Abstract
Professional drivers show a higher prevalence of obstructive sleep apnoea (OSA) compared with the general population. Furthermore, there is concern about the association between OSA and car crash risk given that drivers with OSA show an increased risk for car accidents. Despite this risk, OSA is often underdiagnosed and undertreated in this population, mainly due to lack of appropriate screening and sleep study referrals. Polysomnography (PSG), the gold standard test, is inappropriate for systematic screening because of its high expense, complexity and relative inaccessibility in this population. Therefore, there is a strong demand for good screening tools, including both subjective and objective data that may assist in early identification of possible OSA among professional drivers and, thus, aid in PSG examination referral and OSA management in an accredited sleep centre. However, there is considerable disagreement over screening methods and criteria for triggering a sleep study referral in different countries. There is also a strong need for further research in the area of OSA screening of commercial drivers in order to improve the diagnostic accuracy of screening tools and ensure that patients with OSA are accurately identified.
Key points
Obstructive sleep apnoea (OSA) is often undiagnosed and undertreated in professional drivers.
Professional drivers often under-report and are reluctant to report OSA symptoms.
Barriers to OSA diagnosis include appropriate screening and sleep study referrals.
Screening tools including both subjective and objective data may assist in early identification of possible OSA among professional drivers.
Educational aims
To evaluate screening instruments currently used to identify OSA risk in professional drivers.
To provide guidance for developing an assessment strategy for OSA by professional driver medical examiners.
Short abstract
OSA is usually undiagnosed and undertreated in professional drivers. Barriers to OSA diagnosis are lack of appropriate screening and sleep study referrals. Screening tools, including both subjective and objective data, may assist in early identification. http://bit.ly/31nD4A9
Professional drivers are an understudied and medically underserved population, with high rates of obesity and related comorbidities [1]. Research has shown that drivers with multiple comorbidities, such as cardiovascular disease, cerebrovascular diseases, psychiatric conditions, diabetes, medication use, uncorrected visual defects and obesity seem to be at increased risk of being involved in a crash [2]. Disorders associated with sleep disturbance and sleepiness, such as obstructive sleep apnoea (OSA) are also recognised to be associated with increased accident risk [3], exceeding the risk associated with many other medical disorders [4].
Given the impact of OSA on sleep quality, daytime sleepiness, psychomotor vigilance and driving simulator performance, it is not surprising that untreated OSA increases the risk of crashes by two- to three-fold in comparison with subjects without OSA [5]. The most common symptom of patients with OSA associated with increased crash risk and fatal accidents is subjective daytime sleepiness, [6, 7]. However, the increased crash risk can be seen in patients even without daytime sleepiness and is aggravated by concurrent use of alcohol or sedatives [8]. Nevertheless, effective treatment of OSA seems to normalise the risk for accidents [9]. Therefore, identifying professional drivers with OSA and treating them effectively should decrease crash-related injuries and fatalities and improve drivers' health.
Professional drivers show a higher prevalence of OSA, between 28% and 78%, compared with the general population [10], probably because they tend to be obese, male and middle-aged, the three most common risk factors for OSA [11]. Despite this risk, OSA is often undiagnosed and undertreated in this population, mainly due to lack of appropriate screening and sleep study referrals [12–14]. In an effort to address the high prevalence of untreated OSA in this population, a new directive 2014/85/EU [15] from the European Union has been adopted regulating, for the first time, requirements for issuing a driver's license for amateur and commercial drivers. Based on this directive, all drivers should be subjected to tighter control of their overall health status, including OSA screening and drivers with diagnosed OSA must receive regular treatment and follow-up [15]. Furthermore, a joint Task Force of the European Respiratory Society and the European Sleep Research Society is currently on production to develop practical recommendations to cope with the problems raised by the new EU directive on issuing driving licences and to suggest a research agenda to improve safety on the road in Europe [16]. Additionally, the American Academy of Sleep Medicine has issued a comprehensive and detailed document on screening, and diagnostic and therapeutic approaches for commercial drivers [10]. However, still there is no consensus in the OSA screening approach and there is a lack of a clear standardised model applicable in different countries.
The purpose of this review is to evaluate screening instruments currently used to identify risk of OSA in professional drivers and provide guidance for developing an assessment strategy for OSA by professional driver medical examiners.
Diagnostic evaluation of OSA
The diagnosis of OSA requires either signs/symptoms or an associated medical or psychiatric disorder coupled with five or more predominantly obstructive respiratory events per hour of sleep during polysomnography (PSG). Alternatively, a frequency of obstructive respiratory events ≥15 events·h−1 satisfies the criteria, even in the absence of associated symptoms or disorders [17]. This definition indicates that there are also subjects who are diagnosed with OSA but without symptoms.
The gold standard for the diagnosis of OSA is attended overnight PSG [18], which is performed in accredited sleep units. However, it is inappropriate for systematic screening because it is expensive, labour-intensive, not feasible in all subjects and probably time consuming for professional drivers who are regularly on the road. Therefore, simple and inexpensive selection of patients with the potentially highest risk of OSA is needed.
The process of diagnosing and treating OSA in professional drivers should begin with effective and consistent screening. Historically, in order to screen drivers for OSA, healthcare providers asked questions about loud snoring, witnessed apnoea or daytime sleepiness. However, the professional driver population presents unique and specific challenges to the successful identification of those with OSA. Several studies have indicated that professional drivers usually under report OSA symptoms or show resistance to OSA assessment, in order to avoid potential consequences on medical certification and employment, economic implications of additional testing and occupational consequences of lost work time [13, 14, 19].
For this reason, there is a strong demand for good screening tools, including both subjective and objective data that may assist in the early identification of possible OSA among professional drivers and thus aid in referring them for PSG examination and OSA management in an accredited sleep centre. Furthermore, even when professional drivers do not complain of OSA symptoms, it is essential to perform periodic clinical screening by a skilled physician, as a way to additionally raise the commercial drivers' awareness of the problem.
Screening tools
Current screening strategy often relies on validated questionnaires to identify subjects at risk for OSA. The ideal diagnostic screening tool would contain a few items and be quick to administer and interpret without the need for complicated calculations or examination techniques. A number of clinical questionnaires have been developed to predict the presence of OSA based on symptoms (e.g. excessive daytime sleepiness, periods of stopping breathing during sleep observed by others), anthropometrics (e.g. body mass index (BMI), neck circumference), demographics (sex and age) and the presence of comorbidities (e.g. hypertension, stroke). However, a high sensitivity with an acceptable specificity is a basic requirement for screening patients for a disease with an important health impact, such as OSA. The sensitivity and specificity of OSA screening tools have demonstrated considerable variability depending on the patient population, and the definition of OSA (different cut-off points of apnoea–hypopnoea index (AHI) for OSA diagnosis). Below we briefly describe some instruments that could be used for OSA screening. Epworth Sleepiness Scale (ESS), Berlin questionnaire, STOP and STOP-BANG are the most commonly known questionnaires and most studied (table 1).
Table 1.
Key features of screening questionnaires for OSA
| ESS | |
| How likely are you to doze off or fall asleep in the following situations, in contrast to feeling just tired? | |
| Situation | Chance of dozing (0–3) |
| Sitting and reading | |
| Watching TV | |
| Sitting inactive in a public place (e.g. a theatre or meeting) | |
| As a passenger in a car for an hour without a break | |
| Lying down to rest in the afternoon when circumstances permit | |
| Sitting and talking to someone | |
| Sitting quietly after a lunch without alcohol | |
| In a car while stopped for a few minutes in the traffic | |
| Berlin questionnaire | |
| Age ______ Gender______ | Weight _______ Height ______ |
| Category 1 | Category 2 |
| 1. Do you snore? | 6. How often do you feel tired or fatigued after your sleep? |
| 2. Your snoring is: | 7. During your waking time do you feel tired, fatigued, or not up to par? |
| a) Slightly louder than breathing | 8. Have you ever nodded off or fallen asleep while driving a vehicle? If yes: |
| b) As loud as talking | 9. How often does this occur? |
| c) Louder than talking | Category 3 |
| 3. How often do you snore? | 10. Do you have high blood pressure? |
| 4. Has your snoring ever bothered other people? | BMI= |
| 5. Has anyone noticed that you quit breathing during your sleep? | |
| STOP–BANG questionnaire | |
| STOP | BANG |
| Snoring | BMI >35 kg·m−2 |
| Tiredness | Age >50 years |
| Observed you stop breathing | Neck circumference >40 cm (15.7 inches) |
| Blood Pressure | Gender Male |
Epworth Sleepiness Scale
The ESS is currently the most used subjective test of daytime sleepiness in clinical practice. It is a simple, self-administered, eight-item questionnaire that measures the risk of falling asleep in eight specific situations that are commonly met. A score of <10 is considered normal. The higher the score (from 10 to 24) the greater the reported subjective daytime sleepiness [20]. Although it is widely used, the real value for patients with OSA is still not clear, as OSA severity does not always correlate with ESS score and even patients with severe OSA may have relatively mild or no daytime sleepiness [21]. Considering its low sensitivity (53.2%) and specificity (58.8%) for diagnosis of moderate and severe OSA syndrome (AHI ≥15 events·h−1), the ESS is not suggested as a screening test for OSA diagnosis amongst candidates for drivers [22]. Furthermore, previous studies have shown that ESS combined with BMI identifies only 12–13% of drivers at high risk of OSA [13, 19], a relatively low percentage compared to the number of commercial drivers estimated to have OSA. Notably, potential denial or deception [13, 19] of self-reported sleepiness should also question the reliability of using ESS as a stand-alone screening tool for OSA risk or as a criterion for determining whether or not a professional driver with OSA should be qualified to drive.
Berlin questionnaire
The Berlin questionnaire is one of the commonly known questionnaires for OSA, first validated in the primary care setting [23]. It has 10 questions covering three categories including: 1) snoring severity (items 1–5); 2) excessive daytime sleepiness (items 6–9); and 3) history of high blood pressure or obesity (item 10). The questionnaire also includes information about age, sex, height and weight. The physician or medical staff are required to analyse the responses and the scoring can be complicated. If the individual scores positive in at least two of the three categories, the patient is found to be at high risk for OSA. The Berlin Questionnaire has been used for occupational health screening of commercial drivers demonstrating marked range of sensitivities (45.6–93.1%) and specificities (16.2–84.6%) for an AHI ≥15 events·h−1 [22–25]. Nevertheless, further research of its usefulness as an OSA screening tool is needed in this population.
STOP-BANG questionnaire
The STOP questionnaire was developed by Chung et al. [26] from patients attending surgical pre-operative assessment clinics. It consists of four yes/no questions about snoring, tiredness, observed apnoeas and blood pressure, and was found to have a sensitivity of 79.5% and a specificity of 48.6% for detecting an AHI of 30 events·h−1. The addition of four additional factors (BMI, age, neck circumference and SEX) to create the STOP-BANG questionnaire led to improvement in sensitivity to 100% at the expense of specificity that decreased to 37% [27]. The questionnaire has the advantage of being very straightforward and can be completed quickly and easily (usually within 1–2 min). A score of any three affirmative responses was used to dichotomise the population into low and high risk for OSA. STOP-BANG has been used with high sensitivities (87–100%) and moderate specificities (40.3–48.7%) and even recommended for screening professional drivers in previous studies [24, 28–32].
NoSAS score
The Lausanne NoSAS (Neck circumference, Obesity, Snoring, Age, Sex) score test is a simple, efficient, and easily employed tool enabling identification of individuals at risk for OSA [33]. The score ranges from 0 to 17 and if the individual has a score ≥8, the patient is found to be at high risk for OSA. Overall, the NoSAS score was able to detect 1666 (98%) out of 1703 participants with severe OSA (AHI >30 events·h−1), with 37 (2%) out of 1703 having a false-negative diagnosis in the HypnoLaus cohort [33]. In a recent validation study in a sleep clinic population, with a NoSAS score ≥8, the sensitivity and specificity (positive-predictive value) for moderate/severe OSA were 89.8% and 27.1%, respectively [34]. Compared with the eight items of STOP-BANG and the three separate calculations required for the Berlin Questionnaire, NoSAS score is easier to use as it only includes five items and helps clinicians decide with a higher accuracy than other questionnaires which individuals should be referred for further testing, thereby reducing the number of missed OSA diagnoses and unnecessary PSGs [33]. Nevertheless, more studies are needed to evaluate the efficacy of this score in drivers' population.
OSA evaluation worksheet
The OSA evaluation worksheet is a company-developed OSA screening tool, composed of various markers of OSA risk. Nine questions are completed by the driver, three of which relate to symptoms of OSA such as loud snoring, fatigue and observed apnoea. Additional information measured by a healthcare provider includes BMI, neck circumference, age, comorbidities and Mallampati class. Although it is not a validated tool, one recent study found the OSA evaluation worksheet along with STOP-Bang Questionnaire to be useful tools for OSA screening of professional drivers [32]. However, in this study a low percentage of those screened positive were referred for sleep testing. The authors concluded that screening drivers is useful only when drivers at high risk are referred for sleep testing and actually schedule sleep tests.
Somni-Sage
A carefully constructed on-line screening instrument with an on-line questionnaire (Somni-Sage), including demographics, comorbidities and symptoms, was found to have a high positive-predictive value leading to a large number of OSA diagnoses [19]. Nonetheless, a significant limitation of this study was that 64% of higher risk drivers had not received diagnostic confirmatory testing by the end of the study. Therefore, given the high loss to follow-up the results from such analyses should be treated with considerable caution.
The limited studies available in professional drivers with objective data (PSG/polygraphy) for validation show a huge range of sensitivities and specificities. Taking this into account, results regarding the predictive value of the above screening instruments should be taken into consideration. Furthermore, the majority of studies show a poor specificity, resulting in many false-positive results, which is associated with more frequent referrals for PSG, queues in sleep apnoea laboratories and high costs of unjustified diagnostic procedures. However, all these instruments are not perfect tools, but only a guide to supplement a careful history. Future studies should focus on more validation testing of the OSA screening questionnaires, as well as identification of subjective and objective tools for reliable excessive daytime sleepiness detection and fitness to drive assessment, before a conclusion can be made regarding which tool has the best OSA predictability in the professional drivers population.
Principles of OSA evaluation in professional drivers
Commercial drivers should require a higher standard for assessment of medical fitness to drive and a lower threshold of diagnostic testing for OSA compared with non-commercial car drivers. The U.S. Preventive Services Task Force (USPSTF) neither supports nor rejects screening of asymptomatic adults for OSA in the general population [35]. However, the USPSTF recommendations do not address individuals performing safety sensitive jobs, such as professional drivers.
Many countries have medical standards for commercial driving licensure that include specific questions about OSA and other sleep disorders, as well as guidelines for treatment and re-evaluation of OSA [16, 36–38]. The European Respiratory Society and the European Sleep Research Society are currently working to develop practical recommendations and address the following questions [16]:
How should the suspicion of moderate or severe OSA be justified?
Are there simple and readily available tools to assess OSA and sleepiness in the population?
What is the consensus on a minimal medical expert standard to establish good compliance to, and effectiveness of, treatment?
Which tests or investigations should be used to certify continued good vigilance?
Furthermore, Ghosh et al. [39] suggested that driving regulatory authorities should take into account specific parameters to assess the risk of road traffic accidents in patients suspected of having OSA, as outlined below.
Driving-related parameters
Taking a break every hour during long journeys
Likelihood of feeling sleepy while driving
Nodded off whilst driving in the past year
Any accidents in the past 3 years related to sleepiness
Clinical parameters
ESS and history of tiredness and sleepiness
Objective testing: AHI, apnoeas and hypopnoeas/time in bed, oxygen desaturation index
In the USA, a Joint Task Force of the American College of Chest Physicians, American College of Occupational and Environmental Health and the National Sleep Foundation has recommended that OSA testing be performed in commercial truck drivers with a BMI ≥35 kg·m−2 [36], while other groups have endorsed BMI thresholds ranging from ≥30 kg·m−2 to ≥40 kg·m−2 [10, 40]. The American Academy of Sleep Medicine recommends that commercial drivers be referred to a sleep medicine specialist for clinical sleep evaluation and diagnostic testing if they meet any of the following criteria [10].
BMI ≥40 kg·m−2
Fatigue or sleepiness during the duty period or involvement in a sleepiness-related crash or accident. Factors suggesting a sleepiness-related crash or accident include single vehicle crash, off-road deviation and rear-ending another vehicle
BMI ≥33 kg·m−2 and either type 2 diabetes or hypertension requiring two or more medications
Although these criteria intend to classify drivers as high risk for OSA, individuals with lower BMI will likely be missed. Adding subjective criteria based on other symptoms and risk factors are also suggested, but the examiners should be thoroughly trained in the presentation of OSA, in eliciting relevant symptoms and appropriately screening for it. Therefore, medical examiners should undergo minimum training and certification in order to reduce the number of missed cases of OSA.
Despite the several recommendations regarding OSA screening, there is some difficulty providing concrete guidance given the variability between different recommendations and working groups. A recent study assessing the screening practices for OSA among occupational/environmental physicians in the US state of Michigan during driver medical examinations showed that 97% of physicians reported doing some type of screening [41].
Clinical assessment in professional drivers
Required driver medical examinations are commonly performed by occupational/environmental practitioners and screening for OSA should be a common consideration as part of the examination. We propose that clinical evaluation of OSA and its symptoms should begin with early recognition, mainly based on patient report or physician questions about symptoms, risk factors and associated comorbidities. Information given by the patient should, when possible, be supplemented by a bed partner, family member or roommate who may have a different insight into the patient's sleep behaviour or daytime mood and cognitive functioning. Typical symptoms associated with the condition include snoring, witnessed apnoeas, gasping or choking for air at night, excessive daytime sleepiness, impaired cognition and mood changes (table 2). Nocturnal symptoms are generally reported by the bed partner. Snoring is the cardinal one and may be so disruptive that the bed partner can be driven to sleep in another room. An absence of snoring does not exclude OSA diagnosis, but virtually all patients snore. A bed partner may also report a witnessed apnoea that is followed by loud snoring or gasping at the end of the apnoeic episode and this usually serves as the trigger for seeking medical attention.
Table 2.
Common symptoms of OSA
| Daytime symptoms | Night-time symptoms |
| Excessive daytime sleepiness | Snoring, gasping or choking in sleep |
| Fatigue | Witnessed apnoea in sleep |
| Non-restorative sleep | Insomnia |
| Cognitive impairment | Restless sleep |
| Mood disorders | Night-time awakenings, dry mouth |
| Morning headaches | Nocturia |
| Impotence, erectile dysfunction | Nocturnal gastro-oesophageal reflux |
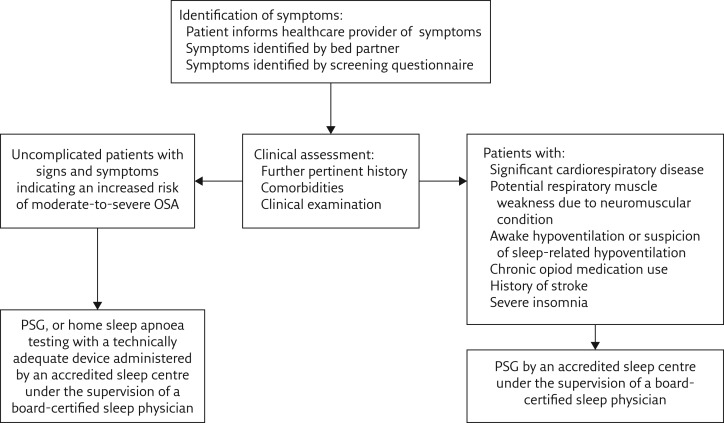
Unfortunately, patients are unlikely to present with a clear complaint consistent with OSA symptoms. Questioning the patient on the key symptoms of OSA, such as snoring and daytime sleepiness, is not so simple as patients often describe sleepiness as “fatigue”, “tiredness” or “lack of energy”. The most common daytime symptom associated with OSA is excessive sleepiness, which in more severe manifestations can result in sleepiness at the wheel while driving. The ESS can be used to help assess the level of daytime sleepiness. However, a number of non-medical and medical conditions, such as a shortage of sleep/sleep restriction due to social or family reasons, shift working or daytime non-shift working, neurological disorders, insomnia, depression and hypothyroidism, should be taken into account when evaluating daytime sleepiness [42]. Physicians also need to be aware that many OSA patients may have minimal or no symptoms. Driving simulators have also been used to identify individual “at-risk” drivers [43]. However, they were found to be insufficiently sensitive, not in widespread clinical use and could not fully replicate real driving [5]. Therefore, a diagnostic strategy is needed including a sleep-oriented history and physical examination. Given the need for stratification to determine patients who urgently require evaluation from a sleep specialist, it would clearly be beneficial to use screening questionnaires, such as the STOP-BANG questionnaire to identify patients who are likely to have OSA. Additionally, adoption of screening tools into the electronic health record as well as training of other medical staff, such as nurses, to help administer screening questionnaires may also help facilitate OSA screening. A clinical care pathway of OSA diagnosis is illustrated in figure 1.
Figure 1.
A proposed clinical care pathway of OSA diagnosis in professional drivers.
However, screening drivers is useful only when drivers found to be at high risk are referred for sleep testing and drivers actually schedule sleep tests. Barriers to referrals of high-risk drivers include concerns of angering drivers, lack of physical driver characteristics typically noted in OSA and losing business from drivers who seek out examiners who provide less rigorous commercial driver medical examinations (doctor shopping). Recommendations to remove these barriers should include clear screening and referral guidelines, employer-facilitated and employer-funded sleep testing, as well as OSA awareness campaigns directed toward drivers, employers and medical examiners.
The role of home sleep studies
Apart from the increasing interest in the use of screening questionnaires there has been a growing interest in ambulatory models of care, such as home sleep monitoring with portable monitors. In-home unattended, portable recording may be used to help in the detection of OSA in specific patient population, such as medically uncomplicated individuals with high pre-test suspicion for moderate-to-severe OSA [44].
Although portable monitors have been proposed as a cheaper and more accessible technology, an important proportion of professional drivers tested will likely require a follow-up with in-laboratory PSG due to invalid results, the relatively low sensitivity and specificity of this method, or potential barriers from human factors [45]. Recently, Lyons et al. [46] described a promising approach in identifying commercial motor vehicle operators likely to be at risk for a sleepiness-related crash due to OSA, by using the spectral qualities of electrocardiography with portable diagnostic ability and without requiring overnight in-laboratory PSG. Nevertheless, portable monitors remain a challenge for large-scale screening and diagnosis of OSA among professional drivers. Further prospective randomised studies conducted in collaboration with sleep centres are needed to determine the utility of portable monitors, comparing various portable monitors and type I PSGs.
Conclusion
Reasonable estimates of crash risk attributable to OSA support the use of screening strategies in commercial drivers. However, while most experts agree to OSA screening of drivers, especially professional drivers, the best screening strategy is not clearly defined; however, this is difficult given the current lack of definitive conclusions from research in the area. Furthermore, another challenge is to eliminate the overall inconsistency of provider referrals and sleep testing of professional drivers. Therefore, there is a strong need for further research in the area of OSA screening of commercial drivers in order to alleviate the burden of traffic accidents worldwide.
Self-evaluation questions
- A 46-year-old obese truck driver with a BMI of 38 kg·m−2 is referred to the sleep disorders center by the occupational practitioner who wishes to test him for OSA. The patient states that he has a history of snoring but has never been observed to be apneic. Besides obesity, his only medical problem is high blood pressure, which is well controlled by two medications. He does not wish to have an overnight sleep study because he states that she has no symptoms of daytime sleepiness. What is the appropriate next step?
- a) Given his lack of symptoms, it is unlikely that he has sleep apnoea and a sleep test is unnecessary
- b) Given his BMI, he has a high probability of having OSA
- c) The patient should be started on a diet and, if that fails, a sleep study should be considered
- d) Reassure the patient that the problem is minor and no further testing is necessary
- Which statement about OSA in professional drivers is not correct?
- a) The increased crash risk can be seen in OSA patients even without daytime sleepiness
- b) The prevalence of OSA in professional drivers is very low compared with the general population
- c) Barriers to professional drivers sleep testing are cost and lack of health insurance
- d) The simplest questionnaire for sleepiness, the ESS, is not able to discriminate drivers at risk for sleep apnoea
- Which of the following options is not seen as a barrier to OSA screening in professional drivers?
- a) Professional drivers voluntarily under report or deny OSA related symptoms on Commercial Driver Medical Examination
- b) Cost of in-laboratory studies
- c) Drivers and their employers may seek out clinics that conduct less rigorous examinations without OSA screening
- d) The ability of drivers and some physicians to appreciate OSA as a serious condition that threatens safe driving
- In evaluating daytime sleepiness, which of the following is true about the ESS?
- a) This scale uses a seven-part questionnaire
- b) It correlates strongly with OSA severity
- c) It is suggested as a screening test for OSA diagnosis amongst candidates for drivers licences
- d) ESS has a low sensitivity for OSA detection in professional drivers
Suggested answers
b
b
d
d
Footnotes
Conflict of interest: S.E. Schiza has nothing to disclose.
Conflict of interest: I. Bouloukaki has nothing to disclose.
References
- 1.Ng MK, Yousuf B, Bigelow PL, et al. . Effectiveness of health promotion programmes for truck drivers: a systematic review. Health Educ J 2015; 74: 270–286. doi: 10.1177/0017896914533953 [DOI] [Google Scholar]
- 2.Thiese MS, Hanowski RJ, Kales SN, et al. . Multiple conditions increase preventable crash risks among truck drivers in a cohort study. J Occup Environ Med 2017; 59: 205–211. doi: 10.1097/JOM.0000000000000937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonçalves M, Amici R, Lucas R, et al. . Sleepiness at the wheel across Europe: a survey of 19 countries. J Sleep Res 2015; 24: 242–253. doi: 10.1111/jsr.12267 [DOI] [PubMed] [Google Scholar]
- 4.Rodenstein D. Driving in Europe: the need of a common policy for drivers with obstructive sleep apnoea syndrome. J Sleep Res 2008; 17: 281–284. doi: 10.1111/j.1365-2869.2008.00669.x [DOI] [PubMed] [Google Scholar]
- 5.Strohl KP, Brown DB, Collop N, et al. . An official American Thoracic Society Clinical Practice Guideline: sleep apnea, sleepiness, and driving risk in noncommercial drivers. An update of a 1994 Statement. Am J Respir Crit Care Med 2013; 187: 1259–1266. doi: 10.1164/rccm.201304-0726ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lévy P, Kohler M, McNicholas WT, et al. . Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 2015; 1: 15015. doi: 10.1038/nrdp.2015.15 [DOI] [PubMed] [Google Scholar]
- 7.Bioulac S, Micoulaud-Franchi JA, Arnaud M, et al. . Risk of motor vehicle accidents related to sleepiness at the wheel: a systematic review and meta-analysis. Sleep 2017; 41: 10.1093/sleep/zsx134. [DOI] [PubMed] [Google Scholar]
- 8.Vakulin A, Baulk SD, Catcheside PG, et al. . Effects of alcohol and sleep restriction on simulated driving performance in untreated patients with obstructive sleep apnea. Ann Intern Med 2009; 151: 447–455. doi: 10.7326/0003-4819-151-7-200910060-00005 [DOI] [PubMed] [Google Scholar]
- 9.Karimi M, Hedner J, Häbel H, et al. . Sleep apnea-related risk of motor vehicle accidents is reduced by continuous positive airway pressure: Swedish Traffic Accident Registry data. Sleep 2015; 38: 341–349. doi: 10.5665/sleep.4486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gurubhagavatula I, Sullivan S, Meoli A, et al. . Management of obstructive sleep apnea in commercial motor vehicle operators: recommendations of the AASM Sleep and Transportation Safety Awareness Task Force. J Clin Sleep Med 2017; 13: 745–758. doi: 10.5664/jcsm.6598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie W, Chakrabarty S, Levine R, et al. . Factors associated with obstructive sleep apnea among commercial motor vehicle drivers. J Occup Environ Med 2011; 53: 169–173. doi: 10.1097/JOM.0b013e3182068ceb [DOI] [PubMed] [Google Scholar]
- 12.Gurubhagavatula I, Maislin G, Nkwuo JE, et al. . Occupational screening for obstructive sleep apnea in commercial drivers. Am J Respir Crit Care Med 2004; 170: 371–376. doi: 10.1164/rccm.200307-968OC [DOI] [PubMed] [Google Scholar]
- 13.Parks P, Durand G, Tsismenakis AJ, et al. . Screening for obstructive sleep apnea during commercial driver medical examinations. J Occup Environ Med 2009; 51: 275–282. doi: 10.1097/JOM.0b013e31819eaaa4 [DOI] [PubMed] [Google Scholar]
- 14.Talmage JB, Hudson TB, Hegmann KT, et al. . Consensus criteria for screening commercial drivers for obstructive sleep apnea: evidence of efficacy. J Occup Environ Med 2008; 50: 324–329. doi: 10.1097/JOM.0b013e3181617ab8 [DOI] [PubMed] [Google Scholar]
- 15.European Commission. Commission Directive 2014/85/EU of 1 July 2014 amending Directive 2006/126/EC of the European Parliament and of the Council on driving licences (Text with EEA relevance). Date last accessed: September 2019; date last updated: 02 July 2014 https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32014L0085&from=EN
- 16.Bonsignore MR, Randerath W, Riha R, et al. . New rules on driver licensing for patients with obstructive sleep apnoea: EU Directive 2014/85/EU. Eur Respir J 2016; 47: 39–41. doi: 10.1183/13993003.01894-2015 [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd Edn Darien, IL, AASM, 2014. [Google Scholar]
- 18.Kushida CA, Littner MR, Morgenthaler T, et al. . Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 2005; 28: 499–521. doi: 10.1093/sleep/28.4.499 [DOI] [PubMed] [Google Scholar]
- 19.Berger M, Varvarigou V, Rielly A, et al. . Employer mandated sleep apnea screening and diagnosis in commercial drivers. J Occup Environ Med 2012; 54: 1017–1025. doi: 10.1097/JOM.0b013e3182572e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14: 540–545. doi: 10.1093/sleep/14.6.540 [DOI] [PubMed] [Google Scholar]
- 21.Gottlieb DJ, Whitney CW, Bonekat WH, et al. . Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Respir Crit Care Med 1999; 159: 502–507. doi: 10.1164/ajrccm.159.2.9804051 [DOI] [PubMed] [Google Scholar]
- 22.Kiciński P, Przybylska-Kuć SM, Tatara K, et al. . Reliability of the Epworth Sleepiness Scale and the Berlin Questionnaire for screening obstructive sleep apnea syndrome in the context of the examination of candidates for drivers. Med Pr 2016; 67: 721–728. doi: 10.13075/mp.5893.00494 [DOI] [PubMed] [Google Scholar]
- 23.Netzer NC, Stoohs RA, Netzer CM, et al. . Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999; 131: 485–491. doi: 10.7326/0003-4819-131-7-199910050-00002 [DOI] [PubMed] [Google Scholar]
- 24.Firat H, Yuceege M, Demir A, et al. . Comparison of four established questionnaires to identify highway bus drivers at risk for obstructive sleep apnea in Turkey. Sleep Biol Rhythm 2012; 10: 231–236. doi: 10.1111/j.1479-8425.2012.00566.x [DOI] [Google Scholar]
- 25.Popević MB, Milovanović A, Nagorni-Obradović L, et al. . Screening commercial drivers for obstructive sleep apnea: translation and validation of Serbian version of Berlin Questionnaire. Qual Life Res 2016; 25: 343–349. doi: 10.1007/s11136-015-1087-3 [DOI] [PubMed] [Google Scholar]
- 26.Chung F, Yegneswaran B, Liao P, et al. . STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008; 108: 812–821. doi: 10.1097/ALN.0b013e31816d83e4 [DOI] [PubMed] [Google Scholar]
- 27.Chung F, Subramanyam R, Liao P, et al. . High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br J Anaesth 2012; 108: 768–775. doi: 10.1093/bja/aes022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ozoh OB, Okubadejo NU, Akanbi MO, et al. . High risk of obstructive sleep apnea and excessive daytime sleepiness among commercial intra-city drivers in Lagos metropolis. Niger Med J 2013; 54: 224–229. doi: 10.4103/0300-1652.119607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ozder A, Gunay E, Huseyin Eker H, et al. . Excessive daytime sleepiness among Turkish public transportation drivers: a risk for road traffic accidents? Acta Med Mediterr 2014; 30: 1121. [Google Scholar]
- 30.Burns N. An integrative review of screening for obstructive sleep apnea in commercial vehicle drivers. Workplace Health Saf 2014; 62: 114–120. doi: 10.1177/216507991406200305 [DOI] [PubMed] [Google Scholar]
- 31.Popević MB, Milovanović A, Nagorni-Obradović L, et al. . Screening commercial drivers for obstructive sleep apnea: validation of STOP-Bang questionnaire. Int J Occup Med Environ Health 2017; 30: 751–761. [DOI] [PubMed] [Google Scholar]
- 32.Evans KA, Yap T, Turner B. Screening commercial vehicle drivers for obstructive sleep apnea: tools, barriers, and recommendations. Workplace Health Saf 2017; 65: 487–492. doi: 10.1177/2165079917692597 [DOI] [PubMed] [Google Scholar]
- 33.Marti-Soler H, Hirotsu C, Marques-Vidal P, et al. . The NoSAS score for screening of sleep-disordered breathing: a derivation and validation study. Lancet Respir Med 2016; 4: 742–748. doi: 10.1016/S2213-2600(16)30075-3 [DOI] [PubMed] [Google Scholar]
- 34.Coutinho Costa J, Rebelo-Marques A, Machado JN, et al. . Validation of NoSAS (Neck, Obesity, Snoring, Age, Sex) score as a screening tool for obstructive sleep apnea: analysis in a sleep clinic. Pulmonology 2019; 25: 263–270. doi: 10.1016/j.pulmoe.2019.04.004 [DOI] [PubMed] [Google Scholar]
- 35.US Preventive Services Task Force. Screening for obstructive sleep apnea in adults: US Preventive Services Task Force recommendation statement. JAMA 2017; 317: 407–414. doi: 10.1001/jama.2016.20325 [DOI] [PubMed] [Google Scholar]
- 36.Hartenbaum N, Collop N, Rosen IM, et al. . Sleep apnea and commercial motor vehicle operators: statement from the joint Task Force of the American College of Chest Physicians, American College of Occupational and Environmental Medicine, and the National Sleep Foundation. J Occup Environ Med 2006; 48: Suppl. 9, S4–37. doi: 10.1097/01.jom.0000236404.96857.a2 [DOI] [PubMed] [Google Scholar]
- 37. https://www.brit-thoracic.org.uk/quality-improvement/clinical-resources/sleep/ British Thoracic Society (BTS) Position Statement, 2014.
- 38.Colvin LJ, Collop NA. commercial motor vehicle driver obstructive sleep apnea screening and treatment in the United States: an update and recommendation overview. J Clin Sleep Med 2016; 12: 113–125. doi: 10.5664/jcsm.5408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ghosh D, Mackay TW, Riha RL. European Union directive 2014/85/EU on driver licensing in obstructive sleep apnoea: early experiences with its application in the UK. Breathe 2016; 12: e59–e63. doi: 10.1183/20734735.008016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.US Federal Register. Proposed recommendations on obstructive sleep apnea www.federalregister.gov/articles/ 2012/04/20/2012-9555/proposed-recommendations-on-obstructivesleep-apnea Date last updated: 20 April 2012. Date last accessed: 09 October 2019.
- 41.Hawkins MR, Durowoju R, Havlichek D, et al. . Sleep apnea screening practices during department of transportation medical examinations. J Occup Environ Med 2017; 59: 966–973. doi: 10.1097/JOM.0000000000001098 [DOI] [PubMed] [Google Scholar]
- 42.Slater G, Steier J. Excessive daytime sleepiness in sleep disorders. J Thorac Dis 2012; 4: 608–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ghosh D, Jamson SL, Baxter PD, et al. . Continuous measures of driving performance on an advanced office-based driving simulator can be used to predict simulator task failure in patients with obstructive sleep apnoea syndrome. Thorax 2012; 67: 815–821. doi: 10.1136/thoraxjnl-2011-200699 [DOI] [PubMed] [Google Scholar]
- 44.Collop NA, Anderson WM, Boehlecke B, et al. . Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 2007; 3: 737–747. doi: 10.5664/jcsm.27032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang C, Berger M, Malhotra A, et al. . Portable diagnostic devices for identifying obstructive sleep apnea among commercial motor vehicle drivers: considerations and unanswered questions. Sleep 2012; 35: 1481–1489. doi: 10.5665/sleep.2194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lyons MM, Kraemer JF, Dhingra R, et al. . Screening for obstructive sleep apnea in commercial drivers using EKG-derived respiratory power index. J Clin Sleep Med 2019; 15: 23–32. doi: 10.5664/jcsm.7562 [DOI] [PMC free article] [PubMed] [Google Scholar]