Abstract
Leishmaniasis involves the participation of several species of both wild and domestic mammal hosts and sandfly vectors, which demonstrates the eco-epidemiological complexity observed in this disease. Bats are among the most abundant types of mammals and the scarcity of research on Leishmania infection in these animals gives evidence of the importance of new studies that aim to clarify this relationship. This study aimed to detect the Leishmania spp. in bats. 146 bats, representing 16 different species belonging to the Molossidae, Vespertilionidae, and Phyllostomidae families, were received and processed for collection of tissues. Skin samples were collected from 100% of the bats, and liver samples were collected from 87% (n = 127). After evaluating the quality of the DNA extracted by means of PCR directed to the IRBP gene, the samples considered suitable for the Leishmania detection test were submitted for PCR directed to Leishmania kDNA, and to confirm positivity, were tested to the SSUrRNA gene-directed Nested-PCR. The Leishmania presence in the species Molossus pretiosus, Nyctinomops macrotis, and Lasiurus cinereus are the first reports this encounter in these species of bats in Brazil. Furthermore, new species of bats as possible hosts for L. infantum are reported, such as Molossus pretiosus, Myotis nigricans, Nyctinomops laticaudatus, Nyctinomops macrotis, and, for L. braziliensis, Lasiurus cinereus and Cynomops planirostris. These findings in bats in an area endemic for leishmaniasis indicate that these animals may be involved in sustaining the disease cycle in this location.
Keywords: Leishmania, Bat, Chiroptera, Reservoir, PCR
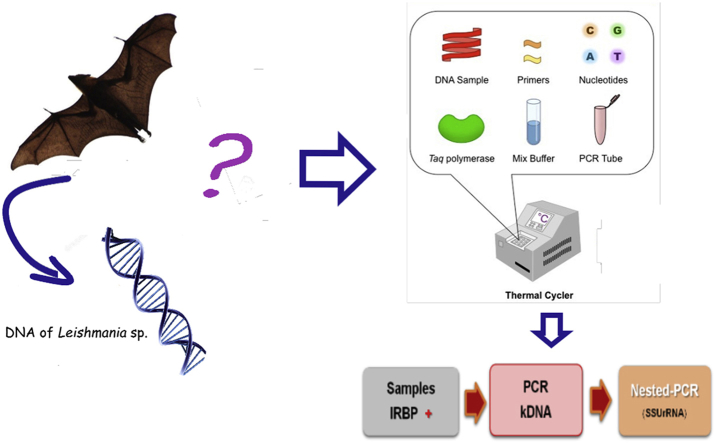
Graphical abstract
Highlights
-
•
Leishmaniasis is an endemic zoonosis that is expanding in Brazil and is considered an important public health problem.
-
•
The role of bats in the epidemiology of leishmaniais is still unclear.
-
•
The ability of bats to disperse and their longevity could facilitate the maintenance and dispersal of Leishmania.
-
•
We detected presence of L. infantum and L. braziliensis DNA in bats in the Brazilian Midwest.
-
•
Infected bats in areas endemic for leishmaniasis may indicate participation in the maintenance of parasites in these places.
1. Introduction
Leishmaniasis is an endemic zoonosis that is expanding in Brazil and is considered an important public health problem that is difficult to control (Brasil, 2014; OPAS, 2019). The disease is caused by obligate intracellular protozoa and presents a wide range of pathological processes, ranging from cutaneous to visceral, due to the multiplication of parasites within the cells of the monocytic phagocytic system of the vertebrate hosts (Desjeux, 2004; WHO, 2010).
The transmission of parasites between their numerous hosts, and, accidently, to humans, is made during the hematophagy of different species of dipterans belonging to the Psychodidae family, subfamily Phlebotominae (Killick-Kendrick et al., 1991; Brandão-Filho, 2004). Akhoundi et al. (2016) in an historical overview proposed an updated list of possible and proven sandfly vectors for each Leishmania species in the Old and New World. These dipterans have been recorded in natural ecosystem and in rural and urban environments close to domestic animals and human habitations (Barata et al., 2004).
The emergence of new cases of leishmaniasis is strongly influenced by environmental, demographic, and human behavioral factors and is associated with changes in the habitat of vectors and natural hosts, which contributes to changes in the disease's eco-epidemiological profile (Gramiccia and Gradoni, 2005; Brasil, 2017). Moreover, the participation of several species of wild and domestic mammals and vector sandflies increases the eco-epidemiological complexity observed in this parasitosis, making it difficult to control due to the different epidemiological patterns observed in each transmission focus. The lack of knowledge about these aspects further aggravates the situation (Ferreira et al., 2010).
Bats are known to be hosts and possible reservoirs of various pathogens (Brown, 2003; Correa et al., 2013; Lei and Olival, 2014; Ferreira et al., 2017). The order Chiroptera has the second largest number of species, is characterized by high mobility, and is present in several environments, including urban and peri-urban environments (Nowak, 1991; Simmons, 2005). These factors may increase the risk of Leishmania spp. transmission, since Chiroptera can act as pathogen hosts or reservoirs, thereby maintaining the protozoa in these different environments (Correa et al., 2013).
Leishmaniasis is an endemic and particularly important public health problem in Mato Grosso do Sul, Brazil (Nunes et al., 1995; Dorval et al., 2006; Reis et al., 2017; Castro et al., 2018; Mato Grosso do Sul, 2019). However, Leishmania spp. infection in bats has been subject to minimal investigation. Thus, the general importance of bats as reservoirs of Leishmania remains unknown. Therefore, the purpose of this study was to evaluate the occurrence of Leishmania spp. in bat populations inhabiting this region to obtain more knowledge about the participation of bats as hosts in endemic local for leishmaniasis as Mato Grosso do Sul.
2. Material and methods
2.1. Bat samples
The bats analyzed in this study were donated by the State Agency for Animal and Plant Health Defense (IAGRO/State Secretaria of Mato Grosso do Sul). These specimens were frozen at −20 °C. At the time of processing of the biological material, the bats were classified according South American bat identification taxonomic key by Díaz et al. (2016), and the tissues of interest in the research (liver and skin) were duly identified and separated using a separate sterile scalpel for each tissue. These samples were frozen at −70 °C until were analyzed using molecular techniques.
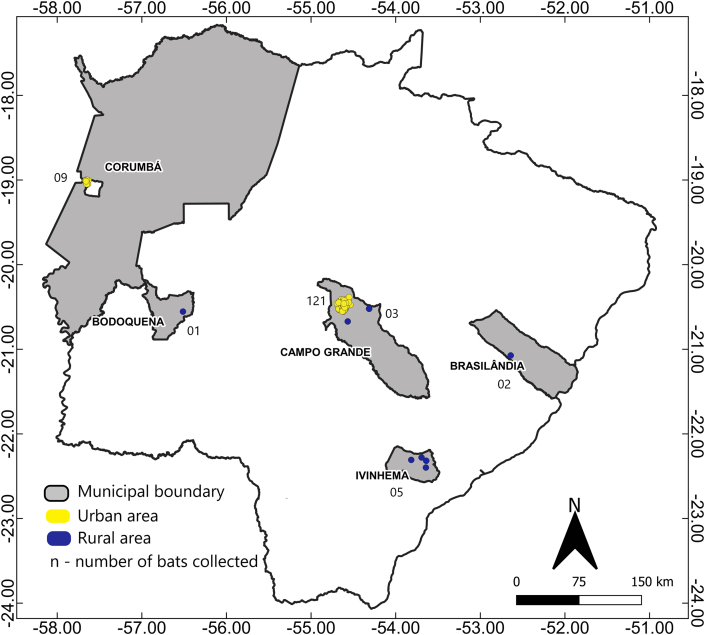
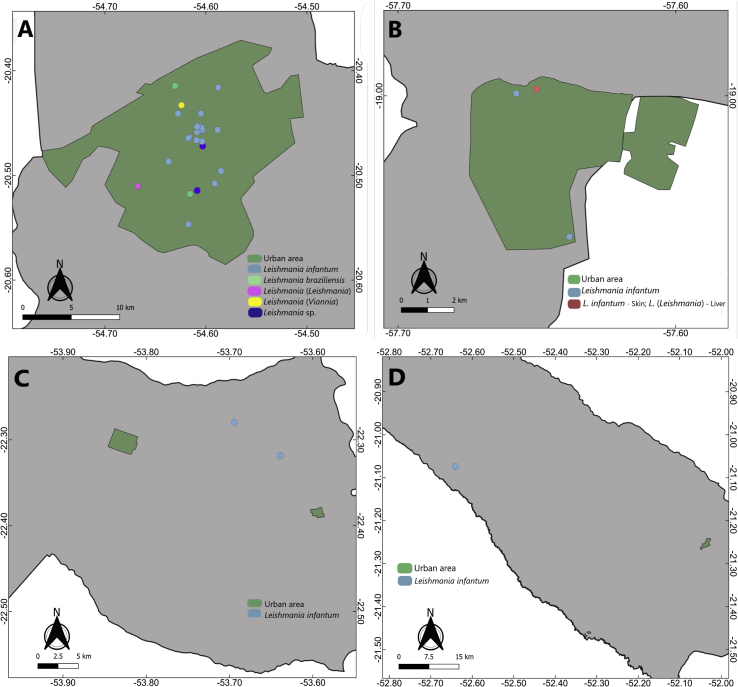
One hundred and forty-six bats, collected in urban and rural areas in and surrounding five different cities in the state of Mato Grosso do Sul, Brazil, were used in this study. The majority of the animals had been collected in the municipality of Campo Grande (n = 124), largely in urban areas (n = 121) (Fig. 1).
Fig. 1.
Bat collection sites in the state of Mato Grosso do Sul, Brazil.
Note: was not possible to trace the collection information in five animals.
2.2. Molecular tests
2.2.1. DNA extraction
Approximately 10 mg of bat tissues were separated and transferred to a sterile 1.5 mL microtube. Subsequently, they were subjected to DNA extraction using a commercial kit (Promega Wizard® Genomic DNA Purification), following the manufacturer's instructions.
2.2.2. IRBP- PCR
IRBP-PCR was performed as a pre-diagnostic step to evaluate DNA quality for further testing for the presence of Leishmania spp. The PCR reaction was performed using 5 μl of target DNA, PCR buffer, 1.5 mM MgCl2, 200 μM dNTP mix, 0.7U Taq DNA polymerase, and 15 pmol of each primer: IRBPfwd: (5′-TCCAACACCACCACTGAGATCTGGAC-3′) and IRBPrev: (5′-GTGAGGAAGAAATCGGACTGGCC-3′), flanking a 227 bp region. IRBP gene amplification followed the following conditions: denaturation at 95 °C for 4 min, followed by 35 cycles at 94 °C for 30 s, 57 °C for 30 s, 72 °C for 1 min and then a final extension step at 72 °C for 5 min (Ferreira et al., 2010).
2.2.3. kDNA- PCR
The samples that were positive for the IRBP gene were submitted to the PCR amplifications of the variable region of the kinetoplastid DNA (kDNA) minicircle molecules to screen for the detection of Leishmania spp. The reactions were carried out using the specific primers A: 5′(C/G)(C/G)(G/C) CC(C/A) CTA T(T/A)T TAC ACC AAC CCC 3′ and kDNA B: 5′ GGG GAG GGG CGT TCT GCG AA 3′, generating a fragment of 120bp (Silva et al., 2004).
The PCR reaction was prepared to a final volume of 25 μL using 5 μL of DNA template, 1.5 mM MgCl2, 200 μM dNTP mix, 3.5U Taq DNA polymerase, and 10 pmol of each primer. The reaction for kDNA gene amplification was based on the following conditions: denaturation at 94 °C for 4 min followed by 35 cycles at 94 °C for 30 s, 60 °C for 30 s, 72 °C for 30 s, and then a final extension step at 72 °C for 5 min.
In all reactions, the DNA of the reference strains Leishmania braziliensis (MHOM/BR/75/M2903), Leishmania infantum (MHOM/BR/74/PP75), and Leishmania amazonensis (IFLA/BR/67/PH8) was used as a positive control. For the negative control, 5 μL of ultra-pure water, DNAse, and RNAse free was added to a mix containing the reagents without DNA.
2.2.4. Nested PCR
Nested PCR for the gene small subunit ribosomal ribonucleic acid (SSUrRNA), LnPCR, was performed for the confirmation of the positive indicated by kDNA-PCR.
The first-stage PCR used the forward primer R221 (5′ GGT TCC TTT CCT GAT TTA CG 3′) with the reverse primer R332 (5′ GGC CGG TAA AGG CCG AAT AG 3′). For the first amplification, 10 μL of DNA solution were added to 40 μL of PCR mix containing 3 mM MgCl2, 200 μM dNTPs, 7.0U Taq DNA polymerase, and 10 pmol of each primer, generating a fragment of 603bp. The cycling conditions were 94 °C for 5 min followed by 30 cycles at 94 °C for 30 s, 60 °C for 30 s, and extension at 72 °C for 30 s, followed by a final extension at 72 °C for 10 min (Cruz et al., 2002).
The second amplification consisted of the reamplification of the previous SSU rRNA PCR product. Thus, 10 μL of 1/40 dilution of the first PCR product were added to 25 μL of PCR mix containing 3 mM MgCl2, 200 μM dNTPs, 7.0U Taq DNA polymerase, and 10 pmol of the Leishmania-specific primers R223 (5′ TCC CAT CGC AAC CTC GGT T 3′) and R333 (5′ AAA GCG GGC GCG GTG CTG 3’), generating a fragment of 350bp. The cycling conditions were 94 °C for 4 min followed by 30 cycles at 94 °C for 30 s, 65 °C for 30 s, and extension at 72 °C for 30 s, followed by a final extension at 72 °C for 10 min (Cruz et al., 2002).
2.2.5. Electrophoresis
The results were visualized on 2.0% agarose gel in 1x TBE buffer (tris base, boric acid and EDTA) in the presence of SYBR® Safe DNA gel stain (Invitrogen, Waltham, EUA) and examined on blue light exposure with a molecular weight marker of 100 bp.
2.2.6. Sequencing
All LnPCR-SSUrRNA PCR positive products were excised from the gel and purified using the PureLink® Quick Gel Extraction Kit (Invitrogen, Waltham, EUA) following the protocol provided by the manufacturer. Direct sequencing of the purified SSUrRNA positive products was performed with forward and reverse primers using the Big-Dye Terminator v3.1 Cycle Sequencing Kit and the automated ABI 3730 DNA Analyser (Applied Biosystems®, Foster City, EUA). Sequences obtained were analyzed and edited using the BioEdit Sequence Alignment Editor. The edited sequences were deposited at GenBank and compared to the others deposited by the BLAST tool.
2.2.7. Statistical analyses
To compare positivity ratios, 95% confidence intervals (CIs) were calculated using the Wald method. A chi-square test was used to verify statistical association between variables. The statistical analysis was performed using Stata software, version 11.
3. Results
We were able to identify 127/146 (87%) bats to the species level, representing 16 different species of bats. For 19 bats (13%), it was only possible to reach identification at the family level because the specimens were in an advanced state of decomposition. Skin samples were obtained from 100% (n = 146) of the bats, whereas liver samples were obtained from 87% (n = 127) of the specimens, because in 13% (n = 19) of them it was not possible to observe fundamental characteristics for organ identification or collection due to the animals’ advanced states of decomposition.
From the molecular tests and electrophoresis, it was possible to verify that 242 (89.3%) of the samples were positive for the IRBP target, of which 125 were skin samples and 117 were liver samples, were all the liver samples derive from bats included in the skin samples.
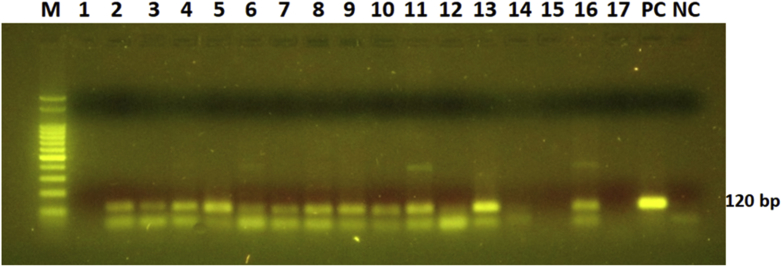
Only the samples that were positive for the IRBP target were submitted for kDNA PCR (n = 242). Leishmania spp. kDNA amplification by PCR was observed in 28.9% (70/242) of the total bat samples. Of the 125 skin samples positive for the IRBP target, six [4.8%; CI (95%) = 1.05%–8.5%] were positive for kDNA, and, of the 117 liver samples positive for IRBP, 64 [54.7%; CI (95%) = 45.7%–63.7%] were positive for kDNA (e.g., Fig. 2).
Fig. 2.
Agarose gel demonstrating kDNA PCR products (120bp). M: 100bp marker. 1–17: analyzed samples, of which 2–11, 13 and 16 were considered positive. PC: positive control of Leishmania spp., NC: negative control.
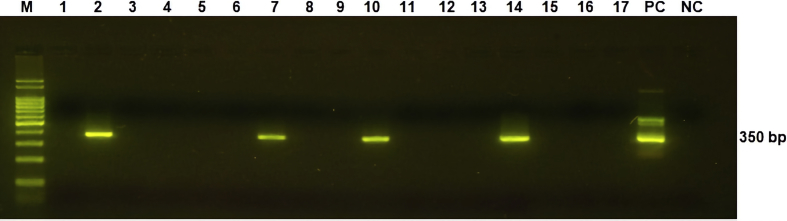
Subsequently, samples positive for the kDNA target were submitted to the nested-PCR for the gene SSU rRNA (LnPCR). Representative positive samples are shown in Fig. 3.
Fig. 3.
Agarose gel demonstrating LnPCR products (350bp). M: 100bp marker, 1–17: analyzed samples, of which 2, 7, 10 and 14 were considered positive. PC: positive control of Leishmania spp., NC: negative control.
The presence of Leishmania was confirmed via both techniques in 4 [3.2%; CI (95%) = 0.1%–6.3%] skin samples (n = 125) and 29 [24.8%; CI (95%) = 17.0%–32.6%] liver samples (n = 117) (Table 1). Significantly more liver samples were positive compared to skin samples (p < 0.001).
Table 1.
Results from PCR testing of skin and liver of bats, collected in and around five cities in the state of Mato Grosso do Sul (2019), for Leishmania using the kDNA and SSUrRNA targets.
| Family | Species | kDNA - Skin positive/n | SSUrRNA – Skin positive/n | kDNA – Liver positive/n | SSUrRNA – Liver positive/n |
|---|---|---|---|---|---|
| Phyllostomidae | Artibeus planirostris | 0/0 | – | 0/1 | – |
| Desmodus rotundus | 0/3 | – | 3/6 | 3/3 | |
| Glossophaga soricina | 0/0 | – | 1/1 | 1/1 | |
|
Lonchophylla thomasi |
0/1 |
– |
1/1 |
0/1 |
|
|
Total per Family |
0/4 |
– |
5/9 |
4/5 |
|
| Vespertilionidae | Eptesicus furinalis | 0/2 | – | 0/1 | – |
| Lasiurus blossevillii | 0/1 | – | 0/0 | – | |
| Lasiurus cinereus | 0/2 | – | 4/5 | 2/4 | |
| Myotis nigricans | 0/2 | – | 2/3 | 1/2 | |
| Unidentified species |
0/8 |
– |
1/3 |
0/1 |
|
|
Total per Family |
0/15 |
– |
7/12 |
3/7 |
|
| Molossidae | Cynomops planirostris | 0/9 | – | 5/7 | 1/5 |
| Eumops glaucinus | 0/4 | – | 1/4 | 0/1 | |
| Molossus molossus | 1/27 | 0/1 | 13/27 | 4/13 | |
| Molossus pretiosus | 2/19 | 2a/2 | 13/18 | 3a/13 | |
| Molossus rufus | 0/10 | – | 4/8 | 2/4 | |
| Nyctinomops laticaudatus | 2/10 | 2/2 | 3/10 | 2/3 | |
| Nyctinomops macrotis | 0/15 | – | 10/13 | 9/10 | |
| Promops centralis | 1/3 | 0/1 | 2/3 | 0/2 | |
| Unidentified species |
0/9 |
– |
1/6 |
1/1 |
|
| Total per Family | 6/106 | 4/6 | 52/96 | 22/52 | |
| TOTAL | 6/125 (4.8%) | 4/6 (66.7%) | 64/117 (54.7%) | 29/64 (45.3%) |
One bat presented Leishmania DNA presence in both liver and skin.
In terms of the bat collection locations, in Campo Grande, where the highest number of bats were collected, bats from the central and peripheral regions of the city were positive for the kDNA target whereas positivity for LnPCR was more concentrated in the central region, with some points on the periphery of the city. In the city of Corumbá, all animals were collected in urban areas, and bats that resulted in positive samples using both techniques were observed in the peripheral regions of the city. In Brasilândia and Ivinhema, all animals were collected in rural areas. The bat collected in the city of Bodoquena was considered negative for Leishmania.
Thus, 33 samples belonging to 32 different bats (one animal had positivity in the skin and the liver) were confirmed as positive. They were submitted to the sequencing technique to identify the Leishmania species involved.
After analysis of the sequences according to the scores obtained in the BLAST (supplementary material), it was possible to determine the species of Leishmania involved in 28 of the samples [84.8%; CI (95%) = 72.6%–97.1%]. Two of these samples (6.1%) were identified as having Leishmania braziliensis. The other 26 samples (78.8%) were confirmed as having Leishmania infantum. In 3 of them [9.1%; CI (95%) = 0%–18.9%], it was possible to conclude to the subgenus level, and 2 of them [6.1%; CI (95%) = 0%–14.2%] were categorized as only belonging to the genus Leishmania (Table 2). The sequences were deposited in GenBank, with accession numbers: MN852406 to MN852438.
Table 2.
Family and species of bats in relation to species of Leishmania found, in addition to the feeding habits and percentage of positive animals per species, Mato Grosso do Sul (2019).
| Family | Bat Species (n) | Feeding habit |
Positive |
Leishmania identification | Tissue | |
|---|---|---|---|---|---|---|
| n | (%) | |||||
| Phyllostomidae | Desmodus rotundus (6) | Hematophagous | 3 | (50%) | L. infantum | Liver |
| Glossophaga soricina (1) | Nectarivorous | 1 | (100%) | L. infantum | Liver | |
| Vespertilionidae | Lasiurus cinereus (5) | Insectivorous | 1 | (40%) | L. braziliensis | Liver |
| 1 | Leishmania (Viannia) sp. | Liver | ||||
| Myotis nigricans (3) | Insectivorous | 1 | (33,3%) | L. infantum | Liver | |
| Molossidae | Cynomops planirostris (9) | Insectivorous | 1 | (11,1%) | L. braziliensis | Liver |
| Molossus molossus (27) | Insectivorous | 2 | (14,8%) | L. infantum | Liver | |
| 1 | Leishmania (Leishmania) sp. | Liver | ||||
| 1 | Leishmania sp. | Liver | ||||
| Molossus pretiosus (19) | Insectivorous | 2 | (26,3%) | L. infantum | Liver | |
| 2a | L. infantum | Skin | ||||
| 1a | Leishmania (Leishmania) sp. | Liver | ||||
| Molossus rufus (10) | Insectivorous | 2 | (20%) | L. infantum | Liver | |
| Nyctinomops laticaudatus (10) | Insectivorous | 2 | (40%) | L. infantum | Liver | |
| 2 | L. infantum | Skin | ||||
| Nyctinomops macrotis (15) | Insectivorous | 8 | (60%) | L. infantum | Liver | |
| 1 | Leishmania sp. | Liver | ||||
| Molossidaeb (9) | - | 1 | (11,1%) | L. infantum | Liver | |
Tissues of the same bat - L. infantum in the skin and L. (Leishmania) in the liver.
Species of bat not identified.
Fig. 4 shows the species of Leishmania identified according to the bat collection location. In Campo Grande there were different points of positivity for L. infantum, with 20 animals identified with this Leishmania specie from 26 positives [76.9%; CI (95%) = 60.7%–93.1%]. In Corumbá, Ivinhema and Brasilândia this same species was identified in positive animals, in both urban and rural areas.
Fig. 4.
Identification of Leishmania according to site of collect of the bats per city, Mato Grosso do Sul, Brazil; Grey area - municipal boundary; A – Campo Grande; B – Corumbá; C – Ivinhema; D – Brasilândia.
4. Discussion
Leishmaniasis is present in the State of Mato Grosso do Sul in very significant numbers. Further, it is expanding and has widespread distribution and record in all municipalities, even with the implementation of control measures, such as the euthanizing of thousands of L. infantum seropositive dogs. It is clear that the existing control measures are not effective (Cunha et al., 2014). Therefore, there is the distinct possibility of the participation of other mammalian (wild or domestic) as possible reservoirs of the parasite in the transmission cycle of leishmaniasis in this area.
Of the total bat samples, Leishmania spp. kDNA amplification by PCR was observed in 28.9% (70/242). These results were similar to research conducted in the state of São Paulo, which found 23.9% (117/488) positivity in bat skin and spleen samples using qPCR for the same target (Oliveira et al., 2015).
This infection is considered an anthropozoonosis, in which more than 100 mammal species have been naturally infected with the parasites (Forattini et al., 1972; De Lima et al., 2002; Brandão-Filho et al., 2003; Ferreira et al., 2010, 2015; Roque and Jansen, 2014). Among them, bats have emerged as one of the most important supposed reservoirs of certain Leishmania species (Gómez-Hernández et al., 2017). The ability of bats to disperse and their longevity could facilitate the maintenance and dispersal of Leishmania, with considerable impacts on disease prevention and control measures (Lampo et al., 2000; Savani et al., 2010).
After the execution of the LnPCR, we observed positivity via both techniques for Leishmania in 33 samples from bats, of which, it was possible to determine the species of Leishmania involved in 28 of the samples. We detected the presence of Leishmania infantum in 26 samples (78.8%) and Leishmania braziliensis in two samples (6.1%). These two species are the most prevalent species in human cases of visceral and cutaneous leishmaniasis, respectively, in the Brazilian Midwest.
Some species of bats reported as being infected in the present study (Molossus molossus, Molossus rufus, Myotis nigricans, Nyctinomops laticaudatus, Desmodus rotundus, and Glossophaga soricina) have been similarly documented in studies carried out in Latin America, especially in Brazil, that recorded the occurrence of bats infected with L. infantum (De Lima et al., 2008; Oliveira et al., 2015; Gómez-Hernández et al., 2017; Rezende et al., 2017), L. amazonensis (Savani et al., 2010; Oliveira et al., 2015; Gómez-Hernández et al., 2017), and L. braziliensis (Shapiro et al., 2013; Ferreira et al., 2017; Gómez-Hernández et al., 2017).
In this study, we report for the first time bats especies like Molossus pretiosus, Myotis nigricans, Nyctinomops laticaudatus and Nyctinomops macrotis as possible hosts for L. infantum. For L. braziliensis, the species Lasiurus cinereus and Cynomops planirostris could be reported as possible hosts in the studied areas. These encounters demonstrate that bats could be contributing to maintaining Leishmania spp. in endemic areas.
In the cities of Campo Grande and Corumbá there were different points of positivity within the urban areas, scenario of occurrence of visceral leishmaniasis transmission, which corroborates with prior research that detected also Leishmania DNA presence in bats in urban areas (Oliveira et al., 2015; Rezende et al., 2017). On the other hand, it was also possible to detect Leishmania in rural areas, specifically in the cities of Ivinhema and Brasilândia, areas already been reported with of positive bats in other studies (Savani et al., 2010; Gómez-Hernández et al., 2017).
Leishmania infantum was the most widely identified species, both in rural and urban areas, this specie has already been identified from bats in other studies in Brazil, in different regions (Oliveira et al., 2015; Gómez-Hernández et al., 2017; Rezende et al., 2017). Moreover, higher prevalence identification of L. infantum in Campo Grande (76.9%) and Corumbá (100%) was expected, precisely because this species is responsible for the visceral manifestation, that is endemic in these cities (Botelho and Natal, 2009; Mato Grosso Do Sul, 2019). In this sense, although dogs are the main reservoir for humans, some wild species, such as bats, could be contributing to the maintenance of Leishmania spp. in these localities (Rezende et al., 2017). This could explain why traditional control measures do not appear to be efficient (Cunha et al., 2014).
Leishmania braziliensis, a species involved in cutaneous and mucosal leishmaniasis, was identified in an urban area of Campo Grande. This demonstrates that, although this species is involved in a pattern of rural and forest-area transmission, it may eventually circulate in cities, especially given bats’ characteristic dispersion patterns. Moreover, to the best of our knowledge, the encounters of Leishmania in the species Molossus pretiosus, Nyctinomops macrotis, and Lasiurus cinereus are the first reports of Leishmania in these bat species in Brazil.
These findings of infected bats in areas endemic for leishmaniasis indicate that these animals may be participating in the maintenance of the disease cycle in these places. However, to validate the true role of these animals in the maintenance of leishmaniasis, further investigation is necessary. A reservoir for Leishmania spp. is required to ensure the subsistence and transmission of the parasite, and extensive ecological studies are needed to define such a reservoir (Berzunza-Cruz et al., 2015). However, bats as possible reservoirs of the causative agents of leishmaniasis should not be disregarded.
Regarding samples, we detected Leishmania more often in liver versus skin samples, with statistical difference (p < 0.001). This difference should be better investigated to establish more clearly how the parasite behaves in this possible host. However, the lower presence of Leishmania DNA in the skin may suggest that bats are not the best source of infection for sandflies.
According to Shaw (2007), only when a better understanding of the genetic diversity of Leishmania species and the reservoirs involved in the enzootic cycle of each species is obtained will it be possible to evaluate what methods of control are most effective. It is important to carry out complementary surveys on all aspects involved in reservoir determination to propose more aggressive measures for prevention and control of the infection (De Lima et al., 2008; Savani et al., 2010; Shapiro et al., 2013; Roque and Jansen, 2014; Berzunza-Cruz et al., 2015; Ferreira et al., 2017).
Considerations
The use of animal samples donated by the IAGRO/MS, local service of the animal health, reinforces the importance of implementing sustainable projects, as it was not necessary to collect other animals exclusively for the development of this research.
Declaration of competing interest
None.
Acknowledgements
The authors would like to thank Agência Estadual de Defesa Sanitária Animal e Vegetal (IAGRO/MS), Universidade Anhanguera-UNIDERP and UFMS (Universidade Federal de Mato Grosso do Sul) for general research support. CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico), Fundect (Fundação de Apoio ao Desenvolvimento do Ensino, Ciência e Tecnologia do Estado de Mato Grosso do Sul) and Institutional Program for the Induction of Science, Technology and Innovation in Health - Generation and Diffusion of Knowledge of Excellence - Young Scientist - Fundação Oswaldo Cruz (PAPESVII/ Fiocruz) for financial support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijppaw.2020.02.008.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Akhoundi M., Kuhls K., Cannet A., Votýpka J., Marty P., Delaunay P., Sereno D. A historical overview of the classification, evolution, and dispersion of Leishmania parasites and sandflies. PLOS neglect. Trop. Doct. 2016;10(3):43–49. doi: 10.1371/journal.pntd.0004349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barata R.A., França-Silva J.C., Costa R.T., Fortes-Dias C.L., Silva J.C., Paula E.V., Prata A., MonteiroI E.M., Dias E.S. Phlebotomine sand flies in Porteirinha, an area of American visceral leishmaniasis transmission in the state of Minas Gerais, Brazil. Mem. Inst. Oswaldo Cruz. 2004;99:481–487. doi: 10.1590/s0074-02762004000500004. [DOI] [PubMed] [Google Scholar]
- Berzunza-Cruz M., Rodriguez-Moreno A., Gutiérrez-Granados G., González-Salazar C., Stephes C.R., Hidalgo-Mihart M., Marina C.F., Rebollar-Téllez E.A., Bailón- Martinez D., Balcells C.D., Ibarra-Cerdeña C.N., Sánchez-Cordero V., Becker I. Leishmania (L.) Mexicana infected bats in Mexico: novel potential reservoirs. PLoS Neglected Trop. Dis. 2015;9:1–15. doi: 10.1371/journal.pntd.0003438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botelho A.C., Natal D. First epidemiological description of visceral leishmaniasis in Campo Grande, state of Mato Grosso do Sul. Rev. Soc. Bras. Med. Trop. 2009;42:503–508. doi: 10.1590/s0037-86822009000500006. [DOI] [PubMed] [Google Scholar]
- Brandão-Filho S.P. Flebotomíneos do Brasil. Cad. Saúde Pública. 2004;20:1436–1437. [Google Scholar]
- Brandão-Filho S.P., Brito M.E., Carvalho F.G., Ishikawa E.A., Cupolillo E., Floeter-Winter L., Shaw J.J. Wild and synanthropic hosts of Leishmania (Viannia) braziliensis in the endemic cutaneous leishmaniasis locality of Amaraji, Pernambuco State, Brazil. Trans. R. Soc. Trop. Med. Hyg. 2003;97:291–296. doi: 10.1016/s0035-9203(03)90146-5. [DOI] [PubMed] [Google Scholar]
- Brasil . 2014. Ministério da Saúde (MS). Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Manual de vigilância e controle da leishmaniose visceral. Brasília. [Google Scholar]
- Brasil . 2017. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância das Doenças Transmissíveis. Manual de vigilância da leishmaniose tegumentar. (Brasília) [Google Scholar]
- Brown C. Virchow revisited: emerging zoonoses. ASM News. 2003;69:493–497. [Google Scholar]
- Castro L.S., França A.O., Ferreira E.C., Lima-Junior M.S.C., Gontijo C., Pereira A.A.S., Dorval M.E.C. Characterization of Leishmania species from central-west region of Brazil. Parasitol. Res. 2018;117:1839–1845. doi: 10.1007/s00436-018-5871-1. [DOI] [PubMed] [Google Scholar]
- Correa M.M.O., Lazar A., Dias D., Bonvicino C.R. Quirópteros hospedeiros de Zoonoses no Brasil. Bol. Soc. Bras. Mastozool. 2013;67:23–38. [Google Scholar]
- Cruz I., Cañavate C., Rubio J.M., Morales M.A., Chicharro C., Laguna F., Jiménez-Mejías M., Sirera G., Videla S., Alvar J. A nested polymerase chain reaction (Ln-PCR) for diagnosing and monitoring Leishmania infantum infection in patients co-infected with human immunodeficiency virus. Trans. R. Soc. Trop. Med. Hyg. 2002;96:185–189. doi: 10.1016/s0035-9203(02)90074-x. [DOI] [PubMed] [Google Scholar]
- Cunha R.C., Andreotti R., Cominetti M.C., Silva E.A. Detection of Leishmania infantum in Lutzomyia longipalpis captured in Campo Grande, MS. Rev. Bras. Parasitol. Vet. 2014;23:269–273. doi: 10.1590/s1984-29612014049. [DOI] [PubMed] [Google Scholar]
- De Lima H., De Guglielmo Z., Rodríguez A., Convit J., Rodriguez N. Cotton rats (Sigmodon hispidus) and black rats (Rattus rattus) as possible reservoirs of Leishmania spp. in Lara state, Venezuela. Mem. Inst. Oswaldo Cruz. 2002;97:169–174. doi: 10.1590/s0074-02762002000200004. [DOI] [PubMed] [Google Scholar]
- De Lima H., Rodríguez N., Barrios M.A., Ávila A., Cañizales I., Gutiérrez S. Isolation and molecular identification of Leishmania chagasi from a bat (Carollia perspicillata) in northeastern Venezuela. Mem. Inst. Oswaldo Cruz. 2008;103:412–414. doi: 10.1590/s0074-02762008000400018. [DOI] [PubMed] [Google Scholar]
- Desjeux P. Leishmaniasis: current situation and new perspectives. Comp. Immunol. Microbiol. Infect. Dis. 2004;27:305–318. doi: 10.1016/j.cimid.2004.03.004. [DOI] [PubMed] [Google Scholar]
- Díaz M.M., Solari S., Aguirre L.F., Aguiar L.M.S., Barquez R.M. 2016. Clave de identificación de los murciélagosde Sudamérica. Publicación Especial N° 2, PCMA (Programa deConservación de los Murciélagos de Argentina) p. 160. [Google Scholar]
- Dorval M.E.C., Oshiro E.T., Cupolillo E., Castro A.C.C., Alves T. Ocorrência de leishmaniose tegumentar americana no Estado Mato Grosso do Sul associada à infecção por Leishmania (Leishmania) amazonensis. Rev. Soc. Bras. Med. Trop. 2006;39:43–46. doi: 10.1590/s0037-86822006000100008. [DOI] [PubMed] [Google Scholar]
- Ferreira E., Cruz I., Cañavate C., De Melo L.A., Pereira A.A., Madeira F.A., Gontijo C.M. Mixed infection of Leishmania infantum and Leishmania braziliensis in rodents from endemic urban area of the New World. BMC Vet. Res. 2015;11:71–78. doi: 10.1186/s12917-015-0392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira E.C., Gontijo C.M., Cruz I., Melo M.N., Silva A.M. Alternative PCR protocol using a single primer set for assessing DNA quality in several tissues from a large variety of mammalian species living in areas endemic for leishmaniasis. Mem. Inst. Oswaldo Cruz. 2010;105:895–898. doi: 10.1590/s0074-02762010000700009. [DOI] [PubMed] [Google Scholar]
- Ferreira E.C., Pereira A., Silveira M., Margonari C., Marcon G.E.B., França A., Castro L.S., Bordignon M., Fischer E., Tomas W., Dorval M.E.C., Gontijo C. Leishmania (V.) braziliensis infecting bats from Pantanal wetland, Brazil: first records for Platyrrhinus lineatus and Artibeus planirostris. Acta Trop. 2017;172:217–222. doi: 10.1016/j.actatropica.2017.05.012. [DOI] [PubMed] [Google Scholar]
- Forattini O.P., Pattoli D.B.G., Rabello E.X., Ferreira A.O. Infecções naturais de mamíferos silvestres em área endêmica de Leishmaniose tegumentar do estado de São Paulo. Brasil. Rev. Saúde Públ. 1972;6:255–261. [PubMed] [Google Scholar]
- Gómez-Hernández C., Bento E., Rezende-Oliveira K., Nascentes G., Barbosa C., Batista L., Ramirez L. Leishmania infection in bats from a non-endemic region of Leishmaniasis in Brazil. Parasitology. 2017;144:1980–1986. doi: 10.1017/S0031182017001500. [DOI] [PubMed] [Google Scholar]
- Gramiccia M., Gradoni L. The current status of zoonotic leishmaniases and approaches to disease control (Invited review) Int. J. Parasitol. 2005;35:1169–1180. doi: 10.1016/j.ijpara.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Killick-Kendrick R., Moroli M., Kiilick-Kendrick M. Bibliography on the colonization of Phlebotomine sandflies. Parassitologia. 1991;33:321–333. [PubMed] [Google Scholar]
- Lampo M., Feliciangeli M.D., Marquez L.M., Bastidas C., Lau P. A possible role of bats as a blood source for the Leishmania vector Lutzomyia longipalpis (Diptera: Psychodidae) Am. J. Trop. Med. Hyg. 2000;62:718–719. doi: 10.4269/ajtmh.2000.62.718. [DOI] [PubMed] [Google Scholar]
- Lei B.R., Olival K.J. Contrasting patterns in mammal–bacteria coevolution: bartonella and leptospira in bats and rodents. PLoS Neglected Trop. Dis. 2014;8:27–38. doi: 10.1371/journal.pntd.0002738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mato Grosso Do Sul . 2019. Informe Epidemiológico das Leishmanioses nº 1/2018 – Leishmaniose Visceral Mato Grosso do Sul, Semana Epidemiológica 1 a 52 de 2017. 2018. Governo do Estado de Mato Grosso do Sul. Secretaria de Saúde do Estado, Coordenadoria Estadual Controle de Vetores, Gerência Estadual de Zoonoses, Campo Grande, Brasil. [Google Scholar]
- Nowak R.M. 5 th. vol. 1. Johns Hopkins University Press; London, USA: 1991. p. 642. (Walker's Mammals of the World). [Google Scholar]
- Nunes V.L.B., Dorval M.E.C., Oshiro E.T., Noguchi R.C., Arão L.B., Hans Filho G., Espíndola M.A., Cristaldo G., Rocha H.C., Serafine L.N., Santos D. Estudo epidemiológico sobre Leishmaniose Tegumentar (LT) no município de Corguinho, Mato Grosso do Sul - estudos na população humana. Rev. Soc. Bras. Med. Trop. 1995;28:185–193. doi: 10.1590/s0037-86821995000300004. [DOI] [PubMed] [Google Scholar]
- Oliveira F.M., Costa L.C., Barros T.L., Katsuda Ito P.R.K., Colombo F., Carvalho C., Pedro W., Queiroz L., Nunes C. First detection of Leishmania spp. DNA in Brazilian bats captured strictly in urban areas. Acta Trop. 2015;150:176–181. doi: 10.1016/j.actatropica.2015.07.010. [DOI] [PubMed] [Google Scholar]
- OPAS - Organización Panamericana De La Salud . 2019. Manual de procedimientos para vigilancia y control de lãs leishmaniasis en las Américas. (Washington, D.C) [Google Scholar]
- Reis L.L., Balieiro A.A.S., Fonseca F.R., Gonçalves M.J.F. Changes in the epidemiology of visceral leishmaniasis in Brazil from 2001 to 2014. Rev. Soc. Bras. Med. Trop. 2017;50:638–645. doi: 10.1590/0037-8682-0243-2017. [DOI] [PubMed] [Google Scholar]
- Rezende M.B., Herrera H.M., Carvalho C.M.E., Carvalho Anjos E.A., Ramos C.A.N., Araújo F.R., Torres J.M., De Oliveira C.E. Detection of Leishmania spp. in bats from an area of Brazil endemic for visceral leishmaniasis. Transbound. Emerg. Dis. 2017;64:36–42. doi: 10.1111/tbed.12597. [DOI] [PubMed] [Google Scholar]
- Roque A.L.R., Jansen A.M. Wild and synanthropic reservoirs of Leishmania species in the Americas. Int J Parasitol Parasites Wildl. 2014;3:251–262. doi: 10.1016/j.ijppaw.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savani E.S.M., Almeida M.F., Camargo M.C.G.O., D'áuria S.R.N., Silva M.M.S., Oliveira M.L., Sacramento D. Detection of Leishmania (Leishmania) amazonensis and Leishmania (Leishmania) infantum chagasi in Brazilian bats. Vet. Parasitol. 2010;168:5–10. doi: 10.1016/j.vetpar.2009.10.019. [DOI] [PubMed] [Google Scholar]
- Shapiro J.T., Da Costa Lima Junior M.S., Dorval M.E., De Oliveira França A., Cepa Matos M.F., Bordignon M.O. First record of Leishmania braziliensis presence detected in bats, Mato Grosso do Sul, southwest Brazil. Acta Trop. 2013;128:171–174. doi: 10.1016/j.actatropica.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Shaw J.J. The leishmaniasis – survival and expansion in a changing world. A mini-review. Mem. Inst. Oswaldo Cruz. 2007;102:541–547. doi: 10.1590/s0074-02762007000500001. [DOI] [PubMed] [Google Scholar]
- Silva E.S., Gontijo C.M.F., Pacheco R.S., Brazil R.P. Diagnosis of human visceral leishmaniasis by PCR using blood samples spotted on filter paper. Genet. Mol. Res. 2004;3:251–257. [PubMed] [Google Scholar]
- Simmons N.B. Chiroptera. In: Wilson D.E., Reeder D.M., editors. Mammal Species of the World: a Taxonomic and Geographic Reference. Johns Hopkins University Press; Baltimore: 2005. p. 124. [Google Scholar]
- World Health Organization (WHO) WHO; Genebra: 2010. Expert Committee on the Control of Leishmaniasis. Control of the Leishmaniasis: Report of a Meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva, 22-26 March 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.