Abstract
Currently, some 50% of the US population has a chronic disease, creating an epidemic, and 86% of health care costs are attributable to chronic disease. The medical profession and its leadership did not recognize or respond appropriately to the rising prevalence of chronic disease. As a consequence, a health care crisis emerged, with inadequate access to care and quality of care together with excessive costs. In the years since the 1950s, when the chronic disease prevalence grew, the clinical literature did not follow. It remained preoccupied with acute disease. Similarly, medical education did not change. Studies and critiques gave little or modest attention to the rising dominance of chronic disease and neglected elements of good care. Recently, some health services responding to their growing number of patients with chronic illness have designed and tested new ways of providing care. They have found that, as a result, the patient's health outcomes were improved, costs of care were lower, and patient satisfaction was higher. These results and experiences provide examples of what can be done. The health care crisis and the emergence of a chronic disease epidemic coincided to a substantial degree. Although the epidemic did not cause the crisis, it contributed significantly. Now, the medical profession and its leadership are confronted by the responsibility to build a practice of medicine and a health care system that better meet the needs of patients with chronic illness and reduces the health care crisis.
Introduction
In the 1950s, a profound transition occurred in the dominant type of health problems in this country—a transition from acute diseases to chronic diseases. The transition began when antibiotic use became widespread, infectious disease prevalence subsided, and the population aged. It is depicted in Figure 1 by the crossover of death rates from infectious (acute) and noninfectious (chronic) lung disease.
Figure 1.
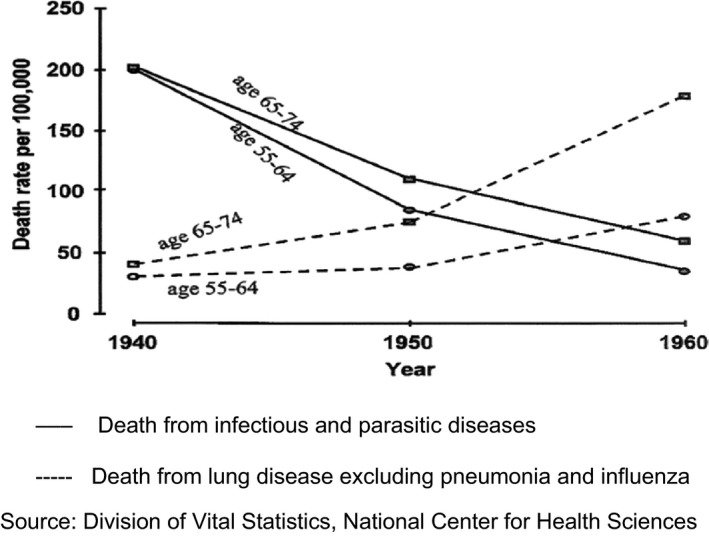
Death rates per 100 000 US white men. Solid lines represent death from infectious and parasitic diseases. Dashed lines represent death from lung disease, excluding pneumonia and influenza. Adapted with permission from Division of Vital Statistics, National Center for Health Sciences.
My professional life, which began in 1955, has witnessed a steadily growing health care crisis: absent or unequal access to care for many, inadequate or poor care for others, and exploding costs of care. In parallel, the clinical training of physicians has not met society's emerging or future needs but rather has served to perpetuate its past. Over the same years, many forces have impacted health care, bending it to their interests—drug and insurance industries, medical associations, social beliefs and prejudices, and government policies 1. But beyond the impacts of these forces, there are other crucial reasons for the present situation. They fall within the purview of the medical profession. The profession and its leadership failed to recognize or respond appropriately to the wave of chronic disease.
Although some health services have worked to improve matters in their own practices or teaching settings or have supported alternative policies, their success has been limited. The profession has accepted, supported, and benefited from the health system that created the current situation.
Soon after the transition, the prevalence of chronic diseases began a steady rise to become the dominant cause of illness in the United States. As the prevalence rose, so did the costs of health care. For example, in the decade of the 1980s, the prevalence of major chronic diseases (eg, diabetes, heart disease, and high blood pressure) rose between 40% and 150%, whereas health care expenditures tripled 2 (Figure 2). In the last 20 years, the prevalence of chronic disease in the United States has grown by a steady 7 to 8 million people every 5 years. Today, chronic disease affects 50% of the population, and its care consumes more than 85% of health care costs 3. It has become an epidemic.
Figure 2.
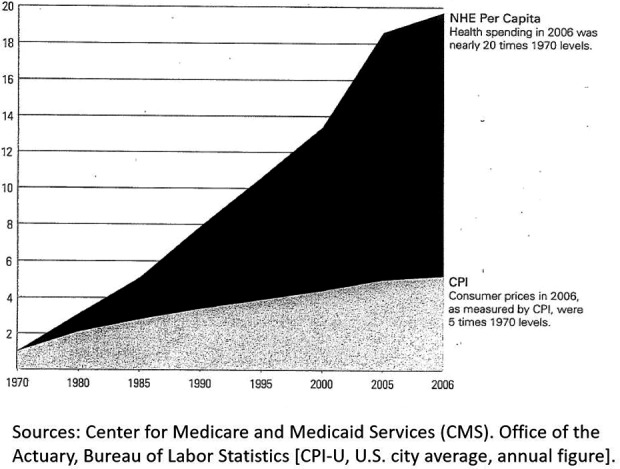
Comparison of the national health expenditure (NHE) annual cost per capita with the annual cost of living. CPI, consumer price index. Adapted with permission from Center for Medicare and Medicaid Servicces (CMS) Office of the Actuary, Bureau of Labor Statisitcs.
What are the differences between acute and chronic disease? Table 1 lists some that have implications for the way care is given. When the central health problem changed, the care did not. For years, there was little or no mention of the emerging chronic disease dominance in the medical literature and little change in the way medicine was practiced or taught. Medical care remained in its acute disease orientation (individual private practice, fee‐for‐service payment, poor continuity and coordination of care, patient passivity, and physician dominance). In 1965, the federal government, recognizing the dire consequences of rising costs, enacted Medicare and Medicaid to assist the elderly and poor in gaining access to care.
Table 1.
Differences between acute and chronic disease that are relevant to health care
| Acute Disease | Chronic Disease |
|---|---|
| Sudden onset | Gradual onset |
| Cure usual | Cure rare |
| Course short | Course lengthy |
| Patient passive | Patient active, caregiver |
| Physician dominant | Team care, patient included |
| Return to normal likely | Return to normal unlikely |
| Future uncertainty rare | Future uncertainty common |
As the cost crisis grew, policy makers urgently sought ways to halt the escalation, seemingly unaware of the cost impacts of chronic disease. Their focus was mainly on financial incentives for physicians to practice more efficiently (managed care, pay‐for‐performance, and Accountable Care Organizations) and on shifting costs to patients (deductibles, copays, and health savings accounts). Independent case management programs and medical homes arose as possible cost‐reducing solutions. None has had more than limited success 4, 5, 6.
In the 1980s important things happened. First, the Centers for Disease Control and Prevention's (CDC's) Morbidity and Mortality Weekly Report began recording information about chronic disease. Second, in 1988, the National Center for Chronic Disease Prevention and Health Promotion was established at the CDC. Thus, reliable information came available to the profession and potentially the public. Third, some health professionals began to study chronic disease and its impact: Lois Verbrugge in 1984, Anselm Strauss in 1987, and Dorothy Rice in 1995 7. This led to analyses of health patterns and to better ways to measure a person's health. In 1990, the National Committee on Quality Assurance was privately formed to establish standards for health care.
In subsequent years, debate intensified as health care costs continued to grow faster than the general cost of living, and the quality of care was often inadequate 8, 9, 10. In 2009, the Institute of Medicine found that some 30% of health care costs were wasted 11, 12, 50% of which was caused by unnecessary or insufficient care mainly related to the way chronic care is managed.
Alleged causes for this situation have ranged from lack of appropriate government insurance programs to excessive regulation of the free market, with many positions in between. The debate ultimately resulted in the passage of the Affordable Care Act (ACA) and continues to this day in the efforts to repeal the ACA. Almost nowhere in the debate has there been meaningful attention to the dominance of chronic disease or the need for a different type of health care to cope with it.
Corrective innovation
By failing to recognize the rising burden of chronic disease, the profession also failed to learn that effective and efficient management of chronic disease requires a different structure of care and practice of medicine from that of acute diseases. But some practices and health services that had to provide care for the burgeoning number of patients with chronic disease began to search for better ways to do it. Innovations were introduced and tested by Group Health Cooperative of Seattle 13, the Kaiser Permanente Health System 14, Intermountain Healthcare 15, the Geisinger Health System 16, Guided Care at Johns Hopkins University 17, Community Care of North Carolina 18, the German National Health Insurance Program 19, and some neighborhood clinics 20 (Table 2).
Table 2.
Practice components employed by innovations
|
|
|
|
|
|
|
Using combinations of these innovations, many of which were joined together in the Chronic Care Model of practice 21, 22, the organizations found that they not only improved the quality of care but also decreased costs. Improved quality arose from enhanced self‐care, fewer complications from disease or treatment, and greater satisfaction for patients and physicians. Lesser costs resulted from greater patient involvement in care, reduced emergency department visits, and fewer hospitalizations. For example, when Group Health Cooperative improved coordination of care, access to care, and goal setting with patients, several things happened: patient involvement increased, hospitalizations declined 6%, emergency department visits declined 29%, and costs diminished $10.3 per patient per month. When Intermountain Healthcare increased self‐care, it found improved outcomes for depression and diabetes and 10% fewer hospitalizations. The German Health Insurance Program compared results from using the Chronic Care Model for 10 000 patients with diabetes with results from an equal number of patients with diabetes receiving usual care over 4 years. The study group had 50% fewer deaths, 25% fewer disease complications, and 11% less costs.
These results were obtained mostly by primary care physicians (family physicians, internists, and pediatricians) who sought to improve their care and teach through practice and service modification. But the results are not just relevant to primary care. In various ways, they are pertinent to any physician or practice whose patients have a chronic illness.
Success of the practice innovations depends on behavior change by all involved, not on different uses of medicines or surgery. The physician becomes a partner of the patient who adjusts treatment to the patient's health state and wishes. The patient, who must bear the consequences of the disease and treatment, becomes a caregiver and care team member, executing the treatment plan daily. A nonphysician team member maintains remote contact with the patient, facilitating the treatment plan. The health service assures support of the health team and needed changes in the treatment plans as they evolve. Such a practice pattern, similar to that proposed by Engel in 1977 23, will create a mood and logic of collegiality that is central to success with a chronic illness.
A glimpse of current practice outcomes
During the years of these practice innovations, the Dartmouth Center for Evaluative Clinical Sciences, analyzed the care given patients with serious chronic illness during the last 2 years of their lives 24, 25. Using Medicare data, the study was nationwide, covering patients from many health services. The results were striking. They revealed widespread variation in the scope and costs of care received by patients with the same diagnosis and in the practices of physicians who had the same certification or specialty. The variation was found between similarly trained physicians located on the same street or in different cities. Substantial variation was also present among the faculty clinical practices of university hospitals, where clinical training of physicians occurs. Such results show that changes or differences in “usual” care are common and could be expanded to improve both quality and cost. The Dartmouth investigators estimated a health care cost saving of 30% if all physicians practiced like the best they encountered.
Although there has been considerable discussion about the reasons for the variation in the Dartmouth studies, such as physician training and patient cultures, there has been no meaningful challenge to the study design, the relevance of the data, or the patient outcomes, which, of course, was death in every case 26.
Elsewhere, other ways to improve care have emerged. An example is the Hospital in the Home Program started in Victoria, Australia 27. Developed to avoid the costs of hospital construction, the program provides usual hospital services in the home. Particularly suitable for patients with chronic disease, it has achieved increased patient satisfaction, reduced mortality, and lower costs compared with regular hospital care. A striking innovation is the British New Care Model program. Patients with complex health needs are given a “personal budget” to purchase their own services. Together with their health care team, patients develop a care plan that covers their perceived medical and social needs 28.
The many innovations and experiences are not in themselves an end. Rather, they are a beginning on which new and better services and practices can be built, and they illustrate the plasticity of medical practice and its potential for change. They are also the basis on which medical education can appropriately prepare students for their futures.
The abdication by medical education
Although some academicians participated in the debate about costs and quality and ultimately in the design of the ACA, they were mostly from economic and policy disciplines. Notably absent were most leaders of medical organizations and medical schools.
The abdication by academic medicine is particularly important. Although organized medicine functions generally as a guild protecting the financial interests of physicians, academic medicine must train the physicians of the future.
After the 1950s, when the transition began, academic medicine was absorbed in the new biology and technology of medicine that emerged from World War II. The understanding of abnormal biology and the extent of medical practice (surgical techniques and new medications) expanded rapidly. “Half‐way technologies” emerged that had benefits for patients but not a cure (organ transplantation, antineoplastic drugs, the artificial heart, immunosuppressants, and psychoactive medications). However, the organization of care and the forms of medical practice remained largely unchanged. Attention to a new type of disease that was chronic and had major implications for the organization and practice of medicine was not on their agenda.
Between 1953 and 2016, some 30 reports appeared calling for reform of medical education. They came from academicians, major medical education agencies, foundations, and medical organizations 29, 30, 31, 32. The proposed reforms dealt with a huge array of matters. Common among them were insistence that medicine serve better the needs of society, criticism of inadequate training in professionalism, the need to cope with burgeoning medical knowledge, and reducing the fragmentation of medical care. However, the ways to do these things were commonly absent, and throughout the reports, there was virtually no mention of the chronic disease predominance or the need to change health care and medical practice to address it. The reports led to little action 33, 34.
The shortcomings of medical education were revealed by two studies from the Johns Hopkins School of Medicine. In 2001, a random sample of all US physicians who practice at least 20 hours weekly were questioned about their training for care of patients with chronic disease 35. They reported that their training had not prepared them to 1) educate patients with chronic disease (66%), 2) coordinate in‐home and community services (66%), 3) provide end‐of‐life care (65%), 4) manage geriatric syndromes (65%), 5) manage psychological and social aspects of chronic care (64%), 7) assess caregiver and family needs (63%), 8) provide nutritional advice (63%), or 9) develop teamwork with nonphysician care providers (61%). It is highly relevant that these education failures accord directly with the needed practice changes identified by the aforementioned health services 15, 16, 17, 18, 19, 20, 21, 22, 23 (Table 2) that have had success in chronic disease care.
The second Johns Hopkins study reported in 2004 on the content of required clerkships and courses at 16 representative US medical schools 36. They surveyed 70 directors of the programs about the teaching in their curriculums of 49 different skills or practices that are widely considered relevant to the management of chronic disease. The directors were asked to rate the importance of each skill or practice in their teaching. Only 29 of the 49 skills were rated moderately important or more, and none was considered essential by the group.
Academic medicine's low concern for chronic disease or the role of the patient with chronic disease was reflected in the agenda items of their meetings or the section headings of their reports. For six broad health policy meetings in 2000‐2001 and for the Association of American Medical Colleges (AAMC) annual meetings in 1996‐2001, the words “chronic disease” or “patient role” appeared only 10 times in 262 agenda items or section headings. For the AAMC, they appeared twice in 150 items in 6 agendas 37.
This is surprising in that medical faculties practice medicine, have witnessed the changing character of disease in their practices, and have had access to the CDC data. Because the medical residency and fellowship are where trainees learn to practice medicine, academic medical practices must epitomize that which is necessary and good for the students’ future practice; concerning chronic disease, which will be the bulk of that practice, they have not. Furthermore, health services research, which is a task of medical schools, has suffered from the neglect of chronic disease care. It struggles to make sense of health care quality and expense in a system marked by fragmentation and fee‐for‐service payment. If the system seriously addressed chronic care, it would have opened the path to creative new investigation.
However, there has been some indirect academic responses to the failures. In 1999, the Accreditation Council for Graduate Medical Education (ACGME) introduced six milestones of clinical competency that had to be met in the training of residents in order for the trainees and the training programs to be accredited 38. Initially, the milestones involved processes of care that the trainees had to learn; in a later version, the processes were replaced by patient outcomes to be achieved. The milestones could apply to any form of practice with acute or chronic disease, and thus accreditation could be given to a candidate or program without competence or teaching in the components of good chronic care.
The literature of the ACGME speaks of “education of physicians to provide care for Americans into the middle of the century” 39. Those years “into the middle” will be inundated with chronic illness, but that literature does not describe an appropriate practice for chronic disease about which programs and trainees should learn and be evaluated. In 2011, Glenn Hackbarth, Chairman of the Medicare Payment Advisory Commission, wrote the following statement:
U.S. health care is too expensive and its quality too inconsistent. To ensure that health care will be affordable for future generations and appropriate for our burgeoning geriatric population, its delivery and organization must change. Physicians should be in the vanguard of this change, and transforming medical education will be instrumental in preparing tomorrow's physicians to lead the way 40.
The commission proposed that Congress authorize Medicare to withhold one‐third of the $9.5 billion it gives annually for graduate medical education (GME). The withheld funds would be awarded as supplements to those GME programs that develop new practices and teachings that lower the costs and improve the quality of health care. However, Congress did not act 41.
The nonrecognition continues
Recently, the National Academy of Medicine completed an initiative entitled “Vital Directions for Health and Health Care.” Summary reports of the 19 working groups of the initiative were published in JAMA on October 25, 2016. They contain useful concepts and suggestions. But most are not new. Most are generalizations without implementation plans. Even when addressing high‐need, high‐cost (chronic disease) patients, there is little mention of the chronic disease epidemic, of the needed change in the practice of medicine, or of the role of the patient.
Most readers of the Academy's initiative, I suspect, will be wondering how all this can be done. A good source of answers to that question was apparently left out by the Academy. As the final editorial of that issue of JAMA indicates, “larger scale exemplars of innovation, efficiency and innovation” appear not to have had much impact in the participant's thinking. Who are those exemplars identified in the editorial? They are the health care organizations described as innovators herein: the Kaiser Permanente Health System, Group Health Cooperative of Seattle, Intermountain Healthcare, and Geisinger Health. Their patterns of care and accomplishments do not appear in the 19 reports.
In the decades since the transition in dominant disease, it is striking that the appropriateness of medical practice has rarely been raised in the vast literature on the health care crisis. The practices appear to be sacrosanct, susceptible to alteration by new bioscience or technology, but not otherwise. It seems not to matter that the major health problem confronting the practice of medicine has changed dramatically; the old practice pattern need not be challenged or altered. This was especially true in the debate on replacing the ACA. It revolved primarily around costs, with little mention of quality of care or of the ways that institutions, here and abroad, have achieved greater effectiveness and efficiency in their practices. The debate was intellectually barren, with few penetrating analyses or new proposals to improve health care.
New beginnings and new roles
The decades have given time for some physicians and services to develop and test some new ways to manage chronic illness. They have had success and have identified ingredients for significant advance in the practice of medicine 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 (Tables 1 and 2).
Adopting this path will reset the profession toward its fundamental responsibility in health care, and it will not require new construction or new technology. Rather, the new forms of medical practice will require new roles for the physician and other health professionals, the patient, and the health service:
The physician becomes a partner with the patient, particularly when guiding and sharing treatment. This ensures that the patient's interests are merged with the care decisions throughout the long illness.
The patient with chronic illness becomes an equal, functioning member of the health care team. This is crucial because she or he must execute much of the treatment and bear the consequences of both the disease and the treatment. Such tasks impact the patient's life activities and must be integrated with them. This requires new learning and coaching for the patient 42, 43. Conversely, the patients’ experiences provide unique and critical understanding of the problem at hand, especially in management situations in which change is necessary and uncertainty prevails.
The health service is responsible for support of these new roles, a task distinct from generating profit.
Successful care of patients with chronic disease, requires change in behavior by all participants. It may be long before we learn how to rectify the abnormal biology of chronic diseases. Until then, we should deal effectively with their consequences.
Conclusions
Sixty years ago, a new and dominating health problem emerged: chronic disease. It has now reached epidemic proportions, affecting 50% of the population and consuming 86% of health care expenditures. The fundamental responsibility of the medical profession is to create a health care system and a practice of medicine that meet the needs of current illnesses and patients. The profession has not done so. The forces that block it are not blind forces. They are decisions made by people, primarily the leadership. The decisions can be analyzed and reversed, and the decision‐makers can be held accountable. Until that occurs, the profession cannot meet its fundamental responsibility. When will we awaken?
Author contributions
Dr. Holman drafted the article, revised it critically for important intellectual content, and approved the final version to be published.
No potential conflicts of interest relevant to this article were reported.
References
- 1. Starr P. The social transformation of American medicine: the rise of a sovereign profession and the making of a vast industry. New York: Basic Books; 1982. [Google Scholar]
- 2. Verbrugge LM. Longer life but worsening heath? Trends in health and mortality of middle‐aged and older persons. Milbank Mem Fund Q Health Soc 1984;62:475–519. [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention . Chronic Disease Prevention and Health Promotion, Chronic Disease Overview, 2017. URL: https://www.cdc.gov/chronicdisesase/overview/.
- 4. Epstein AM. Pay for performance at the tipping point. N Engl J Med 2007;356:515–7. [DOI] [PubMed] [Google Scholar]
- 5. Congressional Budget Office . Lessons from Medicare's demonstration projects on disease management, care coordination, and value‐based payment. 2012. URL: https://www.cbo.gov/sites/default/files/112th-congress-2011-2012/reports/01-18-12-MedicareDemoBrief.pdf.
- 6. Pinkovskiy ML. The impact of the manage care backlash on health care costs: evidence from state regulation of managed care cost containment practices. New York: Federal Reserve Bank of New York; 2013. [Google Scholar]
- 7. Hoffman C, Rice D, Sung HY. Persons with chronic conditions: their prevalence and costs. JAMA 1996;276:1473–9. [PubMed] [Google Scholar]
- 8. McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003;348:2635–45. [DOI] [PubMed] [Google Scholar]
- 9. Institute of Medicine . The 1st annual Crossing the Quality Chasm Summit: a focus on communities: report of a summit. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 10. Schoen C, Davis K, How SK, Schoenbaum SC. U.S. health system performance: a national scorecard. Health Aff (Millwood) 2006;25:w457–75. [DOI] [PubMed] [Google Scholar]
- 11. Berwick DM, Hackbartth AD. Eliminating waste in US health care. JAMA 2012;307:1513–6. [DOI] [PubMed] [Google Scholar]
- 12. Cutler DM. What is the US health spending problem? [perspective]. Health Aff (Millwood) 2018;37:493–7. [DOI] [PubMed] [Google Scholar]
- 13. Reid RJ, Coleman K, Johnson EA, Fishman PA, Hsu C, Soman MP, et al. The group health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29:835–43. [DOI] [PubMed] [Google Scholar]
- 14. Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large‐scale hypertension program. JAMA 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reiss‐Brennan B, Brunisholz KD, Dredge C, Briot P, Grazier K, Wilcox A, et al. Association of integrated team‐based care with health care quality, utilization, and cost. JAMA 2016;316:826–34. [DOI] [PubMed] [Google Scholar]
- 16. Paulus RA, Davis K, Steele GD. Continuous innovation in health care: implications of the Geisinger experience. Health Aff (Millwood) 2008;27:1235–45. [DOI] [PubMed] [Google Scholar]
- 17. Hostetter M, Klein S, McCarthy D, Hayes SL. Guided care: a structured approach to providing comprehensive primary care for complex patients. New York: The Commonwealth Fund; 2016. [Google Scholar]
- 18. Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA Jr. Community care of North Carolina: improving care through community health networks. Ann Fam Med 2008;6:361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stock S, Drabik A, Busher G, Graf C, Ullrich W, Gerber A, et al. German diabetes management programs improve quality of care and curb costs. Health Aff (Millwood) 2010;29:2197–205. [DOI] [PubMed] [Google Scholar]
- 20. Bodenheimer T. Lessons from the trenches: a high‐functioning primary care clinic. N Engl J Med 2011;365:5–8. [DOI] [PubMed] [Google Scholar]
- 21. Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78. [DOI] [PubMed] [Google Scholar]
- 22. Holman H. Chronic disease: the need for a new clinical education. JAMA 2004;292:1057–9. [DOI] [PubMed] [Google Scholar]
- 23. Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977;196:129–36. [DOI] [PubMed] [Google Scholar]
- 24. Wennberg J, Fisher E. The care of patients with severe chronic illness: a report on the Medicare program. Lebanon, NH: Dartmouth Atlas of Health Care; 2006. [PubMed] [Google Scholar]
- 25. Medicare Payment Advisory Commission . Report to the Congress: measuring regional variation in service use. Washington, DC: Medicare Payment Advisory Commission; 2009. [Google Scholar]
- 26. Holman H. Variations Revisited. Health Aff (Millwood) 2004;23 Suppl 2:VAR‐5–VAR‐144. [Google Scholar]
- 27. Ticona L, Schulman KA. Extreme home makeover: the role of intensive home health care. N Engl J Med 2016;375:1707–9. [DOI] [PubMed] [Google Scholar]
- 28. O'Shea L, Bindman AB. Personal health budgets for patients with complex needs. N Engl J Med 2016;375:1815–7. [DOI] [PubMed] [Google Scholar]
- 29. Milstein A. Trailing winds and personal risk tolerance: transforming medical education and training to meet the needs of patients and society. Paper presented at the 2010 American Board of Internal Medicine Foundation Forum; 2010; Vancouver, Canada.
- 30. Cooke M, Irby DM, Sullivan W, Ludmerer KM. American medical education 100 years after the Flexner report. N Engl J Med 2006;355:1339–44. [DOI] [PubMed] [Google Scholar]
- 31. Cooke M. Cost consciousness in patient care: what is medical education's responsibility? [perspective]. N Engl J Med 2010;362:1253–5. [DOI] [PubMed] [Google Scholar]
- 32. Iglehart JK. Financing graduate medical education: mounting pressure for reform. N Engl J Med 2012;366:1562–3. [DOI] [PubMed] [Google Scholar]
- 33. Ludmerer KM. The history of calls for reform in graduate medical education and why we are still waiting for the right kind of change. Acad Med 2012;87:34–40. [DOI] [PubMed] [Google Scholar]
- 34. Christakis NA. The similarity and frequency of proposals to reform US medical education: constant concerns. JAMA 1995;274:706–11. [PubMed] [Google Scholar]
- 35. Darer JD, Hwang W, Pham HH, Bass EB, Anderson G. More training needed in chronic care: a survey of US physicians. Acad Med 2004;79:541–8. [DOI] [PubMed] [Google Scholar]
- 36. Pham HH, Simonson L, Elnicki DM, Fried LP, Goroll AH, Bass EB. Training U.S. medical students to care for the chronically ill. Acad Med 2004;79:32–40. [DOI] [PubMed] [Google Scholar]
- 37. Holman H. With Privilege Comes Responsibility: Does Academic Medicine Lead? Presidential Gold Medal Address to the American College of Rheumatology. 2001, November 13.
- 38. Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system: rationale and benefits. N Engl J Med 2012;366:1051–56. [DOI] [PubMed] [Google Scholar]
- 39. Nasca TJ, Weiss KB, Bagian JP. Improving clinical learning environments for tomorrow's physicians. N Engl J Med 2014;370:991–3. [DOI] [PubMed] [Google Scholar]
- 40. Hackbarth G, Boccuti C. Transforming graduate medical education to improve health care value. N Engl J Med 2011;364:693–5. [DOI] [PubMed] [Google Scholar]
- 41. Witteles RM, Verghese A. Accreditation Council for Graduate Medical Education (ACGME) milestones: time for a revolt? [viewpoint]. JAMA Intern Med 2016;176:1599–1600. [DOI] [PubMed] [Google Scholar]
- 42. Bodenheimer T, Handley MA. Goal‐setting for behavior change in primary care: an exploration and status report. Patient Educ Couns 2009;76:174–80. [DOI] [PubMed] [Google Scholar]
- 43. Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW Jr, Bandura A, et al. Chronic disease self‐management program: 2‐year health status and health care utilization outcomes. Med Care 2001;39:1217–23. [DOI] [PubMed] [Google Scholar]


