Abstract
The transition of chronically ill adolescents and young adults to adult health care is poorly managed, leading to poor outcomes due to insufficient disease knowledge and a lack of requisite skills to self-manage their chronic disease. This review analyzed 33 articles published between 2009 and 2019 to identify factors associated with transition readiness in adolescents and young adults with chronic diseases, which can be used to design effective interventions. Studies were predominantly cross-sectional survey designs that were guided by interdisciplinary research teams, assessed adolescents and young adults ages 12–26 years, and conducted in the outpatient setting. Modifiable factors, including psychosocial and self-management/transition education factors, and non-modifiable factors, including demographic/ecological and disease factors, associated with transition readiness were identified. Further research is necessary to address gaps identified in this review prior to intervention development, and there is a need for additional longitudinal studies designed to provide perspective on how transition readiness changes over time.
Keywords: transition readiness, transitions, adolescents, young adults, chronic disease, systematic review
The majority of youth with chronic diseases live into adulthood and must transition to the adult health care setting for continued disease management and health promotion. Transition has been defined as the “purposeful, planned movement of adolescents and young adults with chronic physical and medical conditions from child-centered to adult-oriented health-care systems,” which implies that strategic steps must be taken to prepare adolescents and young adults for the change in expectations between the pediatric and adult health care setting (Blum et al., 1993). Despite frequent calls to improve transitional care, transition preparation that encourages adolescents and young adults to assume independent responsibility for disease self-management and to make timely changes in their health care team is still inadequate (McManus et al., 2013). Although advancements have been made to improve quality of life and life expectancy for many pediatric chronic diseases, transition to adult health care poses significant risk to continuity of care, disease management, and to the adolescent and young adult’s quality of life and livelihood (McManus et al., 2013; Stam, Hartman, Deurloo, Groothoff, & Grootenhuis, 2006).
Negative outcomes related to poor transition have been reported in many different chronic disease populations including diabetes (Garvey et al., 2012), liver transplantation (Annunziato et al., 2007), sickle cell disease (Blinder et al., 2013; Brousseau, Owens, Mosso, Panepinto, & Steiner, 2010), inflammatory bowel disease (de Silva & Fishman, 2014), chronic kidney disease (Fenton, Ferris, Ko, Javalkar, & Hooper, 2015), human immunodeficiency virus (Fish et al., 2014), congenital heart disease (Goossens et al., 2011), attention-deficit hyperactivity disorder (Montano & Young, 2012), and hydrocephalus (Simon et al., 2009). Studies looking at adherence found that after poor transitions, there were increased rates of non-adherence in liver transplantation recipients (Annunziato et al., 2007) and increased hemoglobin A1c levels in young adults with type 1 diabetes (Garvey et al., 2012; Helgeson et al., 2013). After transition to adult health care, there is a decrease in routine outpatient care health care utilization (Blinder et al., 2013) and an increase in hospital admissions and emergency room visits (Brousseau et al., 2010; Dickerson, Klima, Rhodes, & O’Brien, 2012). Latent increases in mortality after the transition to adult health care for chronic diseases such as sickle cell disease and human immunodeficiency virus have also been reported (Fish et al., 2014; Quinn, Rogers, McCavit, & Buchanan, 2010). Studies reporting adolescents and young adults’ experiences of the transition to adult health care found that they believed they had insufficient knowledge and self-management skills to successfully manage their disease (Asp, Bratt, & Bramhagen, 2015; Burström, Öjmyr-Joelsson, Bratt, Lundell, & Nisell, 2016). In addition, they reported being unable to identify appropriate adult health care providers (Bemrich-Stolz, Halanych, Howard, Hilliard, & Lebensburger, 2015) and found it challenging to establish a trusting patient-provider relationship in their new adult health care setting (Bemrich-Stolz et al., 2015; Garvey et al., 2014; Huang et al., 2011). The issue of trust is crucial as adolescents and young adults are more likely to disengage from health care if they fail to establish a trusted relationship with their adult health care provider similar to what they had experienced in pediatrics (Bemrich-Stolz et al., 2015; Garvey et al., 2014; Lewis & Noyes, 2013). Preparation for transition to adult care should become a priority within pediatric clinical practice in order to positively impact health and utilization outcomes.
Pediatric health care providers must make transition preparation a routine practice by developing and implementing evidence-based approaches to increase the level of adolescent and young adult’s disease-specific knowledge and help them develop self-management skills needed for successful transition to adult care (American Academy of Pediatrics, 2002). This level of preparation is known as transition readiness. Routine assessment of transition readiness provides a baseline of the adolescent and young adult’s current understanding about their condition and their capacity to perform disease self-management (Zhang, Ho, & Kennedy, 2014). Understanding factors associated with transition readiness is an essential first step to developing interventions to positively influence adolescents and young adult’s transition readiness. Yet little is known about factors that positively and/or negatively influence transition readiness in adolescents and young adults. To the best of our knowledge, no systematic reviews had been conducted on this topic. The primary purpose of this systematic review was to explore the literature regarding factors associated with transition readiness in adolescents and young adults with chronic diseases and to identify factors that could be used to design effective interventions.
Methods
This systematic review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. A meta-analysis was not completed due to the heterogeneity of the available literature.
Inclusion Criteria
For the purpose of this review, transition readiness was defined as the following: the attainment of disease-specific knowledge and the development of effective self-management skills needed for successful transition from pediatric to the adult health care settings. To be included, a study needed to be a primary, peer-reviewed research that assessed transition readiness in adolescents and young adults aged 12–30 years living with a chronic disease, be available in full-text, and be written in English. Studies were excluded if the chronic disease limited the adolescent’s or young adult’s ability to become fully independent in disease self-management or were not peer reviewed.
Search Strategy
Databases were searched for years 1990–2019 and included PubMed, Google Scholar, CINAHL, Medline, and PsycINFO. The year 1990 was selected, because it is the first year in which transition was mentioned as a significant issue in the care of adolescents and young adult’s health care (Blum et al., 1993). Search strategies and key terms were guided by a medical librarian, and they included restricting the language to English and studies involving humans. Chronic diseases included in the search terms were those common to childhood that continue to require lifelong medical management. Key terms included “transition,” “transition readiness,” “chronic disease,” “chronic illness,” “sickle cell,” “diabetes,” “epilepsy,” “asthma,” “spina bifida,” “cystic fibrosis,” “adolescent,” “teen,” “youth,” and “young adult.”
Article Selection
The search strategy was first trialed in PubMed and PsycINFO; once it was found that the strategy was effective in identifying articles appropriate for inclusion, Google Scholar, CINAHL, and Medline were searched. After identifying potential articles from PubMed, Google Scholar, CINAHL, Medline, and PsycINFO databases, articles were excluded first by assessing titles and abstracts for duplicates and then applying the inclusion criteria. Next, the remaining full-text articles were read to ensure that inclusion criteria were met, and if so, then the articles were assessed for quality. Bibliographies of the articles were also screened for potential articles that may meet the inclusion criteria. These articles were then located and screened for inclusion and quality appraisal. The article selection process is detailed in Figure 1.
Figure 1.
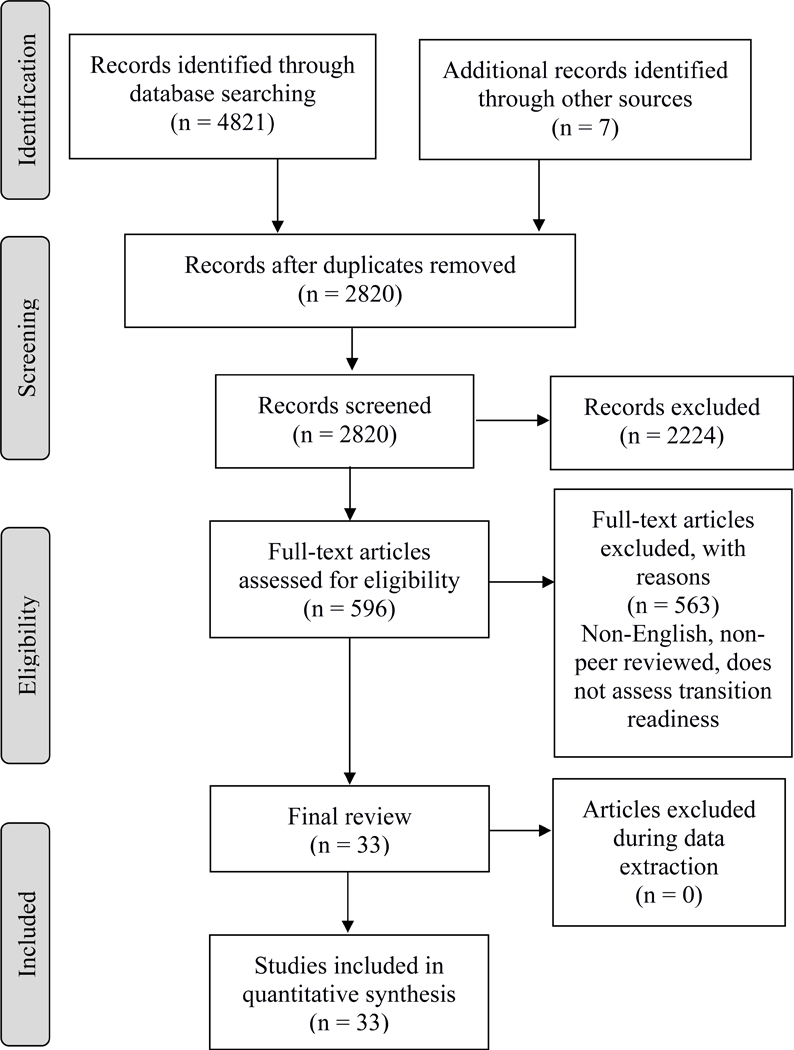
PRISMA Flow Diagram
Quality Appraisal
An analysis of study quality was conducted for each study using the Joanna Briggs Institute critical appraisal tools (Joanna Briggs Institute, 2018). These tools were designed to assess the rigor of quantitative research designs (e.g., cross-sectional and randomized clinical trials). Each included study was read completely a second time for the purpose of evaluating quality using a critical appraisal tool consistent with the reported study design. Specifically, quality was appraised for inclusion and exclusion criteria, sample adequacy, setting, validity and reliability of study methods, identification and management of potential study bias, and appropriateness of the statistical analysis plan. Based on the appraisal, it was determined that all 33 studies were of sufficient quality to be included in this analysis.
Data Extraction
Data extraction included the following broad categories: chronic disease diagnosis/diagnoses, research methods, theoretical models, study setting, sample characteristics, sampling methods, measurement tools used, factors assessed in each study, results of analysis, study limitations, professions included in the research team, and publication information. Each of these items were recorded in a spreadsheet to aid in later analysis. Missing categories of data were noted in the spreadsheet.
Analysis Process
After data had been extracted to a spreadsheet, each category was analyzed across studies looking for patterns. Factors identified as potentially influential in transition readiness were further reviewed to determine if there was a statistically significant association to transition readiness. Those that were statistically significant were further categorized as modifiable or non-modifiable. Finally, factors found to be associated with transition readiness were grouped by similarities and patterns among the factors. In addition, gaps in the findings were noted.
Results
There were 33 studies published between 2009 and 2019 included in this analysis that assessed factors associated with transition readiness in adolescents and young adults living with a chronic disease. Articles published between 1990 and 2009 yielded no factors associated with transition readiness; rather, these articles focused on defining transition readiness and developing measurement tools to assess transition readiness. Thirty-two of the 33 studies were cross-sectional survey designs, and the remaining one was a longitudinal study. Study participant ages ranged from 12–26 years, but age ranged varied within studies. Twenty-four of 33 studies were conducted in the outpatient setting. There were four categories of factors associated with transition readiness: (a) demographic and ecological factors, (b) psychosocial factors, (c) self-management/transition readiness education factors, and (d) health outcome factors. Within each of the four categories, there were modifiable and non-modifiable categories. Six studies used a theory or model to guide the research, including the Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART), the Lerner Model, the Developmental Transitional Model, and the Health Care Transition Research Consortium Model.
Methodological Quality
Table 1 provides details about the findings from the quality assessment. When assessing methodological quality using the Joanna Briggs Institute critical appraisal tools, it was determined that all 33 included articles provided sufficient detail regarding the studies’ inclusion and exclusion criteria, sample adequacy, setting characteristics, and appropriateness of the statistical analysis plan. The two areas that were noted to be less rigorous were use of valid and reliable measures and bias.
Table 1.
Quality Assessment of Included Study Methodology
= authors adequately addressed
There were a variety of validated tools used across the studies to assess transition readiness. The most commonly utilized tools included the University of North Carolina STARx scale (Cohen et al., 2015; Ferris et al., 2015), University of North Carolina TRxNSITION (Ferris et al., 2012), and the Transition Readiness Assessment Questionnaire (Sawicki et al., 2011; Wood et al., 2014). Twenty-nine of the 33 studies utilized measurement tools that were not specific to any diseases, whereas four of the 33 studies utilized a disease-specific tool. Though a majority of the included studies utilized validated tools, six studies used non-validated tools.
The majority of the studies did not adequately address threats of bias. All 33 studies recognized the potential issues with utilizing self-reported measures of transition readiness and only measuring the adolescents and young adults’ perspective; only a few studies reported using strategies to address this bias (Eluri et al., 2017; Fredericks et al., 2010; Gilleland, Amaral, Mee, & Blount, 2011; Gilleland Marchak, Reed-Knight, Amaral, Mee, & Blount, 2015; Sawicki, Kelemen, & Weitzman, 2014; Speller-Brown et al., 2015). Six of the 33 studies included both adolescent/young adult and parent self-report as a mechanism to reduce self-report bias. A single study included a provider report of transition readiness (Gilleland Marchak et al., 2015).
Demographic and Ecological Factors
There were a variety of demographic and ecological factors found to have a relationship to transition readiness. See Table 2 for a list of demographic and ecological factors that demonstrated associations with transition readiness. Twenty-six studies assessed age, and 19 found it to be positively related to transition readiness (Beal et al., 2016; Bingham, Scalzi, Groh, Boehmer, & Banks, 2015; Dwyer-Matzky, Blatt, Asselin, & Wood, 2018; Eaton et al., 2017; Fredericks et al., 2010; Gilleland et al., 2012; Gray et al., 2015; Gumidyala et al., 2018; Haarbauer-Krupa et al., 2019; Hart, Pollock, Hill, & Maslow, 2017; Javalkar, Fenton, Cohen, & Ferris, 2014; Javalkar et al., 2016; Lazaroff, Meara, Tompkins, Peters, & Ardoin, 2018; Mackie et al., 2016; Rosen et al., 2016; Sawicki, Kelemen, & Weitzman, 2014; Speller-Brown et al., 2015; Stewart et al., 2017; Whitfield, Fredericks, Eder, Shpeen, & Adler, 2015). Studies found that increasing age was positively related to decreasing knowledge deficits in youth with sickle cell disease or heart disease (McPherson, Thaniel, & Minniti, 2009; Uzark et al., 2015). Two studies found that age was associated with increased levels of self-management skills needed for successful transition for youth with sickle cell disease or heart disease (Treadwell et al., 2016; Uzark et al., 2015) and with decreased problems with transition in the sickle cell disease population (McPherson et al., 2009). Not all studies found that transition readiness increased with age. Four studies did not find a significant relationship between age and transition readiness in youth with inflammatory bowel disease (Carlsen et al., 2017), eosinophilic esophagitis/eosinophilic gastroenteritis (Eluri et al., 2017), kidney transplants (Fenton et al., 2015), or neurogenic bladders (Grimsby et al., 2016).
Table 2.
Demographic and Ecological Factors Found to have Significant or Inconsistent Relationships to Transition Readiness
| Study | Chronic Disease of Focus |
Age | Gender | Median Household Income |
Sex Composition of Community |
Household Structure |
Insurance Type |
Health Literacy |
Academic Performance |
|---|---|---|---|---|---|---|---|---|---|
| Beal (2016) | MCD* | ✓ | -- | ✓ | ✓ | ||||
| Bingham (2015) | Rheumatology Diseases | ✓ | ✓ | ||||||
| Carlsen (2017) | IBD** | -- | |||||||
| Dwyer-Matzky (2018) | MCD | ✓ | -- | -- | |||||
| Eaton (2017) | MCD | ✓ | ✓ | ||||||
| Eluri (2017) | Eosinophili esophagitis/ eosinophilic gastroenteritis | -- | -- | ||||||
| Fenton (2015) | Kidney transplant | -- | -- | ||||||
| Fredericks (2010) | Liver transplant | ✓ | -- | ||||||
| Gilleland (2011) | Kidney Transplant | ||||||||
| Gilleland Marchak (2015) | Kidney Transplant | ✓ | |||||||
| Gray (2015) | IBD | ✓ | ✓ | ||||||
| Grimsby (2016) | Neurogenic bladder | -- | -- | ||||||
| Gumidyala (2018) | IBD | ✓ | -- | ||||||
| Gutierrez-Colina (2017) | Pediatric Transplant | ||||||||
| Haarbauer-Krupa (2019) | MCD | ✓ | ✓ | ||||||
| Hart (2017) | MCD | ✓ | ✓ | ||||||
| Javalkar (2014) | Chronic kidney disease | ✓ | ✓ | ✓ | |||||
| Javalkar (2016) | MCD | ✓ | ✓ | ✓ | ✓ | ||||
| Jensen (2017) | MCD | ||||||||
| Johnson (2015) | MCD | ||||||||
| Lazaroff (2018) | Juvenile Idiopathic Arthritis | ✓ | ✓ | ||||||
| Mackie (2016) | Heart disease/ transplant | ✓ | -- | ||||||
| McPherson (2009) | Sickle cell disease | ✓ | |||||||
| Nazareth (2016) | MCD | ||||||||
| Pakdeeprom (2012) | MCD | ||||||||
| Rosen (2016) | IBD | ✓ | |||||||
| Sawicki et al. (2014) | MCD | ✓ | ✓ | ||||||
| Speller-Brown (2015) | Sickle cell disease | ✓ | -- | -- | |||||
| Stewart (2017) | Heart disease | ✓ | -- | ||||||
| Szalda (2017) | Cancer | ||||||||
| Treadwell (2016) | Sickle cell disease | ✓ | -- | -- | |||||
| Uzark (2015) | Heart disease | ✓ | -- | ||||||
| Whitfield (2015) | IBD | ✓ | |||||||
MCD – Multiple chronic diseases,
IBD – Inflammatory bowel disease,
= significance at the 0.05 level,
= studied but no association found
Seven studies found that female youths with a variety of chronic diseases had statistically significantly higher transition readiness scores (Eaton et al., 2017; Gray et al., 2015; Hart et al., 2017; Javalkar et al., 2014, 2016; Lazaroff et al., 2018; Sawicki et al., 2014). Additionally, females with sickle cell disease or heart disease had higher self-management behavior scores, indicating they were more prepared for transition to adult care (McPherson et al., 2009; Stewart et al., 2017). One study found that females with sickle cell disease perceived higher levels of difficulty with transition to adult care (McPherson et al., 2009). This finding about female gender was not consistent across all studies; 11 studies which assessed gender did not find an association between gender and transition readiness (Beal et al., 2016; Dwyer-Matzky et al., 2018; Eluri et al., 2017; Fenton et al., 2015; Fredericks et al., 2010; Grimsby et al., 2016; Gumidyala et al., 2018; Mackie et al., 2016; Speller-Brown et al., 2015; Treadwell et al., 2016; Uzark et al., 2015).
A few studies assessed social determinants of health factors for potential relationships with transition readiness. Positive associations for transition readiness included higher median household income (Javalkar et al., 2016), two-parent households (Beal et al., 2016; Javalkar et al., 2016), and private insurance status (Javalkar et al., 2014). Adolescents and young adults’ higher health literacy (Beal et al., 2016; Bingham et al., 2015) and academic performance (Haarbauer-Krupa et al., 2019) had increased transition readiness scores. Findings regarding the relationship between income and transition readiness was not consistent across studies. Two studies found that income did not have a relationship with transition readiness (Speller-Brown et al., 2015; Stewart et al., 2017). Other demographic and ecological factors that did not demonstrate any significant associations with transition readiness included race/ethnicity (Beal et al., 2016; Dwyer-Matzky et al., 2018; Grimsby et al., 2016; Gumidyala et al., 2018; Javalkar et al., 2016; Treadwell et al., 2016; Uzark et al., 2015), parental age (Bingham et al., 2015), parent education level (Beal et al., 2016; Bingham et al., 2015; Javalkar et al., 2014; Rosen et al., 2016; Speller-Brown et al., 2015; Stewart et al., 2017), having a job (Bingham et al., 2015; Treadwell et al., 2016), youth education level (Bingham et al., 2015; Treadwell et al., 2016), household size (Javalkar et al., 2016), parent marital status (Speller-Brown et al., 2015), and socioeconomic status (Carlsen et al., 2017; Hart et al., 2017; Rosen et al., 2016).
Disease Factors
Few associations between disease factors and transition readiness were identified. One study assessing multiple chronic diseases found that chronic conditions impacting cognitive ability were associated with lower transition readiness compared to healthy peers (Beal et al., 2016). Having a family member with a similar disease and length of illness duration were found to be positively associated with transition readiness in one study (Bingham et al., 2015). However, in other studies assessing illness duration, no relationship to transition readiness was identified (Carlsen et al., 2017; Gray et al., 2015; Javalkar et al., 2014; Pakdeeprom, In-Iw, Chintanadilok, Wichiencharoen, & Manaboriboon, 2012; Whitfield et al., 2015). In the sickle cell disease population, disease severity was negatively associated with adolescents and young adults’ interest in learning about the transition process (McPherson et al., 2009). This was not supported by other studies assessing transition readiness in adolescents and young adults living with sickle cell disease (McPherson et al., 2009; Speller-Brown et al., 2015), chronic kidney disease (Fenton et al., 2015), and inflammatory bowel disease (Gray et al., 2015; Gumidyala et al., 2018). For adolescents and young adults with congenital heart disease, having a history of a primary repair or undergoing cardiac interventions was positively associated with higher disease self-management scores and better transition readiness (Stewart et al., 2017). This same study noted the use of cardiac medications was associated with higher self-advocacy, but not with overall transition readiness (Stewart et al., 2017).
None of the studies identified an association between transition readiness and adherence to medical therapies for chronic diseases (Rosen et al., 2016; Whitfield et al., 2015). Other disease factors that did not demonstrate any significant associations with transition readiness included diagnosis (Bingham et al., 2015; Carlsen et al., 2017; Gumidyala et al., 2018; Mackie et al., 2016; Rosen et al., 2016; Stewart et al., 2017; Uzark et al., 2015), active symptoms (Eluri et al., 2017), active steroid use (Eluri et al., 2017), dietary therapy (Eluri et al., 2017), disease burden (Fenton et al., 2015), pain scores (Bingham et al., 2015), hospitalizations (Rosen et al., 2016), ambulation status (Grimsby et al., 2016), use of individualized education plan (Javalkar et al., 2014), and disease-related absences from school (Carlsen et al., 2017).
Psychosocial Factors
A variety of disparate psychosocial factors were found to be associated with transition readiness. See Table 3 for a list of psychosocial factors that demonstrated associations with transition readiness. Self-efficacy was found to be positively associated with transition readiness in nine out of ten studies that focused on a variety of different chronic diseases and populations (Carlsen et al., 2017; Eaton et al., 2017; Gilleland Marchak et al., 2015; Gumidyala et al., 2018; Pakdeeprom et al., 2012; Sawicki et al., 2014; Stewart et al., 2017; Treadwell et al., 2016; Uzark et al., 2015). Eluri et al. (2017) was the only study that did not find a relationship between self-efficacy and transition readiness. A number of other factors associated with transition readiness were identified in single studies that used heterogeneous populations including autonomous motivation (Dwyer-Matzky et al., 2018), family cohesion (Fenton et al., 2015), social support (Pakdeeprom et al., 2012), hopeful future expectations (Hart et al., 2017), preferred source of information (Johnson et al., 2015), locus of control (Nazareth et al., 2016), patient activation levels (Lazaroff et al., 2018), anxiety (Pakdeeprom et al., 2012), disease-associated stress (Uzark et al., 2015), executive functioning (Gutierrez-Colina et al., 2017), and quality of life (Treadwell et al., 2016). Psychosocial factors that did not demonstrate any significant associations with transition readiness included overall well-being (Bingham et al., 2015), resiliency (Carlsen et al., 2017), perceived competence (Dwyer-Matzky et al., 2018), quality of life (Fenton et al., 2015; Uzark et al., 2015), coping strategies (Fenton et al., 2015), confidence in readiness to transfer (Beal et al., 2016; Gray et al., 2015), and perception of illness uncertainty (Stewart et al., 2017).
Table 3.
Psychosocial Factors Found to have Significant or Inconsistent Relationships to Transition Readiness
| Study | Chronic Disease of Focus |
Self- efficacy |
Autonomous Motivation |
Family Cohesion |
Social Support |
Hopeful Future Expectations |
Locus of Control |
Patient Activation Levels |
Anxiety | Executive Functioning |
|---|---|---|---|---|---|---|---|---|---|---|
| Beal (2016) | MCD | |||||||||
| Bingham (2015) | Rheumatology Diseases | |||||||||
| Carlsen (2017) | IBD** | ✓ | ||||||||
| Dwyer-Matzky (2018) | MCD | ✓ | ||||||||
| Eaton (2017) | MCD | ✓ | ||||||||
| Eluri (2017) | Eosinophilic esophagitis/ eosinophilic gastroenteritis | -- | ||||||||
| Fenton (2015) | Kidney transplant | ✓ | ||||||||
| Fredericks (2010) | Liver transplant | |||||||||
| Gilleland (2011) | Kidney Transplant | |||||||||
| Gilleland Marchak (2015) | Kidney Transplant | ✓ | ||||||||
| Gray (2015) | IBD | |||||||||
| Grimsby (2016) | Neurogenic bladder | |||||||||
| Gumidyala (2018) | IBD | ✓ | ||||||||
| Gutierrez-Colina (2017) | Pediatric Transplant | ✓ | ||||||||
| Haarbauer-Krupa (2019) | MCD | |||||||||
| Hart (2017) | MCD | ✓ | ||||||||
| Javalkar (2014) | Chronic kidney disease | |||||||||
| Javalkar (2016) | MCD | |||||||||
| Jensen (2017) | MCD | |||||||||
| Johnson (2015) | MCD | |||||||||
| Lazaroff (2018) | Juvenile Idiopathic Arthritis | ✓ | ||||||||
| Mackie (2016) | Heart disease/ transplant | |||||||||
| McPherson (2009) | Sickle cell disease | |||||||||
| Nazareth (2016) | MCD | ✓ | ||||||||
| Pakdeeprom (2012) | MCD | ✓ | ✓ | ✓ | ||||||
| Rosen (2016) | IBD | |||||||||
| Sawicki et al. (2014) | MCD | ✓ | ||||||||
| Speller-Brown (2015) | Sickle cell disease | |||||||||
| Stewart (2017) | Heart disease | ✓ | ||||||||
| Szalda (2017) | Cancer | |||||||||
| Treadwell (2016) | Sickle cell disease | ✓ | ||||||||
| Uzark (2015) | Heart disease | ✓ | ||||||||
| Whitfield (2015) | IBD | |||||||||
MCD – Multiple chronic diseases,
IBD – Inflammatory bowel disease,
= significance at the 0.05 level,
= studied but no association found
Self-Management and Transition Education Factors
There were a number of studies that identified factors related to self-management and transition education that influenced transition readiness. See Table 4 for a list of self-management and transition education factors that demonstrated associations with transition readiness. Disease knowledge was positively related to transition readiness in studies of adolescents and young adults with congenital heart disease, kidney transplants, and other chronic diseases (Dwyer-Matzky et al., 2018; Gilleland et al., 2011; Gilleland Marchak et al., 2015; Stewart et al., 2017). Adolescents and young adults across multiple different chronic diseases who perceived greater overall responsibility for their disease self-management also had higher levels of transition readiness (Eaton et al., 2017; Gilleland et al., 2011; Gilleland Marchak et al., 2015; Haarbauer-Krupa et al., 2019; Speller-Brown et al., 2015). In addition, youth with sickle cell disease who thought they were ready to assume complete responsibility also reported higher levels of transition readiness (Speller-Brown et al., 2015).
Table 4.
Self-management and Transition Education Factors Found to have Significant or Inconsistent Relationships to Transition Readiness
| Study | Chronic Disease of Focus |
Disease- specific Knowledge |
Adolescent Disease Responsibility |
Discussions about Transition |
Parent Involvement |
Perceived Medication Barriers |
|---|---|---|---|---|---|---|
| Beal (2016) | MCD* | |||||
| Bingham (2015) | Rheumatology Diseases | |||||
| Carlsen (2017) | IBD** | |||||
| Dwyer-Matzky (2018) | MCD | ✓ | ||||
| Eaton (2017) | MCD | ✓ | -- | |||
| Eluri (2017) | Eosinophilic esophagitis/ eosinophilic gastroenteritis | |||||
| Fenton (2015) | Kidney transplant | |||||
| Fredericks (2010) | Liver transplant | |||||
| Gilleland (2011) | Kidney Transplant | ✓ | ✓ | ✓ | ✓ | |
| Gilleland Marchak (2015) | Kidney Transplant | ✓ | ✓ | ✓ | ||
| Gray (2015) | IBD | |||||
| Grimsby (2016) | Neurogenic bladder | |||||
| Gumidyala (2018) | IBD | ✓ | ||||
| Gutierrez-Colina (2017) | Pediatric Transplant | |||||
| Haarbauer-Krupa (2019) | MCD | ✓ | ✓ | |||
| Hart (2017) | MCD | |||||
| Javalkar (2014) | Chronic kidney disease | |||||
| Javalkar (2016) | MCD | |||||
| Jensen (2017) | MCD | |||||
| Johnson (2015) | MCD | |||||
| Lazaroff (2018) | Juvenile Idiopathic Arthritis | |||||
| Mackie (2016) | Heart disease/ transplant | |||||
| McPherson (2009) | Sickle cell disease | |||||
| Nazareth (2016) | MCD | |||||
| Pakdeeprom (2012) | MCD | |||||
| Rosen (2016) | IBD | |||||
| Sawicki et al. (2014) | MCD | -- | ||||
| Speller-Brown (2015) | Sickle cell disease | ✓ | ✓ | |||
| Stewart (2017) | Heart disease | ✓ | ✓ | |||
| Szalda (2017) | Cancer | |||||
| Treadwell (2016) | Sickle cell disease | |||||
| Uzark (2015) | Heart disease | |||||
| Whitfield (2015) | IBD | |||||
MCD – Multiple chronic diseases,
IBD – Inflammatory bowel disease,
= significance at the 0.05 level,
= studied but no association found
Proactive discussions about the transition to adult care between the adolescents or young adults, parents, and providers was found to positively impact transition readiness (Gumidyala et al., 2018). Parental involvement in care was inversely associated with transition readiness for youth with a history of a kidney transplant or sickle cell disease (Gilleland et al., 2011; Gilleland et al., 2015; Speller-Brown et al., 2015). Perceived barriers to medication adherence were negatively associated with transition readiness across multiple chronic diseases (Gilleland et al., 2011; Haarbauer-Krupa et al., 2019). Finally, parents’ perception of the adolescents or young adults’ transition readiness was positively associated with the adolescents and young adults’ overall responsibility for their disease self-management (Speller-Brown et al., 2015). Other self-management and transition education factors that did not demonstrate any significant associations with transition readiness included occurrence of transition (Jensen et al., 2017), adherence (Fredericks et al., 2010; Rosen et al., 2016), and engagement with providers after transition (Szalda et al., 2017).
Health Outcome Factors
Only one study identified a relationship between transition readiness, and health and health care utilization outcomes. As transition readiness increased in adolescents and young adults who had undergone kidney transplants, emergency room utilization decreased (Fenton et al., 2015). In addition, transition readiness was positively related to adherence in the same study (Fenton et al., 2015). No studies assessed the relationship between transition readiness levels prior to transition, and health or health care utilization outcomes after transition.
Discussion
The purpose of this systematic review was to explore the literature regarding factors associated with transition readiness in adolescents and young adults with chronic disease, and to identify factors useful to intervention design. Thirty-three studies met the inclusion criteria and were included in the analysis. A variety of modifiable factors were found to be significantly associated with transition readiness; however, most of these factors were only studied in a single study or in a single chronic disease population. One of the most commonly identified modifiable factor was self-efficacy, which was found to be significantly, positively associated with transition readiness across multiple studies and disease populations. This finding is supported by the literature on pediatric chronic disease management where self-efficacy has been found to have a positive effect on chronic disease self-management (Noser, Huffhines, Clements, & Patton, 2017; Rhee, Belyea, Ciurzynski, & Brasch, 2009; Smith et al., 2018). Self-efficacy is an important concept to consider when designing transition readiness interventions, because it encompasses disease self-management and the knowledge and skills needed to independently navigate the health care system.
Adolescent and young adult’s responsibility for disease management, disease-specific knowledge, perceived barriers to medication adherence, and parental involvement in disease management were also found to be significantly associated with transition readiness. While these factors were not studied as frequently as self-efficacy, they show promise as factors that are potentially amenable to intervention. Adolescent and young adult’s responsibility for disease management and parental involvement in disease management, otherwise known as allocation of treatment responsibility, have been studied within the context of self-management and treatment adherence, but not for transition readiness (Pai et al., 2010; Pai et al., 2011). Additionally, few studies in this review assessed concepts related to family functioning. There is a need for more research in this area as it is critical to future interventions that the family’s role in development of transition readiness be accounted for. The majority of disease management occurs within the home, and it is negotiated between parents and adolescents or young adults. Understanding how disease management is shared or distributed between parents and adolescents or young adults could help predict an adolescent or young adult’s readiness to transition. It could help researchers and health care providers better understand how to develop interventions that encourage the transfer of responsibilities for disease management from parents to adolescents and young adults.
This analysis looked at primary studies that assessed adolescents and young adults with chronic conditions that encompassed a number of different diseases. This approach was not intended to overlook the particular nuances of a specific chronic disease; rather, this strategy offered an opportunity to understand how researchers could translate current knowledge of transition readiness to other chronic disease populations. While self-management may vary by disease, knowledge found in this review of transition readiness could be applied to chronic diseases that share similar characteristics. Factors associated with transition readiness that were only studied in a single study or a single chronic disease population, but should be considered important for future research include autonomous motivation, family cohesion, social support, hopeful future expectations, patient activation levels, anxiety, and disease-associated stress. This review highlighted the need to understand more about how these modifiable factors relate to each other, and to transition readiness across different chronic disease populations.
A variety of non-modifiable factors were found to be significantly associated with transition readiness. As with the modifiable factors, many of the non-modifiable factors were studied in a single cross-sectional study or in a single chronic disease population. Age and gender were the only non-modifiable factors whose association with transition readiness was reaffirmed across multiple studies and populations. While these factors are not modifiable, they potentially impact transition readiness; therefore, it is important that researchers and health care providers understand how these factors relate to transition readiness and consider them when designing interventions. For healthy adolescents, the development of individuality and independence is often gradual, and it is guided by a progressive shift of responsibility from the parent to the adolescent. Disease self-management for an adolescent or young adult with a chronic disease would optimally take a similar approach (Michaud, Suris, & Viner, 2004; Suris et al., 2004). Researchers should consider controlling for non-modifiable factors when designing interventions to improve transition readiness.
Other major findings of this review were gaps related to methodology. Transition readiness measurement was inconsistent across studies, and there was no agreement about the best method of measurement (de Silva & Fishman, 2014). The majority of studies included in this review used validated tools to measure transition readiness, but these tools were not disease specific. This review notes contradictory information about the benefit of disease-neutral versus disease-specific transition readiness assessment tools. It has been noted that disease-neutral tools may be the most desirable as the tools can be used to design general transition interventions that can be used across disease populations (Stinson et al., 2014). This view is disputed by Mackie et al. (2015) who noted that disease-neutral tools did not necessarily have questions that allowed them to adequately assess the adolescents and young adults’ disease self-management practices specific to their disease. The benefits of disease-neutral versus disease-specific transition readiness tools need to be further explored. While some aspects of transition are the same for all adolescents and young adults, such as the change in health provider, many differences exist such as the specifics of self-management for each chronic disease. A disease-neutral tool could be used if it included subcomponents that could be tailored to the specifics of the chronic disease.
This review primarily focused on transition readiness from the perspective of the adolescent and young adult; however, transition readiness does not occur in isolation from caregivers/parents and health care providers. All three perspectives are important to developing transition readiness preparation interventions as each stakeholder has a different perspective and role to play during this change. Future research should consider measuring transition readiness from all three perspectives so as to obtain a broader understanding of the adolescent or young adult’s progress towards developing optimal transition readiness.
This review also highlighted a gap in the understanding of how transition readiness may predict health outcomes of adolescents and young adults with chronic disease after transition. Only one study assessed health outcomes in relationship to transition readiness (Fenton et al., 2015). In addition, there were no longitudinal studies to assess how transition readiness scores affected the transition experience and subsequent health outcomes after transition. Measurement tools to assess transition readiness were designed so that health care providers could assess how the adolescent or young adult was progressing towards transition readiness prior to transition (Ferris et al., 2012; Gilleland et al., 2012; Sawicki et al., 2011; Stinson et al., 2014); however, to date, no studies have utilized these tools over time to understand transition readiness from a longitudinal perspective.
Finally, the findings of this review are limited by quality and level of evidence provided in the primary studies. A majority of the included studies were cross-sectional, correlational studies using small sample sizes and lacking power analysis. Transition readiness was assessed entirely using self-report, which means that the true level of transition readiness may have been under-or over-reported. Only a few studies utilized other perspectives, such as parents or provider’s views, to assess transition readiness. In addition, most of the studies were sampled from a single institution, which decreased the ability to generalize the findings. Finally, the lack of theory supporting the studies made it difficult to align findings across the body of work.
The transition to the adult health care system has the potential for significant negative effects on the health and well-being of adolescents and young adults living with chronic disease. Transition readiness is an important area of research still requiring further descriptive research to understand factors that contribute to the development of transition readiness. Modifiable factors, such as self-efficacy, the adolescent and young adult’s responsibility for disease management, disease-specific knowledge, perceived barriers to medication adherence, and parental involvement in disease management, are all amenable to intervention. Non-modifiable factors, such as age and gender, should be considered when developing research or carrying out statistical analysis. Further research is necessary to address gaps identified in this review, and there is a need for more longitudinal studies designed to provide perspective on how transition readiness changes over time and how health care providers can intervene to ensure successful transition to the adult health care setting.
Contributor Information
Maureen Varty, University of Missouri-Columbia Sinclair School of Nursing, Columbia, MO.
Lori L. Popejoy, University of Missouri-Columbia Sinclair School of Nursing, Columbia, MO.
References
- American Academy of Pediatrics (2002). A consensus statement on health care transitions for young adults with special health care needs. Pediatrics, 110(Supplement 3), 1304–1306. [PubMed] [Google Scholar]
- Annunziato RA, Emre S, Shneider B, Barton C, Dugan CA, & Shemesh E. (2007). Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatric Transplantation, 11(6), 608–614. doi:doi: 10.1111/j.1399-3046.2007.00689.x [DOI] [PubMed] [Google Scholar]
- Asp A, Bratt E-L, & Bramhagen A-C (2015). Transfer to adult care: Experiences of young adults with congenital heart disease. Journal of Pediatric Nursing, 30(5), e3–e10. doi: 10.1016/j.pedn.2015.05.025 [DOI] [PubMed] [Google Scholar]
- Beal SJ, Riddle IK, Kichler JC, Duncan A, Houchen A, Casnellie L, … Corathers SD (2016). The associations of chronic condition type and individual characteristics with transition readiness. Academic Pediatrics, 16(7), 660–667. doi: 10.1016/j.acap.2016.06.007 [DOI] [PubMed] [Google Scholar]
- Bemrich-Stolz CJ, Halanych JH, Howard TH, Hilliard LM, & Lebensburger JD (2015). Exploring adult care experiences and barriers to transition in adult patients with sickle cell disease. International Journal of Hematology & Therapy, 1(1), 10.15436/12381–11404.15415.15003. doi: 10.15436/2381-1404.15.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham CA, Scalzi L, Groh B, Boehmer S, & Banks S. (2015). An assessment of variables affecting transition readiness in pediatric rheumatology patients. Pediatric Rheumatology Online Journal, 13(1), 42–42. doi: 10.1186/s12969-015-0040-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blinder MA, Vekeman F, Sasane M, Trahey A, Paley C, & Duh MS (2013). Age-related treatment patterns in sickle cell disease patients and the associated sickle cell complications and healthcare costs. Pediatric Blood & Cancer, 60(5), 828–835. doi: 10.1002/pbc.24459 [DOI] [PubMed] [Google Scholar]
- Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, & Slap GB (1993). Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. Journal of Adolescent Health, 14(7), 570–576. [DOI] [PubMed] [Google Scholar]
- Brousseau DC, Owens PL, Mosso AL, Panepinto JA, & Steiner CA (2010). Acute care utilization and rehospitalizations for sickle cell disease. Journal of the American Medical Association, 303(13), 1288–1294. doi: 10.1001/jama.2010.378 [DOI] [PubMed] [Google Scholar]
- Burström Å, Öjmyr-Joelsson M, Bratt E-L, Lundell B, & Nisell M. (2016). Adolescents with congenital heart disease and their parents: Needs before transfer to adult care. Journal of Cardiovascular Nursing, 31(5), 399–404. doi: 10.1097/jcn.0000000000000288 [DOI] [PubMed] [Google Scholar]
- Carlsen K, Gordon J, Haddad N, Phan BL, Benkov K, Dubinsky MC, … Keefer L. (2017). Self-efficacy and resilience are useful predictors of transition readiness scores in adolescents with inflammatory bowel diseases. Inflammatory Bowel Diseases, 23(3), 341–346. doi: 10.1097/MIB.0000000000001038 [DOI] [PubMed] [Google Scholar]
- Cohen SE, Hooper SR, Javalkar K, Haberman C, Fenton N, Lai H, … Ferris M. (2015). Self-management and transition readiness assessment: Concurrent, predictive and discriminant validation of the STARx questionnaire. Journal of Pediatric Nursing, 30(5), 668–676. doi: 10.1016/j.pedn.2015.05.006 [DOI] [PubMed] [Google Scholar]
- de Silva PSA, & Fishman LN (2014). Transition of the patient with IBD from pediatric to adult care: An assessment of current evidence. Inflammatory Bowel Diseases, 20(8), 1458–1464. doi: 10.1097/MIB.0000000000000045 [DOI] [PubMed] [Google Scholar]
- Dickerson AK, Klima J, Rhodes MM, & O’Brien SH (2012). Young adults with SCD in US children’s hospitals: Are they different from adolescents? Pediatric Blood & Cancer, 58(5), 741–745. doi:doi: 10.1002/pbc.23262 [DOI] [PubMed] [Google Scholar]
- Dwyer-Matzky K, Blatt A, Asselin BL, & Wood DL (2018). Lack of preparedness for pediatric to adult-oriented health care transition in hospitalized adolescents and young adults. Academic Pediatrics, 18(1), 102–110. doi: 10.1016/j.acap.2017.07.008 [DOI] [PubMed] [Google Scholar]
- Eaton CK, Davis MF, Gutierrez-Colina AM, LaMotte J, Blount RL, & Suveg C. (2017). Different demands, same goal: Promoting transition readiness in adolescents and young adults with and without medical conditions. Journal of Adolescent Health, 60(6), 727–733. doi: 10.1016/j.jadohealth.2017.01.002 [DOI] [PubMed] [Google Scholar]
- Eluri S, Book WM, Kodroff E, Strobel MJ, Gebhart JH, Jones PD, … Dellon ES (2017). Lack of knowledge and low readiness for health care transition in eosinophilic esophagitis and eosinophilic gastroenteritis. Journal of Pediatric Gastroenterology and Nutrition, 65(1), 53–57. doi: 10.1097/MPG.0000000000001415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton N, Ferris M, Ko Z, Javalkar K, & Hooper SR (2015). The relationship of health care transition readiness to disease-related characteristics, psychosocial factors, and health care outcomes: Preliminary findings in adolescents with chronic kidney disease. Journal of Pediatric Rehabilitation Medicine, 8(1), 13–22. doi: 10.3233/PRM-150314 [DOI] [PubMed] [Google Scholar]
- Ferris M, Cohen S, Haberman C, Javalkar K, Massengill S, Mahan JD, … Hooper SR (2015). Self-management and transition readiness assessment: Development, reliability, and factor structure of the STARx questionnaire. Journal of Pediatric Nursing, 30(5), 691–699. doi: 10.1016/j.pedn.2015.05.009 [DOI] [PubMed] [Google Scholar]
- Ferris ME, Harward DH, Bickford K, Layton JB, Ferris MT, Hogan SL, … Hooper SR (2012). A clinical tool to measure the components of health-care transition from pediatric care to adult care: The UNC TRxANSITION Scale. Renal Failure, 34(6), 744–753. doi: 10.3109/0886022X.2012.678171 [DOI] [PubMed] [Google Scholar]
- Fish R, Judd A, Jungmann E, O’Leary C, Foster C, & Network HYP (2014). Mortality in perinatally HIV-infected young people in England following transition to adult care: An HIV Young Persons Network (HYPNet) audit. HIV Medicine, 15(4), 239–244. doi:doi: 10.1111/hiv.12091 [DOI] [PubMed] [Google Scholar]
- Fredericks EM, Dore-Stites D, Well A, Magee JC, Freed GL, Shieck V, & James Lopez M. (2010). Assessment of transition readiness skills and adherence in pediatric liver transplant recipients. Pediatric Transplantation, 14(8), 944–953. doi: 10.1111/j.1399-3046.2010.01349.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey KC, Beste MG, Luff D, Atakov-Castillo A, Wolpert HA, & Ritholz MD (2014). Experiences of health care transition voiced by young adults with type 1 diabetes: A qualitative study. Adolescent Health, Medicine and Therapeutics, 5, 191–198. doi: 10.2147/AHMT.S67943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey KC, Wolpert HA, Rhodes ET, Laffel LM, Kleinman K, Beste MG, … Finkelstein JA (2012). Health care transition in patients with type 1 diabetes: Young adult experiences and relationship to glycemic control. Diabetes Care, 35(8), 1716–1722. doi: 10.2337/dc11-2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilleland J, Amaral S, Mee L, & Blount R. (2012). Getting ready to leave: Transition readiness in adolescent kidney transplant recipients. Journal of Pediatric Psychology, 37(1), 85–96. doi: 10.1093/jpepsy/jsr049 [DOI] [PubMed] [Google Scholar]
- Gilleland Marchak J, Reed-Knight B, Amaral S, Mee L, & Blount RL (2015). Providers’ assessment of transition readiness among adolescent and young adult kidney transplant recipients. Pediatric Transplantation, 19(8), 849–857. doi: 10.1111/petr.12615 [DOI] [PubMed] [Google Scholar]
- Goossens E, Stephani I, Hilderson D, Gewillig M, Budts W, Van Deyk K, & Moons P. (2011). Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: An analysis of transfer destinations. Journal of the American College of Cardiology, 57(23), 2368–2374. doi: 10.1016/j.jacc.2010.11.068 [DOI] [PubMed] [Google Scholar]
- Gray WN, Hommel KA, Morgan PJ, Holbrook E, Saeed SA, & Denson LA (2015). Transition readiness skills acquisition in adolescents and young adults with inflammatory bowel disease: Findings from integrating assessment into clinical practice. Inflammatory Bowel Diseases, 21(5), 1125–1131. doi: 10.1097/MIB.0000000000000352 [DOI] [PubMed] [Google Scholar]
- Grimsby GM, Burgess R, Culver S, Schlomer BJ, & Jacobs MA (2016). Barriers to transition in young adults with neurogenic bladder. Journal of Pediatric Urology, 12(4), 258.e251–258.e255. doi: 10.1016/j.jpurol.2016.04.015 [DOI] [PubMed] [Google Scholar]
- Gumidyala AP, Plevinsky JM, Poulopoulos N, Greenley RN, Lerner D, Cabrera J, … Kahn SA (2018). Moving on: Transition readiness in adolescents and young adults with IBD. Inflammatory Bowel Diseases, 24(3), 482–489. doi: 10.1093/ibd/izx051 [DOI] [PubMed] [Google Scholar]
- Gutierrez-Colina AM, Reed-Knight B, Eaton C, Lee J, Loiselle Rich K, Mee L, … Blount RL (2017). Transition readiness, adolescent responsibility, and executive functioning among pediatric transplant recipients: Caregivers’ perspectives. Pediatric Transplantation, 21(3), e12898. doi:doi: 10.1111/petr.12898 [DOI] [PubMed] [Google Scholar]
- Haarbauer‐Krupa J, Alexander NM, Mee L, Johnson A, Wise J, Arora Gupta N, … Gilleland Marchak J. (2019). Readiness for transition and health‐care satisfaction in adolescents with complex medical conditions. Child: Care, Health and Development, 45(3), 463–471. doi: 10.1111/cch.12656 [DOI] [PubMed] [Google Scholar]
- Hart LC, Pollock M, Hill S, & Maslow G. (2017). Association of transition readiness to intentional self-regulation and hopeful future expectations in youth with illness. Academic Pediatrics, 17(4), 450–455. doi: 10.1016/j.acap.2016.12.004 [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, Snyder PR, Palladino DK, Becker DJ, Siminerio L, & Escobar O. (2013). Characterizing the transition from paediatric to adult care among emerging adults with Type 1 diabetes. Diabetic Medicine, 30(5), 610–615. doi:doi: 10.1111/dme.12067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang JS, Gottschalk M, Pian M, Dillon L, Barajas D, & Bartholomew LK (2011). Transition to adult care: Systematic assessment of adolescents with chronic illnesses and their medical Teams. The Journal of Pediatrics, 159(6), 994–998.e992. doi: 10.1016/j.jpeds.2011.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javalkar K, Fenton N, Cohen S, & Ferris M. (2014). Socioecologic factors as predictors of readiness for self-management and transition, medication adherence, and health care utilization among adolescents and young adults with chronic kidney disease. Preventing Chronic Disease, 11, E117–E117. doi: 10.5888/pcd11.140072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javalkar K, Johnson M, Kshirsagar AV, Ocegueda S, Detwiler RK, & Ferris M. (2016). Ecological factors predict transition readiness/self-management in youth with chronic conditions. Journal of Adolescent Health, 58(1), 40–46. doi: 10.1016/j.jadohealth.2015.09.013 [DOI] [PubMed] [Google Scholar]
- Jensen PT, Paul GV, LaCount S, Peng J, Spencer CH, Higgins GC, … Ardoin SP (2017). Assessment of transition readiness in adolescents and young adults with chronic health conditions. Pediatric Rheumatology Online Journal, 15(1), 70–70. doi: 10.1186/s12969-017-0197-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joanna Briggs Institute. (2018). The JBI Approach. Retrieved from http://joannabriggs.org/jbi-approach.html#tabbed-nav=Levels-of-Evidence
- Johnson MAJ, Javalkar K, Van Tilburg M, Haberman C, Rak E, & Ferris ME (2015). The relationship of transition readiness, self-efficacy, and adherence to preferred health learning method by youths with chronic conditions. Journal of Pediatric Nursing, 30(5), e83–e90. doi: 10.1016/j.pedn.2015.05.014 [DOI] [PubMed] [Google Scholar]
- Lazaroff SM, Meara A, Tompkins MK, Peters E, & Ardoin SP (2018). How do health literacy, numeric competencies, and ptient activation relate to transition readiness in adolescents and young adults with rheumatic diseases? Arthritis Care & Research. doi: 10.1002/acr.23739 [DOI] [PubMed] [Google Scholar]
- Lewis SA, & Noyes J. (2013). Effective process or dangerous precipice: Qualitative comparative embedded case study with young people with epilepsy and their parents during transition from children’s to adult services. BMC Pediatrics, 13, 169–169. doi: 10.1186/1471-2431-13-169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackie AS, Rempel GR, Islam S, Rankin K, McCurdy C, Vonder Muhll I, … Kovacs AH (2016). Psychosocial maturity, autonomy, and transition readiness among young adults with congenital heart disease or a heart transplant. Congenital Heart Disease, 11(2), 136–143. doi:doi: 10.1111/chd.12300 [DOI] [PubMed] [Google Scholar]
- McManus MA, Pollack LR, Cooley WC, McAllister JW, Lotstein D, Strickland B, & Mann MY (2013). Current status of transition preparation among youth with special needs in the United States. Pediatrics, 131(6), 1090–1097. doi: 10.1542/peds.2012-3050 [DOI] [PubMed] [Google Scholar]
- McPherson M, Thaniel L, & Minniti CP (2009). Transition of patients with sickle cell disease from pediatric to adult care: Assessing patient readiness. Pediatric Blood & Cancer, 52(7), 838–841. doi: 10.1002/pbc.21974 [DOI] [PubMed] [Google Scholar]
- Michaud PA, Suris JC, & Viner R. (2004). The adolescent with a chronic condition. Part II: Healthcare provision. Archives of Disease in Childhood, 89(10), 943–949. doi: 10.1136/adc.2003.045377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montano CB, & Young J. (2012). Discontinuity in the transition from pediatric to adult health care for patients with attention–deficit/hyperactivity disorder. Postgraduate Medicine, 124(5), 23–32. doi: 10.3810/pgm.2012.09.2591 [DOI] [PubMed] [Google Scholar]
- Nazareth M, Richards J, Javalkar K, Haberman C, Zhong Y, Rak E, … Van Tilburg MAL (2016). Relating health locus of control to health care use, adherence, and transition readiness among youths with chronic conditions, North Carolina, 2015. Preventing Chronic Disease, 13. doi: 10.5888/pcd13.160046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noser AE, Huffhines L, Clements MA, & Patton SR (2017). Diabetes conflict outstrips the positive impact of self-efficacy on youth adherence and glycemic control in type 1 diabetes. Pediatric Diabetes, 18(7), 614–618. doi: 10.1111/pedi.12471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai ALH, Gray E, Kurivial K, Ross J, Schoborg D, & Goebel J. (2010). The Allocation of Treatment Responsibility scale: A novel tool for assessing patient and caregiver management of pediatric medical treatment regimens. Pediatric Transplantation, 14(8), 993–999. doi:doi: 10.1111/j.1399-3046.2010.01391.x [DOI] [PubMed] [Google Scholar]
- Pai ALH, Ingerski LM, Perazzo L, Ramey C, Bonner M, & Goebel J. (2011). Preparing for transition? The allocation of oral medication regimen tasks in adolescents with renal transplants. Pediatric Transplantation, 15(1), 9–16. doi: 10.1111/j.1399-3046.2010.01369.x [DOI] [PubMed] [Google Scholar]
- Pakdeeprom B, In-Iw S, Chintanadilok N, Wichiencharoen DK, & Manaboriboon B. (2012). Promoting factors for transition readiness of adolescent chronic illnesses: Experiences in Thailand. Journal of the Medical Association of Thailand, 95(8), 1028–1034. [PubMed] [Google Scholar]
- Quinn CT, Rogers ZR, McCavit TL, & Buchanan GR (2010). Improved survival of children and adolescents with sickle cell disease. Blood, 115(17), 3447–3452. doi: 10.1182/blood-2009-07-233700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhee H, Belyea MJ, Ciurzynski S, & Brasch J. (2009). Barriers to asthma self-management in adolescents: Relationships to psychosocial factors. Pediatric Pulmonology, 44(2), 183–191. doi: 10.1002/ppul.20972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen D, Annunziato R, Colombel JF, Benkov K, & Dubinsky M. (2016). Transition of inflammatory bowel disease care: Assessment of transition readiness factors and disease outcomes in a young adult population. Inflammatory Bowel Diseases, 22(3), 702–708. doi: 10.1097/MIB.0000000000000633 [DOI] [PubMed] [Google Scholar]
- Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, … Wood D. (2011). Measuring the transition readiness of youth with special healthcare needs: Validation of the TRAQ--Transition Readiness Assessment Questionnaire. Journal of Pediatric Psychology, 36(2), 160–171. doi: 10.1093/jpepsy/jsp128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawicki GS, Kelemen S, & Weitzman ER (2014). Ready, set, stop: Mismatch between self-care beliefs, transition readiness skills, and transition planning among adolescents, young adults, and parents. Clinical Pediatrics, 53(11), 1062–1068. doi: 10.1177/0009922814541169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon TD, Lamb S, Murphy NA, Hom B, Walker ML, & Clark EB (2009). Who will care for me next? Transitioning to adulthood with hydrocephalus. Pediatrics, 124(5), 1431–1437. doi: 10.1542/peds.2008-3834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G, Modi AC, Johnson EK, Shegog R, Austin JK, & Wagner JL (2018). Measurement in pediatric epilepsy self-management: A critical review. Epilepsia, 59(3), 509–522. doi: 10.1111/epi.13992 [DOI] [PubMed] [Google Scholar]
- Speller-Brown B, Patterson Kelly K, Vangraafeiland B, Feetham S, Sill A, Darbari D, & Meier ER (2015). Measuring transition readiness: A correlational study of perceptions of parent and adolescents and young adults with sickle cell disease. Journal of Pediatric Nursing, 30(5), 788–796. doi: 10.1016/j.pedn.2015.06.008 [DOI] [PubMed] [Google Scholar]
- Stam H, Hartman EE, Deurloo JA, Groothoff J, & Grootenhuis MA (2006). Young adult patients with a history of pediatric disease: Impact on course of life and transition into adulthood. Journal of Adolescent Health, 39(1), 4–13. doi.org/10.1016/j.jadohealth.2005.03.011 [DOI] [PubMed] [Google Scholar]
- Stewart KT, Chahal N, Kovacs AH, Manlhiot C, Jelen A, Collins T, & McCrindle BWJPC (2017). Readiness for transition to adult health care for young adolescents with congenital heart disease. Pediatric Cardiology, 38(4), 778–786. doi: 10.1007/s00246-017-1580-2 [DOI] [PubMed] [Google Scholar]
- Stinson J, Kohut Sara A, Spiegel L, White M, Gill N, Colbourne G, … Kaufman M. (2014). A systematic review of transition readiness and transfer satisfaction measures for adolescents with chronic illness. International Journal of Adolescent Medicine and Health (Vol. 26, pp. 159). [DOI] [PubMed] [Google Scholar]
- Suris JC, Michaud PA, & Viner R. (2004). The adolescent with a chronic condition. Part I: Developmental issues. Archives of Disease in Childhood, 89(10), 938–942. doi: 10.1136/adc.2003.045369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szalda D, Piece L, Brumley L, Li Y, Schapira MM, Wasik M, … Schwartz LA (2017). Associates of engagement in adult-oriented follow-up care for childhood cancer survivors. Journal of Adolescent Health, 60(2), 147–153. doi: 10.1016/j.jadohealth.2016.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treadwell M, Johnson S, Sisler I, Bitsko M, Gildengorin G, Medina R, … Smith Wally R. (2016). Self-efficacy and readiness for transition from pediatric to adult care in sickle cell disease. International Journal of Adolescent Medicine and Health, 28(4), 381–388. doi: 10.1515/ijamh-2015-0014 [DOI] [PubMed] [Google Scholar]
- Uzark K, Smith C, Donohue J, Yu S, Afton K, Norris M, & Cotts T. (2015). Assessment of transition readiness in adolescents and young adults with heart disease. The Journal of Pediatrics, 167(6), 1233–1238. doi: 10.1016/j.jpeds.2015.07.043 [DOI] [PubMed] [Google Scholar]
- Whitfield EP, Fredericks EM, Eder SJ, Shpeen BH, & Adler J. (2015). Transition readiness in pediatric patients with inflammatory bowel disease. Journal of Pediatric Gastroenterology and Nutrition, 60(1), 36–41. doi: 10.1097/mpg.0000000000000555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood DL, Sawicki GS, Miller MD, Smotherman C, Lukens-Bull K, Livingood WC, … Kraemer DF (2014). The transition readiness assessment questionnaire (TRAQ): Its Factor structure, reliability, and validity. Academic Pediatrics, 14(4), 415–422. doi: 10.1016/j.acap.2014.03.008 [DOI] [PubMed] [Google Scholar]
- Zhang LF, Ho JSW, & Kennedy SE (2014). A systematic review of the psychometric properties of transition readiness assessment tools in adolescents with chronic disease. BMC Pediatrics, 14, 4–4. doi: 10.1186/1471-2431-14-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


