Abstract
Primary retroperitoneal mucinous cystadenoma (PRMC) is a rare tumour. It was first reported in 1965, and since then, less than 100 cases have been reported. It is cystic in nature and most commonly affects the female population. It becomes symptomatic in later stages due to its mass effect, making the diagnosis challenging in its early asymptomatic stage. We report a case of a 32-year-old female who presented with abdominal pain and a mass in left iliac fossa. Diagnostic imaging revealed a large cystic lesion in retroperitoneum. A midline laparotomy was performed, and a complete surgical excision was accomplished without any spillage. Surgical histology confirmed the diagnosis of PRMC. The patient was discharged on postoperative day 2. There was no evidence of tumour recurrence on repeat imaging at 90-day follow-up. Surgical approach, with complete resection and without any spillage, remains the most effective and appropriate treatment for this tumour.
Keywords: primary retroperitoneal mucinous cystadenoma, PRMC, benign
INTRODUCTION
Primary retroperitoneal mucinous cystadenoma (PRMC) has been described as a rare tumour, as since 1965 only less than 100 cases have been reported. It is a cystic tumour, most commonly affecting females, and has a histological association with ovarian mucinous cystadenoma.
The histogenesis of PRMC remains unclear. Epithelial tissue does not normally exist in the retroperitoneum, and there are four main theories on the origins of PRMC. These include seeding of ectopic ovarian tissue [1], monodermal variant of teratomas, enterogenic duplication of cyst and coelomic metaplasia [2].
In its early stages, PRMC is often asymptomatic. Initial presentation is usually non-specific abdominal pain due to its mass effect. Imaging can aid the differential diagnosis, but due to lack of distinctive tumour characteristics, surgical resection is often undertaken without a clear pre-op diagnosis, relying on subsequent histopathological analysis [3]. Open surgery remains the most effective treatment although successful laparoscopic approach has also been reported [4–6].
CASE REPORT
A 32-year-old female was referred to general surgery clinic with a 9-month history of central abdominal pain and no other associated symptoms. Her past medical history included squamous cell carcinoma of the tongue for which she had right hemiglossectomy with reconstruction 10 years ago.
She had a low body mass index of 16. Examination revealed a soft and non-tender abdomen with a large immobile mass in the left iliac fossa, which was firm and non-pulsatile.
Blood tests were normal with haemoglobin of 132 g/l, white blood cell count of 4.8 × 109/l and C reactive protein of <4 mg/l.
Subsequent computed tomography (CT) scan revealed a lesion in the retroperitoneum, measuring 11 cm in coronal plane and resulting in the anterior displacement of the descending colon (Fig. 1).
Figure 1.
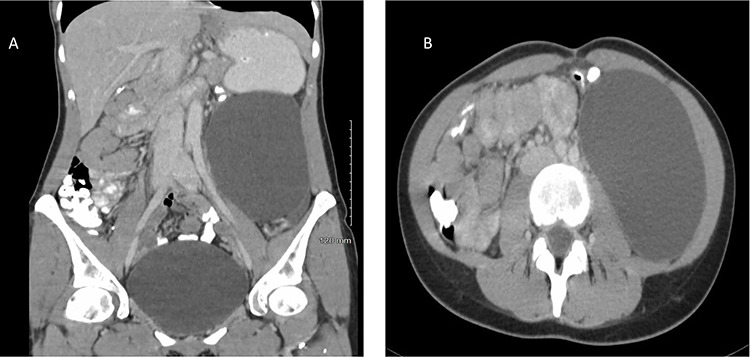
Contrast-enhanced CT of a 32-year-old woman presenting with chronic abdominal pain and a mass in left iliac fossa. The image demonstrates a retroperitoneal space occupying lesion measuring 11 cm in coronal plane (A) and resulting in anterior displacement of the descending colon (B).
In order to characterize the lesion further, magnetic resonance scan was organized. This demonstrated a 10 × 7 × 15 cm cystic lesion in the left flank between Gerota’s fascia and the descending colon, confirming its retroperitoneal location. The fluid within the lesion was described as simple, with homogenously high T2 and low T1 signals. A possible thin septation was seen within the superior aspect of the cyst, but there was no evidence of any soft tissue component. There was no enhancement within the cyst or its wall (Fig. 2). The most likely differentials at this stage included a lymphangioma or mucinous cystadenoma.
Figure 2.
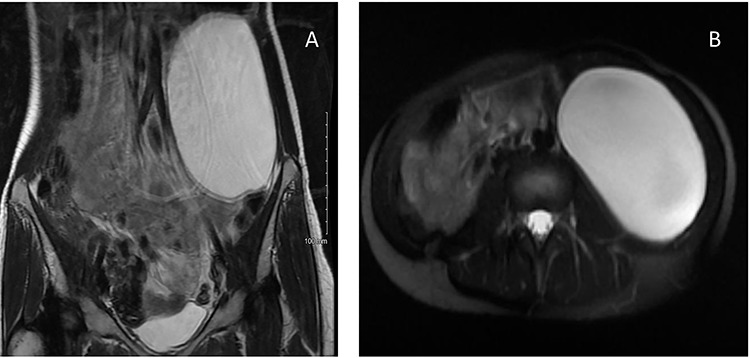
MRI of a 32-year-old woman presenting with chronic abdominal pain and a mass in left iliac fossa. (A) Axial T2-weighted fat-saturated images demonstrate a 10 × 7 × 15 cm cystic lesion in the left flank between Gerota’s fascia and the descending colon. (B) Coronal T2-weighted images confirm the absence of internal nodularity or invasive features.
The patient’s case was discussed in the Lower Gastrointestinal and Sarcoma Multidisciplinary Team Meetings, both recommending surgical resection.
On the day of surgery, the left ureter was stented in order to allow easier intraoperative identification and minimize the risk of iatrogenic injury. The intraperitoneal cavity was approached via midline laparotomy. The left colon and mesocolon were mobilized and carefully separated from the cyst. Dissection plane was kept deliberately on the cyst wall, taking care to preserve the retroperitoneal structures: the left ureter, gonadal vessels, branches of the lumbar plexus and the duodenum. The cyst was resected successfully in its entirety without rupture. The left ureteric stent was removed at the end of the procedure. Total surgical time was of 1 hour and 45 minutes.
There were no perioperative complications, and the patient was discharged on postoperative day 3. At 3 months of follow-up, the patient remains symptom-free and there was no evidence of disease recurrence on repeat CT scan.
On histopathological analysis, the surgical specimen was described as a 17 × 7 × 12 cm cystic lesion with a smooth capsule and a unilocular cavity filled with clear serous fluid. The internal surface had several thickened areas, but there was no suspicious papillary projection seen.
Microscopic examination revealed a fibrous capsule lined by a single layer of mixed mucinous epithelium and attenuated mesothelial cells with no cytological atypia or mitotic activity (Fig. 3A).
Figure 3.
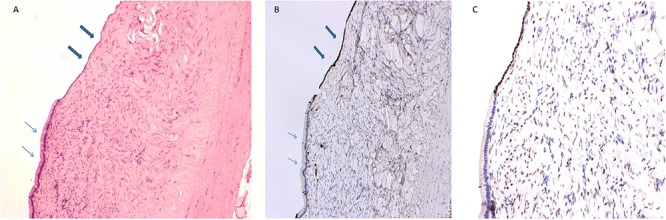
Retroperitoneal mucinous cystadenoma in a 32-year old woman presenting with chronic abdominal pain and a mass in left iliac fossa. (A) The section shows full thickness of the cyst wall, which is lined by a single layer of mucinous epithelium (thin arrows) alternating with attenuated mesothelial cells (thick arrows) (hematoxylin & eosin stain, ×100 magnification). (B) Immunochemistry for calretinin highlights the mesothelial lining (thick arrows) and is negative in the mucinous epithelium (thin arrows) (calretinin stain, ×100 magnification). (C) Immunochemistry showing nuclear positivity for oestrogen receptor in the mesothelial lining and stromal cells (oestrogen receptor stain, ×100 magnification).
Immunochemistry for calretinin was positive in the mesothelial lining and negative in the mucinous epithelium (Fig. 3B). The mucinous epithelium was strongly positive for BerEP4, whereas the stromal and mesothelial cells were shown to express oestrogen receptor (Fig. 3C). Based on these histopathological features, a diagnosis of PRMC was made.
DISCUSSION
PRMC is a rare but important differential diagnosis for any retroperitoneal cystic mass. Early investigations and prompt treatment should be pursued to reduce the risk of infection or malignant transformation and to avoid secondary complications due to its mass effect such as bowel obstruction and hydronephrosis [7, 8].
PRMC often poses a diagnostic challenge because of several reasons. It usually presents late due to its non-specific and low-grade symptoms. Furthermore, it cannot be confidently diagnosed solely on imaging, because it lacks clear differentiating features. Radiological investigations are useful in characterizing the lesion preoperatively; however, the ultimate diagnosis always requires histopathological confirmation [6].
Because of its rarity, there are no formal guidelines on the management of PRMC; however, general consensus supports early operative management. Both open and laparoscopic approaches have been utilized successfully, each with its own benefits and drawbacks. Regardless of surgical approach, the risk of intraoperative cyst rupture should be minimized as it may lead to intra-abdominal spread of potentially malignant fluid resulting in Pseudomyxoma peritonei [9]. Laparoscopically, the trans-abdominal approach is most frequently used when compared to retroperitoneal approach as it provides a large working space and the ability to investigate intra-abdominal pathologies at the same time. The retroperitoneal approach decreases the risk of bowel damage and intraperitoneal dissemination in case of cyst rupture [10]. However, in case of a large tumour size, invasion of other organs or suspected malignancy, an open surgical technique is considered safe and effective and still remains the most widely used surgical approach.
CONCLUSION
In summary, this case describes a successful surgical management of PMRC. We recommend that patients presenting with this rare tumour should undergo prompt investigation and their management is best decided by multidisciplinary team after careful review of their preoperative imaging. Open surgery remains a safe and effective approach to deal with these challenging tumours. However, with current advancements in laparoscopic and robotic surgery, these modalities are likely to become attractive alternatives in selected cases of PMRC.
ACKNOWLEDGEMENTS
None.
Conflict of interest statement
None declared.
References
- 1. Tapper EB, Shrewsberry AB, Oprea G, Majmudar B. A unique benign mucinous cystadenoma of the retroperitoneum: a case report and review of the literature. Arch Gynecol Obstet 2010;281:167–9. [DOI] [PubMed] [Google Scholar]
- 2. Blount SE, Cobb C, Raza AS. Non-pancreatic retroperitoneal mucinous neoplasms and a discussion of the differential diagnosis. J Gastrointest Oncol 2016;7:S75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee SE, Oh HC, Park YG, Choi YS, Kim MK. Laparoscopic excision of primary retroperitoneal mucinous cystadenoma and malignant predicting factors derived from literature review. Int J Surg Case Rep 2015;9:130–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Koyama R, Maeda Y, Minagawa N, Shinohara T, Hamada T. Laparoscopic resection of a primary retroperitoneal mucinous cystadenoma. Case Rep Gastroenterol 2019;13:159–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tokai H, Nagata Y, Taniguchi K, Matsumura N, Kitasato A, Tokunaga T, et al. The long-term survival in primary retroperitoneal mucinous cystadenocarcinoma: a case report. Surg Case Rep 2017;3:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Subramony C, Habibpour S, Hashimoto LA. Retroperitoneal mucinous cystadenoma. Arch Pathol Lab Med 2001;125:691–4. [DOI] [PubMed] [Google Scholar]
- 7. Neville A, Herts BR. CT characteristics of primary retroperitoneal neoplasms. Crit Rev Comput Tomogr 2004;45:247–70. [PubMed] [Google Scholar]
- 8. Kassab A, El-Bialy G, Clark J, Callen P, Powari M, Jones H. Unusual presentation of 22-kg retroperitoneal Müllerian serous cystadenoma. Gynecol Oncol 2007;104:257–9. [DOI] [PubMed] [Google Scholar]
- 9. Tan A, Li R, Rafique M, Qin S, Pham T. A rare case of giant extra-ovarian mucinous cystadenoma arising from sigmoid mesocolon. J Surg Case Rep 2018;2018:rjy038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fujita K, Yamamoto Y, Yamaguchi S. Laparoscopic resection of primary retroperitoneal mucinous cystadenoma by retroperitoneal approach. Int J Urol 2011;18:607–8. [DOI] [PubMed] [Google Scholar]


