Abstract
Policy Points.
Because bundled payments are relatively new and require a different type of collaboration among payers, providers, and other actors, their design and implementation process is complex.
By sorting the 53 key elements that contribute to this complexity into specific pre‐ and postcontractual phases as well as the actors involved in the health system, this framework provides a comprehensive overview of this complexity from a payer's perspective.
Strategically, the design and implementation of bundled payments should not be approached by payers as merely the introduction of a new contracting model, but as part of a broader transformation into a more sustainable, value‐based health care system.
Context
Traditional fee‐for‐service (FFS) payment models in health care stimulate volume‐driven care rather than value‐driven care. To address this issue, increasing numbers of payers are adopting contracts based on bundled payments. Because their design and implementation are complex, understanding the elements that contribute to this complexity from a payer's perspective might facilitate their adoption. Consequently, the objective of our study was to identify and structure the key elements in the design and implementation of bundled payment contracts.
Methods
Two of us independently and systematically examined the literature to identify all the elements considered relevant to our objective. We then developed a framework in which these elements were arranged according to the specific phases of a care procurement process and actors’ interactions at various levels of the health system.
Findings
The final study sample consisted of 147 articles in which we identified the 53 elements included in the framework. These elements were found in all phases of the pre‐ and postcontractual procurement process and involved actors at different levels of the health care system. Examples of elements that were cited frequently and are typical of bundled payment procurement, as opposed to FFS procurement, are (1) specification of care services, patients’ characteristics, and corresponding costs, (2) small and heterogeneous patient populations, (3) allocation of payment and savings/losses among providers, (4) identification of patients in the bundle, (5) alignment of the existing care delivery model with the new payment model, and (6) limited effects on quality and costs in the first pilots and demonstrations.
Conclusions
Compared with traditional FFS payment models, bundled payment contracts tend to introduce an alternative set of (financial) incentives, touch on almost all aspects of governance within organizations, and demand a different type of collaboration among organizations. Accordingly, payers should not strategically approach their design and implementation as merely the adoption of a new contracting model, but rather as part of a broader transformation toward a more sustainable value‐based health care system, based less on short‐term transactional negotiations and more on long‐term collaborative relationships between payers and providers.
Keywords: alternative payment models, value‐based purchasing, bundled payments, design and implementation process
The most common provider payment method in health care today is the fee‐for‐service (FFS) model. Under this model, provider organizations are paid a predetermined amount for each service they deliver, regardless of whether it contributes to a higher value of care for their patients. The lack of incentives to improve quality can result in overtreatment, waste, and avoidable complications.1, 2, 3 In addition, most current health care delivery systems are highly fragmented because providers are paid separately for their services. FFS forms a major obstacle to multidisciplinary collaboration among providers and to the coordination of care for individual patients, resulting in low‐value care.4 Therefore, several countries are now taking steps to transition their provider payment systems from volume‐based FFS to value‐based alternative‐payment models (APMs).5, 6 The aim is to enable the delivery of value‐based health care by rewarding providers for the value of their care for patients, that is, for achieving better‐quality outcomes at lower costs.7, 8
One payment model in particular has recently become more prominent: bundled payments. A bundled payment may be defined as a one‐off or periodic lump‐sum payment for a range of services delivered by one or more providers based on best practices or by following clinical pathways with an increasing emphasis on outcomes.3 Bundled payments can be supplemented with shared‐savings and shared‐risk components based on pay‐for‐performance structures.9 There are many different types of bundled payments. They can, for example, be episode‐based for acute or elective care activities (eg, hip and knee replacements), or periodic‐based for patients with chronic diseases (eg, diabetes and chronic obstructive pulmonary disease).3, 10 More detailed information on the definition of “bundled payments” that we use in this study can be found in Online Appendix A. The goal of bundled payment contracts is to overcome the flaws of FFS models, with their main strength perhaps explicitly shifting the financial and clinical accountability associated with a care episode to a single provider organization or a group of collaborative provider organizations. This incentivizes provider organizations to coordinate care across settings, limit the total amount spent on all services, deliver appropriate care, and further align their interests with the payer's interests. It also provides them with the flexibility to deliver services in different ways.
Although the scientific knowledge supporting bundled payments is growing, the empirical evidence for the effect of such contracts on cost containment and quality improvement is still limited and inconsistent.11, 12, 13, 14 Consequently, many new studies focus primarily on the effects, with only a few addressing design and implementation and the numerous associated operational issues.15, 16, 17 The current scientific literature describes multiple operational barriers and facilitators that payers need to take into account when implementing a bundled payment contract. Some of these are relatively well known, like privacy barriers to sharing information, difficulties defining quality criteria, and “gaming.” Others have been less well analyzed, such as issues regarding the identification of patients to be included in the bundle, the deteriorating income of some care professionals, and potential limitations to patients’ freedom of choice.18, 19 This lack of a comprehensive and systematic overview of the various elements at different health system levels causes great uncertainty for payers (and other actors) in the design and implementation of bundled payment contracts. Consequently, this process is seen as complex and adoption rates are slow.20, 21 Although a number of publications from innovators and early adopters report on the key elements in the design and implementation of such a contract from a payer's perspective, they do not offer a comprehensive overview. Accordingly, we used a scoping review of the literature to identify and structure the key elements in the design and implementation of bundled payment contracts into a framework that is generic and recognizable to payers. A better understanding of these elements can also help reduce the complexity for payers who want to adopt bundled payment models.
Methods
In collaboration with a university librarian (Johannes Ket), we created a review protocol based on the PRISMA‐statement.22 Sander Steenhuis and Ket then searched the following sources from their inception: PubMed and Embase.com, Ebsco/PsycInfo, Ebsco/CINAHL, Thomson Reuters/Web of Science, Wiley/Cochrane Library, Proquest/ABI‐INFORM Global, Ebsco/Business Source Elite, Proquest/IBSS and Google Scholar (until March 2018). The following terms were used (including synonyms and closely related words) as index terms or free‐text words: “bundled payments,” or “episode‐based payments,” or “value‐based payments,” and “design,” or “implementation,” or “contracting,” or “barriers,” or “facilitators.” The full search strategy can be found in Online Appendix B. Only articles written in English were included. In addition, we included relevant grey literature (eg, government and third‐party evaluation reports), first identified through ad hoc online searches, reference mining, and recommendations from experts.
After removing the duplicates, Steenhuis and Eric van der Hijden independently screened the remaining articles by title and abstract for relevance to our research objective. If they could not reach consensus on whether or not to include an article, Jeroen Struijs made the final call. Steenhuis and van der Hijden then independently examined the remaining articles in full, which resulted in the final study sample. Articles that did not describe specific barriers, facilitators, or other factors concerning the design and implementation of bundled payments or the associated operational issues were excluded. Those articles that did not match the detailed definition of a bundled payment as presented in Online Appendix A also were excluded. Finally, for generalizability, articles from non‐OECD countries were excluded as well.
Beside using standard systematic review methods, we followed the five stages of the methodological framework as developed by Arksey and O'Malley and enhanced by Levac and colleagues.23, 24 To ensure that we covered the literature comprehensively, we followed an iterative process requiring us to engage with each stage reflexively and to repeat steps when necessary.23
The following information was extracted and entered into a data‐charting form: title, journal, year of publication, author(s), the country to which the article refers, and the specific medical condition and/or specific care sector. We then performed qualitative text analysis methods in which Steenhuis and van der Hijden independently identified, shaded, and coded all the barriers and facilitators described in the literature as relevant to the design and implementation of bundled payments. Then, in an iterative process, they searched for consensus and collated the identified clusters of barriers and facilitators into comprehensively defined key elements until reaching a saturation point. This saturation was then externally assessed by two expert panels, consisting of twelve experienced care procurement professionals from five different payer organizations. In these 3‐hour sessions, we discussed and confirmed our findings from the review and sometimes discovered new elements not identified in the literature.23 More detailed information about the expert panels can be found in Online Appendix C. We used this list of identified elements to provide a full overview of the complexity in the design and implementation of a bundled payment contract.
In order to connect and contextualize the identified elements, we constructed a framework with two axes. On the horizontal axis we combined the frameworks for health care procurement from a payer's perspective of Van Raaij, Sanderson, and Van Weele and ordered the elements into six phases25, 26, 27 representing a generic care procurement process (as is currently also used in FFS contracting). Such a process generally starts with a (more tactical) precontractual phase in which purchasing needs are specified (eg, determining the care services included in the bundle) and providers are selected and contracted. This is followed by a (more operational) postcontractual phase in which the patients are identified and allocated to the bundle and the care is delivered and monitored. The final step is the actual payment for care and the evaluation of the contract. In general, despite the many different types of bundled payment contracts with different characteristics, the design and implementation of bundled payments can be ascribed to these six procurement phases because the vast majority of bundled payment contracts are currently “built” on the existing FFS architecture, with a retrospective payment strategy (in which the actual payments are made while or after the care is delivered, based on FFS claims rather than being paid in advance).
To further unravel the complexity of bundled payment contracts, we added a vertical axis in which we ordered the elements according to the interactions among the different actors in the health care system (regulator, payer, provider organization, professional, patient).28, 29 In contrast to the design and implementation of traditional FFS contracts (on which usually only a procurement team from the payer and the provider organization's financial department agree), this axis is necessary for the design and implementation of bundled payment contracts because the objective of those contracts is usually to facilitate a redesign of care delivery processes.30 A more detailed explanation of the six procurement phases and the interactions among the actors is presented in Online Appendix D1.
We plotted an identified element in the framework based on the specific procurement phase and system level to which it applied. In most cases, the best fit for an element in the framework was clear from the literature. When necessary, Steenhuis and van der Hijden used their own insights to find the most appropriate fit, externally assessing this in the expert panels (see Online Appendix C). Some elements could apply to all phases and system levels (eg, the “degree of trust and collaboration between payer and provider” [element 8]) and so were placed according to how they were most often described in the literature included in the final study sample.
Results
Study Retrieval
Our initial search resulted in 7,360 articles. We found five more articles by hand‐searching key journals, resulting in a total of 4,486 unique articles after removing duplicates. After screening titles and abstracts, we examined the full text of 210 articles and included 147 articles in the final study sample (Figure 1).
Figure 1.
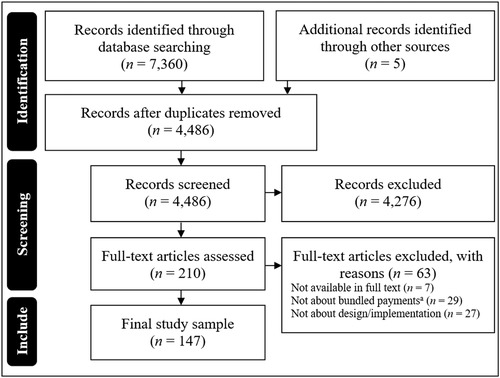
Flow Diagram of the Systematic Search
See Online Appendix A for the applied definition of a bundled payment.
Study Characteristics
The final study sample comprised 147 articles, of which about half (56.5%) were published between 2015 and March 2018, and about two‐thirds (64.6%) were focused on bundled payments in the United States. Of all the included articles, 64.4% were generic and did not cover a specific medical condition; 15.6% covered bundled payments in orthopedic care, 4.8% in cardiovascular care, 3.4% in oncological care, and 11.6% in another specific medical condition.
Key Elements for Bundled Payment Contracts
We identified 53 elements in all (Figure 2), 52 from the literature and 1 (element 38) based on input from the expert panel. The two‐axis framework presents a structured overview of which elements, at which health system level, and in which phase of the procurement process are considered relevant to the design and implementation of a bundled payment contract. As Figure 2 shows, the principal elements were found in all phases of a care procurement process and involve all relevant health system actors.
Figure 2.
Framework with 53 Key Elements in the Design and Implementation of Bundled Payment Contracts
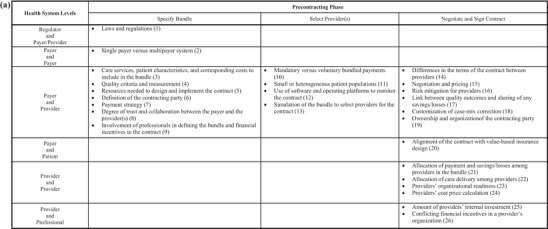
Next we describe the framework and its most important elements, following the six procurement phases on the framework's vertical axis. Due to the restricted length of this article, we limit our descriptions of elements to those frequently identified and typical for bundled payment procurement, as opposed to FFS procurement. For a more detailed explanation of all 53 identified elements, the numbers given in brackets in Figure 2 correspond to the complete list of definitions, explanations, and literature references in Online Appendix D2. Here when we refer to a “provider,” we mean a “provider organization” (which can contract with a payer, such as a hospital or general practice), rather than an individual care professional. When we refer to a “professional,” we mean an individual who is employed by the provider (and cannot directly contract with a payer), like a physician or physical therapist. In the case of a small or solo practice, one actor may operate as both a provider and a professional.
Specifying the Bundle
The precontractual design process of a new bundled payment contract starts with a specification phase in which the general characteristics of the contract are designed by the payer, usually in consultation with one or more providers. Out of the nine elements we identified in this phase, seven were associated with interactions between the payer and provider(s), and the other two were associated with the regulator‐payer/provider and the payer‐payer levels. No elements were associated with the other health system levels during this procurement phase. The most frequently identified element for bundled payment contracts, in contrast to FFS contracts, is element 3: “care services, patient characteristics and corresponding costs to include in the bundle.” This key element concerns the specification of the care services included in the bundle and their corresponding health care costs (eg, which medical condition is covered, the included and excluded care components, the starting and end point of the bundle, patient identification criteria and trigger events, agreements on dealing with multi‐ and comorbidity, complications, and readmissions). Multiple studies show that choices made on the inclusion of care in the bundle can either have a hampering or facilitating effect on the design and implementation process and that these effects are often the consequence of a trade‐off between the ease of implementation and the expected outcomes of the contract. For instance, from a payer's perspective, which care to include in an episodic bundle for an elective hip replacement procedure is often less complex to define than is a periodic bundle for chronic diabetes care (eg, because the latter usually involves more providers and has a higher level of comorbidity), but the potential impact on the reduction in health care expenditures is also lower (because diabetes is a chronic and more expensive condition).20, 31, 32 Another frequently identified element that can either hamper or facilitate the design and implementation process in this phase is the “definition of the contracting party for the bundle” (element 6), for example, specifying one or more provider organization(s) as a “designated recipient” or a (new or existing) third legal entity.18 Some researchers believe that ideally, in order to reduce complexity, bundled payment contracts should be closed with one main contracting party receiving and distributing the single payment among the providers. This party should be given technical and analytical abilities to monitor the contract and coordinate the care delivery process, thereby allowing it to effectively manage expenditures and to maximize profits for all the affiliated providers.33, 34 In this case, there may no longer be a direct interaction between the payer and the subcontracted provider organization, which can create a different contracting environment (eg, in terms of competition, negotiating power, and allocation of care delivery).35
Selecting Provider(s)
In the second phase of the design and implementation process, the payer selects providers based on the selection criteria and specific preferences for contracting bundles (eg, the characteristics of the provider network) as determined in the specification phase. All four key elements that were identified in this phase were associated with interactions between the payer and provider(s). For example, this phase of the design and implementation process is influenced by whether the “bundled payment contract is mandatory or voluntary” (element 10). In a voluntary contract, the providers’ willingness to participate may differ. On the one hand, well‐organized providers may be more likely to participate and underperforming providers (with a higher potential for significant efficiency gains) may not, because, for example, it would be necessary for them to make more immediate internal investments in order to achieve any potential savings.36 On the other hand, if payments include a shared‐savings approach, well‐organized providers may be less likely to participate than underperforming providers would, because they have already achieved any possible savings and thus have nothing to gain from participating. Nonetheless, if bundled payment contracts are well designed, they may not need to be mandatory. Several researchers believe that most providers will voluntarily sign a contract that rewards them for providing higher‐quality care at a lower cost as long as they are held accountable for only the performance risk (which they can control) and not the insurance risk (which they cannot control).37, 38 This important precondition also applies to a second element in this phase, regarding the barriers that can be caused by “small and heterogeneous patient populations” (element 11). For provider organizations with a relatively low volume of patients eligible for inclusion in the contract, random variation and outliers in the demand for care can have a disproportionate and unpredictable impact on the average bundle's expenditures.33 Moreover, separating performance and insurance risk becomes more complex if the variability increases and the predictability and standardization of the health condition's care and costs decrease.39 To overcome these barriers, payers can decide not to include specific providers based on minimum patient volume criteria, or they can customize the contract (eg, with case‐mix corrections or stop‐loss provisions to limit downside risk) in the “negotiate and contract” phase.
Negotiating and Contracting
This third procurement phase entails the payer and the selected provider(s) negotiating and agreeing on the variable aspects of the contract, such as price and volume, weights of the case‐mix method, quality and cost targets, and the distribution of shared savings. If an agreement is reached, this phase will end with the signing of the contract, marking the start of the postcontractual phases. Our study found 13 elements contributing to the degree of complexity in this phase. Whereas in the previous phases, the payer and provider organization(s) were the primary actors, Figure 2 shows that in this phase, more actors become involved. Many barriers and facilitators in the design and implementation process relate to the degree of alignment between the incentives in the bundled payment contract between the payer and provider(s), the mutual contract(s) between bundled providers, and the employment contracts between provider(s) and professional(s). In addition, on the payer‐patient level, the “alignment of the bundled payment contract with the patient's value‐based insurance design” (element 20) is reported regularly as a facilitator (when sufficient) or a barrier (when insufficient).
On the provider‐provider level of this phase, the two most frequently cited elements are the “allocation of payments and savings/losses” and the “allocation of care delivery” among the providers in the bundle (elements 21 and 22). Agreeing on the allocation of care tasks and the distribution of payments and closing a joint contract with a payer are new and complex for most providers transitioning from a FFS to a bundled payment model.40 To reduce this complexity, several new entities that act as intermediary organizations between providers have been established and are often reported as a facilitating factor in this phase of the design and implementation process.33, 35 In contrast, on the provider‐professional level, “conflicting financial incentives within providers” (element 26) are frequently reported as a potential barrier. The influence of different (embedded) employer‐employee contracts (including gain‐sharing arrangements) on provider organizations can create conflicts of interest and harm internal relationships.37 For example, a hospital that transitions from a volume‐based FFS contract to an outcomes‐based bundled payment contract should always integrate these new financial incentives in the variable component of its employee contracts. Not doing so might lead to care professionals’ direct deterioration of income and therefore increase the complexity of implementation.18
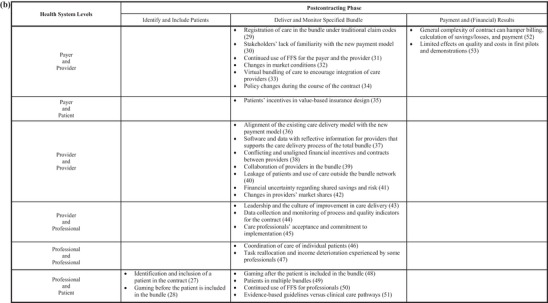
Identifying Patients
The first step of the postcontractual phase refers to the ability of health care professionals to accurately assign eligible patients to the bundle based on precontractually specified trigger events, risk stratifications, categorizations, and/or inclusion criteria. We found two elements, both on the professional‐patient level. The triage process to “identify and include a patient in the contract” (element 27) forms a critical link between the pre‐ and postcontractual phase and throughout the literature is regularly reported as a barrier.20, 37 Those contracts with a retrospective payment strategy especially report significant differences of more than 20% between the number of patients included in the bundle by providers and the number of patients identified in the payer data.33 The accurate specification of the criteria for this triage process in the contract facilitates the successful implementation of bundled payments because it allows the provider to identify the included patients—not just the payer—and thus prevents mismatches in data between the provider's care delivery process and the payer's financial‐monitoring systems.33 Also, to coordinate the patients among the different bundle providers, it is important that all the providers are able to identify all the included patients based on the same independent and reproducible method.
The second frequently identified element in this phase is “gaming before the patient is included in the bundle” (element 28), in which a care professional deliberately influences the process of care delivery to optimize his or her own personal (financial) benefit. An example is “cherry picking,” that is, selecting healthier or more cooperative patients and assigning the more time‐consuming patients to other professionals (also referred to as “lemon dropping” and “cream skimming”). However, most forms of gaming were reported “after the patient is included in the bundle” (element 48) during the care delivery and monitoring phase. In all cases, gaming is described as a barrier to the implementation of bundled payment contracts.9, 40, 41, 42
Delivering and Monitoring
After patients have been identified, the providers deliver care as agreed on in the contract, with the payer monitoring this process. We found 23 different elements in all associated with this phase on (almost) all levels of the health care system. This confirms that during this second postcontractual phase, the bundled payment contract can have a significant impact on the entire health care system and all its actors.
A frequently cited element in this phase is the impact of bundled payment contracts on “changes in market shares and conditions” (elements 42 and 32). The bundling of care services by provider organizations can shift market and negotiating power, which can result in higher prices and barriers to new providers entering the market.34 On the payer‐patient level, several studies reported on using “patient incentives in value‐based insurance design” (element 35) (eg, deductibles and copayments) to encourage patients to use high‐value care (ie, care services in the bundle) and/or to discourage them from using low‐value care (ie, care services not in the bundle). Another element that was frequently identified (on both the payer‐provider and the professional‐patient level) is the “continued use of FFS” (elements 31 and 50). Several authors of the articles in our final study sample argued that one cannot “fix a broken payment system” by merely building a new layer of incentives on it. They maintained that using the FFS model as a foundation perpetuated unwanted risks for, again, conflicting financial incentives within providers that may substantially reduce the commitment to and acceptance of the new payment model by both the providers and the professionals.18
Another key element for bundled payment contracts in this phase is the “alignment of the existing care delivery model with the new payment model” (element 36). Bundled payment contracts often require a redesign of care processes and a different type of collaboration among providers. Multidisciplinary care protocols thus need to be developed, and professionals and treatments should be integrated based on the patients’ health.33, 43, 44 Also, several authors stated that real success comes only if providers can create an organizational culture that supports good internal relationships and collaborations, engages professionals, and facilitates changes in their behavior.13, 36 In order to adapt to the new payment model, providers need time to educate administrative personnel, build relationships with other providers, and shift market shares. Most authors suggest approaching this complex transition from the old to the new payment model in small steps.40 This may mitigate the effects of the transition in the beginning but increases the chances of the implementation's success in the long term.
Payment and (Financial) Results
The final phase of the design and implementation process is assessing financial results and payment for care. The payment method depends to a large extent on the strategy decided in the contract's “specification” phase. This can be either a prospective payment (made just before the start of the postcontractual phase) or a retrospective payment (made during and/or at the end of the postcontractual phase) (element 7), but in practice almost all current bundled payment contracts use a retrospective payment strategy in which the provider(s) submit their FFS‐based claims for the care delivered according to what was agreed on in the contract. Depending on the terms in the contract, savings are then paid to the provider based on the achieved quality and financial results. In addition, both the payer and the providers evaluate the contract, which might be extended or a new (and improved) contract might be concluded. This phase contains two elements identified from the literature, both on the payer‐provider level. The most frequently identified element in this phase was the “limited effects in pilots and demonstrations” (element 53) in regard to quality improvement, financial results, and (potential) savings. If the results are disappointing during the first stages of the contract, then both the payer and provider organization(s) may be unwilling to prolong it and/or to enter into new bundled payment projects. But for as long as early adopters increase their experience with bundled payment contracts and more evidence of positive effects becomes available, the confidence, acceptance, and motivation for this new payment model will grow. Over time, we are likely to see an increasing awareness that current payment models are not delivering and a transition to bundled payments (or other APMs) is unavoidable, which will further facilitate implementation on a larger scale.45
Discussion
Main Findings
The aim of our study was to identify and provide a structured overview of the key elements involved in the design and implementation of bundled payment contracts from a payer's perspective. We constructed a framework that contains 53 key elements and that gives payers and other actors a comprehensive literature‐based overview and further insights into the sources of complexity in the design and implementation of bundled payment contracts.
Strengths and Limitations
In this study we used the PRISMA statement review protocol as well as rigorous and transparent methods throughout the entire process. To ensure a broad search of the literature, we searched nine scientific databases (see Online Appendix B), and two independent reviewers assessed the articles to reduce the risk of bias and subjectivity. We also organized two expert panel sessions to externally test our findings. Nonetheless, we acknowledge the limitations of our scoping design.23 We did not formally appraise the quality of evidence in the primary research reports. Consequently, our study offers only an overview and descriptions of the publicly available scientific research and gray literature. Despite our attempts to be as comprehensive as possible, our study might not have identified all the key elements in the literature. Although our search strategy included multiple terms (in English) used previously to describe the barriers and facilitators in the design and implementation process of bundled payment contracts, other terms may also exist. We may have missed some barriers and facilitators because we assumed that successful bundled payment implementations were more likely to be reported than were failed implementations. Finally, the context in which a bundled payment contract is designed depends to a large extent on a health system's “laws and regulations” (element 1) and whether it has a “single or a multipayer system” (element 2). Since our objective was to develop a generic framework, we included articles from different health system contexts with different bundled payment contract types and a wide variety in contract characteristics (eg, with one or multiple providers, with or without shared savings/losses, payer‐, provider‐ or jointly initiated). Therefore, some elements may not apply to all health systems and specific bundled payment contracts, and others may also apply to different APMs. For example, the elements concerning market conditions and market shares may apply solely to systems and contracts with some form of managed competition among multiple payers, providers, and patients. Moreover, because the definition of a bundled payment varies in the literature, our definition of a bundled payment (see Online Appendix A) may influence the interpretability of our findings. Our focus is on the design and implementation of bundled payment contracts that are built into the existing FFS architecture because these are the most common. Finally, we have presented our findings from a payer's perspective. A more specific context or bundled payment contract type, a different bundled payment definition, and/or another actor perspective might have led to a different framework structure.
Results in Perspective
In most health care systems, bundled payments are still a very new payment model. When bundled payment contracts are well designed, they should entail a shift in performance risk, and explicitly not in insurance risk, from the payer to the provider(s).8, 38, 39 Compared with the design and implementation process of FFS contracts, this requires a different type of collaboration between payers and providers and also among the providers themselves. This collaboration should not focus on the volume and price of separate health care products, but on the patients’ full care cycle and the integral costs and outcomes associated with it. This would have a significant influence on the various interactions among all actors in the health care system.
In an FFS model, a government or other payer composes lists with rigid definitions of billable care “outside” the interaction between payers and providers. Then, in (annual) contract negotiations, the main actors involved in closing the contract usually are the board of the provider organization and a procurement team from the payer, which usually results in an agreement on price and volume per separate service and/or a maximum annual budget. Although this contracting process can be challenging owing to the opposite interests of the payer and the provider, it is clear to all parties how it works and what the rules are. There is no explicit “specification” phase because each year the same lists with predefined billable care are used. This does not encourage the providers to redesign their care processes toward quality improvement or cost containment. Compared with the design and implementation of bundled payments, this is often a much more strategic procurement process. It encompasses “a continuous search for the best interventions to purchase, the best providers to purchase from, and the best payment mechanisms and contracting arrangements to pay for such interventions.”46, 47 (p105)
In contrast to FFS models, under a bundled payment model, the payer and provider(s) try to agree on a contract that better aligns their interests and facilitates a redesign of care processes in order to achieve better‐quality outcomes at lower costs. This entails bundling the full patient journey, which in the past was billed under numerous billable claim codes and from multiple health care organizations. The payer and provider(s) thus need to specify and agree on the specific “care services, patient characteristics and corresponding costs to include in the bundle” (element 3). This can be a cluster of existing billable services (eg, diagnosis‐related groups), but it can also include services that previously may not have been billable (eg, prevention, “shared decision making,” or e‐health). In addition, the payer and provider(s) need to set their expectations and agree on goals concerning the quality of care and (if applicable) potential savings that are feasible and acceptable for both. Although potential shared savings and losses are difficult to predict for both actors, they can (in contrast to the rigid price and volume negotiations under FFS models) be key to a better alignment of their interests (depending on the impact of the bundled payment contract on the provider's total [FFS‐based] revenue). Also, the payer and provider(s) are well advised to “engage professionals in defining the bundle and financial incentives in the contract” (element 9), because several articles report on the importance of this precontractual element to the “acceptance and commitment to implementation of the contract by care professionals” (element 45) in the postcontractual phase.19, 39 For the successful implementation of bundled payments, it is therefore essential that the payer, provider(s), and health care professionals have a clear and explicitly shared understanding of the desired impact of a care bundle on costs and quality and on how this impact is spelled out in the contract.
In short, bundled payment contracts introduce a different set of financial agreements that create both opportunities and risk. They can involve savings and losses based on quality indicators, touch almost all aspects of governance within organizations, and demand a different type of collaboration among organizations. These substantial differences between traditional FFS contracts (which take only price and volume into account) and bundled payments make the transition complex and require a different design and implementation approach. This approach must be more strategic and based less on short‐term transactional negotiations and more on long‐term collaborative relationships between payers and providers.
Implications for Policy and Further Research
The goal of bundled payment contracts is to overcome the flaws of FFS models by reallocating accountability, integrating care across settings, and facilitating value‐based health care delivery, which often requires a change in the behavior of care professionals. Payers must be aware that changing behaviors, especially in the traditions of health care, is very challenging.48 The strategic approach to coordination and adaptation that is needed to achieve this should not be ignored.46 Even if there are clear benefits for patients’ outcomes and financial rewards, the availability of convincing evidence and the implementation of a new procurement contract are generally not enough to ensure widespread change.49 In addition to the payer's perspective, therefore, it is important that future research also focuses on specific barriers and facilitators from the provider's and patient's perspective. Our study shows that bundled payment contracts affect a broad range of health system actors, so their design and implementation should not be approached as merely the introduction of a new contracting model, but as part of a broader transformation to a more sustainable, value‐based health care system. This approach should not focus on the volume and price of separate health care products but on the full care cycle of patients and the integral costs and outcomes associated with it.7, 13
Assuming that the degree of complexity in the design and implementation of bundled payments is influenced not only by the separate elements we have identified but also by the various mutual interactions among these elements, future research should focus on studying these interactions between pre‐ and postcontractual elements in order to develop a better understanding of the causes of this complexity. Based on the many articles we found on the barriers and facilitators related to it, making the right precontractual design choices on the “care services, patient characteristics and corresponding costs to include in the bundle” element is likely to be central. For example, choosing a condition‐based chronic care bundle with a high level of comorbidity and multiple involved providers generally affects more health care costs and therefore might have more potential for positive effects. But these broad bundles also have much more complex interactions among the elements and are therefore harder to implement successfully. While opting for a relatively small, procedure‐based episodic care bundle without comorbidities and with only one involved provider may have less risk and is less complex to implement, the expected positive effects are also likely to be fewer.16, 31, 32 The main challenge for payers that want to implement bundled payment contracts is to find the right balance among these various design options. Future research should therefore concentrate on the impact of precontractual design choices for bundled payments, their underlying design options (and their trade‐offs), and these options’ interactions with the postcontractual care process in order to eventually enable the development of operational implementation strategies for bundled payment contracts.
Conclusions
Our framework provides a structured overview of the principal, literature‐based elements of the design and implementation of bundled payment contracts from a payer's perspective. We identified 53 elements that involve all procurement phases and relate to actors on all levels of the health care system. A better understanding of these elements can help payers and other actors devise a strategic approach and reduce the complexity of implementing these contracts. Compared with traditional FFS models, bundled payment contracts introduce an alternative set of financial incentives that affect the entire health care system, involve almost all aspects of governance within organizations, and demand a different type of collaboration among organizations. This is what makes the design and implementation of bundled payment contracts complex and is why they should not be strategically approached by payers as merely the adoption of a new contracting model but, rather, as part of a broader transformation to a more sustainable value‐based health care system, based less on short‐term transactional negotiations and more on long‐term collaborative relationships between payers and providers.
Supporting information
Appendix A. Definition of a Bundled Payment Contract
Appendix B. Search Strategy
Appendix C. Expert Panel Sessions
Appendix D. Definitions, Explanations, and Literature References
Funding/Support
The Talma Institute health care research program received funding from the Dutch insurance companies Zilveren Kruis, VGZ, CZ, and Menzis, and from the pharmaceutical company GSK.
Conflict of Interest Disclosures: All authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest. Eric van der Hijden reported that he is a part‐time employee of Dutch insurance company Zilveren Kruis.
References
- 1. Ginsburg PB, Grossman JM. When the price isn't right: How inadvertent payment incentives drive medical care. Health Aff (Millwood). 2005;24:W5‐376‐384. [DOI] [PubMed] [Google Scholar]
- 2. McGuire TG. Physician agency and payment for primary medical care. In: Glied S, Smith PC, eds The Oxford Handbook of Health Economics. Oxford, NY: Oxford University Press; 2012. [Google Scholar]
- 3. OECD . Better ways to pay for health care. Organisation for Economic Co‐operation and Development; 2016. https://www.oecd.org/els/health-systems/Better-ways-to-pay-for-health-care-FOCUS.pdf. Accessed December 5, 2019. [Google Scholar]
- 4. Tsiachristas A. Payment and economic evaluation of integrated care. Rotterdam, Netherlands: Erasmus School of Health Policy & Management, Erasmus University; 2015. [Google Scholar]
- 5.(HCP‐LAN ) HCPLAN. Alternative payment model framework. McLean, VA: MITRE Corporation; 2017. https://hcp-lan.org/workproducts/apm-refresh-whitepaper-final.pdf. Accessed December 5, 2019. [Google Scholar]
- 6. Nussbaum S, McClellan M, Metlay G. Principles for a framework for alternative payment models. JAMA. 2018;319(7):653‐654. [DOI] [PubMed] [Google Scholar]
- 7. Porter ME, Kaplan RS. How to pay for health care. Harvard Business Review. 2016;94(7‐8):88‐98, 100, 134. [PubMed] [Google Scholar]
- 8. Miller HD. From volume to value: better ways to pay for health care. Health Aff (Millwood). 2009;28(5):1418‐1428. [DOI] [PubMed] [Google Scholar]
- 9. Berenson RA, Upadhyay DK, Delbanco SF, Murray R. Payment methods: how they work. Urban Institute and Catalyst for Payment Reform; 2016. https://www.urban.org/research/publication/payment-methods-how-they-work. Accessed December 5, 2019. [Google Scholar]
- 10. Prometheus Analytics . Episodes of Care Definitions . Vol. 5.5. Altarum; 2018. http://www.prometheusanalytics.net/deeper-dive/definitions-readable. Accessed December 5, 2019.
- 11. Gronniger T, Fiedler M, Patel K, Adler L, Ginsburg PB. How should the Trump administration handle Medicare's new bundled payment programs? Health Affairs Blog; 2017. https://www.healthaffairs.org/do/10.1377/hblog20170410.059551/full/. Accessed December 5, 2019. [Google Scholar]
- 12. Dummit LA, Kahvecioglu D, Marrufo G, et al. Association between hospital participation in a Medicare bundled payment initiative and payments and quality outcomes for lower extremity joint replacement episodes. JAMA. 2016;316(12):1267‐1278. [DOI] [PubMed] [Google Scholar]
- 13. Wojtak A, Purbhoo D. Perspectives on advancing bundled payment in Ontario's home care system and beyond. Healthcare Q. 2015;18(1):18‐25. [DOI] [PubMed] [Google Scholar]
- 14. Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Evaluation of Medicare's bundled payments initiative for medical conditions. N Engl J Med. 2018;379(3):260‐269. [DOI] [PubMed] [Google Scholar]
- 15. Tavare A, Jayakumar P. The experience and impact of bundled payment in orthopaedic surgery: a systematic review. Value in Health. 2017;20(5):A42‐A43. [Google Scholar]
- 16. Joynt Maddox KE, Sen AP, Samson LW, Zuckerman RB, DeLew N, Epstein AM. Elements of program design in Medicare's value‐based and alternative payment models: a narrative review. J Gen Intern Med. 2017;32(11):1249‐1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Struijs JN, van Gils P, de Vries EF, Baan CA, Rosenthal MB. Current state of bundled payments around the world. Issue Brief. New York, NY: Commonwealth Fund; 2018. [Google Scholar]
- 18. Miller HD. Ten barriers to healthcare payment reform and how to overcome them. Center for Healthcare Quality & Payment Reform; 2012. http://www.chqpr.org/downloads/OvercomingBarrierstoPaymentReform.pdf. Accessed December 5, 2019.
- 19. Conrad DA. The theory of value‐based payment incentives and their application to health care. Health Serv Res. 2015;50(Suppl. 2):2057‐2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pham HH, Ginsburg PB, Lake TK, Maxfield MM. Episode‐based payments: charting a course for health care payment reform. NIHCR Policy Analysis, no. 1. Washington, DC: National Institute for Health Care Reform; 2010. https://www.nihcr.org/publications/episode-based-payments/. Accessed December 5, 2019. [Google Scholar]
- 21. Blumenthal D, Squires D. The Promise and Pitfalls of Bundled Payments. To the Point. New York, NY: Commonwealth Fund; 2016. https://www.commonwealthfund.org/blog/2016/promise-and-pitfalls-bundled-payments. Accessed December 5, 2019. [Google Scholar]
- 22. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Meth. 2005;8(1):19‐32. [Google Scholar]
- 24. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5(69). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sanderson J, Lonsdale C, Mannion R, Matharu T. Towards a framework for enhancing procurement and supply chain management practice in the NHS: lessons for managers and clinicians from a synthesis of the theoretical and empirical literature. Southampton, UK: Health Services and Delivery Research; 2015. [PubMed] [Google Scholar]
- 26. van Raaij EM. Purchasing value: purchasing and supply management's contribution to health service performance. Rotterdam, Netherlands: Erasmus School of Health Policy & Management, Erasmus University; 2016. [Google Scholar]
- 27. van Weele AJ, van Berkel‐Schoonen J, Walhof G. Procurement from a Strategic Perspective. 7th ed Alphen, Netherlands: Vakmedianet; 2017. [Google Scholar]
- 28. Concannon TW, Meissner P, Grunbaum JA, et al. A new taxonomy for stakeholder engagement in patient‐centered outcomes research. J Gen Intern Med. 2012;27(8):985‐991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Reschovsky JD, Rich EC, Lake TK. Factors contributing to variations in physicians’ use of evidence at the point of care: a conceptual model. J Gen Intern Med. 2015;30(Suppl. 3):S555‐S561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Porter ME, Kaplan RS. How should we pay for health care? Harvard Business Review. 2014:15‐041. [PubMed] [Google Scholar]
- 31. Bailit M, Burns MBAM, Houy MPPM. Bundled payments one year later: an update on the status of implementations and operational findings. Health Care Incentives Improvement Institute; 2015. http://www.bailit-health.com/publications/2013-0610-HCI3-issue%20brief.pdf. Accessed December 5, 2019. [Google Scholar]
- 32. Matchar DB, Nguyen HV, Tian Y. Bundled payment and care of acute stroke: what does it take to make it work? Stroke. 2015;46(5):1414‐1421. [DOI] [PubMed] [Google Scholar]
- 33. Mechanic RE. Medicare's Bundled Payment Initiatives: Considerations for Providers. Washington, DC: American Hospital Association; 2016. [Google Scholar]
- 34. Conrad DA, Grembowski D, Hernandez SE, Lau B, Marcus‐Smith M. Emerging lessons from regional and state innovation in value‐based payment reform: balancing collaboration and disruptive innovation. Milbank Q. 2014;92(3):568‐623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ridgely MS, de Vries D, Bozic KJ, Hussey PS. Bundled payment fails to gain a foothold in California: the experience of the IHA bundled payment demonstration. Health Aff (Millwood). 2014;33(8):1345‐1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. RAND Corporation . Analysis of Bundled Payment. Santa Monica, CA: RAND Corporation; 2009. https://www.rand.org/pubs/technical_reports/TR562z20/analysis-of-bundled-payment.html. Accessed December 5, 2019. [Google Scholar]
- 37. Averill RF, Goldfield NI, Hughes JS, Eisenhandler J, Vertrees JC. Developing a prospective payment system based on episodes of care. J Ambulatory Care Manage. 2009;32(3):241‐251. [DOI] [PubMed] [Google Scholar]
- 38. Hussey PS, Ridgely MS, Rosenthal MB. The PROMETHEUS bundled payment experiment: slow start shows problems in implementing new payment models. Health Aff (Millwood). 2011;30(11):2116‐2124. [DOI] [PubMed] [Google Scholar]
- 39. George M, Bencic S, Bleiberg S, Alawa N, Sanghavi D. Case study: delivery and payment reform in congestive heart failure at two large academic centers. Healthcare (Amsterdam). 2014;2(2):107‐112. [DOI] [PubMed] [Google Scholar]
- 40. Hussey PS, Mulcahy AW, Schnyer C, Schneider EC. Closing the quality gap: revisiting the state of the science (vol. 1: bundled payment: effects on health care spending and quality). Evid Rep Technol Assess. 2012;(208.1):1‐155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bushnell BD. Bundled payments in orthopedic surgery. Orthopedics. 2015;38(2):128‐135. [DOI] [PubMed] [Google Scholar]
- 42. Shih T, Chen LM, Nallamothu BK. Will bundled payments change health care? Examining the evidence thus far in cardiovascular care. Circulation. 2015;131(24):2151‐2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Porter ME, Lee TH. From volume to value in health care: the work begins. JAMA. 2016;316(10):1047‐1048. [DOI] [PubMed] [Google Scholar]
- 44. Sutherland JM, Hellsten E, Yu K. Bundles: An opportunity to align incentives for continuing care in Canada? Health Policy. 2012;107(2‐3):209‐217. [DOI] [PubMed] [Google Scholar]
- 45. Conrad DA, Vaughn M, Grembowski D, Marcus‐Smith M. Implementing value‐based payment reform: a conceptual framework and case examples. Med Care Res Rev. 2016;73(4):437‐457. [DOI] [PubMed] [Google Scholar]
- 46. Sanderson J, Lonsdale C, Mannion R. What's needed to develop strategic purchasing in healthcare? Policy lessons from a realist review. Int J Health Policy Manage. 2018:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. WHO . The World Health Report 2000—Health Systems: Improving Performance. Geneva, Switzerland: World Health Organisation; 2000. https://www.who.int/whr/2000/en/. Accessed December 5, 2019. [Google Scholar]
- 48. Bohmer RMJ. The hard work of health care transformation. N Engl J Med. 2016;375(8):709‐711. [DOI] [PubMed] [Google Scholar]
- 49. Moriates C, Arora V, Shah N. Implementing value‐based initiatives: a new challenge for clinicians and healthcare systems. In McGraw‐Hill Education, Understanding Value‐Based Healthcare, chap. 16. 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix A. Definition of a Bundled Payment Contract
Appendix B. Search Strategy
Appendix C. Expert Panel Sessions
Appendix D. Definitions, Explanations, and Literature References


