Abstract
Study Objective:
The objective of the study was to identify factors associated with negative patient experiences with Essure.
Design:
This was a retrospective cohort study and follow-up survey.
Setting:
The study was conducted in an academic setting.
Patients:
Patients included women who had an Essure placed between 2002 and 2017.
Methods:
The hospitals' database was queried to identify subjects and charts were reviewed to confirm medical information. Subjects were invited by mail, e-mail, or phone call to participate a survey regarding symptoms and satisfaction with Essure. A comparison was made between women who reported a negative experience with Essure versus those who did not. A multivariable logistic regression analysis was performed to identify subject or procedural characteristics associated with any negative experience with Essure sterilization.
Results:
Two hundred eighty-four women underwent Essure sterilization between 2002 and 2017, 42.3% of whom responded to the follow-up survey. Satisfaction with Essure was reported by 61.9% of respondents. Thirty-three percent of the respondents have undergone removal or desire removal of the device. The most frequent symptoms attributed to Essure were pelvic pain, dyspareunia, and vaginal bleeding. Forty-eight percent of the respondents were identified as having any negative experience with Essure. Factors associated with negative experiences with Essure included young age at placement (odds ratio [OR] 0.86; 95% confidence interval [CI] 0.79–0.94; P < .001), high gravidity (OR 1.39; 95% CI 1.14–1.71; P = .002), and absent history of abdominal surgery (OR 0.35; 95% CI 0.12–1.00; P = .049).
Conclusion:
Young age at placement, high gravidity, and absent history of abdominal surgery are factors associated with negative patient experiences following Essure sterilization. A negative experience with Essure is common, although dissatisfaction with the device is not always attributable to symptoms. This information could be considered when counseling women who plan removal of Essure.
Implications Statement:
Our study provides new follow-up data with respect to hysteroscopic sterilization. This research is the first to examine any cause for negative patient experiences with Essure. Understanding factors associated with negative patient experiences could improve patient counseling regarding the extent to which symptoms could be attributed to Essure as well as counseling women who want to undergo removal of the device. These factors could in turn prove to be predictors for successful resolution of symptoms after removal of Essure. Results of this study could also be used for developing future hysteroscopic sterilization techniques.
Keywords: adverse events, Essure, hysteroscopic sterilization, patient satisfaction, removal
INTRODUCTION
In 2002, the Essure (Bayer, Whippany, NJ) device was introduced as a hysteroscopic sterilization technique in the United States. The 4-cm-long flexible device consists of outer nitinol coils and an inner component of polyethelene terephthalate and stainless steel.1,2 For the sterilization procedure, a device is placed in each fallopian tube transcervically at time of hysteroscopy. This results in tubal fibrosis and occlusion of the proximal fallopian tubes within 3 months. In comparison with laparoscopic sterilization, hysteroscopic sterilization does not require abdominal incisions or general anesthesia and can be performed in the office setting with a quick recovery. This may be of benefit specifically for women with significant comorbidities or if laparoscopic surgery is contraindicated.3,4 A 5-year effectiveness rate up to 99.8% has been reported, and follow-up studies demonstrate that most the women who undergo the procedure are highly satisfied.5,6
Although Essure is an effective sterilization method, there is emerging criticism about the device and the potential for adverse effects.7 Because of these concerns, the manufacturer stopped sales in the United States as of the end of 2018.8 Symptoms that have been attributed to Essure include pelvic pain, abnormal vaginal bleeding, dyspareunia, allergy, headaches, fatigue, skin issues, bloating, nausea, weight gain, and depression.9 Research investigations have reported a 1.1–4.2% risk of postprocedure adverse events related to the Essure device.7,12 Removal of the Essure device is increasingly performed, although may not resolve symptoms in all cases9,10 Prior investigations into adverse events related to Essure are predominantly based on subjects who eventually reported a concern or requested device removal. Less information is available about the symptoms experienced by the population as a whole who underwent the Essure procedure and whether certain factors can identify women at higher risk to develop problems with the device. Women who are at higher risk to develop problems with Essure may benefit the most from Essure removal.
The primary objective of this study is to determine whether any subject or procedural characteristics are associated with negative patient experience after Essure sterilization. Understanding these risk factors could improve patient counseling regarding the extent to which symptoms could be attributed to Essure as well as counseling women who want to undergo removal of the device.
METHODS
We performed a retrospective cohort study of all women who underwent the Essure procedure at Brigham and Women's or Brigham and Women's Faulkner Hospital between 2002 and 2017. The research was approved by the Partner's Institutional Review Board.
To identify cases, the hospital's Research Patient Data Registry was queried using Current Procedural Terminology code 58565 for hysteroscopy, surgical, with bilateral fallopian tube cannulation to induce occlusion by placement of permanent implants. Medical records were then reviewed and cases in which the procedure was discontinued because of placement failure were excluded. Cases in which a confirmatory operative note could not be found were excluded as well because these subjects could not be assumed with certainty to have Essure inserted.
Data were collected by both chart review and mixed-mode subject surveys. Information that was abstracted from the medical records included subject age at procedure, race/ethnicity, body mass index (BMI), gravidity, parity, years since placement, and indication for the procedure. Details collected about the Essure procedure itself included number of coils visible after insertion, intraoperative complications, use of confirmatory imaging, and whether both coils were placed according to the manufacturer's instructions for use stating that 3–8 coils should be visible at the uterotubal junction after placement.11
The survey questions were piloted with both patients and subject matter experts. Patients who were being seen in the Minimally Invasive Gynecologic Surgery clinic were given the survey and interviewed by research staff regarding the readability and comprehensiveness of the questionnaire. After incorporating edits with the patient perspectives, the authors further refined the survey questions. This was done over several rounds to ensure the optimal wording and most inclusive survey questions.
Subjects were invited to participate in the survey by mail, e-mail, or phone call. Additional surveys and reminders were sent to nonresponders after 3 weeks. Those who did not reply by 6 weeks were phoned again to ask for participation. The subject questionnaire included three questions regarding satisfaction with the Essure device on a five-level Likert scale that included a neutral option. In addition to inquiring about occurrence, timing, and duration of symptoms related to the device, the survey also requested information about the demographics of the subject and medical and obstetric history (all of which was confirmed by medical record review if possible). If the information collected by chart review and the survey happened to be discordant, chart review was assumed to be correct. The patient's medical history was complemented with information from the survey. Subjects were also asked about their education and income levels, whether they participated in social media groups related to Essure, and whether they planned or had undergone removal of the device, including information on resolution of symptoms following removal. [Supplemental Attachment 1: Survey Tool].
Based on the survey responses, we divided subjects into two groups (“negative experience with Essure” versus “no negative experience with Essure”). A respondent was classified as having a negative experience with Essure if they reported dissatisfaction, ongoing symptoms attributed to Essure or had undergone/planned removal of the Essure device. Dissatisfaction was defined as negative response (<3 out of 5 on Likert scale) to one of three questions asking about procedure satisfaction, recommendation to a friend or if they would do the procedure again if they had the choice. The baseline characteristics of survey responders and nonresponders were compared, as were characteristics and outcomes among the survey respondents who reported negative experience with Essure versus those who did not. Differences between groups were examined t-tests for normally distributed continuous variables, Wilcoxon rank-sum tests for non-normally distributed continuous variables, and χ2 tests for categorical variables. A multivariable logistic regression analysis was performed to identify factors associated with negative patient experiences after Essure sterilization, controlling for: age at time of procedure, BMI, gravidity, previous abdominal surgery, presences of pain syndrome and psychiatric disease. Outcomes with p-value < 0.05 were considered statistically significant. All statistic tests were performed using Statistical Analysis Software SAS®, version 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
With the Current Procedural Terminology code, 310 subjects were found. Fourteen subjects were excluded because the procedure was discontinued and twelve subjects were excluded because of lack of a confirmatory operative note. In total, 284 subjects met the study inclusion criteria. One hundred and twenty subjects responded to the survey, for a 42.3% response rate. Two subjects responded but did not complete the survey.
Demographics and baseline characteristics for those who responded to the survey and for those who did not respond to the survey were not significantly different for any baseline variable which could be obtained from the medical record [see Supplemental Attachment 2]. All subjects underwent the Essure procedure because of desire for permanent birth control (as opposed to need to occlude hydrosalpinx prior to in vitro fertilization, for example). The primary reasons cited for choosing Essure above other methods for permanent sterilization included (not mutually exclusive): “my doctor suggested it” (43.9% in those with negative experience with Essure, 45.9% in those without negative experience with Essure); “I wanted to avoid abdominal surgery” (33.3% and 49.2%, respectively); “I wanted a short recovery time” (33.3% and 44.3%, respectively); and “I wanted to avoid anesthesia (12.3% and 23%, respectively). Intraprocedural complications reported by the surgeon included lack of vision because of adhesions or thickened endometrial tissue in 5.1% of cases and tubal spasm in 1.7% of cases. Seventy-eight percent of all subjects and 80% of survey respondents underwent confirmation imaging with hysterosalpingogram. Two women had a pelvic ultrasound instead of hysterosalpingogram because of contrast allergy or inability to tolerate a speculum. In one case, the device was removed prior to confirmatory imaging because of symptoms.
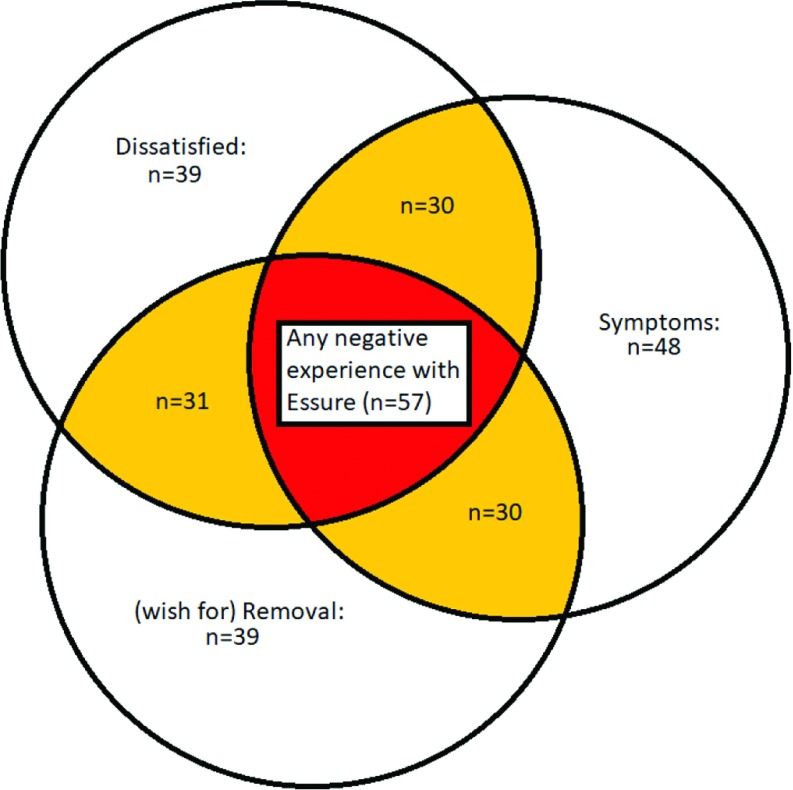
Seventy respondents (59.3%) reported being very satisfied or extremely satisfied with the Essure procedure. Thirteen respondents (11.0%) reported moderate satisfaction and 35 respondents (29.7%) noted (extreme) dissatisfaction with the Essure. Sixty-nine respondents (58.5%) reported that they would have the Essure procedure again if they were faced with the decision, and 70 respondents (59.3%) stated they would recommend the procedure to a friend or family. Thirty-nine respondents (33.1%) with mean Likert score < 3 of 5 on the satisfaction questions were defined as being dissatisfied with the procedure. Seventy-three (61.9%) respondents were satisfied with Essure. Six respondents (5.0%) could not be defined as satisfied or dissatisfied because of neutral responses.
Seven respondents (5.9%) had already undergone removal of the device at the time of the survey, and 32 women (27.1%) reported that they are planning removal of Essure. Reasons for (planning) removal include symptoms attributed to Essure (56.4%) and wish for fertility (10.3%). Thirty-eight percent of the respondents did not specify their reason. Reasons for removal were not mutually exclusive. The median time between procedure and removal of the Essure device was 5.5 y, with the majority being removed via laparoscopy. A total of five women (71.4%) who underwent removal of the device reported symptom relief after removal.
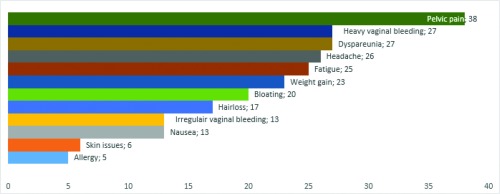
Sixty-one respondents (51.7%) reported that they never experienced any symptoms because of the Essure device, whereas nine respondents (7.6%) reported only temporary symptoms attributed to Essure and no ongoing symptoms. Forty-eight respondents (40.7%) reported currently having symptoms they attribute to the Essure device [see Figure 1]. Additional reported symptoms included panic attacks, cramping or painful hips and breasts during menstruation, recurrent bacterial vaginosis, back pain, cancer, symptoms of metal poisoning, and pain in entire body. Thirteen of satisfied respondents (17.8%) reported currently having symptoms attributed to Essure. Nine of dissatisfied respondents (23.1%) do not currently have symptoms attributed to Essure. Reasons for dissatisfaction reported by respondents without symptoms include sterilization regret. The mean age at placement of respondents with desire for future fertility is 30 y versus a mean age of 33 y for women who did not report ongoing desire for fertility. Twenty of the respondents with symptoms (41.7%) reported having endometriosis, adenomyosis, fibroids, uterine polyps, ovarian cysts, a sexually transmitted infection, or pelvic inflammatory disease. It is unknown whether these gynecologic conditions were diagnosed before or after Essure placement. Thirty-four of the respondents who reported symptoms (70.8%) had used hormonal contraception prior to Essure. Two of these respondents (5.9%) continued hormonal contraception after the Essure procedure.
Figure 1.
Current symptoms attributed to the Essure device by respondents who reported symptoms (n = 48). Presented are the number of subjects and the symptoms attributed to Essure. Symptoms are not mutually exclusive.
A total of 57 respondents (48.3%) were identified as having any negative experience with Essure [see Figure 2]. Table 1 shows the comparison between the subject and procedural characteristics of the group who had a negative experience versus those who did not [see Supplemental Attachment 3 for all assessed characteristics]. The respondents who reported a negative Essure experience were on average younger than those without a negative experience (33.1 versus 37 y, P < .001). Higher gravidity and parity were associated with higher incidence of negative experiences (mean of 5.2 versus 3.7, P = .002 and 3.4 versus 2.2, P < .001, respectively). Similarly, respondents with a negative experience were more likely to have a low education level or income (17.5% versus 37.7% with bachelor's degree or higher, P = .025, and 91.2% versus 77.1% with an income lower than $90,000/year, P = .004). Among the assessed medical conditions, pain syndromes (64.9% versus 37.7%, P = .003) and psychiatric disease (57.9% versus 32.8%, P = .006) were also associated with higher incidence of negative experiences. Respondents who participate in social media groups based on problems with Essure more often had a negative experience with Essure (38.6% versus 13.1%, P = .003). Years after placement, race and BMI were not different between groups. Prior ectopic pregnancy, prior hormonal contraception use, previous abdominal surgery, and procedure characteristics also did not differ significantly.
Figure 2.
Group composition of respondents with a negative experience with Essure. Groups are not mutually exclusive. Size of the circles and the surface of overlapping areas do not exactly represent the data.
Table 1.
Subject and Procedure Characteristics Compared Across Respondents Who Have a Negative Experience with the Essure Device Versus Those Who Do Not
| Characteristica | Any Negative Experience | No Negative Experience | P Value |
|---|---|---|---|
| n = 57 | n = 61 | ||
| Age at procedure (y), mean ± SD | 33.1 ± 5.3 | 37 ± 5.2 | < .001 |
| Race/ethnicity, n (%) | |||
| White non-Hispanic | 7 (12.3) | 11 (18.0) | .440 |
| Black non-Hispanic | 11 (19.3) | 17 (27.9) | |
| Hispanic | 38 (66.7) | 31 (50.8) | |
| Asian | 1 (1.8) | 1 (1.6) | |
| BMI, mean ± SD | 31.1 ± 5.7 | 31.0 ± 7.8 | .941 |
| Highest achieved level of education, n (%) | |||
| Some college or lower | 44 (77.2) | 38 (62.3) | .025 |
| Bachelor's degree or higher | 10 (17.5) | 23 (37.7) | |
| Level of income, n (%) | |||
| Less than $89999/y | 52 (91.2) | 47 (77.1) | .004 |
| More than $90000/y | 1 (1.8) | 11 (18.0) | |
| Gravidity, mean ± SD | 5.2 ± 2.8 | 3.7 ± 2.1 | .002 |
| Parity, mean ± SD | 3.4 ± 1.5 | 2.2 ± 1.1 | < .001 |
| Prior hormonal contraceptive use, n (%) | 40 (70.2) | 35 (57.4) | .151 |
| Previous abdominal surgery, n (%) | |||
| Laparotomy | 6 (10.5) | 16 (26.2) | .058 |
| Laparoscopy | 6 (10.5) | 7 (11.5) | .578 |
| Medical conditions, n (%)b | |||
| Gynecologic | 26 (45.6) | 26 (42.6) | .744 |
| Pain syndromes | 37 (64.9) | 23 (37.7) | .003 |
| Psychiatric disease | 33 (57.9) | 20 (32.8) | .006 |
| Both coils inserted according to manufacturer's instructions, n (%) | 27 (47.4) | 34 (55.7) | .430 |
| Social media use, n (%) | 22 (38.6) | 8 (13.1) | .003 |
A respondent was classified as having a negative experience if she reported dissatisfaction, ongoing symptoms attributed to Essure, or had undergone/planned removal of the Essure device. BMI, body mass index.
Sample size is smaller for some of the characteristics because of missing data.
Gynecologic conditions include endometriosis, adenomyosis, fibroids, uterine polyps, ovarian cysts, sexually transmitted disease, and pelvic inflammatory disease. Pain syndromes include chronic pelvic pain, interstitial cystitis, migraines, chronic back pain, and fibromyalgia. Psychiatric disease includes depression and anxiety.
Regarding respondents who planned/underwent removal of the Essure device versus those who did not, the following characteristics were significantly associated with desire for removal: younger age at procedure (32.5 versus 36.3 y, P < .001), higher gravidity (5.2 versus 4.0, P = .014) and parity (3.5 versus 2.4, P < .001), presence of pain syndromes (69.2% versus 40.8%, P = .006) or psychiatric disease (59.0% versus 38.2%, P = .047), social media use (43.6% versus 15.8%, P = .003), and prior hormonal contraceptive use (20.5% versus 38.2%, P = .047) [see Supplemental Attachment 4]. In particular, 30 respondents (25.4%) were 30 y or younger during Essure placement, of whom 23 (76.7%) were identified as having any negative experience with Essure. Sixteen of these subjects (69.6%) planned or underwent removal of Essure. In comparison, 88 respondents (74.6%) were 31 y or older during placement, of whom 34 (38.6%) reported any negative experience with Essure, and 23(67.6%) planned or underwent removal of Essure.
Upon multivariable analysis of factors associated with negative Essure experience [Table 2], a significant association was found between a negative experience and lower age at procedure (odds ratio [OR] 0.86; 95% confidence interval [CI] 0.79–0.94; P < .001) as well as higher gravidity (OR 1.39; 95% CI 1.14–1.71; P = .002) and lack of prior abdominal surgery (OR 0.35; 95% CI 0.12–1.00; P = .049).
Table 2.
Logistic Regression Analysis Examining Risk Factors for Association with Negative Experience with Essure
| Variable | aOR | 95% CI | P Value |
|---|---|---|---|
| Age at procedure | 0.86 | 0.79–0.94 | < .001 |
| BMI | 1.00 | 0.96–1.05 | .869 |
| Gravidity | 1.39 | 1.14–1.71 | .002 |
| Previous abdominal surgerya | 0.35 | 0.12–1.00 | .049 |
| Pain syndromeb | 2.42 | 0.98–5.97 | .055 |
| Psychiatric diseasec | 2.23 | 0.89–5.62 | .088 |
aOR, adjusted odds ratio; CI, confidence interval; BMI, body mass index.
Previous abdominal surgery includes either prior laparotomy or laparoscopy.
Pain syndromes include chronic pelvic pain, interstitial cystitis, migraines, chronic back pain, and fibromyalgia.
Psychiatric disease includes depression and anxiety, adjusted for all variables in table.
DISCUSSION
This study examined factors associated with negative patient experiences after Essure sterilization. Of the 118 respondents, 57 women (48.3%) were identified as having a negative experience with the Essure device. Several subject characteristics were found to be associated with a negative experience following Essure, including young age at placement, high gravidity, and absent history of abdominal surgery.
The present study expands on the literature that searched for predictors of adverse outcomes after hysteroscopic sterilization. Consistent with prior work,12,13 our results show a significant association between negative experience with Essure and presence of pain syndromes, including chronic pelvic pain, chronic back pain, migraines, interstitial cystitis, and fibromyalgia, although these findings did not remain significant upon multivariable regression. Inconsistent with prior research, however, we found high gravidity to possibly be a significant factor associated with negative experience and desire for device removal. One possible explanation for this discrepancy is that although previous studies have focused on obstetric history as related to placement failure or postprocedure symptoms,12,14–16 we were interested to assess any negative experience with Essure including self-reported satisfaction or desire for removal and these outcomes may not be directly comparable. Regarding the finding that women with a history of prior abdominal surgery are more likely to be satisfied with Essure, it is conceivable that this group of women are more aware of the potential complications and long recovery associated with surgery and thus be more accepting of a solution that avoids abdominal surgery.
Within our study population, the satisfaction rate was 61.9%, lower than previously reported 88%–99% satisfaction rates.5,6,17–22 This difference may be explained by the fact that our duration of follow-up is relatively long (mean 6.1 ± 2.5 y after Essure placement versus 1 to 5 y in prior studies). There is also the opportunity for response bias given less than 50% response rate or the possibility that the nature of the survey questions introduced negative bias against the device. It is remarkable to note that not every subject who has symptoms was dissatisfied; however, conversely, dissatisfaction may not be solely related to symptoms. In our study, nearly 23.1% of dissatisfied women do not currently have symptoms attributed to Essure. Reasons for dissatisfaction reported by women without symptoms include desire for future fertility and sterilization regret. The mean age at placement of women with desire for future fertility is 30 y versus a mean age of 33 y for women who did not report ongoing desire for fertility. This may indicate an age relationship to sterilization regret, as reported in prior work,23 and highlights the importance of patient counseling with respect to permanent sterilization particularly in younger patients. The importance of patient counseling is also supported by our finding that young women are more likely to have a negative experience with Essure, including wish for removal of the device.
We observed that symptom prevalence after Essure is common (40.7% of respondents reported current symptoms), although it is far from certain that all symptoms attributed to Essure have a direct causal relation with the device. Interestingly, 34 of these respondents (70.8%) used hormonal contraception prior to the Essure procedure, which may mask at least some preexisting symptoms. It has been reported that a pain-generating gynecologic condition is diagnosed in 44%–50% of women based on surgical findings and pathology after removal of the device.9,24 Although in our study no significant association was found between negative Essure experience and history of gynecologic conditions, a comparable percentage (41.7%) of our respondents with symptoms reported having endometriosis, adenomyosis, fibroids, uterine polyps, ovarian cysts, a sexually transmitted infection, or pelvic inflammatory disease. Our findings suggest that removal of Essure does not always result in pain resolution. Although we have a small number of respondents who had undergone Essure removal, 71.4% reported symptom relief, consistent with the 53.1%–88.5% symptom improvement reported in prior studies.9,10
Kamencic et al.24 discussed the potential role of social media and its influence on the patient's symptom understanding and demand for treatment. Our results show a significant difference in participation in social media groups reporting problems related to Essure between women who had a negative experience versus those who did not (P = .003). The role of social media in procedure satisfaction deserves further investigation, especially in women who are planning removal of the device to optimize expectations.
In addition, the impact of socioeconomic factors on our patient satisfaction rate should be noted. Respondents with a negative experience were more likely to have a low education level or income. This is in line with previous literature describing the role of socioeconomic factors on health care in the United States.25,26
Factors we found to be associated with a negative patient experience with Essure could be considered for use in counseling women who want to undergo removal of the device. It is conceivable that women with these risk factors are more satisfied after Essure removal because they had a higher risk of being dissatisfied with Essure a priori. Therefore, young age at placement, relative high gravidity, and no history of abdominal surgery could be associated with successful Essure removal.
Strength of this study includes the relatively long follow-up provided. To the authors' knowledge, this is the first study to investigate a variety of causes for negative experience with Essure sterilization, which is a more clinically relevant outcome in terms of patient counseling. We also include the results for subjects without symptoms or dissatisfaction, thereby providing a more reliable denominator than previous studies. This study is unique because it provides updated (dis)satisfaction data. Our study is limited to an academic medical center population and thus potentially less generalizable to all patients. Because of the retrospective study design and the use of a questionnaire, the results are subject to potential recall and response bias. In addition, most of the data reflect subjective assessments. Self-selection bias could not have been excluded. Overestimation of negative experience with Essure is conceivable because dissatisfaction with Essure may stimulate participation; however, it is reassuring that the nonrespondents did not differ from respondents in terms of baseline characteristics. Additionally, because our questionnaire was not formally validated, results must be interpreted with due caution. We did not consider differences in Essure designs and a third-generation Essure model has been employed since 2007,14 but because the material of both designs are identical and the difference is minimal, it seems unlikely to have caused major differences in outcomes.
CONCLUSION
A patient-reported negative experience following hysteroscopic sterilization is common. Symptoms attributed to Essure include pelvic pain, dyspareunia, and vaginal bleeding. Nevertheless, dissatisfaction with Essure is not always due to symptoms. Young age at placement, relative high gravidity, and no history of abdominal surgery are factors associated with negative experience after Essure sterilization. This information could be considered when counseling women who plan removal of Essure because it is conceivable that these factors could potentially be associated with successful removal of Essure, and could be useful for development of future hysteroscopic sterilization techniques. When introducing a new sterilization technique, long-term follow-up and assessment of multimodal patient outcomes should be considered before introducing the new technique on the market. Further studies are required to confirm degree of symptom relief with removal of the Essure device.
Contributor Information
Emilie V. J. van Limburg Stirum, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston Massachusetts..
Nisse V. Clark, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston Massachusetts..
Alexis Lindsey, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston Massachusetts..
Xiangmei Gu, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston Massachusetts..
Andreas L. Thurkow, Department of Obstetrics and Gynecology, Amsterdam UMC, AMC, Amsterdam, The Netherlands..
Jon I. Einarsson, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston Massachusetts..
Sarah L. Cohen, Division of Minimally Invasive Gynecologic Surgery, Brigham and Women's Hospital, Boston Massachusetts..
References:
- 1. Casey J, Cedo-Cintron L, Pearce J, Yunker A. Current techniques and outcomes in hysteroscopic sterilization: current evidence, considerations, and complications with hysteroscopic sterilization micro inserts. Curr Opin Obstet Gynecol. 2017;29:218–224. [DOI] [PubMed] [Google Scholar]
- 2. Bouillon K, Bertrand M, Bader G, Lucot JP, Dray-Spira R, Zureik M. Associaton of hysteroscopic vs laparoscopic sterilization with procedural, gynecological, and medical outcomes. JAMA. 2018;319:375–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Clark NV, Endicott SP, Jorgensen EM, et al. Review of sterilization techniques and clinical updates. J Minim Invasive Gynecol. 2018;25:1157–1164. [DOI] [PubMed] [Google Scholar]
- 4. Hurskainen R, Hovi SL, Gissler M, et al. Hysteroscopic tubal sterilization: a systematic review of the Essure system. Fertil Steril. 2010;94:16–19. [DOI] [PubMed] [Google Scholar]
- 5. Connor VF. Essure: a review six years later. J Minim Invas Gynecol. 2009;16:282–290. [DOI] [PubMed] [Google Scholar]
- 6. Franchini M, Zizolfi B, Coppola C, et al. Essure permanent birth control, effectiveness and safety: an Italian 11-year survey. J Minim Invasive Gynecol. 2017;24:640–645. [DOI] [PubMed] [Google Scholar]
- 7. AAGL Advisory Statement. Essure hysteroscopic sterilization. J Minim Invasive Gynecol. 2016;23:658–659. [DOI] [PubMed] [Google Scholar]
- 8. U.S. Food and Drug administration. Essure permanent birth control. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/EssurePermanentBirthControl/default.htm, accessed 02/20/2019.
- 9. Clark NV, Rademaker D, Mushinski AA, Ajao MO, Cohen SL, Einarsson JI. Essure removal for the treatment of device-attributed symptoms: an expanded case series and follow-up survey. J Minim Invasive Gynecol. 2017;24:971–976. [DOI] [PubMed] [Google Scholar]
- 10. Casey J, Aguirre F, Yunker A. Outcomes of laparoscopic removal of the Essure sterilization device for pelvic pain: a case series. Contraception. 2016;94:190–192. [DOI] [PubMed] [Google Scholar]
- 11. Arthuis CJ, Simon EG, Hébert T, Marret H. Intraoperative factors that predict the successful placement of Essure microinserts. J Minim Invasive Gynecol. 2017;24:803–810. [DOI] [PubMed] [Google Scholar]
- 12. Yunker AC, Ritch JMB, Robinson EF, Golish CT. Incidence and risk factors for chronic pelvic pain after hysteroscopic sterilization. J Minim Invasive Gynecol. 2015;22:390–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Carney PI, Yao J, Lin J, Law A. Occurrence of chronic pelvic pain, abnormal uterine bleeding, and hysterectomy postprocedure among women who have undergone female sterilization procedures: a retrospective claims analysis of commercially insured women in the US. J Minim Invasive Gynecol. 2018;25:651–660. [DOI] [PubMed] [Google Scholar]
- 14. Leyser-Whalen O, Rouhani M, Rahman M, Berenson AB. Tubal risk markers for failure to place transcervical sterilization coils. Contraception. 2012;85:384–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Savage UK, Masters SJ, Smid MC, et al. Hysteroscopic sterilization in a large group practice: experience and effectiveness. Obstet Gynecol. 2009;114:1227–1231. [DOI] [PubMed] [Google Scholar]
- 16. Panel P, Grosdemouge I. Predictive factors of Essure (R) implant placement failure: prospective, multicenter study of 495 patients. Fertil Steril. 2010;93:29–34. [DOI] [PubMed] [Google Scholar]
- 17. Chudnoff SG, Nichols JE, Levie M. Hysteroscopic Essure inserts for permanent contraception: extended follow-up results of a phase III multicenter international study. J Minim Invasive Gynecol. 2015;22:951–960. [DOI] [PubMed] [Google Scholar]
- 18. Duffy S, Marsh F, Rogerson L, et al. Female sterilisation: a cohort controlled comparative study of ESSURE versus laparoscopic sterilisation. BJOG An Int J Obstet Gynaecol. 2005;112:1522–1528. [DOI] [PubMed] [Google Scholar]
- 19. Arjona JE, Miño M, Cordón J, Povedano B, Pelegrin B, Castelo-Branco C. Satisfaction and tolerance with office hysteroscopic tubal sterilization. Fertil Steril. 2008;90:1182–1186. [DOI] [PubMed] [Google Scholar]
- 20. Sinha D, Kalathy V, Gupta JK, Clark TJ. The feasibility, success and patient satisfaction associated with outpatient hysteroscopic sterilisation. BJOG An Int J Obstet Gynaecol. 2007;114:676–683. [DOI] [PubMed] [Google Scholar]
- 21. Câmara S, de Castro Coelho F, Freitas C, Remesso L. Essure present controversies and 5 years' learned lessons: a retrospective study with short- and long-term follow-up. Gynecol Surg. 2017;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Levie M, Weiss G, Kaiser B, Daif J, Chudnoff SG. Analysis of pain and satisfaction with office-based hysteroscopic sterilization. Fertil Steril. 2010;94:1189–1194. [DOI] [PubMed] [Google Scholar]
- 23. Hillis SD, Marchbanks PA, Tylor LR, Peterson HB. Poststerilization regret: findings from the United States Collaborative Review of Sterilization. Obstet Gynecol. 1999;93:889–895. [DOI] [PubMed] [Google Scholar]
- 24. Kamencic H, Thiel L, Karreman E, Thiel J. Does Essure cause significant de novo pain? A retrospective review of indications for second surgeries after Essure placement. J Minim Invasive Gynecol. 2016;23:1158–1162. [DOI] [PubMed] [Google Scholar]
- 25. Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389:1475–1490. [DOI] [PubMed] [Google Scholar]
- 26. Lynch J, Smith GD, Harper S, et al. Is income inequality a determinant of population health? Part 1. A systematic review. Milbank Q. 2004;82:5–99. [DOI] [PMC free article] [PubMed] [Google Scholar]