Abstract
Missed nursing care is an important measure of nursing care quality that is sensitive to nurse staffing and is associated with patient outcomes in medical-surgical and pediatric inpatient settings. Missed nursing care during labor and birth has not been studied, yet childbirth represents the most common reason for hospitalization in the United States. The Missed Nursing Care (MISSCARE) Survey, a measure of medical-surgical nursing quality with substantial evidence for validity and reliability, was adapted to maternity nursing care using data from focus groups of labor nurses, physicians, and new mothers and an on-line survey of labor nurses. Content validity was evaluated via participant feedback, and exploratory factor analysis was performed to identify the factor structure of the instrument. The modified version, the Perinatal Missed Care Survey, appears to be a feasible and promising instrument with which to evaluate missed nursing care of women during labor and birth in hospitals.
Keywords: nursing care, maternity nursing, psychometrics, survey methodology
Precis
The Perinatal Missed Care Survey appears to be a feasible and promising instrument with which to evaluate missed nursing care of women during labor and birth.
Childbirth is the most frequent reason for admission to hospitals in the United States (McDermott, Elixhauser, & Sun, 2017), and nearly 4 million births occur each year (Martin, Hamilton, Osterman, Driscoll, & Drake, 2018) in more than 3000 hospitals (Simpson, 2011). Pregnancy, childbirth, and newborn care account for almost one-fourth of annual U.S. hospitalizations (McDermott et al., 2017), yet associations among the quality and amount of maternity nursing care and specific outcomes for mothers and newborns have not been well studied. Research on maternity nursing care and nurse staffing in the inpatient setting relative to patient outcomes is limited.
During the last decade, several teams of nurse researchers have studied nurse staffing in the non-maternity acute care setting using the concept of missed nursing care (Ball et al., 2016, 2018; Kalisch, Gosselin, & Choi, 2012; Kalisch, Landstrom, & Hinshaw, 2009; Kalisch, Landstrom, & Williams, 2009; Kalisch & Lee, 2012; Kalisch, McLaughlin, & Dabney, 2012; Kalisch, Tschannen, & Lee, 2011, 2012; Lake et al., 2017; Lake, Germack, & Viscardi, 2016; Tubbs-Cooley et al., 2017). As concluded by Griffiths et al. (2018) in their systematic review, results of these investigations have made important contributions to the study of adequacy of nurse staffing as it affects the work of nurses who provide direct patient care and associated outcomes such as patient falls, medication errors, pressure ulcers, hospital readmissions, and patient satisfaction among medical-surgical patients. Researchers have used various terms to describe the scenario in which nurses are too busy or units are too short-staffed for nurses to do all that is required to provide safe and effective care for their patients. These terms include missed care, care omissions, care left undone, and care rationing. These terms apply to nursing care that is not done at all, partially done, or significantly delayed.
Background
Kalisch and colleagues were the first to study the concept of missed nursing care, which they defined as “any aspect of required care that is omitted either in part or in whole or delayed” (Kalisch & Williams, 2009, p. 211). They used multiple approaches that ultimately led to the development and testing of the Missed Nursing Care (MISSCARE) Survey (Kalisch, 2006; Kalisch, Landstrom, & Williams, 2009; Kalisch, Landstrom, & Hinshaw, 2009). These researchers initially conducted 25 focus groups (N = 173 staff) in two hospitals to identify what nursing care was missed and why it was missed (Kalisch, 2006). Nine elements of regularly missed nursing care (ambulation, turning, delayed or missed feedings, patient teaching, discharge planning, emotional support, hygiene, intake and output documentation, and surveillance) and seven themes related to the reasons that nurses gave for missing this care (Too Few Staff, Poor Use of Existing Staff Resources, Time Required for the Nursing Intervention, Poor Teamwork, Ineffective Delegation, Habit, and Denial) were identified (Kalisch, 2006). Based on these data, the MISSCARE Survey was constructed (Kalisch & Williams, 2009).
The MISSCARE Survey includes two parts: 22 items about required medical-surgical nursing care that may be delayed, unfinished, or completely missed and 16 items about potential reasons for missed nursing care. Kalisch and Williams (2009) measured missed nursing care; they offered participating nurses lists of nursing activities and asked them to indicate how often these activities were not done on their units and potential reasons why the activities might be missed. Response options for aspects of nursing care that could be missed were rarely, occasionally, frequently, always, and not applicable. Response options for potential reasons for missing care were significant factor, moderate factor, minor factor, and not a reason (Kalisch & Williams, 2009). A specific time frame was not used in the questions. The survey was extensively tested in two studies (three hospitals, N = 459 nurses) and (one hospital, N = 639 nurses) using content analysis and factor analysis. The investigators reported psychometrics for both studies in the same article, and psychometric testing measures produced favorable results in both (Kalisch & Williams, 2009). Eight-five percent of participants completed the entire survey, which indicated high acceptability. Answers to survey questions were consistent among nurses from various participating hospitals who reported a substantial amount of missed care (13% to 89% missed, depending on the specific item on the elements of missed care section). Item sets for the three domains of reasons for missed care (Communication, Material Resources, and Labor Resources) demonstrated acceptable to strong internal consistency with Chronbach’s alpha coefficients from 0.64 to 0.86. The construct validity of this three-factor structure was supported by confirmatory factor analysis (Kalisch & Williams, 2009).
A nursing research team in Pennsylvania studied nurse staffing and missed nursing care in hospital settings, including pediatrics and the NICU (Lake et al., 2016, 2017; Lucero, Lake, & Aiken, 2010; Smith, Morin, Wallace, & Lake, 2018). Lake and colleagues (2017) measured missed nursing care by providing nurses a list of 12 specific nursing activities and asking “on the most recent shift you worked,” which of the following “activities were necessary but left undone because you lacked the time to complete them” (p. 379). A nursing research team in Ohio also conducted research about missed nursing care in pediatric and NICU units using a modified version of the MISSCARE survey. However, in contrast to Kalisch and Williams (2009), Tubbs-Cooley and colleagues used a time-specific measure of missed nursing care similar to Lake et al. (2016, 2017) by asking participant nurses to report the frequency with which they individually missed specific care activities on the last shift worked when considering 35 items of missed care (Tubbs-Cooley et al., 2017; Tubbs-Cooley, Mara, Carle, Mark, & Pickler, 2019; Tubbs-Cooley, Pickler, Younger, & Mark, 2015).
In the United Kingdom and Europe, research groups also studied the concept of missed nursing care and its association with nurse staffing using various other descriptions such as care left undone and care rationing via the RN4CAST survey. In this survey, nurse respondents were asked to report how frequently they were unable to perform any of 13 nursing activities on their last shifts because of time constraints; options included never, sometimes, and often (Ball et al., 2016, 2018; Griffiths et al., 2014; Rafferty et al., 2007). In European hospitals, researchers also used the Basel Extent of Rationing Nursing Care Assessment survey to study missed care (Schubert, Clarke, Glass, Schaffert-Witvliet, & De Geest, 2009; Schubert, Glass, Clarke, Schaffert-Witvliet, & De Geest, 2007). In these two studies, nurse respondents were asked to note the number of necessary nursing tasks for patients withheld or otherwise not performed in the last seven working days. While various teams of researchers in the United States and Europe have essentially been studying the same concept of missed nursing care in non-maternity, acute care settings, differences in measurement based on time frames and item options among studies make it challenging to compare results in this body of research.
In 2012, the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) sponsored a study about nurse staffing during labor and birth in the United States. After reviewing the literature on nurse staffing and patient outcomes, the study team decided to use the concept of missed nursing care to evaluate the potential implications of not having enough nurses to provide safe and effective care to women and their fetuses during labor and birth. This decision was based in part on shared experiences of 887 AWHONN members who participated in an on-line survey on what should be considered during the development of nurse staffing guidelines (Simpson, Lyndon, Wilson, & Ruhl, 2012). Nurses described in detail what they did not have time to do when the unit was short-staffed and the consequences of inadequate nurse staffing (Simpson et al., 2012; Simpson, Lyndon, & Ruhl, 2016). In the context of missed nursing care for women during labor and birth, nurses reported near-miss events; increased risk of adverse outcomes for women and their fetuses or newborns; high stress, burn-out, and fatigue among nurses; and negative implications for staff and patient satisfaction (Simpson et al., 2012, 2016). To develop a survey instrument to measure missed care in the maternity setting, we determined that the MISSCARE Survey (Kalisch & Williams, 2009) provided a framework for adaptation because it included items relevant to multiple nursing settings and had well-supported validity. The purpose of this article is to describe the development of an adaptation of the MISSCARE Survey to measure missed nursing care in the perinatal setting.
Adaptation of the MISSCARE Survey
We carefully evaluated the process the Kalisch team used to develop and test the MISSCARE Survey. We determined that adapting the survey to labor and birth would require drafting proposed item revisions, exploring the concept of missed care with labor and delivery nurses because of substantial differences between nursing care for women in labor and nursing care for medical-surgical and intensive care patients, exploring the concept of missed nursing care with childbearing women and with physicians, and revising and testing the instrument with labor nurses. Figure 1 illustrates the steps in adapting the MISSCARE Survey to the maternity care setting, which resulted in development of the Perinatal Missed Care Survey. Each step built on the previous work of our team and included key stakeholders in maternity care.
Figure 1.
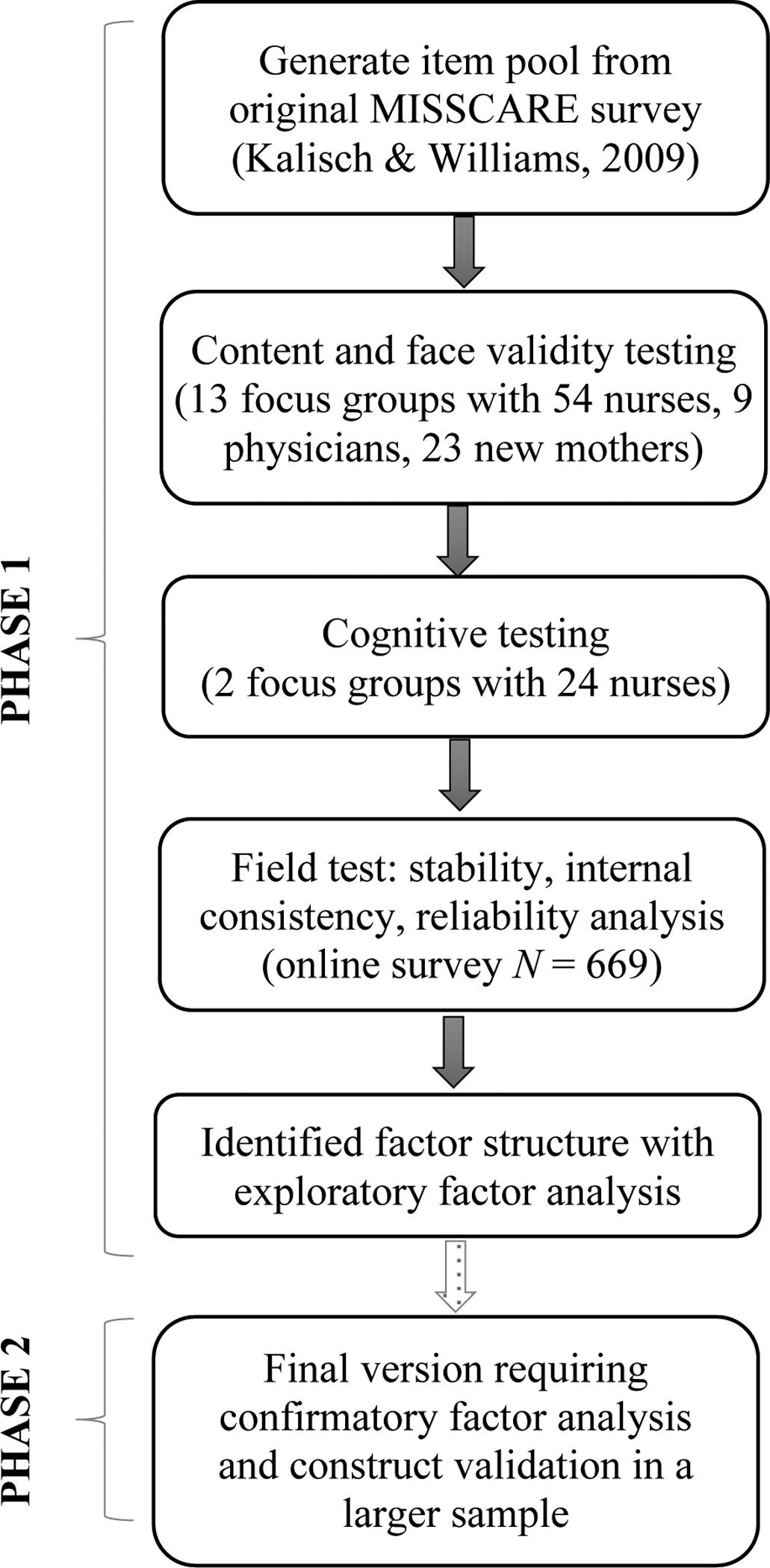
Steps in adapting the MISSCARE Survey to the maternity care setting.
Preparation of Initial Draft of Perinatal Missed Care Survey
We critically reviewed each of the items on the MISSCARE Survey for its application to nursing care for women during labor and birth. Five of the 22 items on required aspects of care were slightly reworded to be more specific to maternity nursing care, eight were left unedited, and nine were replaced. We made minor edits to two of the 16 items on potential reasons for missed care.
Through this process we generated a draft version of an adapted survey with 22 items related to required nursing care for women during labor and birth and 16 items related to potential reasons for missing these aspects of nursing care. We named the adapted instrument the Perinatal Missed Care Survey. We adapted the definition of missed care (Kalisch & Williams, 2009) to missed care during labor and birth as follows: delayed, unfinished, or completely missed nursing care that was expected as part of routine care for childbearing women and their fetuses or newborns during labor and birth and the 2-hour postpartum recovery period. We used the same response options as those on the MISSCARE Survey for all survey items (Kalisch & Williams, 2009): rarely, occasionally, frequently, always, and not applicable. For reasons items, the response options were significant factor, moderate factor, minor factor, and not a reason. Beatrice J. Kalisch reviewed a draft of our survey and identified extra words in several items that did not add value. She advised us to keep the items as short as possible (personal communication, November 2013). The items were edited accordingly.
Exploration of Perinatal Missed Care
We conducted focus groups with nurses, new mothers, and physicians to examine aspects of nursing care these stakeholders deemed important during labor, aspects of nursing care that might be missed, reasons for missed care during labor and birth, and consequences of missed care. The methods and results of our concept exploration are reported elsewhere (Lyndon, Simpson, & Spetz, 2017; Simpson & Lyndon, 2017). In brief, nurses identified 15 categories of care that might be missed: explaining, assessments, surveillance, timely examinations or review of results, medication administration, intake and output, repositioning, comfort care/pain management, labor support, breastfeeding support, skin-to-skin care, answering call lights, safety checks, communication, and documentation (Simpson & Lyndon, 2017). Nurses, new mothers, and physicians all agreed that support and advocacy were critical aspects of the nurse’s role and that these aspects of care were sometimes missed (Lyndon et al., 2017).
Content Analysis
We conducted the content analysis of the proposed Perinatal Missed Care Survey in conjunction with the exploratory groups described above and with additional groups of nurses.
Focus groups with nurses.
We conducted nine focus groups with experienced labor nurses (N=54 with 6–8 nurses per group) to explore missed care and validate the content of the draft Perinatal Missed Care Survey. We held these groups in four hospitals in the Washington, DC/Baltimore area (two focus groups per hospital) and one in rural Missouri (one focus group). Sites for the focus groups represented a range of annual birth volumes from 750 births per year to 8,500 births per year. The investigators’ institutional review boards (IRBs), an independent IRB for academic and nonacademic institutions, and participating hospitals that required IRB approval specific to their facilities at the focus group sites all approved the study.
Inclusion criteria for focus group participants were currently working as a labor and birth staff nurse and at least 2 years of experience in that role. After conducting the exploration of potential missed nursing care described above, we explained the history of the MISSCARE Survey and its use on medical-surgical units. Each nurse received a copy of the original version of the MISSCARE instrument and our revised version (draft Perinatal Missed Care Survey), and we solicited feedback as to whether the original items and proposed substituted items specifically related to perinatal care were appropriate to capture possible missed care during labor and birth. The participants rated each of the items as applicable or not applicable.
We iteratively summarized participant demographic characteristics and the applicability of existing and proposed missed nursing care items between groups. We also considered data from thematic analysis of focus group discussions (Lyndon et al., 2017; Simpson & Lyndon, 2017) to guide development of the next version of the Perinatal Missed Care Survey. In total we modified three items (pericare added to patient bathing/skin care, item on discharge teaching reworded to make it shorter, item on uterine activity shortened to remove definition of tachysystole) and added three items (thorough review of prenatal records, recognize and respond to new maternal complications within 10 minutes, thorough patient handoff).
We then convened two focus groups of labor nurses (N = 17) at a community hospital in St. Louis, MO to validate the revised version of the Perinatal Missed Care Survey, which included a total of 25 required nursing care items and 16 potential reasons for missed care. Based on their suggestions, we made several minor edits to the items.
Focus groups with new mothers.
Next, we convened two focus groups of women who recently gave birth (N = 23) to elicit their input on important aspects of nursing care during labor and birth, what aspects of that care should be measured (Lyndon et al., 2017), and to validate the content of the 25 proposed required nursing care items. These focus groups were held in a community hospital in St. Louis, MO and approved under the same IRBs as described above. We used the same process as with the nurse focus groups: first, we explored participants’ perspectives on important aspects of nursing care during labor and birth and what might be missed (Lyndon et al., 2017); then we explained the history of the original MISSCARE survey and solicited feedback on the draft required nursing care items for the adapted Perinatal Missed Care Survey. We evaluated participants’ responses in the context of potential missing items on aspects of care important to new mothers. We did not add items based on these focus groups; participants noted they felt the existing items adequately covered their perspectives on nursing care during labor and birth.
Focus groups with physicians.
Finally, we conducted two focus groups with clinically active physicians (N=9) who practiced in two hospitals in Northern California: a community hospital and an academic medical center. We used the same IRB approvals and followed the same process as outlined above. First, we explored physicians’ perspectives on important aspects of nursing care and what could be missed (Lyndon et al., 2017); then we explained the history of the MISSCARE survey and solicited feedback on the draft required nursing care items for the Perinatal Missed Care Survey. We did not identify any new items based on these two focus groups because physician participants confirmed the items to be inclusive.
Testing for Clarity and Ease of Use
The next step was to test the process of taking the Perinatal Missed Care Survey to ensure ease of use and check for clarity of instructions and items. We held two focus groups of practicing labor nurses (N=24) at the 2015 AWHONN convention. We administered the survey to all nurses in these groups and asked for feedback on individual items, clarity of instructions, and overall ease of use. We made minor modifications to the instructions based on this feedback, but no individual items needed further changes at that time.
Psychometric Testing
Following adaptation of the MISSCARE survey to be applicable to labor and birth we administered the resulting Perinatal Missed Care Survey to a large sample of nurses for the purposes of psychometric testing of the new instrument.
Methods
We administered the Perinatal Missed Care Survey to labor nurses in selected hospitals in California, Michigan, and New Jersey between July 2016 and May 2017 via an on-line survey nurses accessed by clicking on a link in an email. Nurse leaders of labor and birth units in these states facilitated survey distribution to labor nurses in their hospitals. Demographic items included age; race; ethnicity; highest level of education; full-time or part-time status; and role on the unit such as staff nurse, charge nurse, nurse manager, clinical specialist, or nurse educator. The investigators’ IRBs approved the study and the study center handled all recruitment and data collection centrally so that participating hospitals were not engaged in human subjects activity. However, we also obtained IRB approval at hospitals that required additional approval before inviting their labor nurses to participate.
Settings and Participants
Email invitations to participate in the study by completing the Perinatal Missed Care Survey were sent to 2,650 labor nurses: 783 nurses opened the survey on line, and 669 surveys had useable data. Respondents were experienced and highly educated: 74% had at least 5 years of experience as labor nurses (mean 13.8, range 0–46) and 62% had Bachelor’s degrees or higher. Most respondents were staff nurses (59%) or staff and charge (23%) and worked full-time (67%). Almost half worked day shift (49%), one-third work night shift (32%), 4% worked evening shift, and 5% worked rotating shifts (Table 1). Respondents represented 67 hospitals in California, Michigan, and New Jersey. Annual birth volumes at these hospitals ranged from less than 200 to greater than 7000 births. The median annual birth volume was 1,802.
Table 1:
Demographic and Employment Characteristics of Nurse Respondents (N = 669)
| Respondent Characteristic | Mean (SD) or n (%) | Range |
|---|---|---|
| Age (years) | 42.9 (11.6) | 23 – 77 |
| Race/Ethnicity | ||
| Hispanic/Latino | 7 (1) | |
| American Indian or Alaska Native | 1 (<1) | |
| Asian | 8 (1) | |
| Hawaiian or other Pacific Islander | 1 (<1) | |
| Black/African American | 18 (3) | |
| White | 509 (76) | |
| Decline to state | 39 (6) | |
| Other | 10 (1) | |
| Missing | 76 (11) | |
| Highest level of nursing education | ||
| Diploma | 30 (4) | |
| Associates | 195 (29) | |
| Bachelors | 318 (48) | |
| Masters | 50 (7) | |
| Doctorate | 2 (<1) | |
| Missing | 74 (11) | |
| Years of experience as a registered nurse | 16.7 (12.0) | 0 – 54 |
| <5 years | 106 (16) | |
| 5 – 9.9 years | 104 (16) | |
| 10 – 19.9 years | 150 (22) | |
| ≥ 20 years | 229 (34) | |
| Missing | 80 (12) | |
| Years of experience in labor and delivery | 13.8 (11.2) | 0 – 46 |
| <5 years | 174 (26) | |
| 5 – 9.9 years | 74 (11) | |
| 10 – 19.9 years | 163 (24) | |
| ≥ 20 years | 175 (26) | |
| Missing | 83 (13) | |
| Shift usually worked | ||
| Days | 327 (49) | |
| Evenings | 24 (4) | |
| Nights | 211 (32) | |
| Rotating | 34 (5) | |
| Missing | 73 (11) | |
| Employment status | ||
| Full-time | 445 (67) | |
| Part-time | 151 (23) | |
| Missing | 73 (11) | |
| Role on the unit | ||
| Staff nurse | 395 (59) | |
| Charge nurse | 13 (2) | |
| Staff nurse and charge nurse | 153 (23) | |
| Administrator | 24 (4) | |
| Clinical nurse specialist/nurse educator | 14 (2) | |
| Missing | 70 (10) |
Data Analysis
We conducted an exploratory factor analysis (EFA) of both sections (required nursing care and potential reasons for missing care) to determine the factor structure of the adapted survey. Based on the distribution of responses, items from the required nursing care section were dichotomized (described in the results section), and inter-item correlations and the EFA were based on tetrachoric correlations as appropriate for dichotomous items. The EFA for reasons for missed care items utilized polychoric correlations (suitable for ordinal data) and promin rotation of the factor solution, which permits factors to be correlated. For both factor analyses (required nursing care, 25 items; and reasons for missed nursing care, 16 items), the number of factors to retain was determined using variance explained, Kaiser’s criteria (eigenvalues >1), and factor loading criteria (a minimum of 5 items with factor loadings [≥ .5]). Internal consistency reliability was determined for both sections using ordinal coefficient alpha, which provides more accurate estimates for binary and ordinal data than Cronbach’s alpha (Gaderman, Guhn, & Zumbo, 2012). Item analysis included calculating inter-item and item-total correlations.
Results
Acceptability
Acceptability and ease of use were assessed by the number of respondents who completed the survey without skipping any items. On surveys that were completed, there were minimal missing data, thus the survey appeared to be acceptable to nurses. Responses of not applicable were not included in the analysis.
Factor Structure
Aspects of required nursing care.
The EFA on the 25 items related to aspects of required nursing care (see Table 2) began with an initial screening of the data for characteristics that can detract from trustworthiness of results. Respondent nurses exhibited a strong tendency to endorse the lowest (rarely) or highest (always) response options on the survey’s 4-point scale. For example, on item 25, “Notification of physician or nurse-midwife in a timely manner to attend birth,” 45.48% of the respondents endorsed rarely and 39.76% endorsed always. In comparison, only 7.53% and 7.23% endorsed the middle response categories of occasionally and frequently respectively. The tendency of respondents to endorse the extreme response options was noted in at least half of the 25 items and was interpreted as evidence that the respondents tended to view the care described by an item (e.g., “Assess pain status every hour”) as fulfilled or not. Respondents appeared to largely disregard the full rating scale and opted instead to respond to the 4-point scale in a yes or no style by endorsing the extreme response options. As per prior research (Finch & Bronk, 2011), we reduced the 4-point scale to a 2-point scale by combining responses to the rarely and occasionally options into one category and by combining responses to the frequently and always options into one category.
Table 2:
Factor Loading Estimates for Aspects of Required Nursing Care During Labor and Birth
| Items | Estimates |
|---|---|
| 1. Assist women to the shower or tub for hydrotherapy. | 0.521 |
| 2. Assess effectiveness of medications. | 0.980 |
| 3. Check bladder status/voiding needs every 2 hours. | 0.951 |
| 4. Assess pain status every hour. | 0.878 |
| 5. Thorough review of prenatal records. | 0.919 |
| 6. Patient teaching about procedures, tests, and other diagnostic studies. | 0.976 |
| 7. Medications administration within 30 minutes before or after scheduled time. | 0.968 |
| 8. Administer oxytocin as per orders or protocol. | - |
| 9. Response to call light is initiated within 5 minutes. | - |
| 10. Emotional support to patient and/or family. | 0.991 |
| 11. Patient bathing, skin care, or pericare. | 0.979 |
| 12. Recognize and respond to indeterminate (Category II) or abnormal (Category III) FHR changes within 15 minutes. | - |
| 13. Recognize and respond to excessive uterine activity within 20 minutes. | - |
| 14. Recognize and respond to new maternal complications within 10 min (e.g., hypertension, bleeding). | - |
| 15. Focused reassessments according to patient condition (e.g., FHR and uterine activity assessment q 15 minutes for women receiving oxytocin for labor induction or augmentation). | 0.977 |
| 16. Real-time or near real-time documentation of maternal-fetal assessments during labor, birth, and recovery. | 0.671 |
| 17. Patient teaching about signs and symptoms, when to call after discharge from obstetric triage. | 0.989 |
| 18. Monitor intake and output. | 0.792 |
| 19. Provide skin-to-skin mother-baby care immediately after birth. | 0.985 |
| 20. Assess vital signs as ordered, or per protocol. | 0.993 |
| 21. Provide thorough patient handoff. | 0.986 |
| 22. Hand washing. | - |
| 23. Breastfeeding within 1 hour after birth for women who are breastfeeding. | - |
| 24. Recovery care consisting of 2 hours of every 15-minute maternal assessments and 2 hours of every 30-minute newborn assessments. | 0.876 |
| 25. Notification of physician or nurse-midwife in a timely manner to attend birth. | - |
The 25 items tended to be highly correlated with each other. Although we expected that items capturing common characteristics among respondents would correlate well, the correlations were high enough to suggest that the scale contained some redundancy. Analyses showed that a typical correlation between any pair of items on the survey was around 0.875; 36 of the correlations approached the maximum value of a correlation (i.e., > 0.95). Items 17 and 20 exhibited a large correlation of 0.982, which indicated that respondents nearly always responded to item 17 in the same way they responded to item 20. The pattern of redundancy was so high for items 8, 9, 12, 13, 14, 22, 23, and 25 that they were not amenable to an exploratory factor analysis and consequently were removed from further analysis. Among the remaining 17 survey items, the factor analysis strongly indicated that the observed responses were largely explained by a single factor. Nearly all the items were highly related to a single unobserved factor as evidenced by the loading estimates (Brown, 2014), which we interpreted as related to nurse staffing. Twelve of the 17 items had loading estimates in excess of 0.900, which indicated that redundancy was present in the survey. Factor loading results are presented in Table 2.
We reviewed the performance of each of the items individually. Because respondents frequently skipped one item (assisting women to the shower or tub for hydrotherapy, 25% missing), we eliminated this item and replaced it with an item about labor support for future use and testing of the survey.
Reasons for missed nursing care.
Initial screening of the data and checks on the trustworthiness of the factor analysis findings suggested few issues with the reasons for missed care items. Responses distributions were unimodal, which approximated normal distributions; only one item demonstrated slight skewness (Item 4: skewness = 1.16, kurtosis = 1.075). Inter-item correlations did not suggest redundancy (range: ρ = .23 to .86) nor did item-total correlations (range: ρ = .51 − .66). Results of the exploratory factor analysis suggested that two factors likely explained responses to the 16 items in the section on reasons for missed care. Specifically, items 1 through 11 appeared to be explained, in part, by one factor while items 12 through 16 appeared to be explained, in part, by a related but second distinct factor (see Table 3). Items displayed strong loadings (range: .498 − .954) on their respective factors, and none displayed cross-loadings less than .30. A review of the loading estimates displayed in Table 3 revealed that the items related well to their respective traits, and there was little justification to drop any of the 16 items. Expert analysis of the content covered by the items clustered onto the two factors suggested that the first factor may represent nurses’ experience with communication problems and the second factor may represent their experience with inadequate staffing resources. Items 9 and 10 exhibited a large correlation unrelated to the factor on which they clustered. This suggested there may be an additional characteristic or unknown factor explaining the observed responses to items 9 and 10 that they share in common, consistent with the three-factor solution in the original MISSCARE Survey (Kalisch & Williams, 2009).
Table 3:
Factor Loading Estimates of Reasons for Missing Required Aspects of Nursing Care During Labor and Birth
| Items | Estimates | |
|---|---|---|
| Factor 1 | Factor 2 | |
| 1. Tension or communication breakdowns within the nursing team | 0.816 | |
| 2. Lack of backup support from team members | 0.673 | |
| 3. Nurse colleague, nursing assistant, or OB technician did not communicate that care was not done | 0.730 | |
| 4. Care giver is off unit or unavailable (care giver includes nurse, nursing assistant, and OB technician) | 0.639 | |
| 5. Tension or communication breakdowns with the medical or midwifery staff | 0.723 | |
| 6. Tension or communication breakdowns with other support departments | 0.893 | |
| 7. Other departments did not provide the care needed | 0.851 | |
| 8. Inadequate handoff from previous shift or sending unit | 0.774 | |
| 9. Supplies/equipment not available when needed | 0.552 | |
| 10. Supplies/equipment not functioning properly when needed | 0.579 | |
| 11. Medications not available when needed | 0.498 | |
| 12. Unexpected rise in patient volume or patient acuity on the unit | 0.886 | |
| 13. Urgent patient situations (e.g., patient’s condition worsening, precipitous birth, emergent cesarean birth) | 0.862 | |
| 14. Inadequate number of staff (patient assignment above recommended nurse-to-patient ratios) | 0.954 | |
| 15. Inadequate number of assistive personnel (e.g., nursing assistants, obstetric technicians) | 0.762 | |
| 16. Unbalanced patient assignments | 0.649 | |
Internal Consistency Reliability
We estimated internal consistency reliability using ordinal alpha coefficients. The ordinal alpha was 0.99 for the section on aspects of missed nursing care and 0.963 and .959 for the communication and staffing domains of potential reasons for missed care, which suggested potential redundancy among items (Tavakol & Dennick, 2011). The results of the exploratory factor analysis, inter-item, and item-total correlations suggest this may be an issue with aspects of missed care items but does not appear to be an issue with potential reasons for missed care. Redundancy in the aspects of missed care may be due to the scale consisting of a list of tasks that co-occur during routine intrapartum and immediate postpartum recovery care.
Scoring and Interpretation
Kalisch previously demonstrated the utility of mean missed care scores at the individual nurse and the unit level in relation to patient outcomes, nurse staffing, and aspects of nurse work environment (Kalisch & Lee, 2010; Tschannen, Kalisch, & Lee, 2010). The Perinatal Missed Care Survey can also potentially be scored and interpreted at the individual nurse level and the maternity unit level. In item analysis, 46% to 63% of respondents reported individual aspects of care were frequently or always missed, and real-time documentation and monitoring intake and output had the highest proportion of reported missed care (Table 4).
Table 4:
Percent of Nurse Participants Who Reported Care Frequently or Always Missed by Item (N=669)
| Item/Scale | Frequently or Always missed |
|---|---|
| 1. Assess effectiveness of medications | 50% |
| 2. Check bladder status/voiding needs every 2 hours | 48% |
| 3. Assess pain status every hour | 55% |
| 4. Thorough review of prenatal records | 55% |
| 5. Patient teaching about procedures, tests, and other diagnostic studies | 51% |
| 6. Medications administered within 30 minutes before or after scheduled time | 50% |
| 7. Administer oxytocin as per orders or protocol | 49% |
| 8. Response to call light is initiated within 5 minutes | 49% |
| 9. Emotional support to patient and/or family | 50% |
| 10. Patient bathing, skin care, or pericare | 48% |
| 11. Recognize and respond to indeterminate (Category II) or abnormal (Category III) FHR changes within 15 minutes | 47% |
| 12. Recognize and respond to excessive uterine activity within 20 minutes | 47% |
| 13. Recognize and respond to new maternal complications within 10 min (e.g. hypertension, bleeding) | 48% |
| 14. Focused reassessments according to patient condition (e.g., fetal heart rate and uterine activity assessment every 15 minutes for women receiving oxytocin for labor induction or augmentation) | 49% |
| 15. Real-time or near real- time documentation of maternal-fetal assessments during labor, birth, and recovery | 63% |
| 16. Patient teaching about signs and symptoms, when to call after discharge from obstetric triage | 46% |
| 17. Monitor intake and output | 57% |
| 18. Provide skin-to-skin mother-baby care immediately after birth | 49% |
| 19. Assess vital signs as ordered, or per protocol | 50% |
| 20. Provide thorough patient handoff | 51% |
| 21. Hand washing | 48% |
| 22. Breastfeeding within 1 hour after birth for women who are breastfeeding | 49% |
| 23. Recovery care consisting of 2 hours of every 15 minute maternal assessments and 2 hours of every 30 minute newborn assessments | 49% |
| 24. Notification of physician or nurse-midwife in a timely manner to attend birth | 47% |
Discussion
Labor nurse participants in the focus groups agreed that the items on the Perinatal Missed Care Survey reflected essential nursing care during labor and birth. Feedback from new mothers who had recently given birth and physicians who attended births were similarly confirmatory. When the survey was administered, minimal data were missing, which suggested acceptability and ease of use of the survey. Item analysis revealed clustering of responses at extremes of the scale in an essentially dichotomous format and EFA revealed substantial item redundancy. From the perspective of an EFA, the redundancy should be eliminated because in general a shorter survey is more likely to be fully completed; however, eliminating the redundancy will lead to a reduction in a large portion of the items of interest regarding specific aspects of care, including items with content substantively valuable to the study of the labor and birth setting.
The research team concluded that each of the items is important for future study using the tool and should be retained based on the content conveyed by the individual items. The two-factor solution in the reasons for missed care section is consistent with content plausibility and likely reflects the three-factor solution found in psychometric analysis of the original MISSCARE Survey of the concepts of communication, equipment availability, and nurse staffing resources (Kalisch & Williams, 2009). We are using the Perinatal Missed Care Survey in a larger, federally funded study that will allow further psychometric testing, including confirmatory factor analysis, construct validation, and determination of the need for any further modification. We aim to evaluate selected patient outcomes for their potential relationships with nurse staffing and missed nursing care during labor and birth.
Limitations
Limitations of our study include a focus only on nursing care during labor, birth, and the immediate postpartum recovery period to the exclusion of the rest of the postpartum stay. Nursing care during labor involves a more concentrated “dose” of nursing care than during the postpartum period, when nurses care for a greater number of patients, despite the potential for high acuity in both phases of care (Simpson et. al, 2016; Simpson & Lyndon, 2017). This may render nursing care during labor less sensitive than postpartum care to variations in staffing and other organizational factors. . The Perinatal Missed Care Survey needs additional confirmatory testing and may not be applicable outside of the North American context due to differences in how care is delivered to laboring women in other parts of the world. However, the instrument represents one building block toward a more robust set of nurse-sensitive measures for maternity care.
Conclusion
The Perinatal Missed Care Survey appears to be a feasible and promising instrument with which to evaluate missed nursing care during labor and birth. The items cover essential aspects of nursing care during labor and birth based on the feedback of women who had recently given birth and nurses and physicians who attend women during labor and birth (Lyndon et al., 2017). The results are consistent with our earlier findings about the potential implications of missed nursing care during labor and birth (Simpson et. al, 2016; Simpson & Lyndon, 2017). Researchers have found the study of missed nursing care allows the evaluation of various aspects of nursing care in medical-surgical, pediatric, NICU, and adult intensive care units (Ball et al., 2018; Griffiths et al., 2018; Kalisch et al., 2011; Lake et al., 2017; Schubert et al., 2007; Tubbs-Cooley et al., 2017). Our adaption of the MISSCARE survey (Kalisch & Williams, 2009) to maternity care has the potential to shed light on a substantial knowledge gap in nurse-sensitive indicators for maternity care and to contribute to measuring the effects of nurse staffing on patient outcomes for women giving birth.
Acknowledgement
Supported in part by the Association of Women’s Health, Obstetric and Neonatal Nurses and by the Agency for Healthcare Research and Quality, grant number R01HS025715. The content is solely the responsibility of the authors and does not necessarily represent the official views of AWHONN or the Agency for Healthcare Research and Quality
Author Bios
Kathleen Rice Simpson, PhD, RNC, CNS-BC, FAAN, is a volunteer perinatal clinical nurse specialist, Mercy Hospital Saint Louis, Saint Louis, MO.
Audrey Lyndon, PhD, RNC, FAAN, is a professor and Assistant Dean for Clinical Research, Rory Meyers College of Nursing, New York University, New York, NY.
Joanne Spetz, PhD, is a professor in the Philip R. Lee Institute for Health Policy Studies, University of California San Francisco, San Francisco, CA.
Caryl L. Gay, PhD, is a research specialist in the Department of Family Health Care Nursing, School of Nursing, University of California San Francisco, San Francisco, CA.
Gay L. Landstrom PhD, RN, NEA-BC, is the System Chief Nursing Officer, Trinity Health, Livonia, MI.
Contributor Information
Kathleen Rice Simpson, Mercy Hospital Saint Louis, Saint Louis, MO..
Audrey Lyndon, Rory Meyers College of Nursing, New York University, New York, NY..
Joanne Spetz, Philip R. Lee Institute for Health Policy Studies, University of California San Francisco, San Francisco, CA..
Caryl L. Gay, Department of Family Health Care Nursing, School of Nursing, University of California San Francisco, San Francisco, CA..
Gay Landstrom, Trinity Health, Livonia, MI..
References
- Ball JE, Bruyneel L, Aiken LH, Sermeus W, Sloane DM, Rafferty AM, … Griffiths P (2018). Post-operative mortality, missed care and nurse staffing in nine countries: A cross-sectional study. International Journal of Nursing Studies, 78, 10–15. doi: 10.1016/j.ijnurstu.2017.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball JE, Griffiths P, Rafferty AM, Lindqvist R, Murrells T, & Tishelman C (2016). A cross-sectional study of ‘care left undone’ on nursing shifts in hospitals. Journal of Advanced Nursing, 72(9), 2086–2097. doi: 10.1111/jan.12976 [DOI] [PubMed] [Google Scholar]
- Brown TA (2014). Confirmatory factor analysis for applied research. New York: Guilford Publications. [Google Scholar]
- Finch WH, & Bronk KC (2011). Conducting confirmatory latent class analysis using Mplus. Structural Equation Modeling, 18(1), 132–151. [Google Scholar]
- Gadermann AM, Guhn M, & Zumbo BD (2012). Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. Practical Assessment, Research & Evaluation, 17, 1–13. [Google Scholar]
- Griffiths P, Dall’Ora C, Simon M, Ball J, Lindqvist R, Rafferty AM, … Aiken LH (2014). Nurses’ shift length and overtime working in 12 European countries: The association with perceived quality of care and patient safety. Medical Care, 52(11), 975–981. doi: 10.1097/mlr.0000000000000233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P, Recio-Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, … Ball J (2018). The association between nurse staffing and omissions in nursing care: A systematic review. Journal of Advanced Nursing, 74(7), 1474–1487. doi: 10.1111/jan.13564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalisch BJ (2006). Missed nursing care: A qualitative study. Journal of Nursing Care Quality, 21(4), 306–313; quiz 314–305. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Gosselin K, & Choi SH (2012). A comparison of patient care units with high versus low levels of missed nursing care. Health Care Management Review, 37(4), 320–328. doi: 10.1097/HMR.0b013e318249727e [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom G, & Williams RA (2009). Missed nursing care: Errors of omission. Nursing Outlook, 57(1), 3–9. doi: 10.1016/j.outlook.2008.05.007 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom GL, & Hinshaw AS (2009). Missed nursing care: A concept analysis. Journal of Advanced Nursing, 65(7), 1509–1517. doi: 10.1111/j.1365-2648.2009.05027.x [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, & Lee KH (2010). The impact of teamwork on missed nursing care. Nursing Outlook, 58, 233–241. doi: 10.1016/j.outlook.2010.06.004 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, & Lee KH (2012). Congruence of perceptions among nursing leaders and staff regarding missed nursing care and teamwork. Journal of Nursing Administration, 42(10), 473–477. doi: 10.1097/NNA.0b013e31826a1fa4 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, McLaughlin M, & Dabney BW (2012). Patient perceptions of missed nursing care. Joint Commission Journal on Quality and Patient Safety, 38(4), 161–167. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Tschannen D, & Lee KH (2011). Do staffing levels predict missed nursing care? International Journal for Quality in Health Care, 23(3), 302–308. doi: 10.1093/intqhc/mzr009 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Tschannen D, & Lee KH (2012). Missed nursing care, staffing, and patient falls. Journal of Nursing Care Quality, 27(1), 6–12. doi: 10.1097/NCQ.0b013e318225aa23 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, & Williams RA (2009). Development and psychometric testing of a tool to measure missed nursing care. Journal of Nursing Administration, 39(5), 211–219. doi: 10.1097/NNA.0b013e3181a23cf5 [DOI] [PubMed] [Google Scholar]
- Lake ET, de Cordova PB, Barton S, Singh S, Agosto PD, Ely B, … Aiken LH (2017). Missed nursing care in pediatrics. Hospital Pediatrics, 7(7), 378–384. doi: 10.1542/hpeds.2016-0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, Germack HD, & Viscardi MK (2016). Missed nursing care is linked to patient satisfaction: a cross-sectional study of US hospitals. BMJ Quality and Safety, 25(7), 535–543. doi: 10.1136/bmjqs-2015-003961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucero RJ, Lake ET, & Aiken LH (2010). Nursing care quality and adverse events in US hospitals. Journal of Clinical Nursing, 19(15–16), 2185–2195. doi: 10.1111/j.1365-2702.2010.03250.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyndon A, Simpson KR, & Spetz J (2017). Thematic analysis of US stakeholder views on the influence of labour nurses’ care on birth outcomes. BMJ Quality and Safety, 26(10), 824–831. doi: 10.1136/bmjqs-2016-005859 [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, & Osterman MJK, Driscoll AK, & Drake P (2018). Births: Final data for 2017. National Vital Statistics Reports, 67(8), 1–50. [PubMed] [Google Scholar]
- McDermott KW, Elixhauser A, & Sun R (2017). Trends in hospital inpatient stays in the United States, 2005–2015: Statistical brief #225. Retreived from https://www.hcup-us.ahrq.gov/reports/statbriefs/sb225-Inpatient-US-Stays-Trends.jsp
- Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, & Aiken LH (2007). Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. International Journal Nursing Studies, 44(2), 175–182. doi: 10.1016/j.ijnurstu.2006.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M, Clarke SP, Glass TR, Schaffert-Witvliet B, & De Geest S (2009). Identifying thresholds for relationships between impacts of rationing of nursing care and nurse- and patient-reported outcomes in Swiss hospitals: A correlational study. International Journal of Nursing Studies, 46(7), 884–893. doi: 10.1016/j.ijnurstu.2008.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M, Glass TR, Clarke SP, Schaffert-Witvliet B, & De Geest S (2007). Validation of the Basel Extent of Rationing of Nursing Care instrument. Nursing Research, 56(6), 416–424. doi: 10.1097/01.Nnr.0000299853.52429.62 [DOI] [PubMed] [Google Scholar]
- Simpson KR, (2011). An overview of distribution of births in United States hospitals in 2008 with implications for small volume perinatal units in rural hospitals. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 40(4), 432–439. doi: 10.1111/j.1552-6909.2011.01262.x [DOI] [PubMed] [Google Scholar]
- Simpson KR, & Lyndon A (2017). Consequences of delayed, unfinished, or missed nursing care during labor and birth. Journal of Perinatal and Neonatal Nursing, 31(1), 32–40. doi: 10.1097/JPN.0000000000000203 [DOI] [PubMed] [Google Scholar]
- Simpson KR, Lyndon A, & Ruhl C (2016). Consequences of inadequate staffing include missed care, potential failure to rescue, and job stress and dissatisfaction. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 45(4), 481–490. doi: 10.1016/j.jogn.2016.02.011 [DOI] [PubMed] [Google Scholar]
- Simpson KR, Lyndon A, Wilson J, & Ruhl C (2012). Nurses’ perceptions of critical issues requiring consideration in the development of guidelines for professional registered nurse staffing for perinatal units. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 41(4), 474–482. doi: 10.1111/j.1552-6909.2012.01383.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JG, Morin KH, Wallace LE, & Lake ET (2018). Association of the nurse work environment, collective efficacy, and missed care. Western Journal of Nursing Research, 40(6), 779–798. doi: 10.1177/0193945917734159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavakol M & Dennick R (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education, 2, 53–55. doi: 10.5116/ijme.4dfb.8dfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschannen D, Kalisch BJ, & Lee KH (2010). Missed nursing care: The impact on intention to leave and turnover. Canadian Journal of Nursing Research, 42(4), 22–39. [PubMed] [Google Scholar]
- Tubbs-Cooley HL, Mara CA, Carle AC, Mark BA, Pickler RH (2019). Association of nurse workload with missed nursing care in the Neonatal Intensive Care Unit. JAMA Pediatrics, 173(1), 44–51. doi: 10.1001/jamapediatrics.2018.3619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubbs-Cooley HL, Pickler RH, Mara CA, Othman M, Kovacs A, & Mark BA (2017). Hospital Magnet designation and missed nursing care in neonatal intensive care units. Journal of Pediatric Nursing, 34, 5–9. doi: 10.1016/j.pedn.2016.12.004 [DOI] [PubMed] [Google Scholar]
- Tubbs-Cooley HL, Pickler RH, Younger JB, & Mark BA (2015). A descriptive study of nurse-reported missed care in neonatal intensive care units. Journal of Advanced Nursing, 71(4), 813–824. doi: 10.1111/jan.12578 [DOI] [PubMed] [Google Scholar]


