Abstract
Objective:
Using an online decision aid developed to support parental decision making about newborn genomic sequencing, we tested whether adding a values clarification exercise to educational content would improve decision making outcomes and influence intention to pursue genomic sequencing. We also examined whether the effect of values clarification varied depending on one’s health literacy level.
Methods:
In an online experiment, women and men aged 18 to 44 who were either pregnant or had a pregnant partner, were currently trying to get pregnant, or were preparing for a pregnancy within the next two years were randomly assigned to complete either a decision aid with educational information about newborn genomic sequencing or a decision aid with the same educational information and a values clarification exercise.
Results:
Of the 1,000 participants who completed the decision aid, those who completed the values clarification exercise reported less decision regret, F(1, 995) = 6.19, p = .01, and were clearer about their personal values, F(1, 995) = 6.39, p = .01. Moderation analyses revealed that the benefit of values clarification on decisional conflict was particularly evident among participants with lower health literacy, B = −3.94, SE = 1.67, t = −2.36, p = .018. There was not a significant moderation effect of health literacy and decision aid condition on decision regret.
Conclusions:
Adding a values clarification exercise to decision aids for parents making decisions about genomic sequencing may improve the decision-making experience and provide some benefit to individuals with lower health literacy.
Keywords: parental decision making, values clarification, newborn screening, health literacy, genomic sequencing
Introduction
Newborn screening provides substantial public health benefits by identifying a variety of conditions that can have severe consequences, including disability and death, if they are not treated early (U.S. NLM, 2018). A multi-site research consortium jointly funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Human Genome Research Institute (NHGRI) is examining whether incorporating genome-scale sequencing into newborn screening would enhance its benefits (Berg et al., 2017). There are a variety of ethical implications and challenges surrounding the implementation of genomic sequencing as a component of newborn screening. Thus, an aim of the NICHD/NHGRI research consortium is to learn about the potential ethical, legal, and social implications of implementing a newborn screening program that includes genomic sequencing (Berg et al., 2017). The North Carolina Newborn Exome Sequencing for Universal Screening (NC NEXUS) project, one of the sites in this research consortium, has developed a decision aid to help parents make informed decisions about pursuing genomic sequencing to identify treatable conditions (Lewis et al., 2016; Milko et al., 2018).
Development of the NC NEXUS decision aid was motivated by the fact that many parents will have little or no experience to draw on when making decisions about whether to accept genomic sequencing for newborn screening. The general population has limited knowledge of genomics (Lea et al., 2011) and current newborn screening is conducted in most states without parental consent (Mandl, Feit, Larson, & Kohane, 2002). Decision aids are commonly used to promote informed decision making based on personal preferences (Stacey et al., 2017). To support this goal, decision aids typically provide educational content along with values clarification exercises. Values clarification exercises are intended to help users clarify the factors that are important to consider as part of the decision-making process. Expert consensus has strongly endorsed the inclusion of values clarification activities in decision aids to assist patients in achieving a deeper understanding and exploration of the options and their implications in order to support patients in making decisions that are consistent with their values (Elwyn et al., 2006). However, there is insufficient evidence examining the influence of key components of decision aids, and it is unclear whether values clarification activities are beneficial (Fagerlin et al., 2013; Garvelink, ter Kuile, Stiggelbout, & de Vries, 2014; Nelson, Han, Fagerlin, Stefanek, & Ubel, 2007; Witteman, Gavaruzzi, et al., 2016).
When making health care decisions, there is frequently no one right choice that applies to all decision makers. Thus, the quality of a decision is often determined by assessing decisional outcomes, such as the degree to which the decision generates decisional conflict and regret (Brehaut et al., 2003; Fagerlin et al., 2013; Hamilton et al., 2017; O’Connor, 1995; Stacey et al., 2017). Decisional conflict is characterized by the expression of uncertainty, wavering between options, a delay in decision making, and lack of clarity regarding personal values (O’Connor, 1995). Decision regret typically involves self-blame, anxiety, and distress (Becerra Pérez, Menear, Brehaut, & Légaré, 2016; Brehaut et al., 2003). Decision regret is also positively associated with decisional conflict (Becerra Pérez et al., 2016; Brehaut et al., 2003). Decision aids and particularly values clarification exercises can reduce decisional conflict by describing the alternatives and their potential consequences as well as making decision aid users active deliberators in considering these alternatives (Elwyn & Miron-Shatz, 2010; O’Connor, 1995). Among the criteria for evaluating the effectiveness of decision aids according to the International Patient Decision Aid Standards (IPDAS) is that they help individuals to be more informed about the options and their features and clear about the option features that matter most, outcomes which are assessed using the feeling informed and values clarity subscales of O’Connor’s (1995) decisional conflict scale (O’Connor et al., 2005; Stacey et al., 2017). The opportunity to weigh the tradeoffs of choosing one option over another also has the potential to reduce regret in the wake of a decision (Becerra Pérez et al., 2016). However, the inclusion of values clarification exercises has not been consistently found to reduce decisional conflict and there is little empirical evidence of their effect on decision regret (Fagerlin et al., 2013; Garvelink et al., 2014).
Another research gap identified in the literature on decision aids and values clarification relates to the potential for an interaction between health literacy and the values clarification process (McCaffery et al., 2013; McCaffery, Smith, & Wolf, 2010; Volk, Llewellyn-Thomas, Stacey, & Elwyn, 2013). A systematic review of research on health literacy and decision-making found that lower health literacy was associated with both greater decisional uncertainty and regret (McCaffery et al., 2013). However, there is little research on characteristics of decision aids that might mitigate these adverse effects of low health literacy on decision outcomes and specifically whether values clarification is beneficial to individuals with low health literacy (Elwyn et al., 2006; McCaffery et al., 2013). Thus, not only is there a need for additional research to examine the effects of values clarification, there is a need to better understand the effects of values clarification among lower literacy individuals (McCaffery et al., 2010).
Research on decision aids also seeks to understand how they influence decisions and behavior. For example, a systematic review of research on the effects of decision aids found that their influence on decisions and behavioral intentions varies depending on the choice under consideration (Stacey et al., 2017). It is worthwhile to examine the effects of decision aids on parental decision making related to genomic sequencing to contribute to our understanding of decision making in this specific context as well as to contribute to the larger body of research on the effects of decision aids on behavior. Although some research has investigated the influence of decision aids and values clarification on behavioral intentions, this research typically does not investigate whether there is a relationship between values clarification, decisional outcomes, and behavioral intentions (Sheridan et al., 2010).
Although including values clarification exercises in decision aids is a best practice as established by the IPDAS (O’Connor et al., 2005), there is a need for empirical research that examines the conditions under which values clarification is beneficial and the mechanisms through which values clarification influences decisions. The purpose of this study was to examine whether the inclusion of a values clarification exercise in a decision aid would improve decision making outcomes in parents making a simulated decision about whether to pursue genomic sequencing for their child for actionable medical conditions, like those found on newborn screening panels. We hypothesized that, compared to participants who completed an education-only version of a decision aid, those who completed a decision aid with the same educational content paired with an added values clarification exercise would report less decisional conflict and less decision regret. We also investigated the following research questions: 1) Does health literacy moderate the relationship between decision aid content and outcomes? and 2) Are decision aid condition and/or decisional outcomes associated with intention to have genomic sequencing for one’s child?
Method
Design and Participants
We conducted an online experiment to compare the effects of two versions of an online decision aid on parental decision making. Participants were randomly assigned to either a version of the decision aid that included only educational information about genomic sequencing for newborns or a version of the decision aid that included the same educational information along with a values clarification exercise.
Participants were recruited for this study by Qualtrics, which draws on multiple sources for samples, including actively managed market research panels. Qualtrics sent potential participants an email invitation informing them that the survey was for research purposes only, how long the survey was expected to take, and about available incentives. To avoid self-selection bias, the survey invitation did not include specific details about the contents of the survey. Eligible participants included women and men ages 18 to 44 who were either currently pregnant or had a spouse or partner who was pregnant, were actively trying to get pregnant, or were contemplating or preparing for pregnancy within the next two years. These criteria were used to screen for and include participants for which the sequencing decision would be relevant.
Of the 1,000 participants who completed the decision aid, 71.6% (n = 716) were female and 28.4% (n = 284) were male, the mean age was 30.19 (SD = 5.29), 64.2% (n = 642) had no children yet at the time of the study, and most were married (83.4%, n = 834). See Table 1 for additional participant characteristics.
Table 1.
Participant Characteristics (n = 1,000)
| n | % | |
|---|---|---|
| Sex | ||
| Female | 716 | 71.6 |
| Male | 284 | 28.4 |
| Marital status | ||
| Single/never married | 34 | 3.4 |
| Married | 834 | 83.4 |
| Marriage-like relationship or domestic partnership | 121 | 12.1 |
| Separated from spouse | 1 | 0.1 |
| Divorced | 5 | 0.5 |
| Other | 5 | 0.5 |
| Education | ||
| Less than high school graduate | 6 | 0.6 |
| High school graduate (or equivalent) | 84 | 8.4 |
| Partial college (at least one year) | 159 | 15.9 |
| Trade school | 22 | 2.2 |
| 2-year college degree | 105 | 10.5 |
| 4-year college degree | 385 | 38.5 |
| Graduate or professional degree | 237 | 23.7 |
| Income | ||
| Less than $14,999 | 24 | 2.4 |
| $15,000 to $29,999 | 90 | 9.0 |
| $30,000 to $44,999 | 145 | 14.5 |
| $45,000 to $59,999 | 149 | 14.9 |
| $60,000 to $74,999 | 147 | 14.7 |
| $75,000 to $89,999 | 140 | 14.0 |
| $90,000 to $104,999 | 98 | 9.8 |
| $105,000 to $119,999 | 75 | 7.5 |
| $120,000 to $134,999 | 40 | 4.0 |
| $135,000 or more | 91 | 9.1 |
| Hispanic/Latino | ||
| Yes | 98 | 9.8 |
| No | 902 | 90.2 |
| Race | ||
| American Indian or Alaska Native | 11 | 1.1 |
| Asian | 85 | 8.5 |
| Black or African American | 67 | 6.7 |
| Pacific Islander | 1 | 0.1 |
| White | 788 | 78.9 |
| Other | 15 | 1.5 |
| Multiracial (chose more than one category) | 32 | 3.2 |
Procedure
This study was reviewed and approved by RTI International’s Institutional Review Board (IRB). Participants were screened for eligibility from an online panel maintained by Qualtrics. As part of the consent process, eligible participants were told they were being asked to participate in a research study to test the usefulness of a web site that was developed with funding from the National Institutes of Health (NIH) to help parents make a decision about whether to enroll their child in a medical research study that would involve screening their newborn baby for genetic conditions. After completing the online consent form and answering questions to assess health literacy and experience with genetic testing, participants were randomly assigned to one of two experimental conditions in which they completed different versions of an online decision aid. Following completion of the decision aid, participants answered questions about the extent to which they experienced conflict and regret related to their decision, their intention to have the sequencing test for their child, and demographics.
At the end of the study, participants were thanked for their participation, reminded of the purpose of the study, and told that they had been randomly assigned to one of two groups. The two study conditions were described and participants were told that the additional tasks in the one condition – identifying whether reasons for and against getting genomic sequencing for their child were important to them and answering some questions – were designed to help people make a more informed decision about whether to choose genomic sequencing for their child. Participant compensation did not exceed $6.00 in value and was provided by Qualtrics, which offers a variety of rewards including cash, airline miles, gift cards, and vouchers.
Decision Aid
The decision aid was developed as part of the larger NC NEXUS study to help parents make informed decisions about genomic sequencing (Lewis et al., 2016; Milko et al., 2018). Decision aid design and content were guided by the International Patient Decision Aid Standards (IPDAS) checklist (O’Connor et al., 2005), input from a multidisciplinary steering committee, interviews with parents, and the literature on user-centered design principles (Lewis et al., 2016).
This study compared the effects of two experimental decision aid conditions. In one condition, participants viewed a decision aid containing educational information about newborn screening and genomic sequencing. The other condition included the same educational information, but also asked participants to complete a values clarification exercise in which they sorted reasons for and against genomic sequencing in terms of the importance to them (Table 2). These reasons for and against pursuing genomic sequencing were developed based on in-depth interviews with a diverse sample of 33 couples who were either pregnant or had recently given birth. The reasons parents gave in support of and against newborn genomic sequencing were reviewed by clinicians for medical accuracy – e.g., to ensure they did not convey a misunderstanding of the testing process or the implications of the results of testing (Fitzgerald et al., 2016; Moultrie et al., under review).
Table 2.
Reasons For and Reasons Against Having Genomic Sequencing for One’s Newborn Child Included in the Values Clarification Exercise
| Reasons For Having Genomic Sequencing | Reasons Against Having Genomic Sequencing |
|---|---|
| 1. Knowing your child has a genetic condition may help him or her get early treatment and support services. | 1. Waiting for genomic sequencing results may cause you to worry or feel anxious. |
| 2. Knowing your child has a genetic condition may help you and your family be prepared if he or she develops the condition. | 2. You do not feel prepared to learn that your child may have a genetic condition. |
| 3. Genomic sequencing may help doctors understand genetic conditions better. | 3. Knowing that the NC NEXUS study team will have your child’s genomic sequencing results makes you uncomfortable. |
| 4. Genomic sequencing may help scientists make better tools for finding serious conditions before people get sick. | 4. You are satisfied with knowing that your child will have standard newborn screening. |
| 5. You would rather not wait to see if any problems occur to find out if your child may have a genetic condition. | 5. You would rather wait to see if your child has any problems before having genetic testing. |
The values clarification exercise was restricted to five reasons in support of and five reasons against genomic sequencing due to limitations of human information processing and memory and the general inability of individuals to consolidate more than five to nine pieces of information at a time, thus limiting the number of beliefs that are likely to impact decision making (Fiske & Taylor, 1991; Miller, 1994). The number of reasons were also balanced across the two categories to avoid biasing attitudes and decisions. After sorting the reasons provided in the decision aid (see Figure 1), participants also had an opportunity to add and sort any additional reasons they felt were relevant to their decision making. Although few participants wrote in additional reasons, examples of reasons added by participants were peace of mind and concerns about unintended consequences. Participants were then shown a summary of the reasons for and against genomic sequencing that they indicated were important to them. Following this sorting exercise, they answered five questions intended to further clarify values (see Figure 2). At the end of the decision aid, participants in both conditions were asked to make a decision about whether they wanted their child to have genomic sequencing for conditions like those found in newborn screening.
Figure 1.
Sorting task in the values clarification exercise
Figure 2.
Questions included in the values clarification exercise
Measures
Decisional conflict.
Decisional conflict was assessed using 14 items from the original 16-item scale developed by O’Connor (1995; 2010). Because participants in this study were asked to make a decision about genomic testing immediately following completion of the decision aid, two items about social influences on decision making in the support subscale were not included on the questionnaire. Responses were given on a 5-point response scale ranging from strongly disagree to strongly agree. The overall decisional conflict score was created by calculating each participant’s average score over the 14 items and rescaling to range from 0 to 100, with larger values indicating greater decisional conflict (M = 28.15, SD = 18.86, α = .95). Consistent with previous research, we also calculated scores for subscales of decisional conflict (O’Conner, 2010; Stacey et al., 2017). Scores for the subscales representing four dimensions of decisional conflict were developed using a similar coding scheme as the overall scale (i.e., calculating the mean score for the items in the subscale and multiplying by 25 to convert scores to a 0–100 scale): uncertainty (M = 32.83 SD = 25.59, α = .92), informed (M = 72.63, SD = 19.08, α = .77), values clarity (M = 73.28, SD = 20.92, α = .82), and effective decision (M = 73.51, SD = 20.18, α = .92). When creating subscales, informed, values clarity, and effective decision were reverse coded so that higher scores represented feeling more informed, being clearer about one’s values, and having more positive perceptions of one’s decision. The uncertainty and values clarity subscales each comprised three items from the broader decisional conflict scale; the informed and effective decision subscales each comprised four items.
Decision regret.
Decision regret was assessed using a 5-item scale developed by Brehaut et al. (2003) (M = 2.05, SD = .66, α = .77): “I will regret the choice I made;” “My choice will do a lot of harm;” “I made the right decision;” “I would make the same choice if I had to do it over again;” and “My decision is a wise one.” Responses ranged from 1 (strongly disagree) to 5 (strongly agree). The last three items were reverse coded so that greater average scores indicated more decision regret.
Behavioral intention.
Behavioral intention was assessed with a single item adapted from measures proposed by Fishbein and Ajzen (2010) and similar to surrogate measures of choice included in Stacey et al.’s (2017) systematic review of the effects of decision aids on decisional and behavioral outcomes. Participants were asked how likely they would be to get the genomic sequencing test described in the decision aid for their child if it were offered (M = 3.74, SD = 1.09). Responses were given on a scale from 1 (extremely unlikely) to 5 (extremely likely).
Health literacy.
Health literacy was assessed using the Single Item Literacy Screener (SILS) developed by Morris et al. (2006) as a brief measure of the need for help with reading health-related materials. This single-item measure performed reasonably well at predicting limited health literacy compared to the Short Test of Functional Health Literacy in Adults (S-TOFHLA) (Brice et al., 2014; Morris et al., 2006). The single item asks participants: How often do you need to have someone help you when you read instructions, pamphlets, or other written material from your doctor or pharmacy? Responses were given on a scale from 1 (never) to 5 (always) and reverse coded so that a higher score represented higher health literacy (M = 4.40, SD = 0.99).
Experience with genetic testing.
Experience with genetic testing was assessed by asking participants a series of questions developed for this study to assess the influence of past experience on decision making (Fishbein & Ajzen, 2010; Juliusson, Karlsson, & Gärling, 2005). The three items asked about participants’ personal experience making a decision about genetic testing or having genetic testing for one’s self or child. Responses were recoded into a new dichotomous variable indicating previous experience (yes/no). Among participants, 21.5% (n = 215) reported having some experience with genetic testing.
Analyses
Analyses were conducted using ANCOVA, including gender, health literacy, and experience with genetic testing as covariates. Chi-square analyses revealed no significant differences between participants randomly assigned to the two decision aid conditions on age, marital status, number of children, education level, income, race, or ethnicity. However, there was a marginally significant difference between the two conditions on gender (p = .05). Although we included gender as a covariate to control for any potential effects in our analyses, gender was not a significant predictor in our models with decisional conflict and decision regret. Moderation and mediation analyses included the same covariates and were conducted using Hayes’ (2013) PROCESS macro, a modeling tool for SPSS that uses regression path analysis to test for direct and indirect effects in mediation models and interactions in moderation models. In moderation analyses, significant interaction effects were explored by conducting simple slopes analyses at the mean and at the mean ±1 SD of the moderator.
Results
Decisional Outcomes
To test our hypothesis, we compared the effects of the two decision aid conditions on decisional conflict and decision regret (Table 3). There was not a significant difference between the two decision aid conditions on overall decisional conflict. However, participants who completed a values clarification exercise in addition to viewing educational content reported less decision regret (M = 2.00, SE = 0.03) than those who were only exposed to the educational content (M = 2.10, SE = 0.03), F(1, 995) = 6.19, p = .013. Examining subscales of decisional conflict revealed that participants who completed a values clarification exercise in addition to viewing educational content were clearer about their personal values (M = 74.99, SE = 0.94) than those who only viewed educational content (M = 71.68, SE = 0.91), F(1, 995) = 6.39, p = .012. There were no significant differences between the two groups for the other subscales of decisional conflict.
Table 3.
Comparison of Decisional Outcomes Between the Control and Experimental Conditions
| Education-only (n = 518) | Education + Values Clarification (n = 482) | |||
|---|---|---|---|---|
| M (SE) | M (SE) | F(1, 995) | p | |
| Decisional conflict | 28.91 (0.82) | 27.33 (0.85) | 1.79 | .181 |
| Values clarity | 71.68 (0.91) | 74.99 (0.94) | 6.39 | .012 |
| Informed | 72.05 (0.83) | 73.25 (0.86) | 1.00 | .317 |
| Certainty | 33.15 (1.11) | 32.48 (1.15) | .17 | .677 |
| Effective decision | 72.87 (0.88) | 74.21 (0.91) | 1.12 | .290 |
| Decision regret | 2.10 (0.03) | 2.00 (0.03) | 6.19 | .013 |
Moderation Analyses
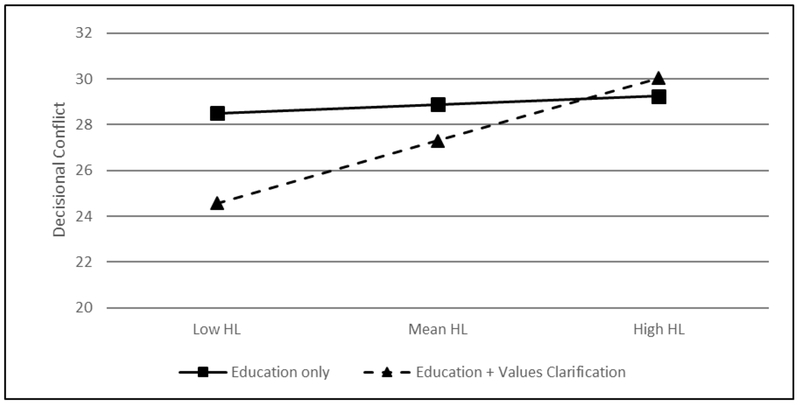
To answer our first research question, we conducted moderation analyses to examine whether the effect of the values clarification exercise varied depending on one’s level of health literacy. There was a significant interaction effect on decisional conflict from exposure to the values clarification exercise by health literacy, F (1, 994) = 4.00, p = .046. Simple slopes analysis revealed that the relationship between decision aid condition and decisional conflict was only significant among those with low health literacy, B = −3.94, SE = 1.67, 95% CI [−7.22, − 0.67], t = −2.36, p = .018 (Figure 3). Among participants with lower health literacy, those who completed the values clarification exercise experienced less decisional conflict than those in the education-only condition. Additional moderation analyses examining the four decisional conflict subscales suggested that this effect was driven by the conditional influence of the values clarification tasks on the informed (F [1, 994] = 4.09, p = .043) and effective decision dimensions (F [1, 994] = 5.35, p = .021). Participants with low health literacy who completed the values clarification exercise reported being more informed, B = 3.64, SE = 1.70, 95% CI [0.31, 6.98], t = 2.14, p = .032, and making more effective decisions, B = 4.27, SE = 1.79, 95% CI [0.76, 7.78], t = 2.39, p = .017, than low health literacy participants in the education-only condition. However, there was not a significant interaction effect of the values clarification exercise and health literacy on decision regret, p = .46.
Figure 3.
Health literacy (HL) as a moderator of the relationship between decision aid condition and decisional conflict.
Behavioral Intention
To answer our second research question, we included covariates, decision aid condition, decisional conflict, and decision regret in one regression model to investigate which variables predicted behavioral intention (i.e., intention to have one’s child tested). Decision aid condition and decision regret were not significant predictors of intention to have one’s child tested. However, lower decisional conflict was a significant predictor of stronger intentions to have one’s child tested, B = −.02, SE = .00, 95% CI [−0.02, −0.01], t(993) = −7.98, p < .001.
Because the direct effect of the decision aid condition on intention to have one’s child tested was not significant, but there was a difference between decision aid conditions on values clarity, a subscale of decisional conflict, we also investigated whether there was an indirect effect of the decision aid condition on intention to have one’s child tested through values clarity. We found a significant indirect effect of decision aid condition on intention to have one’s child tested mediated by values clarity, B = 0.05, SEbootstrap = 0.02, 95% CIbootstrap [0.01, 0.10], p = .015. Thus, participants in the values clarification condition reported greater values clarity and this, in turn, was associated with a greater intention to have one’s child tested.
Discussion
Our study contributes to the limited empirical research examining the effect of values clarification in decision aids on decision-related outcomes (Fagerlin et al., 2013). We did not find that the inclusion of a values clarification exercise influenced overall decisional conflict. This is inconsistent with the conclusion of a recent systematic review which found that decision aids reduced decisional conflict (Stacey et al., 2017). However, in this systematic review, the results for the overall decisional conflict scale – and many of the subscales – were mixed. We did find an effect of the values clarification exercise on the values clarity subscale of decisional conflict. Future and expectant parents who completed a values clarification exercise in addition to reviewing educational content had greater values clarity than those who only reviewed educational content. The systematic review by Stacey et al. (2017) found strong evidence that, compared to usual care, decision aids help individuals to feel more informed about options and to clarify their personal values. We found no difference between the two decision aid conditions on the informed subscale of decisional conflict, likely because they both contained educational content. The difference we found in values clarity supports the proposition that the finding in the systematic review is likely due to the inclusion of values clarification exercises in decision aids.
We also found that those who completed the values clarification exercise reported less decision regret than those who did not have an opportunity to engage in values clarification. Evaluations of decision aids often fail to find an effect on decision regret (Stacey et al., 2017). However, it may be that an effect on decision regret is contingent upon whether the decision aid includes a values clarification exercise. Future research should further examine the relationship between values clarification and decision regret.
Our research also makes a contribution to improving our understanding of how some benefits provided by decision aids and values clarification may vary by level of health literacy. Participants with lower health literacy in the values clarification condition reported less decisional conflict than those in the education-only condition. After conducting additional moderation analyses with decisional conflict subscales, we found that this effect was driven by the informed and effective decision subscales. Participants with low health literacy reported being more informed and making more effective decisions in the values clarification condition than in the education-only condition. Health literacy did not moderate the effect of the decision aid condition on decision regret.
According to our findings, engaging in values clarification may mitigate the effects of low health literacy on decisional conflict. However, health literacy did not moderate the effect of decision aid condition on decision regret. Instead, participants generally experienced less decision regret in the values clarification condition than in the education-only condition, irrespective of health literacy level. Thus, more time spent on deliberation while completing the values clarification exercise – considering reasons for and against having genomic sequencing done for one’s child and the implications of the decision – seems to provide valuable decision support for individuals across levels of health literacy.
Our study also suggests that values clarification exercises may influence behavioral intentions by affecting decisional conflict. We found that lower decisional conflict was associated with a stronger behavioral intention to get the sequencing test for one’s child. In a separate analysis, we found that participants in the values clarification condition endorsed reasons not to get genomic sequencing less strongly, which was in turn associated with stronger intentions to get the sequencing test (Paquin et al., 2018). Together, the findings from these two studies suggest that the values clarification process may help to reduce concerns about sequencing that contribute to decisional conflict and are barriers to getting sequencing.
A potential limitation of this research was that we asked participants to make a decision based on a hypothetical scenario rather than including participants actually facing a real-world decision. There were several reasons for this: 1) genomic sequencing is not a routine part of newborn screening so this decision does not yet widely exist in a real-world context, and 2) because this is a new decision-making context for which little research exists, we felt that ethically it was useful to test the effects of the decision aid in a hypothetical context prior to its use in a real-world context. A systematic review of studies examining the effects of values clarification in decision aids revealed that effects may be stronger (more positive or more negative) when participants were facing an actual decision compared to a hypothetical decision (Witteman, Gavaruzzi, et al., 2016). However, there was no reason to believe the effects would vary in other ways. The validity of hypothetical decision-making is also a critical question and concern within research in psychology more broadly, as much of this research has been conducted in laboratory settings. Here, too, there is evidence to suggest that human decision-making is often similar across hypothetical and real-world scenarios (Kühberger, Schulte-Mecklenbeck, & Perner, 2002; Tversky & Kahneman, 1981; Wiseman & Levin, 1996).
Another limitation related to the hypothetical nature of this study is the use of parent-reported behavioral intentions rather than actual decisions and behavior. However, a randomized controlled trial to evaluate the utility of genomic sequencing as part of newborn screening and the efficacy of the decision aid to support parental decision making is currently in the final stages of data collection (Milko et al., 2018). Once completed, the findings from this research will provide additional information about the influence of the decision aid and values clarification exercise on decisional outcomes among parents making actual decisions about whether to get genomic sequencing for their newborn child.
It is worth noting that in this study participants were asked to make a decision at the end of the decision aid and decisional outcomes were assessed immediately afterward. However, parents making decisions in the real world about whether to have genomic sequencing done for their child may have a lengthier period of deliberation. Indeed, in the larger randomized controlled trial currently underway for which this decision aid was designed, parents who initially decide that they are interested in genomic sequencing at the end of the decision aid then consult with a genetic counselor and have an opportunity to make a final decision following the consultation (Milko et al., 2018). Additional time for deliberation has the potential to influence decision-related outcomes (Busemeyer & Townsend, 1993; Elwyn & Miron-Shatz, 2010). However, the focus of this study was to assess the effect of including a values clarification exercise and, for practical purposes, we assessed decisional conflict and regret immediately following the use of the decision aid. It is not clear how length of time following exposure to a decision aid and values clarification exercises influences decisional outcomes (Stacey et al., 2017). Research indicates that delayed decision making is associated with greater decisional conflict and greater regret (Brehaut et al., 2003; O’Conner, 1995). Several factors that might influence preferences – and decision-related outcomes – over time are knowledge decay, exposure to additional information, and social influences (Elwyn et al., 2010; O’Conner, 1995). Future research could examine how these factors play a role in an extended period of deliberation.
Thus far, there is little understanding of how values clarification exercises may influence decision making. Our study contributes to this understanding by examining the influence of values clarification on decisional outcomes and the role of health literacy in the values clarification process. Future research that systematically tests the effects of varying approaches to values clarification on decisional outcomes will help to further our understanding of how values clarification contributes to the benefits provided by decision aids (Witteman, Scherer, et al., 2016).
Acknowledgments
Funding Sources
Financial support for this study was provided entirely by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Human Genome Research Institute (1 U19 HD077632–01), National Institutes of Health. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Financial Disclosure
D.B.B. currently receives research funding from The John Merck Fund and Asuragen. He provides research support in the form of contributed reagents and equipment but has no personal or financial relationship with The John Merck Fund or Asuragen. All other authors declare no conflict of interest.
Footnotes
Related Presentations
This research was presented at the 39th Annual Meeting & Scientific Sessions of the Society of Behavioral Medicine (SBM) within the Health Decision Making Special Interest Group, New Orleans, LA, April 11-14, 2018.
References
- Becerra Pérez MM, Menear M, Brehaut JC, Légaré F (2016). Extent and predictors of decision regret about health care decisions: A systematic review. Medical Decision Making, 36(6), 777–790. 10.1177/0272989X16636113 [DOI] [PubMed] [Google Scholar]
- Berg JS, Agrawal PB, Bailey DB Jr., Beggs AH, Brenner SE, Brower AM, … Wise AL (2017). Newborn sequencing in genomic medicine and public health. Pediatrics, 139(2), e20162252. doi: 10.1542/peds.2016-2252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehaut JC, O’Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, & Feldman-Stewart D (2003). Validation of a decision regret scale. Medical Decision Making, 23(4), 281–292. doi: 10.1177/0272989X03256005 [DOI] [PubMed] [Google Scholar]
- Brice JH, Foster MB, Principe S, Moss C, Shofer FS, Falk RJ, … DeWalt DA (2014). Single-item or two-item literacy screener to predict the S-TOFHLA among adult hemodialysis patients. Patient Education and Counseling, 94, 71–75. [DOI] [PubMed] [Google Scholar]
- Busemeyer JR, & Townsend JT (1993). Decision field theory: A dynamic-cognitive approach to decision making in an uncertain environment. Psychological Review, 100(3), 432–459. [DOI] [PubMed] [Google Scholar]
- Elwyn G, & Miron-Shatz T (2010). Deliberation before determination: The definition and evaluation of good decision making. Health Expectations, 13(2), 139–147. doi: 10.1111/j.1369-7625.2009.00572.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwyn G, O’Connor A, Stacey D, Volk R, Edwards A, Coulter A, … International Patient Decision Aids Standards, C. (2006). Developing a quality criteria framework for patient decision aids: Online international Delphi consensus process. BMJ, 333(7565), 417. doi: 10.1136/bmj.38926.629329.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerlin A, Pignone M, Abhyankar P, Col N, Feldman-Stewart D, Gavaruzzi T, … Witteman HO (2013). Clarifying values: An updated review. BMC Medical Informatics and Decision Making, 13 Suppl 2, S8. doi: 10.1186/1472-6947-13-s2-s8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, & Ajzen I (2010). Predicting and changing behavior: The reasoned action approach. New York: Psychology Press. [Google Scholar]
- Fiske ST, & Taylor SE (1991). Social cognition (2nd ed.). New York, NY: McGraw-Hill. [Google Scholar]
- Fitzgerald TM, Lewis MA, Moultrie RR, Zulkiewicz BA, Rini C, Roche M, & Bailey DB (2016). Couple dynamics in decisions about newborn screening via whole exome sequencing. Paper presented at the 2016 APHL Newborn Screening and Genetic Testing Symposium, St. Louis, MO. [Google Scholar]
- Garvelink MM, ter Kuile MM, Stiggelbout AM, & de Vries M (2014). Values clarification in a decision aid about fertility preservation: Does it add to information provision? BMC Medical Informatics and Decision Making, 14, 68. doi: 10.1186/1472-6947-14-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JG, Lillie SE, Alden DL, Scherer L, Oser M, Rini C, … Waters EA (2017). What is a good medical decision? A research agenda guided by perspectives from multiple stakeholders. Journal of Behavioral Medicine, 40(52), 52–68. doi: 10.1007/s10865-016-9785-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press. [Google Scholar]
- Juliusson EÁ, Karlsson N, & Gärling T (2005). Weighing the past and the future in decision making. European Journal of Cognitive Psychology, 17(4), 561–575. doi: 10.1080/09541440440000159 [DOI] [Google Scholar]
- Kühberger A, Schulte-Mecklenbeck M, & Perner J (2002). Framing decisions: Hypothetical and real. Organizational Behavior and Human Decision Processes, 89(2), 1162–1175. doi: 10.1016/S0749-5978(02)00021-3 [DOI] [PubMed] [Google Scholar]
- Lea DH, Kaphingst KA, Bowen D, Lipkus I, & Hadley DW (2011). Communicating genetic and genomic information: Health literacy and numeracy considerations. Public Health Genomics, 14(4–5), 279–289. doi: 10.1159/000294191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Paquin RS, Roche MI, Furberg RD, Rini C, Berg JS, … Bailey DB Jr. (2016). Supporting parental decisions about genomic sequencing for newborn screening: The NC NEXUS decision aid. Pediatrics, 137 Suppl 1, S16–23. doi: 10.1542/peds.2015-3731E [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandl KD, Feit S, Larson C, & Kohane IS (2002). Newborn screening program practices in the United States: notification, research, and consent. Pediatrics, 109(2), 269–273. [DOI] [PubMed] [Google Scholar]
- McCaffery KJ, Holmes-Rovner M, Smith SK, Rovner D, Nutbeam D, Clayman ML, … Sheridan SL (2013). Addressing health literacy in patient decision aids. BMC Medical Informatics and Decision Making, 13 Suppl 2, S10. doi: 10.1186/1472-6947-13-s2-s10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffery KJ, Smith SK, & Wolf M (2010). The challenge of shared decision making among patients with lower literacy: A framework for research and development. Medical Decision Making, 30(1), 35–44. doi: 10.1177/0272989X09342279 [DOI] [PubMed] [Google Scholar]
- Milko LV, Rini C, Lewis MA, Butterfield RM, Lin F-C, Paquin RS, … Powell CM (2018). Evaluating parents’ decisions about next-generation sequencing for their child in the NC NEXUS (North Carolina Newborn Exome Sequencing for Universal Screening) study: A randomized controlled trial protocol. Trials, 19(1), 344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GA (1994). The magical number seven, plus or minus two: Some limits on our capacity for processing information. Psychological Review, 101(2), 343–352. [DOI] [PubMed] [Google Scholar]
- Morris NS, MacLean CD, Chew LD, & Littenberg B (2006). The single item literacy screener: Evaluation of a brief instrument to identify limited reading ability. BMC Family Practice, 7(21), 21. doi: 10.1186/1471-2296-7-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moultrie RR, Paquin R, Bailey DB, Rini C, Roche MI, Berg JS, … Lewis MA (under review). Parental views on newborn next generation sequencing: Implications for decision support. [DOI] [PubMed]
- Nelson WL, Han PK, Fagerlin A, Stefanek M, & Ubel PA (2007). Rethinking the objectives of decision aids: A call for conceptual clarity. Medical Decision Making, 27(5), 609–618. doi: 10.1177/0272989X07306780 [DOI] [PubMed] [Google Scholar]
- O’Connor AM (1995). Validation of a decisional conflict scale. Medical Decision Making, 15(1), 25–30. doi: 10.1177/0272989X9501500105 [DOI] [PubMed] [Google Scholar]
- O’Connor A, Elwyn G, Barratt A, Barry M, Coulter A, Holmes-Rovner M, … Whelan T (2005). IPDAS 2005: Criteria for judging the quality of patient decision aids. Retrieved from http://www.ipdas.ohri.ca/IPDAS_checklist.pdf
- O’Connor AM (2010). User manual – Decisional conflict scale. Retrieved from https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Decisional_Conflict.pdf
- Paquin RS, Peinado S, Lewis MA, Biesecker BB, Rini C, Roche M, … Bailey DB (2018). A behavior-theoretic evaluation of values clarification on parental beliefs and intentions toward genomic sequencing for newborns. Social Science and Medicine. doi: 10.1016/j.socscimed.2018.11.017 [DOI] [PMC free article] [PubMed]
- Sheridan SL, Griffith JM, Behrend L, Gizlice Z, Jianwen C, & Pignone MP (2010). Effect of adding a values clarification exercise to a decision aid on heart disease prevention: a randomized trial. Medical Decision Making, 30(4), E28–39. doi: 10.1177/0272989X10369008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey D, Legare F, Lewis K, Barry MJ, Bennett CL, Eden KB, … Trevena L (2017). Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews, 4, CD001431. doi: 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tversky A, & Kahneman D (1981). The framing of decisions and the psychology of choice. Science, 211(4481), 453–458. [DOI] [PubMed] [Google Scholar]
- U.S. National Library of Medicine (NLM). (2018, November 13). What is newborn screening? Retrieved from https://ghr.nlm.nih.gov/primer/newbornscreening/nbs
- Volk RJ, Llewellyn-Thomas H, Stacey D, & Elwyn G (2013). Ten years of the International Patient Decision Aid Standards Collaboration: Evolution of the core dimensions for assessing the quality of patient decision aids. BMC Medical Informatics and Decision Making, 13(Suppl 2), S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiseman DB, & Levin IP (1996). Comparing risky decision making under conditions of real and hypothetical consequences. Organizational Behavior and Human Decision Processes, 66(3), 241–250. doi: 10.1006/obhd.1996.0053 [DOI] [Google Scholar]
- Witteman HO, Gavaruzzi T, Scherer LD, Pieterse AH, Fuhrel-Forbis A, Chipenda Dansokho S, … Fagerlin A (2016). Effects of design features of explicit values clarification methods: A systematic review. Medical Decision Making, 36(6), 760–776. doi: 10.1177/0272989X16634085 [DOI] [PubMed] [Google Scholar]
- Witteman HO, Scherer LD, Gavaruzzi T, Pieterse AH, Fuhrel-Forbis A, Chipenda Dansokho S, … Fagerlin A (2016). Design features of explicit values clarification methods: A systematic review. Medical Decision Making, 36(4), 453–471. doi: 10.1177/0272989X15626397 [DOI] [PubMed] [Google Scholar]