Abstract
Purpose
To report a case of bilateral serous retinal detachments in a patient found to have burkitt lymphoma.
Observations
A patient who presented with bilateral serous retinal detachments and “B” symptoms underwent extensive workup and was found to have burkitt lymphoma. Multiagent chemotherapy was initiated with resolution of the serous retinal detachments and visual recovery occurring in parallel to disease remission.
Conclusions and Importance
Burkitt lymphoma can present with serous retinal detachments and should be included in the differential for a patient with bilateral serous retinal detachments along with Vogt-Koyanagi-Harada syndrome.
Keywords: Lymphoma, Retina, Ocular manifestations of systemic diseases
1. Introduction
Burkitt Lymphoma (BL) is an aggressive B-cell non-Hodgkin lymphoma (NHL) caused by a rearrangement of the MYC oncogene leading to its overexpression and rapid cell division.1 Clinical features of BL include “B” symptoms and complications include tumor lysis syndrome and CNS relapse.1 Reported ocular manifestations of BL primarily involve infiltration of the orbital soft tissues resulting in chemosis, lid edema, tortuosity of retinal vessels, exophthalmos, corneal anesthesia, exposure keratopathy and optic neuropathy.2,3 This report describes a patient with bilateral serous retinal detachments (RD) found to have BL.
2. Case report
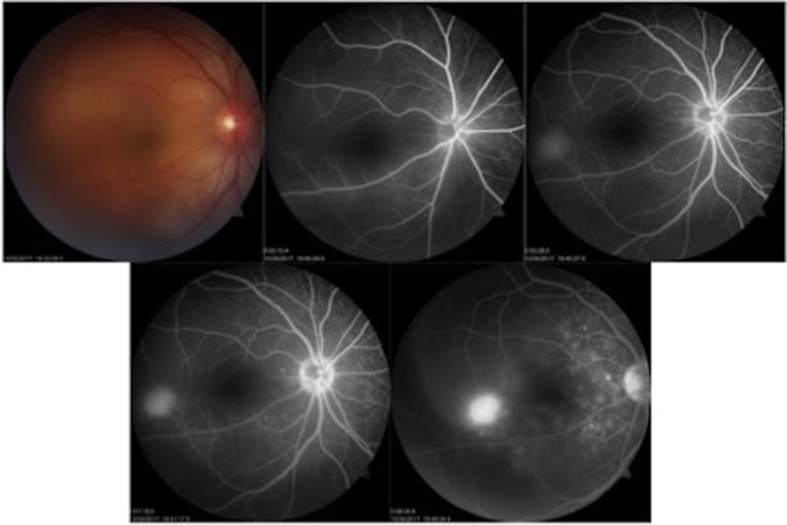
A 38-year-old male with no prior medical history presented with 1 week of subjective fever, myalgias and blurry vision in both eyes. Additionally, he endorsed profuse sweating, generalized body pain, decreased appetite, weight loss and inguinal lymphadenopathy. He denied cough, bloody sputum, diarrhea, urinary symptoms or rash. His best-corrected visual acuity (BCVA) was 20/800 in the right eye and 20/200 in the left. Pupils were round and reactive without an APD. Intraocular pressures and anterior segment exam were normal. Fundus examination was notable for serous retinal detachments involving the macula in both eyes. Optical coherence tomography confirmed the presence of subretinal fluid in both eyes (Fig. 1) and fluorescein angiography (FA) revealed multiple, punctate, hyperfluorescent areas of leakage at the level of the RPE (Fig. 2). He underwent an extensive infectious, inflammatory and neoplastic workup. CT abdomen revealed a 1cm axillary lymphadenopathy, hepatomegaly and peritoneal thickening with ascitic fluid. Laboratory workup was notable for elevated white blood cell count with lymphocytosis, low platelets, increased uric acid and LDH. EBV, HSV, Hepatitis B core Ab and quantiferon gold returned positive though CT chest did not reveal any evidence of active tuberculosis. Remaining laboratory workup returned negative including HIV RNA, monospot, Hep B surface Ag, HCV, Syphilis, ESR, RF, ANA, Lyme, ACE. Blood cultures were negative and lumbar puncture did not reveal malignant cells. Given his lymphocytosis the patient underwent a bone marrow biopsy confirming BL. Allopurinol and rasburicase were started as he was in tumor lysis syndrome. R-Hyper CVAD chemotherapy (Rituximab, cyclophosphamide, vincristine, Adriamycin and dexamethasone alternating with high dose methotrexate and cytarabine) was initiated for treatment of BL. Two weeks later his BCVA had improved to 20/100 and 20/50 respectively with improvement in his serous RDs. Four months later his BCVA had improved to 20/25 bilaterally with complete resolution of his serous RDs.
Fig. 1.
Optical coherence tomography of the right and left eyes demonstrating bilateral macular detachments.
Fig. 2.
Fundus photo of the right eye with large serous retinal detachment. FA of the right eye showing multiple, punctate, hyperfluorescent areas of leakage at the level of the RPE with an inferotemporal area of staining.
3. Discussion
The differential for bilateral serous RDs is broad and includes infectious, inflammatory, vascular and neoplastic etiologies.4 With respect to malignancy, bilateral serous RDs have previously been associated with both acute and chronic myeloid leukemia, acute lymphocytic leukemia, multiple myeloma and diffuse large B-cell lymphoma.2,4, 5, 6, 7, 8, 9 Additionally, one prior case of serous RD has been reported in a patient with BL, however this case was unilateral and occurred in a patient with HIV with extensive spread of malignancy including to the brain.2 In patients with serous RDs associated with malignancy, FA often demonstrates multiple, punctate, hyperfluorescent lesions at the level of the RPE, giving the appearance of a starry sky.2,5,6 The mechanism is not fully understood, however, it has been proposed that it is related to choroidal infiltration with subsequent ischemia and dysfunction of the retinal pigment epithelium.6 In this case, the initial differential included Vogt-Koyanagi-Harada syndrome, however, extensive workup was undertaken to look for an alternative underlying etiology given the patients additional symptoms. As with other systemic causes of serous RD, treatment consists of treating the underlying disease, with resolution of serous RDs and recovery of vision typically occurring in parallel to remission of the underlying disease as was seen in our case.
Patient consent
Written patient consent was obtained for publication of this case report.
Acknowledgements & disclosures
Funding
This research was funded by grants from Lewis Henkind and the Estate of Irving and Branna Sisenwein.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures related to the presented work: MW, JF, SR.
Acknowledgements
None.
Contributor Information
Matthew S. Wieder, Email: mawieder@montefiore.org.
Jay A. Fleischman, Email: retsurg@gmail.com.
Saadia Rashid, Email: srashid@montefiore.org.
References
- 1.Casulo C., Friedberg J.W. Burkitt lymphoma- a rare but challenging lymphoma. Best Pract Res Clin Haematol. 2018;31:279–284. doi: 10.1016/j.beha.2018.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Andreoli C.M., Husain D., Davis T.S., Loewenstein J.I. Chorioretinal changes heralding metastatic malignancy. Arch Ophthalmol. 2006;124:1790–1792. doi: 10.1001/archopht.124.12.1790. [DOI] [PubMed] [Google Scholar]
- 3.Payne T., Karp L.A., Zimmerman L.E. Intraocular involvement in Burkitt's lymphoma. Arch Ophthalmol. 1971;85:295–298. doi: 10.1001/archopht.1971.00990050297009. [DOI] [PubMed] [Google Scholar]
- 4.Wolfensberger T.J., Tufail A. Systemic disorders associated with detachment of the neurosensory retina and retinal pigment epithelium. Curr Opin Ophthalmol. 2000;11:455–461. doi: 10.1097/00055735-200012000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Fackler T.K., Bearelly S., Odom T., Fekrat S., Cooney M.J. Acute lymphoblastic leukemia presenting as bilateral serous macular detachments. Retina. 2006;26:710–712. doi: 10.1097/01.iae.0000236484.24808.bb. [DOI] [PubMed] [Google Scholar]
- 6.Moussa K., Bradbury M., Wu D.M. Middle-aged man with bilateral subretinal fluid. JAMA Ophthalmol. 2018 doi: 10.1001/jamaophthalmol.2018.2759. [DOI] [PubMed] [Google Scholar]
- 7.Reche-Sainz J.A., Peral-Ortiz de la Torre M.J., Carpio-Bailen R., Toledano-Fernandez N. [Diffuse large B cell lymphoma presenting with a bilateral serous macular detachment] Arch Soc Esp Oftalmol. 2007;82:559–562. doi: 10.4321/s0365-66912007000900009. [DOI] [PubMed] [Google Scholar]
- 8.Kishimoto T., Fukuda K., Nishiuchi T., Hayashi N., Fukushima A. Unilateral serous retinal detachment with choroidal thickening as a first presenting sign of acute myeloid leukemia. Am J Ophthalmol Case Rep. 2019;14:51–54. doi: 10.1016/j.ajoc.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mistry S., Sudharshan S., Ganesan S., Akbar A.B., Biswas J. Vogt-Koyanagi-Harada disease like presentation in patients with chronic myeloid leukemia. Am J Ophthalmol Case Rep. 2018;10:221–225. doi: 10.1016/j.ajoc.2018.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]