Abstract
Background
Recurrent apnea is common in preterm infants particularly at very early gestational ages. These episodes of loss of effective breathing can lead to hypoxemia and bradycardia, which may be severe enough to require resuscitation including use of positive pressure ventilation or other treatments. Physical stimulation is often used to restart breathing and it is possible that repeated kinesthetic stimulation might be used to treat infants with apnea and prevent its consequences.
Objectives
To determine the effect of kinesthetic stimulation on apnea and bradycardia, the use of mechanical ventilation or continuous positive airways pressure, and neurodevelopmental disability in preterm infants with apnea.
Search methods
The standard search strategy of the Cochrane Neonatal Review Group was used. An updated search was performed in October 2009 of MEDLINE and PREMEDLINE, EMBASE, CINAHL and CENTRAL (The Cochrane Library).
Selection criteria
All trials using random or quasi‐random patient allocation that compared kinesthetic stimulation to placebo or no treatment in preterm infants with apnea of prematurity.
Data collection and analysis
Standard methods of the Cochrane Collaboration and its Neonatal Review Group were used. As all three included trials were crossover trials, the data were extracted from all exposure periods and combined where appropriate.
Main results
Three crossover studies (Korner 1978; Tuck 1982; Jirapaet 1993) were identified that compared a form of kinesthetic stimulation to control for the treatment of apnea of prematurity. No study reported a clinically important reduction (> 50%) in apnea. Using a lower threshold (> 25%), Korner 1978 reported less apnea and bradycardia in infants while on an oscillating water bed. Tuck 1982 demonstrated a reduction in frequency of apneas (> 12 seconds) associated with bradycardia (< 100 bpm), apneas associated with hypoxia (TcP02 < 50 mmHg), and apneas requiring stimulation in infants on a rocking bed. Individual patient data were not available from the author to determine if there was an important reduction in clinical apnea. No outcome could be extracted from the study using a 'vertical pulsating stimulus' by Jirapaet 1993 that was consistent with the definition of clinically important apnea. Jirapaet 1993 reported no infants required resuscitation or ventilation. Adverse events such as death, intraventricular hemorrhage and neurodevelopmental disability were not reported.
Authors' conclusions
There is insufficient evidence to recommend kinesthetic stimulation as treatment for clinically significant apnea of prematurity. Previous reviews have suggested that kinesthetic stimulation is not effective at preventing apnea of prematurity (Henderson‐Smart 2005) and is not as effective as theophylline at treating clinically significant apnea of prematurity (Osborn 2005).
Plain language summary
Kinesthetic stimulation for treating apnea in preterm infants
Rocking therapy and physical stimulation have been advocated to assist preterm infants to breathe regularly and some have been designed to mimic in utero movements. A pause in breathing (apnea) is common in very preterm infants but it can lead to a lack of oxygen in the blood, so that the infant needs resuscitation and assisted ventilation. Pauses in breathing could also affect brain development and proper functioning of other organs. Physical stimulation is recognised as a means to wake up preterm infants who then start breathing on their own. Three controlled studies have used different gentle rocking motions (irregularly oscillating water beds, regularly rocking bed trays or a vertical pulsating stimulus) to reduce the occurrence of apnea in a total of 49 babies. However, there was no clinically useful reduction of periods of apnea, although only a small number of infants were studied. Shorter breathing pauses were reported to be reduced by one study but it is not thought to be clinically important. No harm has reported to be done to the preterm infants with these interventions.
Background
Description of the condition
Apnea in infants has been defined as a pause in breathing of greater than 20 seconds or an apneic event less than 20 seconds associated with bradycardia and/or cyanosis (Nelson 1978). Recurrent episodes of apnea are common in preterm infants and the incidence and severity increases at lower gestational ages. Although apnea can occur spontaneously and be attributed to prematurity alone, it can also be provoked or made more severe if there is some additional insult such as infection, hypoxemia or intracranial pathology (Henderson‐Smart 1995).
Description of the intervention
Various treatments for apnea in preterm infants have been used, including physical stimulation by nursing staff, pharmacological stimulation including methylxanthines (HendersonSmart 2005b) and continuous positive airway pressure (CPAP) (HendersonSmart 2005b). Kinesthetic stimulation using various forms of oscillating mattress has been used for prevention of apnea, and compared to use of methylxanthines which are the subject of other Cochrane reviews (Osborn 2005; Henderson‐Smart 2005). This review examines the effects of kinesthetic stimulation for treatment of apnea in preterm infants.
How the intervention might work
Physical stimulation by nursing staff is commonly used to arouse the apneic infant and so stimulate breathing. This raises the question of whether frequent physical stimuli might reduce the number of apneic events. Furthermore, some believe that the preterm infant is deprived of the frequent stimuli that would be felt in utero and that substituting these with an oscillating mattress to provide kinesthetic stimulation might improve growth and development.
Why it is important to do this review
If prolonged, apnea can lead to hypoxemia and reflex bradycardia which may require active resuscitative efforts to reverse. There are clinical concerns that these episodes might be harmful to the developing brain or cause dysfunction of the gut or other organs. Frequent episodes may be accompanied by respiratory failure of sufficient severity as to lead to intubation and the use of intermittent positive pressure ventilation (IPPV).
Objectives
To determine the effect of kinesthetic stimulation on apnea and bradycardia, the use of mechanical ventilation or continuous positive airways pressure (CPAP), and neurodevelopmental disability in preterm infants with apnea.
Methods
Criteria for considering studies for this review
Types of studies
All trials using random or quasi‐random patient allocation were included. Crossover trials were included.
Types of participants
Preterm infants with recurrent clinical apnea with or without associated bradycardia, cyanosis or hypoxia.
Types of interventions
Kinesthetic stimulation (various forms of oscillating mattresses or other repetitive stimulation involving moving the baby) used as treatment for apnea of prematurity compared to placebo or no treatment.
Types of outcome measures
Measures of severity of apnea as well as the response to treatment must be consistent with an evaluation of 'clinical apnea' as defined by the American Academy of Pediatrics (see above). A reduction in the frequency of 'clinical apnea' that might be expected to affect clinical practice is taken as a greater than 50% reduction in the frequency of 'clinical apnea' compared to the control.
Primary outcomes
1) Persisting apneas +\‐ bradycardia; 2) Mean rates of apnea/bradycardia; 3) Death before hospital discharge;
Secondary outcomes
4) Hypoxemic episodes associated with apnea; 5) Failure of treatment as indicated by use of additional measures such as use of pharmacological stimulation, IPPV or CPAP; 6) Rate of intraventricular haemorrhage; 7) Neurodevelopmental status at follow up.
Search methods for identification of studies
Electronic searches
The search was updated October 2009 including searches of CENTRAL (The Cochrane Library, Issue 4, 2009), EMBASE, MEDLINE, PREMEDLINE and CINAHL, supplemented by searches of abstracts of the Society for Pediatric Research that were hand searched for the years 2005 to 2009 inclusive and the Perinatal Society of Australia and New Zealand years 2000 to 2009.
An updated search was performed of MEDLINE and PREMEDLINE, EMBASE, CINAHL and CENTRAL in October 2009 using the search terms ['kinesthetic or (water bed) or (air bed) or oscillating or rocking or (vertical pulsating)] and [infant or neonat*] and [apnoea or apnea].
Original search: The standard search strategy of the Cochrane Neonatal Review Group was used. This included searches of the Oxford Database of Perinatal Trials, Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 4, 2004), MEDLINE (1966‐December 2004), EMBASE (1966 to December 2004) and CINAHL (1982 to December 2004) were searched. Abstracts of the Society for Pediatric Research were hand searched for the years 1996 to 2004 inclusive.
The Cochrane Controlled Trials Register was searched using search terms 'kinesthetic', 'water bed', 'air bed', 'oscillating', '(apnoea or apnea) and (infant or preterm or neonate or newborn)', 'rocking', and 'vertical pulsating'.
MEDLINE was searched using MeSH headings 'apnea and infant‐premature'; and text words 'kinesthetic', 'water bed', 'air bed', 'oscillating', '(apnea or apnoea) and (infant or preterm or neonate or newborn)', 'rocking', and 'vertical pulsating'.
The Oxford Database of Perinatal Trials was searched using search term 'apnea'.
Searching other resources
Additional searches were performed of previous reviews including cross references, abstracts, conferences and symposia proceedings, expert informants, and journal hand searching mainly in the English language. Abstracts of the Society for Pediatric Research were hand searched for the years 1996 to 2004 inclusive.
An updated search was performed of abstracts of the Pediatric Academic Society Conferenceand Perinatal Society of Australia and New Zealand (2005 to 2009).
Data collection and analysis
Standard methods of the Cochrane Collaboration and its Neonatal Review Group were used.
Selection of studies
Trial eligibility was assessed independently by both review authors. DIfferences were resolved through consensus.
Data extraction and management
Each author extracted the data separately into a standard data table and then compared and resolved differences. Trial details were entered into 'table of included studies' and data into 'data and analyses' using REVMAN software.
Assessment of risk of bias in included studies
The methodological quality of each trial was reviewed by the second author blinded to trial authors and institution(s). Studies were assessed for selection bias (blinding of randomisation), performance bias (blinding of intervention), attrition bias (complete follow‐up), and detection bias (blinding of outcome measurement). Each criterion were characterized as Yes, Can’t tell, No. This information was added to the Characteristics of Included Studies Table.
In addition, the following issues were evaluated and entered into the Risk of Bias table:
1. Sequence generation: Was the allocation sequence adequately generated?
2. Allocation concealment: Was allocation adequately concealed?
3. Blinding of participants, personnel and outcome assessors: Was knowledge of the allocated intervention adequately prevented during the study? At study entry? At the time of outcome assessment?
4. Incomplete outcome data: Were incomplete outcome data adequately addressed?
5. Selective outcome reporting: Are reports of the study free of suggestion of selective outcome reporting?
6. Other sources of bias: Was the study apparently free of other problems that could put it at a high risk of bias?
Measures of treatment effect
The standard methods of the Neonatal Review Group were followed. Statistical analyses were performed using Review Manager software (RevMan5, Cochrane Collaboration). Categorical data were analyzed using relative risk (RR), risk difference (RD) and the number needed to treat (NNT). Continuous data were analyzed using weighted mean difference (WMD). The 95% Confidence interval (CI) was reported on all estimates. As all three trials were crossover trials, the data were extracted from all exposure periods and combined where appropriate.
Unit of analysis issues
The unit of analysis was intended to be the unit of randomisation. For crossover trials, the data were extracted from all exposure periods and combined where appropriate.
Dealing with missing data
Authors of studies with missing data were contacted.
Assessment of heterogeneity
We examined heterogeneity between trials by inspecting the forest plots and quantifying the impact of heterogeneity using the I‐squared statistic.
Data synthesis
If multiple studies were identified and meta‐analysis was judged to be appropriate, meta‐analysis was performed using RevMan5. For estimates of typical relative risk and risk difference, we used the Mantel‐Haenszel method. For measured quantities, we used the inverse variance method. All meta‐analyses were done using the fixed effect model.
Results
Description of studies
Update 2009: No new eligible studies were found.
Ten trials were identified, seven of which failed to meet inclusion criteria (see table 'Characteristics of Excluded Studies'). Three trials were included (Korner 1978; Tuck 1982; Jirapaet 1993) that compared a form of kinesthetic stimulation to control for the treatment of apnea of prematurity. Details of each study have been entered into the table of included studies. All three studies enrolled preterm infants with established apnea with exclusion of secondary causes, and not currently on any treatment with a respiratory stimulant. In the study by Korner 1978, it was unclear as to how many apneas were required to be eligible for enrolment. In the study by Tuck 1982, infants were eligible if they had > 2 apneas in 24 hours. In the study by Jirapaet 1993, infants were eligible if they had > 3 apneas within six hours.
All three studies were crossover trials with alternating periods of treatment and control in the infants studied. Tuck 1982 is a two‐period crossover trial, whereas Korner 1978 and Jirapaet 1993 were multiple crossover trials, each studying four consecutive alternating periods.
The type of kinesthetic stimulation differed between the three trials. Korner 1978 examined the effect of an irregularly oscillating water bed (12 to 14/min); Tuck 1982 examined the effect of a regularly rocking bed tray (10 to 22/min); and Jirapaet 1993 examined the effect of a 'vertical pulsating stimulus' (blood pressure cuff placed under the thorax inflated 12 to 20/min).
Apnea and bradycardia were recorded by nursing staff (monitors set for apnea >20 seconds duration and bradycardia < 80 bpm) and by polygraphic recording of apnea (>10 seconds) and bradycardia (< 80 bpm) in the study by Korner 1978. Apnea (> 12 seconds), bradycardia (< 100 bpm) and transcutaneous oxygen were recorded by polygraphic recording (with the researcher at the bedside) in the study by Tuck 1982. Apnea and bradycardia were recorded by nursing staff (monitors set for apnea > 15 seconds and bradycardia < 100 bpm), and by polygraphic recording (apnea > 15 seconds and bradycardia < 100 bpm) in the study by Jirapaet 1993.
Data could be extracted only from the study by Korner 1978 to calculate the number of apneas (> 20 seconds) in 24 hours.
Risk of bias in included studies
Details of the methodological quality of each trial are given in the table 'Characteristics of Included Studies' and 'Risk of Bias' table.
Allocation
All three trials were crossover trials, with Tuck 1982 using a two‐period crossover, and Korner 1978 and Jirapaet 1993 using multiple crossover periods. In two trials there was random order of treatment (Tuck 1982; Jirapaet 1993). In the third trial (Korner 1978) the method of allocation was unclear. Tuck 1982 used a coin toss to determine order (letter from author), but the actual methods of randomization or alternation were unclear in the other two studies.
Blinding
Due to the nature of the treatments, blinding of intervention was not possible in any of the studies.
Polygraphic recordings, but not nursing documented apnea and bradycardia, were assessed blindly in the study by Jirapaet 1993. Blinding of the assessment of polygraphic recordings was unclear in the study by Tuck 1982. Nursing documented apnea and bradycardia was not blinded in the study by Korner 1978.
Incomplete outcome data
All studies had complete follow‐up of enrolled infants.
Effects of interventions
See 'summary of analyses'.
Clinically significant reductions in apnea: No study reported a clinically significant reduction in apnea consistent with the prespecified criteria in this review. For apnea > 20s, Korner 1978 using the oscillating water bed reported no significant difference in number of infants with > 4 / day or > 9 / day (Outcomes 1.1, 1.2). For apnea associated with bradycardia, Korner 1978 reported no significant difference in number of infants with > 4 / day or > 9 apneas / day (Outcomes 1.3, 1.4). For apnea associated with bradycardia, Korner 1978 reported no significant difference in the number of infants having a < 50% reduction in frequency of apnea (Outcome 1.5). Tuck 1982 using the rocking bed reported frequency of apneas (> 12 seconds) associated with bradycardia (< 100 bpm), number of apneas associated with hypoxia (TcP02 < 50 mmHg), and number of apneas requiring stimulation in infants on the rocking bed. However, the events for individual patients were combined and individual patient data were not available from the author to determine if there was an important reduction in clinical apnea.
Other reported apnea: Using a lower threshold (> 25% reduction), Korner 1978 reported less apnea and bradycardia in infants on the oscillating water bed (RR 0.14, 95% CI 0.02, 0.91) (Outcome 1.6). For apnea associated with bradycardia, both Korner 1978 and Tuck 1982 found significant reductions in the number of infants with more frequent episodes. Tuck 1982 reported reductions in the frequency of apneas (> 12 seconds) associated with bradycardia (< 100 bpm) whereas Korner 1978 reported apnea >15s associated with bradycardia <80bpm / day. Meta‐analysis of these two studies found a significant reduction in the number of infants with more frequent episodes (RR 0.11, 95% CI 0.03, 0.42) (Outcome 1.7). No outcome could be extracted from the study using the 'vertical pulsating stimulus' by Jirapaet 1993 that was consistent with the definition of clinically important apnea. Jirapaet 1993 reported the number of episodes of apnea > 15s / day and found a significant reduction (MD ‐15.78, 95% CI ‐21.20, ‐10.36) in infants whilst receiving the 'vertical pulsating stimulus' (Outcome 1.8). Korner 1978 reported the number of episodes of apnea >15s associated with bradycardia < 80 bpm / day and found no significant difference (Outcome 1.9). Tuck 1982 reported a significant reduction in apnea > 12s associated with hypoxia (TcO2 < 50 mmHg) (RR 0.13, 95% CI 0.02, 0.85) (Outcome 1.10), but no significant difference in the frequency of apnea requiring stimulation (RR 0.20, 0.03, 1.47) (Outcome 1.11).
Other events: Jirapaet 1993 reported that no infants required resuscitation or ventilation in either group. Adverse events such as death, intraventricular haemorrhage and neurodevelopmental follow‐up were not reported.
Discussion
Summary of main results
There is no evidence from these studies that kinesthetic stimulation is effective in producing a clinically important reduction in clinically important apnea of prematurity (> 20 seconds duration or a shorter apnea associated with bradycardia or cyanosis), or in reducing clinically important outcomes such as need for IPPV, CPAP or respiratory stimulants.
However, using a lower threshold that has uncertain clinical significance, the trials indicate that kinesthetic stimulation reduces the rates of apnea (with or without associated bradycardia and hypoxia) in infants with apnea of prematurity. The results were consistent despite the use of three different methods of providing kinesthetic stimulation.
This review suggests that kinesthetic stimulation is effective at reducing apnea and bradycardia in infants with apnea of prematurity. Whether it produces a clinically important reduction in clinical apnea of prematurity remains unproven. Previous reviews have suggested that kinesthetic stimulation is not effective at preventing apnea of prematurity (Henderson‐Smart 2005) and is not as effective as theophylline in treating clinically significant apnea of prematurity (Osborn 2005).
Overall completeness and applicability of evidence
Because of the small number of infants enrolled in the three trials included in this review, measures of effect are imprecise and a small benefit of kinesthetic stimulation in reducing clinically important apnea is not precluded. The three trials used different methods of kinesthetic stimulation, and different definitions for apnea and bradycardia.
Quality of the evidence
The limitations of the studies included in this review are their small sample size (the three eligible trials included only 49 babies in total) and the use of a crossover design which removes the ability to measure effects on late outcomes.
Potential biases in the review process
This review is hindered by the clinical heterogeneity of the eligible trials, which limits the ability to synthesize their results. It has not been possible for the reviewers to obtain individual patient data or dichotomous data for some clinically important outcomes. These would be needed for synthesis of data on these outcomes.
Authors' conclusions
Implications for practice.
There is insufficient evidence to recommend kinesthetic stimulation as treatment for clinically important apnea of prematurity.
Implications for research.
A further trial of kinesthetic stimulation compared to control using clinically important outcomes and with adequate power is required before kinesthetic stimulation can be recommended to treat clinically important apnea with or without bradycardia.
What's new
| Date | Event | Description |
|---|---|---|
| 27 October 2009 | New search has been performed | This updates the review "Kinesthetic stimulation for treating apnea in preterm infants" published in The Cochrane Library, Issue 1, 2002 (Osborn 2002). No new eligible studies found in an updated search October 2009. |
History
Protocol first published: Issue 4, 1997 Review first published: Issue 1, 1999
| Date | Event | Description |
|---|---|---|
| 15 October 2008 | Amended | Converted to new review format. |
| 1 December 2004 | New search has been performed | This review updates the existing review of 'Kinesthetic stimulation for treating apnea in preterm infants' published in The Cochrane Library, Issue 1, 1999 and previously updated in Issue 2, 2002. No additional studies or data were found on the updated search to December 2004. |
| 2 February 2002 | New search has been performed | This review updates the existing review of 'Kinesthetic stimulation for treating apnea in preterm infants' published in The Cochrane Library, Issue 1, 1999. In the current update, we considered for inclusion several additional studies of kinesthetic stimulation in preterm infants, but found them not to be eligible. This was usually because apnea was not an outcome reported, or the study was not a randomized or quasi‐randomized trial. Thus, there is no change to the conclusion that there is insufficient evidence to recommend kinesthetic stimulation as treatment for clinically important apnea of prematurity |
Acknowledgements
Dr Tuck provided information about the methods of his study.
The Cochrane Neonatal Review Group has been funded in part with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN267200603418C.
Data and analyses
Comparison 1. Kinesthetic stimulation vs control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Apnea (>20s) > 4/day | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.69, 1.45] |
| 2 Apnea (>20s) > 9/day | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.53, 1.38] |
| 3 Apnea and bradycardia > 4/day | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.63, 1.23] |
| 4 Apnea and bradycardia > 9/day | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.49, 1.18] |
| 5 < 50 % reduction in frequency of apnea/bradycardia | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.49, 1.18] |
| 6 < 25% reduction in frequency of apnea/bradycardia | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 0.91] |
| 7 Apnea / bradycardia more frequent | 2 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.03, 0.42] |
| 8 Episodes of central apnea > 15 seconds (number/day) | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | ‐15.78 [‐21.20, ‐10.36] |
| 9 Episodes of apnea > 15s & bradycardia < 80 (number/day) | 1 | 16 | Mean Difference (IV, Fixed, 95% CI) | ‐9.42 [‐20.77, 1.93] |
| 10 More frequent apnea with hypoxia (TcO2<50mmHg) | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.02, 0.85] |
| 11 More frequent apnea requiring stimulation | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.03, 1.47] |
| 12 Use of IPPV or CPAP | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Need for resuscitation for apnea | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
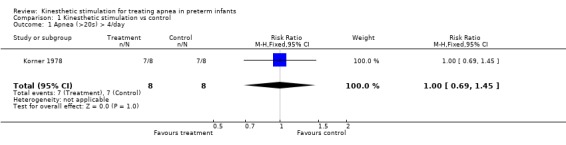
Comparison 1 Kinesthetic stimulation vs control, Outcome 1 Apnea (>20s) > 4/day.
1.2. Analysis.
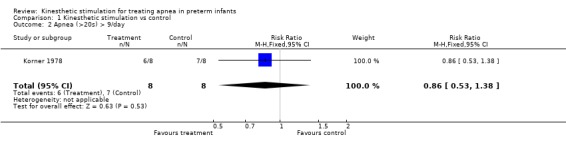
Comparison 1 Kinesthetic stimulation vs control, Outcome 2 Apnea (>20s) > 9/day.
1.3. Analysis.
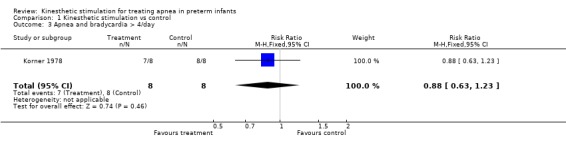
Comparison 1 Kinesthetic stimulation vs control, Outcome 3 Apnea and bradycardia > 4/day.
1.4. Analysis.
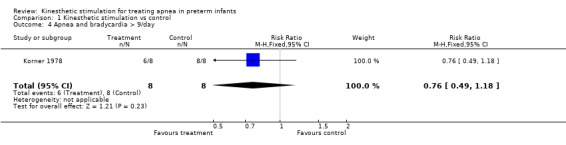
Comparison 1 Kinesthetic stimulation vs control, Outcome 4 Apnea and bradycardia > 9/day.
1.5. Analysis.
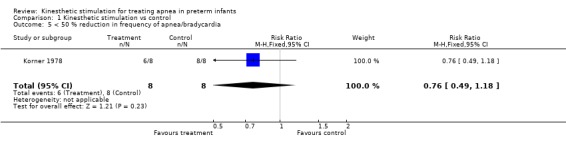
Comparison 1 Kinesthetic stimulation vs control, Outcome 5 < 50 % reduction in frequency of apnea/bradycardia.
1.6. Analysis.
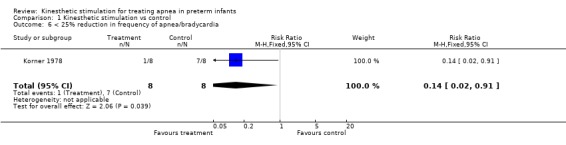
Comparison 1 Kinesthetic stimulation vs control, Outcome 6 < 25% reduction in frequency of apnea/bradycardia.
1.7. Analysis.
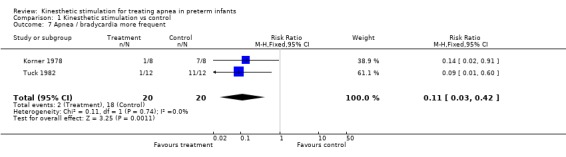
Comparison 1 Kinesthetic stimulation vs control, Outcome 7 Apnea / bradycardia more frequent.
1.8. Analysis.
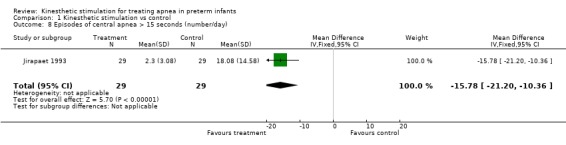
Comparison 1 Kinesthetic stimulation vs control, Outcome 8 Episodes of central apnea > 15 seconds (number/day).
1.9. Analysis.
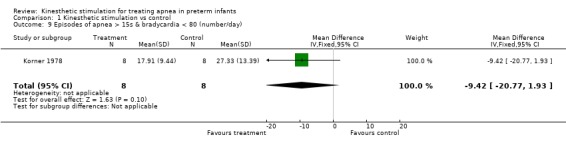
Comparison 1 Kinesthetic stimulation vs control, Outcome 9 Episodes of apnea > 15s & bradycardia < 80 (number/day).
1.10. Analysis.
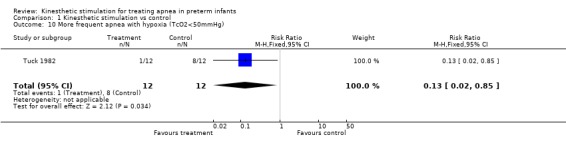
Comparison 1 Kinesthetic stimulation vs control, Outcome 10 More frequent apnea with hypoxia (TcO2<50mmHg).
1.11. Analysis.
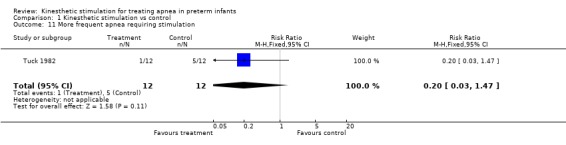
Comparison 1 Kinesthetic stimulation vs control, Outcome 11 More frequent apnea requiring stimulation.
1.12. Analysis.
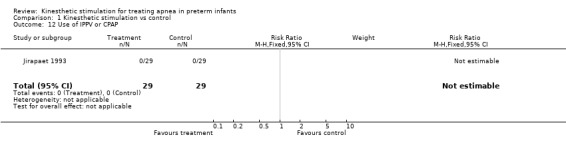
Comparison 1 Kinesthetic stimulation vs control, Outcome 12 Use of IPPV or CPAP.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jirapaet 1993.
| Methods | Multiple crossover trial with randomized order of treatment. Single center. | |
| Participants | Preterm infants with > 2 apneas in 24 hours (n = 29). 29 ‐ 34 weeks gestation (mean 32.3 weeks). Birth weight 890‐2300g (mean 1474 g). Age day 2 ‐ 13 (mean 4.4 days). Secondary causes of apnea excluded. No respiratory stimulant or ventilator support. | |
| Interventions | Multiple crossover trial with four equal, alternate 6 hour periods of "Vertical pulsating stimulus" ( inflating BP cuff placed under thorax) at 12 ‐ 20 cycles per minute, and alternate period of no 'VPS'. | |
| Outcomes | Polygraphic recorded apnea >15 seconds and bradycardia < 100 bpm. Type of apnea (mixed, central and obstructive). Use of IPPV. Need for resuscitation. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Method not stated. |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? Treatment | High risk | Not possible. |
| Blinding? All outcomes | Low risk | |
| Incomplete outcome data addressed? All outcomes | Low risk | No losses. |
Korner 1978.
| Methods | Multiple crossover trial of kinesthetic treatment. Single center trial. | |
| Participants | Preterm infants with apnea (n = 8). Gestation 27 ‐ 32 weeks (mean 30 weeks). Birth weight 1072 ‐ 1650 g (mean 1270 g). Age 7 ‐ 28 days (mean day 15). No oxygen therapy, no medications and secondary causes of apnea excluded. | |
| Interventions | Multiple crossover design with four equal, alternate 6 hour periods of irregularly oscillating water bed 12 ‐ 14 cycles per minute, and non‐oscillating water bed. | |
| Outcomes | Nursing recorded apnea/bradycadia (monitor alarms for apnea > 20 seconds and bradycardia <80 bpm). Polygraphic recorded apnea >10 seconds with bradycardia (moderate 80 ‐ 120 bpm, severe <80bpm). Duration and distribution of sleep and wake cycles. | |
| Notes | Criteria for frequency and severity of apnea for enrolment not stated. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Possibly quasi‐random with alternation of first exposure. |
| Allocation concealment? | Unclear risk | B ‐ Unclear. |
| Blinding? Treatment | High risk | Not possible. |
| Blinding? All outcomes | High risk | No for nursing observations of apnea/bradycardia. Not clear for polygraphic recording. |
| Incomplete outcome data addressed? All outcomes | Low risk | No losses. |
Tuck 1982.
| Methods | Two‐period crossover trial with randomized order of treatment. Single center study. | |
| Participants | Preterm infants with > apneas in 24 hours (n = 12). Gestation 26 ‐ 32 weeks (mean 29.5). Birth weight 800 ‐ 1700 g (mean 1210 g). Age 2 ‐ 45 days (mean 14 days). Four in oxygen, no theophylline, no secondary cause of apnea. | |
| Interventions | Single crossover with two consecutive, equal alternate 4 ‐ 8 hour periods of regularly rocking bed (using bellows under the tray) at 10 ‐ 22 cycles per minute, and non‐rocking bed. | |
| Outcomes | Polygraphic recorded apnea (> 12 seconds), bradycardia (< 100 bpm) and transcutaneous oxygen concentration. Need for stimulation. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | 'tossing a coin'. |
| Allocation concealment? | Unclear risk | Unclear. |
| Blinding? Treatment | High risk | Not possible. |
| Blinding? All outcomes | High risk | Observer at bedside. |
| Incomplete outcome data addressed? All outcomes | Low risk | No losses. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Frank 1973 | Reported 11 methods of stimulating infants with apnea. Stimulus only applied during apnea. |
| Garcia 1993 | Randomised crossover trial. Ineligible comparison. Compared tactile (moderate shaking of the leg) to taste stimulation of infants with apnea. |
| Groswasser 1995 | Crossover study using a rocking mattress in infants at 39 weeks postmentrual age with obstructive sleep apnea. |
| Kattwinkel 1975 | Ineligible comparison of kinesthetic stimulation and CPAP in preterm infants with apnea. Kinesthetic stimulation given by rubbing the extremeties for 5 out every 15 minute period for total of 3 hours. Method of allocation to treatment not stated. |
| Korner 1981 | Study abandoned. Data incomplete. |
| Lovell 1999 | Randomised study of vibrotactile stimulation of preterm infants with apnea. Excess losses as only one of 7 infants randomised had apnea. |
| Svenningsen 1995 | Historical controls used. |
Contributions of authors
DO and DHS performed all aspects of the review and review updates collaboratively. Eligibility, critical appraisal and data extraction were performed independently by both reviewer authors with differences resolved by consensus.
Sources of support
Internal sources
NSW Centre for Perinatal Health Services Research, University of Sydney, Australia.
Department of Neonatal Medicine, Royal Prince Alfred Hospital, Sydney, Australia.
External sources
No sources of support supplied
Declarations of interest
None.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Jirapaet 1993 {published data only}
- Jirapaet V, Subramanian KNS. The effect of vertical pulsating stimulus on apnea of prematurity. Journal of the Medical Association of Thailand 1993;76:319‐26. [PubMed] [Google Scholar]
Korner 1978 {published data only}
- Korner AF, Guilleminault C, Hoed J, Baldwin RB. Reduction of sleep apnea and bradycardia in preterm infants on oscillating water beds: a controlled polygraphic study. Pediatrics 1978;61:528‐33. [PubMed] [Google Scholar]
Tuck 1982 {published and unpublished data}
- Tuck SJ, Monin P, Duvivier C, May T, Vert P. Effect of a rocking bed on apnoea of prematurity. Archives of Disease in Childhood 1982;57:475‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Frank 1973 {published data only}
- Frank UA, Bordiuk JM, Borromeo‐McGrail V, Saltzman MB, Keitel HG. Treatment of apnea in neonates with an automated monitor‐actuated apnea arrestor. Pediatrics 1973;51:878‐83. [PubMed] [Google Scholar]
Garcia 1993 {published data only}
- Garcia AP, White‐Traut R. Preterm infants' responses to taste/smell and tactile stimulation during an apneic episode. Journal of Pediatric Nursing 1993;8:245‐52. [PubMed] [Google Scholar]
Groswasser 1995 {published data only}
- Groswasser J, Sottiaux M, Rebuffat E, Simon T, Vandeweyer M, Kelmanson I, Blum D, Kahn A. Reduction in obstructive breathing events during body rocking: a controlled polygraphic study in preterm and full‐term infants. Pediatrics 1995;96:64‐8. [PubMed] [Google Scholar]
Kattwinkel 1975 {published data only}
- Kattwinkel J, Nearman HS, Fanaroff AA, Katona PG, Klaus MH. Apnea of prematurity. Comparative therapeutic effects of cutaneous stimulation and nasal continuous positive airway pressure. Journal of Pediatrics 1975;86:588‐92. [DOI] [PubMed] [Google Scholar]
Korner 1981 {published data only}
- Korner AF. What we don't know about water beds and apneic preterm infants [letter]. Pediatrics 1981;68:306‐7. [PubMed] [Google Scholar]
Lovell 1999 {published data only}
- Lovell JR, Eisenfeld L, Rosow E, Adam J, Lapin C, Bronzino JD. Vibrotactile stimulation for treatment of neonatal apnea: a preliminary study. Connecticut Medicine 1999;63:323‐5. [PubMed] [Google Scholar]
- Lovell JR, Eisenfeld L, Rosow E, Adam J, Lapin C, Bronzino JD. Vibrotactile stimulation for treatment of neonatal apnea: a preliminary study. Neonatal Intensive Care 1999;12:36‐7, 39‐41. [PubMed] [Google Scholar]
Svenningsen 1995 {published data only}
- Svenningsen NW, Wittstrom C, Hellstrom‐Westas L. OSCILLO‐oscillating air mattress in neonatal care of very preterm babies. Technology and Health Care 1995;3:43‐6. [PubMed] [Google Scholar]
Additional references
Henderson‐Smart 1995
- Henderson‐Smart DJ. Recurrent apnoea. In: Ed Yu VYH editor(s). Bailliere's Clinical Paediatrics. Vol. 3 No. 1 Pulmonary Problems in the Perinatal Period and their Sequelae, London: Bailliere Tindall, 1995:203‐22. [Google Scholar]
Henderson‐Smart 2005
- Henderson‐Smart DJ, Osborn DA. Kinesthetic stimulation for preventing apnea in preterm infants. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD000373] [DOI] [PubMed] [Google Scholar]
HendersonSmart 2005a
- Henderson‐Smart DJ, Steer P. Methylxanthine treatment for apnea in preterm infants. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD000140] [DOI] [Google Scholar]
HendersonSmart 2005b
- Henderson‐Smart DJ, Subramaniam P, Davis PG. Continuous positive airway pressure versus theophylline for apnea in preterm infants. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD001072] [DOI] [PubMed] [Google Scholar]
Nelson 1978
- Nelson NM. Members of the Task Force on rolonged Apnea of the American Academy of Pediatrics. Prolonged apnea. Pediatrics 1978;61:651‐2. [PubMed] [Google Scholar]
Osborn 2005
- Osborn DA, Henderson‐Smart DJ. Kinesthetic stimulation vs theophylline for apnea in preterm infants. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD000502] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Osborn 1999
- Osborn DA, Henderson‐Smart DJ. Kinesthetic stimulation for treating apnea in preterm infants. Cochrane Database of Systematic Reviews 1999, Issue 1. [DOI: 10.1002/14651858.CD000499] [DOI] [PMC free article] [PubMed] [Google Scholar]
Osborn 2002
- Osborn DA, Henderson‐Smart DJ. Kinesthetic stimulation for treating apnea in preterm infants. Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD000499] [DOI] [PMC free article] [PubMed] [Google Scholar]


