Abstract
Global surgery is an essential component of Universal Health Coverage. Surgical conditions account for almost one-third of the global burden of disease, with the majority of patients living in low-income and middle-income countries (LMICs). Children account for more than half of the global population; however, in many LMIC settings they have poor access to surgical care due to a lack of workforce and health system infrastructure to match the need for children’s surgery. Surgical providers from high-income countries volunteer to visit LMICs and partner with the local providers to deliver surgical care and trainings to improve outcomes. However, some of these altruistic efforts fail. We aim to share our experience on developing, implementing and sustaining a partnership in global children’s surgery in Tanzania. The use of participatory methods facilitated a successful 17-yearlong partnership, ensured a non-hierarchical environment and encouraged an understanding of the context, local needs, available resources and hospital capacity, including budget constraints, when codesigning solutions. We believe that participatory approaches are feasible and valuable in developing, implementing and sustaining global partnerships for children’s surgery in LMICs.
Keywords: child health, paediatrics, health policy, surgery
Summary box.
Children account for more than half of the global population, and provision of children’s surgical care is critical for ensuring Universal Health Coverage (UHC).
A number of global surgery partnerships between high-income and low-income countries may fail due to complex ethical, cultural and financial challenges, and poor planning.
Use of participatory approaches have the potential of enhancing sustainable partnerships, through facilitating a non-hierarchical environment, promoting mutual trust, and shared values of cultural humility and reciprocity.
Surgical health systems strengthening through interdisciplinary and holistic workforce development; medical student training; and research capacity building, are important strategies for improving quality of care in children’s surgery.
Introduction
Neglected surgical conditions account for almost one-third of the global burden of disease, with the majority of patients living in low-income and middle-income countries (LMICs).1 Global surgery is an essential component of Universal Health Coverage (UHC),2 impacting directly on life, death and disability, and indirectly on economic growth. The misconception that surgery is expensive has led to a significant disparity in the access to safe and affordable surgical care worldwide.3
Provision of children’s surgical care is critical to ensuring UHC; however, in many LMIC settings, there is a lack of workforce and health system infrastructure to match the need for children’s surgery. Children account for more than half of the global population, yet <8% of the child population of LMICs has access to surgical care.4–6
The context for children’s surgery in Tanzania
By 2018, Tanzania had a population of 54.2 million, of which half were children.7 The country’s ratio of Surgeons, Obstetricians and Anaesthesiologists (SOA) per 100 000 population is 0.46, far lower than the recommended 20 SOA workforce/100 000 population.8 The government’s expenditure on health is approximately 10% of its gross domestic product.9
Children’s surgery in Tanzania is served by two main hospitals: Muhimbili National Hospital (MNH) in Dar Es Salaam is a national referral centre and university teaching hospital, with 1500 beds, up to 1000 outpatients per day and 1200 inpatient admissions per week.10 MNH’s Children’s Surgery Unit is responsible with all the general surgical cases of children under 11 years, from the entire country. Currently, up to 10 general paediatric surgical cases are performed daily; however, this was not always the case. Kilimanjaro Christian Medical Centre (KCMC), another referral hospital (located at the foothills of the Mount Kilimanjaro) has a capacity of 630 official beds caring for 500–800 inpatients, 40 baby incubators and 1300 staff. Prior to 2002, there was only one operating theatre in each of KCMC and MNH, shared by adults and children.
Historical background of the Tanzania–Oxford partnership
With the formation of a new medical school in 2002, Kilimanjaro Christian Medical University (KCMU), the vice chancellor of KCMU made an official invitation to a retired surgical colleague in Oxford to help develop a surgical specialities curriculum and training. Starting as a multi-disciplinary surgical partnership, aiming to support the training and development of children’s surgical services to provide safe children’s surgery at the institution and Tanzania more widely, this initial invitation commenced the now 17-yearlong sustainable partnership in children’s surgery between Oxford and Tanzania. The partnership evolved yearly from 2002 to 2012 at KCMC, and later from 2012 to present, at MNH. There is now a dedicated children’s operating theatre and children’s surgical ward (fully staffed), performing an average of three complex cases daily, along with community-based staff and resources for follow-up and awareness of children’s surgical cases. An ambulatory children’s surgical at a close by district general hospital is also supported. The move from KCMC to MNH was in response to an urgent need for children’s surgical workforce development, due to the untimely deaths of the senior children’s surgeons at MNH.
Surgical volunteerism
In response to invitations from Tanzanian colleagues, a multi-disciplinary team (MDT) of clinical staff from Oxford made voluntary, self-funded visits, lasting 10–14 days, using their annual leave for the first few years of the partnership. More recently, the partnership has been fully funded, through the generous philanthropic legacy of the Hugh Greenwood Foundation, through the University of Oxford. Traditionally, surgical volunteerism has been at the forefront of global surgery efforts responding to the significant burden of surgical disease in LMICs. Surgical providers from high-income countries (HICs) volunteer to visit LMICs and partner with the local providers to deliver surgical care and trainings to improve outcomes. Collaborations with international organisations have been active in provision of healthcare services in LMICs. However, some of these altruistic efforts fail due to complex ethical, cultural and financial challenges and poor planning.11 Guidelines and recommendations on establishing partnerships and missions in LMICs have been put forward to maximise effectiveness and minimise risks of potential harm.12 13 There is however, limited information on models guiding the development and sustainability of global children’s surgery partnerships in resource-limited countries. We aim to share our experience on developing, implementing and sustaining, a successful 17-yearlong partnership in global children’s surgery in Tanzania.
Participatory approaches to partnership building and health systems strengthening
The Tanzania–Oxford children’s surgery partnership used a model of participatory learning and action cycles to build healthcare infrastructure and workforce relating to children’s surgery, focusing on three of the six pillars of surgical health systems: infrastructure, workforce and service delivery.14
Participatory approaches focus on: (1) concrete contexts and relationship of stakeholders, (2) reflective and dialogical learning processes and (3) democratic and inclusive decision-making.15 Instead of basing priorities for children’s surgery on predefined values, norms and principles, local priorities were cocreated between partners. We used an iterative process (figure 1) by which all local stakeholders for children’s surgical care provision in Tanzania were encouraged (through facilitated group discussions) to critical reflect on and identify the areas of need within their health system, and to make formal invitations to the team based at Oxford University Hospitals NHS Trust to further analyse these priority areas, linking these to the health system building blocks, to ensure a systems-based approach to strengthening children’s surgical services. The team (including clinical staff, technicians, paramedical staff, allied health workers and hospital administrators) then took collective action to meet the priority areas, revisiting these priorities on an annual basis. Finally, the team reflected on the work accomplished, encouraged further creative thinking to solve local problems, using local resources and empowered locally based leadership in children’s surgery, anaesthetics and nursing care.
Figure 1.
A cycle of process of participatory action taken during our partnership.
The importance of cultural humility and reciprocity
At the heart of the partnership model were the values of cultural humility and reciprocity. It was important for the visiting team, not to exert their cultural influences and ways of working into another health system, where many of these practices would not be adoptable or sustainable in the local Tanzanian context. The use of participatory methods facilitated a non-hierarchical environment. As well as encouraging an understanding of the context, local needs, available resources and hospital capacity (including budget constraints); when codesigning solutions, the egalitarian nature of the partnership, facilitated constancy of the partnership during times of change.
Some examples of the innovative solutions generated in response to participatory action and learning cycles are outlined below.
Example 1: In response to the identified problem of providing healthy inpatient meals for children, action was taken by KCMC hospital staff to provide nutrition to inpatients, by growing fresh vegetables on site for their patient’s daily meals. By engaging resident family members in this process of vegetable cultivation, the scope of the work further expanded to engage families in issues around handwashing, hygiene, climate change, recycling and children’s nutrition (figure 2).
Figure 2.
Nutrition; hospital garden with home-grown produce.
Example 2: As children’s services expanded to include neonatal surgical patients, the need was identified for more neonatal incubators in the hospital. Traditional incubators from the UK can cost up to US$40 000.00 and rely heavily on a power source, and require maintenance and back-end support for technical difficulties. The KCMC hospital in response, developed its own low-cost neonatal incubators costing US$10 per incubator. The innovation of a low-cost incubator by-passed the need for background technical support and provided the humidity and warmth required in the immediate neonatal period at a low cost (figure 3).
Figure 3.
Innovation of low-cost incubator. (A) US$40 000.00 and (B) US$10.00.
Many LMIC hospitals receive donated equipment with good intentions, but without considering the necessary training, IT support and electricity needs to maintain the equipment.16 Working in low resource settings, understanding the financial constraints and adapting to available resources are a few of the many skills gained by the HIC partner and taken back to the UK, as part of the participatory approach and reverse innovation taking place during the partnership.
Challenges in providing children’s surgical services in Tanzania
Prior to the partnership, Tanzania had no practicing children’s surgeons. Children’s surgical care was provided by adult general surgeons. This limited the scope of operating to general children’s surgery, with a lack of specialisation to deal with complex congenital malformations and children’s cancer surgery. Adult general surgeons, anaesthetists, surgical trainees, medical students and nursing staff had not been exposed to children’s surgery as a specialist area, requiring specific clinical skills. Training and education in children’s surgery were needed and required to be delivered taking into account the multi-disciplinary nature of children’s surgery.
At MNH, children’s surgery came under the umbrella of general surgery, both sharing and competing for operating theatre time and space with adult surgery and obstetrics. This had resulted in a 3-year waiting-list for elective children’s surgery. Lack of designated operating theatre space and time had meant that elective children’s surgery was neglected in favour of adult emergency cases.
Strengthening the health system: workforce development
Education and training programme
The training and education components focused on clinical settings: (1) operating theatre, (2) clinic, (3) ward and (4) community (table 1).
Table 1.
Workforce development
| Workforce | Training content | Output |
| ENT surgeons | ENT clinicians trained to develop as medical educators through Masters in Medical Education (MMed) programmes. | Two ENT surgeons were supported to completion of their MMed. |
| Paediatric surgeons | Continuing professional development: adult general surgeons trained to perform paediatric procedures. Professional advancement through Surgical fellowship scheme (COSECSA). |
12 Surgeons trained (10 practicing purely paediatric surgery, 2 mixing adult and children surgery). |
| Overseas visits for surgeons | Tanzanian surgeons visited Oxford University Hospitals for 4–6 weeks. | Eight surgeons received targeted training in paediatric surgery. |
| Anaesthetics | Oxford anaesthesia team made five visits to Tanzania to train local staff. | Two anaesthetists trained in paediatric anaesthesia. 10 Operating theatre practitioners trained. |
| Radiology | Visiting Oxford and in-country training. | Four trainees learnt about interventional radiology and MRI |
| Nursing | In-ward training during visits, bedside teaching. | Four nurses trained in theatre organisation, and laparoscopic set-up. Community healthcare. |
| Clinical officers | WHO basic surgical care. | 40 Clinical officers trained in basic surgical care. |
| Medical students | Student electives in Tanzania and UK. | Tanzanian students spent time in Oxford. Formation of OxPLORE. |
| Research capacity building | Mentor–mentee model; encourage and establish research programmes, grant application and publications. | Publication in peer-reviewed journals.5 17–31 Establishment of MNH–Oxford Research partnership. |
COSECSA, College of Surgeons of East Central and Southern Africa; ENT, ear, nose and throat; MNH, Muhimbili National Hospital; OxPLORE, Oxford Paediatric Surgery Linking our research with Electives.
Skills training
Capacity for children’s surgery was built by first training adult general surgeons to perform children surgery. Adult general surgeons were then progressively supervised and supported to become bona fide children’s surgeons. Surgeons were selected based on recommendation by the LMIC and HIC leads, for 6 weeks to 3 months of targeted training in children’s surgery in Oxford. Capacity was built for bowel surgery, including anorectal malformations, surgical management of Hirschsprung’s disease, liver surgery (including biliary atresia surgery); complex paediatric urology, including cloacal abnormalities, complex staged surgery for urological and gastroenterological abnormalities and children’s oncological surgery. Adult general surgeons were also supported in forming and running MDT meetings in children’s oncology, and encouraged to audit their surgical practice regularly through monthly morbidity and mortality meetings. A joint clinic with a local Tanzanian and UK surgeon was conducted at each visit for review of complex cases.
In parallel to the surgical collaboration, a team of theatre nurses, anaesthetists, neonatal nurses and allied health workers from the Oxford provided holistic surgical care and training on subjects including WHO surgical safety checklist, preparing a theatre trolley for common paediatric surgical emergencies and infection control within the operating theatre and wards.
To meet the needs of children’s nursing for paediatric surgical patients, local nurses working on the general medical children’s ward received training on children’s surgery ward skills, including wound and colostomy care and catheter care for patients with spina bifida. Additionally, the nursing teams worked on developing a community outreach service for complex children’s surgery patients and their families.
Patient care
The core value of the partnership has been to provide quality children’s surgical care in Tanzania. There is now a dedicated ward for children’s surgery with trained children’s surgical nurses. This has encouraged interprofessional learning through joint ward rounds with paediatricians, clinical meetings with oncology and neonatology teams for planning managements and refresher training during the annual visits. Community nurses are now engaging with ward staff on patients with spina bifida. There is now dedicated surgical junior and senior staff for children’s surgeries, who are working to make MNH a hub to both children’s surgical care and research in the country. Local paediatricians from the adjacent medical children’s ward were approached to collaborate and perform daily ward rounds on children’s surgical side.
Training was given in various modes, from short courses, informal trainings, electives for medical students to formal master-level training. Three of the fully trained paediatric surgical trainees from Oxford, who were engaged in this partnership, have subsequently moved to LMIC contexts to start their careers in children’s surgery as consultants.
The partnership is now working in collaboration with the College of Surgeons of East Central and Southern Africa (COSECSA) to address the limited training opportunity in children’s surgery in sub-Saharan Africa, and developing a curriculum for children’s surgery for clinical officers (a cadre of health professional in Tanzania who often perform minor surgical operations in both main and district hospitals).
Training of medical students
The Tanzania–Oxford partnership further embraced their medical schools in developing an elective programme for Tanzanian students. A fully funded elective programme was instituted by the Oxford University Nuffield Department of Surgery for Tanzanian students to spend their electives at the Oxford University medical school from 2008 to 2012. A number of bursaries were offered by individuals from the UK teams to medical students. This collaboration led to the formation of joint research projects and platforms for sharing educational skills among medical students from the two institutions. This further led to the formation of Oxford Paediatric Surgery Linking Our Research with Electives to harness the power of medical students in global surgery research. Students from Oxford with an interest in global health were selected and supervised by the HIC lead (KL). Students were trained and oriented to the partnership and prepared to work alongside their LMIC partner.
Developing research capacity
To date, the Tanzania partnership has generated 14 publications in peer-reviewed journals and 54 abstracts presented at international research meetings, 18 book chapters, 4 international fellowships in children’s surgery and 5 scholarships for training in better resourced parts of Africa.5 17–31 The Tanzanian research team are actively collaborating on the multi-site Global Paedsurg sub-Saharan African research21 and are one of four centres implementing the gastroschisis care bundle.20 Building capacity to young researchers through the partnership will enable independent local researchers to pursue funding and research opportunities to improve global children surgery.
Improving health systems infrastructure and service delivery
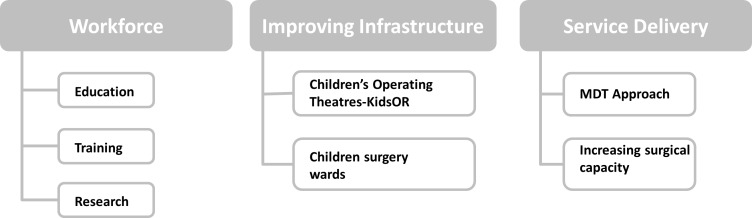
A systems-based approach was adopted for improvement of children’s surgical services, addressing various levels of health system constraints for quality improvement of children’s surgery and programme development32 and taking into account the building blocks of health systems (table 2; figure 4).
Table 2.
Areas of focus on the health system for high-quality healthcare
| Level of health system | Interventions to improvement |
| Macro level | Development of children’s surgical leadership; Working in partnership with NGOs: KidsOR to build operating theatres; Forming children’s surgical training programme with COSECSA. |
| Meso level | Workforce capacity building through targeted education and training; Developing a holistic curriculum; Training of clinical managers; CPD programme development in partnership with COSECSA; Building research capacity. |
| Micro level | Surgical procedures training; Radiological investigation training; Medical student electives. |
COSECSA, College of Surgeons of East Central and Southern Africa; CPD, continuing professional development; KidsOR, Kids operating room; NGO, non-profit organisation.
Figure 4.
Summary of the impact areas of the partnership. KidsOR, kids operating room; MDT, multi-disciplinary team.
Children’s operations were done on two half-days in a week, with two operating tables within each adult theatre rooms since there were no specific theatres for children.
In response to this need for designated children’s surgery operating theatres and operating theatre time at MNH, the Tanzania–Oxford partnership engaged and worked in partnership with a non-profit organisation called kids operating room (KidsOR).33 In 2017, KidsOR installed two fully equipped new theatres and refurbished children’s surgical ward (free of charge) for specialist children’s surgical services to be delivered at MNH. This remains the largest general paediatric surgery centre in the country. The installation of the two designated children’s operating theatres in Tanzania helped erase the 3 years elective surgery waiting-list in just 3 months.
Previously children’s cancer surgery was performed only by visiting surgeons from HICs, or the children were sent for treatment outside of Tanzania. Now, local surgeons feel empowered and confident enough to perform cancer-related surgery in-country, with local follow-up care, and are no longer reliant on overseas teams to visit. A study done at MNH reported in-hospital survival of 87% for solid tumour surgery in children.23
Refurbishment of the children’s ward to include surgical cases also had the unintended effect of fostering a spirit of mutual cooperation between the children’s surgical and medical teams who now conduct joint ward rounds. The nursing programme on catheter care for spina bifida and colostomy care helped to reduce re-admissions for catheter and stoma-related problems.
Conclusion
We have presented a participatory approach to partnership development around children’s surgical services in Tanzania. In our experience, the success of this partnership has been in building trust through the shared values of cultural humility and reciprocity (box 1). Often in the establishment of partnerships between HIC and LMIC, the terms of the partnership are dictated by funding bodies or sharing of resources from the HIC to LMIC. Some of the priorities for funding bodies and HIC partners may not match the needs and interests of the LMIC partners, and can lead to problems of uptake and sustainability, as well as propagation of cultural hierarchies. Sustainable strategies for providing children’s surgical care in LMICs settings depend on bilateral collaborative working to ensure effective and contextually relevant solutions to locally identified problems.34
Box 1. Steps in partnership approach.
Summary of steps
Respond to invitations from local people.
Listen to the people’s needs and respond accordingly.
Work within their environmental and financial constraints.
Consider long-term impact and sustainability.
Train all levels and all health professionals involved in children’s surgery; from ward, clinic and theatre.
Involve hospital management.
Improve working environments—refurbish and upgrade operating theatres and wards.
Education at each level of health system and service provision.
Ensure that local surgeons receive qualifications that will enable them to disseminate knowledge to their trainees—through provision of MMed and research methods training.
Work on the local resources and capacity for example, training general surgeons.
Developing a research centre for children’s surgery.
Workforce densities to population ratio remain to be a big challenge in Tanzania in achieving access to safe surgery. To date, there is no specialised training in children’s surgery or anaesthesia in Tanzania. Collaborating with the COSECSA has provided opportunity for learning and improving workforce for children’s surgery in Tanzania. Improvements of hospital infrastructure have enabled retention of workforce and in-country training and learning of more specialised and even complex surgical procedures. The 12 surgeons trained in paediatric surgery are now working across Tanzania and cascading training to other surgeons.
Targeting the transformation of the whole health system in the provision of children’s surgical care has led to greater impact and sustainability of the programme. We have shown that this model can be useful in guiding partnerships, to align with the six core surgical indicators and strategic objectives of National Surgical Obstetric and Anaesthesia plans (NSOAPs) in achieving universal coverage for all children requiring essential surgery.1 8 The launch of Tanzania NSOAP and its commitment to UHC is an important document to guide the future of children’s surgery in Tanzania, in order to ensure that the country can achieve safe surgery for everyone. Teaching hospitals like MNH and KCMC are uniquely positioned to lead sustainable global surgery efforts that may have impact on the whole nation.
The Tanzania–Oxford partnership has contributed to health systems strengthening in relation to children’s surgery in Tanzania, through focusing on the workforce, infrastructure for children’s surgery and service delivery. Longer training time due to the secondment of children’s surgical trainees to other hospitals created delays in developing the service to completion and succession planning. The biggest challenge was the interferences by other HIC visiting teams building their own partnerships rather than working collaboratively. In addition to visionary local leadership, we believe that participatory approaches are feasible and valuable in developing, implementing and sustaining global partnerships for children’s surgery.
Acknowledgments
The authors would like to thank Dr Griff Fellows and Prof John Shao for their initial commitment to the development of this partnership. The projects explained in this paper were supported by the Hugh Greenwood Foundation and the Oxford University Grants scheme. The authors also acknowledge all the partner institutions (Oxford University, MNH and KCMC) for their ongoing support.
Footnotes
Handling editor: Seye Abimbola
Twitter: @GodfreySama, @ShobhanaNagraj
Contributors: GSP helped in information retrieval, assembly and leading the writing team for this paper. SN performed the information review, designed the format and helped in writing to the final article. ZMB helped in providing the background of review and approved the final document. KL provided mentorship in the writing, background information of the partnership and advised on the format and model used.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available.
References
- 1.Meara JG, Leather AJM, Hagander L, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386:569–624. 10.1016/S0140-6736(15)60160-X [DOI] [PubMed] [Google Scholar]
- 2.Okoroh JS, Chia V, Oliver EA, et al. Strengthening health systems of developing countries: inclusion of surgery in universal health coverage. World J Surg 2015;39:1867–74. 10.1007/s00268-015-3031-7 [DOI] [PubMed] [Google Scholar]
- 3.Bae JY, Groen RS, Kushner AL. Surgery as a public health intervention: common misconceptions versus the truth. Bull World Heal Organ 2011;89:394 10.2471/BLT.11.088229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mullapudi B, Grabski D, Ameh E, et al. Estimates of number of children and adolescents without access to surgical care. Bull World Health Organ 2019;97:254–8. 10.2471/BLT.18.216028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grabski D, Ameh E, Lakhoo K, et al. Optimal resources for children's surgical care: Executive summary. World J Surg 2019;43:978–80. 10.1007/s00268-018-04888-7 [DOI] [PubMed] [Google Scholar]
- 6.Ozgediz D, Langer M, Kisa P, et al. Seminars in pediatric surgery pediatric surgery as an essential component of global child health. Semin Pediatr Surg 2016;25:3–9. [DOI] [PubMed] [Google Scholar]
- 7.National Bureau Statistics Tanzania in figures 2018, 2019. [Google Scholar]
- 8.United THE, Of R, Health MOF, et al. The United Republic Of Tanzania Gender, Elderly and Children National Surgical, Obstretric and Anaesthesia Plan (NSOAP), 2018: 2018–25. [Google Scholar]
- 9.Lee B, Tarimo K. Analysis of the government of Tanzania ’ S budget allocation to the health sector for fiscal year 2017/18, 2018. [Google Scholar]
- 10.MUHIMBILI Muhimbili National Hospital, 2019. Available: http://www.mnh.or.tz/index.php/our-profile [Accessed 4 Oct 2019].
- 11.Welling DR, Ryan JM, Burris DG, et al. Seven Sins of humanitarian medicine. World J Surg 2010;34:466–70. 10.1007/s00268-009-0373-z [DOI] [PubMed] [Google Scholar]
- 12.THET Health Partnership Scheme, Impact Report 2011-2019, 2019. [Google Scholar]
- 13.THET Principles of partnership. Available: https://www.thet.org/principles-of-partnership/ [Accessed 20 Oct 2019].
- 14.Citron I, Jumbam D, Dahm J, et al. Towards equitable surgical systems: development and outcomes of a national surgical, obstetric and anaesthesia plan in Tanzania. BMJ Glob Heal 2019;4:e001282 10.1136/bmjgh-2018-001282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Metselaar S, Widdershoven G, Porz R, et al. Evaluating clinical ethics support: a participatory approach. Bioethics 2017;31:258–66. 10.1111/bioe.12348 [DOI] [PubMed] [Google Scholar]
- 16.Marks IH, Thomas H, Bakhet M, et al. Medical equipment donation in low-resource settings: a review of the literature and guidelines for surgery and anaesthesia in low-income and middle-income countries. BMJ Glob Heal 2019;4:e001785 10.1136/bmjgh-2019-001785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moore SW, Tshifularo N, Banieghbal B, et al. Anorectal atresia with gross terminal colonic distension in Africa. Pediatr Surg Int 2013;29:1287–91. 10.1007/s00383-013-3346-0 [DOI] [PubMed] [Google Scholar]
- 18.Bradshaw CJ, Bandi AS, Muktar Z, et al. International study of the epidemiology of paediatric trauma: PAPSA research study. World J Surg 2018;42:1885–94. 10.1007/s00268-017-4396-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kisa P, Grabski DF, Ozgediz D, et al. Unifying children's surgery and anesthesia stakeholders across institutions and clinical disciplines: challenges and solutions from Uganda. World J Surg 2019;43:1435–49. 10.1007/s00268-018-04905-9 [DOI] [PubMed] [Google Scholar]
- 20.Wright N, Abantanga F, Amoah M, et al. Developing and implementing an interventional bundle to reduce mortality from gastroschisis in low-resource settings. Wellcome Open Res 2019;4:46 10.12688/wellcomeopenres.15113.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright NJ. Global PaedSurg – A multi-centre international prospective cohort study. Available: http://globalpaedsurg.com/paedsurg-africa/ [Accessed 20 Oct 2019].
- 22.Wright NJ, Leather A, Sevdalis N, Global PaedSurg Research Collaboration . Management and outcomes of gastrointestinal congenital anomalies in low, middle and high income countries: protocol for a multicentre, international, prospective cohort study. BMJ Open 2019;9:e030452 10.1136/bmjopen-2019-030452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ford K, Gunawardana S, Philipo GS, et al. Investigating Wilms ’ Tumours Worldwide : A Report of the OxPLORE Collaboration — A Cross-Sectional Observational Study. World J Surg 2019;44:1–8. [DOI] [PubMed] [Google Scholar]
- 24.Nasir AA, Lakhoo K. Evaluation of clinical research reporting in African Journal of paediatric surgery. Afr J Paediatr Surg 2013;10:13–16. 10.4103/0189-6725.109376 [DOI] [PubMed] [Google Scholar]
- 25.Ringo Y, Drake D, Sillo T, et al. Parasitic twin within spina BI FI dA. African J Paediatr Surg 2012;9:240–3. [DOI] [PubMed] [Google Scholar]
- 26.Mhando S, Young B, Lakhoo K. The scope of emergency paediatric surgery in Tanzania. Pediatr Surg Int 2008;24:219–22. 10.1007/s00383-007-2072-x [DOI] [PubMed] [Google Scholar]
- 27.Nandi B, Mungongo C, Lakhoo K. A comparison of neonatal surgical admissions between two linked surgical departments in Africa and Europe. Pediatr Surg Int 2008;24:939–42. 10.1007/s00383-008-2177-x [DOI] [PubMed] [Google Scholar]
- 28.Moore SW, Alexander A, Sidler D, et al. The spectrum of anorectal malformations in Africa. Pediatr Surg Int 2008;24:677–83. 10.1007/s00383-008-2131-y [DOI] [PubMed] [Google Scholar]
- 29.Mhando S, Lyamuya S, Lakhoo K. Challenges in developing paediatric surgery in sub-Saharan Africa. Pediatr Surg Int 2006;22:425–7. 10.1007/s00383-006-1669-9 [DOI] [PubMed] [Google Scholar]
- 30.Butler MW, Ozgediz D, Poenaru D, et al. The global paediatric surgery network: a model of subspecialty collaboration within global surgery. World J Surg 2015;39:335–42. 10.1007/s00268-014-2843-1 [DOI] [PubMed] [Google Scholar]
- 31.Lakhoo K. Global help: free medical information. Eur J Pediatr Surg 2014;24:430 10.1055/s-0034-1371717 [DOI] [PubMed] [Google Scholar]
- 32.Kruk ME, Gage AD, Arsenault C, et al. The Lancet Global Health Commission High-quality health systems in the Sustainable Development Goals era : time for a revolution. Lancet Glob Heal 2018;6:1196–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.KidsOR KidsOR; surgery for children. Available: https://www.kidsor.org/what-we-do/#whatSection
- 34.Krishnaswami S, Stephens CQ, Yang GP, et al. An academic career in global surgery: a position paper from the Society of university surgeons Committee on academic global surgery. Surgery 2018;163:954–60. 10.1016/j.surg.2017.10.019 [DOI] [PubMed] [Google Scholar]