Abstract
Purpose of Review:
To examine associations between video game play and obesity in children.
Recent findings:
Based on a scoping review of 26 studies (25 cross-sectional; 1 longitudinal) published in 2013–2018, 14 studies (53%) reported no association between video game play and obesity, and 12 studies reported positive associations. In a review of 8 systematic reviews, there was preliminary evidence on the effectiveness of exergame (physically active) play for weight reduction and to attenuate weight gain but little indication that interventions effectively reduced video game play or general screen-time.
Summary:
This review found ambiguous evidence on the extent to which video game play is or is not significantly associated with obesity in children and preliminary evidence of exergame play as a tool for weight reduction and attenuation of weight gain. Several gaps existed in understanding the relationship between video game play and obesity, and prospective and interventional trials are needed.
Keywords: pediatric, childhood obesity, video games, exergames, scoping review
INTRODUCTION
U.S. consumers spent $29.1 billion dollars on video games in 2017, a $10 billion dollar increase over the last 5 years, yet relatively little is documented in the scientific literature on the effects of video game play on young players [1]. Video games, an electronic game in which players control images on a video screen, first came into the world sixty years ago with two lines and a bouncing dot in “Tennis for Two” [2]. The popularity of this rudimentary game led to the development of computer devices specifically for games, called consoles, in 1972, followed by hand-held devices in 1989, 3-D gaming in 1995, motion-activated active video games (called “exergames”) that require bodily movement to control on-screen play, and online gaming [3]. The additional use of screens in daily life is a major concern as high amounts of television (TV) viewing have been linked to higher obesity prevalence in children [4] and adverse energy-balance related behaviors including consumption of unhealthy foods while viewing TV [5] and lower physical activity, as screen-time has traditionally been a sedentary behavior [6]. Research assessing the impact of video game play on young players is needed to keep pace with a rapidly evolving video game industry that remains highly popular and increasingly complex.
At a time when youth are surrounded by a multitude of screen and technology options, the popularity of video games has stood the test of time. The majority of adolescents (13–17 years) have smart phones (95%), and 90% report they play video games on a cellphone, console or computer [7]. Accordingly, video games may be better called “digital games” as they reach diversified platforms like smartphones and tablets and push the limits of immersive gaming through virtual reality and augmented reality. Time spent playing video games is quickly exceeding TV viewing in children [8], potentially due to the virtual and immersive social interaction [9] and the proliferation of inexpensive or free digital games on a variety of devices. This evolution has concerned the public health and lay community as video games have been linked to poor social development and delayed cognition in children as young as preschool [10]. As for physical development, previous evidence has found traditional seated video games to be associated with increased caloric intake [11] and a 2-fold increase in obesity per hour/day played [12].
Early reports in 2004, including a meta-analysis and a cross-sectional examination, found children who had a higher weight status reported more frequent video game play [13, 14]. Interest in this sedentary behavior continued with a meta-analysis in 2008 that found inconsistent results with video game play and obesity in children, though when video games were combined with TV, there was a significant positive association [15]. Around this time, video games were becoming repurposed to utilize for positive health-related changes, most notably exergames that required the player to engage in upper and/or lower body movement [16]. No longer solely a sedentary pastime, exergaming was investigated in early studies as a genre of video game that indicated promise for improving players’ physical activity levels [17] and consequently reduce body fat and obesity [18].
Prior systematic reviews have focused on relationships of screen-time in general with children’s adiposity without specifically focusing on video game play. For example, a recent systematic review that examined 40 studies published from 2010–2017 indicated a positive association of screen-time with adiposity in children and adolescents in 85% of the studies (mostly cross-sectional, though six longitudinal and one intervention was included), yet this review did not specifically examine video game play isolated from other screen activities nor did it specify effects of newer generation games like exergames on obesity [19]. The increasing exposure and advances in video games in the past five years, coupled with the historically high prevalence of childhood obesity, warrant an updated review of the association of video game play with childhood obesity. Therefore, the aim of this study was to critically review potential associations between video game play and obesity in children by examining recently published observational studies and interventions. Accordingly, we sought to answer three main questions.
What is the current state of observational evidence (cross-sectional and prospective data published in the most recent 5 years) on the relationship between video game play and childhood obesity? (Part 1)
To what extent do video games serve as an effective intervention tool for healthy weight in children? (Part 2)
What gaps still exist in understanding the relationship between video games and obesity, in particular energy balance behaviors? (Part 3)
Part 1: Scoping Review: Video Games and Obesity in Children
Methods
A systematic search of PubMed, PsycINFO, and CINAHL databases was conducted for studies published in the English language from December 2013 until November 2018. The search terms included a combination of MeSH Terms or engine specific search terms of video games (video gam*, active video gam*, exergam*) and obesity (obesity, adiposity). Observational studies in a child population (average age 2.0–18.9 years old) that assessed the relationship between obesity and video games (or vice versa) were included. Studies that included video games as a mediator or moderator of an association between a predictor variable (obesity-related behaviors such as sleep or diet) and obesity were also included [20,21]. Studies were excluded if they were conducted in children with a chronic condition (such as autism) or in adults; used a non-observational study design (such as case study, intervention, qualitative study, or systematic review); involved video game development (such as characters or features of video games); or were specific to video game addiction tendencies.
Two authors (CLK and EDJ) independently screened abstracts retrieved from the initial search. Full text articles of selected abstracts were independently assessed for inclusion by the same authors. Any disagreement in eligibility after the abstract or full text process was resolved by the third author (AES). Reference lists of the included articles were scanned for relevance. Data were extracted into a pre-piloted form including type of study; population characteristics (age, race, setting, and country); study methodology; measures of video game play and obesity; and main results.
Results
The selection of studies is detailed in Figure 1. Three hundred and twenty articles, including 319 articles from initial search and one article through reference lists of included full text articles, were identified. After removing 84 duplicates, 236 original articles were screened. In abstract screening, 164 abstracts did not pass screening as they included children with chronic conditions (n=17), were in adults (n=7), were interventions or qualitative studies (n=52), were systematic reviews or meta-analyses (n=43), assessed another media device (n=4), were focused on video game addiction (n=3), or were the outside of the scope of the review (n=38). The 38 abstracts that were outside of scope included those with no measure of video game play or assessed general sedentary behaviors (n=19), no measure of obesity (n=7), validation studies (n=4), assessed parental habits on obesity (n=3), were not in English (n=2), assessed only children who had obesity introducing no variability (n=1), were reporting on child-care general screen-time policies (n=1), or were an education guide for parents (n=1). Forty-three systematic reviews or meta-analyses from original screening of 236 articles were assessed for eligibility in Part 2. Thirty-nine articles excluded as they assessed broad energy balance behaviors (n=14), were outside of scope (n=12), addressed only video game play or obesity but not both (n=7), or were overall opinion pieces (n=6). The remaining 4 articles are discussed in Part 2 they pertain to exergames [22–24] or general video games [25], and they present aggregate findings.
Figure 1.
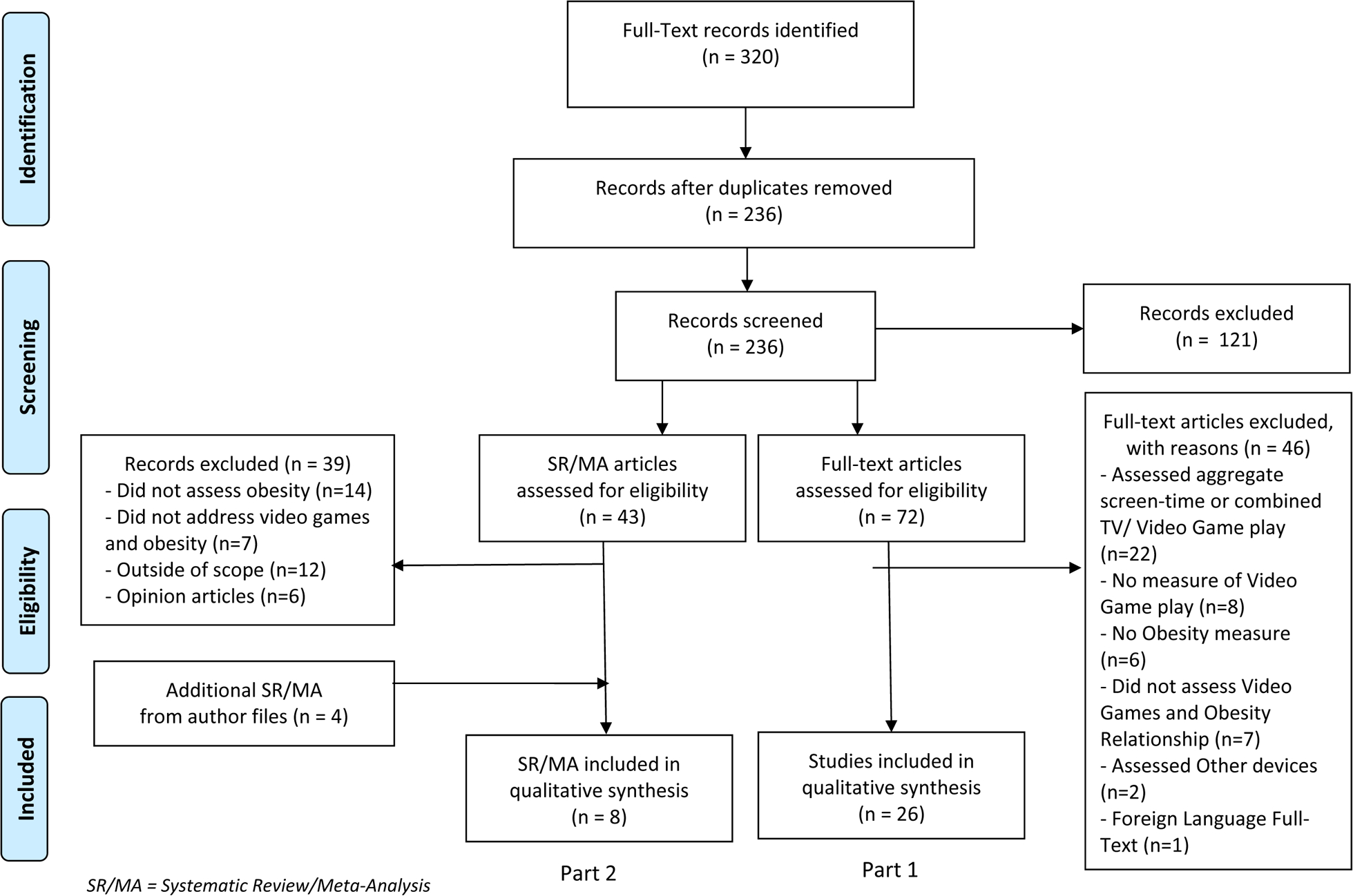
Flow Chart of Study Selection
Seventy-two articles remained for full-text screening. Forty-six articles did not pass full-text screening as many articles (n=22) assessed aggregate screen time or combined TV/video games without specifically reporting on video game play separate from the other types of screen-time. Twenty-six articles were ultimately selected for data extraction [20, 21, 26–49].
Descriptive characteristics of the included articles are reported in Table 1. In total, 25 cross-sectional studies and one longitudinal study with follow-up of 2 years were identified. Sample sizes of included studies ranged from 91 to 24,800 (median: 938), and half of studies were conducted in Canada (n=7) or the US (n=6). The youngest age range included was 2–13 years [29], as most focused on the 10–12 year old age range [28, 30, 36, 45–47, 49] or included a broad age range of adolescents ages 11–18 years old [20, 26, 27, 32, 37, 39, 42]. The oldest data were collected in 2001 [35], and the most recent data collection was 2015 [48], with all other studies occurring between these time points.
Table 1.
Descriptive Characteristics of Included Studies in Part 1 (n=26)^
| Author, Year, Country | Sample size | Age Range | Video Game Measure, quantity (groups) | Obesity Measure, objective vs. self-report (groups) | Association (−, 0, +) |
Key Relevant Findings |
|---|---|---|---|---|---|---|
| Video Game, Duration Played (n=11 studies) | ||||||
| Bickham, 2013, USA | 91 | 13–15 years | VG play, reported as 15-minute blocks during day using questionnaire (TUD) delivered via ecological momentary assessment. | BMI, Objective measure | 0 | No association between VG play and BMI in crude model and in model adjusted for gender, physical activity level, and ecological momentary assessment adherence. |
| Busch, 2013, Netherlands | 2,425 | 11–18 years | Excessive VG console use, h/day (grouped as ≥14 h/week, < 14 h/week) | Overweight, Self-Report (normal, overweight) | 0 | No relationship between excessive VG console use and overweight status in crude model and model adjusted for age, sex, school, school year, education, ethnicity, and socioeconomic status. |
| Cameron, 2016, Canada | 283 | 14–18 years | VG (Seated) time, number of hours per day | BMI z-score, Objective measure | 0 | No association between VG time and BMI z-score in indirect model adjusted for age, sex, race/ethnicity, parent education, physical activity, Tanner Stage, television viewing, and computer use. No crude models reported. |
| Falbe, 2013, USA | 7,892 | 11–19 years | Combined VG/Computer Game time, number of hours/week (0–31+) of electronic games (video/computer) | Change in BMI over 2 years (2004–2006; 2006–2008), Self-Report | + (girls) 0 (boys) |
Among girls, baseline VG/computer game time associated with gains in BMI in crude model and model adjusted for age, race, Tanner stage, menarche status, and months in between questionnaires. No associations found for boys. |
| Fragkou, 2016, Greece | 306 | 10–15 years | VG/Computer/Mobile/Tablet Use, hours/day | BMI, Self-Report (normal, overweight/ obese) | + | Children who used VG/computer/mobile/ tablet were more likely to be overweight/obese in crude model and model adjusted for gender and television in the bedroom. VG use not assessed individually. |
| Herman, 2014, Canada | 534 | 8–10 years | VG/Computer time, average hours per day | BMI, WC, Objective measure (normal, overweight/obese) | 0 | No difference in VG/Computer time between normal and overweight/obese status in crude model. No adjusted model reported. |
| Hilpert, 2017, Germany | 781 | 6.5–7.2 years | VG/Computer time, average minutes per day | BMI, Objective measure | 0 | No association between VG/computer time and BMI in model adjusted for age, gender, migration status, socioeconomic status and sports/activity level. No crude model reported. |
| Leatherdale, 2015, Canada | 23,031 | 9–12 grade students (~14–18 years) | VG/Computer Game Use, minutes/day | BMI, Self-Report (normal, overweight, obese) | + | VG/computer games use positively associated with overweight and obese status in models adjusted for gender, grade, ethnicity, weekly spending money, smoking, drinking, marijuana use, physical activity and fruit and vegetable consumption. No crude model reported. |
| Robinson, 2015, Australia | 264 | 7–10 years | VG/Computer Games (Non-active E-games), number of hours/day | BMI, WC, Objective measure | 0 | No association between non-active e-games and adiposity in crude model or model adjusted for sex, school cluster, physical activity, accelerometer wear, and diet composite score. |
| Shakir, 2018, Australia | 234 | 10–13 years | VG Use, average minutes/day, MARCA | BMI, WC, WHR, %BF, Objective measure | + (boys) 0 (girls) |
VG use positively associated in boys with %BF in models adjusted for age, income, physical activity, Tanner stage, sleep, bedtime, and wake time. No association in girls. No crude model reported. |
| Wijtzes, 2014, Netherlands | 5,913 | 5–7 years | VG/Computer Use, average minutes of use per day (<1 h/day, ≥ 1 h/day) | BMI z-score, %BF mass, Objective measure (normal, overweight /obese) | 0 | VG/computer game use positively associated with BMI z-score but not %BF mass in crude model. No association when adjusted for age, sex, ethnicity, maternal education, income, maternal employment. |
| Video Game Play on Weekdays (n=8 studies) | ||||||
| Arango, 2014, Columbia | 546 | 11–18 years | VG/PC Use, options: no use, <1/h day, 1 h/day, 2 h/day, 3 h/day, 4 h/day, 5+ h/day (<2 h/day,≥ 2 h/day) | BMI z-score, WC, Objective measure | 0 | No relationship between PC/VG use and WC or BMI z score in crude models or models adjusted for age, school location (urban or rural), physical activity level, school, carbonated sweetened beverage consumption, fast food consumption, high fat consumption or cardiorespiratory fitness. |
| Gates, 2013, Canada | 348 | 10–18 years | VG/Internet Use After School, hours/day (≤ 2h, > 2h) | BMI, Self-Report (normal, overweight, obese) | + (boys) 0 (girls) |
VG/internet use amount positively related to weight status in boys in the crude comparison and in models including adjusted standardized residuals. VG not associated with weight status in crude or adjustment standardized residuals for girls. |
| Kenney, 2017, USA | 24,800 | 14–18 years | VG/Computer/Smart Phone/Tablet (screen device) Use, hours per average school day (never, <1 h, 1 h, 2 hs, 3 hs, 4 hs, 5+ hs) | BMI percentile, Self-report (non-obese, obese) | + | Using screen devices for 5 or more hours daily associated with higher odds of obesity in models adjusted for age, sex, race/ethnicity, and screen use. A dose-response relationship was observed between higher daily use and higher risk of obesity in models adjusted for the same covariates. No crude models reported. |
| Lowry, 2013, USA | 11,429 | 9th-12th grade students (~14–18 years) | VG/Computer Use, average hours of use/school day (≤3 h/day or >3 h/day) | BMI percentile, Objective measure (underweight, normal, overweight, obese) | 0 | No relationship between obesity and VG/computer use in crude models or models adjusted for age, sex, race/ethnicity, grade in school, physical activity participation, and environmental support for physical activity. |
| Marttinen, 2017, USA | 14,285 | 12–18 years | Non-School Related VG/Computer Use, hours per day | BMI, Self-Report (normal, overweight / obese) | 0 | VG/Computer use higher in children who were overweight/had obesity compared to normal weight children in crude models. No association found after adjustment for gender, grade in school, ethnicity, TV viewing or physical activity level. |
| Mwaikambo, 2015, Tanzania | 1,722 | 7–14 years | VG Use, if VG are usually played (i.e. at least once per week) (yes or no) | BMI, Objective measure (normal, overweight, obese) | 0 | Prevalence of overweight and obesity higher in children who usually played video games in the crude model. No association found after adjustment for age, gender, school, number of siblings, parental education, active transport, TV viewing, and computer use. |
| Stamatakis, 2013, Portugal | 14,752 | 2–13 years | VG (Electronic Games), hours/day (0.5 h/day, 0.5–1 h/day, >1 h/day) | BMI z-score, sum of skinfold, Objective measure | 0 | No significant association between electronic games and both adiposity indices in crude model and model adjusted for age, sex, parental education, parental BMI, crime perception, sleep, birthweight, breastfeeding, diet, and physical activity. |
| Stroebele, 2013, USA | 1,095 | 5th grade students(~10–11 years) | VG/computer on average school day (<2 h/day, ≥2 h/day) | BMI, Self-Report (normal, overweight) | 0 | No difference in VG/computer use by weight status in crude models. No adjusted model reported. |
| Video Games Played before Bed (n=5 studies) | ||||||
| Arora, 2013a, UK | 632 | 11–18 years | VG Use at bedtime, TUQ, (no, sometimes, usually, always) | BMI z-score, Objective measure | + | VG use at bedtime positively associated with BMI z score in crude model and model adjusted for age, sex, ethnicity, school, snacking, caffeine, depression, school transport, sleep apnea, bedroom sharing, napping, and sleep duration. |
| Arora, 2013b, UK | 624 | 11–18 years | VG Use before Bedtime, TUQ, (never, sometimes, usually, always) | BMI z-score, Objective measure | + | VG use categories positively associated with BMI z-score in crude model and models adjusted for age, sex, ethnicity, physical activity, school, snacking, depression, bedroom sharing, and morning-eveningness. |
| Chahal, 2013, Canada | 3,398 | 5th grade students (~10–11 years) | VG/Computer games before Bed, options: never, monthly, 1–3 times/week, 1/night, several times/night (≤1 time per week, >1 time per week) | BMI, Objective measure (normal, overweight, obese) | 0 | No association between VG/computer games before bed and overweight or obesity in independent crude models or models adjusted for gender, income, parental education, and area of residence. |
| Dube, 2017, Canada | 2,334 | 5th grade students (~ 10–11 years) | VG Access in Bedroom, coded with VG use before bed (no access and no use, use and no access, access and no use, use and access) | BMI, Objective measure, (normal, overweight, obese) | + | Access to VG and frequent use of VG not associated with overweight in crude model but was associated after adjustment for gender, income, region, parental education, and electronic device use. Access to VG and never user was associated with obesity in crude model and model adjusted for same covariates. |
| Turel, 2017, USA | 125 | 9–17 years | VG duration 4 hours before bed, minutes/day | Abdominal adiposity (WHR), WC, Objective measure | 0 | No association between VG session duration before bed and WHR in crude model. |
| Video Game during Holidays (n=1 study) | ||||||
| Chou, 2017, Taiwan | 3,251 | 10–12 years | VG/Computer Use during Holidays, number of hours per device (none, <1 h, 1–2 h, 2–3 h, >3 h) | BMI, Objective measure (underweight, normal, overweight, obese) | + | VG use amount higher in children who were overweight or had obesity compared to normal or underweight children in crude model. 1 hours and 2–3 h of VG/computer use associated with a higher BMI compared to those who did not engage in VG/computer use in model adjusted for sex, physical activity, television viewing, and body shape perception. |
| Video Game Presence in Child’s Bedroom (n=2 studies) | ||||||
| Dube, 2017, Canada | 2,334 | 5th graders (~ 10–11 years) | VG Access in Bedroom, coded with VG use before bed (no access and no use, use and no access, access and no use, use and access) | BMI, Objective measure (normal, overweight, obese) | + | Access to VG and frequent use of VG not associated with overweight in crude model but was associated after adjustment for gender, income, region, parental education, and electronic device use. Access to VG but never using VG in bedroom were more likely to have obesity compared to normal weight in crude model and model adjusted for same covariates. |
| Ferrari, 2015, Brazil | 441 | 9–11 years | VG in Bedroom (yes, no) | BMI, Objective measure | + | No association found in crude model. Presence of VG in bedroom associated with a higher BMI in model adjusted for gender, school, and income. |
^26 studies in total, Dube, 2017 is represented twice in the table; + = Video games positively associated with obesity in most fully adjusted model; 0 = no association; - = inverse association; BMI = Body Mass Index; h = Hours; PC= Personal Computer; %BF= percent body fat; TUD= Time-Use Diaries; VG= video game; MARCA= Multimedia Activity Recall for Children and Adolescents; WC= waist circumference; WHR= Weight to Height Ratio.
Articles were grouped by characterization of video game play, including total hours of video game play in general (n=11), video game play on weekdays (n=8), video game play before bed (n=5), video game play during school holiday (n=1), and video game presence in the child’s bedroom (n=2). One article was reported twice in Table 1 as the study reported both on video game play before bed and presence of a video game console in the bedroom [49], and two articles came from one research study [39, 40].
Fourteen of the 26 articles (53%) reported no association between video game play and obesity, whereas 12 reported a positive association. No article found an inverse relationship between video game play and obesity. In the 11 articles that assessed duration of video game play in general, seven articles did not find an association in adjusted models [21, 31, 33–35, 37, 43] while the other four articles reported significant associations [26, 28, 38, 47]. Two of these significant findings only found associations in boys or girls but not overall; one article reported that video game hours played was positively associated with percent body fat in boys but not girls [28], while the other article found baseline video game/computer game hours was associated with larger BMI gains in girls but not in boys [26]. Of the other two articles reporting significant associations, one article found that a combined media use score (including use of video game/computer/mobile/tablet) was associated with a higher risk of obesity (OR: 3.24 [95% CI: 1.42 −7.27]) [47] though video game use itself was not assessed. Another article found children who had overweight/obesity had more minutes of video game play per day (36.3 ± 1.7 min/day) compared to children who were normal weight (8.7 ± 1.7 min/day) in adjusted models [38].
For the eight articles specifically reporting on weekday use of video games, six articles (75%) reported no significant association between video game play and obesity [29, 32, 36, 41, 42, 44]. Two of the non-significant article found positive associations between video game play on weekdays and obesity in crude models but this association was no longer significant in models adjusted for sociodemographic variables or other health behaviors [42, 44]. For the two articles that did observe significant associations between weekday video game play and obesity, Gates et al. (2013) found that more boys who were overweight or had obesity played video games/used the internet after school more than 2 hours per day than boys who were normal weight in a sample of First Nation youth in Ontario [27]. Kenney and Gortmaker (2017) found children with 5+ hours of other screen viewing (including video game play) on weekdays had a higher risk of obesity in adjusted models (OR: 1.34 [1.21, 1.71]) [48]. Of the five articles examining video game play before bedtime, one article reported no association between video games before bed and obesity [30], with the other four reporting significant associations with frequency of video games [39], access to video games [49] or via a mediation model including poor sleep [20, 40]. Only two articles reported video game presence in the child’s bedroom, and both found that access to video games in the bedroom was associated with higher weight [45, 49].
Few articles reported on the indirect relationships between video gaming and obesity via other health behaviors. Preliminary evidence indicated that video game play may be related to higher carbohydrate intake [21] and insufficient sleep [20, 39], but this evidence is limited.
There were patterns distinguishing the articles that did or did not observe a significant association of video game play with obesity. Articles that found a positive association between video game play and obesity typically collected data after 2012 [20, 45–49] except for one where data were collected in 2009 [39, 40]. Articles reporting a positive association also typically combined video games with other screen devices (namely mobile phones and computer use), making it difficult to parse out the independent relationship of video game play and obesity aside from these other types of screen-time [47, 48]. However, articles that combined video game play with computer or other devices that collected data prior to 2012 found little or no association [30, 32, 33, 35, 36]. There were no consistent differences in results based on whether obesity was classified by self-report or objectively measured. There is limited comment to be made on the longitudinal influence of video games on the incidence of obesity as only one longitudinal study was identified, and this study drew upon data collected more than 10 years ago [26].
Summary
Overall, there is inconsistent evidence of the relationship between video gaming and obesity, with just over half of articles indicating no significant association between video game play and obesity. Longitudinal studies that report specifically on video game play (exclusive of other screen time) and include newer generation video games like exergames and mobile games is required to understand relationships between modern video game play and obesity in this quickly evolving technological landscape. Further, the role of video game play on obesity-related behaviors warrants further attention.
Part 2: Video Games as an Intervention for Healthy Weight (Review of Reviews)
In recent years, video game play has been a behavioral target for weight reduction and attenuation among children and adolescents – on the one hand, to reduce sedentary video game play and, conversely, to manipulate traditionally sedentary video games into physically active game play. This section summarizes the systematic reviews published from 2013–2018 that utilized video games in weight reduction interventions or weight attenuation, including 4 reviews identified in the literature search and 4 identified by the authors’ files. Descriptive characteristics of the included reviews are shown in Table 2.
Table 2.
Descriptive Characteristics of Included Studies in Part 2 (n=8)^
| Reducing Video Game Play and Screen-Time for Weight Reduction (n=2) | |||||||
|---|---|---|---|---|---|---|---|
| Author, Year, Country | SR/MA | Years Searched | Criteria | Total Studies Included | Relevant studies | Outcomes | Key Relevant Findings |
| Marsh et al., 2014 [50] | SR | Inception - 2012 | Family based RCTs with children (2–18 years) | 17 | 2 RCTs using exergames | Sedentary screen time, body weight, body composition | 1 home based RCT reduced sedentary screen time. 1 home based RCT reported no difference in sedentary screen time but found a decrease in body weight and body composition. |
| Wu et al., 2016 [25] | SR/MA | Inception −2015 | RCTs | 14 | 12 (5 RCT in children <6 y, 7 RCTs in 6–17 y) | Screen time (hours/week), BMI | There was no significant effect on screen time or BMI in either sub-group (< 6 y or 6–17 y). |
| Using Video Games to Reduce Weight or Attenuate Weight Gain (n=6) | |||||||
| Author, Year, Country | SR/MA | Years Searched | Criteria | Total Studies Included | Studies with Obesity Measure | Obesity Measure | Key Relevant Findings |
| Gao et al., 2015 [23] | SR/MA | 1985–2015 | Children (<18 years) | 35 | 9 interventions | Body composition | Small effect sizes were found for exergame play compared to field-based physical activity on decreasing body composition. |
| Gao & Chen, 2014 [24] | SR | 1985–2013 | Children (<18 years) field based setting | 34 | 6 RCTs, 2 interventions | BMI, %BF, weight loss | In home based settings, 4 RCTs found no effect on BMI or weight loss. In school settings, 2 RCTs and 2 intervention studies reported weight loss. |
| Lamboglia et al., 2013 [22] | SR | 2008–2012 | Children (6–15 years) | 9 | 8 RCTs | BMI, WC | 2 RCTs reported lower obesity outcomes (WC and BMI). 1 RCT found increases in BMI. 5 RCTs reported no effect on obesity outcomes. |
| LeBlanc et al., 2013 [60] | SR | 1992–2012 | Children (0–17 years) | 51 | 6 RCTs, 3 Interventions | BMI, BMI z-score, %BF, weight gain | 3 RCTs attenuated weight gain in children with OV/OB. 1 RCT with NW children attenuated weight gain, and 2 RCTs found no effect. 3 intervention studies reported no effect in children who were NW or with OV/OB. |
| Lu et al., 2013 [53] | SR | 2005–2013 | Children (<18 years) | 28 | 14 Interventions | BMI, BMI z-score, WC, Skinfolds, BIA, WHR | 4 interventions reported differences in obesity outcomes, and all of these interventions included only children with OV/OB. 1 intervention reported effects in the first half of study and 1 intervention found effect only among girls. 8 interventions found no effect on obesity outcomes. |
| Zeng & Gao, 2016 [59] | SR | 2010–2016 | Children with OV/OB (<18 y) | 12 | 7 RCTs | BMI, BF, WC, body weight, | 4 RCTs reported reduction in BMI and BF. 3 RCTs showed no effect on BMI, WC, or body weight. |
SR = systematic Review; MA = meta-analysis; RCTs = Randomized Control Trials; OV/OB = overweight and obesity; NW= normal weight; BMI = Body Mass Index; %BF= percent body fat; WC= waist circumference; BIA= bioelectrical impedance analysis; WHR= Weight to Height Ratio.
Current State of Evidence
Reducing Video Game Play and Screen-Time for Weight Reduction
Two systematic reviews published in the past 5 years surveyed randomized controlled trials (RCTs) that targeted screen-time reduction in children and adolescents; both reviews revealed that most interventions have failed to effectively reduce screen-time [25, 50]. Without effectively changing the behavioral target, it is challenging to examine the influence of reduced screen-time (or, more specifically, reduced time spent playing video games) on weight.
Wu et al. identified 12 trials published prior to September 2015; pooled mean differences indicated no significant change in youths’ screen-time nor a change in BMI [25]. Marsh et al. (2014) identified 17 trials of family-based RCTs to reduce sedentary time in children ages 2–18 years that actively involved parents; notably, these trials were published prior to April 2012 [50]. Most trials restricted screen-time as the main strategy to reduce sedentary time, with the interventions delivered through counseling/group sessions, TV monitoring devices, or the promotion of physical activity to displace sedentary screen-time. Two trials created a behavioral contingency where the child was required to be physically active to watch TV, and two trials examined exergames as a strategy to incorporate physical activity into video games. There were inconsistencies in the effectiveness of these interventions to reduce sedentary time: ten trials significantly reduced sedentary time whereas seven did not. Sixteen of the 17 trials reported body weight or body composition as a secondary outcome. Two RCTs that were described as effective for weight loss included a 2-year screen-time reduction intervention for preschool-aged children (n=70) that significantly reduced BMIz compared to a monitoring control group [51] and a 6-month exergaming intervention that reduced BMIz and fat mass among children ages 10–14 years (n=322) who received exergames vs. those who received sedentary video games [52]. Findings on weight outcomes from the other 14 trials were not reported.
Using Video Games to Reduce Weight
Contrary to restricting screen-time, video games have also been examined as potential tools to reduce weight and improve obesogenic behaviors in children and adolescents, using the games to teach or reinforce healthy eating strategies or to engage the player in physical activity. Lu et al. (2013) conducted a systematic review on the effects of health video games on childhood obesity and identified 28 studies published between 2005 and 2013 [53]. Three published trials involved health games that researchers developed to promote healthy eating; two of these trials effectively improved eating habits including fruit and vegetable consumption whereas one did not; however, none affected obesity outcomes. The other 25 video games examined were exergames, which has become the predominant video game genre being examined for potential weight-related outcomes.
Exergames may offer opportunities for moderate-to-vigorous physical activity (MVPA), which the Physical Activity Guidelines for Americans concluded is associated with reduced risk of excess weight gain in children [54]. The Youth Compendium of Physical Activities, compiled from a literature search of published energy expenditure data in youth, reported physical activity intensities from exergame play based on the specific type of exergame and the age range; intensities ranged from the lowest of 1.3 METs indicating light intensity activity for Nintendo Wii muscle conditioning exergames to the highest of 7.7 METs indicating vigorous intensity physical activity for action running exergames [55]. Of the 116 intensity classifications for exergames (29 types of exergames catalogued across 4 age groups), 8% were classified as vigorous, 52% as moderate, and 48% as light intensity. Further, a meta-analysis of 35 studies conducted by Gao et al. (2015) indicated that exergames elicited small to moderate increases in intensity based on heart rate above laboratory-based exercises activities such as brisk walking and biking, but exergaming was lower in intensity than laboratory-based running [23]. Other systematic reviews and meta-analyses published prior to 2013 similarly indicated that exergaming can reach levels of light-to-moderate intensity physical activity [56–58]. Therefore, exergames have been examined in recent years a potential physical activity tool to reduce excessive weight gain among children and adolescents.
Six systematic reviews were identified that surveyed the effects of exergaming interventions on change in weight among children and adolescents and included in this analysis [22–24, 53, 59, 60]. In general, authors across the systematic reviews acknowledged that the evidence for exergaming affecting obesity outcomes is inconclusive. As expected, there was significant overlap in the included studies across the systematic reviews. The most recently published systematic review was from Zeng & Gao (2016), which identified 12 studies published from January 2010 to May 2016 that were specifically conducted in overweight youth or youth with obesity [59]. Seven RCTs examined adiposity as an outcome variable, with four of these RCTs demonstrating a significant improvement in BMI, body composition, or body fat but the other three RCTs observing no significant changes. Similarly, Gao & Chen (2014) identified 34 studies of field-based exergaming with variable effects on obesity-related outcomes, with the authors pointing out issues related to design, measurement, and methodology that produced inconsistent results [24]. LeBlanc et al. (2013) reviewed 51 unique studies published from 2006–2012 and identified six RCTs and three interventions that examined changes in weight [60]. Four of the six RCTs attenuated weight gain, including all three RCTs focused exclusively on overweight youth or youth with obesity and one RCT that included normal weight participants. None of the three non-RCT intervention studies observed weight loss among youth who were normal weight or overweight. Lamboglia et al. (2013) identified nine exergaming studies including eight that measured obesity; two of these studies observed significant reductions in an obesity outcome [22]. Finally, Lu et al. (2013) reviewed 14 studies of 28 health video games published between 2005 and 2013 and observed significant reductions in obesity in six studies, and all six of the effective studies utilized exergaming [53].
Exergaming has been incorporated into two published pediatric weight loss trials [61, 62]. Trost et al. conducted a group-randomized clinical trial comparing a 16-week family weight management program with or without exergaming among 75 overweight children aged 8 to 12 years [61]. The exergaming group received a game console and two exergames to play at home, and this group significantly reduced BMIz by −0.12 and increased MVPA by 1 hour/week compared to the non-exergaming group. A second study was a pilot feasibility study that assigned 48 children between 8 and 16 years of age to an “Exergaming for Health” multidisciplinary weight management program involving 10 weekly 2-hour sessions, with 1-hour consisting of exercise/exergaming and 1-hour of nutrition instruction [62]. Exergames were housed at the recreation center where families attended weight management sessions, and participants were encouraged to engage in 3 hours of additional exercise each week outside of the sessions. The 40 children who completed the program attained an average BMIz reduction of −0.07; however, there was no comparator group. The manuscript did not report the extent to which children played exergames outside of the group sessions, so it is not possible to examine the influence of exergame play on children’s weight loss. Both studies failed to meet thresholds of BMIz reduction considered to be clinically meaningful (≥0.25 units) [63].
Newer mobile-based video games such as geocaching and augmented reality games like Pokemon Go have been recently investigated as strategies to promote physical activity, but there were no systematic reviews available. Gamification has also been identified as a potential strategy to promote healthy behaviors. A systematic review that identified 19 empirical studies (4 in the pediatric population) on the effect of gamification on health and well-being observed improvements in children’s fruit and/or vegetable consumption, but weight changes were not reported [64]. However, gamification does not meet the definition of a video game; gamification applies game design principles such as competition or rewards to a non-game context, without involving a fully immersive video game [65].
Part 3: Areas for Future Research
Overall, there is inconclusive evidence that video games directly influence childhood obesity, from both observational and intervention studies. There are multiple opportunities for future areas of research into video game play and its potential effects on childhood obesity, including better capturing quality or content not just quantity of video game play as related to obesity and related behaviors. Video games may positively influence snacking and unhealthy energy intake, which can lead to positive energy balance and excess weight gain [21, 66]. Similar mechanisms have been proposed for TV viewing, which may evoke similar sedentary behavior as traditional console-based sedentary video game play but differ from mobile-based gaming [50, 67, 68]. There is a growing interest in video game play before bedtime due to delaying sleep onset and shortening sleep duration, as youth with shorter sleep duration have been shown to consume more calories [69, 70] and have higher prevalence of obesity [71].
Co-participation and within game socialization are areas to be investigated as social interaction is a main feature of many video games and may differentially impact obesity-related behaviors [72]. Two-thirds of parents play video games with their child at least once a week, thus reducing parental screen-time may influence child video game play [1]. This area warrants additional research.
Understanding the extent to which exergames may be integrated into comprehensive behavioral change programs is warranted, as coupling exergames with nutrition education and psychosocial counseling has produced reduction in children’s weight status [62]. The assessment of video game play needs to extend into other popular modalities such as esport leagues, which are competitive video game leagues including both individual and team options [73]. Esports are quickly growing popularity and projected to reach a $23.5 billion industry itself by 2020 [74]. The mass use and social acceptability of video gaming may have downstream influences on energy-related behaviors on children [75].
While this review did not specifically examine video game addiction, further investigations are needed into pathways of video game addiction and potential links to obesity [72]. Video game addiction has been associated other negative outcomes, including lower school performance and higher substance use in adolescence [76] and problematic gaming behaviors later in life [77].
Strengths of the current body of literature include that there are several reports of video game play and obesity specifically in children and adolescents. The relationship of video game play with other obesity metrics (such as body fat percentage) are also beginning to be reported in the scientific literature to add precision beyond anthropometry [28, 29, 43]. Further, more investigation of potential mediation and moderation models [20, 40] will help to advance the understanding of the complex relationship between video game play and obesity via behavioral mechanisms.
There are still many limitations and areas of improvement in this field. A chief limitation is the lack of prospective trials. In the 12 of 26 articles that did report significant associations between video game play and obesity, it is not possible to identify causal relationships. Is video game play causing childhood obesity, or are children with obesity more likely to play video games, or does video game play cluster with other obesogenic behaviors like higher dietary intake and poor sleep and these behaviors may independently explain observed associations? Another limitation of the literature is that video games advance at a much faster speed than study protocols. This lag limits the potential for long-term studies and creates a constantly evolving definition of video games. These challenges may be surmountable with nimble protocol designs and industry-research partnerships [78]. Finally, the objective measurement of video game play has not yet advanced, and research has continually relied on self-report data. Objective measures of television use are possible [79], but video game consoles can also be used for many other purposes (streaming services), video games can be played on multiple platforms (cell phone, console, or computer), and modern video game play varies widely in terms of content (e.g. from first person shooter to dance and sports games to augmented reality in a fantasy world). Therefore, it is increasingly difficult to unobtrusively and objectively quantify children’s video game play.
CONCLUSIONS
Overall, there is inconclusive evidence that video games are associated with obesity and, due to the lack of longitudinal studies, virtually no evidence to evaluate if video game play directly contributes to obesity or weight gain in children. On the other hand, there is some (limited) evidence that video game play that involves physical activity can be integrated within behavioral programs to help children to lose weight and attenuate weight gain. Future research should delve into the co-occurrence of video game play with obesogenic behaviors and continue to keep pace with the constantly growing and evolving video game industry to understand the impact of this popular pastime on children’s health.
Acknowledgements:
We would like to acknowledge Lori Steib and Stacie Davis for their assistance in retrieving journal articles for the review.
Funding: CLK was supported by T32DK064584from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. AES was supported in part by 1 U54 GM104940 from the National Institute of General Medical Sciences of the NIH, which funds the Louisiana Clinical and Translational Science Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest: Kracht, Joseph, and Staiano declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent: This article does not contain any studies with human subjects performed by any of the authors.
REFERENCES
- 1.Entertainment Software Association. Essential facts about the computer and video game industry [press release] (2018. May 14) [cited 2019 Mar 27]. Available from: http://www.theesa.com/wp-content/uploads/2018/05/EF2018_FINAL.pdf.
- 2.Tretkoff E This month in physics history, October 1958: physicist invents first video game [Internet]. American Physical Society; 2008. [cited 2019 Mar 27]. Available from: https://www.aps.org/publications/apsnews/200810/physicshistory.cfm [Google Scholar]
- 3.HISTORY. Video game history [Internet]. A & E Television Networks; 2017. [updated 2018 Aug 21; cited 2019 Mar 27]. Available from: https://www.history.com/topics/inventions/history-of-video-games [Google Scholar]
- 4.Hu EY, Ramachandran S, Bhattacharya K, Nunna S. Obesity Among High School Students in the United States: Risk Factors and Their Population Attributable Fraction. Prev Chronic Dis. 2018;15:E137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghobadi S, Hassanzadeh-Rostami Z, Salehi-Marzijarani M, Bellissimo N, Brett NR, Totosy de Zepetnek JO, et al. Association of eating while television viewing and overweight/obesity among children and adolescents: a systematic review and meta-analysis of observational studies. Obes Rev. 2018;19(3):313–20. [DOI] [PubMed] [Google Scholar]
- 6.Dutra GF, Kaufmann CC, Pretto AD, Albernaz EP. Television viewing habits and their influence on physical activity and childhood overweight. J Pediatr. 2015;91(4):346–51. [DOI] [PubMed] [Google Scholar]
- 7.*.Pew Research Center. Teens, social media & technology 2018 [press release] (2018. May 31) [cited 2019 Mar 27]. Available from: http://www.pewinternet.org/2018/05/31/teens-social-media-technology-2018/.; This report provides recent evidence of video game use by teenagers, including use of different devices.
- 8.Bucksch J, Inchley J, Hamrik Z, Finne E, Kolip P, Germany HSG. Trends in television time, non-gaming PC use and moderate-to-vigorous physical activity among German adolescents 2002–2010. BMC Public Health. 2014;14:351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dobbins S, Hubbard E, Flentje A, Dawson-Rose C, Leutwyler H. Play provides social connection for older adults with serious mental illness: A grounded theory analysis of a 10-week exergame intervention. Aging Ment Health. 2018:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carson V, Lee EY, Hesketh KD, Hunter S, Kuzik N, Predy M, et al. Physical activity and sedentary behavior across three time-points and associations with social skills in early childhood. BMC Public Health. 2019;19(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaput JP, Visby T, Nyby S, Klingenberg L, Gregersen NT, Tremblay A, et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr. 2011;93(6):1196–203. [DOI] [PubMed] [Google Scholar]
- 12.Stettler N, Signer TM, Suter PM. Electronic games and environmental factors associated with childhood obesity in Switzerland. Obes Res. 2004;12(6):896–903. [DOI] [PubMed] [Google Scholar]
- 13.Marshall SJ, Biddle SJ, Gorely T, Cameron N, Murdey I. Relationships between media use, body fatness and physical activity in children and youth: a meta-analysis. Int J Obes Relat Metab Disord. 2004;28(10):1238–46. [DOI] [PubMed] [Google Scholar]
- 14.Vandewater EA, Shim MS, Caplovitz AG. Linking obesity and activity level with children’s television and video game use. J Adolesc. 2004;27(1):71–85. [DOI] [PubMed] [Google Scholar]
- 15.Rey-Lopez JP, Vicente-Rodriguez G, Biosca M, Moreno LA. Sedentary behaviour and obesity development in children and adolescents. Nutr Metab Cardiovasc Dis. 2008;18(3):242–51. [DOI] [PubMed] [Google Scholar]
- 16.Baranowski T, Buday R, Thompson DI, Baranowski J. Playing for real: video games and stories for health-related behavior change. Am J Prev Med. 2008;34(1):74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Staiano AE, Calvert SL. Exergames for Physical Education Courses: Physical, Social, and Cognitive Benefits. Child Dev Perspect. 2011;5(2):93–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Foley L, Maddison R. Use of active video games to increase physical activity in children: a (virtual) reality? Pediatr Exerc Sci. 2010;22(1):7–20. [DOI] [PubMed] [Google Scholar]
- 19.Tripathi M, Mishra SK. Screen time and adiposity among children and adolescents: a systematic review. J Public Health. 2019. doi: 10.1007/s10389-019-01043-x [DOI] [Google Scholar]
- 20.*.Turel O, Romashkin A, Morrison KM. A model linking video gaming, sleep quality, sweet drinks consumption and obesity among children and youth. Clin Obes. 2017;7(4):191–8. [DOI] [PubMed] [Google Scholar]; This study evaluated a potential mediation mechanism linking video games to obesity through sleep quality and sweet drinks consumption.
- 21.Cameron JD, Maras D, Sigal RJ, Kenny GP, Borghese MM, Chaput JP, et al. The mediating role of energy intake on the relationship between screen time behaviour and body mass index in adolescents with obesity: The HEARTY study. Appetite. 2016;107:437–44. [DOI] [PubMed] [Google Scholar]
- 22.Lamboglia CM, da Silva VT, de Vasconcelos Filho JE, Pinheiro MH, Munguba MC, Silva Junior FV, et al. Exergaming as a strategic tool in the fight against childhood obesity: a systematic review. J Obes. 2013;2013:438364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao Z, Chen S, Pasco D, Pope Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes Rev. 2015;16(9):783–94. [DOI] [PubMed] [Google Scholar]
- 24.Gao Z, Chen S. Are field-based exergames useful in preventing childhood obesity? A systematic review. Obes Rev. 2014;15(8):676–91. [DOI] [PubMed] [Google Scholar]
- 25.**.Wu L, Sun S, He Y, Jiang B. The effect of interventions targeting screen time reduction: A systematic review and meta-analysis. Medicine (Baltimore). 2016;95(27):e4029. [DOI] [PMC free article] [PubMed] [Google Scholar]; This systematic review and meta-analysis evaluated interventions that utilized screen time reduction to target obesity. This review highlights opportunities to improve interventions targeting screen-time and preventing excess weight gain.
- 26.Falbe J, Rosner B, Willett WC, Sonneville KR, Hu FB, Field AE. Adiposity and different types of screen time. Pediatrics. 2013;132(6):e1497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gates M, Hanning RM, Martin ID, Gates A, Tsuji LJ. Body Mass Index of First Nations youth in Ontario, Canada: influence of sleep and screen time. Rural Remote Health. 2013;13(3):2498. [PubMed] [Google Scholar]
- 28.Shakir RN, Coates AM, Olds T, Rowlands A, Tsiros MD. Not all sedentary behaviour is equal: Children’s adiposity and sedentary behaviour volumes, patterns and types. Obes Res Clin Pract. 2018;12(6):506–12. [DOI] [PubMed] [Google Scholar]
- 29.Stamatakis E, Coombs N, Jago R, Gama A, Mourao I, Nogueira H, et al. Associations between indicators of screen time and adiposity indices in Portuguese children. Preventive Medicine. 2013;56(5):299–303. [DOI] [PubMed] [Google Scholar]
- 30.Chahal H, Fung C, Kuhle S, Veugelers PJ. Availability and night-time use of electronic entertainment and communication devices are associated with short sleep duration and obesity among Canadian children. Pediatric Obesity. 2013;8(1):42–51. [DOI] [PubMed] [Google Scholar]
- 31.Bickham DS, Blood EA, Walls CE, Shrier LA, Rich M. Characteristics of Screen Media Use Associated With Higher BMI in Young Adolescents. Pediatrics. 2013;131(5):935–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arango CM, Parra DC, Gomez LF, Lema L, Lobelo F, Ekelund U. Screen time, cardiorespiratory fitness and adiposity among school-age children from Monteria, Colombia. J Sci Med Sport. 2014;17(5):491–5. [DOI] [PubMed] [Google Scholar]
- 33.Robinson S, Daly RM, Ridgers ND, Salmon J. Screen-Based Behaviors of Children and Cardiovascular Risk Factors. J Pediatr. 2015;167(6):1239–45. [DOI] [PubMed] [Google Scholar]
- 34.Herman KM, Sabiston CM, Mathieu ME, Tremblay A, Paradis G. Sedentary behavior in a cohort of 8-to 10-year-old children at elevated risk of obesity. Preventive Medicine. 2014;60:115–20. [DOI] [PubMed] [Google Scholar]
- 35.Hilpert M, Brockmeier K, Dordel S, Koch B, Weiss V, Ferrari N, et al. Sociocultural Influence on Obesity and Lifestyle in Children: A Study of Daily Activities, Leisure Time Behavior, Motor Skills, and Weight Status. Obesity Facts. 2017;10(3):168–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stroebele N, McNally J, Plog A, Siegfried S, Hill JO. The Association of Self-Reported Sleep, Weight Status, and Academic Performance in Fifth-Grade Students. J School Health. 2013;83(2):77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Busch V, Manders LA, de Leeuw JRJ. Screen Time Associated with Health Behaviors and Outcomes in Adolescents. American Journal of Health Behavior. 2013;37(6):819–30. [DOI] [PubMed] [Google Scholar]
- 38.Leatherdale ST, Harvey A. Examining communication- and media-based recreational sedentary behaviors among Canadian youth: Results from the COMPASS study. Preventive Medicine. 2015;74:74- [DOI] [PubMed] [Google Scholar]
- 39.Arora T, Hosseini-Araghi M, Bishop J, Yao GL, Thomas GN, Taheri S. The complexity of obesity in UK adolescents: relationships with quantity and type of technology, sleep duration and quality, academic performance and aspiration. Pediatric Obesity. 2013;8(5):358–66. [DOI] [PubMed] [Google Scholar]
- 40.Arora T, Hussain S, Lam KBH, Yao GL, Thomas GN, Taheri S. Exploring the complex pathways among specific types of technology, self-reported sleep duration and body mass index in UK adolescents. International Journal of Obesity. 2013;37(9):1254–60. [DOI] [PubMed] [Google Scholar]
- 41.Lowry R, Lee SM, Fulton JE, Demissie Z, Kann L. Obesity and other correlates of physical activity and sedentary behaviors among US high school students. Journal of obesity. 2013;2013:276318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marttinen R, Vernikoff L, Phillips S, Fletcher N. Physical Activity, Screen Time, and Obesity: A Statistical Inquiry into Latina/o Youth. Californian Journal of Health Promotion. 2017;15(1):27–35. [Google Scholar]
- 43.Wijtzes AI, Bouthoorn SH, Jansen W, Franco OH, Hofman A, Jaddoe VW, et al. Sedentary behaviors, physical activity behaviors, and body fat in 6-year-old children: the generation R study. Int J Behav Nutr Phys Act. 2014;11:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mwaikambo SA, Leyna GH, Killewo J, Simba A, Puoane T. Why are primary school children overweight and obese? A cross sectional study undertaken in Kinondoni district, Dar-es-salaam. BMC Public Health. 2015;15:1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ferrari GLD, Araujo TL, Oliveira LC, Matsudo V, Fisberg M. Association between electronic equipment in the bedroom and sedentary lifestyle, physical activity, and body mass index of children. J Pediat-Brazil. 2015;91(6):574–82. [DOI] [PubMed] [Google Scholar]
- 46.Chou LN, Chen ML. Influencing Factors of the Body Mass Index of Elementary Students in Southern Taiwan. Int J Env Res Pub He. 2017;14(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fragkou D, Galanis P, Pantelidis P. Prevalence and Determinants of Overweight/Obesity in Adolescents: A Cross-Sectional Study in Greece. International Journal of Caring Sciences. 2016;9(3):827- [Google Scholar]
- 48.Kenney EL, Gortmaker SL. United States Adolescents’ Television, Computer, Videogame, Smartphone, and Tablet Use: Associations with Sugary Drinks, Sleep, Physical Activity, and Obesity. J Pediatr. 2017;182:144–9. [DOI] [PubMed] [Google Scholar]
- 49.Dube N, Khan K, Loehr S, Chu Y, Veugelers P. The use of entertainment and communication technologies before sleep could affect sleep and weight status: a population-based study among children. International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Marsh S, Foley L, Wilks D, Maddison R. Family‐based interventions for reducing sedentary time in youth: a systematic review of randomized controlled trials. Obesity reviews. 2014;15(2):117–33. [DOI] [PubMed] [Google Scholar]
- 51.Epstein LH, Roemmich JN, Robinson JL, Paluch RA, Winiewicz DD, Fuerch JH, et al. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162(3):239–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maddison R, Foley L, Ni Mhurchu C, Jiang Y, Jull A, Prapavessis H, et al. Effects of active video games on body composition: a randomized controlled trial. Am J Clin Nutr. 2011;94(1):156–63. [DOI] [PubMed] [Google Scholar]
- 53.Lu AS, Kharrazi H, Gharghabi F, Thompson D. A Systematic Review of Health Videogames on Childhood Obesity Prevention and Intervention. Games Health J. 2013;2(3):131–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Powell KE, King AC, Buchner DM, Campbell WW, DiPietro L, Erickson KI, et al. The Scientific Foundation for the Physical Activity Guidelines for Americans, 2nd Edition. J Phys Act Health. 2018:1–11. [DOI] [PubMed] [Google Scholar]
- 55.Butte NF, Watson KB, Ridley K, Zakeri IF, McMurray RG, Pfeiffer KA, et al. A Youth Compendium of Physical Activities: Activity Codes and Metabolic Intensities. Medicine and science in sports and exercise. 2018;50(2):246–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Barnett A, Cerin E, Baranowski T. Active video games for youth: a systematic review. J Phys Act Health. 2011;8(5):724–37. [DOI] [PubMed] [Google Scholar]
- 57.Biddiss E, Irwin J. Active video games to promote physical activity in children and youth: a systematic review. Arch Pediatr Adolesc Med. 2010;164(7):664–72. [DOI] [PubMed] [Google Scholar]
- 58.Peng W, Lin JH, Crouse J. Is playing exergames really exercising? A meta-analysis of energy expenditure in active video games. Cyberpsychol Behav Soc Netw. 2011;14(11):681–8. [DOI] [PubMed] [Google Scholar]
- 59.**.Zeng N, Gao Z. Exergaming and obesity in youth: current perspectives. Int J Gen Med. 2016;9:275–84. [DOI] [PMC free article] [PubMed] [Google Scholar]; This systematic review identified recent exergaming studies and the impacts of exergaming on adiposity and other components of child health. This systematic review provides a comprehensive evaluation of exergames on child health and suggestions for future randomized controlled trials of exergames.
- 60.LeBlanc AG, Chaput JP, McFarlane A, Colley RC, Thivel D, Biddle SJ, et al. Active video games and health indicators in children and youth: a systematic review. PLoS One. 2013;8(6):e65351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Trost SG, Sundal D, Foster GD, Lent MR, Vojta D. Effects of a pediatric weight management program with and without active video games a randomized trial. JAMA Pediatr. 2014;168(5):407–13. [DOI] [PubMed] [Google Scholar]
- 62.Christison A, Khan HA. Exergaming for Health: A Community-Based Pediatric Weight Management Program Using Active Video Gaming. Clin Pediatr. 2012;51(4):382–8. [DOI] [PubMed] [Google Scholar]
- 63.Ford AL, Hunt LP, Cooper A, Shield JPH. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Archives of Disease in Childhood. 2010;95(4):256–61. [DOI] [PubMed] [Google Scholar]
- 64.Johnson D, Deterding S, Kuhn KA, Staneva A, Stoyanov S, Hides L. Gamification for health and wellbeing: A systematic review of the literature. Internet Interv. 2016;6:89–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.*.Cotton V, Patel MS. Gamification Use and Design in Popular Health and Fitness Mobile Applications. Am J Health Promot. 2018:890117118790394. [DOI] [PMC free article] [PubMed] [Google Scholar]; This systematic review assessed the frequency of gamification principles in common health behavior-related mobile applications. This systematic review found many mobile applications are using gamification components, but there are areas of improvement.
- 66.Chaput JP, Tremblay A, Pereira B, Boirie Y, Duclos M, Thivel D. Food intake response to exercise and active video gaming in adolescents: effect of weight status. Br J Nutr. 2016; 115(3):547–553. [DOI] [PubMed] [Google Scholar]
- 67.Boulos R, Vikre EK, Oppenheimer S, Chang H, Kanarek RB. ObesiTV: how television is influencing the obesity epidemic. Physiol Behav. 2012;107(1):146–53. [DOI] [PubMed] [Google Scholar]
- 68.Pearson N, Biddle SJ. Sedentary behavior and dietary intake in children, adolescents, and adults. A systematic review. Am J Prev Med. 2011;41(2):178–88. [DOI] [PubMed] [Google Scholar]
- 69.Chaput JP. Sleep patterns, diet quality and energy balance. Physiol Behav. 2014;134:86–91. [DOI] [PubMed] [Google Scholar]
- 70.Chaput JP, Tremblay MS, Katzmarzyk PT, Fogelholm M, Hu G, Maher C, et al. Sleep patterns and sugar-sweetened beverage consumption among children from around the world. Public Health Nutr. 2018;21(13):2385–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chaput JP, Lambert M, Gray-Donald K, McGrath JJ, Tremblay MS, O’Loughlin J, et al. Short sleep duration is independently associated with overweight and obesity in Quebec children. Can J Public Health. 2011;102(5):369–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Colder Carras M, Van Rooij AJ, Van de Mheen D, Musci R, Xue QL, Mendelson T. Video Gaming in a Hyperconnected World: A Cross-sectional Study of Heavy Gaming, Problematic Gaming Symptoms, and Online Socializing in Adolescents. Comput Human Behav. 2017;68:472–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pluss MA, Bennett KJM, Novak AR, Panchuk D, Coutts AJ, Fransen J. Esports: The Chess of the 21st Century. Front Psychol. 2019;10:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Holden JT, Rodenberg RM, Kaburakis A. Esports corruption: Gambling, doping, and global governance. Md J Int’l L. 2017;32:236. [Google Scholar]
- 75.Holden JT, Kaburakis A, Rodenberg RM. Esports: Children, stimulants and video-gaming-induced inactivity. J Paediatr Child Health. 2018;54(8):830–1. [DOI] [PubMed] [Google Scholar]
- 76.VANR AJ, Kuss DJ, Griffiths MD, Shorter GW, Schoenmakers MT, VDM D. The (co-)occurrence of problematic video gaming, substance use, and psychosocial problems in adolescents. J Behav Addict. 2014;3(3):157–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brunborg GS, Mentzoni RA, Froyland LR. Is video gaming, or video game addiction, associated with depression, academic achievement, heavy episodic drinking, or conduct problems? J Behav Addict. 2014;3(1):27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Baranowski T, Blumberg F, Gao Z, Kato PM, Kok G, Lu AS, et al. Getting Research on Games for Health Funded. Games Health J. 2017;6(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maddison R, Marsh S, Foley L, Epstein LH, Olds T, Dewes O, et al. Screen-Time Weight-loss Intervention Targeting Children at Home (SWITCH): a randomized controlled trial. Int J Behav Nutr Phys Act. 2014;11:111. [DOI] [PMC free article] [PubMed] [Google Scholar]


