies
See Characteristics of included studies for details of individual studies and Table 4 for a summary table of the characteristics of the included studies.
1. Summary of included studies table.
| Study | Diagnosis and Co‐morbidity |
Participant Characteristics (M age, age range, sex, country of residence) |
Co‐Use of Medication | N |
Intervention Type & Therapist Duration Contact |
Comparison | Assessment Points | Outcomes | |
| Andersson et al (2009) |
Specific Phobia, Spider Type co‐morbidity not reported |
M age=25.6 (4.1) 18‐65 years 84.8% women Sweden |
Not reported | 27 | IBT with email: 4 wks; 5 online modules | M total time spent per participant = 25 min | Orientation and 1 3‐hour live exposure session | post‐treatment 12‐month follow‐up |
specific phobia sx; general anxiety sx |
| Andersson et al (2012a) |
Social Phobia co‐morbidity included but not reported |
ICBT M age=38.1 (11.3) WLC M age=38.4 (10.9) 19‐71 years 61% women Sweden |
13.7% using medication | 204 | ICBT with email: 9 wks; 9 online modules | M time spent per participant per week = 15 min | Online Discussion Group | post‐treatment | diagnostic status; social phobia sx; QOL; general anxiety sx; |
| Andersson et al (2012b) |
GAD 22.2% Social Phobia, 19.8% PD, 3.7% OCD, 23.5% MDD |
ICBT M age=44.4 (12.8) IPDTM age=36.4 (9.7) WLC M age=39.6 (13.7) 19‐66 years 76.5% women Sweden |
32.1% using medication | 81 | ICBT with email: 8 wks; 8 online modules | M total time spent per participant = 92 min (SD=61) | (1) Waiting List Control (2) IPDT: 8 wks; 8 online modules |
post‐treatment | diagnostic status, GAD sx; general anxiety sx; QOL |
| Andersson et al. (2013) |
Specific Phobia, Snake Type comorbidity not reported |
M age=27.2 (8.1) 19‐54 years 84.6% women Sweden |
Not reported | 30 | IBT with email: 4 wks; 4 online modules | M total time spent per participant = 25 min | Orientation and 1 3‐hour live exposure session | post‐treatment 12‐month follow‐up |
specific phobia sx; general anxiety sx |
| Berger et al (2009) |
Social Phobia 26.9% co‐morbid Axis I disorder |
M age=28.9 (5.3) 19‐43 years 44.2% women Switzerland, France, Belgium |
Excluded | 52 | ICBT with email: 10 wks; 5 online modules |
M=5.5 emails from participant weekly emails from therapist |
Waiting List Control | post‐treatment | social phobia sx; treatment satisfaction |
| Berger et al (2011) |
Social Phobia 38% co‐morbid Axis I disorder; 12% PD, 10% Specific Phobia, 2% GAD, 22% MDD/Dysthymia, 2% ED |
M age=37.2 (11.2) 19‐62 years 53.1% women Switzerland |
7.4% using medication | 81 | ICBT with email: 10 wks; 5 online modules |
M=6.16 (SD=4.56; range=1‐17) emails from participant M=12.44 (SD=2.85; range=6‐17) emails from therapist |
(1) Unguided ICBT 10 weeks; 5 online modules (2) Step‐up on demand ICBT |
post‐treatment 6‐month follow‐up |
diagnostic status; social phobia sx; treatment satisfaction |
| Berger et al. (2014) |
33.3% PD with or without Agoraphobia 85.6% Social Phobia 25% GAD 37.1% PD with or without Agoraphobia, Social Phobia, or GAD, 13.6% MDD, 15.9% Specific Phobia, 5.3% OCD, 12.1% other Axis I disorder |
M age=35.1 (11.4) 18‐65 years 56.1% women Switzerland, Germany, Austria |
14.4% using medication | 132 | ICBT with email: 8 wks; 8 online modules |
M=6.53 (SD=7.2; range=0‐36) emails from participant M=12.6 (SD=4.6; range=8‐35) emails from therapist |
(1) Waiting List Control (2) Tailored ICBT: 8 wks; 8 online modules |
post‐treatment 6‐month follow‐up |
diagnostic status; anxiety sx; general anxiety sx; treatment satisfaction |
| Bergstrom et al (2010) |
15.4% PD 84.6% PD with Agoraphobia co‐morbidity not reported |
ICBT M age=33.8 (9.7) GCBT M age=34.6 (9.2) 18 years or older 61.5% women Sweden |
45% using medication; 34% SSRI/SNRIs, 13% BZ, 24% BZ derivatives or neuroleptics; 5% TCAs | 104 | ICBT with email: 10 wks; 10 online modules |
M=11.3 (SD=4.3) emails from therapist M total time spent per participant = 35.4 min (SD=19) |
10 weekly 2‐hour sessions of GCBT | post‐treatment 6 month follow‐up |
diagnostic status; PD sx; QOL |
| Carlbring et al (2001) |
PD co‐morbidity included but not reported |
M age=34 (7.5) 21‐51 years 71% women Sweden |
64% using medication; 44% SSRIs, 10% BZ, 5% TCAs, 5% beta‐blockers | 41 | ICBT with email: 7‐12 wks; 6 online modules |
M reciprocal emails = 7.5 (SD=1.2; range=6‐15) M total time spent per participant = 90 min |
Waiting List Control | post‐treatment | diagnostic status; PD sx; QOL; general anxiety sx; treatment satisfaction |
| Carlbring et al (2005) |
49% PD 51% PD with Agoraphobia 49% Anxiety Disorder; 6% MDD |
M age=35.0 (7.7) 18‐60 years old 71% women Sweden |
30.6% SSRIs, 8.2% BZ, 6.1% TCAs, 6.1% beta blockers | 49 | ICBT with email: 10 wks; 10 online modules |
M reciprocal emails =15.4 (SD=5.5; range=4‐31) M total time spent per participant =150 min |
10 weekly 45‐60 min sessions of individual CBT | post‐treatment 12‐month follow‐up |
diagnostic status; PD and agoraphobia sx; general anxiety sx; QOL |
| Carlbring et al (2006) |
PD co‐morbidity included but not reported |
M age=36.7 (10) 18‐60 years 60% women Sweden |
54% using medication | 60 | ICBT with email & phone: 10 wks; 10 online modules |
M reciprocal contacts = 13.5 (SD =4.4; range=7‐29) M time spent per participant per week = 12 min M length phone call = 11.8 min (range= 9.6‐15.6) |
Waiting List Control | post‐treatment | diagnostic status; PD and agoraphobia sx; general anxiety sx; QOL; treatment satisfaction |
| Carlbring et al (2007) |
Social Phobia co‐morbidity included but not reported |
ICBT M age=32.4 (9.1) WLC M age=32.9 (9.2) 18‐60 years 64.9% women Sweden |
Included but not reported | 60 | ICBT with email & phone: 9 wks; 9 online modules |
M time spent per participant per week = 22 min M length phone call = 10.5 min (SD= 3.6) |
Waiting List Control | post‐treatment | social phobia sx; general anxiety sx; QOL |
| Carlbring et al (2011) |
9% PD 22% PD with Agoraphobia 39% Social Phobia 20% GAD 13% ADNOS 2% OCD, 2% PTSD, 20% MDD, 7% mild depression; 15% Dysthymia |
M age=38.8 (10.7) 22‐63 years 76% women Sweden |
26% using an antidepressant or anxiolytic | 54 | ICBT with email: 10 wks; 6‐10 online modules | M time spent per participant per week = 15 min | Attention Control 10 wks of posts in an online support forum |
post‐treatment | diagnostic status; anxiety sx (broadly); QOL; general anxiety sx |
| Furmark et al (2009a) |
Social Phobia co‐morbidity not reported |
ICBT M age=35 (10.2) WLC M age=35.7 (10.9) Bib M age=37.7 (10.3) 18 years or older 67.5% women Sweden |
13.9% using medication | 120 | ICBT with email: 9 wks; 9 online modules | M time spent per participant per week = 15 min | (1) Biblio‐therapy: 9 wks; 9 lessons (2) Waiting List Control |
post‐treatment | social phobia sx; general anxiety sx; QOL |
| Furmark et al (2009b) |
Social Phobia co‐morbidity not reported |
ICBT M age=34.9 (8.4) Bib M age=32.5 (8.5) Applied Relaxation M age=36.4 (9.8) 18 years or older 67.8% women Sweden |
6.7% using medication | 115 | ICBT with email: 9 wks; 9 online modules | M time spent per participant per week = 15 min | (1) Biblio‐therapy: 9 wks; 9 lessons (2) Biblio‐therapy and discussion group: 9 wks; 9 lessons (2) Internet‐based applied relaxation: 9 wks; 9 online modules |
post‐treatment | social phobia sx; general anxiety sx; QOL |
| Greist et al. (2012) |
OCD 32% Anxiety Disorder, 31% Mood Disorder, 7% Substance Disorder, 7% ADHD, 2% ED |
M age=38.34 (13.93) 18 years or older 63% women USA |
19.5% using medication | 87 | ICBT with phone: 12 wks; 9 online modules | Weekly phone calls | (1) Unguided ICBT: 12 wks; 9 online modules (2) Lay Coaching ICBT: 12 wks; 9 online modules |
post‐treatment | OCD sx; QOL; treatment satisfaction |
| Hedman et al (2011) |
Social Phobia 47.5% Anxiety Disorder, 15.1% MDD |
ICBT M age=35.2 (11.1) GCBT M age=35.5 (11.6) 18‐64 years 35.7% women Sweden |
19.8% SSRIs, 4.8% SNRIs | 126 | ICBT with email: 15 wks; 15 online modules |
M=17.4 emails per participant M time spent per participant per week = 5.5 min (SD=3.6) |
15 weekly 2.5‐hour sessions of GCBT | post‐treatment 6 month follow‐up |
diagnostic status; social phobia sx; QOL; general anxiety sx |
| Ivarsson et al. (2014) |
PTSD comorbidity not reported |
M age=46 (11.7) 21‐67 years 82.3% women Sweden |
Included but not reported | 62 | ICBT with email: 8 wks; 8 online modules | M time spent per participant per week = 28 min (SD=19.8) | Attention Control: sent weekly question on wellbeing, stress, sleep | post‐treatment | diagnostic status; PTSD sx; general anxiety sx; QOL |
| Johnston et al (2011) |
20.6% PD with or without Agoraphobia 34.4% Social Phobia 45% GAD 29% Anxiety Disorder, 9.2% Affective Disorder, 32.1% both disorders |
M age=41.62 (12.83) 19‐79 years 58.8% women Australia |
29% using medication | 139 | ICBT with email & phone: 10 wks; 8 online modules |
M=8.83 (SD=3.29) emails per participant M=7.54 (SD=2.43) phone calls per participant M total time spent per participant = 69.09 min (SD=32.29) |
Waiting List Control | post‐treatment | disorder‐specific sx; general anxiety sx; QOL; treatment satisfaction |
| Kiropoulos et al (2008) |
41.9% PD 58.1% PD with Agoraphobia 72.1% co‐morbid Mood, Anxiety, Somatoform, or Substance Disorder |
M age=38.96 (11.13) 20‐64 years 72.1% women Australia |
47.7% using medication | 86 | ICBT with email: 6 wks, 6 required & 2 optional online modules |
M=18.24 (SD=9.82) emails from therapist M=10.64 (SD=8.21) emails from participant M total time spent per participant = 352 min (SD=240) |
12 weekly 1‐hour sessions of individual CBT | post‐treatment | diagnostic status; PD and agoraphobia sx; general anxiety sx; QOL; treatment satisfaction |
| Kok et al. (2012) |
41% PD with Agoraphobia 17% Agoraphobia 53.3% Social Phobia 83.5% Specific Phobia Comorbidity included but not reported |
M age=34.6 (11.7) 18 years or older 61% women Netherlands |
43% using medication | 212 | IBT with email: 5wks, 8 online modules | weekly contact by therapist | Waiting List Control: also sent self‐help book without instructions | post‐treatment | phobia sx; general anxiety sx; treatment satisfaction |
| Newby et al. (2013) |
84% GAD Comorbidity included but not fully reported; 56% MDD |
M age=44.3 (12.2) 21‐80 years 77.8% women Australia |
40.4% using medication | 100 | ICBT with email and phone: 10 wks; 6 online modules | M total time spent per participant = 23.37 min (SD=12.15) | Waiting List Control | post‐treatment | GAD sx; QOL; treatment satisfaction |
| Nordgren et al. (2012) |
31% PD with or without Agoraphobia 8% Agoraphobia 32% Social Phobia 10% GAD 19% ADNOS 21% Anxiety Disorder, 43% Mood Disorder, 1% Hypochon‐driasis |
ICBT M age=35 (13) WLC M age=36 (12) 19‐68 years 63% women Sweden |
26% using medication | 100 | ICBT with email: 10 wks; 7‐10 online modules | M time spent per participant = 15 min/week | Attention Control: sent weekly questions on wellbeing | post‐treatment | anxiety sx; general anxiety sx; QOL |
| Paxling et al (2012) |
GAD co‐morbidity included but not fully reported; 22.5% MDD |
M age=39.3 (10.8) 18‐66 years 79.8% women Sweden |
37.1% using medication | 89 | ICBT with email: 8 wks; 8 online modules | M total time spent per participant = 97 min (SD=52) | Waiting List Control | post‐treatment | GAD sx; general anxiety sx; QOL |
| Richards et al (2006) |
21.9% PD 78.1% PD with Agoraphobia 22% Social Phobia, 13% GAD, 9% Specific Phobia, 6% PTSD, 9% MDD, 6% Hypochondriasis, 3% Somatization |
M age=36.59 (9.9) 18‐70 years 68.8% women Australia |
15.6% anti‐depressants, 12.5% BZ, 9.4% antidepressants and BZ | 23 | ICBT with email: 8 wks, 6 online modules |
M=18 (SD=6.5) emails from therapist M=15.3 (SD=12.8) emails from participant M total time spent per participant =376.3 min (SD=156.8) |
Information Only Control Weekly status updates to clinician and access to online non‐CBT info |
post‐treatment | diagnostic status; PD and agoraphobia sx; general anxiety sx; QOL |
| Robinson et al (2010) |
GAD co‐morbidity included but not reported |
M age=46.96 (12.7) 18‐80 years 68.3% women Australia |
Included but not reported | 101 | ICBT with email and phone: 10 wks; 6 online modules |
M =33.2 (SD=4) emails/calls per participant M total time spent per participant = 80.8 min (SD=22.6) |
Waiting List Control | post‐treatment | diagnostic status; GAD sx; QOL; treatment satisfaction |
| Silfvernagel et al (2012) |
7% PD 83% PD with Agoraphobia 16% Social Phobia 19% GAD 2% ADNOS 32% co‐morbid disorder |
M age=32.4 (6.9) 20‐45 years 65% women Sweden |
47% using medication | 57 | ICBT with email: 8 wks; 6‐8 online modules | M time spent per participant = 15 min/week | Waiting List Control | post‐treatment | diagnostic status; PD sx; general anxiety sx; QOL |
| Spence et al (2011) |
PTSD 62% MDD, 33% Social Phobia, 31% PD with or without Agoraphobia, 26% GAD; 17% OCD |
M age=42.6 (13.1) 21‐68 years 81% women Australia |
60% using medication | 44 | ICBT with email & phone: 8 wks; 7 online modules |
M=5.39 (SD=3.54) emails per participant M=7.87 (SD=2.56) phone calls per participant M total time spent per participant = 103.91 min (SD=96.53) |
Waiting List Control | post‐treatment | diagnostic remission; PTSD sx; QOL; general anxiety sx; treatment satisfaction |
| Tillfors et al (2008) |
Social Phobia co‐morbidity included but not reported |
ICBT M age=32.3 (9.7) ICBT+exposure M age= 30.4 (6.3) 19‐53 years 78.9% women Sweden |
Included but not reported | 38 | ICBT with email: 9 wks; 9 online modules | M=35 min per participant per week | ICBT with email (9 online modules) + 5 live 2.25‐hour exposure sessions; 9 wks | post‐treatment 12‐month follow‐up |
social phobia sx; general anxiety sx; QOL; treatment satisfaction |
| Titov et al (2008a) |
Social Phobia co‐morbidity included but not reported |
M age=38.13 (12.24) 18‐72 years 59% women Australia |
29% using medication | 105 | ICBT with email: 10 wks; 6 online modules | M total time spent per participant = 125 min (SD=25) | Waiting List Control | post‐treatment | social phobia sx; QOL; treatment satisfaction |
| Titov et al (2008b) |
Social Phobia co‐morbidity included but not reported |
M age=36.79 (10.93) 20‐61 years 62.96% women Australia |
25.9% using medication | 88 | ICBT with email: 10 wks; 6 online modules | M total time spent per participant = 126.76 min (SD=30.89) | Waiting List Control | post‐treatment | social phobia sx; QOL; treatment satisfaction |
| Titov et al (2008c) |
Social Phobia co‐morbidity included but not reported |
M age=37.97 (11.29) 18‐64 years 61.05% women Australia |
25.9% using medication | 98 | ICBT with email: 10 wks; 6 online modules | M total time spent per participant = 168 min (SD=40) | (1) Unguided ICBT 10 wks; 6 online modules (2) Waiting List Control |
post‐treatment | social phobia sx; QOL; treatment satisfaction |
| Titov et al (2009) |
GAD co‐morbidity included but not reported |
M age=44 (12.98) 18 years or older 76% women Australia |
29% using medication | 48 | ICBT with email & phone: 9 wks, 6 online modules |
M =23.7 emails, 5.5 instant messages, and 4.1 calls per participant M total time spent per participant = 130 min |
Waiting List Control | post‐treatment | diagnostic status; GAD sx; QOL; treatment satisfaction |
| Titov et al (2010) |
26.9% PD with Agoraphobia 29.5% Social Phobia 43.6% GAD 28.2% Anxiety Disorder, 20.5% Affective Disorder, 26.9% both disorders |
M age=39.5 (13) 18 years or older 67.9% women Australia |
47.4% using medication | 86 | ICBT with email & phone: 8 wks; 6 online modules |
M =23.6emails from therapist M total time spent per participant = 46 min (SD=16) |
Waiting List Control | post‐treatment | diagnostic status; disorder‐specific anxiety sx; QOL; treatment satisfaction |
| Titov et al (2011) |
10% PD with or without Agoraphobia 11% Social Phobia 28% GAD 51% MDD 81% had a co‐morbidity |
M age=43.9 (14.6) 18‐79 years 73% women Australia |
54% using medication | 74 | ICBT with email & phone: 10 wks; 8 online modules |
M=5.45 (SD=3.57) emails per participant M=9.35 (SD=2.96) phone calls per participant M total time spent per participant = 84.76 min (SD=50.37) |
Waiting List Control | post‐treatment | disorder‐specific sx; general anxiety sx; QOL; treatment satisfaction |
| Van Ballegooijen et al (2013) |
78% PD with or without Agoraphobia 14% Agoraphobia co‐morbidity included but not reported |
M age=36.6 (11.4) 18‐67 years 67.5% women Netherlands |
Included but not reported | 126 | ICBT with email: 12 wks; 6 online modules | M total time spent per participant = 1 to 2 hours | Waiting List Control | post‐treatment | PD sx; general anxiety sx |
| Wims et al (2010) |
PD with or without Agoraphobia 21% Social Phobia, 31% GAD, 10% OCD, 7% PTSD, 21% MDD |
M age=42.08 (12.29) 18 years or older 76% women Australia |
31% using medication | 59 | ICBT with email: 8 wks; 6 online modules |
M =7.5 emails from therapist M total time spent per participant = 75 min |
Waiting List Control | post‐treatment | diagnostic status; PD & agoraphobia sx; QOL |
| Wootton et al. (2013) |
OCD 26.9% Social Phobia, 40.4% GAD, 15.4% PD, 11.5% PTSD, 38.5% MDD |
ICBT M age=39.93 (12.57) Bib M age=35.55 (9.68) WLC M age=38.58 (10.51) 18‐64 years 75% women Australia |
61.5% using SSRIs | 56 | ICBT with phone: 8 wks, 5 online modules |
M=15.05 (SD=3.93) phone calls per participant M total time spent per participant = 88.63 min (SD=46.41) |
1) Guided bibliotherapy: 8 wks, 5 lessons 2) Waiting List Control |
post‐treatment | diagnostic status; OCD sx; general anxiety sx; treatment satisfaction |
Notes: All data in the above table represent only that included in/relevant to the present review.
ADNOS = anxiety disorder, not otherwise specified; Bib = Bibliotherapy; BZ = benzodiazepine; ED = eating disorder; GAD = generalized anxiety disorder; GCBT = group cognitive behavioural therapy; IBT = internet‐based behavioural therapy; ICBT = internet‐based cognitive behavioural therapy; IPDT = internet‐based psychodynamic therapy; MDD = major depressive disorder; PD = panic disorder; QOL = quality of life; SNRI = serotonin‐norepinephrine re‐uptake inhibitor; SSRI = selective serotonin re‐uptake inhibitor; sx = symptoms; TCA = tricyclic antidepressant; VCBT = videoconferencing cognitive‐behavioural therapy; WLC = waiting list control.
Design
All of the 38 included studies were parallel group RCTs. For studies in which participants in the waiting list, attention, information, or online discussion group only control were given the opportunity to complete the treatment after their time on the waiting list, only data from the original comparison were used in the meta‐analyses. There were no cross‐over or cluster randomised trials.
Ten studies included multiple intervention arms: two (Titov 2008c; Furmark 2009a) compared the intervention of interest to two eligible comparators (a waiting list, and unguided CBT) so were included in multiple meta‐analyses (ICBT versus waiting list control, and ICBT versus unguided CBT), and eight (Richards 2006; Furmark 2009b; Robinson 2010; Berger 2011; Johnston 2011; Berger 2014; Greist 2012; Kok 2012) included a third treatment arm not relevant to the present review.
Sample sizes
Sample sizes of included studies ranged from 21 (12 in the intervention arm, 9 in the comparator arm (Richards 2006)) to 212 participants (105 in the intervention arm, 107 in the comparator arm (Kok 2012)). The average study sample size was 85 participants. In most studies there was an equal distribution of participants between the treatment and control arms. Only 2 studies had < 30 participants, 16 studies had 30 to 60 participants, 9 studies had 60 to 90 participants, and 9 studies had 90 to 140 participants, with 2 outliers at 204 participants (Andersson 2012a) and 212 participants (Kok 2012).
Setting
Included studies came from one research group in Sweden (18 trials), two groups in Australia (Klein et al.: 2 trials; Titov et al.: 12 trials), two groups in the Netherlands (Kok et al.: 1 trial; van Ballegooijen et al.: 1 trial), a research group in Switzerland (3 trials), and one in the USA (1 trial).
Whereas researchers and treating clinicians were located at university‐affiliated hospitals or mental health centres, participants received the intervention of interest in their home. Treatment took place over the Internet and by telephone. Face‐to‐face CBT, when included in a trial, was conducted in a psychiatric setting (for example, hospital, mental health clinic).
Participants
Participants were men and women over 18 years of age. The average mean age of study participants was 37.3 years. Women represented an average of 67.7% of participants in each study. The ethnicity of participants was not reliably reported. For most studies, participants were recruited via media advertisements or a recruitment website (33 studies); in a minority of studies participants were recruited via clinic referrals (Bergstrom 2010; Hedman 2011; Kok 2012; Nordgren 2012). One study recruited using both methods (Greist 2012).
All included participants qualified for one of the following anxiety disorder diagnoses: social phobia (11 trials), PD with or without agoraphobia (8 trials), GAD (5 trials), PTSD (2 trials), OCD (2 trials), and specific phobia (2 trials). The eight remaining studies included participants with a range of anxiety disorder diagnoses. Thirty‐two trials included participants with co‐morbid diagnoses and six studies did not report on their inclusion and exclusion criteria. Among all studies, regardless of their inclusion or exclusion of co‐morbidities, 29 studies excluded participants who scored above a certain threshold on a measure of depressive symptoms, for example, above 30 on the Montgomery‐Asberg Depression Rating Scale (MADRS) (Svanborg 1994), and 33 studies excluded participants who endorsed suicidal ideation, for example, on the MADRS suicide item, with the rationale that they were unclear about how to handle this high risk participant via a distance treatment. Nineteen studies excluded participants with substance misuse or dependence problems and 19 studies excluded participants with active psychosis with the rationale that these problems could interfere with anxiety treatment.
Thirty‐five trials included participants who were using psychiatric medication (including selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, benzodiazepines, benzodiazepine derivatives, neuroleptics, tricyclic antidepressants, beta‐blockers) concurrent with study participation (Berger 2009 excluded those using medication, and Andersson 2009 and Andersson 2013 did not report on co‐use of medication). Participants were typically included only if they had been at a stable dose for a certain time period (one to three months) preceding the study. Six studies (Carlbring 2001; Carlbring 2005; Carlbring 2006; Greist 2012; Newby 2013; van Ballegooijen 2013) included participants engaged in another type of psychological therapy concurrent with study participation, one of which had no participants that met this characteristic (Carlbring 2006).
Interventions
Experimental interventions
Thirty‐five studies included in the present review tested ICBT, while three studies investigated Internet‐based BT with a focus on exposure (Andersson 2009; Kok 2012; Andersson 2013). Interventions involved participants following 4 (Andersson 2013) to 15 (Hedman 2011) online treatment modules (mean = 7; median = 7; mode = 6). Twenty‐nine studies provided e‐mail support from therapists only, two studies provided telephone support from therapists only (Greist 2012; Wootton 2013), and seven studies provided therapist support by email and telephone (Titov 2009; Robinson 2010; Titov 2010; Johnston 2011; Spence 2011; Titov 2011; Newby 2013). Seven studies also included participation in an online discussion forum (Tillfors 2008; Furmark 2009a; Furmark 2009b; Bergstrom 2010; Spence 2011, Titov 2011; Andersson 2012a).
Interventions ranged in length from 4 (Andersson 2009; Andersson 2013) to 15 weeks (Hedman 2011) (mean = 9; median = 9; mode = 10). The degree of therapist involvement in the included interventions was widely variable; the average total time spent by a therapist with a participant ranged from a minimum of 23 minutes (Newby 2013) to a maximum of 376 minutes (Richards 2006), with the overall mean = 128 minutes and median = 120 minutes. Five studies (Berger 2009; Berger 2011; Greist 2012; Kok 2012; Berger 2014) did not report therapist contact time. Similarly, among studies that reported this information, the average number of contacts made by study therapists (email and/or telephone) ranged from a minimum of 5 (Kok 2012) to a maximum of 33 (Robinson 2010), with the overall mean = 15 contacts and median = 14 contacts.
Of the 38 included studies, 13 specified that treatment was provided by a clinical psychologist, 9 specified that treatment was provided by clinical psychology graduate students in training, and 12 specified treatment was provided by both. The four remaining studies described treatment providers as therapists trained by the treatment founder who also provided supervision (Andersson 2009), a clinical psychologist and a clinical social worker (Greist 2012), a practice manager supervised by a clinical psychologist (Newby 2013), and a psychiatry registrar (Wims 2010). Clinical psychology graduate students providing therapy were enrolled in masters or doctoral psychology programs as required for them to practice in their country. Of those studies in which licensed clinical psychologists delivered the treatment, eight specified that clinicians were provided with supervision from an expert in the field. Similarly, of those studies in which clinical psychology students provided treatment, 16 specified that supervision from an expert in the field was provided. Details on the experience and training of study therapists, if provided, can be found in the Characteristics of included studies section.
Comparator Interventions
Twenty‐eight studies compared therapist‐supported ICBT to a waiting list, attention, information, or online discussion group only control. All but eight of these studies included strict waiting list control conditions with no treatment provided to participants and assessments occurring after the designated waiting list period. Of the remaining eight studies, the control condition in one study included a weekly self‐report assessment but no intervention (Furmark 2009a) and in two studies participants completed weekly questions on stress, wellbeing, and/or sleep (Nordgren 2012; Ivarsson 2014). The control condition in two studies (Richards 2006; van Ballegooijen 2013) provided basic non‐treatment disease‐related information to participants and one of these studies (Richards 2006) included weekly status check‐ins by phone. In one study (Kok 2012), participants in the control condition were sent a self‐help book but not provided with any information on how to use it. Finally, the control condition in two studies permitted participants to engage in an online discussion group (Carlbring 2011; Andersson 2012a).
Five studies compared therapist‐supported ICBT to unguided CBT (that is, self‐help). Finally, seven studies compared therapist‐supported ICBT to traditional, face‐to‐face group or individual CBT. This number of studies adds up to more than the total number of included studies because two studies included more than one comparator.
Outcomes
Primary outcomes
Each of the included studies reported on the efficacy of therapist‐supported ICBT. Seventeen studies assessed participants post‐treatment for clinically important improvement in anxiety (a dichotomous outcome) and three studies reassessed this outcome at a follow‐up of 6 to 12 months later. Each of the included studies reported on participants' disorder‐specific anxiety symptom severity using a validated self‐report or observer‐rated instrument (a continuous outcome) at post‐treatment. Eight studies assessed anxiety symptom severity at a follow‐up of 6 to 12 months later. Twenty‐six of the included studies also measured participants' symptoms of general anxiety using validated self‐report instruments at post‐treatment. Seven studies assessed general anxiety at a follow‐up of 6 to 12 months later. Please see Table 4 and Characteristics of included studies for more details of outcome assessment.
It was rare for studies to report adverse events. In fact, adverse events could only be assumed from measures of participants' symptom deterioration during the study or reasons for participant dropout related to the treatment.
Secondary outcomes
Twenty‐nine studies measured quality of life at post‐treatment, while six studies included quality of life as an outcome at 6 to 12 month follow‐up.
Participant satisfaction with treatment was indexed by 19 studies at post‐treatment. A variety of different measures of treatment satisfaction were used ranging in degrees of comprehensiveness and complexity. Across different measurement approaches, participants were most commonly asked to indicate their overall satisfaction with the treatment program, their satisfaction with particular portions of the treatment program (for example, therapist correspondence, Internet modules), and their satisfaction with the pace of the treatment program. Of the 19 studies, only four reported treatment satisfaction for both the experimental and comparator interventions; the remaining trials compared the experimental intervention to a waiting list control, which did not lend itself to an evaluation of satisfaction.
Excluded studies
Studies were excluded for a variety of reasons (see Characteristics of excluded studies and Figure 1, the former of which lists a number of studies that were most like the included studies but differed in important ways that prevented inclusion). Studies were frequently excluded because the intervention was: (a) not distance‐based, (b) distance‐based but included more than two sessions of face‐to‐face contact between therapist and participant, (c) not delivered by a therapist (that is, was a self‐help program), or (d) not CBT. Similarly, studies were excluded if participants did not meet our criteria because they had subclinical anxiety symptoms or an anxiety disorder was not their primary diagnosis. We also excluded a number of studies because a closer look showed that they were not RCTs or did not compare the intervention of interest to a comparison group that met the eligibility criteria.
Ongoing studies
There is a total of nine ongoing studies: Bishop 2012; Clark 2012; Rollman 2012; Titov 2012; Tulbure 2012; Lindner 2013; Miclea 2014, together with Carlbring 2012 and Richards 2014, which we previously classified as awaiting classification (communication with the study authors revealed that these latter two studies are yet to be completed).
A study previously listed as ongoing (Kok 2012) has since been completed and entered as an included study in this review update. Results of two other studies (also previously listed as ongoing) revealed that they no longer qualified for inclusion and have been moved to the excluded studies section (von Essen 2008; Andrews 2012b).
Studies awaiting classification
There are now just two studies awaiting classification compared to 14 listed in the previous version of this review (those identified from the precision maximizing update search of the CCDANCTR Registers in September 2014 (Appendix 1).
The changes (documented below) leave Schreuders 2008 awaiting classification, together with a new study (Tabari 2013) identified from the search of 16 March 2015. These studies appear to qualify for entry in this review but we have been unable to obtain additional data from the trialists who have unfortunately failed to responded to our enquiries.
Studies previously listed as awaiting classification which have now been analysed and entered as included studies include: Greist 2012; Nordgren 2012; Andersson 2013; Newby 2013; Berger 2014; Ivarsson 2014.
We previously listed the following studies as awaiting classification, but the results of the latest search update reveal they no longer qualify for inclusion and so we have moved them to the excluded studies section: Berger 2012; Andrews 2011b; Andrews 2012a. These studies were abandoned due to lack of recruitment.
A closer look at the references of Andrews 2011c and Andrews 2011d (previously awaiting classification) revealed that they were secondary reports of Newby 2013 and Titov 2010 respectively.
Risk of bias in included studies
Results of the risk of bias assessments of included studies are summarized succinctly in Figure 2 and Figure 3. Overall, the risk of bias in the included studies was low, with some notable exceptions related to the nature of clinical trials of psychological treatments.
2.
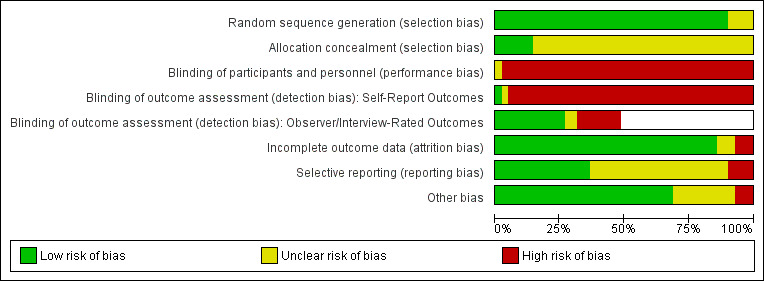
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
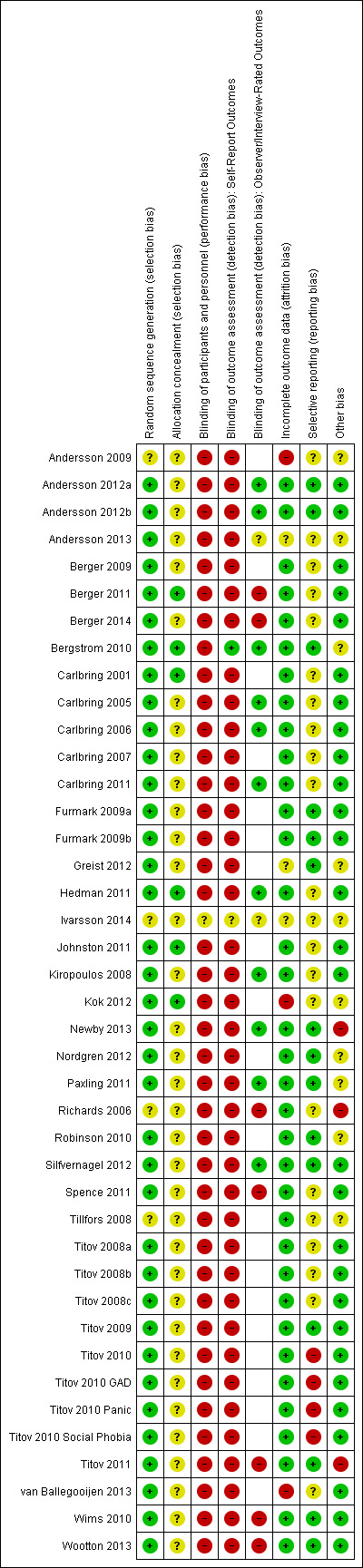
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The majority of included studies (n = 35) used an adequate method of randomisation, primarily an online random number generator, to avoid selection bias. The three remaining studies reported that participants were randomised but did not describe the randomisation procedure.
Most study authors (n = 32) did not adequately report allocation concealment. The remaining six studies reported allocation concealment procedures that would have minimized the risk of selection bias (for example, random assignment was maintained by an independent research team member not involved in other study aspects who gave randomisations to participants just prior to treatment commencement).
Blinding
The blinding of participants and study personnel is difficult when investigating the efficacy of psychological treatments. Unlike pharmacological trials in which medication type can be concealed, it is very difficult to blind participants to the characteristics of the treatment they are receiving as they are active participants. Similarly, it is impossible to blind study therapists to the treatment they are delivering as they take an active role in its execution. As such, each of the included studies was rated as having a high risk of bias because participants and personnel were not blind to treatment assignment. Because this study characteristic was a limitation across studies, we did not conduct sensitivity analyses based on the characteristic. We did however, downgrade study evidence based on this risk of bias in order to remain consistent with the use of GRADE across other disciplines and conditions. With interventions that are difficult or impossible to blind, there are strategies to limit related biases (e.g. participants or therapists who do not favour interventions, intervention providers in both groups believing they are delivering the ‘best’ treatment, and measuring potential impact by asking patients in all groups if they believe they received the ‘effective’ treatment). Downgrading gives an opportunity to highlight potential biases in observed effects and make recommendations for future studies to limit (or at least explore potential impact of) this source of bias.
We indexed blinding of outcome assessment separately for self‐report versus observer or interview‐rated outcome measures. As participants were not blind to their treatment condition in the included studies, self‐report outcomes measured in all of the included studies were not blinded. Nineteen studies measured outcomes using observer‐rated instruments. In 12 of these studies, interviewers who were blind to the treatment condition conducted the outcome assessments ensuring a low risk of bias. Of the remaining seven studies, two were compromised by participants who too frequently revealed their treatment condition to interviewers (Berger 2011; Berger 2014) and five used at least one interviewer who was aware of participants' random assignment (Richards 2006; Wims 2010; Spence 2011; Titov 2011; Wootton 2013).
Incomplete outcome data
Attrition bias was not a significant issue in 33 of the included studies. These 33 studies used an ITT analysis by either carrying forward the last observations, imputing missing values, or using mixed models analyses to control for outcomes lost to attrition. Moreover, rates of attrition were often quite similar between treatment conditions. Two studies did not use an ITT approach and as such may have been biased due to attrition (Andersson 2009; Andersson 2013). An additional two studies did use ITT analyses but had large attrition that may have biased the findings despite the use of ITT analyses (Kok 2012; van Ballegooijen 2013). One study did not report on their study dropout or data analytic approach and so was rated as having an unclear risk of bias (Greist 2012). We investigated the effect of these studies using sensitivity analyses.
Selective reporting
Twenty‐four of the included studies had been registered as clinical trials allowing for a more accurate analysis of selective reporting. Of these 24 studies, 16 reported on all outcomes outlined in the trial registration. For seven of the studies, one outcome outlined in the trial registration was not reported in the final manuscript (Titov 2008a; Titov 2008b; Titov 2008c; Berger 2009; Johnston 2011; Kok 2012; van Ballegooijen 2013) and they were rated as having an unclear risk of bias. One study (Titov 2010) had many outcomes indicated in the trial registration that were not reported in the final manuscript and was rated as having a high risk of bias. Those studies that were not registered reported results for each of the outcomes they measured, as described in their method; however, given the lack of trial registration or protocol publication, these studies were rated as having an unclear risk of bias.
Other potential sources of bias
Three of the included studies had a high risk of bias due to differences in baseline severity between treatment groups (Richards 2006; Titov 2011; Newby 2013). Seven studies did not report any evaluations of differences in baseline severity and so were rated as having unclear risk of bias in this domain (Tillfors 2008; Andersson 2009; Bergstrom 2010; Paxling 2011; Greist 2012; Nordgren 2012; Andersson 2013). One study reported differences in age and marital status between study groups (Robinson 2010) and another reported differences in psychotropic medication use at baseline (Kok 2012); as it was unclear if this would have an effect on study results, these studies were rated as having unclear risk of bias in this domain.
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings for the main comparison. Therapist‐supported ICBT compared to waiting list, attention, information, or online discussion group only control for anxiety disorders in adults.
| Therapist‐Supported ICBT compared to waiting list, attention, information, or online discussion group only control for anxiety disorders in adults | ||||||
| Patient or population: patients with anxiety disorders Settings: outpatient care via Internet with e‐mail or telephone support, or both Intervention: therapist‐supported ICBT Comparison: waiting list, attention, information, or online discussion group only control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Waiting list, attention, information, or online discussion group only control | Therapist‐supported ICBT | |||||
| Clinically important improvement in anxiety at post‐treatment Indexed by a standardized interview or clinically accepted measure cut‐off score1 | Study population | RR 3.75 (2.51 to 5.60) | 866 (12 studies) | ⊕⊕⊝⊝ low2 | ||
| 14 per 100 | 53 per 100 (35 to 79) | |||||
| Moderate | ||||||
| 10 per 100 | 39 per 100 (26 to 58) | |||||
| Disorder‐specific anxiety symptom severity at post‐treatment Indexed by a range of disorder‐specific self‐report measures | The mean anxiety symptom severity at post‐treatment in the intervention groups was 1.06 standard deviations lower (1.29 to 0.82 lower) | 2147 (28 studies) | ⊕⊕⊝⊝ low3,4 | A standard deviation of 0.80 or greater represents a large difference between groups5 | ||
| General anxiety symptom severity at post‐treatment Indexed by a range of measures of anxiety symptoms in general | The mean general anxiety symptom severity at post‐treatment in the intervention groups was 0.75 standard deviations lower (0.98 to 0.52 lower) | 1496 (19 studies) | ⊕⊕⊝⊝ low4,6 | A standard deviation of 0.80 or greater represents a large difference between groups5 | ||
| Quality of life at post‐treatment Indexed by self‐report measures of quality of life or functional disability | The mean quality of life at post‐treatment in the intervention groups was 0.47 standard deviations higher (0.38 to 0.57 higher) | 1639 (23 studies) | ⊕⊕⊕⊝ moderate6 | A standard deviation of 0.50 represents a moderate difference between groups5 | ||
| Adverse events at post‐treatment not reported | Study population | Not estimable | 0 (0) | See comment | Because adverse events were so rarely reported, they could not be meaningfully reported by comparison and are instead described in the review text | |
| See comment | See comment | |||||
| Moderate | ||||||
| Participant satisfaction Indexed by a mix of qualitative and quantitative self‐report measures | Study population | Not estimable | 0 (13) | See comment | Studies reported high overall treatment satisfaction for therapist‐supported ICBT | |
| See comment | See comment | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 For clinically important improvement in anxiety, an event is indicative of a participant achieving clinically important improvement. 2 Downgraded for risk of bias (‐1) primarily because four of the included studies did not blind their outcome assessors to participants' group assignment and due to lack of blinding of participants and study therapists. Downgraded for publication bias (‐1) because only 12 studies reported this outcome. Not downgraded for inconsistency (0) because heterogeneity was reduced following subgroup analysis by anxiety disorder. 3 Downgraded for risk of bias (‐1) primarily due to minor concerns with selective outcome reporting, incomplete outcome data, baseline imbalances in a few studies, and lack of blinding of participants and study therapists. 4 Downgraded for inconsistency (‐1) because the heterogeneity amongst the included studies was quite high. This may be explained by the variety of anxiety disorders investigated and differences in the treatment details; however, the number of studies that could be included in subgroup analyses was not sufficient to provide useful reasons for this heterogeneity. 5 According to Cohen's (1969) interpretation of effect sizes. 6 Downgraded for risk of bias (‐1) primarily because two studies included baseline imbalances in participant severity across study groups and due to lack of blinding of participants and study therapists.
Summary of findings 2. Therapist‐supported ICBT compared to unguided CBT for anxiety disorders in adults.
| Therapist‐supported ICBT compared to unguided CBT for anxiety disorders in adults | ||||||
| Patient or population: patients with anxiety disorders Settings: outpatient care via Internet with e‐mail or telephone support, or both Intervention: therapist‐supported ICBT Comparison: unguided ICBT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Unguided ICBT | Therapist‐supported ICBT | |||||
| Clinically important improvement in anxiety at post‐treatment Indexed by a standardized interview or clinically accepted measure cut‐off score1 | See comment | See comment | Not estimable | 54 (1 study) | ⊕⊝⊝⊝ very low2,3 | Not pooled because only one study in this comparison for this outcome |
| Disorder‐specific anxiety symptom severity at post‐treatment Indexed by a range of disorder‐specific self‐report measures | The mean disorder‐specific anxiety symptom severity at post‐treatment in the intervention groups was 0.22 standard deviations lower (0.56 lower to 0.13 higher) | 312 (5 studies) | ⊕⊝⊝⊝ very low4,5,6 | A standard deviation of 0.20 represents a small difference between groups7 | ||
| General anxiety symptom severity at post‐treatment Indexed by a range of measures of anxiety symptoms in general | The mean general anxiety symptom severity at post‐treatment in the intervention groups was 0.28 higher (2.21 lower to 2.78 higher) | 138 (2 studies) | ⊕⊝⊝⊝ very low3,4 | |||
| Quality of life at post‐treatment Indexed by self‐report measures of quality of life or functional disability | The mean quality of life at post‐treatment in the intervention groups was 0.07 standard deviations higher (0.37 lower to 0.5 higher) | 199 (3 studies) | ⊕⊝⊝⊝ very low4,5,6 | A standard deviation of 0.10 represents a small difference between groups7 | ||
| Adverse events at post‐treatment not reported | Study population | Not estimable | 0 (0) | See comment | Because adverse events were so rarely reported, they could not be meaningfully reported by comparison and are instead described in the review text | |
| See comment | See comment | |||||
| Moderate | ||||||
| Participant satisfaction Indexed by a mix of qualitative and quantitative self‐report measures | See comment | See comment | Not estimable | 0 (2 studies) | See comment | Studies generally reported higher satisfaction with therapist‐supported ICBT |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 For clinically important improvement in anxiety, an event is indicative of a participant achieving clinically important improvement. 2 Downgraded for risk of bias (‐1) primarily because of lack of blinding of outcome assessors, participants, and study therapists. 3 Downgraded for imprecision (‐2) as there is only one or two studies within the comparison for this outcome. 4 Downgraded for risk of bias (‐1) due to lack of blinding of participants and study therapists. 5 Downgraded for inconsistency (‐1) as the heterogeneity amongst the included studies was quite high. 6 Downgraded for imprecision (‐1) as there is a limited number of studies included in the comparison for this outcome. 7 According to Cohen's (1969) interpretation of effect sizes.
Summary of findings 3. Therapist‐supported ICBT compared to face‐to‐face CBT for anxiety disorders in adults.
| Therapist‐supported ICBT compared to face‐to‐face CBT for anxiety disorders in adults | ||||||
| Patient or population: adults with anxiety disorders Settings: outpatient care via Internet with e‐mail or telephone support, or both Intervention: therapist‐supported ICBT Comparison: face‐to‐face CBT | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Face‐to‐face CBT | Therapist‐supported ICBT | |||||
| Clinically important improvement in anxiety at post‐treatment Indexed by a standardized interview or clinically accepted measure cut‐off score1 | Study population | RR 1.09 (0.89 to 1.34) | 365 (4 studies) | ⊕⊕⊝⊝ low2,3 | ||
| 41 per 100 | 44 per 100 (36 to 54) | |||||
| Moderate | ||||||
| 45 per 100 | 49 per 100 (40 to 61) | |||||
| Disorder‐specific anxiety symptom severity at post‐treatment Indexed by a range of disorder‐specific self‐report measures | The mean anxiety symptom severity at post‐treatment in the intervention groups was 0.06 standard deviations higher (0.25 lower to 0.37 higher) | 450 (7 studies) | ⊕⊕⊝⊝ low4,5 | There was no significant difference between groups | ||
| General anxiety symptom severity at post‐treatment Indexed by a range of measures of anxiety symptoms in general | The mean general anxiety symptom severity at post‐treatment in the intervention groups was 0.06 standard deviations higher (0.42 lower to 0.55 higher) | 343 (6 studies) | ⊕⊕⊝⊝ low4,5 | There was no significant difference between groups | ||
| Quality of life at post‐treatment Indexed by self‐report measures of quality of life or functional disability | The mean quality of life at post‐treatment in the intervention groups was 0.26 standard deviations higher (0.06 to 0.45 higher) | 392 (5 studies) | ⊕⊕⊝⊝ low2,3 | A standard deviation of 0.20 represents a small difference between groups6 | ||
| Adverse events at post‐treatment ‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | Because adverse events were so rarely reported, they could not be meaningfully reported by comparison and are instead described in the review text |
| Participant satisfaction Indexed by a mix of qualitative and quantitative self‐report measures | Study population | Not estimable | 0 (2) | See comment | Studies reported high overall treatment satisfaction across both conditions | |
| See comment | See comment | |||||
| Moderate | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 For clinically important improvement in anxiety, an event is indicative of a participant achieving clinically important improvement at post‐treatment.
2 Downgraded for imprecision (‐1) primarily due to small sample size.
3 Downgraded for risk of bias (‐1) due to lack of blinding of participants and study therapists. 4 Downgraded for risk of bias (‐1) primarily because two included studies provided incomplete outcome data (though sensitivity analyses suggest no difference in findings when these studies are excluded) and due to lack of blinding of participants and study therapists.
5 Downgraded for inconsistency (‐1) primarily due to unexplained heterogeneity. 6 According to Cohen's (1969) interpretation of effect sizes.
Primary and secondary outcomes are reported by comparison below. Because adverse events were so rarely reported, they are not reported by comparison but are instead reported here. Only five studies included a measure that allowed for the assessment of participant deterioration over the course of treatment, for example, the CGI (Guy 1976). Andersson 2012a and Titov 2011 each identified one participant in the treatment condition who had deteriorated over the course of the study, but in neither case could their deterioration be linked to the treatment itself. Carlbring 2011 reported that no participants in their treatment condition had deteriorated. Hedman 2011 found one to two participants had deteriorated in each of the ICBT and face‐to‐face CBT conditions, but there was no difference between conditions. Ivarsson 2014 found that while eight participants in their control group showed a deterioration, only two participants in the treatment group showed a deterioration.
1. Therapist‐supported ICBT versus waiting list, attention, information, or online discussion group only control
Twenty‐eight studies compared therapist‐delivered distance CBT with a waiting list, attention, information, or online discussion group only control: Carlbring 2001; Carlbring 2006; Richards 2006; Carlbring 2007; Titov 2008a; Titov 2008b; Titov 2008c; Berger 2009; Furmark 2009a; Titov 2009; Robinson 2010; Titov 2010; Wims 2010; Carlbring 2011; Johnston 2011; Paxling 2011; Spence 2011; Titov 2011; Andersson 2012a; Andersson 2012b; Kok 2012; Nordgren 2012; Silfvernagel 2012; Newby 2013; van Ballegooijen 2013; Wootton 2013; Berger 2014; Ivarsson 2014. See Table 5 for subgroup analysis details.
2. Subgroup analyses. Comparison 1: therapist‐supported ICBT versus waiting list control.
| Outcome and Subgroup | No. of Studies |
No. of Participants ICBT Comparator |
Statistical Method | Effect Size | I2 | |||
| Clinically Important Improvement in Anxiety at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 2 | 42 | 39 | RR, M‐H, Random | 18.32 [2.50, 134.18] | 3 | ||
| ii) Social Phobia | 1 | 102 | 102 | RR, M‐H, Random | 6.00 [2.64, 13.62] | ‐‐ | ||
| iii) GAD | 3 | 91 | 94 | RR, M‐H, Random | 2.58 [1.48, 4.51] | 36 | ||
| iv) PTSD | 2 | 54 | 50 | RR, M‐H, Random | 3.48 [1.78, 6.80] | 0 | ||
| v) OCD | 1 | 15 | 14 | RR, M‐H, Random | 14.06 [0.88, 225.47] | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 3 | 129 | 134 | RR, M‐H, Random | 3.76 [1.68, 8.43] | 53 | ||
| b. By Therapist Contact | ||||||||
| i) High | 1 | 12 | 9 | RR, M‐H, Random | 6.92 [0.42, 114.19] | ‐‐ | ||
| ii) Medium | 6 | 155 | 153 | RR, M‐H, Random | 4.34 [2.43, 7.76] | 31 | ||
| iii) Low | 4 | 204 | 202 | RR, M‐H, Random | 4.13 [1.73, 9.82] | 70 | ||
| c. By Research Group | ||||||||
| i) Sweden | 5 | 210 | 215 | RR, M‐H, Random | 5.12 [2.63, 9.98] | 38 | ||
| ii) Australia‐Klein | 1 | 47 | 48 | RR, M‐H, Random | 2.10 [1.44, 3.04] | ‐‐ | ||
| iii) Australia‐Titov | 5 | 149 | 140 | RR, M‐H, Random | 3.33 [1.88, 5.91] | 44 | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 1 | 62 | 69 | RR, M‐H, Random | 2.30 [1.41, 3.74] | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| Anxiety Symptom Severity at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 6 | 165 | 158 | SMD, Random | ‐1.52 [‐2.56, ‐0.48] | 93 | ||
| ii) Social Phobia | 8 | 336 | 325 | SMD, Random | ‐1.38 [‐1.63, ‐1.13] | 48 | ||
| iii) GAD | 6 | 194 | 200 | SMD, Random | ‐0.80 [‐1.19, ‐0.42] | 69 | ||
| iv) PTSD | 2 | 54 | 50 | SMD, Random | ‐0.78 [‐1.38, ‐0.17] | 55 | ||
| v) OCD | 1 | 15 | 17 | SMD, Random | ‐0.63 [‐1.35, 0.08] | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 7 | 319 | 314 | SMD, Random | ‐0.81, [‐1.20, ‐0.41] | 81 | ||
| b. By Therapist Contact | ||||||||
| i) High | 1 | 12 | 9 | SMD, Random | ‐0.80 [‐1.70, 0.11] | ‐‐ | ||
| ii) Medium | 14 | 472 | 468 | SMD, Random | ‐1.34 [‐1.69, ‐0.99] | 82 | ||
| iii) Low | 10 | 420 | 416 | SMD, Random | ‐0.83 [‐1.15, ‐0.50] | 78 | ||
| c. By Research Group | ||||||||
| i) Sweden | 12 | 464 | 471 | SMD, Random | ‐1.50 [‐1.88, ‐1.11] | 85 | ||
| ii) Australia‐Klein | 1 | 12 | 9 | SMD, Random | ‐0.80 [‐1.70, 0.11] | ‐‐ | ||
| iii) Australia‐Titov | 12 | 365 | 350 | SMD, Random | ‐0.84 [‐1.06, ‐0.61] | 50 | ||
| iv) Netherlands‐Kok | 1 | 104 | 106 | SMD, Random | ‐0.16 [‐0.44, 0.11] | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 1 | 63 | 63 | SMD, Random | ‐0.30 [‐0.66, 0.05] | ‐‐ | ||
| vi) Switzerland | 2 | 75 | 65 | SMD, Random | ‐1.04 [‐1.63, ‐0.46] | 59 | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| General Anxiety Symptom Severity at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 4 | 126 | 122 | SMD, Random | ‐0.74 [‐1.35, ‐0.13] | 78 | ||
| ii) Social Phobia | 3 | 171 | 170 | SMD, Random | ‐0.64 [‐0.85, ‐0.42] | 0 | ||
| iii) GAD | 2 | 67 | 71 | SMD, Random | ‐1.91 [‐3.57, ‐0.26] | 94 | ||
| iv) PTSD | 2 | 54 | 50 | SMD, Random | ‐0.63 [‐1.02, ‐0.23] | 0 | ||
| v) OCD | 1 | 15 | 17 | SMD, Random | ‐1.05 [‐1.79, ‐0.30] | ‐‐ | ||
| v) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Trans‐diagnostic | 7 | 319 | 314 | SMD, Random | ‐0.49 [‐0.69, ‐0.29] | 31 | ||
| b. By Therapist Contact | ||||||||
| i) High | 1 | 12 | 9 | SMD, Random | 0.07 [‐0.79, 0.94] | ‐‐ | ||
| ii) Medium | 10 | 326 | 324 | SMD, Random | ‐0.92 [‐1.32, ‐0.52] | 83 | ||
| iii) Low | 6 | 266 | 261 | SMD, Random | ‐0.61 [‐0.82, ‐0.39] | 25 | ||
| c. By Research Group | ||||||||
| i) Sweden | 11 | 426 | 427 | SMD, Random | ‐0.94 [‐1.29, ‐0.59] | 82 | ||
| ii) Australia‐Klein | 1 | 12 | 9 | SMD, Random | 0.07 [‐0.79, 0.94] | ‐‐ | ||
| iii) Australia‐Titov | 4 | 103 | 95 | SMD, Random | ‐0.59 [‐0.88, ‐0.30] | 0 | ||
| iv) Netherlands‐Kok | 1 | 104 | 106 | SMD, Random | ‐0.21 [‐0.48, 0.07] | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 1 | 63 | 63 | SMD, Random | ‐0.39 [‐0.74, ‐0.04] | ‐‐ | ||
| vi) Switzerland | 1 | 44 | 44 | SMD, Random | ‐0.91 [‐1.23, ‐0.59] | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
Primary outcomes
1.1 Clinically important improvement in anxiety
Twelve studies assessed clinically important improvement in anxiety at post‐treatment after therapist‐supported ICBT versus a waiting list, attention, information, or online discussion group only control. A meta‐analysis with 433 treatment participants and 433 controls yielded a RR of 3.75 (95% CI 2.51 to 5.60; Analysis 1.1) in favour of the experimental intervention, with substantial heterogeneity (I2 = 50%). These results did not change significantly following sensitivity analyses according to active waiting list control conditions, high risk of bias (ROB), or assuming dropouts were treatment responders. Results continued to favour the experimental intervention (though the size of the effect varied) following subgroup analyses by anxiety disorder (social phobia: 1 trial; PD: 2 trials; GAD: 3 trials; PTSD: 2 trials; OCD: 1 trial; mixed anxiety: 3 trials), amount of therapist contact (high: 1 trial; medium: 6 studies; low: 4 studies; not reported: 1 trial), or research group (Sweden: 5 trials; Australia‐Klein et al.: 1 trial; Australia‐Titov et al.: 5 trials; Switzerland: 1 trial).
1.1. Analysis.
Comparison 1 Therapist‐supported ICBT versus waiting list control, Outcome 1 Clinically Important Improvement in Anxiety at Post‐Treatment.
1.2 Reduction in disorder‐specific anxiety symptom severity
All 30 studies that compared therapist‐supported ICBT to a waiting list, attention, information, or online discussion group only control assessed disorder‐specific anxiety symptoms at post‐treatment. Taken together, these 30 studies included 1083 treatment participants and 1064 control participants. Meta‐analytic findings showed a significant SMD of ‐1.06 (95% CI ‐1.29 to ‐0.82; Analysis 1.2; see Figure 4) in favour of the experimental condition, with considerable heterogeneity (I2 = 83%). These results did not change significantly following sensitivity analyses according to active waiting list control conditions or high ROB. One study, Titov 2010, included three separate anxiety disorder subgroups that completed disorder‐specific measures so this study was entered as three studies in this meta‐analysis: Titov 2010 GAD; Titov 2010 Panic; and Titov 2010 Social Phobia. Results continued to favour the experimental intervention following subgroup analyses by anxiety disorder (social phobia: 7 trials; PD: 5 trials; GAD: 5 trials; PTSD: 2 trials; mixed anxiety: 8 trials), amount of therapist contact (medium: 14 trials; low: 10 trials; unreported: 3 trials), or research group (Sweden: 11 trials; Australia‐Klein et al.: 1 trial; Australia‐Titov et al.: 12 trials; Switzerland: 2 trials; Netherlands‐Kok et al.: 1 trial; Netherlands‐van Ballegooijen et al.: 1 trial). Exceptions were the single trials in each of the categories of OCD (Wootton 2013), high therapist contact (Richards 2006), Australia‐Klein group (Richards 2006), Netherlands‐Kok group (Kok 2012), and Netherlands‐van Bellegooijen group (van Ballegooijen 2013) did not emerge as significantly favouring the experimental intervention.
1.2. Analysis.
Comparison 1 Therapist‐supported ICBT versus waiting list control, Outcome 2 Anxiety Symptom Severity at Post‐Treatment.
4.
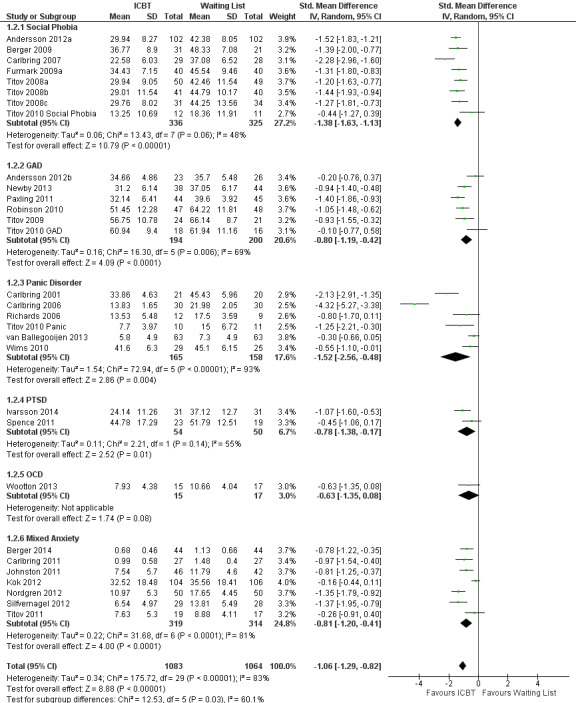
Forest plot: therapist‐supported ICBT versus waiting list control for anxiety symptom severity at post‐treatment.
1.3 Reduction in general anxiety symptom severity
Nineteen studies assessed participants' general anxiety after therapist‐supported ICBT (752 treatment participants) versus a waiting list, attention, information, or online discussion group only control (744 controls). Data analysis resulted in a SMD of ‐0.75 (95% CI ‐0.98 to ‐0.52; Analysis 1.3) showing a significantly greater decrease in general anxiety following the experimental intervention, with considerable heterogeneity (I2 = 78%). Results were consistent following sensitivity analyses according to active waiting list control conditions and high ROB. Results continued to favour the experimental intervention following subgroup analyses by anxiety disorder (social phobia: 3 trials; PD: 4 trials; GAD: 2 trials; PTSD: 2 trials; OCD: 1 trial; mixed anxiety: 7 trials), amount of therapist contact (medium: 10 trials; low: 6 trials; unreported: 2 trials), or research group (Sweden: 11 trials; Australia‐Titov et al.: 4 trials; Switzerland: 1 trial; Netherlands‐van Ballegooijen et al.: 1 trial). Again, exceptions here were that the high therapist contact trial (Richards 2006), the 1 Australia‐Klein trial (Richards 2006), and the 1 Netherlands‐Kok trial (Kok 2012) did not significantly favour the experimental intervention.
1.3. Analysis.
Comparison 1 Therapist‐supported ICBT versus waiting list control, Outcome 3 General Anxiety Symptom Severity at Post‐Treatment.
Secondary outcomes
1.4 Quality of life
Twenty‐three studies reported on participants' quality of life following therapist‐supported ICBT (826 treatment participants) versus a waiting list, attention, information, or online discussion group only control (813 controls). Analysis resulted in a SMD of 0.47 (95% CI 0.38 to 0.57; Analysis 1.4) in favour of the experimental intervention, with minimal heterogeneity (I2 = 0%) that may not be important. Results did not change significantly following sensitivity analyses according to active waiting list control conditions or high ROB.
1.4. Analysis.
Comparison 1 Therapist‐supported ICBT versus waiting list control, Outcome 4 Quality of Life at Post‐Treatment.
1.5 Participant satisfaction with the intervention
A comparison of treatment satisfaction was not warranted as authors expectedly did not report on the satisfaction of participants in the waiting list, attention, information, or online discussion group only controls. Seventeen studies reported on participants' satisfaction with treatment. Overall, participants reported a high level of satisfaction with the intervention, with roughly 90% of participants across these studies reporting being very or mostly satisfied with the treatment. Several studies reported that over 90% of participants found the quality of the online treatment modules and their correspondence with a therapist to be excellent or good. When measures of treatment satisfaction were used, participants' scores generally reflected being somewhat to very satisfied with the intervention (e.g., M = 3.34 on the Client Satisfaction Questionnaire ‐ 8, Berger 2014; M = 25.64 out of a possible 30 on a combined measure of treatment satisfaction, Newby 2013).
Only a few studies mentioned any problems or dissatisfaction with the intervention. Most notably, three studies reported that a majority of participants (70%) found the treatment moved too quickly (Carlbring 2006; Titov 2008a; Titov 2008b). Several studies reported small numbers of participants who had been dissatisfied with treatment: 3% dissatisfied with treatment (Carlbring 2006); 6% rated quality of therapist correspondence as neutral or somewhat dissatisfied, 1% rated quality of therapist contact as very dissatisfied (Titov 2008b); 11% dissatisfied with treatment (Berger 2009); 13% neutral or somewhat dissatisfied with treatment, 2% rated quality of therapist correspondence as unsatisfactory (Robinson 2010); 5% rated quality of therapist correspondence as unsatisfactory (Titov 2010); 16% neutral or somewhat dissatisfied with treatment, (Johnston 2011). Titov 2008c also reported that 7% of participants found that their confidence in their ability to manage their symptoms and their motivation to continue practicing their skills had not changed. Berger 2009 reported that one participant rated the self‐help modules as too difficult and one participant indicated that they did not understand the purpose of the self‐help modules.
2. Therapist‐supported ICBT versus unguided CBT
Five studies compared therapist‐supported ICBT with unguided CBT: Titov 2008c; Furmark 2009a; Furmark 2009b; Berger 2011; Greist 2012. See Table 6 for subgroup analysis details for this comparison.
3. Subgroup analyses. Comparison 2: therapist‐supported ICBT versus unguided CBT.
| Outcome and Subgroup | No. of Studies |
No. of Participants ICBT Comparator |
Statistical Method | Effect Size | I2 | |||
| Clinically Important Improvement in Anxiety at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Social Phobia | 1 | 27 | 27 | RR, M‐H, Random | 1.07 [0.67, 1.69] | ‐‐ | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) OCD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Medium | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Low | 1 | 27 | 27 | RR, M‐H, Random | 1.07 [0.67, 1.69] | ‐‐ | ||
| c. By Research Group | ||||||||
| i) Sweden | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 1 | 27 | 27 | RR, M‐H, Random | 1.07 [0.67, 1.69] | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| Anxiety Symptom Severity at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Social Phobia | 4 | 127 | 126 | SMD, Random | ‐0.24 [‐0.69, 0.21] | 68 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) OCD | 1 | 31 | 28 | SMD, Random | ‐0.14 [‐0.65, 0.37] | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Medium | 3 | 100 | 99 | SMD, Random | ‐0.18 [‐0.78, 0.41] | 77 | ||
| iii) Low | 1 | 27 | 27 | SMD, Random | ‐0.43 [‐0.97, 0.11] | ‐‐ | ||
| c. By Research Group | ||||||||
| i) Sweden | 2 | 69 | 69 | SMD, Random | 0.12 [‐0.22, 0.45] | 0 | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 1 | 31 | 30 | SMD, Random | ‐0.82 [‐1.34, ‐0.29] | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 1 | 27 | 27 | SMD, Random | ‐0.43 [‐0.97, 0.11] | ‐‐ | ||
| vii) USA | 1 | 31 | 28 | SMD, Random | ‐0.14 [‐0.65, 0.37] | ‐‐ | ||
| General Anxiety Symptom Severity at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Social Phobia | 2 | 69 | 69 | MD, Random | 0.28 [‐2.21, 2.78] | 0 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) OCD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Medium | 2 | 69 | 69 | MD, Random | 0.28 [‐2.21, 2.78] | 0 | ||
| iii) Low | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| c. By Research Group | ||||||||
| i) Sweden | 2 | 69 | 69 | MD, Random | 0.28 [‐2.21, 2.78] | 0 | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| Clinically Important Improvement in Anxiety at Follow‐up | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Social Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Medium | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Low | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| c. By Research Group | ||||||||
| i) Sweden | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| Anxiety Symptom Severity at Follow‐up | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Social Phobia | 3 | 96 | 96 | SMD, Random | ‐0.30 [‐0.58, ‐0.01] | 0 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) OCD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact at Follow‐up | ||||||||
| i) High | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Medium | 2 | 69 | 69 | SMD, Random | ‐0.31 [‐0.65, 0.03] | 3 | ||
| iii) Low | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| c. By Research Group | ||||||||
| i) Sweden | 2 | 69 | 69 | SMD, Random | ‐0.31 [‐0.65, 0.03] | 3 | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 1 | 27 | 27 | SMD, Random | ‐0.26 [‐0.80, 0.27] | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| General Anxiety Symptom Severity at Follow‐up | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Social Phobia | 2 | 69 | 69 | MD, Random | 0.72 [‐2.12, 3.57] | 0 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) OCD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Medium | 2 | 69 | 69 | MD, Random | 0.72 [‐2.12, 3.57] | 0 | ||
| iii) Low | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| c. By Research Group | ||||||||
| i) Sweden | 2 | 69 | 69 | MD, Random | 0.72 [‐2.12, 3.57] | 0 | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
Primary outcomes
2.1 Clinically important improvement in anxiety
Only Berger 2011 assessed clinically important improvement in anxiety after therapist‐supported ICBT versus unguided CBT. They reported that 16/27 participants receiving therapist‐supported ICBT and 15/27 participants completing unguided CBT no longer met the diagnostic criteria post‐treatment (Analysis 2.1).
2.1. Analysis.
Comparison 2 Therapist‐supported ICBT versus unguided CBT, Outcome 1 Clinically Important Improvement in Anxiety at Post‐Treatment.
2.2 Reduction in disorder‐specific anxiety symptom severity
The five studies that compared therapist‐supported ICBT to unguided CBT (that is, self‐help) assessed disorder‐specific anxiety symptoms at post‐treatment. Combined, these studies included 158 treatment and 154 control participants and resulted in a non‐significant SMD of ‐0.22 (95% CI ‐0.56 to 0.13; Analysis 2.2), with substantial heterogeneity (I2 = 58%). At 6 to 12 month follow‐up, 3 studies reported on this outcome; a meta‐analysis of 96 treatment and 96 comparator participants resulted in a significant SMD of ‐0.30 (95% CI ‐0.58 to ‐0.01; Analysis 2.3) in favour of the experimental intervention with minimal but difficult to estimate heterogeneity (I2 = 0%). No sensitivity analyses were required.
2.2. Analysis.
Comparison 2 Therapist‐supported ICBT versus unguided CBT, Outcome 2 Anxiety Symptom Severity at Post‐Treatment.
2.3. Analysis.
Comparison 2 Therapist‐supported ICBT versus unguided CBT, Outcome 3 Anxiety Symptom Severity at Follow‐up.
Results for this outcome at post‐treatment remained non‐significant following subgroup analyses by anxiety disorder (social phobia: 4 trials; OCD: 1 trial), therapist contact (medium: 3 trials; not reported: 2 trials), and research group (Australia‐Titov et al.: 1 trial; Switzerland: 1 trial; Sweden: 2 trials: USA: 1 trial). Subgroup analyses based on anxiety disorder were not warranted at follow‐up as all studies investigated social phobia.
Results for this outcome at follow‐up following subgroup analyses by therapist contact (medium: Furmark 2009a; Furmark 2009b; not reported: Berger 2011) resulted in a non‐significant difference with minimal but difficult to estimate heterogeneity (SMD ‐0.31, 95% CI ‐0.65 to 0.03; I2 = 3%). The same was true for results for this outcome at follow‐up following subgroup analyses by research group (Switzerland: Berger 2011; Sweden: Furmark 2009a; Furmark 2009b; SMD ‐0.31, 95% CI ‐0.65 to 0.03; I2 = 3%).
2.3 Reduction in general anxiety symptom severity
Only two studies assessed participants' general anxiety after therapist‐supported ICBT (69 treatment participants) versus self‐help interventions (69 comparator participants). Data analysis resulted in a non‐significant mean difference of 0.28 (95% CI ‐2.21 to 2.78; Analysis 2.4), with minimal but difficult to estimate heterogeneity (I2 = 0%). A similar result was found at 12 month follow‐up with the same studies; the mean difference was 0.72 (95% CI ‐2.12 to 3.57; Analysis 2.5), with minimal but difficult to estimate heterogeneity (I2 = 0%). No sensitivity analyses were required. Subgroup analyses all relevant characteristics of the included studies were the same.
2.4. Analysis.
Comparison 2 Therapist‐supported ICBT versus unguided CBT, Outcome 4 General Anxiety Symptom Severity at Post‐Treatment.
2.5. Analysis.
Comparison 2 Therapist‐supported ICBT versus unguided CBT, Outcome 5 General Anxiety Symptom Severity at Follow‐up.
Secondary outcomes
2.4 Quality of life
Three studies indexed quality of life of participants following therapist‐supported ICBT (100 treatment participants) versus unguided CBT (99 control participants). Data analysis resulted in a non‐significant SMD of 0.07 (95% CI ‐0.37 to 0.50; Analysis 2.6), with moderate to substantial heterogeneity (I2 = 58%). At six to 12 month follow‐up, only two of these studies indexed quality of life of participants following treatment (69 treatment and 69 comparator participants), with meta‐analysis showing a similar non‐significant SMD of ‐0.19 (95% CI ‐0.53 to 0.14; Analysis 2.7), with minimal but difficult to estimate heterogeneity (I2 = 0%). No sensitivity analyses were required.
2.6. Analysis.
Comparison 2 Therapist‐supported ICBT versus unguided CBT, Outcome 6 Quality of Life at Post‐Treatment.
2.7. Analysis.
Comparison 2 Therapist‐supported ICBT versus unguided CBT, Outcome 7 Quality of Life at Follow‐up.
2.5 Participant satisfaction with the intervention
Two studies indexed participant satisfaction with the intervention. Berger 2011 found that treatment satisfaction was significantly higher in the therapist‐supported ICBT condition as compared to the self‐help condition according to the Client Satisfacton Questionnaire (Attkisson 1982). Similarly, Titov 2008c found that a significantly greater number of participants in the therapist‐supported ICBT condition as compared to the self‐help condition were very or mostly satisfied with their treatment (no participants reported being dissatisfied with treatment). However, Titov 2008c reported no differences between conditions in perceptions of how logical the treatment was, participants' confidence in recommending the treatment to a friend, and the extent to which treatment had increased participants' confidence in managing their symptoms. Seven per cent of participants in the ICBT condition reported that the treatment had not changed their confidence in managing their symptoms or their motivation to keep practicing techniques they had learned.
3. Therapist‐supported ICBT versus face‐to‐face CBT
Seven studies compared therapist‐supported ICBT with face‐to‐face CBT: Carlbring 2005; Kiropoulos 2008; Tillfors 2008; Andersson 2009; Bergstrom 2010; Hedman 2011; Andersson 2013. See Table 7 for subgroup analysis details for this comparison.
4. Subgroup analyses. Comparison 3: therapist‐supported ICBT versus face‐to‐face CBT.
| Outcome and Subgroup | No. of Studies |
No. of Participants ICBT Comparator |
Statistical Method | Effect Size | I2 | |||
| Clinically Important Improvement in Anxiety at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 3 | 121 | 118 | RR, M‐H, Random | 1.06 [0.85, 1.32] | 0 | ||
| ii) Social Phobia | 1 | 64 | 62 | RR, M‐H, Random | 1.45 [0.77, 2.76] | ‐‐ | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) OCD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 1 | 46 | 40 | RR, M‐H, Random | 1.11 [0.57, 2.15] | ‐‐ | ||
| ii) Medium | 1 | 25 | 24 | RR, M‐H, Random | 1.20 [0.85, 1.69] | ‐‐ | ||
| iii) Low | 2 | 114 | 116 | RR, M‐H, Random | 1.08 [0.72, 1.60] | 34 | ||
| c. By Research Group | ||||||||
| i) Sweden | 3 | 139 | 140 | RR, M‐H, Random | 1.09 [0.88, 1.36] | 0 | ||
| ii) Australia‐Klein | 1 | 46 | 40 | RR, M‐H, Random | 1.11 [0.57, 2.15] | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| Anxiety Symptom Severity at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 3 | 119 | 115 | SMD, Random | 0.29 [0.03, 0.54] | 0 | ||
| ii) Social Phobia | 2 | 83 | 80 | SMD, Random | ‐0.18 [‐0.92, 0.57] | 76 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Specific Phobia | 2 | 26 | 27 | SMD, Random | ‐0.02 [‐0.56, 0.52] | ‐‐ | ||
| vi) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 2 | 63 | 55 | SMD, Random | 0.42 [0.05, 0.78] | 0 | ||
| ii) Medium | 1 | 25 | 24 | SMD, Random | 0.05 [‐0.51, 0.61] | ‐‐ | ||
| iii) Low | 4 | 140 | 143 | SMD, Random | ‐0.10 [‐0.53, 0.33] | 64 | ||
| c. By Research Group | ||||||||
| i) Sweden | 6 | 184 | 185 | SMD, Random | ‐0.03 [‐0.34, 0.28] | 49 | ||
| ii) Australia‐Klein | 1 | 44 | 37 | SMD, Random | 0.49 [0.05, 0.93] | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| General Anxiety Symptom Severity at Post‐Treatment | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 2 | 67 | 62 | SMD, Random | 0.42 [‐0.75, 1.60] | 90 | ||
| ii) Social Phobia | 2 | 83 | 80 | SMD, Random | ‐0.18 [‐0.49, 0.13] | 0 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Specific Phobia | 2 | 26 | 25 | SMD, Random | ‐0.14 [‐1.07, 0.79] | 64 | ||
| vi) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 2 | 61 | 56 | SMD, Random | 0.49 [‐0.57, 1.56] | 86 | ||
| ii) Medium | 1 | 25 | 24 | SMD, Random | ‐0.19 [‐0.75, 0.38] | ‐‐ | ||
| iii) Low | 3 | 90 | 87 | SMD, Random | ‐0.18 [‐0.59, 0.22] | 29 | ||
| c. By Research Group | ||||||||
| i) Sweden | 5 | 134 | 129 | SMD, Random | ‐0.17 [‐0.42, 0.07] | 0 | ||
| ii) Australia‐Klein | 1 | 42 | 38 | SMD, Random | 1.01 [0.54, 1.48] | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| Clinically Important Improvement in Anxiety at Follow‐up | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 2 | 75 | 78 | RR, M‐H, Random | 1.09 [0.93, 1.28] | 0 | ||
| ii) Social Phobia | 1 | 64 | 62 | RR, M‐H, Random | 1.15 [0.73, 1.83] | ‐‐ | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Specific Phobia | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| ii) Medium | 1 | 25 | 24 | RR, M‐H, Random | 1.05 [0.87, 1.27] | ‐‐ | ||
| iii) Low | 2 | 114 | 116 | RR, M‐H, Random | 1.17 [0.92, 1.50] | 0 | ||
| c. By Research Group | ||||||||
| i) Sweden | 3 | 139 | 140 | RR, M‐H, Random | 1.10 [0.94, 1.27] | 0 | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| Anxiety Symptom Severity at Follow‐up | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 2 | 75 | 78 | SMD, Random | ‐0.04 [‐0.36, 0.28] | 0 | ||
| ii) Social Phobia | 2 | 83 | 80 | SMD, Random | ‐0.39 [‐0.71, ‐0.08] | 0 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Specific Phobia | 2 | 26 | 25 | SMD, Random | ‐0.09 [‐0.64, 0.46] | 0 | ||
| vi) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 1 | 19 | 18 | SMD, Random | ‐0.11 [‐0.76, 0.53] | ‐‐ | ||
| ii) Medium | 1 | 25 | 24 | SMD, Random | ‐0.04 [‐0.60, 0.52] | ‐‐ | ||
| iii) Low | 4 | 140 | 141 | SMD, Random | ‐0.24 [‐0.48, 0.00] | 3 | ||
| c. By Research Group | ||||||||
| i) Sweden | 6 | 184 | 183 | SMD, Random | ‐0.20 [‐0.41, 0.00] | 0 | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| General Anxiety Symptom Severity at Follow‐up | ||||||||
| a. By Disorder | ||||||||
| i) Panic | 1 | 25 | 24 | SMD, Random | ‐0.17 [‐0.74, 0.39] | ‐‐ | ||
| ii) Social Phobia | 2 | 83 | 80 | SMD, Random | ‐0.14 [‐0.45, 0.17] | 0 | ||
| iii) GAD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) PTSD | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Specific Phobia | 2 | 26 | 25 | SMD, Random | ‐0.06 [‐0.61, 0.49] | 0 | ||
| vi) Trans‐diagnostic | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| b. By Therapist Contact | ||||||||
| i) High | 1 | 19 | 18 | SMD, Random | ‐0.19 [‐0.83, 0.46] | ‐‐ | ||
| ii) Medium | 1 | 25 | 24 | SMD, Random | ‐0.17 [‐0.74, 0.39] | ‐‐ | ||
| iii) Low | 3 | 90 | 87 | SMD, Random | ‐0.10 [‐0.40, 0.19] | 0 | ||
| c. By Research Group | ||||||||
| i) Sweden | 5 | 134 | 129 | SMD, Random | ‐0.13 [‐0.37, 0.11] | 0 | ||
| ii) Australia‐Klein | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iii) Australia‐Titov | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| iv) Netherlands‐Kok | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| v) Netherlands‐van Ballegooijen | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vi) Switzerland | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
| vii) USA | 0 | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ‐‐ | ||
Primary outcomes
3.1 Clinically important improvement in anxiety
Four studies assessed clinically important improvement in anxiety at post‐treatment after therapist‐supported ICBT (185 treatment participants) versus face‐to‐face CBT (180 comparator participants). Meta‐analysis yielded a non‐significant RR of 1.09 (95% CI 0.89 to 1.34; Analysis 3.1), with minimal heterogeneity that may not be important (I2 = 0%). At 6 to 12 month follow‐up, the results of 3 studies that reported on clinically important improvement in anxiety, with 139 treatment and 140 comparator participants, resulted in a non‐significant RR of 1.10 (95% CI 0.94 to 1.27; Analysis 3.2), again with minimal heterogeneity (I2 = 0%). Results did not change significantly following a sensitivity analysis assuming dropouts were treatment responders. Results for this outcome remained non‐significant following subgroup analyses by anxiety disorder (social phobia: 1 trial; PD: 3 trials) , therapist contact (high: 1 trials; medium: 1 trial; low: 2 trials), and research group (Sweden: 3 trials: Australia‐Klein et al.: 1 trial).
3.1. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 1 Clinically Important Improvement in Anxiety at Post‐Treatment.
3.2. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 2 Clinically Important Improvement in Anxiety at Follow‐up.
3.2 Reduction in disorder‐specific anxiety symptom severity
The seven studies that compared therapist‐supported ICBT to face‐to‐face CBT assessed changes in symptom specific anxiety. Using these seven studies, including 228 treatment participants and 222 control participants, meta‐analysis resulted in a non‐significant SMD of 0.06 (95% CI ‐0.25 to 0.37; Analysis 3.3; see Figure 5), with substantial heterogeneity (I2 = 60%). At 6 to 12 month follow‐up, data from six studies, including 184 treatment participants and 183 comparator participants, could be used to assess changes in symptom specific anxiety. Meta‐analysis resulted in a non‐significant SMD of ‐0.20 (95% CI ‐0.41 to 0.0; Analysis 3.4) with minimal heterogeneity that may not be important (I2 = 0%). Results remained non‐significant following a sensitivity analysis excluding two studies that did not use ITT analysis and had high ROB (Andersson 2009; Andersson 2013).
3.3. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 3 Anxiety Symptom Severity at Post‐Treatment.
5.
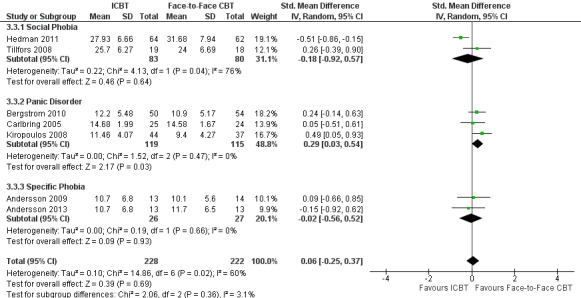
Forest plot: therapist‐supported ICBT versus face‐to‐face CBT for anxiety symptom severity at post‐treatment.
3.4. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 4 Anxiety Symptom Severity at Follow‐Up.
Results for this outcome at post‐treatment were somewhat variable following subgroup analyses by anxiety disorder (social phobia: 2 trials; PD: 3 trials; specific phobia: 2 trials). A meta‐analysis of the studies investigating PD (Carlbring 2005; Kiropoulos 2008; Bergstrom 2010) found a significant SMD of 0.29 (95% CI 0.03 to 0.54) with minimal but difficult to estimate heterogeneity (I2 = 0%) in favour of face‐to‐face CBT. In contrast, a meta‐analyses of two studies investigating social phobia (Tillfors 2008; Hedman 2011; SMD ‐0.18, 95% CI ‐0.92 to 0.5; I2 = 76%) and two studies investigating specific phobia (Andersson 2009; Andersson 2013; SMD ‐0.02, 95% CI ‐0.56 to 0.52; I2 = 0%) remained non‐significant (in line with the overall meta‐analysis).
Unexpectedly, at 6 to 12 month follow‐up it was only the meta‐analysis of social phobia studies (Tillfors 2008; Hedman 2011) that showed a significant difference between groups, with an SMD of ‐0.39 (95% CI ‐0.71 to ‐0.08) with minimal but difficult to estimate heterogeneity (I2 = 0%) in favour of the experimental intervention, while the meta‐analysis of PD studies (Carlbring 2005; Bergstrom 2010) was non‐significant (SMD ‐0.04, 95% CI ‐0.36 to 0.28; I2 = 0%), as was the meta‐analysis of specific phobia studies (Andersson 2009; Andersson 2013; SMD ‐0.09, 95% CI ‐0.64 to 0.46; I2 = 0%).
Results for this outcome at post‐treatment were also somewhat variable following subgroup analyses by therapist contact (high: 2 trials; medium: 1 trial; low: 4 trials). A subgroup analysis of studies with high therapist contact (Kiropoulos 2008; Tillfors 2008) resulted in a significant SMD of 0.42 (95% CI 0.05 to 0.78), with minimal but difficult to estimate heterogeneity (I2 = 0%), in favour of face‐to‐face CBT at post‐treatment. The meta‐analysis of studies with low therapist contact remained non‐significant (SMD ‐0.10, 95% CI ‐0.53 to 0.33) with substantial heterogeneity (I2 = 64%) (Andersson 2009; Bergstrom 2010; Hedman 2011; Andersson 2013). At follow‐up, results for this outcome remained non‐significant following subgroup analyses by therapist contact.
Results for this outcome at post‐treatment and follow‐up remained non‐significant following subgroup analysis of the 6 trials by the Sweden research group (SMD=‐0.03, 95% CI ‐0.34 to 0.28, I2 = 49%), however at post‐treatment the one Australia‐Klein trial (Kiropoulos 2008) resulted in a significant difference in favour of face‐to‐face CBT.
3.3 Reduction in general anxiety symptom severity
Six studies reported participants' levels of general anxiety post‐treatment. The six studies combined in the meta‐analysis included 176 treatment participants and 167 comparator participants and resulted in a non‐significant SMD of 0.06 (95% CI ‐0.42 to 0.55; Analysis 3.5), with substantial to considerable heterogeneity (I2 = 78%). When the Kiropoulos 2008 study was removed from the analysis (because it presented transformed data, which we back‐transformed to include in the analysis), the resulting SMD remained non‐significant at ‐0.17 (95% CI ‐0.42 to 0.07) and heterogeneity was reduced (I2 = 0%). At 6 to 12 month follow‐up, five studies reported participants' level of general anxiety. The five studies included 134 treatment participants and 129 comparator participants and yielded a non‐significant SMD of ‐0.13 (95% CI ‐0.37 to 0.11; Analysis 3.6) with minimal heterogeneity that may not be important (I2 = 0%). Results remained non‐significant following a sensitivity analysis excluding two studies that did not use ITT analyses and had high ROB (Andersson 2009; Andersson 2013). Results for this outcome remained non‐significant following subgroup analyses at post‐treatment and follow‐up by anxiety disorder (social phobia: 2 trials; PD: 2 trials; specific phobia: 2 trials), therapist contact (high: 2 trials; medium: 1 trial; low: 3 trials), and research group (Sweden: 5 trials). The single Australia‐Klein trial (Kiropoulos 2008) did find a significant difference in favour of the face‐to‐face CBT condition at post‐treatment.
3.5. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 5 General Anxiety Symptom Severity at Post‐Treatment.
3.6. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 6 General Anxiety Symptom Severity at Follow‐up.
Secondary outcomes
3.4 Quality of life
Five studies reported on participants' quality of life following therapist‐supported ICBT (198 treatment participants) versus face‐to‐face CBT (194 comparator participants). Analysis resulted in a SMD of 0.26 (95% CI 0.06 to 0.45; Analysis 3.7) in favour of the experimental intervention, with minimal heterogeneity that may not be important (I2 = 0%). This trend continued at 6 to 12 month follow‐up. Four studies comprising 158 treatment and 158 comparator participants resulted in a SMD of 0.33 (95% CI 0.11 to 0.55; Analysis 3.8) in favour of the experimental intervention, again with minimal heterogeneity (I2 = 0%). No sensitivity analyses were required.
3.7. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 7 Quality of Life at Post‐Treatment.
3.8. Analysis.
Comparison 3 Therapist‐supported ICBT versus face‐to‐face CBT, Outcome 8 Quality of Life at Follow‐up.
3.5 Participant satisfaction with the intervention
Two studies indexed participant satisfaction with the intervention. Overall, treatment satisfaction was high across both therapist‐supported ICBT and face‐to‐face CBT. In one study (Tillfors 2008), only one participant in the ICBT condition and two participants in the face‐to‐face condition reported being "neutral/somewhat dissatisfied with treatment" and no participants reported being "very dissatisfied" with treatment. Both studies found no significant difference between conditions in participants' overall satisfaction with the intervention or their perceptions of improvement as a result of treatment.
A notable significant difference between treatment conditions appeared in one instance: Kiropoulos 2008 found that participants receiving therapist‐supported ICBT reported significantly less enjoyment in communicating with their therapist as compared to participants receiving face‐to‐face CBT.
Sensitivity analysis
Sensitivity analyses are detailed in the results section above. Given the available studies for this review, some of the planned sensitivity analyses were not warranted. First, sensitivity analyses based on the blinding of participants or personnel, or both, in the included studies were not conducted because blinding of participants and personnel is not standard practice with this type of clinical trial. Second, as none of the included studies were cluster randomised trials and none of the included studies with multiple intervention arms had selective reporting of intervention comparisons, sensitivity analyses based on these characteristics were not conducted. Third, as we were not required to impute any standard deviations, we also eliminated that planned sensitivity analysis. Only one study included transformed data (Kiropoulos 2008) and it was discussed in section 3.3 above, and only two studies did not use ITT data (Andersson 2009; Andersson 2013) and are discussed in sections 3.2 and 3.3 above. Finally, as LOCF was the primary method of ITT analysis reported by authors, we did not exclude studies using LOCF.
Discussion
Summary of main results
Please refer to the Table 1, Table 2, and Table 3 for a summary of the main results.
The present review investigated the efficacy of therapist‐supported ICBT in treating anxiety disorders in adults. We identified 38 studies to be included in the review, comparing the intervention of interest to a waiting list, attention, information, or online discussion group only control, unguided CBT, and face‐to‐face group or individual CBT.
The present findings suggest that therapist‐supported ICBT is more efficacious than a waiting list, attention, information, or online discussion group only control in leading to clinically important improvement in anxiety, reducing anxiety symptoms (both disorder‐specific and general), and improving quality of life. Results also generally showed no difference in outcomes following therapist‐supported ICBT versus unguided CBT at post‐treatment, though results are limited by very low quality evidence due to a limited number of studies (that is, imprecision). Moreover, results suggest that therapist‐supported ICBT may not be significantly different from face‐to‐face group and individual CBT in treating anxiety disorders. Meta‐analyses revealed no significant differences in clinically important improvement in anxiety or reduction in anxiety symptoms (both disorder‐specific and general) at post‐treatment or follow‐up for these two interventions.
At 6 to 12 month follow‐up, results generally mirror the post‐treatment findings but are limited by the small number of studies and the degree of variability in the interventions under investigation across studies. Thus, these findings should be interpreted with caution.
All findings largely remained robust following sensitivity analyses conducted to explore the impact of potential sources of bias or heterogeneity. Subgroup analyses suggest that there may be some differences in outcome based on the type of anxiety disorder being treated or the amount of therapist contact in the intervention; however, the small number of studies within each subgroup limits our ability to draw firm conclusions based on these analyses. More research is needed in these areas.
Overall completeness and applicability of evidence
Taken together, the studies included in the present review help us answer the question, is therapist‐supported ICBT an efficacious treatment for anxiety disorders in adults? In particular, the included studies are of sufficient number to comprehensively compare the efficacy of therapist‐supported ICBT to a waiting list, attention, information, or online discussion group only control. There are fewer, but still sufficient, studies to compare the efficacy of therapist‐supported ICBT to traditional face‐to‐face CBT. In comparison, the number of studies comparing therapist‐supported ICBT to unguided CBT (that is, self‐help) is limited and therefore findings with respect to this comparison must be interpreted with some caution.
In terms of the applicability of the evidence to ICBT interventions and particular patient populations, several factors warrant consideration when interpreting the present findings. First, the included interventions are quite heterogeneous. While all studies investigated therapist‐supported ICBT, the nuances of each intervention (for example, length, number of online modules, nature of therapist support) varied widely. It seems prudent to note that while these interventions seem efficacious as a whole, the optimal characteristics of these interventions have yet to be identified and their heterogeneity reduces the quality of the body of evidence investigated here.
Second, the included studies investigated a number of different anxiety disorders with a particular focus on PD, social phobia, and GAD, either separately or as part of a transdiagnostic treatment package. As such, we can be most confident that the present findings apply to the treatment of these disorders. More research is needed into ICBT for other anxiety disorders, such as OCD, PTSD, and specific phobia.
Third, researchers have previously raised some concerns about the participants included in investigations of ICBT, as many of these studies recruit participants from the community via media advertisements (for example, Cuijpers 2009). There is some question as to whether these participants are similar enough to participants recruited for face‐to‐face CBT RCTs, who tend to be recruited via clinic referrals. Despite this concern, research by Titov and colleagues (Titov 2010b) found that ICBT participants are as severe in terms of symptom severity, distress, and disability as individuals attending a face‐to‐face clinic and more severe than individuals identified via an epidemiological survey. We also attempted to account for this possible difference in participant characteristics by including only individuals with an anxiety disorder diagnosed using a standardized instrument.
Despite the heterogeneity of the interventions and populations across studies, the robustness of findings following sensitivity analyses lends credence to the efficacy of therapist‐supported ICBT as an alternative method of delivering CBT to those with anxiety disorders who are in need of intervention.
Quality of the evidence
We considered the quality of the evidence of the included studies using the GRADE tool (Higgins 2011b). Most of the evidence contributing to the comparisons in this review was rated as low quality; however, simply dismissing findings based on this determination is hasty. A careful look at reasons for the downgrading of quality of evidence is warranted to best interpret the findings.
With respect to risk of bias, the included evidence is of moderate quality as there were only a few concerns with the internal validity of the included studies. There were some difficulties with (a) blinding of outcome assessors, and (b) incomplete outcome data in several of the included studies. Sensitivity analyses excluding these studies suggest that any potential bias introduced by these studies did not affect the meta‐analytic outcomes. Risk of bias ratings were inflated across comparisons in this review due to the nature of clinical psychotherapy trials, which precludes keeping the treatment condition concealed from the participant or the therapist delivering the treatment. It is important to note that there is no way to blind participants or study therapists, suggesting that reaching a higher quality study design would be difficult. Neverthless, downgrading evidence based on this characteristic of risk of bias gives an opportunity to make recommendations for future studies to limit (or at least explore potential impact of) this source of bias, perhaps by recruiting clients or therapists who do not favour interventions, by ensuring intervention providers in both groups believe they are delivering the ‘best’ treatment, and by measuring the potential impact by asking patients in all groups if they believe they received the ‘effective’ treatment. In addition to these risk of bias domains, it should be noted that there may also be some concerns with selective outcome reporting, but these remain unclear. Selective outcome reporting has been found to be an important concern in non‐pharmaceutical trials (Milette 2011), such as those included here. Approximately one third of the studies included in this review were not prospectively registered on a trial database. As such, it is impossible to discern if these studies are biased by selective reporting. It may be that with the advent of trial registration becoming more common (and expected), updates to this review will be able to provide a more clear estimate of the risk of selective outcome reporting.
There is a large degree of heterogeneity in a number of the meta‐analyses in this review, reducing the quality of some of the evidence. Subgroup and sensitivity analyses provide some indication of what may account for the heterogeneity, but there is by no means a clear answer. Some degree of heterogeneity may have emerged because we included studies of a range of anxiety disorders, including PD, social phobia, GAD, specific phobia, OCD, and PTSD, in the meta‐analyses. It seems possible there are nuances unique to each of these disorders and their treatment that might facilitate or hamper the efficacy of their treatment via therapist‐supported ICBT. Some subgroup analyses by anxiety disorder resulted in an important decrease in heterogeneity, however, in other cases heterogeneity did not decrease at all. This may have been in part because even within studies of the same disorder, researchers employed different outcome measures to assess treatment outcomes. The variability in outcome measures within and across studies may account for some important heterogeneity. Support for this hypothesis may be found in the fact that the quality of life outcome tends to show the least heterogeneity across comparisons as well as the least variability in assessment measures used. Also of importance, the nature of the ICBT interventions included in this review is quite diverse in terms of length, number of online modules, and nature of therapist contact. It may be that the nuances of these treatments led to nuanced differences in treatment outcome. However, subgroup analyses based on amount of therapist contact, for example, did not sufficiently and consistently reduce heterogeneity. Similarly, subgroup analyses by research group did not consistently lead to decreases in heterogeneity. This is surprising given the assumption that studies conducted within the same research laboratory would have some degree of consistency in methods, outcome measures, participants, etc. Nevertheless, these studies did vary over the years in terms of the anxiety disorder investigated and amount and nature of therapist contact with participants.
All subgroup analyses are complicated by the fact that only a small number of trials tended to be included in each analysis, making it difficult to estimate heterogeneity. Thus, heterogeneity does remain somewhat of a concern in the present review. While this was unexpected, it may be that there is simply too much variability in study methods, populations, outcome measures, etc. across studies and not enough studies to support meaningful subgroup analyses at this time. Importantly, our speculation is that this heterogeneity might be explained by the expected factors discussed here as opposed to any bias in the included studies. An increase in the number of studies in this area in the future may allow us to explore heterogeneity more robustly and meaningfully. In the future, we will also explore further subgroup analyses on other factors that may contribute to varying treatment outcomes, including length of the intervention in question. We are limited somewhat in the subgroup analyses we can conduct given that some potentially relevant factors (e.g., history of disorder) are variable within studies and thus not conducive to a study‐by‐study comparison.
In considering the quality of the evidence, we also examined indirectness of the included studies (that is, the degree to which the included studies address the review objective) and the imprecision of each study's findings. Across included studies, we had no concerns with indirectness. As far as imprecision, some of the included studies are limited by small sample size. The meta‐analyses attempt to address such small samples by combining studies, where appropriate. Precision of findings may also be affected by rates of dropout across interventions, particularly if there is the chance that one of the two interventions being compared is likely to lead to greater dropout. Given some of the characteristics of ICBT (for example, engaging from a distance, no requirement to commit to appointment times or be accountable), one might expect there to be greater dropout rates with this type of treatment. However, the present findings suggest this may not be the case. There were generally quite similar rates of dropout across the interventions investigated (experimental and comparator). Almost all studies used a rigorous and somewhat conservative method to account for missing data. Sensitivity analyses on dichotomous outcomes, assuming dropouts were treatment responders, did not significantly change the meta‐analytic outcomes. These details suggest that the precision of findings are not significantly threatened by treatment dropout rates.
Finally, we considered whether publication bias might have affected the evidence. The number of studies within each comparison in the present review only permitted the analysis of funnel plots for several outcomes for the comparison of the intervention and a waiting list control (Figure 6; Figure 7; Figure 8; Figure 9). A visual inspection of these funnel plots suggested that there may have been a small study effect (that is, the potential for some publication bias). Because there were less than 10 studies in the other meta‐analyses in this review (in accordance with the guidelines for the use of funnel plots in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a)), we did not analyze publication bias using funnel plots for the remaining comparisons. To complement the use of funnel plots, we looked to match trials recorded in clinical trial registries with published manuscripts. Accounting for the fact that many of the most recent registered trials are still ongoing or may be in the process of being published, we only observed a handful of registries that could not be matched with a published trial. This would suggest that, at least recently (since trial registration has been strongly encouraged), publication bias may not be a significant concern for this review. However, our findings with respect to the consistency between trial registries and published studies do not rule out earlier publication bias or the possibility of bias due to smaller‐scale, unfunded studies that may not have been registered. In a further effort to assess for publication bias, we contacted authors in the field to inquire about any unpublished findings and were only informed of two studies that were unfinished and unpublished, one due to difficulties with funding, the other due to difficulties with recruitment. With these factors in mind, we cannot make a conclusive statement about publication bias. Publication bias may not limit the quality of the included evidence but readers should keep the possibility of this bias in mind when interpreting the review findings.
6.
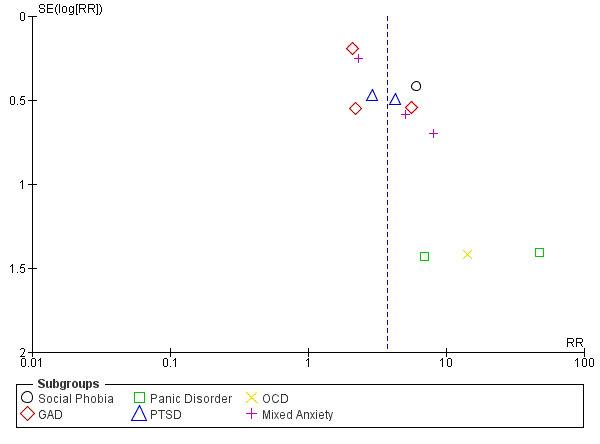
Funnel plot of the outcome clinically important improvement in anxiety at post‐treatment for therapist‐supported ICBT versus waiting list control.
7.
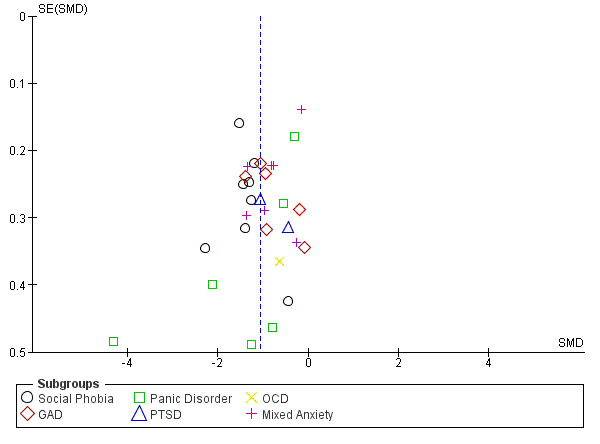
Funnel plot the outcome anxiety symptom severity at post‐treatment for therapist‐supported ICBT versus waiting list control.
8.
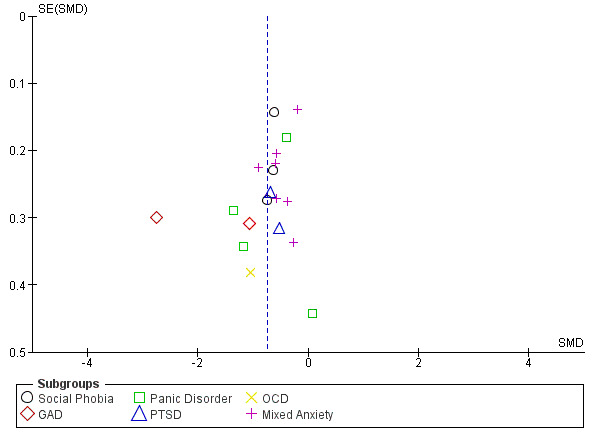
Funnel plot of the outcome general anxiety symptom severity at post‐treatment for therapist‐supported ICBT versus waiting list control.
9.
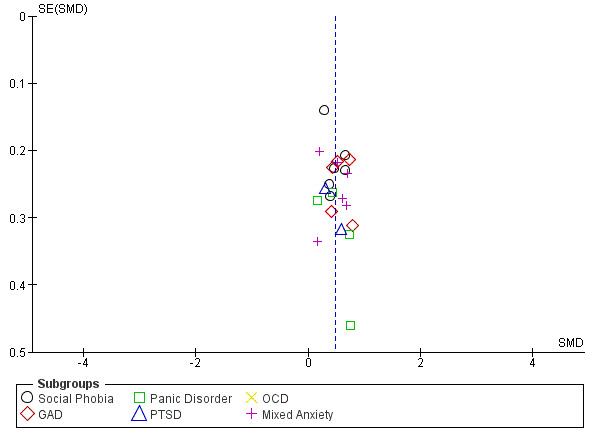
Funnel plot of the outcome quality of life at post‐treatment for therapist‐supported ICBT versus waiting list control.
Overall, the included evidence, across studies and comparisons, is of low quality. In many cases reductions in quality tend to be due to heterogeneity, which may be explained by meta‐analytic methods rather than the evidence itself.
Potential biases in the review process
Given the variability within ICBT interventions, it is possible that there are several biases inherent in the present review. First, we elected to include only those interventions that did not include face‐to‐face therapist contact during active treatment. This may have excluded studies that were simply conducted within therapists' offices for practical purposes but could in fact have been followed online by a client at home as well. In this way, the included studies may not comprehensively include all possible ICBT treatments. Second, we included only interventions with active therapist involvement. This decision was made because (a) there seems to be an important distinction between guided and unguided treatment, and (b) some prior research has suggested that therapist involvement may be an important part of distance treatment (Spek 2007; Andersson 2009b). Nevertheless, this decision impacted the types of trials included in the present review and led to the exclusion of some Internet‐based studies that did not directly involve therapists but included interactive voice response software (Greist 2002). While preliminary work has been done, further research will need to investigate the importance of active versus automated versus no therapist involvement in ICBT.
Another potential bias in the review process may have been introduced as we elected to include only those studies in which participants were identified as meeting diagnostic criteria for an anxiety disorder, as determined by a validated measure. While this is good practice for the empirical validity of the present review, it may not accurately reflect clinical practice. It is likely that as a part of regular clinical practice, clients with subclinical diagnoses might be assigned to pursue ICBT. We might assume that these treatments would be as effective for individuals with subclinical symptom patterns as they are for those with diagnosed disorders (for example, Spek 2007); however, our exclusion of these populations prevents any firm statements in this regard.
The present review is also potentially biased in the way that we have measured one of our primary outcomes, clinically important improvement in anxiety. This outcome would possibly be more clinically useful had it been narrowed to assess diagnostic remission, in particular, or divided into two outcomes assessing remission and recovery separately. This issue is larger than the field of ICBT and is a result of the lack of consensus in clinical psychology research in general regarding the most robust way to assess clinically significant improvement resulting from treatment. Consequently, there are a variety of ways to assess treatment outcome, including measures of remission, recovery, clinically significant improvement, and high end state functioning. Because this issue is quite prevalent in ICBT for anxiety studies as well, we elected to combine each of these unique ways of determining notable changes in symptomatology and functioning post‐treatment by creating the clinically important improvement outcome. While relevant and useful, the nuances of remission and recovery may be lost by being subsumed within this category. As the field expands, and consistency in reporting treatment outcomes increases, it may be useful to subdivide this outcome to more clearly capture remission and recovery.
It is also worth mentioning that given the conceptual and operational overlap between quality of life and disability measures in the anxiety disorder literature (Mogotsi 2000), we included both outcomes within the same meta‐analysis. However, given research suggesting that these concepts are overlapping but also distinct (Hambrick 2003), it may be that some variability in the impact of treatment on these measures was missed through their amalgamation. Future studies on ICBT should consider assessing both quality of life and disability as separate treatment outcomes.
Finally, it is necessary to note that our method of statistical analysis may have introduced some bias into the results. In combining multiple measures within one study that assessed the same outcome (for example, combining several measures of panic symptoms into one mean and standard deviation) we made use of a method described by Borenstein 2009 that requires the availability of bivariate correlations between the study measures in order for them to be combined. In four studies in the present review, these correlations were not available. In these situations we simply excluded the measure in question from the overall mean and measure of variance. The general concordance between each of the symptom measures within each study (that is, a series of symptom measures tended to show similar direction and degree of change from pre‐ to post‐treatment) means that the exclusion of one measure should not significantly impact the results. However, this process may have introduced some small degree of bias into the findings.
Agreements and disagreements with other studies or reviews
A number of prior meta‐analyses have investigated the efficacy of ICBT. These meta‐analyses have ranged from a quite broad scope investigating the efficacy of Internet interventions for any health problems (d = 0.53; Barak 2008) to a more focused scope investigating the efficacy of ICBT for clinical and subclinical anxiety and mood symptoms (d = 0.96; Spek 2007) or anxiety and mood disorders in Sweden (d = 0.91; Andersson 2007). Taken together, these reviews support the present findings that ICBT is efficacious in reducing anxiety symptoms as compared to control interventions (for example, waiting list control). Within their broad meta‐analysis, Barak 2008 found that interventions designed to treat PTSD and those targeting PD showed the largest effect sizes (g = 0.88 and 0.80, respectively). Spek 2007 found that those interventions that included therapist contact, as opposed to those that did not, showed a particularly large effect size (d = 1.00). It should be noted that some concerns were raised about the methodological quality of the studies included in these types of reviews given their small sample sizes, the absence of details about randomisation and treatment allocation methods, and lack of adequate information about treatment compliance and credibility (Postel 2008).
Recently, Mayo‐Wilson 2013 completed a review of media‐delivered self‐help BT and CBT for anxiety disorders. Within their review they included ICBT studies delivered both with and without therapist contact. In line with the present findings, their review suggested that media‐delivered self‐help BT and CBT were more efficacious than no treatment (that is, a waiting list control). In contrast to the present findings, their review resulted in some suggestion that media‐delivered self‐help BT and CBT were somewhat inferior to face‐to‐face CBT with the conclusion that for those who can access it, face‐to‐face CBT is probably superior. The differences between these findings and those in the present review may be due in part to the differences in therapist involvement between included studies across the two reviews. Therapist involvement in media‐delivered treatments, such as ICBT, may lead the treatments to be more similar in efficacy to face‐to‐face CBT than those interventions without therapist support.
In addition, several meta‐analyses have investigated the effects of computer‐based psychotherapy for mental health problems more broadly, the results of which are also in accordance with the present findings. In a meta‐analysis of computer‐aided psychotherapy (including treatment delivered via stand‐alone or Internet‐linked computers, smart phones, palm pilots, interactive voice response, and CDs or DVDs) for anxiety disorders, Cuijpers 2009 found that computer‐aided psychotherapy was more effective than control conditions (d = 1.08) in reducing anxiety symptoms, and computer‐aided psychotherapy outcomes did not differ significantly from those outcomes achieved through face‐to‐face treatment. Similarly, Reger 2009 found medium to large effects sizes when comparing computer‐based CBT and ICBT to waiting list, placebo, or treatment as usual comparators in treating anxiety. When they investigated the effects of therapist involvement on their findings, no significant differences were identified based on amount of therapist contact. Most recently, Andrews 2010 investigated the effects of computer therapy for anxiety and depression (including both computer‐ and Internet‐aided treatments) as compared to control conditions and face‐to‐face treatment. They found computer‐based therapy to be superior to control for the treatment of social phobia (g = 0.92), PD (g = 0.83), and GAD (g = 1.12). They also found a non‐significant difference in outcome between computer‐based and face‐to‐face CBT.
It is important to note that these latter meta‐analyses looked more broadly at methods of administering treatment via computer technology, including but not limited to the Internet. Moreover, they included research into non‐therapist supported interventions, interventions administered using interactive voice response, as well as those that included substantial face‐to‐face contact. Nevertheless, despite the differences between these meta‐analyses and our own, the overall body of research serves to add further evidence for the efficacy of therapist‐supported ICBT in treating anxiety disorders.
Authors' conclusions
Implications for practice.
The present findings, in consideration of the quality and quantity of the included studies, suggest that therapist‐supported ICBT is more efficacious in treating anxiety disorders among adults than a waiting list, attention, information, or online discussion group only control. The evidence also suggests that therapist‐supported ICBT may not differ from unguided ICBT in efficacy; however, this evidence is significantly limited by a lack of studies in this comparison and must be interpreted with caution. In addition, findings suggest that therapist‐supported ICBT may not result in significantly different anxiety outcomes as compared to face‐to‐face CBT. Face‐to‐face CBT is currently the intervention of choice for the treatment of anxiety disorders (Bisson 2007; Hunot 2007; Norton 2007; Stewart 2009).
Our results, in conjunction with the findings of prior meta‐analyses (for example, Cuijpers 2009; Andrews 2010), clearly support further research and development of this technology and type of treatment delivery. The benefit of Internet delivery is in its ability to extend treatment to individuals who may not be able to access treatment through traditional means. It is evidently a promising method to overcome obstacles to treatment delivery.
One important next step for this field is to extend research beyond the two laboratories (Sweden and Australia) that are responsible for almost all of the studies in this area. Replication of results across research sites and groups will go far toward increasing practitioners' confidence in the intervention as well as interest in exploring greater incorporation of this type of treatment into general practice. Another important step will be to uncover the most effective way to make this type of service delivery available to potential clients. For example, it may be possible to administer it as an extended service through regular mental health clinics, offering clients the choice to engage in Internet‐based or face‐to‐face treatment. Alternatively, ICBT may be more easily administered through clinics or divisions of clinics devoted entirely to this type of treatment.
Given the findings of the present review, it seems timely to start to think about the best ways to incorporate ICBT into clinical practice and explore the effectiveness of these methods. Widespread rollout of ICBT may not yet be warranted, but continued steps toward this goal should be pursued. Internet‐based programs appear to be efficacious in reducing anxiety symptoms and there are many individuals in need of treatment who could benefit from this type of delivery.
Implications for research.
The present review suggests some important directions for future research. First, further research is needed into the efficacy of ICBT for the anxiety disorders that have not yet been extensively examined, including OCD, PTSD, and specific phobia. The fact that these disorders tend to be thought of as more complex, and rely heavily on exposure‐based elements, may have deterred researchers from translating them into an ICBT intervention. However, given the similarities in CBT for these disorders and CBT for the already investigated disorders (PD, social phobia, and GAD), including other disorders with a heavy emphasis on exposure (that is, PD), it seems possible that ICBT would also be efficacious in treating these disorders and thus warrants investigation. With respect to specific phobia, it is possible that this category of disorder has received less attention as it is less commonly treated in clinics because it tends to be less functionally impairing relative to other anxiety disorders and often requires only short interventions. An extensive collection of self‐help manuals to treat specific phobias exists; suggesting that this type of treatment would be very amenable to an ICBT delivery and would likely lead to efficacious interventions. Further research into these disorders would be an important area of investigation.
Second, while research comparing therapist‐supported ICBT to a waiting list, attention, information, or online discussion group only control is substantial, studies comparing therapist‐supported ICBT to face‐to‐face therapy are somewhat fewer. Subgroup analyses in the present review suggest some ambiguity with respect to the comparable efficacy of treatment between ICBT and face‐to‐face CBT for social phobia and PD. Further studies would help clarify this question. Moreover, the nature of the included studies is only sufficient for us to conclude that there may not be significant differences in treatment outcome between face‐to‐face CBT and ICBT with therapist support. Future equivalence trials are warranted to further clarify the direct comparability of ICBT with therapist support and face‐to‐face CBT for anxiety.
Third, the importance of the therapist in ICBT remains somewhat unclear. On the one hand prior work has suggested an important association between therapist involvement and ICBT treatment outcome (Spek 2007; Andersson 2009b). On the other hand the studies included in our comparison of therapist‐supported ICBT versus unguided CBT (each of which focused on social phobia) suggest no difference in treatment outcome between the two interventions. More studies comparing therapist‐supported ICBT versus unguided CBT are needed to clarify the role of the therapist. Moreover, if therapist contact is important, the amount of contact that would optimise treatment outcome as well as the use of resources has yet to be determined. Each of the included studies in this review employed various amounts of therapist contact in delivering ICBT. Subgroup analyses based on the amount of therapist contact did not suggest many differences from the overall pooled analysis; however, the subgroups were rather small and set somewhat arbitrarily. Future research into the optimal amount of therapist contact would help maximize the efficacy and efficiency with which ICBT could be delivered.
Fourth, with respect to the assessment of study outcomes, the inclusion of diagnostic assessment post‐treatment is encouraged in future trials in this field. While all studies measured anxiety symptoms via self‐report, more objective measures of participants' diagnostic profile will help in determining the clinical significance of treatment outcomes. Fifth, this review highlighted the limited number of studies conducting follow‐up assessments of participants' symptoms. While the present results do not suggest a significant relapse in symptoms after a six month follow‐up period, further studies are needed.
Sixth, it is important to note that any adverse effects of ICBT have not been well‐examined. Evidently, this type of treatment did not result in significant symptom reduction for each participant. There were also a small number of participants across studies who reported being dissatisfied with this type of treatment. More research is needed to better define and measure 'harms' that might result from this type of treatment.
Finally, as suggested above, future effectiveness studies examining the best way to incorporate ICBT into regular clinical practice seem to be an important next step in the field.
What's new
| Date | Event | Description |
|---|---|---|
| 24 February 2016 | New citation required but conclusions have not changed | Review updated |
| 24 February 2016 | New search has been performed | New search conducted 16 March 2015 and eight new studies incorporated |
History
Review first published: Issue 3, 2015
| Date | Event | Description |
|---|---|---|
| 15 September 2015 | Feedback has been incorporated | Addressed reviewers' comments in this version. |
Acknowledgements
The authors would like to thank Karen Neves, Reference and Research Librarian at Dalhousie University, and Sarah Dawson, Trial Search Co‐ordinator for the Cochrane Collaboration Depression, Anxiety, and Neurosis Group (CCDAN), for their help in developing and conducting the search strategy for the present review. We would also like to thank Leah Jones for her administrative and research assistance with the review process. Finally, we would like to thank the CCDAN editorial team, particularly Chris Champion and Jessica Sharp, for their advice and assistance.
Appendices
Appendix 1. CCDANCTR searches (to Sept 2014)
CCDANCTR Search 1 (all years to 12‐April‐2013) (as per protocol)
The CCDANCTR‐Studies Register was searched using the following terms: 1. Condition = (anxiety or *phobi* or PTSD or post‐trauma* or “post trauma*” or posttrauma* or “stress disorder” or panic or OCD or obsess* or compulsi* or GAD) 2. Intervention = (CBT or cognitive or behavio* or *therap* or treatment or intervention or training or counsel*) 3. Age Group = (adult or aged or unclear or “not stated”) 4. Free‐Text = (computer* or distance* or remote or tele* or Internet* or web* or WWW or phone or mobile or e‐mail* or email* or online* or on‐line or videoconferenc* or video‐conferenc* or “chat room*” or “instant messaging” or iCBT) 5. (1 and 2 and 3 and 4)
The CCDANCTR‐References Register was searched using the following terms to find additional untagged/uncoded reports of RCTs: 1. (anxiety or *phobi* or PTSD or post‐trauma* or “post trauma*” or posttrauma* or (stress and disorder*) or panic or OCD or obsess* or compulsi* or GAD):ti,ab,kw 2. (therap* or train*):ti,ab 3. (psychotherap* or cognitive* or behavio* or CBT):ti,ab,kw 4. (acceptance* or assertive* or brief* or commitment* or exposure or group or implosive or “problem solving” or problem‐solving or "solution focused" or solution‐focused or schema):ti,ab,kw 5. (CBT or cognitive* or behavio* or “contingency management” or “functional analys*” or mindfulness* or “mind training” or psychoeducat* or relaxation or “role play*”):ti,ab,kw 6. ((2 or 3) and 4) or 5 7. (computer* or distance* or remote or tele* or Internet* or web* or WWW or phone or mobile or e‐mail* or email* or online* or on‐line or videoconferenc* or video‐conferenc* or "chat room*" or "instant messaging" or iCBT):ti,ab,kw 8. 1 and 6 and 7
CCDANCTR Search 2 (12‐April 2013 to 15‐Sept‐2014) (precision maximizing)
Prior to publication of the first version of this review, CCDAN’s Trials Search Co‐ordinator performed a precision maximizing update search of the CCDANCTR Registers. The results were screened at the CCDAN’s editorial base and by the first author of this review and relevant studies placed in awaiting classification or ongoing (as appropriate).
1. (internet* or online or web*):ti 2. (*phobi* or panic or "anxiety disorder*" or (anxiety and depression) or GAD or "general* anxiety" or OCD or obsess* or PTSD or *trauma* or "stress disorder*"):ti 3. (assisted or administer* or coach* or guided or guidance or *therapist* or ((telephone or email) next (support or assist*))):ti,ab 4. (1 and 2 and 3) 5. (2012* or 2013* or 2014*):yr,xdd
[CRS platform, key to field codes: ti:title; ab:abstract; yr:year; xdd:record entry date]
Data and analyses
Comparison 1. Therapist‐supported ICBT versus waiting list control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinically Important Improvement in Anxiety at Post‐Treatment | 12 | 866 | Risk Ratio (M‐H, Random, 95% CI) | 3.75 [2.51, 5.60] |
| 1.1 Social Phobia | 1 | 204 | Risk Ratio (M‐H, Random, 95% CI) | 6.0 [2.64, 13.62] |
| 1.2 GAD | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 2.58 [1.48, 4.51] |
| 1.3 Panic Disorder | 2 | 81 | Risk Ratio (M‐H, Random, 95% CI) | 18.32 [2.50, 134.18] |
| 1.4 PTSD | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 3.48 [1.78, 6.80] |
| 1.5 OCD | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 14.06 [0.88, 225.47] |
| 1.6 Mixed Anxiety | 3 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 3.76 [1.68, 8.43] |
| 2 Anxiety Symptom Severity at Post‐Treatment | 30 | 2147 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.06 [‐1.29, ‐0.82] |
| 2.1 Social Phobia | 8 | 661 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.38 [‐1.63, ‐1.13] |
| 2.2 GAD | 6 | 394 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.19, ‐0.42] |
| 2.3 Panic Disorder | 6 | 323 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.52 [‐2.56, ‐0.48] |
| 2.4 PTSD | 2 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.78 [‐1.38, ‐0.17] |
| 2.5 OCD | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.35, 0.08] |
| 2.6 Mixed Anxiety | 7 | 633 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.20, ‐0.41] |
| 3 General Anxiety Symptom Severity at Post‐Treatment | 19 | 1496 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐0.98, ‐0.52] |
| 3.1 Social Phobia | 3 | 341 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐0.85, ‐0.42] |
| 3.2 GAD | 2 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.91 [‐3.57, ‐0.26] |
| 3.3 Panic Disorder | 4 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.35, ‐0.13] |
| 3.4 PTSD | 2 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.02, ‐0.23] |
| 3.5 OCD | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐1.79, ‐0.30] |
| 3.6 Mixed Anxiety | 7 | 633 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.69, ‐0.29] |
| 4 Quality of Life at Post‐Treatment | 23 | 1639 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.38, 0.57] |
| 4.1 Social Phobia | 6 | 586 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.28, 0.61] |
| 4.2 GAD | 5 | 360 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [0.35, 0.78] |
| 4.3 Panic Disorder | 4 | 176 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.15, 0.75] |
| 4.4 PTSD | 2 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.41 [0.02, 0.80] |
| 4.5 OCD | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.6 Mixed Anxiety | 6 | 413 | Std. Mean Difference (IV, Random, 95% CI) | 0.47 [0.27, 0.67] |
Comparison 2. Therapist‐supported ICBT versus unguided CBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinically Important Improvement in Anxiety at Post‐Treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Social Phobia | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Anxiety Symptom Severity at Post‐Treatment | 5 | 312 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.56, 0.13] |
| 2.1 Social Phobia | 4 | 253 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.69, 0.21] |
| 2.2 OCD | 1 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.65, 0.37] |
| 3 Anxiety Symptom Severity at Follow‐up | 3 | 192 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.58, ‐0.01] |
| 3.1 Social Phobia | 3 | 192 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.58, ‐0.01] |
| 4 General Anxiety Symptom Severity at Post‐Treatment | 2 | 138 | Mean Difference (IV, Random, 95% CI) | 0.28 [‐2.21, 2.78] |
| 4.1 Social Phobia | 2 | 138 | Mean Difference (IV, Random, 95% CI) | 0.28 [‐2.21, 2.78] |
| 5 General Anxiety Symptom Severity at Follow‐up | 2 | 138 | Mean Difference (IV, Random, 95% CI) | 0.72 [‐2.12, 3.57] |
| 5.1 Social Phobia | 2 | 138 | Mean Difference (IV, Random, 95% CI) | 0.72 [‐2.12, 3.57] |
| 6 Quality of Life at Post‐Treatment | 3 | 199 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.37, 0.50] |
| 6.1 Social Phobia | 3 | 199 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.37, 0.50] |
| 7 Quality of Life at Follow‐up | 2 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.53, 0.14] |
| 7.1 Social Phobia | 2 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.53, 0.14] |
Comparison 3. Therapist‐supported ICBT versus face‐to‐face CBT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Clinically Important Improvement in Anxiety at Post‐Treatment | 4 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.89, 1.34] |
| 1.1 Social Phobia | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [0.77, 2.76] |
| 1.2 Panic Disorder | 3 | 239 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.85, 1.32] |
| 2 Clinically Important Improvement in Anxiety at Follow‐up | 3 | 279 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.94, 1.27] |
| 2.1 Social Phobia | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.73, 1.83] |
| 2.2 Panic Disorder | 2 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.93, 1.28] |
| 3 Anxiety Symptom Severity at Post‐Treatment | 7 | 450 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.25, 0.37] |
| 3.1 Social Phobia | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.92, 0.57] |
| 3.2 Panic Disorder | 3 | 234 | Std. Mean Difference (IV, Random, 95% CI) | 0.29 [0.03, 0.54] |
| 3.3 Specific Phobia | 2 | 53 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.56, 0.52] |
| 4 Anxiety Symptom Severity at Follow‐Up | 6 | 367 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.41, 0.00] |
| 4.1 Social Phobia | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.71, ‐0.08] |
| 4.2 Panic Disorder | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.36, 0.28] |
| 4.3 Specific Phobia | 2 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.64, 0.46] |
| 5 General Anxiety Symptom Severity at Post‐Treatment | 6 | 343 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.42, 0.55] |
| 5.1 Social Phobia | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.49, 0.13] |
| 5.2 Panic Disorder | 2 | 129 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.75, 1.60] |
| 5.3 Specific Phobia | 2 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐1.07, 0.79] |
| 6 General Anxiety Symptom Severity at Follow‐up | 5 | 263 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.37, 0.11] |
| 6.1 Social Phobia | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.45, 0.17] |
| 6.2 Panic Disorder | 1 | 49 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.74, 0.39] |
| 6.3 Specific Phobia | 2 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.61, 0.49] |
| 7 Quality of Life at Post‐Treatment | 5 | 392 | Std. Mean Difference (IV, Random, 95% CI) | 0.26 [0.06, 0.45] |
| 7.1 Social Phobia | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.09, 0.53] |
| 7.2 Panic Disorder | 3 | 229 | Std. Mean Difference (IV, Random, 95% CI) | 0.28 [0.02, 0.54] |
| 8 Quality of Life at Follow‐up | 4 | 316 | Std. Mean Difference (IV, Random, 95% CI) | 0.33 [0.11, 0.55] |
| 8.1 Social Phobia | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | 0.36 [0.01, 0.70] |
| 8.2 Panic Disorder | 2 | 153 | Std. Mean Difference (IV, Random, 95% CI) | 0.28 [‐0.04, 0.60] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andersson 2009.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Specific Phobia, Spider Type Method of diagnosis: SCID‐IV N: 27 Age: M = 25.6 (SD = 4.1); range = 18 to 65 years Sex: 84.8% women Country of residence: Sweden Method of enrolment: responded to media advertisements in community Baseline depression severity: (BDI‐II) ICBT M = 7.9 (SD = 5.9); Live exposure M = 6.9 (SD = 6.2) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based BT with e‐mail support (n = 13) Duration: 5 online modules completed over 4 weeks Treatment protocol*: participants completed online modules on psychoeducation and exposure, with e‐mail support from a therapist for module exercises Therapists: trained and supervised in this treatment protocol by treatment founder (Ӧst) Therapist contact: 25 min per participant Face‐to‐face contact: none Dropout: n = 0; 0% (2) Live exposure (n = 14) Duration: 2 face‐to‐face sessions over 1 week Treatment protocol*: participants attended an orientation session and one graded exposure session with a therapist Therapists: trained and supervised in this treatment protocol by treatment founder (Ӧst) Therapist, face‐to‐face contact: one orientation session and one 3 hr exposure session Dropout: n = 0; 0% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 1 year follow‐up Primary outcomes: (1) specific phobia symptoms: Behavioural Avoidance Test; Spider Phobia Questionnaire; Fear Survey Schedule‐III (2) general anxiety: Beck Anxiety Inventory |
|
| Notes | *treatment based on: Ӧst, L.‐G. (1997). Rapid treatments of specific phobias. In G.C.L. Davey (Ed.), Phobias: A handbook of theory, research and treatment (pp. 227–246). Chichester, UK: Wiley. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Thirty participants...were randomised by an independent person to either..." Comment: insufficient detail about method of randomisation provided to determine risk |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus face‐to‐face CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Three participants were dropped because of computer problems (n=1) or lack of time (n=2)." Comment: unclear which treatment condition the dropouts were from; ITT analyses were not used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Unclear risk | Group comparisons at baseline not reported |
Andersson 2012a.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: SCID‐IV N: 204 Age: for ICBT, M = 38.1 (SD = 11.3); for discussion group, M = 38.4 (SD = 10.9); range = 19 to 71 years Sex: 61% women Country of residence: Sweden Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: 13.7% Method of enrolment: responded to online study advertisement Baseline depression severity: (MADRS‐S) ICBT M = 13.45 (SD = 7.14); Discussion group M = 14.29 (SD = 6.63) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 102) Duration: 9 online modules completed over 9 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, social skills, and relapse prevention, with email support from a therapist for module exercises Therapists: 7 licensed clinical psychologists (avg. 3 years experience; previous experience with Internet treatment) and 6 clinical psychology students in their last year of the master's program; all had basic CBT training; students had clinical supervision during study Therapist contact: 15 min per participant each week Face‐to‐face contact: none Dropout: n = 8; 7.8% (2) Online discussion group (n = 102) Duration: 9 weeks Treatment protocol: participants made weekly posts in an online topic‐relevant discussion group Therapist, face‐to‐face contact: none Dropout: n = 2; 2% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) social phobia symptoms: Liebowitz Social Anxiety Scale, Social Phobia Scale, Social Interaction Anxiety Scale, Social Phobia Screening Questionnaire (2) general anxiety: Beck Anxiety Inventory (3) clinically important improvement: Clinical Global Impression Improvement Scale Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on: Furmark, T., Holmstrom, A., Sparthan, E., Carlbring, P., & Andersson, G. (2006). Social fobi – Effectiv hjalp med kognitiv beteendeterapi [Social phobia – effective help via CBT]. Stockholm: Liber. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed by an independent third‐party using an online true random‐number service (www.random.org)." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus online discussion group) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "Outcome assessors were not aware of treatment status before the interview." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Eight participants in the treatment group and 2 in the control group did not complete posttreatment data yielding a 5% dropout. In accordance with the ITT principle, all participants were asked to complete posttreatment and follow‐up assessments, regardless of how many treatment modules they had completed and all were included in the analyses." Comment: a small number of dropouts from both conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results were reported for all outcome measures outlined in the trial registration |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Andersson 2012b.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of diagnosis: SCID‐IV N: 81 Age: for ICBT, M = 44.4 (SD = 12.8); for internet psychodynamic therapy, M = 36.4 (SD = 9.7); for WLC, M = 39.6 (13.7); range = 19 to 66 years Sex: 76.5% women Country of residence: Sweden Psychiatric co‐morbidity: 22.2% Social Phobia, 19.8% Panic Disorder, 3.7% OCD, 23.5% Major Depression Co‐use of adjunct therapy: excluded Co‐use of medication: 32.1% Method of enrolment: responded to study advertisements in community and online Baseline depression severity: (MADRS‐S) ICBT M = 22.30 (SD = 6.52); WLC M = 21.41 (SD = 5.99) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail support (n = 27) Duration: 8 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, applied relaxation, worry time, cognitive restructuring, problem solving, exposure, sleep management, and relapse prevention, with e‐mail support from a therapist for module exercises Therapists: 2 licensed psychologists (previous experience with Internet treatment) and 3 psychology students in their final year; all had CBT training; supervised by a senior researcher and licensed CBT therapist Therapist contact: M total time spent by therapist per participant = 92 min (SD = 61) Face‐to‐face contact: none Dropout: n = 7; 25.9% (2) Internet‐based psychodynamic therapy with email support (n = 27) Duration: 8 online modules completed over 8 weeks Treatment Protocol^: participants completed online modules on seeing, understanding, and breaking unconscious patterns that contribute to emotional difficulties and guarding against future relapses, with email support and encouragement from a therapist Therapists: a licensed psychologist and 3 students in their final year of a clinical psychology program; all trained in psychodynamic therapy Therapist contact: M total time spent by therapist per participant = 113 min (SD = 41) Face‐to‐face contact: none Dropout: n = 5; 18.5% (3) Waiting list control (n = 27) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout: n = 2; 7.4% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcomes: (1) generalized anxiety disorder symptoms: Penn State Worry Questionnaire, Generalized Anxiety Disorder Questionnaire IV (2) general anxiety: State Trait Anxiety Inventory, Beck Anxiety Inventory (3) clinically important improvement: SCID‐IV Secondary outcome: (1) quality of life: Quality of Life Inventory (at post‐treatment): participants reported if they were completely, moderately, or not satisfied with treatment |
|
| Notes | *treatment based on: Paxling, B., Almlov, J., Dahlin, M., Carlbring, P., Breitholtz, E., Eriksson, T., & Andersson, G. (2011). Internet‐delivered cognitive behaviour therapy for generalized anxiety disorder: A randomised controlled trial. Cognitive Behaviour Therapy, 40, 159‐173. ^treatment based on: Silverberg, F. (2005). Make the leap: A practical guide to breaking the patterns that hold you back. New York: Marlow and Company. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization procedure was managed by an external administrator who was not otherwise involved in the study. A true random number service (www.random.org) was used to ensure complete randomness. Randomization was done after inclusion wherein participants were randomized to the three groups with no stratification." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus online discussion group) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "After the treatment period, the interviewers were blinded concerning participant status and allocation (given that the posttreatment interviewers did not have access to information about the participants). In addition, participants were asked not to reveal whether they had received treatment." Comment: interviewers were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | A small number of dropouts from each condition (depending on outcome measure, 4 to 7 for Internet CBT, 1 to 5 dropouts for Internet psychodynamic therapy and 1 to 2 dropouts for waiting list control) and intention‐to‐treat analyses were used |
| Selective reporting (reporting bias) | Low risk | All results were reported for all outcome measures outlined in the trial registration |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Andersson 2013.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Specific Phobia, Snake Type Method of diagnosis: SCID‐IV N: 30 Age: M = 27.2 (SD = 8.1); range 19 to 54 years Sex: 84.6% women Country of residence: Sweden Psychiatric co‐morbidity: not reported Co‐use of adjunct therapy: not reported Co‐use of medication: not reported Method of enrolment: online and media advertisements Baseline depression severity: (BDI) IBT M = 3.6 (SD = 3.4); face‐to‐face BT M = 2.2 (SD = 2) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based BT with email support (n = 15) Duration: 4 online modules completed over 4 weeks Treatment protocol*: participants completed online modules on exposure techniques, with email support from a therapist Therapist: 3 clinical psychology students, 1 licensed psychologist Therapist contact: M time spent by therapist per participant overall = 25 Face‐to‐face contact: none Dropout: n = 2; 13.3% (2) Face‐to‐face individual BT (n = 15) Duration: 9 online modules completed over 12 weeks Treatment protocol*: participants attended an orientation session and one graded exposure session with a therapist Therapist: 3 clinical psychology students, 1 licensed psychologist Therapist/Face‐to‐face contact: 180 mins Dropout: n = 2; 13.3% |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment and 1 year follow‐up Primary outcomes: (1) specific phobia symptoms: Behavioural Avoidance Test, Fear Survey Schedule – III, Snake Phobia Questionnaire (2) general anxiety: Beck Anxiety Inventory |
|
| Notes | *Ost, L.‐G. (1997). Rapid treatments of specific phobias. In G. C. L. Davey (Ed.), Phobias: A handbook of theory, research and treatment (pp. 227‐246). Chichester: Wiley. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A total of 30 participants met the inclusion criteria and were randomized by an independent person to either OST or guided Internet treatment (using a computerized randomization procedure)." Comment: Adequate randomization method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (guided internet‐based treatment or live treatment) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Unclear risk | Unclear how the one observer‐rated measure was evaluated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "However, two immediately dropped out (one in each condition), and two completed the treatment but did not provide follow‐up data (also one in each condition), leaving a total of 26 participants in the trial. Given the small sample size, we made no attempt to impute the missing data of the four missing cases." Comment: Dropouts reported were small and similar across conditions but reasons for dropouts were not clear; ITT analyses were not used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Unclear risk | Group comparisons at baseline not reported |
Berger 2009.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: SCID‐IV N: 52 Age: M = 28.9 (SD = 5.3); range = 19 to 43 years Sex: 44.2% women Country of residence: 88% Switzerland, 10% France, 2% Belgium Psychiatric co‐morbidity: 26.9% had a co‐morbid Axis I diagnosis Co‐use of adjunct therapy or medication: excluded Method of enrolment: responded to study advertisements in community and online Baseline depression severity: (BDI‐II) ICBT M = 16.6 (SD = 6.2); WLC M = 17.9 (SD = 10.4) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email support (n = 31) Duration: 5 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, self‐focused attention, safety behaviours, in vivo exposure, and cognitive restructuring, with email support from a therapist for module exercises Therapists: 6 master’s level clinical psychologists; 4 in their first year of a CBT training program, 2 in a postgraduate clinical psychology and psychotherapy course Therapist contact: M e‐mails from participant = 5.5 (range = 0 to 16); in addition to responding to these, therapists sent weekly motivating e‐mails Face‐to‐face contact: none Dropout: n = 3; 9.7% (2) Waiting list control (n = 21) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 2; 9.5% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcome: (1) social phobia symptoms: Liebowitz Social Anxiety Scale – Self‐Report; Social Phobia Scale; Social Interaction Anxiety Scale Secondary outcome: (1) treatment satisfaction (at post‐treatment): participants reported if they were completely, moderately, or not satisfied with treatment |
|
| Notes | *treatment based on: Stangier, U., Heidenreich, T., & Peitz, M. (2003). Soziale Phobien. Ein kognitiv‐verhaltenstherapeutisches Behandlungsmanual [Social phobia. A cognitive‐behavioral treatment manual]. Weinheim: Beltz. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We used a weighted randomizations procedure (Altman, 1991), such that 60% were assigned to the treatment condition and 40% to the waiting‐list control group. According to a computer‐generated randomizations scheme..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "After randomizations, 5 participants (3 in the treatment group and 2 in the control group) dropped out during the course of the study and did not complete post assessment (9.6%). According to an ITT paradigm..." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | Trial registration suggests that the State Trait Anxiety Inventory was completed by participants, however, results are not reported for this outcome; all other outcomes outlined in the protocol are reported in the manuscript |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Berger 2011.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: SCID‐IV N: 81 Age: M = 37.2 (SD = 11.2); range = 19 to 62 years Sex: 53.1% women Country of residence: Switzerland Psychiatric co‐morbidity: 38% had at least one other Axis I diagnosis; 12% PD, 10% Specific Phobia, 2% GAD, 22% MDD or Dysthymia, 2% Eating Disorder Co‐use of adjunct therapy: excluded Co‐use of medication: 7.4% Method of enrolment: responded to study advertisements in community and online Baseline depression severity: (BDI‐II) Guided ICBT M = 18.2 (SD = 11.5); Unguided ICBT M = 17.7 (SD = 9.8) |
|
| Interventions | Participants were randomly assigned to one of: (1) Guided internet‐based CBT (with e‐mail support) (n = 27) Duration: 5 online modules completed over 10 weeks (M hrs spent online = 10) Treatment protocol*: participants completed online modules on motivational interviewing, psychoeducation, cognitive restructuring, self‐focused attention, and exposure, with weekly e‐mail support from a therapist Therapists: 2 clinical psychology master's level graduate students, 2 master’s level clinical psychologists in post‐graduate CBT training, 2 licensed psychologists with more than 5 years research and clinical experience Therapist contact: M e‐mails from participant = 6.16 (SD = 4.56; range = 1 to 17); M e‐mails from therapist = 12.44 (SD = 2.85; range = 6 to 17) Face‐to‐face contact: none Dropout: n = 3; 11.1% (2) Unguided internet‐based CBT (n = 27) Duration: 5 online modules completed over 10 weeks (M hrs spent online = 9.5) Treatment protocol*: participants completed online modules on motivational interviewing, psychoeducation, cognitive restructuring, self‐focused attention, and exposure independently Therapist, face‐to‐face contact: none Dropout: n = 1; 3.7% (3) Step‐up on demand Internet‐based CBT (with e‐mail or phone support) (n = 27) Duration: 5 online modules completed over 10 weeks (M hrs spent online = 10.5) Treatment protocol*: participants completed online modules on motivational interviewing, psychoeducation, cognitive restructuring, self‐focused attention, and exposure, with e‐mail or phone support, or both, from a therapist as requested Therapists: 2 clinical psychology master's level graduate students, 2 master’s level clinical psychologists in post‐graduate CBT training, 2 licensed psychologists with more than 5 years research and clinical experience Therapist contact: 52% of participants did not request contact, 33% requested weekly e‐mail contact, 7% requested weekly e‐mail and phone contact Face‐to‐face contact: none |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 6 month follow‐up Primary outcomes: (1) social phobia symptoms: Liebowitz Social Anxiety Scale – Self‐Report; Social Phobia Scale; Social Interaction Anxiety Scale (2) clinically important improvement: SCID‐IV Secondary outcome: (1) treatment satisfaction (at post‐treatment): Client Satisfaction Questionnaire |
|
| Notes | *treatment based on: Stangier, U., Heidenreich, T., & Peitz, M. (2003). Soziale Phobien. Ein kognitiv‐verhaltenstherapeutisches Behandlungsmanual [Social phobia. A cognitive‐behavioral treatment manual]. Weinheim: Beltz. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomised into one of the three conditions using a computerized random number generator (www.random.org)." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation schedule was generated by an independent researcher and was unknown to the investigators." Comment: allocation likely concealed sufficiently to prevent deviations from protocol |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (guided versus unguided versus step‐up on demand Internet‐based CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | High risk | Quote: "The interviewers could not be kept blind regarding group assignment at post‐assessment because some participants disclosed aspects of the group assignment during the interview." Comment: attempts were made to ensure interviewers were blind to treatment condition, however, participants revealed their treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Six participants (7.4%) dropped out before post‐treatment assessment (one in the self‐help group, three in the guided self‐help group, and two in the step‐up of support on demand condition)."; "There was no significant difference in terms of demographics, pre‐treatment, or post‐treatment scores between those who provided post‐treatment and follow‐up data and those who did not..."; "All analyses were based on the ITT sample." Comment: a small and similar number of dropouts from the three treatment conditions was reported; reasons were provided for dropouts (self‐help: disappointed with group assignment; guided self‐help: wanted face‐to‐face contact or had internet trouble; step‐up on demand: vacation or no reason); ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Berger 2014.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with or without Agoraphobia (33.3%), Social Phobia (85.6%), Generalized Anxiety Disorder (25%) Method of diagnosis: SCID‐IV N: 132 Age: M = 35.1 (SD = 11.4); range = 18 to 65 years Sex: 56.1% women Country of residence: Switzerland, Germany, Austria Psychiatric co‐morbidity: 37.1% Panic Disorder with or without Agoraphobia, Social Phobia, or Generalized Anxiety Disorder, 13.6% Major Depressive Disorder, 15.9% Specific Phobia, 5.3% Obsessive Compulsive Disorder, 12.1% other Axis I Disorder Co‐use of adjunct therapy: excluded Co‐use of medication: 14.4% Method of enrolment: via online and media advertisements Baseline depression severity: (BDI‐II) Standard ICBT M = 19.1 (SD = 10.4); Tailored ICBT = 20.2 (11.7); Waiting List M = 20.3 (SD = 10.1) |
|
| Interventions | Participants were randomly assigned to one of: (1) Standard disorder‐specific Internet‐based CBT with email support (n = 44) Duration: 8 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on motivational enhancement, psychoeducation, cognitive restructuring, mindfulness, exposure, lifestyle, problem‐solving, and relapse prevention specific to their primary diagnosis, with email support from a therapist Therapist: 5 clinical psychology graduate students, 1 clinical psychologist, 1 CBT therapist Therapist contact: M emails sent by therapist = 12.6 (SD = 4.6); M emails sent by participant = 6.53 (SD = 7.2) Face‐to‐face contact: none Dropout: n = 5; 11.4% (2) Tailored Internet‐based CBT with email support (n = 44) Duration: 8 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on motivational enhancement, psychoeducation, cognitive restructuring, mindfulness, exposure, lifestyle, problem‐solving, and relapse prevention tailored to their anxiety symptoms, with email support from a therapist Therapist: 5 clinical psychology graduate students, 1 clinical psychologist, 1 CBT therapist Therapist contact: M emails sent by therapist = 12.6 (SD = 4.6); M emails sent by participant = 6.53 (SD = 7.2) Face‐to‐face contact: none Dropout: n = 4; 9.1% (3) Waiting list control (n = 44) Duration: 8 weeks Therapist/Face‐to‐face contact: none Dropout: n = 4; 9.1% |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment and 6 month follow‐up Primary outcomes: (1) anxiety symptoms: Brief Symptom Inventory, Social Phobia Scale, Social Interaction Anxiety Scale, Agoraphobic Cognitions Questionnaire, Body Sensations Questionnaire, Mobility Inventory, Penn State Worry Questionnaire (2) general anxiety: Beck Anxiety Inventory (3) clinically important improvement: SCID‐IV Secondary outcome: (1) treatment satisfaction: Client Satisfaction Questionnaire – 8 |
|
| Notes | *based on established CBT approaches for Social Phobia (Clark, D. M., & Wells, A. (1995). A cognitive model of social phobia. New York: Guilford Press.; Stangier, U., Heidenreich, T., & Peitz, M. (2003). Soziale Phobien. Ein kognitiv‐verhaltenstherapeutisches Behandlungsmanual. Weinheim: Beltz.), Panic Disorder (Margraf, J., & Schneider, S. (1989). Panik. Angstanfalle und ihre Behandlung. Berlin: Springer.; Schneider, S., & Margraf, J. (1998). Fortschritte der psychotherapie: Agoraphobie und panikstorung. Gottingen: Hogrefe.), and Generalized Anxiety Disorder (Becker, E., & Margraf, J. (2002). Generalisierte Angststorung. Ein Therapieprogramm. Weinheim: Beltz Verlag.) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "…a stratified randomization procedure was applied such that a balanced distribution of primary diagnosis groups in the three treatment arms was ensured. The allocation lists were made using a computerized random number generator and were unknown to the investigators" Comment: Adequate randomization method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The allocation lists were made using a computerized random number generator and were unknown to the investigators." Comment: Possibly adequate allocation concealment; but unsure how it occurred |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (guided internet‐based treatment or live treatment) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | High risk | Quote: "Fifth, a further study limitation is that interrator reliability of the Structured Clinical Interview was not assessed in this sample, and that the interviewers could not be kept blind regarding group assignment at postassessment because some participants disclosed aspects of the group assignment during the interview." Comment: Many participants broke assessor blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Thirteen participants (9.8%) dropped out before the posttreatment assessment (four in the tailored condition, five in the standardized condition, and four in the wait‐list condition)."; "At posttreatment, missing data were placed by the last‐observation‐carried‐forward method (LOCF)." Comment: Dropouts reported and were small and similar across conditions; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Quote: "There were no statistically significant differences between the treatment and control groups with regard to demographics, the diagnoses of participants, or pre‐treatment self‐report scores." Comment: No baseline group differences |
Bergstrom 2010.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder (n=16) or Panic Disorder with Agoraphobia (n = 88) Method of diagnosis: MINI N: 104 Age: for ICBT, M = 33.8 (SD = 9.7); for face‐to‐face CBT, M = 34.6 (SD = 9.2) Sex: 61.5% women Country of residence: Sweden Co‐use of adjunct therapy: excluded Co‐use of medication: 45% (34% SSRI or SNRI, 13% benzodiazepines, 24% benzodiazepine derivatives or neuroleptics, 5% tricyclic antidepressants) Method of enrolment: referred to study by health professionals or self‐referred to study clinic Baseline depression severity: (MADRS‐S) ICBT M = 8.9 (SD = 5.2); face‐to‐face CBT M = 9.5 (SD = 4.9) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 50) Duration: 10 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, and relapse prevention, with e‐mail support from a therapist for module exercises, and posted on an online discussion forum Therapists: psychologists Therapist contact: M e‐mails from therapist = 11.3 (SD = 4.3); M total time spent by therapist per participant = 35.4 min (SD = 19) Face‐to‐face contact: none Dropout: n = 9; 17% (2) Face‐to‐face group CBT (n = 54) Duration: 10 face‐to‐face group therapy sessions over 10 weeks Treatment protocol*: group sessions focused on psychoeducation, cognitive restructuring, exposure, and relapse prevention Therapists: 2 regular clinical psychologists, not specially trained for this study Therapist, face‐to‐face contact: 10 x 2 hr group sessions Dropout: n = 11; 18.3% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 6 month follow‐up Primary outcomes: (1) panic symptoms: Panic Disorder Severity Scale; Anxiety Sensitivity Index (2) clinically important improvement: MINI Secondary outcome: (1) quality of life: Sheehan Disability Scale |
|
| Notes | *treatment based on: Barlow D.H., & Craske M.G. (2000). Mastery of your anxiety and panic (MAP‐3). San Antonio: The Psychological Corporation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participants were divided into two groups...by an independent random number procedure..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Low risk | Quote: "...where each patient was assigned to either treatment by the opening of sealed numbered envelopes." Comment: adequate allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based applied relaxation versus Internet‐based CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | Low risk | Quote: "All outcome measures...were administered during the clinical interview..." Comment: self‐report outcomes were not completed |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "The psychiatrists performing the clinical interviews at post‐treatment and follow‐up were blind to treatment condition."; "All outcome measures...were administered during the clinical interview..." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Nine participants dropped out after randomisation but before commencing treatment. Various reasons were given for not starting treatment, but all pertained to different life circumstances of the individual participants and not to randomisation status. These initial dropouts were excluded from the statistical analyses."; "A number of patients did not return for the clinical interview at post‐treatment... a mixed effects models approach was used in the statistical analysis to adjust for these missing values." Comment: a similar number of dropouts from both treatment conditions was reported (during treatment: six from treatment, five from comparator); mixed effects models were used to account for missing data |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Unclear risk | Group comparisons at baseline not reported |
Carlbring 2001.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder Method of diagnosis: CIDI and ADIS‐IV N: 41 Age: M = 34 (SD = 7.5); range = 21 to 51 years Sex: 71% women Country of residence: Sweden Psychiatric co‐morbidity: included Co‐use of adjunct therapy: ongoing for > 6 months and not CBT (n = 1) Co‐use of medication: 64% (44% SSRIs, 10% benzodiazepines, 5% beta‐blockers, 5% tricyclic antidepressants) Method of enrolment: responded to media advertisements in community Baseline depression severity: (BDI‐II) ICBT M = 11.4 (SD = 3.7); WLC M = 13.1 (SD = 6.2) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email support (n = 21) Duration: 6 online modules completed over 7 to 12 weeks Treatment protocol*: participants completed online modules on psychoeducation, breathing retraining, cognitive restructuring, exposure, and relapse prevention, with email support from a therapist for module exercises Therapists: a clinical psychology graduate student Therapist contact: M reciprocal e‐mail contacts = 7.5 (SD = 1.2; range = 6 to 15); M total time spent by therapist per participant = 90 min Face‐to‐face contact: none Dropout: n = 4; 19% (2) Waiting list control (n = 20) Duration: 7 to 12 weeks Therapist, face‐to‐face contact: none Dropout: n = 1; 5% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) panic and agoraphobia symptoms: Body Sensations Questionnaire; Agoraphobic Cognitions Questionnaire; Mobility Inventory (2) general anxiety: Beck Anxiety Inventory Secondary outcomes: (1) quality of life: Quality of Life Inventory (2) treatment satisfaction (at post‐treatment): Evaluation of Self‐Help Program and Advisory Service |
|
| Notes | *treatment based on: Barlow, D.H., & Craske, M.G. (1994). Mastery of your anxiety and panic. San Antonio, TX: The Psychological Corporation. AND Zuercher‐White, E. (1998). An end to panic: Breakthrough techniques for overcoming panic disorder (2nd ed.). Oakland, CA: New Harbinger Publications. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were divided into two groups by the drawing of lots. These were drawn for the two treatment groupings pairwise for participants who had completed their baseline measurements. In other words, as soon as two participants had completed their baseline measurements, one was allocated to the treatment group and the other to the waiting‐list group." Comment: adequate randomization method |
| Allocation concealment (selection bias) | Low risk | Appears that lots were drawn immediately before assignment so allocation was likely concealed adequately |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (waiting list versus Internet‐based CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐reported and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "After randomizations, five people dropped out during the course of the study. There were four dropouts from the treatment group and one from the waiting‐list group, χ2(1) = 2.9, P < 0.05. In the treatment group, lack of time was given as the main reason for discontinuing (n = 3). One patient dropped out because of a newly discovered cancer. The person who left the waiting‐list group gave no reason."; "...intention‐to‐treat evaluation of the results." Comment: though there was a difference in the number of dropouts between the two treatment conditions, the number of dropouts was small and reasons did not relate directly to treatment components; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Carlbring 2005.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder (49%) or Panic Disorder with Agoraphobia (51%) Method of diagnosis: SCID‐IV N: 49 Age: M = 35 (SD = 7.7); range = 18 to 60 years Sex: 71% women Country of residence: Sweden Psychiatric co‐morbidity: 49% another Anxiety Disorder, 6% Major Depression Co‐use of adjunct therapy: ongoing for > 6 months and not CBT (4%) Co‐use of medication: 30.6% SSRIs, 8.2% benzodiazepines, 6.1% beta‐blockers, 6.1% tricyclic antidepressants Method of enrolment: responded to media advertisements in community Baseline depression severity: (BDI‐II) ICBT M = 11.8 (SD = 7.8); face‐to‐face CBT M = 15.9 (SD = 9.0); (MADRS‐S) ICBT M = 13.4 (SD = 5.3); face‐to‐face CBT M = 16.0 (SD = 4.3) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email support (n = 25) Duration: 10 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, breathing retraining, cognitive restructuring, exposure, and relapse prevention, with e‐mail support from a therapist for module exercises Therapists: 4 licensed clinical psychologists (research or clinical experience, or both, with anxiety disorders), 3 advanced graduate students with a master's degree in clinical psychology, 1 student in final semester of master's degree program; all supervised by a licensed CBT psychologist and supervisor Therapist contact: M reciprocal e‐mail contacts = 15.4 (SD = 5.5; range = 4‐31); M total time spent by therapist per participant = 150 min Face‐to‐face contact: none Dropout: n = 3; 12% (2) Face‐to‐face individual CBT (n = 24) Duration: 10 individual face‐to‐face sessions over 10 weeks Treatment protocol*: sessions focused on psychoeducation, breathing retraining, cognitive restructuring, exposure, and relapse prevention Therapists: 4 licensed clinical psychologists (research and/or clinical experience with anxiety disorders), 3 advanced graduate students with a master's degree in clinical psychology, 1 student in the final semester of their master's degree program; all supervised by a licensed CBT psychologist and supervisor Therapist, face‐to‐face contact: 10 x 45 to 60 min sessions Dropout: n = 3; 12.5% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 1 year follow‐up (1) panic and agoraphobia symptoms: Body Sensations Questionnaire; Agoraphobic Cognitions Questionnaire; Mobility Inventory (2) general anxiety: Beck Anxiety Inventory (3) clinically important improvement: SCID‐IV Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on: Barlow, D.H., & Craske, M.G. (1994). Mastery of your anxiety and panic. San Antonio, TX: The Psychological Corporation. AND Zuercher‐White, E. (1998). An end to panic: Breakthrough techniques for overcoming panic disorder (2nd ed.). Oakland, CA: New Harbinger Publications. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were divided into two groups...by a true random‐number‐service (http://www.random.org)." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (face‐to‐face CBT or Internet‐based CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "...a clinical re‐interview (SCID) was administered by an independent psychologist blind for treatment condition." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "After randomizations, six people dropped out during the course of the study. There were three dropouts from the LIVE therapy group and three from the IT group. Lack of time was given as the main reason for discontinuing. However, in accordance with the intention to treat paradigm...post‐treatment data were collected from all dropouts." Comment: a small and similar number of dropouts reported in the two treatment conditions; used ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Carlbring 2006.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder Method of Diagnosis: SCID‐IV N: 60 Age: M = 36.7 (SD = 10); range = 18 to 60 years Sex: 60% women Country of residence: Sweden Psychiatric co‐morbidity: included Co‐use of adjunct therapy: none Co‐use of medication: 54% Method of enrolment: responded to media advertisements in community Baseline depression severity: (BDI‐II) ICBT M = 17.7 (SD = 8.8); WLC CBT M = 15.4 (SD = 7.4); (MADR‐S) ICBT M = 16.4 (SD = 7.2); WLC CBT M = 15.1 (SD = 6.0) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail and phone support (n = 30) Duration: 10 online modules completed over 10 weeks Treatment protocol: participants completed online modules on psychoeducation, breathing retraining, cognitive restructuring, exposure, and relapse prevention, with email support from a therapist for module exercises Therapists: 1 licensed psychologist, 2 students in their final year of a clinical psychology master's program; all had regular supervision from an experienced CBT psychologist Therapist contact: M reciprocal contacts = 13.5 (SD = 4.4; range = 7‐29); M time spent by therapist per participant per week = 12 min; M length of weekly phone conversations = 11.8 min (range = 9.6 to 15.6) Face‐to‐face contact: none Dropout: n = 2; 6.7% (2) Waiting list control (n = 30) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 1; 3.3% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) panic and agoraphobia symptoms: Body Sensations Questionnaire; Agoraphobic Cognitions Questionnaire; Mobility Inventory (2) general anxiety: Beck Anxiety Inventory (3) clinically important improvement: SCID‐IV Secondary outcomes: (1) quality of life: Quality of Life Inventory (2) treatment satisfaction (at post‐treatment): participants reported if they were satisfied, very satisfied, or dissatisfied with treatment and gave their opinion on the pace of the program |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participants were divided into two groups, treatment or a waiting list, by a true random‐number service." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "...a reinterview administered by an independent psychologist who was blind to treatment condition." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "One participant dropped out during the study; shortage of time was said to be the main reason. However, in accordance with the intention‐to‐treat paradigm... posttreatment data were also collected from the participant who dropped out. Two participants in the treatment condition and one on the waiting list did not return their posttreatment questionnaires. Therefore, their pretreatment scores were carried forward to the posttreatment assessment point." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Carlbring 2007.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of Diagnosis: SCID‐IV N: 60 Age: for ICBT, M = 32.4 (SD = 9.1); for WLC, M = 32.9 (SD = 9.2); range = 18 to 60 years Sex: 64.9% women Country of residence: Sweden Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: included Method of enrolment: responded to media advertisements in community Baseline depression severity: (MADRS‐S) ICBT M = 13.4 (SD = 8.4); WLC CBT M = 13.5 (SD = 6.0) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail and phone support (n=30) Duration: 9 online modules completed over 9 weeks Treatment protocol*: participants completed online modules, with e‐mail support from a therapist for module exercises Therapists: 2 students completing their last semester of a clinical psychology master’s degree Therapist contact: M time spent by therapist per participant per week = 22 min; M length of weekly phone conversations = 10.5 min (SD = 3.6) Face‐to‐face contact: none Dropout: n = 2; 6.7% (2) Waiting list control (n = 30) Duration: 9 weeks Therapist, face‐to‐face contact: none Dropout: n = 2; 6.7% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) social phobia symptoms: Liebowitz Social Anxiety Scale – Self‐Report; Social Phobia Scale; Social Interaction Anxiety Scale; Social Phobia Screening Questionnaire (2) general anxiety: Beck Anxiety Inventory Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on: Furmark, T., Holmstrom, A., Sparthan, E., et al. (2006). Social Phobia – effective treatment with cognitive‐behavioural therapy (in Swedish). Liber. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...were divided into two groups (treatment or waiting‐list control) by an online true random‐number service independent of the investigators and therapists. This service is run by the Department of Computer Science at the University of Dublin and the numbers are generated using a purely random process (atmospheric disturbances in space)." Comment: adequate randomisation process |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Two participants, one in each condition, were excluded from the analysis since they started other treatment during the period. A total of 27 of the 29 people in the treatment group completed all nine modules within the intended 9‐week time frame. Lack of time was provided as the explanation for terminating treatment prematurely. One of them did not send in post‐treatment measures, which explains why intention‐to‐treat analysis was used. Finally, after randomisation but before answering the pre‐treatment questionnaires, one person in the waiting‐list chose to refrain from participating because of lack of computer access. Thus, data for 29 participants in the treatment group and 28 in the control group were eligible for analysis." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Carlbring 2011.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder (9%), Panic Disorder with Agoraphobia (22%), Social Phobia (39%), Generalized Anxiety Disorder (20%), Anxiety Disorder not otherwise specified (13%) Method of diagnosis: SCID‐IV N: 54 Age: M = 38.8 (SD = 10.7); range = 22 to 63 years Sex: 76% women Country of residence: Sweden Psychiatric co‐morbidity: 2% OCD, 2% PTSD, 20% MDD, 7% mild Depression, 15% Dysthymia Co‐use of adjunct therapy: excluded Co‐use of medication: 26% using an antidepressant or anxiolytic Method of enrolment: responded to study advertisements in community and online Baseline depression severity: (MADRS‐S) ICBT M = 20.41 (SD = 7.31); attention control M = 19.59 (SD = 7.43) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 27) Duration: 6 to 10 online modules completed over 10 weeks Treatment protocol*: participants completed online modules as prescribed by a therapist on topics related to their diagnosis, with e‐mail support from a therapist for module exercises Therapists: 8 clinical psychology master's students in last semester of training Therapist contact: M time spent by therapist per participant per week = 15 min Face‐to‐face contact: none Dropout: n = 2; 7.4% (2) Attention control (n = 27) Duration: 10 weeks Treatment protocol: participants made weekly posts in a confidential online support group based on a theme posted by a therapist Therapists: 8 clinical psychology master's students in last semester of training Therapist contact: therapist spent 1 hr per week monitoring forum Face‐to‐face contact: none Dropout: n = 0; 0% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) anxiety symptoms: Clinical Outcomes in Routine Evaluation – Outcome Measure (2) general anxiety: Beck Anxiety Inventory (3) clinically important improvement: Clinical Global Impression Scale Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on Internet‐based programs described in: Andersson, G., Carlbring, P., Holmström, A., Sparthan, E., Furmark, T., Nilsson‐Ihrfelt, E., et al. (2006). Internet‐based self‐help with therapist feedback and in vivo group exposure for social phobia: a randomised controlled trial. Journal of Consulting and Clinical Psychology, 74, 677‐686.; Carlbring, P., Westling, B. E., Ljungstrand, P., Ekselius, L, & Andersson, G. (2001). Treatment of panic disorder via the Internet: A randomised trial of a self‐help program. Behavior Therapy, 32, 751‐764.; AND Vernmark, K., Lenndin, J., Bjärehed, J., Carlsson, M., Karlsson, J., Öberg, J., et al. (2010). Internet administered guided self‐help versus individualized e‐mail therapy: a randomised trial of two versions of CBT for major depression. Behaviour Research and Therapy, 48, 368‐376. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participants were divided into two groups... by an online true random‐number service independent of the investigators and therapists." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based applied relaxation versus Internet‐based CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "...a clinical global impression of improvement (CGI‐I) was mapped on a 7‐point scale (CGI; Guy, 1976) after a telephone interview by a blind assessor who had no earlier contact with the participants and no knowledge of to which group they had been randomly allocated." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The response rate was... 96.3% (52/54) at post‐treatment."; "Since the missing data at post‐treatment was only in the treatment group, repeated ANOVAs with conservative imputation according to the last observation‐carried‐forward method in case of missing data was used in the analysis of the immediate results." Comment: a small and similar number of dropouts from both treatment conditions was reported (two from treatment, zero from comparator); used ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Furmark 2009a.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: SCID‐IV N: 120 Age: for Internet CBT, M = 35 (SD = 10.2); for bibliotherapy, M = 37.7 (SD = 10.3); for waiting list, M = 35.7 (SD = 10.9) Sex: 67.5% women Country of residence: Sweden Co‐use of adjunct therapy: excluded Co‐use of medication: 13.9% Method of enrolment: responded to study advertisements in community and online |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail support (n = 40) Duration: 9 online modules completed over 9 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, social skills, and relapse prevention, with e‐mail support from a therapist for module exercises, and posted on an online discussion forum Therapists: 6 licensed clinical psychologists, 7 clinical psychology students in final year of master's program; students had clinical supervision during the study Therapist contact: 15 min per week Face‐to‐face contact: none Dropout: n = 1; 2.5% (2) Bibliotherapy (n = 40) Duration: 9 sections of the manual completed over 9 weeks Treatment protocol*: participants received a self‐help manual in the mail and completed it independently Therapist, face‐to‐face contact: none Dropout: n = 1; 2.5% (3) Waiting list control (n = 40) Duration: 9 weeks, completed weekly assessment measure Therapist, face‐to‐face contact: none Dropout: n = 1; 2.5% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) social phobia symptoms: Liebowitz Social Anxiety Scale – Self‐Report; Social Phobia Scale; Social Interaction Anxiety Scale; Social Phobia Screening Questionnaire (2) general anxiety: Beck Anxiety Inventory Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on: Carlbring, P., Furmark, T., Steczkó, J., Ekselius, L., & Andersson, G. (2006). An open study of internet‐based bibliotherapy with minimal therapist contact via email for social phobia. Clinical Psychology, 10, 30‐38.; Andersson, G., Carlbring, P., Holmström, A., Sparthan, E., Furmark, T., Nilsson‐Ihrfelt, E., et al. (2006). Internet‐based self‐help with therapist feedback and in‐vivo group exposure for social phobia: A randomised controlled trial. Journal of Consulting and Clinical Psychology, 74, 677‐686.; Carlbring, P., Gunnarsdóttir, M., Hedensjö, L., Andersson, G., Ekselius, L., & Furmark, T. (2007). Treatment of social phobia: randomised trial of internet‐delivered cognitive–behavioural therapy with telephone support. British Journal of Psychiatry, 190, 123‐128.; AND Tillfors, M., Carlbring, P., Furmark, T., Lewenhaupt, S., Spak, M., Eriksson, A., et al. (2008). Treating university students with social phobia and public speaking fears: internet delivered self‐help with or without live group exposure sessions. Depression and Anxiety, 25, 708‐717. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was performed by an independent third party using an online true random‐number service." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus pure bibliotherapy versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | Quote: "...assessors were not masked with regard to the treatment assignment. However, all assessments were conducted online with standardised written instructions and automatic scoring, reducing the risk of reactivity or experimenter effects." Comment: all outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Two participants, one each from the pure bibliotherapy and waiting‐list groups, withdrew immediately after randomisation because of personal reasons and one additional participant (ICBT group) did not provide post‐treatment data."; "For all randomised participants, missing data were replaced by the last obtained score (pre‐ or post‐treatment), i.e., last observation carried forward."; "Ten participants (4.3%) withdrew from the study after the first (n=6) or second (n=4) treatment week, the main reasons being lack of time or motivation and personal problems unrelated to the treatment. In accordance with the intention‐to‐treat principle, all participants were asked to complete post‐treatment and follow‐up assessments, regardless of how many treatment modules they had completed." Comment: one participant from each of ICBT, waiting list, and bibliotherapy did not complete post‐treatment measures; reasons for dropout from treatment seem unrelated to treatment condition although are not provided based on treatment condition; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Furmark 2009b.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: SCID‐IV N: 115 Age: for internet CBT, M = 34.9 (SD = 8.4); for bibliotherapy, M = 32.5 (SD = 8.5); for bibliotherapy and discussion group, M = 35 (SD = 10.4); for internet applied relaxation, M = 36.4 (SD = 9.8) Sex: 67.8% women Country of residence: Sweden Co‐use of adjunct therapy: excluded Co‐use of medication: 6.7% Method of enrolment: responded to study advertisements in community and online |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail support (n 2 9) Duration: 9 online modules completed over 9 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, social skills, and relapse prevention, with e‐mail support from a therapist for module exercises, and posted on an online discussion forum Therapists: 6 licensed clinical psychologists, 7 clinical psychology students in final year of master's program; students had clinical supervision during the study Therapist contact: 15 min per week Face‐to‐face contact: none Dropout: n = 0; 0% (2) Bibliotherapy (n = 29) Duration: 9 sections of the manual completed over 9 weeks Treatment protocol*: participants received a self‐help manual in the mail and completed it independently Therapist, face‐to‐face contact: none Dropout: n = 0; 0% (3) Bibliotherapy and discussion group (n=28) Duration: 9 sections of the manual completed over 9 weeks Treatment protocol*: participants received a self‐help manual in the mail and completed it independently as well as posting weekly on an online discussion forum Therapist, face‐to‐face contact: none Dropout: n = 0; 0% (4) Internet‐based applied relaxation (n = 29) Duration: 9 online modules completed over 9 weeks Treatment protocol^: participants completed online modules on psychoeducation, relaxation, and relapse prevention, with e‐mail support from a therapist for module exercises, and posted weekly on an online discussion forum Therapists: a licensed clinical psychologist, clinical psychology graduate students Therapist contact: 15 min per week Face‐to‐face contact: none Dropout: n = 0; 0% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) social phobia symptoms: Liebowitz Social Anxiety Scale – Self‐Report; Social Phobia Scale; Social Interaction Anxiety Scale; Social Phobia Screening Questionnaire (2) general anxiety: Beck Anxiety Inventory Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on: Carlbring, P., Furmark, T., Steczkó, J., Ekselius, L., & Andersson, G. (2006). An open study of internet‐based bibliotherapy with minimal therapist contact via email for social phobia. Clinical Psychology, 10, 30‐38.; Andersson, G., Carlbring, P., Holmström, A., Sparthan, E., Furmark, T., Nilsson‐Ihrfelt, E., et al. (2006). Internet‐based self‐help with therapist feedback and in‐vivo group exposure for social phobia: A randomised controlled trial. Journal of Consulting and Clinical Psychology, 74, 677‐686.; Carlbring, P., Gunnarsdóttir, M., Hedensjö, L., Andersson, G., Ekselius, L., & Furmark, T. (2007). Treatment of social phobia: randomised trial of internet‐delivered cognitive–behavioural therapy with telephone support. British Journal of Psychiatry, 190, 123‐128.; AND Tillfors, M., Carlbring, P., Furmark, T., Lewenhaupt, S., Spak, M., Eriksson, A., et al. (2008). Treating university students with social phobia and public speaking fears: internet delivered self‐help with or without live group exposure sessions. Depression and Anxiety, 25, 708‐717. ^treatment based on: Ӧst, L.G. (1997). Tillӓmpad avslappning [applied relaxation]. Stockholm, Sweden: Repro HSC. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was performed by an independent third party using an online true random‐number service." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (ICBT versus pure bibliotherapy versus waiting list versus applied relaxation) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | Quote: "...assessors were not masked with regard to the treatment assignment. However, all assessments were conducted online with standardised written instructions and automatic scoring, reducing the risk of reactivity or experimenter effects." Comment: all outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Two participants, one each from the pure bibliotherapy and waiting‐list groups, withdrew immediately after randomisation because of personal reasons and one additional participant (ICBT group) did not provide post‐treatment data."; "For all randomised participants, missing data were replaced by the last obtained score (pre‐ or post‐treatment), i.e., last observation carried forward."; "In accordance with the intention‐to‐treat principle, all participants were asked to complete post‐treatment and follow‐up assessments, regardless of how many treatment modules they had completed." Comment: there was a very small and similar number of participants from each treatment condition who did not complete post‐treatment measures; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Greist 2012.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Obsessive Compulsive Disorder Method of diagnosis: SCID‐IV N: 87 Age: M = 38.34 (SD = 13.93) Sex: 63% women Country of residence: USA Psychiatric co‐morbidity: 32% Anxiety Disorder, 31% Mood Disorder, 7% Substance Use Disorder, 7% Attention Deficit Hyperactivity Disorder, 2% Eating Disorder Co‐use of adjunct therapy: 23% Co‐use of medication: 33.3% Method of enrolment: newspaper advertisements and clinic referrals Baseline depression severity: not assessed |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with clinician phone support (n = 31) Duration: 9 online modules completed over 12 weeks Treatment protocol*: participants completed online modules on psychoeducation, exposure and response prevention, identifying triggers, goal setting, peer support, and troubleshooting, with phone support from a therapist Therapist: 2 CBT therapists Therapist contact: regularly scheduled weekly phone calls Face‐to‐face contact: none Dropout: not reported (2) Internet‐based CBT with lay phone support (n = 28) Duration: 9 online modules completed over 12 weeks Treatment protocol*: participants completed online modules on psychoeducation, exposure and response prevention, identifying triggers, goal setting, peer support, and troubleshooting, with phone support from a lay coach Therapist: 1 lay coach Therapist contact: regularly scheduled weekly phone calls Face‐to‐face contact: none Dropout: not reported (3) Unguided Internet‐based CBT (n = 28) Duration: 9 online modules completed over 12 weeks Treatment protocol*: participants completed online modules on psychoeducation, exposure and response prevention, identifying triggers, goal setting, peer support, and troubleshooting Therapist/Face‐to‐face contact: none Dropout: not reported |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment Primary outcome: (1) OCD symptoms: YBOCS Secondary outcomes: (1) quality of life: Work and Social Adjustment Scale (2) treatment satisfaction: System Usability Scale, User Satisfaction Scale |
|
| Notes | *“BT Steps” program | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomized using a computer‐generated randomization schedule." Comment: Adequate randomization method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (guided internet‐based treatment or live treatment) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts were not reported; data analytic details not reported |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Unclear risk | Group comparisons at baseline not reported |
Hedman 2011.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of d: SCID‐IV and MINI N: 126 Age: for ICBT, M = 35.2 (SD = 11.1); for face‐to‐face CBT, M = 35.5 (SD = 11.6); range = 18 to 64 years Sex: 38% women Country of residence: Sweden Psychiatric co‐morbidity: 18% another Anxiety Disorder, 15% MDD Co‐use of adjunct therapy: excluded Co‐use of medication: 19.8% SSRIs, 4.8% SNRIs Method of enrolment: referred to study by health professionals or self‐referred to study clinic Baseline depression severity: (MADRS‐S) ICBT M = 12.7 (SD = 6.5); face‐to‐face CBT M = 14.0 (SD = 8.0) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 64) Duration: 15 online modules completed over 15 weeks Treatment protocol*: participants completed online modules on social phobia treatment themes such as exposure and cognitive restructuring, with email support from a therapist for module activities Therapists: 8 clinical psychologists (1 to 4 years experience with Internet CBT) Therapist contact: M emails by therapists = 17.4; M time spent by therapist per participant per week = 5.5 min (SD = 3.6) Face‐to‐face contact: none Dropout: n = 1; 1.6% (2) Face‐to‐face group CBT (n = 62) Duration: 15 face‐to‐face group sessions over 15 weeks Treatment protocol^: participants attended face‐to‐face group therapy sessions on social phobia treatment themes including cognitive restructuring and exposure Therapists: 6 clinical psychologists (2‐15 years experience with CBT for social phobia); supervised by a licensed psychotherapist experienced in CBT for social phobia Therapist, face‐to‐face contact: 15 x 2.5 hr group therapy sessions Dropout: n = 0; 0% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 6 month follow‐up Primary outcomes: (1) social phobia symptoms: Liebowitz Social Anxiety Scale – Clinician; Social Phobia Scale; Social Interaction Anxiety Scale; Anxiety Sensitivity Index (2) general anxiety: Beck Anxiety Inventory (3) clinically important improvement: SCID‐IV Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on: Andersson, G., Carlbring, P., Holmström, A., Sparthan, E., Furmark, T., Nilsson‐Ihrfelt, E., et al. (2006). Internet‐based self‐help with therapist feedback and in‐vivo group exposure for social phobia: A randomised controlled trial. Journal of Consulting and Clinical Psychology, 74, 677‐686.; Carlbring, P., Gunnarsdóttir, M., Hedensjö, L., Andersson, G., Ekselius, L., & Furmark, T. (2007). Treatment of social phobia: randomised trial of internet‐delivered cognitive–behavioural therapy with telephone support. British Journal of Psychiatry, 190, 123‐128.; AND Tillfors, M., Carlbring, P., Furmark, T., Lewenhaupt, S., Spak, M., Eriksson, A., et al. (2008). Treating university students with social phobia and public speaking fears: internet delivered self‐help with or without live group exposure sessions. Depression and Anxiety, 25, 708‐717. ^treatment based on: Heimberg, R.G., & Becker, R.E. (2002). Cognitive‐behavioral group therapy for social phobia. Basic mechanisms and clinical strategies. New York: Guilford Press. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A true random number service (http://www.random.org) was used to ensure randomizations... Participants were allocated to CBGT or ICBT in a 1:1 ratio using simple randomizations with no restrictions or matching." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomizations procedure involved two external persons not involved in the study; one provided randomizations data and the other monitored that no manipulation of treatment allocation was performed by the research group."; "The random sequence was generated after inclusion of participants to ensure that assignment of intervention was concealed from assessing psychiatrists and researchers of the study." Comment: adequate allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (internet‐based CBT versus face‐to‐face CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "To ensure the integrity of the blinding procedure, participants were instructed not to mention which treatment they had received during the post‐treatment and follow‐up interviews. After completing the interviews, the assessing psychiatrists guessed allocation status for each participant."; "In four instances blinding was broken. On two occasions participants accidentally mentioned their treatment allocation status to the assessor, and in another two occasions it was deemed necessary to break the blinding because of the need to assess increased depressive symptoms during treatment... There was no significant association between assessors' guess and actual treatment allocation (χ2 = 0.27, df = 1, p = .61), indicating successful blinding." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | A similar number of dropouts from both treatment conditions was reported (13 for ICBT; 12 for CBGT); ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | It is unclear if several outcomes in the trial registration (described as WQ, TIC‐P, SSP) were reported in the manuscript; all other outcome measures outlined in the trial registration were reported in the manuscript |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Ivarsson 2014.
| Methods | Randomized controlled trial | |
| Participants |
Diagnosis: DSM‐IV Posttraumatic Stress Disorder Method of diagnosis: CAPS N: 62 Age: M = 46 (SD = 11.7); range = 21 to 67 years Sex: 82.3% women Country of residence: Sweden Psychiatric co‐morbidity: not reported Co‐use of adjunct therapy: excluded Co‐use of medication: included Method of enrolment: advertisements in national and local newspapers Baseline depression severity: (BDI‐II) ICBT M = 26.61 (SD = 11.42); Attention Control M = 26.35 (SD = 10.88) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email support (n = 31) Duration: 8 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, anxiety coping skill training, exposure, and cognitive restructuring, with email support from a therapist Therapist: clinical psychology students Therapist contact: M time spent by therapist per participant per week = 28 min (SD = 19.8; range = 11 to 52) Face‐to‐face contact: none Dropout: n = 3; 9.7% (2) Attention/Waiting list control (n = 31) Duration: 8 weeks Treatment protocol*: sent questions on wellbeing to respond to weekly Therapist/Face‐to‐face contact: none Dropout: n = 5; 16.1% |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment Primary outcomes: (1) posttraumatic stress symptoms: Impact of Events Scale – Revised, Post‐traumatic Stress Diagnostic Scale (2) general anxiety: Beck Anxiety Inventory (3) clinically important improvement: Clinician‐administered PTSD Scale Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on Bisson, J. I., Ehlers, A., Matthews, R., Pilling, S., Richards, D., & Turner, S. (2007). Psychological treatments for chronic post‐traumatic stress disorder: Systematic review and meta‐analysis. British Journal of Psychiatry, 190, 97‐104.; Harvey, A. G., Bryant, R. A., & Tarrier, N. (2003). Cognitive behaviour therapy for posttraumatic stress disorder. Clinical Psychology Review, 23, 501‐522. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomization was conducted by an individual who was not otherwise involved in the research project, using an online true random‐number service (www.random.org)." Comment: Adequate randomization method |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (guided internet‐based treatment or attention control) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | Unclear risk | for self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Unclear risk | Quote: "The post‐treatment interviewers were blind to participant status (i.e. treatment or control)." Comment: Assessment interviewers were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "The total response rate on self‐report measures was 87% (n=54) at post‐treatment. In addition, one participant had one of the self‐report measures missing at post‐treatment assessment. The proportions of missing data did not significantly differ between conditions at post‐treatment."; "...we relied on full information maximum likelihood estimation, which provides unbiased estimates under standard data missing assumptions of ignorable missing..." Comment: Dropouts reported and were similar across conditions; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Unclear risk | Quote: "The groups did not differ significantly with regard to the demographic, diagnostic, or trauma characteristics at baseline." Comment: No baseline group differences |
Johnston 2011.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with or without agoraphobia (20.6%), Social Phobia (34.4%), generalized anxiety disorder (45%) Method of diagnosis: MINI N: 139 Age: M = 41.62 (SD = 12.83); range = 19 to 79 years Sex: 58.8% women Country of residence: Australia Psychiatric co‐morbidity: 29% another Anxiety Disorder only, 9.2% another Affective Disorder only, 32.1% another Anxiety and Affective disorder Co‐use of adjunct therapy: excluded Co‐use of medication: 29% Method of enrolment: responded to online study advertisements Baseline depression severity: (PHQ‐9) ICBT with clinician M = 11.63 (SD = 5.96); WLC M = 11.71 (SD = 6.31) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail and phone support from a clinician (n = 47) Duration: 8 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on disorder‐specific psychoeducation, cognitive restructuring, core beliefs, exposure, assertiveness communication and interpersonal boundaries, and relapse prevention, with email and phone support from a therapist for module activities Therapists: 1 clinical psychologist with specialist post‐graduate training in clinical psychology and 2.5 years postgraduate experience Therapist contact: M emails by therapist = 8.83 (SD = 3.19); M phone calls by therapist = 7.54 (SD = 2.43); M time spent by therapist per participant overall = 69.09 min (SD = 32.29) Face‐to‐face contact: none Dropout: n = 5; 10.6% (2) Internet‐based CBT with e‐mail and phone support from a coach (n = 46) Duration: 8 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on disorder‐specific psychoeducation, cognitive restructuring, core beliefs, exposure, assertiveness communication and interpersonal boundaries, and relapse prevention, with email and phone support from a coach for module activities (no clinical support) Therapists: 1 clinical psychologist with specialist post‐graduate training in clinical psychology and 2.5 years postgraduate experience Therapist contact: M e‐mails by coach = 8.88 (SD = 4.38); M phone calls by coach = 7.56 (SD = 1.19); M time spent by coach per participant overall = 69.09 min (SD = 30.75) Face‐to‐face contact: none Dropout: n = 4; 8.7% (2) Waiting list control (n = 46) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 5; 10.9% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcomes: (1) disorder‐specific symptoms: Penn State Worry Questionnaire; Social Phobia Scale/Social Interaction Anxiety Scale – Short Form; Panic Disorder Severity Scale – Self‐Rating (2) general anxiety symptoms: GAD‐7, Depression Anxiety Stress Scales – 21 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: A 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *treatment based on: Titov , N., Andrews, G., Johnston, L., Robinson, E., Spence, J. (2010). Transdiagnostic Internet treatment for anxiety disorders: A randomised controlled trial. Behaviour Research and Therapy, 48, 890‐9. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...were randomised via a true randomizations process (www.random.org), generated by an independent person, to either..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation sequence preceded pre‐treatment diagnostic interviews and was concealed from LJ and JS [pre‐treatment interviewers]." Comment: unclear how allocation concealment occurred but it seems to have taken place |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list control) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcomes were self‐report outcome measures, participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All post‐treatment and 3‐month follow‐up analyses involved an intention‐to‐treat (ITT) design and missing data was addressed by carrying forward the first available data (baseline‐observation‐carried‐forward; BOCF)." Comment: ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | One measure that appears in the trial protocol (Agoraphobic Cognitions Questionnaire) is not reported; all other outcomes in the trial registration are reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Kiropoulos 2008.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder (41.9%) or Panic Disorder with Agoraphobia (58.1%) Method of diagnosis: ADIS‐IV N: 86 Age: M = 38.96 (SD = 11.13); range = 20 to 64 years Sex: 72.1% women Country of residence: Australia Psychiatric co‐morbidity: 16% Social Phobia, 17% GAD, 10% Specific Phobia, 3% PTSD, 10% MDD, 5% Dysthymia, 1% Alcohol Abuse, 8% Hypochondriasis Co‐use of adjunct therapy: excluded Co‐use of medication: 47.7% Method of enrolment: responded to media advertisements in community and online Baseline depression severity: (DASS depression, log transformed) ICBT M = 2.72 (SD = 1.80); face‐to‐face CBT M = 2.98 (SD = 1.61) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 46) Duration: 6 online modules (+ 2 optional modules) completed over 6 weeks Treatment protocol*: participants completed online modules on deep breathing, cognitive restructuring, and exposure, with e‐mail support from a therapist for module activities (optional modules on stress and benzodiazepines) Therapists: 9 registered and 1 probationary psychologist; all trained in CBT Therapist contact: M e‐mails by therapist = 18.24 (SD = 9.82); M e‐mails by participant = 10.64 (SD = 8.21); M time spent by therapist per participant = 352 min (SD = 240) Face‐to‐face contact: none Dropout: n = 5; 10.9% (2) Face‐to‐face individual CBT (n = 40) Duration: 12 face‐to‐face group sessions over 12 weeks Treatment protocol^: participants attended face‐to‐face group therapy sessions on social phobia treatment themes including cognitive restructuring and exposure Therapists: registered psychologists Therapist, face‐to‐face contact: 12 x 60 to 90 min sessions; M = 568 min (SD = 255.12) Dropout: n = 2; 5% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) panic and agoraphobia symptoms: Panic Disorder Severity Scale; Body Vigilance Scale; Agoraphobic Cognitions Questionnaire; Anxiety Sensitivity Profile (2) general anxiety: DASS Stress and Anxiety subscales (3) clinically important improvement: ADIS‐IV Secondary outcomes: (1) quality of life: WHO Quality of Life – BREF subscales (2) treatment satisfaction (at post‐treatment): Treatment Satisfaction Questionnaire ‐ Modified |
|
| Notes | *on‐line treatment program: Panic Online ^treatment based on: Barlow, D.H., & Craske, M.G. (2000). Mastery of your anxiety and panic: MAP‐3. New York: Graywind Publications. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...they were randomly allocated using a random numbers table..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus face‐to‐face CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "All assessors were blind to treatment allocation of eligible participants into the study." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The attrition rates were 10.9% (5/46) and 5% (2/40) for the PO and face‐to‐face treatment conditions, respectively. A Fisher's exact test revealed no difference in attrition rates between the two treatment conditions, χ2 (1, N = 86) = .44, P > .05. Reasons for non‐completion of either treatment included participants not being contactable, changing their mind about taking part in the study, because they could no longer commit to the 12‐week treatment program or because they no longer had access to the Internet."; "Data analysis involved intention‐to‐treat analyses." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Kok 2012.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with Agoraphobia (41%), Agoraphobia (17%), Social Phobia (53.3%), and Specific Phobia (83.5%) Method of diagnosis: CIDI N: 212 Age: M = 34.6 (SD = 11.7) Sex: 61% women Country of residence: Netherlands Psychiatric co‐morbidity: included, but not reported Co‐use of adjunct therapy: not reported Co‐use of medication: 43% Method of enrolment: referred by general practitioners Baseline depression severity: (CES‐D) ICBT M = 24.99 (SD = 8.58); Waiting List M = 24.75 (SD = 8.39) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based BT with email support (n = 105) Duration: 8 online modules completed over 5 weeks Treatment protocol*: participants completed online modules on psychoeducation and exposure, with email support from a therapist Therapist: 1 psychotherapist Therapist contact: weekly by email; amount not reported Face‐to‐face contact: non‐therapeutic session to assess treatment needs Dropout: n = 49; 46.7% (2) Waiting list control (n = 107) Duration: 5 weeks Treatment protocol*: sent a self‐help book on exposure therapy but no instructions or support provided Therapist contact: none Face‐to‐face contact: non‐therapeutic session to assess treatment needs Dropout: n = 35; 32.7% |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment Primary outcomes: (1) phobia symptoms: Fear Questionnaire (2) general anxiety: Beck Anxiety Inventory Secondary outcome: (1) treatment satisfaction: Client Satisfaction Questionnaire |
|
| Notes | *Adapted from De Neef, M., & Cuijpers, P. (2007). Fobieen. Amsterdam: Boom Uitgeverij. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated randomization table was prepared by a researcher not involved in the data collection. Randomization was stratified at a clinic level and performed at a 1:1 ratio. To ensure approximately equal randomization ratios per clinic, blocks of 8 were used." Comment: Adequate randomization method |
| Allocation concealment (selection bias) | Low risk | Quote: "An external researcher not involved in the project supervised a list of sequentially numbered allocations and assigned participants to the conditions. All project members involved in data collection were unaware of allocation status until randomization was definitive." Comment: Adequate method of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Due to the nature of this trial, neither participants nor researchers could be blinded to treatment allocation." Comment: Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (guided internet‐based treatment or live treatment) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Thirdly, although we corrected for missing values at follow‐up by using multiple imputation, the results should be interpreted with caution due to the large amount of missing data." Comment: Dropout rates were almost as high as 40% and definite differences were noted in symptom severity (BAI, CES‐D) between completers and dropouts; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | Results for all outcome measures reported in the published study protocol were reported in the manuscript, with the exception of results for the EuroQol and the CAGE questionnaire, the latter of which is not relevant to the present review |
| Other bias | Unclear risk | Baseline differences only in psychotropic medication use between conditions were noted |
Newby 2013.
| Methods | Randomized controlled trial | |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of diagnosis: MINI N: 100 (84 with clinical Generalized Anxiety Disorder included in review) Age: M = 44.3 (SD = 12.2) Country of residence: Australia Psychiatric co‐morbidity: 56% of clinical Generalized Anxiety Disorder sample had comorbid Major Depressive Disorder Co‐use of adjunct therapy: 6.1% Co‐use of medication: 40.4% Method of enrolment: responded to online study advertisement Baseline depression severity: (PHQ‐9) ICBT M = 10.39 (SD = 3.9); Waiting List M = 11.62 (SD = 4.8) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with phone and email support (n = 46) Duration: 6 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on CBT techniques (e.g., activity scheduling, graded exposure), with email and phone support from a therapist Therapist: 1 practice manager, 1 clinical psychologist Therapist contact: M time spent by therapist per participant overall = 23.37 mins (SD = 12.15; range = 7 to 60) Face‐to‐face contact: none Dropout: n = 3; 6.5% (2) Waiting list control (n = 54) Duration: 10 weeks Therapist/Face‐to‐face contact: none Dropout: n = 6; 11.1% |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment Primary outcome: (1) generalized anxiety symptoms: GAD‐7, PSWQ Secondary outcomes: (1) quality of life: WHO Disability Assessment Schedule – II (1) treatment satisfaction: participants rated how logical the program was, their confidence that the program was successful at teaching them techniques for managing symptoms, and their confidence in recommending the program to a friend with similar concerns |
|
| Notes | *“Worry and Sadness Program” delivered via https://www.virtualclinical.org.au | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random numbers were generated using a random number service (http://random.org)." Comment: Adequate randomization method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Concealment of allocation was maintained until the applicant met all inclusion criteria and an offer of participation was made." Comment: No mention of method of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment, nor therapists to the treatment they delivered (guided internet‐based treatment or live treatment) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "The non‐blinded structured interviews at 3‐month follow‐up…" Comment: Assessors were not blinded at follow‐up, however the assessments in question were not included in this review so ROB was not downgraded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Intent‐to‐treat (ITT) marginal model analyses using the restricted maximum likelihood method were used to account for missing data due to participant dropouts." Comment: Dropouts reported were small and similar across conditions (3 in the treatment group and 1 in the control condition between pre‐ to post‐treatment); ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Only one outcome (not relevant to the present review) indicated in the trial registration was not reported in the trial manuscript, all other outcomes in the trial registration were reported in the manuscript |
| Other bias | High risk | Quote: "There were no differences between the groups on age, pre‐treatment BDI‐II, GAD‐7, NEO‐FFI‐N, PHQ‐9, K‐10, or PSWQ scores (p's < 0.05). However, the control group reported significantly higher disability on the WHODAS‐II (t97 = 2.35, p = 0.02)." Comment: Difference in baseline severity of disability between groups at pre‐treatment |
Nordgren 2012.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with or without Agoraphobia (31%), Agoraphobia (8%), Social Phobia (32%), Generalized Anxiety Disorder (10%), Anxiety Disorder Not Otherwise Specified (19%) Method of diagnosis: SCID‐IV N: 100 Age: for Internet CBT, M = 35 (SD = 13); for waiting list, M = 36 (SD = 12); range = 19 to 68 years Sex: 63% women Country of residence: Sweden Psychiatric co‐morbidity: 31% Anxiety Disorder, 43% Mood Disorder, 1% Hypochondriasis Co‐use of adjunct therapy: excluded Co‐use of medication: 26% Method of enrolment: referred by primary care physician Baseline depression severity: (MADRS‐S) ICBT M = 19.62 (SD = 0.96); Waiting List M = 17.84 (SD = 0.96) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email support (n = 50) Duration: 7 to 10 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on cognitive restructuring, social anxiety, generalized anxiety, panic, agoraphobia, behavioural activation, relaxation, mindfulness, assertive problem solving, stress management, and stress, with email support from a therapist, as selected and tailored by a therapist Therapist: 7 clinical psychology master’s students Therapist contact: 15 mins/week Face‐to‐face contact: none Dropout: n = 4; 8% (2) Waiting list control (n = 50) Duration: 10 weeks Therapist/Face‐to‐face contact: none Dropout: n = 5; 10% |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment Primary outcomes: (1) anxiety symptoms: Clinical Outcomes in Routine Evaluation – Outcome Measure (2) general anxiety: Beck Anxiety Inventory Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *adapted from: Andersson, G., Carlbring, P., Holmstrom, A., Sparthan, E., Furmark, T., Nilsson‐Ihrfelt, E., … Ekselius, L. (2006). Internet‐based self‐help with therapist feedback and in vivo group exposure for social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 74, 677‐686.; Carlbring, P., Bohman, S., Brunt, S., Buhrman, M., Westling, B. E., Ekselius, L., & Andersson, G.(2006). Remote treatment of panic disorder: A randomized trial of internet‐based cognitive behavior therapy supplemented with telephone calls. American Journal of Psychiatry, 163, 2119‐2125.; Paxling, B., Almlov, J., Dahlin, M., Carlbring, P., Breitholtz, E., Eriksson, T., & Andersson, G. (2011). Guided internet‐delivered cognitive behavior therapy for generalized anxiety disorder: A randomized controlled trial. Cognitive Behaviour Therapy, 40, 159‐173.; Vernmark, K., Lenndin, J., Bjarehed, J., Carlsson, M., Oberg, J., … Andersson, G. (2010). Internet administered guided self‐help versus individualized e‐mail therapy: A randomized trial of two versions of CBT for major depression. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "…randomly assigned by an online true random‐number service independent of the investigators and therapists to either immediate treatment or control." Comment: Adequate randomization method |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition, nor therapists to the treatment they delivered (guided internet‐based treatment or waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "In the treatment group three persons dropped out, and two were excluded, leaving 45 participants remaining in the treatment group at the end of the ten‐week treatment period. In the control group, eight persons withdrew their application before starting the treatment."; "...we used intention‐to‐treat analysis. This method accounts for missing data without assuming that the last measurement was stable..." Comment: Dropouts reported and were small and similar across conditions; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial protocol were reported |
| Other bias | Unclear risk | Authors did not comment on baseline group differences/similarities |
Paxling 2011.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of diagnosis: SCID‐IV N: 89 Age: M = 39.3 (SD = 10.8); range = 18 to 66 Sex: 79.8% women Country of residence: Sweden Psychiatric co‐morbidity: included; 22.5% MDD Co‐use of adjunct therapy: excluded Co‐use of medication: 37.1% Method of enrolment: responded to media advertisements in the community and online Baseline depression severity: (BDI‐II) ICBT M = 17.66 (SD = 9.81); WLC M = 16.93 (SD = 7.91) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail support (n = 44) Duration: 8 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, applied relaxation, worry time, cognitive restructuring, problem solving, sleep management, exposure, and relapse prevention with email support from a therapist for module activities Therapists: psychologists in their final year of training; all trained for 1 week in CBT protocol; supervision provided by experienced clinician Therapist contact: M time spent by therapist per participant = 97 min (SD = 52) Face‐to‐face contact: none Dropout: n = 6; 13.6% (2) Waiting list control (n = 45) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout: n = 1; 2.2% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) generalized anxiety symptoms: Penn State Worry Questionnaire, Generalized Anxiety Disorder Questionnaire – IV (2) general anxiety symptoms: State Trait Anxiety Inventory, Beck Anxiety Inventory Secondary outcomes: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on parts of: Ost, L.G. (1987) Applied relaxation: Description of a coping technique and review of controlled studies. Behaviour Research and Therapy, 25, 379‐409.; Borkovec, T.D., & Costello, E. (1993). Efficacy of applied relaxation and cognitive‐behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology, 61, 611‐9.; Borkovec, T.D., Wilkinson, L., Folensbee, R., & Lerman, C. (1983). Stimulus control applications to treatment of worry. Behaviour Research and Therapy, 21, 247‐51.; Borkovec, T.D., & Sharpless, B. (2004). Generalized anxiety disorder: Bringing cognitive‐behavioral therapy into the valued present. In S. C. Hayes, V.M. Follette, & M.M. Linehan (Eds.), Mindfulness and acceptance (pp. 209‐42). New York, NY: Guilford Press.; Zetterqvist, K., Maanmies, J., Strom, L., & Andersson, G. (2003). Randomized controlled trial of Internet‐based stress management. Cognitive Behaviour Therapy, 3, 151‐60.; Sanderson, W. C., & Rygh, J.L. (2004). Treating generalized anxiety disorder: Evidence‐based strategies, tools, and techniques. New York, NY: Guilford Press.; Strom, L., Pettersson, R., & Andersson, G. (2004). Internet‐based treatment for insomnia: A controlled evaluation. Journal of Consulting and Clinical Psychology, 72, 113‐20.. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 89 participants were randomised...by an independent person not involved in the study. A computer‐generated random list was obtained via www.random.org, which utilizes atmospheric noise to create random sequences of numbers." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list control) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "The interviewers were blinded concerning participant status (e.g. treatment or control) since the posttreatment interviewers did not have access to information about the participants and started each interview by asking the participants not to say whether they were in the treatment or control condition." Comment: interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Posttreatment measures were obtained from 38 or 44 randomised participants in the treatment group (86%) and 44 of 45 in the control group (98%)."; "In order to account for dropouts without assuming that the first measurement was stable (i.e., the last observation carried forward assumption), we used a mixed‐effects models approach...Mixed‐effect models are able to accommodate missing data and integrate time‐varying factors." Comment: very little data was incomplete; an ITT approach was used |
| Selective reporting (reporting bias) | Low risk | Results were reported for all outcome measures outlined in the trial registration |
| Other bias | Unclear risk | Group comparisons at baseline not reported |
Richards 2006.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder (21.9%) or Panic Disorder with Agoraphobia (78.1%) Method of diagnosis: ADIS‐IV N: 23 Age: M = 36.59 (SD = 9.9); range = 18 to 70 Sex: 68.8% women Country of residence: Australia Psychiatric co‐morbidity: 22% Social Phobia, 13% GAD, 9% Specific Phobia, 6% PTSD, 9% MDD, 6% Hypochondriasis, 3% Somatization Disorder Co‐use of adjunct therapy: excluded Co‐use of medication: 15.6% antidepressants, 12.5% benzodiazepines, 9.4% both antidepressants and benzodiazepines Method of enrolment: responded to online study advertisements Baseline depression severity: (DASS depression) ICBT M = 21.25 (SD = 12.3); control M = 6.79 (SD = 6.4) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail support (n = 12) Duration: 6 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on relaxation strategies, cognitive restructuring, and exposure, with e‐mail support from a therapist for module activities Therapists: 1 clinical psychologist, 3 doctoral clinical psychology students; all experienced in CBT Therapist contact: M emails by therapist = 18 (SD = 6.5); M e‐mails by participant = 15.3 (SD = 12.8); M time spent by therapist per participant = 376.30 min (SD = 156.8) Face‐to‐face contact: none Dropout: n = 2; 16.7% (2) Internet‐based CBT and stress management with email support (n = 11) Duration: 12 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on relaxation strategies, cognitive restructuring, and exposure, as well as several stress management modules, with email support from a therapist for module activities Therapists: 1 clinical psychologist, 3 doctoral clinical psychology students; all experienced in CBT Therapist contact: M e‐mails by therapist = 12.9 (SD = 3.8); M e‐mails by participant = 11.6 (SD = 13.3); M time spent by therapist per participant = 309.30 min (SD = 111.3) Face‐to‐face contact: none Dropout: n = 1; 9% (3) Internet‐based information control (n = 9) Duration: 8 weeks Treatment protocol: participants read online non‐CBT panic resources and provided weekly status reports to a therapist via e‐mail Therapists: 1 doctoral clinical psychology student Therapist contact: limited to weekly status update e‐mails Face‐to‐face contact: none Dropout: n = 2; 22.2% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcomes: (1) panic and agoraphobia symptoms: Panic Disorder Severity Scale; Body Vigilance Scale; Agoraphobic Cognitions Questionnaire; Anxiety Sensitivity Profile (2) general anxiety: DASS Stress and Anxiety subscales (3) clinically important improvement: ADIS‐IV Secondary outcome: (1) quality of life: WHO Quality of Life subscales |
|
| Notes | *on‐line treatment program: Panic Online | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | ABC block randomisation was used (information provided by authors via personal correspondence); unclear if sequential design or a more rigorous randomisation method was used |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based without stress management versus Internet‐based with stress management versus Internet‐based information control) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | High risk | Quote: "The two assessors were the second author of the present study and a probationary registered psychologist/PhD candidate. The second author was not blind to treatment allocation, although the other assessor was... To evaluate reliability of assessment, a third assessor (the 3rd author), who was blind to the treatment allocation, reviewed 15% of the clinical interviews..."; "The two clinicians who conducted the assessments did not provide any treatment." Comment: not all interviewers were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The attrition rate for PO1 was 16.7% (2/12), 9% (1/11) in PO2 and 22% (2/9) in IC. Reasons given for discontinuing treatment in the PO1 condition were a lack of motivation or an episode of major depression. The PO2 person discontinued because of a wish to commence selective serotonin reuptake inhibitor medication halfway through the study. Of the two IC participants, no reason for discontinuing was given."; "Data analysis involved intention‐to‐treat analyses." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | High risk | At baseline, treatment groups scored significantly higher on the DASS depression subscale than control participants |
Robinson 2010.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of diagnosis: MINI N: 101 Age: M = 46.96 (SD = 12.70); range = 18 to 80 Sex: 68.3% women Country of residence: Australia Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: included Method of enrolment: responded to online study advertisements Baseline depression severity: (PHQ‐9) ICBT with clinician M = 11.40 (SD = 4.63); WLC M = 12.5 (SD = 4.73) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail and phone support from a clinician (n = 51) Duration: 6 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on cognitive restructuring, challenging core beliefs, and exposure, with e‐mail and phone support from a therapist for module activities Therapists: 1 registered clinical psychologist Therapist contact: M e‐mails or calls by therapist = 33.2 (SD = 4); M time spent by therapist per participant = 80.8 min (SD = 22.6) Face‐to‐face contact: none Dropout: n = 5; 9.8% (2) Internet‐based CBT with e‐mail and phone support from a technician (n = 50) Duration: 6 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on cognitive restructuring, challenging core beliefs, and exposure, with e‐mail and phone encouragement and instructions from a technician Therapists: no therapist; clinic manager acted as technician Therapist contact: none; M e‐mails or calls by technician = 31.1 (SD =3.1); M time spent by clinician per participant = 74.5 min (SD = 7.8) Dropout: n = 5; 10% Face‐to‐Face Contact: none (3) Waiting list control (n = 49) Duration: 11 weeks Therapist, face‐to‐face contact: none Dropout: n = 2; 4.1% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcomes: (1) generalized anxiety symptoms: Penn State Worry Questionnaire (2) clinically important improvement: GAD‐7 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction (at post‐treatment): A 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *on‐line treatment program: Worry Program ‐ Titov N, Andrews G, Robinson E, Schwencke G, Johnston L, et al. (2009). Clinician‐assisted Internet‐based treatment is effective for generalized anxiety disorder: a randomised controlled trial. Australian and New Zealand Journal of Psychiatry, 43, 905–912. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 150 people accepted into the program were randomised by NT [2nd author] via a true randomisation process (www.random.org)..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Allocation preceded the diagnostic telephone call." Comment: insufficient detail about method of allocation concealment provided to determine risk |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT clinician versus Internet‐based CBT technician versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment data was collected from 45 (90%) TA, 46 (98%) CA group members, and from 47/48 (98%) of control group participants."; "In accordance with the ITT and LOCF paradigm..." Comment: a small and similar number of participants from both treatment conditions did not complete post‐treatment measures; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Unclear risk | There were significant differences in marital status and age between the control and treatment groups at baseline |
Silfvernagel 2012.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Anxiety Disorder Method of diagnosis: SCID‐IV N: 57 Age: M = 32.4 (SD = 6.9); range = 20 to 45 Sex: 65% women Country of residence: Sweden Psychiatric co‐morbidity: 32% Co‐use of adjunct therapy: excluded Co‐use of medication: included if stable dose for past 3 months Method of enrolment: responded to media advertisements in community and online Baseline depression severity: (MADRS‐S) ICBT M = 15.81 (SD = 7.35); WLC M = 17.93 (SD = 8.38) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support from a clinician (n = 29) Duration: 6 to 8 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, and exposure, with e‐mail support from a therapist for module activities Therapists: 3 clinical psychology master's students; completed clinical training; supervised by experienced clinical psychologists Therapist contact: 15 min/week; approximately 19 e‐mail exchanges between therapist and participant during treatment Face‐to‐face contact: none Dropout: n = 10; 34.5% (2) Waiting list control (n = 28) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 2; 7.1% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) panic symptoms: Panic Disorder Severity Scale (2) general anxiety: Beck Anxiety Inventory; Clinical Outcomes in Routine Evaluation ‐ Outcome Measure Secondary outcome: (1) quality of life: Quality of Life Inventory |
|
| Notes | *treatment based on Internet‐based programs described in: Andersson, G., Carlbring, P., Holmström, A., Sparthan, E., Furmark, T., Nilsson‐Ihrfelt, E., et al. (2006). Internet‐based self‐help with therapist feedback and invivo group exposure for social phobia: a randomised controlled trial. Journal of Consulting and Clinical Psychology, 74, 677‐686.; Carlbring, P., Westling, B.E., Ljungstrand, P., Ekselius, L, & Andersson, G. (2001). Treatment of panic disorder via the Internet: A randomised trial of a self‐help program. Behavior Therapy, 32, 751‐764.; AND Vernmark, K., Lenndin, J., Bjärehed, J., Carlsson, M., Karlsson, J., Öberg, J., et al. (2010). Internet administered guided self‐help versus individualized e‐mail therapy: a randomised trial of two versions of CBT for major depression. Behaviour Research and Therapy, 48, 368‐376.; Carlbring, P., Maurin, L., Törngren, C., Linna, E., Eriksson, T., Sparthan, E., et al. (2011). Individually‐tailored, Internet‐based treatment for anxiety disorders: A randomised controlled trial. Behaviour Research and Therapy, 49, 18‐24.; Andersson, G., Estling, F., Jakobsson, E., Cuijpers, P., & Carlbring, P. (2011). Can the patient decide which modules to endorse? An open trial of tailored internet treatment of anxiety disorders. Cognitive Behavior Therapy, 40, 57‐64. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participants were divided into two groups so that the two predetermined age groups 18–30 years (young adults) and 31–45 years(adults) were equally represented in each condition. The blocked randomizations process was conducted through an online true random number‐generation service (random.org) independent of the investigators and therapists." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The blocked randomizations process was conducted...independent of the investigators and therapists." Comment: no more specific mention of allocation concealment present |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT clinician versus Internet‐based CBT technician versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | Low risk | Quote: "At posttreatment participants were instructed via email to complete the follow‐up questionnaires and to participate in a semistructured telephone interview carried out by a blinded assessor who had no earlier contact with the participants." Comment: assessors were blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "A mixed‐models approach with an unstructured covariance structure was endorsed as a way to handle missing data at posttreatment." Comment: ITT analysis was used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Spence 2011.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Post‐traumatic Stress Disorder Method of Diagnosis: MINI N: 44 Age: M = 42.6 (SD = 13.1); range = 21 to 68 Sex: 81% women Country of residence: Australia Psychiatric co‐morbidity: 62% MDD, 33% Social Phobia, 31% PD with or without Agoraphobia, 26% GAD, 17% OCD Co‐use of adjunct therapy: excluded Co‐use of medication: 60% Method of enrolment: responded to media advertisements in community and online Baseline depression severity: (PHQ‐9) ICBT M = 15.61 (SD = 7.35); WLC CBT M = 15.05 (SD = 4.9) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail and phone support from a clinician (n = 23) Duration: 7 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, de‐arousal strategies, cognitive restructuring, graded exposure, and relapse prevention with e‐mail and phone support from a therapist for module activities Therapists: 1 clinical psychologist Therapist contact: M e‐mails by therapist = 5.39 (SD = 3.54); M phone calls by therapist = 7.87 (SD = 2.56); M time spent by therapist per participant = 103.91 min (SD = 96.53) Face‐to‐face contact: none Dropout: n = 2; 8.7% (2) Waiting list control (n = 21) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout: n = 3; 14.3% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) post‐traumatic stress symptoms: Post‐traumatic Stress Disorder Checklist – Civilian (2) general anxiety symptoms: GAD‐7 (3) clinically important improvement: Post‐traumatic Stress Disorder Checklist – Civilian Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction (at post‐treatment): a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *treatment is based on: Andrews, G. (2003). The treatment of anxiety disorders: Clinician guides and patient manuals. Cambridge: Cambridge University Press.; Perini, S., Titov, N., & Andrews, G. (2008). The climate sadness program of Internet‐based treatment for depression: A pilot study. Journal of Applied Psychology, 4, 18‐24.; Robinson, E., Titov, N., Andrews, G., McIntyre, K., Schwencke, G., & Solley, K. (2010). Internet treatment for generalized anxiety disorder: A randomised controlled trial comparing clinician vs. technician assistance. PLoS ONE, 5, e10942.; Wims, E., Titov, N., Andrews, G., & Choi, I. (2010). Clinician‐assisted Internet‐based treatment is effective for panic: A randomised controlled trial. Australian and New Zealand Journal of Psychiatry, 44, 599‐607.; Titov, N., Andrews, G., Johnston, L., Robinson, E., & Spence, J. (2010). Transdiagnostic Internet treatment for anxiety disorders: A randomised controlled trial. Behaviour Research and Therapy, 48, 890‐9. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...randomised via a true randomizations process (www.random.org), generated by an independent person..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus online discussion group) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | High risk | Quote: "The assessments were conducted by JS and KS, who were not blind to the participants' condition." Comment: interviewers were not blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All post‐treatment analyses involved a conservative intention‐to‐treat (ITT) design where missing data was addressed by carrying forward the first available data (i.e. Baseline‐observation‐carried‐forward model)."; "Five participants did not complete the program: one for unknown reasons; three because of competing time commitments; and one because of a relapse of depressive symptoms. There were no formal withdrawals during the treatment program."; "Post‐treatment data were collected from 21/23 (91%) Treatment and 18/21 (86%) Control group participants." Comment: very little data were missing; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Tillfors 2008.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of Diagnosis: SCID‐IV N: 38 Age: for ICBT, M = 32.3 (SD = 9.7); for ICBT + exposure, M = 30.4 (SD = 6.3); range = 19 to 53 Sex: 78.9% women Country of residence: Sweden Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: included Method of enrolment: responded to media advertisements in community and online Baseline depression severity: (MADRS‐S) ICBT M = 11.3 (SD = 7.3); ICBT + exposure M = 12.4 (SD = 6.4) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 19) Duration: 9 online modules completed in 9 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, social skills, and relapse prevention, with e‐mail support from a therapist for module activities, and participated in an online discussion forum Therapists: 2 licensed clinical psychologists (research or clinical experience, or both, in social phobia), 2 clinical psychology students in final year of master's program; supervised by licensed CBT psychotherapist Therapist contact: 35 min per week Face‐to‐face contact: none Dropout: n = 1; 5.3% (2) Internet‐based CBT with e‐mail support and face‐to‐face exposure (n = 19) Duration: 9 online modules and 5 face‐to‐face group exposure sessions over 9 weeks Treatment protocol*^: participants completed online modules on psychoeducation, cognitive restructuring, exposure, social skills, and relapse prevention, with e‐mail support from a therapist for module activities, and participated in an online discussion forum as well as attending 5 face‐to‐face group therapy sessions Therapists: 2 licensed clinical psychologists, 2 psychologist candidates Therapist contact: 35 min per week by e‐mail and 5 x 2.25 hr exposure sessions Face‐to‐face contact: 5 x 2.25 hr exposure sessions Dropout: n = 1; 5.3% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 1 year follow‐up Primary outcomes: (1) social phobia symptoms: Liebowitz Social Anxiety Scale – Self‐Report; Social Phobia Scale; Social Interaction Anxiety Scale; Social Phobia Screening Questionnaire (2) general anxiety: Beck Anxiety Inventory Secondary outcomes: (1) quality of life: Quality of Life Inventory (2) treatment satisfaction (at post‐treatment): participants reported on the quality of the overall treatment, its components, and its tempo as well as perceptions of their own improvement |
|
| Notes | *treatment based on: Rodebaugh, T.L., Holaway, R.M., & Heimberg, R.G. (2004). The treatment of social anxiety disorder. Clinical Psychology Review, 24, 883–908. AND Clark, D.M., & Wells, A. (1995). A cognitive model of social phobia. In R.G. Heimberg, M.R. Liebowitz, D.A. Hope, & F.R. Schneier (Eds.), Social phobia: Diagnosis, assessment and treatment (pp. 69‐93). New York, NY: Guilford Press. ^exposure sessions based on Heimberg, R.G., & Becker, R.E. (2002). Cognitive‐behavioral group therapy for social phobia: basic mechanisms and clinical strategies. New York, NY: Guilford Press. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...38 were eventually randomised into either..." Comment: no information on method of randomisation provided |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus Internet‐based CBT plus live exposure) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "At post‐test, all participants except one answered their computerized questionnaires. The pre‐test score of that participant was carried forward to the post‐test assessment point (e.g., last observation carried forward)." Comment: though there were a number of participants who did not complete all treatment modules (n = 10 ICBT + Exp; n = 9 ICBT) the numbers were relatively equal across conditions and participants still provided post‐treatment data; ITT analyses used |
| Selective reporting (reporting bias) | Unclear risk | No study protocol or trial registration available |
| Other bias | Unclear risk | Group comparisons at baseline not reported |
Titov 2008a.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: CIDI N: 105 Age: M = 38.13 (SD = 12.24); range = 18 to 72 Sex: 59% women Country of residence: Australia Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: 29% Method of enrolment: responded to media advertisements in community Baseline depression severity: (PHQ‐9) ICBT M = 8.0 (SD = 4.95); WLC M = 8.02 (SD = 5.32) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 50) Duration: 6 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, and relapse prevention, with email support from a therapist for module activities Therapists: 1 clinical psychologist Therapist contact: M time spent by therapist per participant = 125 min (SD = 25) Face‐to‐face contact: none Dropout: n = 6; 12% (2) Waiting list control (n = 55) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 6; 10.9% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcome: (1) social phobia symptoms: Social Interaction Anxiety Scale; Social Phobia Scale Secondary outcomes: (1) quality of life: WHO Disability Assessment Schedule (2) treatment satisfaction (at post‐treatment): a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *online treatment program: Shyness Programme (based on CLIMATEGP program written by Drobny and Einstein) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...were randomised via a true randomizations process (www.random.org) to either..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Eleven members of the treatment group (22%) failed to complete all six lessons within the required time frame. Of these non‐completers, two formally withdrew citing lack of time and motivation after experiencing a death or illness in the family; one reported that the exposure exercises were too anxiety provoking; one reported he did not find the programme helpful; one reported taking an overseas holiday; three cited a change in work or study commitments affecting their ability to complete the programme requirements; one reported complications due to her pregnancy and two did not give a reason."; "Post‐treatment data were collected from 93 participants (44/50 treatment group participants and 49/49 waitlist control group participants). In accordance with the intention‐to‐treat paradigm, the pre‐treatment scores of these six participants who did not complete the post‐treatment questionnaires were replicated as their post‐treatment scores." Comment: there were a number of dropouts from the treatment group, however some of these dropouts still provided post‐treatment data; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | Results for one outcome measure outlined in the trial registry (GAD‐7) are not reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2008b.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: CIDI N: 88 Age: M = 36.79 (SD = 10.93); range = 20 to 61 Sex: 62.96% women Country of residence: Australia Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: 25.9% Method of enrolment: responded to media advertisements in community Baseline depression severity: (PHQ‐9) ICBT M = 8.44 (SD = 5.7); WLC M = 7.35 (SD = 4.19) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email support (n = 43) Duration: 6 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, and relapse prevention, with email support from a therapist for module activities Therapists: 1 clinical psychologist Therapist contact: M time spent by therapist per participant = 126.76 min (SD = 30.89) Face‐to‐face contact: none Dropout: n = 5; 11.6% (2) Waiting list control (n = 45) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 5; 11.1% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcome: (1) social phobia symptoms: Social Interaction Anxiety Scale; Social Phobia Scale Secondary outcomes: (1) quality of life: WHO Disability Assessment Schedule (2) treatment satisfaction (at post‐treatment): a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *online treatment program: Shyness Programme (based on CLIMATEGP program written by Drobny and Einstein) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 88 people accepted into the programme were randomised via a true randomizations process (www.random.org) to either..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Eight members of the treatment group (20%) failed to complete all six lessons within the require time frame. Of these eight non‐completers, one said the programme was not helpful, and one reported they had improved sufficiently."; "...post‐treatment data were collected from 78 participants (38/41 treatment group participants and 40/40 waitlist control group participants). In accordance with the intention‐to‐treat paradigm, the pre‐treatment scores...were replicated as their post‐treatment scores." Comment: a small and similar number of participants from both treatment conditions did not complete post‐treatment measures; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | Results for one outcome measure outlined in the trial registry (GAD‐7) are not reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2008c.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of Diagnosis: MINI N: 98 Age: M = 37.97 (SD = 11.29); range = 18 to 64 Sex: 61.05% women Country of residence: Australia Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: 25.9% Method of enrolment: responded to media advertisements in community Baseline depression severity: (PHQ‐9) ICBT M = 7.65 (SD = 4.72); Unguided ICBT M = 7.0 (SD = 5.27); WLC M = 7.03 (SD = 5.28) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with e‐mail support (n = 32) Duration: 6 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, and relapse prevention, with email support from a therapist for module activities Therapists: 2 clinical psychologists Therapist contact: M time spent by therapist per participant = 168 minutes (SD = 40) Face‐to‐face contact: none Dropout: n = 2; 6.3% (2) Internet‐based CBT (n = 31) Duration: 6 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, and relapse prevention independently Therapist, face‐to‐face contact: none Dropout: n = 4; 12.9% (3) Waiting list control (n = 35) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 1; 2.9% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcome: (1) social phobia symptoms: Social Interaction Anxiety Scale; Social Phobia Scale Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *online treatment program: Shyness Programme (based on CLIMATEGP program written by Drobny and Einstein) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 98 people accepted into the programme were randomised via a true randomizations process (www.random.org) to either..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (clinician‐assisted computerized CBT versus non‐clinician‐assisted computerized CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment data were collected from 91 participants (30/31 CaCCBT group participants, 27/30 CCBT group participants, and from 34/34 control group participants). In accordance with the ITT paradigm, the pre‐treatment scores of the four participants who did not complete their post‐treatment questionnaires were replicated as their post‐treatment scores." Comment: a small and similar number of participants from both treatment conditions did not complete post‐treatment measures; ITT analyses were used |
| Selective reporting (reporting bias) | Unclear risk | Results for one outcome measures (GAD‐7) outlined in the trial registration were not reported; all other outcome measures outlined in the trial registration were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2009.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of Diagnosis: MINI N: 48 Age: M = 44 (SD = 12.98) Sex: 76% women Country of residence: Australia Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: 29% Method of enrolment: responded to online study advertisements Baseline depression severity: (PHQ‐9) ICBT M = 11.58 (SD = 5.24); WLC M = 13.0 (SD = 6.19) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail and phone support (n = 25) Duration: 6 online modules completed over 9 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, core beliefs, and relapse prevention, with e‐mail and phone support from a therapist for module activities Therapists: 1 clinical psychologist Therapist contact: M e‐mails by therapist = 23.7; M telephone calls by therapist = 4.1; M instant messages by therapist = 5.5; M time spent by therapist per participant = 130 min Face‐to‐face contact: none Dropout: n = 5; 20% (2) Waiting list control (n = 23) Duration: 9 weeks Therapist, face‐to‐face contact: none Dropout: n = 4; 17.4% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) general anxiety symptoms: Penn State Worry Questionnaire (2) clinically important improvement: GAD‐7 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: A 7‐item questionnaire based on the Credibility/ Expectancy Questionnaire |
|
| Notes | *online treatment program: Worry Programme, developed for this study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 48 people accepted into the programme were randomised by NT [Nickolai Titov] via a true randomizations process (www.random.org) to either..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Allocation preceded the screening phone call." Comment: unclear if allocation was kept concealed from screener |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment data were collected from 21/24 (88%) treatment group participants and 19/21 (90%) of control group participants. In accordance with the ITT paradigm, the pre‐treatment scores of the five participants who did not complete the post‐treatment questionnaires were replicated as their post‐treatment scores." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2010.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with Agoraphobia (26.9%), Social Phobia (29.5%), Generalized Anxiety Disorder (43.6%) Method of Diagnosis: MINI N: 86 Age: M = 39.5 (SD = 13) Sex: 67.9% women Country of residence: Australia Psychiatric co‐morbidity: 28.2% another Anxiety Disorder only, 20.5% another Affective Disorder only, 26.9% another Anxiety and Affective Disorder Co‐use of adjunct therapy: excluded Co‐use of medication: 47.4% Method of enrolment: responded to online study advertisements Baseline depression severity: (PHQ‐9) ICBT M = 10.77 (SD = 5.20); WLC M = 10.84 (SD = 6.26) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email and phone support (n = 42) Duration: 6 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on disorder‐specific psychoeducation, cognitive restructuring, exposure, assertiveness training, and relapse prevention, with email and phone support from a therapist for module activities Therapists: 2 clinical psychologists Therapist contact: M e‐mails by therapist = 23.6; M time spent by therapist per participant = 46 min (SD = 16) Face‐to‐face contact: none Dropout: n = 6; 14.3% (2) Waiting list control (n=44) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout: n = 8; 18.2% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) disorder‐specific symptoms: Penn State Worry Questionnaire; Social Phobia Screening Questionnaire; Panic Disorder Severity Scale – Self‐Rating (2) clinically important improvement: GAD‐7 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *online treatment program: Anxiety Programme, developed for this study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eighty six applicants met all inclusion criteria and were randomised by NT [Nickolai Titov] via a true randomizations process (www.random.org)..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Allocation preceded the screening phone call." Comment: unclear if screener was aware of group allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT vs. waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment data (Time 2) was collected from 38/40 (95%) treatment group participants and 40/40 (100%) control group participants... In accordance with the ITT and BOCF principles, the pre‐treatment scores of participants who did not complete the post‐treatment... questionnaires were replicated as their post‐treatment... scores." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | High risk | Results for several outcome measures (Beck Anxiety Inventory, Social Phobia Scale, Social Interaction Anxiety Scale, Agoraphobic Cognitions Questionnaire, Body Vigilance Scale, WHO Disability Assessment Schedule II) outlined in the trial registration were not reported and other scales not in the trial registration (Penn State Worry Questionnaire, Social Phobia Screening Questionnaire, Panic Disorder Severity Scale) were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2010 GAD.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of Diagnosis: MINI N: 34 Age^: M = 39.5 (SD = 13) Sex^: 67.9% women Country of residence: Australia Psychiatric co‐morbidity^: 28.2% another Anxiety Disorder only, 20.5% another Affective Disorder only, 26.9% another Anxiety and Affective Disorder Co‐use of adjunct therapy: excluded Co‐use of medication^: 47.4% Method of enrolment: responded to online study advertisements Baseline depression severity^: (PHQ‐9) ICBT M = 10.77 (SD = 5.20); WLC M = 10.84 (SD = 6.26) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email and phone support (n = 18) Duration: 6 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, assertiveness training, and relapse prevention, with email and phone support from a therapist for module activities Therapists: 2 clinical psychologists Therapist contact^: M emails by therapist = 23.6; M time spent by therapist per participant = 46 min (SD = 16) Face‐to‐face contact: none Dropout^: n = 6; 14.3% (2) Waiting list control (n = 16) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout^: n = 8; 18.2% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) generalized anxiety disorder symptoms: Penn State Worry Questionnaire (2) clinically important improvement: GAD‐7 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *online treatment program: Anxiety Programme, developed for this study ^statistics for entire Titov 2010 sample |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eighty six applicants met all inclusion criteria and were randomised by NT [Nickolai Titov] via a true randomizations process (www.random.org)..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Allocation preceded the screening phone call." Comment: unclear if screener was aware of group allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment data (Time 2) was collected from 38/40 (95%) treatment group participants and 40/40 (100%) control group participants... In accordance with the ITT and BOCF principles, the pre‐treatment scores of participants who did not complete the post‐treatment... questionnaires were replicated as their post‐treatment... scores." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | High risk | Results for several outcome measures outlined in the trial registration were not reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2010 Panic.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with Agoraphobia Method of Diagnosis: MINI N: 21 Age^: M = 39.5 (SD = 13) Sex^: 67.9% women Country of residence: Australia Psychiatric co‐morbidity^: 28.2% another Anxiety Disorder only, 20.5% another Affective Disorder only, 26.9% another Anxiety and Affective Disorder Co‐use of adjunct therapy: excluded Co‐use of medication^: 47.4% Method of enrolment: responded to online study advertisements Baseline depression severity^: (PHQ‐9) ICBT M = 10.77 (SD = 5.20); WLC M = 10.84 (SD = 6.26) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail and phone support (n = 10) Duration: 6 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, assertiveness training, and relapse prevention, with e‐mail and phone support from a therapist for module activities Therapists: 2 clinical psychologists Therapist contact^: M e‐mails by therapist = 23.6; M time spent by therapist per participant = 46 min (SD = 16) Face‐to‐face contact: none Dropout^: n = 6; 14.3% (2) Waiting list control (n = 11) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout^: n = 8; 18.2% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) panic symptoms: Panic Disorder Severity Scale – Self‐Rating (2) clinically important improvement: GAD‐7 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *online treatment program: Anxiety Programme, developed for this study ^statistics for entire Titov 2010 sample |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eighty six applicants met all inclusion criteria and were randomised by NT [Nickolai Titov] via a true randomizations process (www.random.org)..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Allocation preceded the screening phone call." Comment: unclear if screener was aware of group allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment data (Time 2) was collected from 38/40 (95%) treatment group participants and 40/40 (100%) control group participants... In accordance with the ITT and BOCF principles, the pre‐treatment scores of participants who did not complete the post‐treatment... questionnaires were replicated as their post‐treatment... scores." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | High risk | Results for several outcome measures outlined in the trial registration were not reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2010 Social Phobia.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: MINI N: 23 Age^: M = 39.5 (SD = 13) Sex^: 67.9% women Country of residence: Australia Psychiatric co‐morbidity^: 28.2% another Anxiety Disorder only, 20.5% another Affective Disorder only, 26.9% another Anxiety and Affective Disorder Co‐use of adjunct therapy: excluded Co‐use of medication^: 47.4% Method of enrolment: responded to online study advertisements Baseline depression severity^: (PHQ‐9) ICBT M = 10.77 (SD = 5.20); WLC M = 10.84 (SD = 6.26) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail and phone support (n = 12) Duration: 6 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, assertiveness training, and relapse prevention, with e‐mail and phone support from a therapist for module activities Therapists: 2 clinical psychologists Therapist contact^: M e‐mails by therapist = 23.6; M time spent by therapist per participant = 46 min (SD = 16) Face‐to‐face contact: none Dropout^: n = 6; 14.3% (2) Waiting list control (n = 11) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout^: n = 8; 18.2% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) social phobia symptoms: Social Phobia Screening Questionnaire (2) clinically important improvement: GAD‐7 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: a 7‐item questionnaire based on the Credibility/ Expectancy Questionnaire |
|
| Notes | *online treatment program: Anxiety Programme, developed for this study ^statistics for entire Titov 2010 sample |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eighty six applicants met all inclusion criteria and were randomised by NT [Nickolai Titov] via a true randomizations process (www.random.org)..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Allocation preceded the screening phone call." Comment: unclear if screener was aware of group allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT versus waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | All outcome measures were self‐report and participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment data (Time 2) was collected from 38/40 (95%) treatment group participants and 40/40 (100%) control group participants... In accordance with the ITT and BOCF principles, the pre‐treatment scores of participants who did not complete the post‐treatment... questionnaires were replicated as their post‐treatment... scores." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | High risk | Results for several outcome measures outlined in the trial registration were not reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Titov 2011.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with or without Agoraphobia (10%), Social Phobia (11%), Generalized Anxiety Disorder (28%), MDD (51%; not included in review) Method of diagnosis: MINI N: 74 Age: M = 43.9 (SD = 14.6); range = 18 to 79 Sex: 73% women Country of residence: Australia Psychiatric co‐morbidity: 81% had another co‐morbid Anxiety or Depressive Disorder Co‐use of adjunct therapy: excluded Co‐use of medication: 54% Method of enrolment: responded to online study advertisements Baseline depression severity: (PHQ‐9) ICBT M = 13.48 (SD = 5.36); WLC M = 12.56 (SD = 5.81) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail and phone support (n = 37) Duration: 8 online modules completed over 10 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, de‐arousal strategies, behavioural activation, exposure, challenging core beliefs, and relapse prevention, with e‐mail and phone support from a therapist for module activities Therapists: 1 clinical psychologist Therapist contact: M e‐mails by therapist = 5.45 (SD = 3.57); M phone calls by therapist = 9.35 (SD = 2.96); M time spent by therapist per participant = 84.76 min (SD = 50.37) Face‐to‐face contact: none Dropout: n = 3; 8.1% (2) Waiting list control (n = 37) Duration: 10 weeks Therapist, face‐to‐face contact: none Dropout: n = 2; 5.4% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) disorder‐specific symptoms: Penn State Worry Questionnaire; Social Phobia – 12; Panic Disorder Severity Scale (2) general anxiety: GAD‐7, Depression Anxiety Stress Scales ‐ 21 Secondary outcomes: (1) quality of life: Sheehan Disability Scale (2) treatment satisfaction: a 7‐item questionnaire based on the Credibility/Expectancy Questionnaire |
|
| Notes | *treatment based on: Andrews, G., Creamer, M., Crino, R., Hunt, C., Lampe, L., & Page, A. (2003). The treatment of anxiety disorders: Clinician guides and patient manuals (2nd ed.). UK: University Press, Cambridge.; Perini, S., Titov, N., & Andrews, G. (2009). Clinician‐assisted Internet‐based treatment is effective for depression: A randomised controlled trial. Australian and New Zealand Journal of Psychiatry, 43, 571‐8.; Titov, N., Andrews, G., Davies, M., McIntyre, K., Robinson, E., & Solley, K. (2010). Internet treatment for depression: A randomised controlled trial comparing clinician vs. technician assistance. PLoS ONE, 5, e10939.; Robinson, E., Titov, N., Andrews, G., McIntyre, K., Schwencke, G., & Solley, K. (2010). Internet treatment for generalized anxiety disorder: A randomised controlled trial comparing clinician vs. technician assistance. PLoS ONE, 5, e10942.; Titov, N., Andrews, G., Schwencke, G., Drobny, J., & Einstein, D. (2008). Shyness 1: Distance treatment of social phobia over the internet. Australian and New Zealand Journal of Psychiatry, 42, 585‐94.; Wims, E., Titov, N., Andrews, G., & Choi, I. (2010). Clinician‐assisted internet‐based treatment is effective for panic: A randomised controlled trial. Australian and New Zealand Journal of Psychiatry, 44, 599‐607. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...randomised via a true randomisation process (www.random.org), generated by an independent person..." Comment: adequate randomisation method" |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based CBT vs. waiting list control) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | High risk | Quote: "These [diagnostic] assessments were conducted by BFD and GS, who were not blind to participant's condition." Comment: interviewers were not blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All post‐treatment analyses involved a conservative intention‐to‐treat (ITT) design where missing data was addressed by carrying forward the first available data (i.e., baseline‐observation‐carried‐forward model; BOCF)." Comment: there were only four formal withdrawals from the study; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | High risk | Treatment group endorsed significantly higher PDSS‐SR scores than controls at baseline |
van Ballegooijen 2013.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with or without Agoraphobia (78%), Agoraphobia without Panic (14%) Method of diagnosis: CIDI N: 126 Age: M = 36.6 (SD = 11.4); range = 18 to 67 Sex: 67.5% women Country of residence: Netherlands Psychiatric co‐morbidity: included Co‐use of adjunct therapy: included Co‐use of medication: included Method of enrolment: responded to media advertisements in community and online Baseline depression severity: (CES‐D) ICBT M = 20.0 (SD = 9.1); WLC M = 21.6 (SD = 9.0) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 63) Duration: 6 online modules completed over 12 weeks Treatment protocol*: participants completed online modules on various cognitive and behavioural techniques and skills, with e‐mail support from a therapist for module activities Therapists: master's level clinical psychology students; supervised by clinical psychologist Therapist contact: M time spent by therapist per participant = 1 to 2 hours Face‐to‐face contact: none Dropout: n = 29; 46% (2) Waiting list control (n = 63) Duration: 12 weeks Treatment protocol: participants had access to online non‐CBT panic resources Therapist, face‐to‐face contact: none Dropout: n = 24; 38.1% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcomes: (1) disorder‐specific symptoms: Panic Disorder Severity Scale (2) general anxiety: Beck Anxiety Inventory |
|
| Notes | *treatment called Don't Panic Online, described in: van Ballegooijen, W., Riper, H., van Straten, A., Kramer, J., Conijn, B., & Cuijpers, P. (2011). The effects of an Internet based self‐help course for reducing panic symptoms‐‐Don't Panic Online: Study protocol for a randomised controlled trial. Trials, 12, 75. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After the interview, all participants were randomized to 1 of the 2 groups. Randomization was stratified for the presence or absence of agoraphobic symptoms (PDSS‐SR item 4 score ≥2) and the use of antidepressants or sedatives. Randomization lists were generated automatically using a computer program." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to the treatment condition they were in (Internet‐based CBT or waiting list control) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Significant drop out in both conditions; ITT analyses were employed via multiple imputation |
| Selective reporting (reporting bias) | Unclear risk | One outcome ‐ quality of life, as measured by the EuroQol Questionnaire ‐ outlined in the published study protocol was not reported; results for all other outcome measures outlined in the study protocol were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Wims 2010.
| Methods | Randomised controlled trial | |
| Participants |
Diagnosis: DSM‐IV Panic Disorder with or without Agoraphobia Method of Diagnosis: MINI N: 2759 Age: M = 42.08 (SD = 12.29) Sex: 76% women Country of residence: Australia Psychiatric co‐morbidity: 21% Social Phobia, 31% GAD, 10% OCD, 7% PTSD, 21% Major Depressive episode Co‐use of adjunct therapy: excluded Co‐use of medication: 31% Method of enrolment: responded to online study advertisements Baseline depression severity: (PHQ‐9) ICBT M = 10.34 (SD = 4.09); WLC M = 10.24 (SD = 5.93) |
|
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support (n = 32) Duration: 6 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, cognitive restructuring, exposure, physiological de‐arousal, and relapse prevention, with email support from a therapist for module activities Therapists: 1 psychiatry registrar Therapist contact: M e‐mails by therapist = 7.5; M time spent by therapist per participant = 75 min Face‐to‐face contact: none Dropout: n = 10; 31.3% (2) Waiting list control (n = 27) Duration: 8 weeks Therapist, face‐to‐face contact: none Dropout: n = 5; 18.5% |
|
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 1 month follow‐up Primary outcome: (1) panic and agoraphobia symptoms: Panic Disorder Severity Scale; Body Sensations Questionnaire; Agoraphobic Cognitions Questionnaire; Mobility Inventory Secondary outcome: (1) quality of life: Sheehan Disability Scale |
|
| Notes | *online treatment program: Panic Program ‐ Wims E, Titov N, Andrews G. (2008). The Panic program: An open trial of Internet‐based treatment for panic disorder. Electronic Journal of Applied Psychology, 4, 2. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 59 people accepted into the program were randomised via a true randomizations process (www.random.org) to either..." Comment: adequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment condition nor therapists to the treatment they delivered (Internet‐based applied relaxation versus Internet‐based CBT) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | High risk | Quote: "...the lack of blinding in the administration of the PDSS is a source of bias, which may account for the larger effect sizes in this domain." Comment: interviewers were not blind to treatment condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Two participants found the program required more time than they were able to set aside, one person dropped out due to increased severity of their anxiety which required inpatient admission, another became ill, another found the course too difficult and the final participant moved house during the program and no longer had internet access."; "Post‐treatment data was collected from 44 participants (22/29 treatment group and 22/25 waitlist control group). In accordance with the intention‐to‐treat paradigm, the pre‐treatment scores of the participants who did not complete the post‐treatment questionnaires were replicated as their post‐treatment scores." Comment: a small and similar number of dropouts from both treatment conditions was reported; ITT analyses were used |
| Selective reporting (reporting bias) | Low risk | Results for all outcome measures outlined in the trial registration were reported |
| Other bias | Low risk | Groups did not differ significantly on any measures at pre‐treatment |
Wootton 2013.
| Methods | Randomized controlled trial | |
| Participants |
Diagnosis: DSM‐IV Obsessive Compulsive Disorder Method of diagnosis: MINI N: 52 Age: for bibliotherapy, M = 35.55 (SD = 9.68); for Internet CBT, M = 39.93 (SD = 12.57); for waiting list, M = 38.58 (SD = 10.51); range = 18 to 64 years Sex: 75% women Country of residence: Australia Psychiatric co‐morbidity: 26.9% Social Phobia, 40.4% Generalized Anxiety Disorder, 15.4% Panic Disorder, 11.5% Posttraumatic Stress Disorder, 38.5% Major Depressive Disorder Co‐use of adjunct therapy: excluded Co‐use of medication: 61.5% SSRIs Method of enrolment: applied online Baseline depression severity: (PHQ‐9) Bibliotherapy M = 12.15 (SD = 5.99); ICBT M = 10.00 (SD = 6.00); Waiting List M = 11.06 (SD = 6.02) |
|
| Interventions | Participants were randomly assigned to one of: (1) Internet‐based CBT with phone support (n = 17) Duration: 5 online modules completed over 8 weeks Treatment protocol*: participants completed online modules on psychoeducation, exposure and response prevention, cognitive biases, and relapse prevention, with phone support from a therapist Therapist: 1 clinical psychologist Therapist contact: M calls by therapist = 15.05 (SD = 3.93); M time spent by therapist per participant overall = 88.63 min (SD = 46.41) Face‐to‐face contact: none Dropout: n = 5; 29.4% (2) Bibliotherapy CBT with phone support (n = 20) Duration: 5 lessons completed over 8 weeks Treatment protocol*: participants read lessons on printed material on psychoeducation, exposure and response prevention, cognitive biases, and relapse prevention, with phone support from a therapist Therapist: 1 clinical psychologist Therapist contact: M calls by therapist = 14.4 (SD = 3.58); M time spent by therapist per participant overall = 102.73 min (SD = 50.52) Face‐to‐face contact: none Dropout: n = 5; 25% (3) Waiting list control (n = 19) Duration: 8 weeks Therapist/Face‐to‐face contact: none Dropout: n = 1; 58.8% |
|
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcomes: (1) OCD symptoms: Dimensional Obsessive Compulsive Scale (2) general anxiety: GAD‐7 (3) clinically important improvement: Yale Brown Obsessive Compulsive Scale Secondary outcome: (1) treatment satisfaction: queried amount of satisfaction with intervention |
|
| Notes | *“The OCD Course” developed by first three study authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization sequences was computer‐generated by an independent overseas colleague using www.random.org." Comment: adequate randomization method |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants to their treatment, nor therapists to the treatment they delivered (guided internet‐based treatment or waiting list) |
| Blinding of outcome assessment (detection bias) Self‐Report Outcomes | High risk | For self‐report outcome measures, participants were not blind to their own treatment condition |
| Blinding of outcome assessment (detection bias) Observer/Interview‐Rated Outcomes | High risk | Quote: "One limitation of this study was the lack of independent evaluation when administering the YBOCS." Comment: One therapist did all assessment and therapy and so was not blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Post‐treatment questionnaires were completed by 15/20 (75%) participants in the bCBT Group, 10/15 (67%) in the iCBT Group, and 16/17 (94%) in the Control Group."; "Pre‐treatment to post‐treatment...changes on outcome measures were analyzed with mixed linear models using an unstructured covariance structure. Effect sizes...were calculated...using the estimated marginal means..." Comment: Dropouts reported were similar across conditions though reasons for not completing post‐assessment measures were not always clear; intention to treat analyses were used |
| Selective reporting (reporting bias) | Low risk | Only one outcome (MINI at post‐treatment) indicated in the trial registration and study method section was not reported in the trial manuscript, all other outcomes in the trial registration were reported in the manuscript |
| Other bias | Low risk | Quote: "The mixed linear models indicated that there were no significant differences between each of the groups on any of the outcome measures at pre‐treatment (p's > 0.05)." Comment: No baseline differences between groups were detected |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andersson 2006 | The intervention involved too much face‐to‐face contact between therapist and participant (i.e., two live exposure sessions) |
| Andersson 2012c | The comparison condition was non‐directive supportive therapy and thus too active for the present comparisons of interest |
| Andrews 2011 | A standardized diagnostic instrument was not used to assess participants for an anxiety disorder |
| Andrews 2011b | Abandoned due to recruitment issues |
| Andrews 2012a | Abandoned due to recruitment issues |
| Andrews 2012b | The treatment was delivered by a technician, not a therapist |
| Bell 2012 | The intervention did not involve therapist support |
| Berger 2012 | A standardized diagnostic instrument was not used to assess participants for an anxiety disorder |
| Carlbring 2003 | The comparison was active applied relaxation and did not fit into one of the present comparisons |
| Carlbring 2010 | The comparator condition included attention bias modification and so did not fit in any of our comparator categories and was not appropriate for inclusion |
| Carlbring 2011b | Both of the treatment conditions in this study qualified as our intervention of interest, so no appropriate comparator |
| Cunningham 2006 | Participants did not meet DSM or ICD criteria for an anxiety disorder diagnosis |
| Dear 2015 | Participants with an anxiety disorder could not be separated from the rest of the sample |
| Ellis 2011 | Participants were not diagnosed with a DSM or ICD anxiety disorder by study investigators |
| Febbraro 2005 | Only a portion of the sample was diagnosed with PD and it could not be separated from the rest of the sample |
| Gilson 2006 | The comparator condition involved internet‐based CBT delivered by a physician (vs. a psychologist) and so was not sufficiently different from the intervention of interest to be appropriate for inclusion |
| Greist 2002 | The intervention was not delivered directly by a therapist but instead used voice response technology |
| Kenardy 2003 | The intervention was computer‐augmented; there were six face‐to‐face sessions between therapist and participant |
| Kenwright 2005 | The comparator condition was also therapist‐delivered distance CBT and so was not sufficiently different from the intervention of interest to be appropriate for inclusion |
| Klein 2001 | The intervention was not therapist‐delivered (i.e., was entirely self‐help) |
| Klein 2006 | Participants were randomised with 'sequential randomisation', which is more accurately described as sequential allocation with no randomisation |
| Klein 2009 | The comparator condition was also therapist‐delivered distance CBT and so was not sufficiently different from the intervention of interest to be appropriate for inclusion |
| Knaevelsrud 2007 | Participants were not diagnosed with a DSM or ICD anxiety disorder by study investigators |
| Lange 2001 | Participants were not diagnosed with a DSM or ICD anxiety disorder by study investigators |
| Lange 2003 | Participants were not diagnosed with a DSM or ICD anxiety disorder by study investigators |
| Litz 2007 | The comparison was active online supportive counselling and thus too active for the present comparisons |
| Lopez 2014 | The telepsychology intervention did not include therapist contact |
| Marks 2004 | The intervention involved too much face‐to‐face contact between therapist and participant (i.e., in addition to the computer‐based session, each session involved 15 minutes of face‐to‐face contact) |
| Newman 1997 | The intervention was computer‐augmented; there were four face‐to‐face sessions between therapist and participant |
| Pittaway 2009 | Participants were not diagnosed with a DSM or ICD anxiety disorder by study investigators |
| Ruwaard 2010 | Participants had panic attacks but were not diagnosed with PD |
| Saul 2007 | Participants were not diagnosed with a DSM or ICD anxiety disorder by study investigators |
| Schneider 2005 | The comparator condition was also distance CBT delivered by a physician, just without exposure, and so was not significantly different from the intervention of interest to be appropriate for inclusion |
| Shandley 2008 | The comparator condition was also distance CBT delivered by a physician and so was not sufficiently different from the intervention of interest to be appropriate for inclusion |
| Titov 2009b | The comparator condition was also therapist‐delivered distance CBT and so was not sufficiently different from the intervention of interest to be appropriate for inclusion |
| van Straten 2008 | Participants were not diagnosed with a DSM or ICD anxiety disorder by study investigators |
| von Essen 2008 | Participants did not meet DSM or ICD criteria for an anxiety disorder diagnosis |
| Wagner 2012 | Participants did not have to have a DSM or ICD anxiety disorder diagnosis to participate in this investigation |
Characteristics of studies awaiting assessment [ordered by study ID]
Schreuders 2008.
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Social Phobia, Specific Phobia, or Agoraphobia Method of diagnosis: unknown Age: unknown Country of residence: Netherlands Psychiatric co‐morbidity: unknown Co‐use of adjunct therapy: unknown Co‐use of medication: unknown |
| Interventions | Participants randomly assigned to either: (1) Internet‐based CBT with e‐mail support Duration: 6 online modules completed over 12 weeks Treatment protocol: participants complete online CBT modules with a focus on exposure with e‐mail support from a therapist Therapists: unknown Therapist contact: unknown Face‐to‐face contact: none (2) Unclear |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcome: (1) anxiety symptoms: measurement method unknown Secondary outcome: (1) treatment satisfaction |
| Notes | NTR 1260 |
Tabari 2013.
| Methods | Randomized controlled trial |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of diagnosis: unknown N: 62 Age: unknown Sex: unknown Country of residence: Iran Psychiatric co‐morbidity: unknown Co‐use of adjunct therapy: excluded Co‐use of medication: unknown Method of enrolment: unknown Baseline depression severity: unknown |
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with email support (n = 31) Duration: 12 online modules Treatment protocol: participants completed online modules with email support from a therapist Therapist: unknown Therapist contact: unknown Face‐to‐face contact: none Dropout: unknown (2) Waiting list control (n = 31) Duration: unknown Face‐to‐face contact: none Dropout: unknown |
| Outcomes |
Timepoints for Assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcomes: (1) general anxiety: Beck Anxiety Inventory |
| Notes |
Characteristics of ongoing studies [ordered by study ID]
Bishop 2012.
| Trial name or title | Development of a web‐based cognitive behavioral treatment for OEF/OIF veterans with PTSD symptoms and substance misuse |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Post‐traumatic Stress Disorder Method of diagnosis: unknown Age: 21 years and older Country of residence: USA Psychiatric co‐morbidity: included Co‐use of adjunct therapy or medication: unknown |
| Interventions | Participants were randomly assigned to either: (1) Internet‐based CBT with e‐mail support Duration: 24 brief online intervention modules Treatment protocol: participants complete online modules on CBT for PTSD with e‐mail support from a therapist Therapists: unknown Therapist contact: unknown Face‐to‐face contact: none (2) Waiting list control Duration: unknown Face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment Primary outcome: (1) post‐traumatic stress symptoms: unknown how these symptoms were measured |
| Starting date | Spring 2012 |
| Contact information | Kyle Possemato, Ph.D.; Syracuse VA Medical Center, Syracuse, NY 13210; kyle.possemato@va.gov |
| Notes |
Carlbring 2012.
| Trial name or title | |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of diagnosis: unknown Age: 18 years and older Country of residence: Sweden Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: permitted if stable |
| Interventions | Participants randomly assigned to either: (1) Internet‐based CBT with e‐mail support Duration: 9 weeks Treatment protocol: participants complete online CBT modules with email support from a therapist for module exercises Therapists: unknown Therapist contact: unknown Face‐to‐face contact: none (2) Waiting list control Duration: 9 weeks Therapist, face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 6 month, 1 year, and 2 year follow‐ups Primary outcomes: (1) generalized anxiety symptoms: Penn State Worry Questionnaire; GAD‐7 (2) general anxiety symptoms: Beck Anxiety Inventory Secondary outcome: (1) quality of life: Quality of Life Inventory |
| Starting date | |
| Contact information | |
| Notes | NCT01570374 |
Clark 2012.
| Trial name or title | A randomised controlled trial of internet‐based cognitive therapy (iCT) and standard cognitive therapy (CT) for social anxiety disorder |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: unknown Age: 18 to 65 years Country of residence: United Kingdom Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: permitted if stable for past two months |
| Interventions | Participants randomly assigned to one of: (1) Internet‐based CT with e‐mail and telephone support Duration: 14 weeks Treatment protocol: participants complete online CT modules, including video demonstrations of procedures and virtual audiences to practice real‐life tasks, with e‐mail and telephone support from a therapist Therapists: unknown Therapist contact: 10 to 15 min phone conversations weekly in addition to e‐mail contact Face‐to‐face contact: none (2) Face‐to‐face CT Duration: 14 weeks Treatment protocol: participants complete 14 weekly individual CT sessions with a therapist Therapists: unknown Therapist contact: 14 x 90 min individual sessions Face‐to‐face contact: 14 x 90 min individual sessions (3) Waiting list control Duration: 14 weeks Therapist, face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 3 month and 1 year follow‐ups Primary outcome: (1) social phobia symptoms: Anxiety Disorders Interview Schedule (Fear and Avoidance Scale) for DSM‐IV; Social Phobia Weekly Summary Scale; Liebowitz Social Anxiety Scale; Fear of Negative Evaluation Scale; Social Phobia Scale; Social Interaction and Anxiety Scale Secondary outcome: (1) quality of life: Sheehan Disability Scale |
| Starting date | January, 2013 |
| Contact information | Professor David M Clark; Oxford Centre for Anxiety Disorders and Trauma, Department of Experimental Psychology, Tinbergen Building, 9 South Parks Road; david.clark@psy.ox.ac.uk |
| Notes |
Lindner 2013.
| Trial name or title | ACT‐smart: Smartphone‐supplemented iCBT for social phobia and/or panic disorder |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Panic Disorder Method of diagnosis: SCID‐IV Age: 18 years or older Country of residence: Sweden Psychiatric co‐morbidity: excluded if another condition requiring specialized treatment Co‐use of adjunct therapy: excluded Co‐use of medication: included if stable for past 3 months |
| Interventions | Participants randomly assigned to one of: (1) Internet‐based CBT plus smart phone with e‐mail support Duration: 10 online modules over 10 weeks Treatment protocol: participants complete online modules on psychoeducation, relaxation, cognitive restructuring, and exposure, with e‐mail and Skype support from a therapist for module exercises Therapists: unknown Therapist contact: 15 min/week; feedback and support provided in response to participants' homework completion Face‐to‐face contact: none (2) Unguided Internet‐based CBT plus smart phone Duration: 10 online modules over 10 weeks Treatment protocol: participants complete online modules on psychoeducation, relaxation, cognitive restructuring, and exposure, with e‐mail and Skype support from a therapist for module exercises Therapists: unknown Therapist, face‐to‐face contact: none (3) Waiting list control Duration: 10 weeks Therapist, face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 1, 3, 6, and 12 month follow‐ups Primary outcome: (1) panic disorder symptoms: Panic Disorder Severity Rating Scale (2) social phobia symptoms: Liebowitz Social Anxiety Scale (3) general anxiety: GAD‐7 Secondary outcome: (1) quality of life: Quality of Life Inventory |
| Starting date | 2013, October |
| Contact information | Per Carlbring, Professor, Stockholm University |
| Notes |
Miclea 2014.
| Trial name or title | PAXonline: A randomized controlled trial assessing the efficacy of an Internet‐based cognitive behavior intervention for panic disorder |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Panic Disorder Method of diagnosis: SCID‐IV Age: 18 to 65 years Country of residence: Romania Psychiatric co‐morbidity: included, except severe Depression, Substance Abuse, Personality Disorders, psychotic disorders, mental retardation Co‐use of adjunct therapy: excluded Co‐use of medication: excluded if using benzodiazepines |
| Interventions | Participants randomly assigned to either: (1) Internet‐based CBT with e‐mail support Duration: 16 online modules over 12 weeks Treatment protocol: participants complete online modules on psychoeducation, relaxation, cognitive restructuring, and exposure, with e‐mail and Skype support from a therapist for module exercises Therapists: unknown Therapist contact: feedback and support provided in response to participants' homework completion Face‐to‐face contact: none (2) Unguided Internet‐based CBT Duration: 16 online modules over 12 weeks Treatment protocol: participants complete online modules on psychoeducation, relaxation, cognitive restructuring, and exposure Therapists: unknown Therapist, face‐to‐face contact: none (3) Waiting list control Duration: 12 weeks Therapist, face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 1, 3, 6, and 12 month follow‐ups Primary outcome: (1) panic disorder symptoms: Panic Disorder Severity Rating Scale, Agoraphobic Cognitions Questionnaire, Body Sensations Questionnaire |
| Starting date | May, 2014 |
| Contact information | Mircea Miclea, Babes‐Bolyai University, School of Psychology and Educational Sciences, Department of Psychology 37, Republicii Street, Cluj ‐ Napoca, Cluj, Romania, 400015; Tel: +40 753 529 753; liviugcrisan.neuro@gmail.com |
| Notes |
Richards 2014.
| Trial name or title | |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Generalized Anxiety Disorder Method of Diagnosis: GAD‐7 Age: 18 years or older Country of residence: Ireland Psychiatric co‐morbidity: included Co‐use of adjunct therapy: excluded Co‐use of medication: excluded |
| Interventions | Participants randomly assigned to either: (1) Internet‐based CBT with e‐mail support Duration: 6 online modules completed weekly Treatment protocol: participants complete online CBT modules about the management of GAD with e‐mail support from a therapist Therapists: clinical psychology graduate students at the master's level Therapist contact: 10‐15 min/week Face‐to‐face contact: none (2) Waiting list control Duration: 6 weeks Therapist, face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 3 month follow‐up Primary outcome: (1) general anxiety symptoms: GAD‐7, Penn State Worry Questionnaire Secondary outcome: (1) quality of life: EuroQol 5D, Work and Social Adjustment questionnaire (2) treatment satisfaction: Helpful Aspects of Therapy Form, Satisfaction with Treatment questionnaire |
| Starting date | |
| Contact information | |
| Notes | ISRCTN16303842 |
Rollman 2012.
| Trial name or title | Online treatments for mood and anxiety disorders in primary care |
| Methods | Randomised controlled trial |
| Participants | 18 to 75 years of age Current major depression, panic and/or generalized anxiety disorder on PRIME‐MD Diagnosis: DSM‐IV Panic Disorder, Generalized Anxiety Disorder, or MDD (not included in review) Method of diagnosis: PRIME‐MD Age: 18 to 75 years Country of residence: USA Psychiatric co‐morbidity: included, except Substance Abuse, Psychosis, Bipolar Disorder Co‐use of adjunct therapy: excluded Co‐use of medication: unknown |
| Interventions | Participants randomly assigned to one of: (1) Internet‐based CBT with e‐mail support Duration: unknown Treatment protocol: participants complete online treatment modules for anxiety with weekly e‐mail support from a therapist Therapist, face‐to‐face contact: unknown (2) Internet‐based CBT with e‐mail support and online support group Duration: unknown Treatment protocol: participants complete online treatment modules for anxiety with weekly e‐mail support from a therapist Therapist, face‐to‐face contact: unknown (3) Usual care Duration: unknown Therapist, face‐to‐face contact: variable by type of intervention provided as part of usual care |
| Outcomes |
Timepoints for assessment: pre‐treatment and 6 or 12 month follow‐ups Primary outcome: (1) general anxiety symptoms: Hamilton Rating Scale for Anxiety (2) general anxiety: GAD‐7 Secondary outcome: (1) quality of life: WHO Health and Work Performance Questionnaire, SF‐12 |
| Starting date | 2011, November |
| Contact information | Bruce Rollman, University of Pittsburgh |
| Notes | NCT01482806 |
Titov 2012.
| Trial name or title | A randomized controlled trial of the effects of disorder‐specific vs. trans‐diagnostic and self‐guided vs. guided Internet‐administered treatment on symptoms of social phobia in Australian adults |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: MINI Age: 18 to 64 years Country of residence: Australia Psychiatric co‐morbidity: included, except Psychosis Co‐use of adjunct therapy: excluded Co‐use of medication: included if stable dose for past month |
| Interventions | Participants randomly assigned to one of: (1) Unguided disorder‐specific Internet‐based CBT Duration: 5 online modules over 8 week Treatment protocol: participants complete online treatment modules for social phobia Therapist, face‐to‐face contact: none (2) Unguided Trans‐diagnostic Internet‐based CBT Duration: 5 online modules over 8 week Treatment protocol: participants complete online treatment modules for anxiety and depression Therapist, face‐to‐face contact: none (3) Disorder‐specific Internet‐based CBT with e‐mail or phone support, or both Duration: 5 online modules over 8 week Treatment protocol: participants complete online treatment modules for social phobia with weekly phone or e‐mail support, or both, from a therapist Therapist contact: weekly Face‐to‐face contact: none (4) Trans‐diagnostic Internet‐based CBT with e‐mail or phone support, or both Duration: 5 online modules over 8 week Treatment protocol: participants complete online treatment modules for anxiety and depression with weekly phone or e‐mail support, or both, from a therapist Therapist contact: weekly Face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 6, 12, and 24 month follow‐ups Primary outcome: (1) social phobia symptoms: MINI ‐ Social Phobia Inventory (2) general anxiety: GAD‐7 Secondary outcome: (1) quality of life: Sheehan Disability Scale |
| Starting date | 2012, April |
| Contact information | Nickolai Titov, Centre for Emotional Health, Department of Psychology, Building/Room C3A 724 Macquarie University, North Ryde, NSW 2109 |
| Notes | ACTRN12612000430831 |
Tulbure 2012.
| Trial name or title | Internet treatment for social anxiety disorder in Romania |
| Methods | Randomised controlled trial |
| Participants |
Diagnosis: DSM‐IV Social Phobia Method of diagnosis: SCID‐IV Age: 18 years or older Country of residence: Romania Psychiatric co‐morbidity: included, except Borderline Personality Disorder or Psychosis Co‐use of adjunct therapy: excluded Co‐use of medication: included if stable dose for past month |
| Interventions | Participants randomly assigned to either: (1) Internet‐based CBT with e‐mail support Duration: 9 online modules over 9 weeks Treatment protocol: participants complete online modules on psychoeducation, cognitive restructuring, and exposure, with e‐mail support from a therapist for module exercises Therapist contact: feedback and support provided in response to participants' homework completion Face‐to‐face contact: none (2) Waiting list control Duration: 9 weeks Therapist, face‐to‐face contact: none |
| Outcomes |
Timepoints for assessment: pre‐ and post‐treatment and 6 month follow‐up Primary outcome: (1) social phobia symptoms: Liebowitz Social Anxiety Scale; Social Phobia Inventory; Social Interaction Anxiety Scale; Social Phobia Screening Questionnaire |
| Starting date | April, 2012 |
| Contact information | Bogdan Tudor Tulbure, Babes‐Bolyai University, Cluj ‐ Napoca, Cluj, Romania, 400084; Tel: 0040 745 753061; bogdan.tulbure@ubbcluj.ro |
| Notes |
Differences between protocol and review
Several changes were made to our protocol (Olthuis 2011) during the transition from protocol to full review. They are listed here.
1. In the protocol, we planned to assess the efficacy of a broader range of distance delivery treatments including Internet‐supported CBT and also CBT delivered by phone or videoconferencing. A reviewer commented that these different types of distance delivery were too broad and dissimilar to be included in the same review. As such, we have now focused the review only on Internet‐supported CBT interventions to increase homogeneity across included studies and to improve interpretation of findings. With the exception of the characteristics of the experimental intervention, the protocol remains largely unchanged.
2. In the protocol we stated that 'relaxation' could qualify as a CBT intervention. This was an oversight; on further consideration the review team decided there were significant differences between relaxation alone and the key components of CT, BT, and CBT. Thus, while relaxation could qualify as part of an intervention of interest if it was presented as a component of a more comprehensive CBT package, we did not include therapist‐supported Internet‐based relaxation as an intervention of interest.
3. We originally planned to include quasi‐RCTs, as stated in our protocol. However, the field was more developed than we anticipated. Thus, in order to increase the strength of the evidence within the review, we elected to exclude quasi‐RCTs and include only RCTs.
4. In the original protocol we had designated the first primary outcome as the efficacy of therapist‐supported ICBT in reducing anxiety, as measured by either remission of anxiety disorder diagnosis or reduction in anxiety symptom severity. With respect to the latter, we specified that a reduction in anxiety symptom severity could be indexed by measures of either disorder‐specific anxiety symptoms or anxiety symptoms in general. On further consideration, we decided amalgamating these two types of measures resulted in lost information about the efficacy of the intervention. Thus, in the review we indexed the efficacy of therapist‐supported ICBT in reducing anxiety as measured by (a) remission of anxiety disorder diagnosis, (b) a reduction in disorder‐specific anxiety symptoms, and (c) a reduction in anxiety symptoms in general.
5. The protocol listed our time periods for outcome assessment as short‐term (less than 12 months) and long‐term (12 months or greater). Later, we decided that we wanted to select one time period that would maximize the number of studies that could be included and would be clinically meaningful. Thus, we consolidated our follow‐up assessment to one time point, 6 to 12 months.
6. In the original protocol, we planned to assess dropout and treatment adherence as a secondary outcome. After reviewing the included studies, we observed that so many different methods of indexing dropout were used (e.g., number of participants not completing entire treatment protocol, number of participants not completing 75% of treatment protocol, number of participants not completing follow‐up questionnaires) that combining these measures across studies did not lend itself to any type of meaningful interpretation. As such, rather than examine dropout and treatment adherence as a separate outcome, we elected to assess this outcome via risk of bias and sensitivity analyses. More specifically, in the risk of bias evaluation, we identified studies that did not use an adequate ITT paradigm in their data analytic procedure; then we excluded these studies using sensitivity analyses.
7. We removed the originally planned sensitivity analysis which would have excluded cross‐over trials with carry‐over effects. The inclusion of this sensitivity analysis in our protocol was an oversight as we had elected to only include data from participants before they crossed over to their second treatment condition.
8. In response to suggestions by review editors, we added in a subgroup analysis (by research group) and two sensitivity analyses (exclusion of studies with an active waiting list control; assuming that treatment dropouts were responders on dichotomous outcomes) that were not proposed in the original published protocol.
Contributions of authors
This review was prepared primarily by Dr Olthuis in close collaboration with respect to its content (search criteria, search methods, data analysis and interpretation) with Dr Watt and Dr Stewart. Data extraction and ROB assessment were completed by Dr Olthuis and Ms Bailey. Dr Hayden provided an extensive contribution with respect to Cochrane protocol and methods throughout the review process and the preparation of the review manuscript.
Sources of support
Internal sources
-
Dalhousie University Department of Psychology and Neuroscience and Department of Psychiatry, Canada.
Dr Stewart is supported by the Department of Psychology and Neuroscience and the Department of Psychiatry at Dalhousie University.
-
Saint Francis Xavier University Department of Psychology, Canada.
Dr Watt is supported by the Department of Psychology at Saint Francis Xavier University.
-
Killam Graduate Student Scholarship (Dalhousie University), Canada.
Dr Olthuis's graduate studies at the time of completion of this review were supported by a Killam Graduate Student Scholarship.
-
Dalhousie University Department of Community Health and Epidemiology, Canada.
Dr Hayden is supported by the Department of Community Health and Epidemiology at Dalhousie University for administrative support and office space.
-
Dalhousie University Department of Psychology, Canada.
Ms Bailey is supported by the Department of Psychology at Dalhousie University.
External sources
-
Nova Scotia Health Research Foundation, Canada.
This project was supported by a Knowledge Transfer/Exchange Systematic Review Grant to Dr Watt, Dr Olthuis, and Dr Stewart from the Nova Scotia Health Research Foundation.
-
Canadian Institutes of Health Research, Vanier Canada Graduate Scholarship, Canada.
Dr Olthuis's graduate studies at the time of completion of this review were supported by a Vanier Canada Graduate Scholarship from the Canadian Institutes of Health Research. At the time of review update she was supported by a Canadian Institutes of Health Research Postdoctoral Fellowship.
-
Canadian Institutes of Health Research, Pain in Child Health Initiative, Canada.
Ms Bailey is supported by Pain in Child Health, a strategic training initiative by the Canadian Institutes of Health Research.
-
Nova Scotia Health Research Foundation, Canada.
The Nova Scotia Health Research Foundation provides infrastructure funding to Dr Hayden to support to the Nova Scotia Cochrane Resource Centre.
-
Canadian Chiropractic Research Foundation/Dalhousie University, Canada.
Dr Hayden is supported by a Research Professorship Award from the Canadian Chiropractic Research Foundation.
Declarations of interest
None of the authors have known competing interests.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Andersson 2009 {published data only (unpublished sought but not used)}
- Andersson G, Jonsson U, Malmaeus F, Carlbring P, Waara J, Ost LG. Treatment of specific phobia delivered via the internet vs. one‐session exposure treatment. 32nd Congress of the British Association for Behavioural and Cognitive Psychotherapist (jointly with the European Association of Behavioural and Cognitive Therapies). Manchester, UK, September 2004:166.
- Andersson G, Waara J, Jonsson U, Malmaeus F, Carlbring P, Ost, L. Internet‐based self‐help versus one‐session exposure in the treatment of spider phobia: A randomized controlled trial. Cognitive Behaviour Therapy 2009;38(2):114‐20. [DOI: 10.1080/16506070902931326] [DOI] [PubMed] [Google Scholar]
Andersson 2012a {published data only}
- Andersson G, Carlbring P, Furmark T, on behalf of the SOFIE Research Group. Therapist experience and knowledge acquisition in Internet‐delivered CBT for social anxiety disorder: A randomized controlled trial. PLoS ONE 2012;7:e37411. [DOI: 10.1371/journal.pone.0037411] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G, Paxling B, Wiwe M, Vernmark K, Felix CB, Lundborg L, et al. Therapeutic alliance in guided internet‐delivered cognitive behavioural treatment of depression, generalized anxiety disorder and social anxiety disorder. Behaviour Research and Therapy 2012;50:544‐50. [DOI: 10.1016/j.brat.2012.05.003] [DOI] [PubMed] [Google Scholar]
- Furmark T. Treating social phobia via the Internet: Genetic influences on the response to Internet‐delivered cognitive‐behavior therapy [UMIN000001383]. WHO International Clinical Trials Registry Platform [www.who.int/ictrp] 2008.
Andersson 2012b {published data only}
- Andersson G. Psychodynamic internet treatment versus cognitive behavioral therapy (CBT) for generalized anxiety disorder [NCT01312116]. ClinicalTrials.gov [www.clinicaltrials.gov] 2011.
- Andersson G, Paxling B, Roch‐Norlund P, Ostman G, Norgren A, Almlov J, et al. Internet‐based psychodynamic versus cognitive behavioral guided self‐help for generalized anxiety disorder: A randomized controlled trial. Psychotherapy and Psychosomatics 2012;81:344‐55. [DOI: 10.1159/000339371] [DOI] [PubMed] [Google Scholar]
Andersson 2013 {published data only}
- Andersson G, Warra J, Jonsson U, Malmaeus F, Carlbring P, Ost L‐G. Internet‐based exposure treatment versus one‐session exposure treatment of snake phobia: A randomized controlled trial. Cognitive Behaviour Therapy 2013;42:284‐91. [DOI: 10.1080/1656073.2013.844202] [DOI] [PubMed] [Google Scholar]
Berger 2009 {published data only}
- Berger T, Hohl E, Caspar F. Internet‐based treatment for social phobia: A randomized controlled trial. Journal of Clinical Psychology 2009;65(10):1021‐35. [DOI: 10.1002/jclp.20603] [DOI] [PubMed] [Google Scholar]
- Berger T, Hohl E, Casper F. Internet‐based treatment for social phobia: A 6‐month follow‐up [Internetbasierte therapie der sozialen phobie: Ergebnisse einer 6‐monate‐katamnese]. Zeitschrift fur Klinische Psychologie und Psychotherapie: Forschung und Praxis 2010;39:217‐21. [DOI: 10.1026/1616-3443/a000050] [DOI] [Google Scholar]
- Caspar F. A randomized controlled trial of a web‐based treatment for social phobia [ISRCTN62304985]. ControlledTrials.com [www.controlled‐trials.com] 2007.
Berger 2011 {published data only}
- Berger T, Caspar F, Richardson R, Kneubuhler B, Sutter D, Andersson G. Internet‐based treatment of social phobia: A randomized controlled trial comparing unguided with two types of guided self‐help. Behaviour Research and Therapy 2011;49(3):158‐69. [DOI: 10.1016/j.brat.2010.12.007] [DOI] [PubMed] [Google Scholar]
- Berger T, Casper F. Internet‐based psychotherapeutic interventions for social phobia: How much and what kind of therapeutic contact is needed? [abstract W06‐03]. European Psychiatry [abstracts from the19th European Congress of Psychiatry, EPA 2011, 12‐15 March Vienna Austria] 2011;26(Suppl 1):2207. [Google Scholar]
Berger 2014 {published data only}
- Berger T, Boettcher J, Caspar F. Internet‐based guided self‐help for several anxiety disorders: A randomized controlled trial comparing a tailored with a standardized disorder‐specific approach. Psychotherapy 2014;51:207‐19. [DOI: 10.1037/a0032527] [DOI] [PubMed] [Google Scholar]
Bergstrom 2010 {published data only (unpublished sought but not used)}
- Bergstrom J, Andersson G, Ljotsson B, Ruck C, Andreewitch S, Karlsson A, et al. Internet‐versus group‐administered cognitive behaviour therapy for panic disorder in a psychiatric setting: A randomised trial. BMC Psychiatry 2010;10:54. [DOI: 10.1186/1471-244X-10-54] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alaoui S, Hedman E, Ljotsson B, Bergstrom J, Andersson E, Ruck C, et al. Predictors and moderators of internet‐ and group‐based cognitive beahviour therapy for panic disorder. PLoS One 2013;8:e79024. [DOI: 10.1371/journal.pone.0079024] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindefors N. Internet‐ versus group‐administered cognitive behavior therapy for panic disorder [NCT00845260]. ClinicalTrials.gov [www.clinicaltrials.gov] 2009.
- Lonsdorf TB, Ruck C, Bergstrom J, Andersson G, Ohman A, Lindefors N, et al. The COMTval158met polymorphism is associated with symptoms relief during exposure‐based cognitive‐behavioral treatment in panic disorder. BMC Psychiatry 2010;10:99. [DOI: 10.1186/1471-244X-10-99] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carlbring 2001 {published and unpublished data}
- Carlbring P, Westling BE, Ljungstrand P, Ekselius L, Andersson G. Treatment of panic disorder via the internet: A randomized trial of a self‐help program. Behavior Therapy 2001;32(4):751‐64. [DOI: 10.1016/S0005-7894(01)80019-8] [DOI] [Google Scholar]
Carlbring 2005 {published data only}
- Andersson G, Carlbring P, Grimlund A. Predicting treatment outcome in internet versus face to face treatment of panic disorder. Computers in Human Behavior 2008;24:1790‐801. [DOI: 10.1016/j.chb.2008.02.003] [DOI] [Google Scholar]
- Carlbring P, Nilsson‐Ihrfelt E, Waara J, Kollenstam C, Buhrman M, Kaldo V, et al. Treatment of panic disorder: Live therapy vs. self‐help via the internet. Behaviour Research and Therapy 2005;43(10):1321‐33. [DOI: 10.1016/j.brat.2004.10.002] [DOI] [PubMed] [Google Scholar]
- Carlbring P, Nilsson‐Ihrfelt E, Waara J, Kollenstam C, Burman M, Kaldo V, et al. Treatment of panic disorder: Live therapy vs. self‐help via the Internet. Congress of the British Association for Behavioural and Cognitive Psychotherapies (jointly with the European Association of Behavioural and Cognitive and Therapies). Manchester, UK, September 2004:166.
Carlbring 2006 {published data only (unpublished sought but not used)}
- Almlov J, Carlbring P, Kallqvist K, Paxling B, Cuijpers P, Andersson G. Therapist effects in guided internet‐delivered CBT for anxiety disorders. Behavioural and Cognitive Psychotherapy 2011;39:311‐22. [DOI: 10.1017/S135246581000069X] [DOI] [PubMed] [Google Scholar]
- Carlbring P, Bohman S, Brunt S, Buhrman M, Westling BE, Ekselius L, et al. Remote treatment of panic disorder: A randomized trial of internet‐based cognitive behavior therapy supplemented with telephone calls. American Journal of Psychiatry 2006;163(12):2119‐25. [DOI: 10.1176/appi.ajp.163.12.2119] [DOI] [PubMed] [Google Scholar]
- Nordgreen T, Havik OE, Ost LG, Furmark T, Carlbring P, Andersson G. Outcome predictors in guided and unguided self‐help for social anxiety disorder. Behaviour Research and Therapy 2012;50:13‐21. [DOI: 10.1016/j.brat.2011.10.009] [DOI] [PubMed] [Google Scholar]
Carlbring 2007 {published data only (unpublished sought but not used)}
- Carlbring P, Bergman Nordgren L, Furmark T, Andersson G. Long‐term outcome of Internet‐delivered cognitive‐behavioural therapy for social phobia: A 30‐month follow‐up. Behaviour Research and Therapy 2009;47:848‐50. [DOI: 10.1016/j.brat.2009.06.012] [DOI] [PubMed] [Google Scholar]
- Carlbring P, Bohman S, Brunt S, Buhrman M, Westling BE, Ekselius L, et al. Remote treatment of panic disorder: A randomized trial of internet‐based cognitive behavior therapy supplemented with telephone calls. American Journal of Psychiatry 2006;163:2119‐25. [DOI: 10.1176/appi.ajp.163.12.2119] [DOI] [PubMed] [Google Scholar]
- Carlbring P, Gunnarsdottir M, Hedensjo L, Andersson G, Ekselius L, Furmark T. Treatment of social phobia: Randomised trial of internet‐delivered cognitive‐behavioural therapy with telephone support. British Journal of Psychiatry 2007;190(2):123‐8. [DOI: 10.1192/bjp.bp.105.020107] [DOI] [PubMed] [Google Scholar]
- Nordgreen T, Havik OE, Ost LG, Furmark T, Carlbring P, Andersson G. Outcome predictors in guided and unguided self‐help for social anxiety disorder. Behaviour Research and Therapy 2012;50:13‐21. [DOI: 10.1016/j.brat.2011.10.009] [DOI] [PubMed] [Google Scholar]
Carlbring 2011 {published data only}
- Carlbring P, Maurin L, Torngren C, Linna E, Eriksson T, Sparthan E, et al. Individually‐tailored, internet‐based treatment for anxiety disorders: A randomized controlled trial. Behaviour Research and Therapy 2011;49(1):18‐24. [DOI: 10.1016/j.brat.2010.10.002] [DOI] [PubMed] [Google Scholar]
Furmark 2009a {published data only}
- Furmark T, Carlbring P, Hedman E, Sonnenstein A, Clevberger P, Bohman B, et al. Guided and unguided self‐help for social anxiety disorder: Randomised controlled trial. British Journal of Psychiatry 2009;195(5):440‐7. [DOI: 10.1192/bjp.bp.108.060996] [DOI] [PubMed] [Google Scholar]
- Hedman E, Furmark T, Carlbring P, Ljótsson B, Rück C, Lindefors N, et al. A 5‐year follow‐up of internet‐based cognitive behavior therapy for social anxiety disorder. Journal of Medical Internet Research 2011;13:e39. [DOI: 10.2196/jmir.1776] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindefors N. Five year follow‐up of internet‐based cognitive behaviour therapy (CBT) for social anxiety disorder (SAD) (SOFIE‐5YFU). ClinicalTrials.gov [www.clinicaltrials.gov] 2010.
- Nordgreen T, Havik OE, Ost LG, Furmark T, Carlbring P, Andersson G. Outcome predictors in guided and unguided self‐help for social anxiety disorder. Behaviour Research and Therapy 2012;50:13‐21. [DOI: 10.1016/j.brat.2011.10.009] [DOI] [PubMed] [Google Scholar]
Furmark 2009b {published data only}
- Furmark T, Carlbring P, Hedman E, Sonnenstein A, Clevberger P, Bohman B, et al. Guided and unguided self‐help for social anxiety disorder: Randomised controlled trial. British Journal of Psychiatry 2009;195(5):440‐7. [DOI: 10.1192/bjp.bp.108.060996] [DOI] [PubMed] [Google Scholar]
- Hedman E, Furmark T, Carlbring P, Ljótsson B, Rück C, Lindefors N, et al. A 5‐year follow‐up of internet‐based cognitive behavior therapy for social anxiety disorder. Journal of Medical Internet Research 2011;13:e39. [DOI: 10.2196/jmir.1776] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindefors N. Five year follow‐up of internet‐based cognitive behaviour therapy (CBT) for social anxiety disorder (SAD) (SOFIE‐5YFU) [NCT01145690]. ClinicalTrials.gov [www.clinicaltrials.gov] 2010.
- Nordgreen T, Havik OE, Ost LG, Furmark T, Carlbring P, Andersson G. Outcome predictors in guided and unguided self‐help for social anxiety disorder. Behaviour Research and Therapy 2012;50:13‐21. [DOI: 10.1016/j.brat.2011.10.009] [DOI] [PubMed] [Google Scholar]
Greist 2012 {published data only}
- Greist R, Kobak K. Computer assisted cognitive behavior therapy for obsessive‐compulsive disorder: A comprehensive stepped‐care approach [NCT01522287]. ClinicalTrials.gov [www.clinicaltrials.gov] 2012.
- Kobak KA, Greist R, Jacobi DM, Levy‐Mack H, Greist JH. Computer‐assisted cognitive behavior therapy for obsessive‐compulsive disorder: A randomized trial on the impact of lay vs. professional coaching. Annals of General Psychiatry 2015;14:10. [DOI: 10.1186/s12991-015-0048-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hedman 2011 {published data only}
- Hedman E, Andersson E, Ljotsson B, Andersson G, Ruck C, Lindefors N. Cost‐effectiveness of Internet‐based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: Results from a randomised controlled trial. Behaviour Research and Therapy 2011;49:729‐36. [DOI: 10.1016/j.brat.2011.07.009] [DOI] [PubMed] [Google Scholar]
- Hedman E, Andersson G, Ljotsson B, Andersson E, Ruck C, Mortberg E, et al. Internet‐based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: A randomized controlled non‐inferiority trial. PLoS ONE 2011;6(3):e18001. [DOI: 10.1371/journal.pone.0018001] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman E, Ljotsson B, Andersson G, Andersson E, Schalling M, Lindefors N, et al. Clinical and genetic outcome determinants of Internet‐ and group‐based cognitive behavior therapy for social anxiety disorder. Acta Psychiatrica Scandinavia 2012;126:126‐36. [DOI: 10.1111/j.1600-0447.2012.01834.x] [DOI] [PubMed] [Google Scholar]
- Lindefors N. A comparison between internet therapy and group therapy for social phobia ‐ A trial using cognitive behavioural therapy [NCT00564967]. ClinicalTrials.gov [www.clinicaltrials.gov] 2007.
Ivarsson 2014 {published data only}
- Ivarsson D, Blom M, Hesser H, Carlbring P, Enderby P, Nordberg R, Andersson G. Guided internet‐delivered cognitive behavior therapy for post‐traumatic stress disorder: A randomized controlled trial. Internet Interventions 2014;1:33‐40. [DOI: 10.1016/j.invent.2014.03.002] [DOI] [Google Scholar]
Johnston 2011 {published data only}
- Johnston L, Titov N, Andrews G, Spence J, Dear BF. A RCT of a transdiagnostic internet‐delivered treatment for three anxiety disorders: Examination of support roles and disorder‐specific outcomes. PLoS ONE 2011;6:e28079. [DOI: 10.1371/journal.pone.0028079] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N. Internet‐based treatment of generalized anxiety disorder, and/or social phobia, and/or panic disorder (the Anxiety program): A randomized controlled study exploring the role of a clinician [ACTRN12610000242022]. Australian New Zealand Clinical Trials Registry [ www.anzctr.org.au] 2010, March.
Kiropoulos 2008 {published data only (unpublished sought but not used)}
- Kiropoulos LA, Klein B, Austin DW, Gilson K, Pier C, Mitchell J, et al. Is internet‐based CBT for panic disorder and agoraphobia as effective as face‐to‐face CBT?. Journal of Anxiety Disorders 2008;22(8):1273‐84. [DOI: 10.1016/j.janxdis.2008.01.008] [DOI] [PubMed] [Google Scholar]
- Kiropoulos LA, Klein B, Austin DW, Pier C, Mitchell J. Is internet‐based CBT for panic disorder and agoraphobia as effective as face‐to‐face CBT?. Australian Association for Cognitive and Behaviour Therapy Annual Conference. Manly, Australia, 2006.
Kok 2012 {published data only}
- Kok RN, Straten A, Beekman A, Bosmans J, Neef M, Cuijpers P. Effectiveness and cost‐effectiveness of web‐based treatment for phobic outpatients on a waiting list for psychotherapy: protocol of a randomised controlled trial. BMC Psychiatry 2012;12:131. [DOI: 10.1186/1471-244X-12-131] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok RN, Straten A, Beekman ATF, Cuijpers P. Short‐term effectiveness of web‐based guided self‐help for phobic outpatients: Randomized controlled trial. Journal of Medical Internet Research 2014;16:e226. [DOI: 10.2196/jmir.3429] [DOI] [PMC free article] [PubMed] [Google Scholar]
Newby 2013 {published data only}
- Andrews G. The Wellbeing6 program for anxiety and depression: A randomised controlled trial [ACTRN12611001055998]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2011.
- Dardennes R, Alanbar N, Docteur A, Mirabel‐Sarron C. Minimal clinical contact may contribute to Internet cognitive behavioural therapy (iCBT) efficacy relative to wait‐list control condition [comment]. Psychological medicine 2014;44:1567. [DOI] [PubMed] [Google Scholar]
- Newby JM, Mackenzie A, Williams AD, McIntyre K, Watts S, Wong N, Andrews G. Internet cognitive behavioural therapy for mixed anxiety and depression: A randomized controlled trial and evidence of effectiveness in primary care. Psychological Medicine 2013;43:2635‐48. [DOI: 10.1017/S0033291713000111] [DOI] [PubMed] [Google Scholar]
- Newby JM, Williams AD, Andrews G. Reductions in negative repetitive thinking and metacognitive beliefs during transdiagnostic internet cognitive behavioural therapy (iCBT) for mixed anxiety and depression. Behaviour Research and Therapy 2014;59:52‐60. [DOI: 10.1016/j.brat.2014.05.009] [DOI] [PubMed] [Google Scholar]
Nordgren 2012 {published data only}
- Carlbring P. Internet‐administrated treatment of anxiety disorders (NOVA II) [NCT01390168]. ClinicalTrials.gov [www.clinicaltrials.gov] 2011.
- Nordgren LB, Andersson G, Kadowaki A, Carlbring P. Tailored internet‐administered treatment of anxiety disorders for primary care patients: Study protocol for a randomised controlled trial. Trials 2012;13:16. [DOI: 10.1186/1745-6215-13-16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordgren LB, Hedman E, Etienne J, Bodin J, Kadowaki A, Eriksson S, et al. Effectiveness and cost‐effectiveness of individually tailored Internet‐delivered cognitive behavior therapy for anxiety disorders in a primary care population: A randomized controlled trial. Behaviour Research and Therapy 2014;59:1‐11. [DOI: 10.1016/j.brat.2014.05.007] [DOI] [PubMed] [Google Scholar]
Paxling 2011 {published data only}
- Andersson G, Paxling B, Wiwe M, Vernmark K, Felix CB, Lundborg L, et al. Therapeutic alliance in guided internet‐delivered cognitive behavioural treatment of depression, generalized anxiety disorder and social anxiety disorder. Behaviour Research and Therapy 2012;50:544‐50. [DOI: 10.1016/j.brat.2012.05.003] [DOI] [PubMed] [Google Scholar]
- Paxling B. A randomized clinical trial of internet‐delivered cognitive behaviour therapy for generalized anxiety disorder [UMIN000001353]. WHO International Clinical Trials Registry Platform [www.who.int/ictrp] 2008.
- Paxling B, Almlov J, Dahlin M, Carlbring P, Breitholtz E, Eriksson T, et al. Guided internet‐delivered cognitive behavior therapy for generalized anxiety disorder: A randomized controlled trial. Cognitive Behaviour Therapy 2011;40:159‐73. [DOI: 10.1080/16506073.2011.576699] [DOI] [PubMed] [Google Scholar]
- Paxling B, Lundgren S, Norman A, Almlov J, & Carlbring P. Therapist behaviours in internet‐delivered cognitive behaviour therapy: Analyses of e‐mail correspondence in the treatment of generalized anxiety disorder. Behavioural and Cognitive Psychotherapy 2013;41:280‐9. [DOI: 10.1017/S1352465812000240] [DOI] [PubMed] [Google Scholar]
Richards 2006 {published data only (unpublished sought but not used)}
- Richards JC, Klein B, Austin DW. Internet cognitive behavioural therapy for panic disorder: Does the inclusion of stress management information improve end‐state functioning?. Clinical Psychologist 2006;10(1):2‐15. [DOI: 10.1080/13284200500378795] [DOI] [Google Scholar]
Robinson 2010 {published data only (unpublished sought but not used)}
- Robinson E, Titov N, Andrews G, McIntryre K, Schwencke G, Solley K. Internet treatment for generalized anxiety disorder: A randomized controlled trial comparing clinician vs. technician assistance. PLoS ONE 2010;5(6):e10942. [DOI: 10.1371/journal.pone.0010942] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N. Internet‐based treatment of generalized anxiety disorder (the Worry program): A randomized controlled study exploring the role of a clinician [ACTRN12609000563268]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2009.
Silfvernagel 2012 {published data only}
- Silfvernagel K, Carlbring P, Kabo J, Edström S, Eriksson J, Månson L, et al. Individually tailored Internet‐based treatment for young adults and adults with panic attacks: Randomized controlled trial. Journal of Medical Internet Research 2012;14:e65. [DOI: 10.2196/jmir.1853] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spence 2011 {published data only}
- Spence J, Titov N, Dear BF, Johnston L, Solley K, Lorian C, et al. Randomized controlled trial of internet‐delivered cognitive behavioral therapy for posttraumatic stress disorder. Depression and Anxiety 2011;28:541‐50. [DOI: 10.1002/da.20835] [DOI] [PubMed] [Google Scholar]
Tillfors 2008 {published data only (unpublished sought but not used)}
- Tillfors M, Carlbring P, Furmark T, Lewenhaupt S, Spak M, Eriksson A, et al. Treating university students with social phobia and public speaking fears: Internet delivered self‐help with or without live group exposure sessions. Depression and Anxiety 2008;25(8):708‐17. [DOI: 10.1002/da.20416] [DOI] [PubMed] [Google Scholar]
Titov 2008a {published data only (unpublished sought but not used)}
- Titov N. A randomized controlled study on the effect of Internet based education for treating social phobia using cognitive behavioural techniques [ACTRN12607000235404]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] May 2007.
- Titov N, Andrews G, Johnston L, Schwencke G, Choi I. Shyness programme: Longer term benefits, cost‐effectiveness, and acceptability. Australian and New Zealand Journal of Psychiatry 2009;43:36‐44. [DOI: 10.1080/00048670802534424] [DOI] [PubMed] [Google Scholar]
- Titov N, Andrews G, Schwencke G, Drobny J, Einstein D. Shyness 1: Distance treatment of social phobia over the internet. Australian and New Zealand Journal of Psychiatry 2008;42(7):585‐94. [DOI: 10.1080/00048670802119762] [DOI] [PubMed] [Google Scholar]
- Titov N, Gibson M, Andrews G, McEvoy P. Internet treatment for social phobia reduces comorbidity. Australian and New Zealand Journal of Psychiatry 2009;43:754‐9. [DOI: 10.1080/00048670903001992] [DOI] [PubMed] [Google Scholar]
Titov 2008b {published data only (unpublished sought but not used)}
- Titov N. A comparison of self‐guided Internet based education for social phobia with automatic reminders vs. telephone reminders: A randomized controlled trial [ACTRN12608000465358]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2008.
- Titov N, Andrews G, Johnston L, Schwenke G, Choi I. Shyness programme: Longer term benefits, cost‐effectiveness, and acceptability. Australian and New Zealand Journal of Psychiatry 2009;43:36‐44. [DOI: 10.1080/00048670802534424] [DOI] [PubMed] [Google Scholar]
- Titov N, Andrews G, Schwencke G. Shyness 2: Treating social phobia online: Replication and extension. Australian and New Zealand Journal of Psychiatry 2008;42(7):595‐605. [DOI: 10.1080/00048670802119820] [DOI] [PubMed] [Google Scholar]
- Titov N, Gibson M, Andrews G, McEvoy P. Internet treatment for social phobia reduces comorbidity. Australian and New Zealand Journal of Psychiatry 2009;43:754‐9. [DOI: 10.1080/00048670903001992] [DOI] [PubMed] [Google Scholar]
Titov 2008c {published and unpublished data}
- Titov N. A randomized controlled study on the role of therapist in an Internet‐based treatment program for social phobia using cognitive behavioural techniques [ACTRN12608000192381]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2008.
- Titov N, Andrews G, Choi I, Schwencke G, Mahoney A. Shyness 3: Randomized controlled trial of guided versus unguided internet‐based CBT for social phobia. Australia and New Zealand Journal of Psychiatry 2008;42(12):1030‐40. [DOI: 10.1080/00048670802512107] [DOI] [PubMed] [Google Scholar]
- Titov N, Andrews G, Johnston L, Schwenke G, Choi I. Shyness programme: Longer term benefits, cost‐effectiveness, and acceptability. Australian and New Zealand Journal of Psychiatry 2009;43:36‐44. [DOI: 10.1080/00048670802534424] [DOI] [PubMed] [Google Scholar]
- Titov N, Gibson M, Andrews G, McEvoy P. Internet treatment for social phobia reduces comorbidity. Australian and New Zealand Journal of Psychiatry 2009;43:754‐9. [DOI: 10.1080/00048670903001992] [DOI] [PubMed] [Google Scholar]
Titov 2009 {published data only (unpublished sought but not used)}
- Lorian CN, Titov N, Grisham JR. Changes in risk‐taking over the course of an Internet‐delivered cognitive behavioral treatment for generalized anxiety disorder. Journal of Anxiety Disorders 2012;26:140‐9. [DOI: 10.1016/j.janxdis.2011.10.003] [DOI] [PubMed] [Google Scholar]
- Titov N. Internet‐based education for generalized anxiety disorder (the Worry Program): A randomized controlled trial [ACTRN12609000136202]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2009.
- Titov N, Andrews G, Robinson E, Schwencke G, Johnston L, Solley K, et al. Clinician‐assisted internet‐based treatment is effective for generalized anxiety disorder: Randomized controlled trial. Australian and New Zealand Journal of Psychiatry 2009;43(10):905‐12. [DOI: 10.1080/00048670903179269] [DOI] [Google Scholar]
Titov 2010 {published data only}
- Andrews G. A randomized controlled trial of Internet based education for social phobia, panic disorder (with or without agoraphobia), and generalised anxiety disorder, comparing immediate education versus delayed education groups on severity of symptoms of anxiety [ACTRN12611000625976]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2011.
- Titov N, Andrews G, Johnston L, Robinson E, Spence J. Transdiagnostic internet treatment for anxiety disorders: A randomized controlled trial. Behaviour Research and Therapy 2010;48(9):890‐9. [DOI: 10.1016/j.brat.2010.05.014] [DOI] [PubMed] [Google Scholar]
Titov 2010 GAD {published data only}
- Titov N, Andrews G, Johnston L, Robinson E, Spence J. Transdiagnostic internet treatment for anxiety disorders: A randomized controlled trial. Behaviour Research and Therapy 2010;48:890‐9. [DOI: 10.1016/j.brat.2010.05.014] [DOI] [PubMed] [Google Scholar]
Titov 2010 Panic {published data only}
- Titov N, Andrews G, Johnston L, Robinson E, Spence J. Transdiagnostic internet treatment for anxiety disorders: A randomized controlled trial. Behaviour Research and Therapy 2010;48:890‐9. [DOI: 10.1016/j.brat.2010.05.014] [DOI] [PubMed] [Google Scholar]
Titov 2010 Social Phobia {published data only}
- Titov N, Andrews G, Johnston L, Robinson E, Spence J. Transdiagnostic internet treatment for anxiety disorders: A randomized controlled trial. Behaviour Research and Therapy 2010;48:890‐9. [DOI: 10.1016/j.brat.2010.05.014] [DOI] [PubMed] [Google Scholar]
Titov 2011 {published data only}
- Dear BF, Titov N, Schwencke G, Andrews G, Johnston L, Craske MG, et al. An open trial of a brief transdiagnostic internet treatment for anxiety and depression [ACTRN12610000555055]. Behaviour Research and Therapy 2011;49(12):830‐7. [DOI] [PubMed] [Google Scholar]
- Titov N. The Wellbeing Program: A randomized controlled trial of internet‐based treatment of anxiety and depression [ACTRN12610000247077]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2010.
- Titov N, Dear BF, Schwencke G, Andrews G, Johnston L, Craske MG, et al. Transdiagnostic internet treatment for anxiety and depression: A randomised controlled trial. Behaviour Research and Therapy 2011;49:441‐52. [DOI: 10.1016/j.brat.2011.03.007] [DOI] [PubMed] [Google Scholar]
van Ballegooijen 2013 {published data only}
- Ballegooijen W, Riper H, Klein B, Ebert DD, Kramer J, Meulenbeek P, Cuijpers P. An Internet‐based guided self‐help intervention for panic symptoms: Randomized controlled trial. Journal of Medical Internet Research 2013;15:e154. [NTR1639] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballegooijen W, Riper H, Straten A, Kramer J, Conijn B, Cuijpers P. The effects of an Internet based self‐help course for reducing panic symptoms ‐ Don't Panic Online: Study protocol for a randomised controlled trial. Trials 2011;12:75. [DOI: 10.1186/1745-6215-12-75] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wims 2010 {published data only (unpublished sought but not used)}
- Wims E. The effectiveness of clinician assisted internet based cognitive behaviour therapy for panic disorder [ACTRN12608000548336]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2008, October.
- Wims E, Titov N, Andrews G, Choi I. Clinician‐assisted internet‐based treatment is effective for panic: A randomized controlled trial. Australian and New Zealand Journal of Psychiatry 2010;44(7):599‐607. [DOI: 10.3109/00048671003614171] [DOI] [PubMed] [Google Scholar]
Wootton 2013 {published data only}
- Wootton BM, Dear BF, Johnston L, Terides MD, Titov N. Remote treatment of obsessive‐compulsive disorder: A randomized controlled trial. Journal of Obessive‐Compulsive and Related Disorders 2013;2:375‐84. [DOI: 10.1016/j.jocrd.2013.07.002] [DOI] [Google Scholar]
References to studies excluded from this review
Andersson 2006 {published data only}
- Andersson G, Carlbring P, Holmström A, Sparthan E, Furmark T, Nilsson‐Ihrfelt E, et al. Internet‐based self‐help with therapist feedback and in vivo group exposure for social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology 2006;74:677‐86. [DOI: 10.1037/0022-006X.74.4.677] [DOI] [PubMed] [Google Scholar]
Andersson 2012c {published data only}
- Andersson E, Enander J, Andren P, Hedman E, Ljotsson B, Hursti T, et al. Internet‐based cognitive behaviour therapy for obsessive‐compulsive disorder: A randomized controlled trial. Psychological Medicine 2012;42:2193‐203. [DOI: 10.1017/S0033291712000244] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson E, Hedman E, Ljotsson B, Wikstrom M, Elveling E, Lindefors N, et al. Cost‐effectiveness of internet‐based cognitive behavior therapy for obsessive‐compulsive disorder: Results from a randomized controlled trial. Journal of obsessive‐compulsive and related disorders 2015;4:47‐53. [Google Scholar]
- Andersson E, Ljotsson B, Hedman E, Enander J, Kaldo V, Andersson G, et al. Predictors and moderators of Internet‐based cognitive behavior therapy for obsessive‐compulsive disorder: Results from a randomized trial. Journal of obsessive‐compulsive and related disorders 2015;4:1‐7. [Google Scholar]
- Andersson E, Steneby S, Karlsson K, Ljotsson B, Hedman E, Enander J, et al. Long‐term efficacy of Internet‐based cognitive behavior therapy for obsessive‐compulsive disorder with or without booster: A randomized controlled trial. Psychological Medicine 2014;44:2877‐87. [DOI] [PubMed] [Google Scholar]
- Ruck C. Internet‐based cognitive behavior therapy (CBT) for obsessive compulsive disorder (OCD) [NCT01347099]. ClinicalTrials.gov [www.clinicaltrials.gov] 2011.
Andrews 2011 {published data only}
- Andrews G. In patients seeking treatment for social phobia internet cognitive behaviour therapy will be compared with face to face cognitive behaviour therapy on the reduction in social phobia scores [ACTRN12611000626965]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] June 2011.
- Andrews G, Davies M, Titov N. Effectiveness randomized controlled trial of face to face versus Internet cognitive behaviour therapy for social phobia. Australian and New Zealand Journal of Psychiatry 2011;45:337‐40. [DOI: 10.3109/00048674.2010.538840] [DOI] [PubMed] [Google Scholar]
Andrews 2011b {published data only}
- Andrews G. A randomised controlled trial comparing clinician‐assisted Internet based treatment for panic disorder with or without agoraphobia vs. a waitlist control on severity of symptoms of panic [ACTRN12611001120965]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2011.
Andrews 2012a {published data only}
- Andrews G. A randomised controlled trial comparing clinician‐assisted Internet based treatment for Obsessive Compulsive Disorder (OCD) vs. a waitlist control condition on severity of symptoms of OCD [ACTRN12612001073897]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2012.
Andrews 2012b {published data only}
- Andrews G. The Obsessive Compulsive Disorder (OCD) Program: A randomised controlled trial of online versus face‐to‐face cognitive behavioural therapy (CBT) [ACTRN12612001306808]. Australian New Zealand Clinical Trials Registry [www.anzctr.org.au] 2012.
Bell 2012 {published data only}
- Bell CJ, Colhoun HC, Carter FA, Frampton CM. Effectiveness of computerised cognitive behaviour therapy for anxiety disorders in secondary care. Australian and New Zealand Journal of Psychiatry 2012;46:630‐40. [DOI: 10.1177/0004867412437345] [DOI] [PubMed] [Google Scholar]
Berger 2012 {published data only}
- Berger M. Internet‐based treatment for obsessive‐compulsive disorder – acceptance and effectiveness [DRKS00004612]. German Clinical Trials Register [www.germanctr.de] 2012.
Carlbring 2003 {published data only}
- Carlbring P, Ekselius L, Andersson G. Treatment of panic disorder via the internet: A randomized trial of CBT vs. applied relaxation. Journal of Behavior Therapy 2003;34(2):129‐40. [DOI: 10.1016/S0005-7916(03)00026-0] [DOI] [PubMed] [Google Scholar]
Carlbring 2010 {published data only}
- Carlbring P. Treatment of social phobia over the internet (SOFIE‐8) [NCT01312571]. ClinicalTrials.gov [www.clinicaltrials.gov] 2010, August.
Carlbring 2011b {published data only}
- Carlbring P, Maurin T, Sjomark J, Maurin L, Westling BE, Ekselius L, et al. All at once or one at a time? A randomized controlled trial comparing two ways to deliver bibliotherapy for panic disorder. Cognitive Behaviour Therapy 2011;40:228‐35. [DOI: 10.1080/16506073.2011.553629] [DOI] [PubMed] [Google Scholar]
Cunningham 2006 {published data only}
- Cunningham V, Lefkoe M, Sechrest L. Eliminating fears: An intervention that permanently eliminates the fear of public speaking. Clinical Psychology & Psychotherapy 2006;13:183‐93. [DOI: 10.1002/cpp.487] [DOI] [Google Scholar]
Dear 2015 {published data only}
- Dear BF, Zou JB, Ali S, Lorian CN, Johnston L, et al. Clinical and cost‐effectiveness of therapist‐guided Internet‐delivered cognitive behavior therapy for older adults with symptoms of anxiety: A randomized controlled trial. Behavior Therapy 2015;46:206‐17. [DOI: 10.1016/j.beth.2014.09.007] [DOI] [PubMed] [Google Scholar]
Ellis 2011 {published data only}
- Ellis LA, Campbell AJ, Sethi S, O'Dea BM. Comparative randomized trial of an online cognitive‐behavioral therapy program and an online support group for depression and anxiety. Journal of CyberTherapy and Rehabilitation 2011;4:461‐7. [Google Scholar]
Febbraro 2005 {published data only}
- Febbraro GAR. An investigation into the effectiveness of bibliotherapy and minimal contact interventions in the treatment of panic attacks. Journal of Clinical Psychology 2005;61:763‐79. [DOI: 10.1002/jclp.20097] [DOI] [PubMed] [Google Scholar]
Gilson 2006 {published data only}
- Gilson K, Pier C, Austin DW, Mitchell J, Schattner P, Pierce D, et al. Evaluation of internet‐based cognitive behavioural therapy for panic disorder in general medical practice. 29th Australian Association for Cognitive and Behaviour Therapy Annual Conference. Manly, Australia, October 2006.
Greist 2002 {published data only}
- Greist JH, Marks IM, Baer L, Kobak KA, Wenzel KW, Hirsch MJ, et al. Behavior therapy for obsessive‐compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. Journal of Clinical Psychiatry 2002;63:138‐45. [DOI: 10.4088/JCP.v63n0209] [DOI] [PubMed] [Google Scholar]
Kenardy 2003 {published data only}
- Kenardy JA, Dow MGT, Johnston DW, Newman MG, Thomson A, Taylor CB. A comparison of delivery methods of cognitive‐behavioral therapy for panic disorder: An international multicenter trial. Journal of Consulting and Clinical Psychology 2003;71:1068‐75. [DOI: 10.1037/0022-006X.71.6.1068] [DOI] [PubMed] [Google Scholar]
Kenwright 2005 {published data only}
- Kenwright M, Marks I, Graham C, Franses A, Mataix‐Cols D. Brief scheduled phone support from a clinician to enhance computer‐aided self‐help for obsessive‐compulsive disorder: Randomized controlled trial. Journal of Clinical Psychology 2005;61:499‐508. [DOI: 10.1002/jclp.20204] [DOI] [PubMed] [Google Scholar]
Klein 2001 {published data only}
- Klein B, Richards JC. A brief internet‐based treatment for panic disorder. Behavioural and Cognitive Psychotherapy 2001;29:113‐7. [DOI: 10.1017/S1352465801001138] [DOI] [Google Scholar]
Klein 2006 {published data only}
- Klein B, Richards JC, Austin DW. Efficacy of internet therapy for panic disorder. Journal of Behavior Therapy and Experimental Psychiatry 2006;37:213‐38. [DOI: 10.1016/j.jbtep.2005.07.001] [DOI] [PubMed] [Google Scholar]
Klein 2009 {published data only}
- Klein B, Austin D, Pier C, Kiropoulos L, Shandley K, Mitchell J, et al. Internet‐based treatment for panic disorder: Does frequency of therapist contact make a difference?. Cognitive Behaviour Therapy 2009;38:100‐13. [DOI: 10.1080/16506070802561132] [DOI] [PubMed] [Google Scholar]
Knaevelsrud 2007 {published data only}
- Knaevelsrud C, Maercker A. Internet‐based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: A randomized controlled clinical trial. BMC Psychiatry 2007;7:13. [DOI: 10.1186/1471-244X-7-13] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lange 2001 {published data only}
- Lange A, Ven JP, Schrieken B, Emmelkamp PM. Interapy. Treatment of posttraumatic stress through the Internet: A controlled trial. Journal of Behavior Therapy and Experimental Psychiatry 2001;32:73‐90. [DOI: 10.1016/S0005-7916(01)00023-4] [DOI] [PubMed] [Google Scholar]
Lange 2003 {published data only}
- Lange A, Rietdijk D, Hudcovicova M, Ven JP, Schrieken B, Emmelkamp PM. Interapy: A controlled randomized trial of the standardized treatment of posttraumatic stress through the Internet. Journal of Consulting and Clinical Psychology 2003;71:901‐9. [DOI: 10.1037/0022-006X.71.5.901] [DOI] [PubMed] [Google Scholar]
Litz 2007 {published data only}
- Bruner V, Gore K, DeDeyn J, Jaffer A, Litz B, Bryant R. A therapist‐guided internet‐based self‐management approach to post‐traumatic stress after military events. International Society for Traumatic Stress Studies. New Orleans, LA, November 2004.
- Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof‐of‐concept trial of an internet‐based, therapist‐assisted self‐management treatment for posttraumatic stress disorder. American Journal of Psychiatry 2007;164(11):1676‐83. [DOI: 10.1176/appi.ajp.2007.06122057] [DOI] [PubMed] [Google Scholar]
Lopez 2014 {published data only}
- Lopez GC, Arbona CB, Castellano SQ, Gomez AR, Rivera RMB. Telepsychology program to treat public‐speaking anxiety among the Mexican population. Psicología Iberoamericana 2014;22:45‐54. [Google Scholar]
Marks 2004 {published data only}
- Marks IM, Kenwright M, McDonough M, Whittaker M, Mataix‐Cols D. Saving clinicians' time by delegating routine aspects of therapy to a computer: A randomized controlled trial in phobia/panic disorder. Psychological Medicine 2004;34:9‐17. [DOI: 10.1017/S003329170300878X] [DOI] [PubMed] [Google Scholar]
Newman 1997 {published data only}
- Newman MG, Kenardy J, Herman S, Taylor CB. Comparison of palmtop‐computer‐assisted brief cognitive‐behavioral treatment to cognitive‐behavioral treatment for panic disorder. Journal of Consulting and Clinical Psychology 1997;65:178‐83. [DOI: 10.1037/0022-006X.65.1.178] [DOI] [PubMed] [Google Scholar]
Pittaway 2009 {published data only}
- Pittaway S, Cupitt C, Palmer D, Arowobusoye N, Milne R, Holttum S, et al. Comparative, clinical feasibility study of three tools for delivery of cognitive behavioural therapy for mild to moderate depression and anxiety provided on a self‐help basis. Mental Health in Family Medicine 2009;6:145‐54. [PMC free article] [PubMed] [Google Scholar]
Ruwaard 2010 {published data only}
- Ruwaard J, Broeksteeg J, Schrieken B, Emmelkamp P, Lange A. Web‐based therapist‐assisted cognitive behavioral treatment of panic symptoms: A randomized controlled trial with a three‐year follow‐up. Journal of Anxiety Disorders 2010;24:387‐96. [DOI: 10.1016/j.janxdis.2010.01.010] [DOI] [PubMed] [Google Scholar]
Saul 2007 {published data only}
- Saul JE. A comparison of Internet‐based versus face‐to‐face cognitive behavioral therapy for snake phobia. Dissertation Abstracts International 2007;67:6077. [Google Scholar]
Schneider 2005 {published data only}
- Schneider AJ, Mataix‐Cols D, Marks IM, Bachofen M. Internet‐guided self‐help with or without exposure therapy for phobic and panic disorders. Psychotherapy and Psychosomatics 2005;74:154‐64. [DOI: 10.1159/000084000] [DOI] [PubMed] [Google Scholar]
Shandley 2008 {published data only}
- Shandley K, Austin DW, Klein B, Pier C, Schattner P, Pierce D, et al. Therapist‐assisted, Internet‐based treatment for panic disorder: Can general practitioners achieve comparable patient outcomes to psychologists?. Journal of Medical Internet Research 2008;10:65‐79. [DOI: 10.2196/jmir.1033] [DOI] [PMC free article] [PubMed] [Google Scholar]
Titov 2009b {published data only}
- Titov N, Andrews G, Schwencke G, Solley K, Johnston L, Robinson E. An RCT comparing effect of two types of support on severity of symptoms for people completing Internet‐based cognitive behaviour therapy for social phobia. Australian and New Zealand Journal of Psychiatry 2009;43:920‐6. [DOI: 10.1080/00048670903179228] [DOI] [Google Scholar]
van Straten 2008 {published data only}
- Straten A, Cuijpers P, Smits N. Effectiveness of a web‐based self‐help intervention for symptoms of depression, anxiety, and stress: Randomized controlled trial. Journal of Medical Internet Research 2008;10:e7. [DOI: 10.2196/jmir.954] [DOI] [PMC free article] [PubMed] [Google Scholar]
von Essen 2008 {published data only}
- Essen L. Treatment of posttraumatic stress disorder among parents of children with cancer with cognitive behavioural therapy over the Internet. Pediatric Blood Cancer 2008;50:9. [Google Scholar]
Wagner 2012 {published data only}
- Wagner B, Brand J, Schulz W, Knaevelsrud C. Online working alliance predicts treatment outcome for posttraumatic stress symptoms in Arab war‐traumatized patients. Depression and Anxiety 2012;29:646‐51. [DOI: 10.1002/da.21962] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Schreuders 2008 {published data only}
- Schreuders B. Phobias under control. Internet‐based guided self‐help for treatment of social, agora‐, or specific phobia(s): a pilot trial [NTR1260]. Nederlands Trial Register [www.trialregister.nl/trialreg/] 2008.
Tabari 2013 {published data only (unpublished sought but not used)}
- Tabari NA. Cognitive behavioural therapy (CBT) via email in general anxiety disorder. CNS spectrums [abstracts of the Neuroscience Education Institute]. Colorado Springs, CO: NEI Psychopharmacology Congress, 2013 Nov 14‐17.
References to ongoing studies
Bishop 2012 {published data only}
- Bishop TM, Possemato K, Acosta M, Lantinga LJ, Maisto S, Marsch L, et al. Moving forward: Update on the development of a web‐based cognitive behavioral treatment for OEF/OIF veterans with PTSD symptoms and substance misuse [abstract]. Alcoholism: Experimental and Clinical Research 2012;36:347A. [Google Scholar]
Carlbring 2012 {published data only}
- Carlbring P. Internet‐based treatment of generalized anxiety disorder [NCT01570374]. ClinicalTrials.gov [www.clinicaltrials.gov] 2012.
Clark 2012 {published data only}
- Clark DM. Internet‐based cognitive therapy for social anxiety disorder [ISRCTN95458747]. Controlled Trials.com [www.controlled‐trials.com] 2012.
Lindner 2013 {published data only}
- Carlbring P. ACT‐smart: Smartphone‐supplemented iCBT for social phobia and/or panic disorder [NCT01963806]. ClinicalTrials.gov 2013.
- Lindner P, Ivanova E, Ly KH, Andersson G, & Carlbring P. Guided and unguided CBT for social anxiety disorder and/or panic disorder via the Internet and a smartphone application: Study protocol for a randomised controlled trial. Trials 2013;14:437. [10.1186/1745‐6215‐14‐437] [DOI] [PMC free article] [PubMed] [Google Scholar]
Miclea 2014 {published data only}
- Miclea M. PAXonline: A randomized controlled trial assessing the efficacy of an Internet‐based cognitive behavior intervention for Panic Disorder [ACTRN12614000547640]. Australian New Zealand Clinical Trials Registry 2014.
Richards 2014 {published data only}
- Richards D. Internet delivered treatment for generalized anxiety symptoms in students [ISRCTN16303842]. ISRCTN Registry [www.isrctn.com] 2013.
- Richards D, Timulak L, Doherty G, Sharry J, McLoughlin O, Rashleigh C, et al. Low‐intensity internet‐delivered treatment for generalized anxiety symptoms in routine care: protocol for a randomized controlled trial. Trials 2014;15:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rollman 2012 {published data only}
- Rollman B. Online treatments for mood and anxiety disorders in primary care [NCT01482806]. ClinicalTrials.gov [http://clinicaltrials.gov] 2011.
Titov 2012 {published data only}
- Titov N. A randomized controlled trial of the effects of disorder‐specific vs. trans‐diagnostic and self‐guided vs. guided Internet‐administered treatment on symptoms of social phobia in Australian adult [ACTRN12612000430831]. Australia New Zealand Clinical Trial Registry 2012.
Tulbure 2012 {published data only}
- Tudor TB. Internet treatment for social phobia (iSOFIE‐Ro) [NCT01557894]. ClinicalTrials.gov [www.clinicaltrials.gov] 2012.
- Tulbure BT, Mansson KNT, Andersson G. Internet treatment for social anxiety disorder in Romania: Study protocol for a randomized controlled trial. Trials 2012;13:202. [DOI: 10.1186/1745-6215-13-202] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Acarturk 2009
- Acarturk C, Smit F, Graaf R, Straten A, Have M, Cuijpers P. Economic costs of social phobia: A population‐based study. Journal of Affective Disorders 2009;115:421‐9. [DOI: 10.1016/j.jad.2008.10.008] [DOI] [PubMed] [Google Scholar]
Alvidrez 1999
- Alvidrez J, Azocar F. Distressed women's clinic patients: preferences for mental health treatments and perceived obstacles. General Hospital Psychiatry 1999;21(5):340‐7. [DOI] [PubMed] [Google Scholar]
Andersson 2007
- Andersson G, Cuijpers P, Carlbring P, Lindefors N. Effects of internet‐delivered cognitive behaviour therapy for anxiety and mood disorders. Review Series: Psychiatry 2007;9:9‐14. [Google Scholar]
Andersson 2009b
- Andersson G. Using the internet to provide cognitive behaviour therapy. Behaviour Research and Therapy 2009;47:175‐80. [DOI: 10.1016/j.brat.2009.01.010] [DOI] [PubMed] [Google Scholar]
Andersson 2012
- Andersson G, Carlbring P, Furmark T. Therapist experience and knowledge acquisition in internet‐delivered CBT for social anxiety disorder: a randomized controlled trial. PLoS ONE 2012;7:e37411. [DOI: 10.1371/journal.pone.0037411] [DOI] [PMC free article] [PubMed] [Google Scholar]
Andrews 2010
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable, and practical health care: A meta‐analysis. PLoS ONE 2010;5:e13196. [DOI: 10.1371/journal.pone.0013196] [DOI] [PMC free article] [PubMed] [Google Scholar]
APA 1980
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd Edition. Washington, DC: American Psychiatric Association, 1980. [Google Scholar]
APA 1987
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd Edition. Washington, DC: American Psychiatric Association, 1987. [Google Scholar]
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual. 4th Edition. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
APA 2000
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
Attkisson 1982
- Attkisson CC, Zwick R. The client satisfaction questionnaire: Psychometric properties and correlations with service utilization and psychotherapy outcome. Evaluation and Program Planning 1982;5(3):233‐7. [DOI] [PubMed] [Google Scholar]
Barak 2008
- Barak A, Hen L, Boniel‐Nissim M, Shapira N. A comprehensive review and a meta‐analysis of the effectiveness of internet‐based psychotherapeutic interventions. Journal of Technology in Human Services 2008;26:109‐60. [DOI: 10.1080/15228830802094429] [DOI] [Google Scholar]
Barlow 1988
- Barlow DH. Anxiety and its disorders: the nature and treatment of anxiety and panic. New York: Guilford Press, 1988. [Google Scholar]
Batelaan 2007
- Batelaan N, Smit F, Graaf R, Balkom A, Vollebergh W, Beekman A. Economic costs of full‐blown and subthreshold panic disorder. Journal of Affective Disorders 2007;104:127‐36. [DOI: 10.1016/j.jad.2007.03.013] [DOI] [PubMed] [Google Scholar]
Beck 1979
- Beck AT, Rush AJ, Shaw BF, Emergy G. Cognitive therapy of depression. New York: The Guilford Press, 1979. [Google Scholar]
Beck 1991
- Beck A, Steer R. Beck Anxiety Inventory manual. San Antonio, TX: The Psychological Corporation, 1991. [Google Scholar]
Beck 2005
- Beck AT, Emery G. Anxiety disorders and phobias: A cognitive perspective. New York: Basic Books, 2005. [Google Scholar]
Bee 2008
- Bee PE, Bower P, Lovell K, Gilbody S, Richards D, Gask L, et al. Psychotherapy mediated by remote communication technologies: a meta‐analytic review. BMC Psychiatry 2008;8:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bisson 2007
- Bisson J, Andrew M. Psychological treatment of post‐traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD003388.pub3] [DOI] [PubMed] [Google Scholar]
Borenstein 2009
- Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta‐analysis. Hoboken, NJ: John Wiley & Sons, Ltd, 2009. [Google Scholar]
Bruce 2005
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, et al. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12‐year prospective study. American Journal of Psychiatry 2005;162(6):1179‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buffett‐Jerrot 2002
- Buffett‐Jerrott SE, Stewart SH. Cognitive and sedative effects of benzodiazepine use. Current Pharmaceutical Design 2002;8(1):45‐58. [DOI] [PubMed] [Google Scholar]
Casey 2004
- Casey LM, Oei TPS, Newcombe PA. An integrated cognitive model of panic disorder: The role of positive and negative cognitions. Clinical Psychology Review 2004;24:529‐55. [DOI: 10.1016/j.cpr.2004.01.005] [DOI] [PubMed] [Google Scholar]
Choy 2007
- Choy Y. Managing side effects of anxiolytics. Primary Psychiatry 2007;14(7):68‐76. [Google Scholar]
Clark 1986
- Clark DM. A cognitive approach to panic. Behaviour Research and Therapy 1986;24(4):461‐70. [DOI] [PubMed] [Google Scholar]
Cuijpers 2009
- Cuijpers P, Marks IM, Straten A, Cavanagh K, Gega L, Andersson G. Computer‐aided psychotherapy for anxiety disorders: A meta‐analytic review. Cognitive Behaviour Therapy 2009;38:66‐82. [DOI: 10.1080/16506070802694776] [DOI] [PubMed] [Google Scholar]
Cuijpers 2010
- Cuijpers P, Donker T, Straten A, Li J, Andersson G. Is guided self‐help as effective as face‐to‐face psychotherapy for depression and anxiety disorders? A systematic review and meta‐analysis of comparative outcome studies. Psychological Medicine 2010;40:1942‐57. [DOI: 10.1017/S0033291710000772] [DOI] [PubMed] [Google Scholar]
Deacon 2004
- Deacon BJ, Abramowitz JS. Cognitive and behavioral treatments for anxiety disorders: a review of meta‐analytic findings. Journal of Clinical Psychology 2004;60(4):429‐41. [DOI] [PubMed] [Google Scholar]
Department of Health 2008
- Department of Health. Improving Access to Psychological Therapies Implementation Plan: National Guidelines for Regional Delivery. London: DoH, 2008. [Google Scholar]
DiNardo 1994
- DiNardo P, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM‐IV. Anxiety Disorders Interview Schedule for DSM‐IV. San Antonio, TX: The Psychological Corporation, 1994. [Google Scholar]
Dugas 2007
- Dugas MJ, Robichaud M. Cognitive‐behavioral treatment for generalized anxiety disorder: From science to practice. New York: Routledge, 2007. [Google Scholar]
DuPont 1996
- DuPont RL, Rice DP, Miller LS, Shiraki SS, Rowland CR, Harwood HJ. Economic costs of anxiety disorders. Anxiety 1996;2:167‐72. [DOI] [PubMed] [Google Scholar]
Ehlers 2000
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy 2000;38:319‐45. [DOI] [PubMed] [Google Scholar]
ESEMeD/MHEDEA 2000 Investigators 2004
- The ESEMeD/MHEDEA 2000 Investigators. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica 2004;109 Suppl 420:21‐7. [DOI] [PubMed] [Google Scholar]
First 2002
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM‐IV‐TR Axis I Disorders, Research Version, Patient Edition (SCID‐I/P). New York: Biometrics Research, New York State Psychiatric Institute, 2002. [Google Scholar]
Foa 2010
- Foa EB. Cognitive behavioral therapy of obsessive‐compulsive disorder. Dialogues in Clinical Neuroscience 2010;12(2):199‐207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frisch 1992
- Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the quality of life inventory: A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment 1992;4:92‐101. [Google Scholar]
Goodman 1989
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale‐Brown Obsessive Compulsive Scale, I: Development, use, and reliability. Archives of General Psychiatry 1989;46(11):1006‐11. [DOI] [PubMed] [Google Scholar]
Greenberg 1999
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JRT, et al. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry 1999;60:427‐35. [DOI: 10.4088/JCP.v60n0702] [DOI] [PubMed] [Google Scholar]
Gureje 2006
- Gureje O, Lasebikan VO, Kola L, Makanjuola VA. Lifetime and 12‐month prevalence of mental disorders in the Nigerian Survey of Mental Health and Well‐Being. British Journal of Psychiatry 2006;188(5):465‐71. [DOI] [PubMed] [Google Scholar]
Guy 1976
- Guy W. ECDEU assessment manual for psychopharmacology. Rockville, MD: US Department of Health Education and Welfare, 1976. [Google Scholar]
Hahlweg 2001
- Hahlweg K, Fiegenbaum W, Frank M, Schroeder B, Witzleben I. Short‐ and long‐term effectiveness of an empirically supported treatment for agoraphobia. Journal of Consulting and Clinical Psychology 2001;69:375‐82. [DOI: 10.1037/0022-006X.69.3.375] [DOI] [PubMed] [Google Scholar]
Hambrick 2003
- Hambrick JP, Turk CL, Heimberg RG, Schneier FR, Liebowitz MR. The experience of disability and quality of life in social anxiety disorder. Depression and Anxiety 2003;18:46‐50. [DOI: 10.1002/da.10110] [DOI] [PubMed] [Google Scholar]
Hamilton 1959
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology 1959;32:50‐5. [DOI] [PubMed] [Google Scholar]
Hauenstein 2006
- Hauenstein EJ, Petterson S, Merwin E, Rovnyak V, Heise B, Wagner D. Rurality, gender, and mental health treatment. Family and Community Health 2006;29(3):169‐85. [DOI] [PubMed] [Google Scholar]
Health Canada 2002
- Health Canada. A report on mental illness in Canada. www.phac‐aspc.gc.ca/publicat/miic‐mmac/index.html. Ottawa, ON: Health Canada Editorial Board, (accessed 25 March 2008).
Heimberg 2002
- Heimberg RG. Cognitive‐behavioral therapy for social anxiety disorder: current status and future directions. Biological Psychiatry 2002;51(1):101‐8. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins J, Thompson S. Quantifying heterogeneity in a meta‐analysis. Statistical Medicine 2002;21(11):1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, White IR, Anzures‐Cabrera J. Meta‐analysis of skewed data: Combining results reported on log‐transformed or raw scales. Statistics in Medicine 2008;27:6072‐92. [DOI: 10.1002/sim.3427] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Review of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochranehandbook.org. The Cochrane Collaboration.
Higgins 2011b
- Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI: 10.1136/bmj.d5928] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hunot 2007
- Hunot V, Churchill R, Teixeira V, Silva de Lima M. Psychological therapies for generalised anxiety disorder. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD001848.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kessler 2004
- Kessler RC, McGonagle KA, Zhoa S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12‐month prevalence of DSM‐III‐R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry 1994;51:8‐19. [DOI: 10.1001/archpsyc.1994.03950010008002] [DOI] [PubMed] [Google Scholar]
Kessler 2005a
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12‐month DSM‐IV disorders in the national comorbidity survey replication. Archives of General Psychiatry 2005;62(6):617‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kessler 2005b
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age‐of‐onset distributions of DSM‐IV disorders in the national comorbidity survey replication. Archives of General Psychiatry 2005;62(6):593‐602. [DOI] [PubMed] [Google Scholar]
Landon 2004
- Landon TA, Barlow DH. Cognitive‐behavioural treatment for panic disorder: current status. Journal of Psychiatric Practice 2004;10(4):211‐26. [PubMed] [Google Scholar]
Leon 1997
- Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International Journal of Psychiatric Medicine 1997;27:93‐105. [DOI] [PubMed] [Google Scholar]
Mattick 1998
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy 1998;36(4):455‐70. [DOI] [PubMed] [Google Scholar]
Mayo‐Wilson 2013
- Mayo‐Wilson E, Montgomery P. Media‐delivered cognitive behavioural therapy and behavioural therapy (self‐help) for anxiety disorders in adults. Cochrane Database of Systematic Reviews 2013, Issue 9. [DOI: 10.1002/14651858.CD005330.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
McNaughton 2008
- McNaughton N. The neurobiology of anxiety: potential for co‐morbidity of anxiety and substance use disorders. In: Stewart SH, Conrod PJ editor(s). Anxiety and substance use disorders. New York, NY: Springer, 2008:19‐33. [Google Scholar]
Milette 2011
- Milette K, Roseman M, Thombs BD. Transparency of outcome reporting and trial registration of randomized controlled trials in top psychosomatic and behavioral health journals: A systematic review. Journal of Psychosomatic Research 2011;70:205‐17. [DOI: 10.1016/j.jpsychores.2010.09.015] [DOI] [PubMed] [Google Scholar]
Mogotsi 2000
- Mogotsi M, Kaminer D, Stein DJ. Quality of life in the anxiety disorders. Harvard Review of Psychiatry 2000;8:273‐82. [DOI: 10.1093/hrp/8.6.273] [DOI] [PubMed] [Google Scholar]
Mohr 2006
- Mohr DC, Hart SL, Howard I, Julian L, Vella L, Catledge C, et al. Barriers to psychotherapy among depressed and nondepressed primary care patients. Annals of Behavior Medicine 2006;32(3):254‐8. [DOI] [PubMed] [Google Scholar]
Norton 2007
- Norton PJ, Price EC. A meta‐analytic review of adult cognitive‐behavioral treatment outcomes across anxiety disorders. Journal of Nervous and Mental Diseases 2007;195(6):521‐31. [DOI] [PubMed] [Google Scholar]
Norton 2014
- Norton PJ, Little TE, Wetterneck CT. Does experience matter? Trainee experience and outcomes during transdiagnostic cognitive‐behavioral group therapy for anxiety. Cognitive Behaviour Therapy 2014;43:230‐8. [DOI: 10.1080/16506073.2014.919014] [DOI] [PubMed] [Google Scholar]
Ohayon 2000
- Ohayon MM, Shapiro CM, Kennedy SH. Differentiating DSM‐IV anxiety and depressive disorders in the general population: Comorbidity and treatment consequences. Canadian Journal of Psychiatry 2000;45:166‐72. [DOI] [PubMed] [Google Scholar]
Olatunji 2010
- Olatunji BO, Hollon SD. Preface: the current status of cognitive behavioral therapy for psychiatric disorders. Psychiatric Clinics of North America 2010;33(3):xiii‐ix. [DOI] [PubMed] [Google Scholar]
Olthuis 2011
- Olthuis JV, Watt MC, Stewart SH. Therapist‐delivered distance cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database of Systematic Reviews 2011, Issue 3. [DOI: 10.1002/14651858.CD009028] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ost 1997
- Ost LG. Rapid treatments of specific phobias. In: GCL Davey editor(s). Phobias: A handbook of theory, research, and treatment. Chichester, UK: Wiley, 1997:227‐46. [Google Scholar]
Otto 2000
- Otto MW, Pollack MH, Maki KM. Empirically supported treatments for panic disorder: costs, benefits, and stepped care. Journal of Consulting and Clinical Psychology 2000;68(4):556‐63. [PubMed] [Google Scholar]
Otto 2005
- Otto MW, Smits JAJ, Reese HE. Combined psychotherapy and pharmacotherapy for mood and anxiety disorders in adults: Review and analysis. Clinical Psychology: Science and Practice 2005;12(1):72‐86. [Google Scholar]
Peters 2008
- Peters J, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour‐enhanced meta‐analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology 2008;61(10):991‐6. [DOI] [PubMed] [Google Scholar]
Postel 2008
- Postel MG, Haan HA, Jong CAJ. E‐therapy for mental health problems: A systematic review. Telemedicine and e‐Health 2008;14:707‐14. [DOI: 10.1089/tmj.2007.0111] [DOI] [PubMed] [Google Scholar]
Pull 2007
- Pull CB. Combined pharmacotherapy and cognitive‐behavioral therapy for anxiety disorders. Current Opinion in Psychiatry 2007;20(1):30‐5. [DOI] [PubMed] [Google Scholar]
Reger 2009
- Reger MA, Gahm GA. A meta‐analysis of the effects of internet‐ and computer‐based cognitive‐behavioral treatments for anxiety. Journal of Clinical Psychology 2009;65(1):53‐75. [DOI] [PubMed] [Google Scholar]
Revicki 2012
- Revicki DA, Travers K, Wyrwich KW, Svedsater H, Locklear J, Stoeckl Mattera M, et al. Humanistic and economic burden of generalized anxiety disorder in North America and Europe. Journal of Affective Disorders 2012;140:103‐12. [DOI: 10.1016/j.jad.2011.11.014] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Robins 1991
- Robins LN, Locke BZ, Regier DA. An overview of psychiatric disorders in America. In: LN Robins, DA Regier editor(s). Psychiatric disorders in America: The Epidemiologic Catchment Area Study. New York: Free Press, 1991:328‐66. [Google Scholar]
Rost 2002
- Rost K, Fortney J, Fischer E, Smith J. Use, quality, and outcomes of care for mental health: the rural perspective. Medical Care Research and Review 2002;59(3):231‐65. [DOI] [PubMed] [Google Scholar]
Salkovskis 1985
- Salkovskis P. Obsessional‐compulsive problems: a cognitive behavioural analysis. Behaviour Research and Therapy 1985;23:571‐83. [DOI] [PubMed] [Google Scholar]
Slade 2007
- Slade T, Johnston A, Oakley Brown MA, Andrews G, Whiteford H. 2007 National Survey of Mental Health and Wellbeing: Methods and key findings. Australian and New Zealand Journal of Psychiatry 2009;43(7):594‐605. [DOI] [PubMed] [Google Scholar]
Spek 2007
- Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet‐based cognitive behaviour for symptoms of depression and anxiety: A meta‐analysis. Psychological Medicine 2007;37:319‐28. [DOI: 10.1017/S0033291706008944] [DOI] [PubMed] [Google Scholar]
Statistics Canada 2004
- Statistics Canada. Canadian Community Health Survey: Mental health and well‐being. http://www.statcan.ca/english/freepub/82‐617‐XIE/index.htm (accessed 25 March 2008).
Stewart 2008
- Stewart SH, Conrod PJ, editors. Anxiety and substance use disorders: the vicious cycle of comorbidity. New York, NY: Springer, 2008. [Google Scholar]
Stewart 2009
- Stewart RE, Chambless DL. Cognitive‐behavioral therapy for adult anxiety disorders in clinical practice: a meta‐analysis of effectiveness studies. Journal of Consulting and Clinical Psychology 2009;77(4):595‐606. [DOI] [PMC free article] [PubMed] [Google Scholar]
Svanborg 1994
- Svanborg P, Asberg M. A new self‐rating scale for depression and anxiety states based on the comprehensive psychopathological rating scale. ACTA Psychiatrica Scandinavica 1994;89:21‐8. [DOI: 10.1111/j.1600-0447.1994.tb01480.x] [DOI] [PubMed] [Google Scholar]
Titov 2010b
- Titov N, Andrews G, Kemp A, Robinson E. Characteristics of adults with anxiety or depression treated at an internet clinic: Comparison with a national survey and an outpatient clinic. PLoS ONE 2010;5:e10885. [DOI: 10.1371/journal.pone.0010885] [DOI] [PMC free article] [PubMed] [Google Scholar]
Westra 1998
- Westra HA, Stewart SH. Cognitive behavioural therapy and pharmacotherapy: complementary or contradictory approaches to the treatment of anxiety?. Clinical Psychology Review 1998;18(3):307‐40. [DOI] [PubMed] [Google Scholar]
WHO 1979
- International Classification of Diseases (9th revision). World Health Organization 1979.
WHO 1999
- International Statistical Classification of Diseases and Related Health Problems (10th revision). World Health Organization 1999.
Wilson 2006
- Wilson KA, Hayward C. Unique contributions of anxiety sensitivity to avoidance: a prospective study in adolescents. Behaviour Research and Therapy 2006;44(4):601‐9. [DOI] [PubMed] [Google Scholar]
Young 2001
- Young AS, Klap R, Sherbourne CD, Wells KB. The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 2001;58(1):55‐61. [DOI] [PubMed] [Google Scholar]
Yuen 1996
- Yuen EJ, Gerdes JL, Gonzales JJ. Patterns of rural mental health care: an exploratory study. General Hospital Psychiatry 1996;18(1):14‐21. [DOI] [PubMed] [Google Scholar]


