Abstract
Background
Early and accurate diagnosis and treatment of schizophrenia may have long‐term advantages for the patient; the longer psychosis goes untreated the more severe the repercussions for relapse and recovery. If the correct diagnosis is not schizophrenia, but another psychotic disorder with some symptoms similar to schizophrenia, appropriate treatment might be delayed, with possible severe repercussions for the person involved and their family. There is widespread uncertainty about the diagnostic accuracy of First Rank Symptoms (FRS); we examined whether they are a useful diagnostic tool to differentiate schizophrenia from other psychotic disorders.
Objectives
To determine the diagnostic accuracy of one or multiple FRS for diagnosing schizophrenia, verified by clinical history and examination by a qualified professional (e.g. psychiatrists, nurses, social workers), with or without the use of operational criteria and checklists, in people thought to have non‐organic psychotic symptoms.
Search methods
We conducted searches in MEDLINE, EMBASE, and PsycInfo using OvidSP in April, June, July 2011 and December 2012. We also searched MEDION in December 2013.
Selection criteria
We selected studies that consecutively enrolled or randomly selected adults and adolescents with symptoms of psychosis, and assessed the diagnostic accuracy of FRS for schizophrenia compared to history and clinical examination performed by a qualified professional, which may or may not involve the use of symptom checklists or based on operational criteria such as ICD and DSM.
Data collection and analysis
Two review authors independently screened all references for inclusion. Risk of bias in included studies were assessed using the QUADAS‐2 instrument. We recorded the number of true positives (TP), true negatives (TN), false positives (FP), and false negatives (FN) for constructing a 2 x 2 table for each study or derived 2 x 2 data from reported summary statistics such as sensitivity, specificity, and/or likelihood ratios.
Main results
We included 21 studies with a total of 6253 participants (5515 were included in the analysis). Studies were conducted from 1974 to 2011, with 80% of the studies conducted in the 1970's, 1980's or 1990's. Most studies did not report study methods sufficiently and many had high applicability concerns. In 20 studies, FRS differentiated schizophrenia from all other diagnoses with a sensitivity of 57% (50.4% to 63.3%), and a specificity of 81.4% (74% to 87.1%) In seven studies, FRS differentiated schizophrenia from non‐psychotic mental health disorders with a sensitivity of 61.8% (51.7% to 71%) and a specificity of 94.1% (88% to 97.2%). In sixteen studies, FRS differentiated schizophrenia from other types of psychosis with a sensitivity of 58% (50.3% to 65.3%) and a specificity of 74.7% (65.2% to 82.3%).
Authors' conclusions
The synthesis of old studies of limited quality in this review indicates that FRS correctly identifies people with schizophrenia 75% to 95% of the time. The use of FRS to diagnose schizophrenia in triage will incorrectly diagnose around five to 19 people in every 100 who have FRS as having schizophrenia and specialists will not agree with this diagnosis. These people will still merit specialist assessment and help due to the severity of disturbance in their behaviour and mental state. Again, with a sensitivity of FRS of 60%, reliance on FRS to diagnose schizophrenia in triage will not correctly diagnose around 40% of people that specialists will consider to have schizophrenia. Some of these people may experience a delay in getting appropriate treatment. Others, whom specialists will consider to have schizophrenia, could be prematurely discharged from care, if triage relies on the presence of FRS to diagnose schizophrenia. Empathetic, considerate use of FRS as a diagnostic aid ‐ with known limitations ‐ should avoid a good proportion of these errors.
We hope that newer tests ‐ to be included in future Cochrane reviews ‐ will show better results. However, symptoms of first rank can still be helpful where newer tests are not available ‐ a situation which applies to the initial screening of most people with suspected schizophrenia. FRS remain a simple, quick and useful clinical indicator for an illness of enormous clinical variability.
Plain language summary
First rank symptoms for schizophrenia
It is important for patients with psychosis to be correctly diagnosed as soon as possible. The earlier schizophrenia is diagnosed the better the treatment outcome. However, other diseases sometimes have similar psychotic symptoms as schizophrenia, for example bipolar disorder. This review looks at how accurate First Rank Symptoms (FRS) are at diagnosing schizophrenia. FRS are symptoms that people with psychosis may experience, for example hallucinations, hearing voices and thinking that other people can hear their thoughts. We found 21 studies, with 6253 participants, that looked at how good FRS are at diagnosing schizophrenia when compared to a diagnosis made by a psychiatrist. These studies showed that for people who actually have schizophrenia, FRS would only correctly diagnose just over half of them as schizophrenic. For people who do not have schizophrenia, almost 20% would be incorrectly diagnosed with schizophrenia. Therefore, if a person is experiencing a FRS, schizophrenia is a possible diagnosis, but there is also a chance that it is another mental health disorder. We do not recommend that FRS alone can be used to diagnose schizophrenia. However, FRS could be useful to triage patients who need to be assessed by a psychiatrist.
Summary of findings
Summary of findings'. 'Summary of findings table.
| What is the diagnostic accuracy of first rank symptoms for schizophrenia? | |||||
| Patients/population | People with psychotic symptoms and admissions to psychiatric ward | ||||
| Prior testing | Most studies did not only include patients with first episode psychosis, so it is likely that patients had experienced prior testing | ||||
| Settings | Mostly inpatient setting | ||||
| Index test | Presence of at least one FRS or number of FRSs was not reported | ||||
| Importance | FRS could be used to screen out the seriously mentally ill for further consideration by more specialised services | ||||
| Reference standard | There is no gold standard for diagnosing schizophrenia. Reference standard used: history and clinical examination collected by a qualified professional, which may or may not involve the use of operational criteria or checklists of symptoms | ||||
| Studies | Prospective and retrospective studies including people with psychosis or admissions to psychiatric ward were used (n = 21) | ||||
| Test / subgroup | Summary accuracy % (95% CI) | No. of participants (studies) | Prevalence median (range) | Implications | Quality and comments |
| Diagnosis of schizophrenia from all other diagnoses | Sensitivity 57.0 (50.4, 63.3) Specificity 81.4 (74.0, 87.1) | 5079 (20) | 48% (15% to 84%) | With a prevalence of 48%, 48 out of every 100 patients will have schizophrenia. Of these, 21 will be missed by FRS (43% of 48). Of the 52 patients without schizophrenia, 10 may be incorrectly diagnosed with schizophrenia. | Important issues regarding patient selection, use of index test and reference standard were not clearly reported, leading to uncertainty in the results. Most studies were conducted in a research setting, rather than a clinical setting. |
| Diagnosis of schizophrenia from other types of psychosis | Sensitivity 58.0 (50.3, 65.3) Specificity 74.7 (85.2, 82.3) | 4070 (16) | 57% (24% to 84%) | With a prevalence of 57%, 57 out of every 100 patients will have schizophrenia. Of these, 24 will be missed by FRS (42% of 57). Of the 43 patients without schizophrenia, 13 may be incorrectly diagnosed with schizophrenia. | Important issues regarding patient selection, use of index test and reference standard were not clearly reported, leading to uncertainty in the results. Most studies were conducted in a research setting, rather than a clinical setting. |
| Diagnosis of schizophrenia from non‐psychotic disorders | Sensitivity 61.8 (51.7, 71.0) Specificity 94.1 (88.0, 97.2) | 1652 (7) | 55% (19% to 89%) | With a prevalence of 55%, 55 out of every 100 patients will have schizophrenia. Of these, 21 will be missed by FRS (38% of 55). Of the 45 patients without schizophrenia, 3 may be incorrectly diagnosed with schizophrenia. | Important issues regarding patient selection, use of index test and reference standard were not clearly reported, leading to uncertainty in the results. Most studies were conducted in a research setting, rather than a clinical setting. |
| CAUTION: The results on this table should not be interpreted in isolation from the results of the individual included studies contributing to each summary test accuracy measure. These are reported in the main body of the text of the review. | |||||
FRS: first rank symptoms
Background
Target condition being diagnosed
Schizophrenia is a psychotic disorder that can occur as a single episode of illness, although the majority of sufferers have remissions and relapses, and for many sufferers the condition becomes chronic and disabling (Bustillo 2001). The most effective method of treatment is antipsychotic medication. These medications produce various side effects (Kane 2001) so low doses, used in as timely a fashion as possible, are indicated. There is some evidence to suggest that early intervention for people with schizophrenia can be beneficial, helping avoid or postpone damaging relapses and the need for prolonged use of medications (Marshall 2011). Early and accurate diagnostic techniques would have particular utility (Marshall 2011).
Index test(s)
The index test being evaluated in this review are Schneider’s First Rank Symptoms (FRS), which include: auditory hallucinations; thought withdrawal, insertion and interruption; thought broadcasting; somatic hallucinations; delusional perception; feelings or actions as made or influenced by external agents (Schneider 1959, Table 2). These are the so‐called positive symptoms, i.e. they are symptoms not usually experienced by people without schizophrenia, and are usually given priority among other positive symptoms. Negative symptoms are deficits of emotional responses or other thought processes. These positive symptoms of first rank are currently incorporated into the major operationalised diagnostic systems of the International Statistical Classification of Diseases‐10 (ICD‐10) (Table 3) and Diagnostic and Statistical Manual of Mental Disorder‐III‐IV (DSM‐III‐IV) (Table 4). These systems, however, go beyond the relatively simple list produced by Schneider.
1. Schneider First Rank Symptoms.
| First rank symptom | Definition | Example |
| Auditory hallucinations | Auditory perceptions with no cause. These auditory hallucinations have to be of particular types: |
|
| hearing thoughts spoken aloud | "I hear my thoughts outside my head." | |
| hearing voices referring to himself/herself made in the third person | "The first voice says 'He used that fork in an odd way' and then the second replies 'Yes, he did'". | |
| auditory hallucinations in the form of a commentary | "They say 'He is sitting down now talking to the psychiatrist'". | |
| Thought withdrawal, insertion and interruption | A person's thoughts are under control of an outside agency and can be removed, inserted (and felt to be alien to him/her) or interrupted by others. | "My thoughts are fine except when Michael Jackson stops them." |
| Thought broadcasting | As the person is thinking everyone is thinking in unison with him/her. | "My thoughts filter out of my head and everyone can pick them up if they walk past." |
| Somatic hallucinations | A hallucination involving the perception of a physical experience with the body | "I feel them crawling over me." |
| Delusional perception | A true perception, to which a person attributes a false meaning. | A perfectly normal event such as the traffic lights turning red may be interpreted by the patient as meaning that Martians are about to land. |
| Feelings or actions experienced as made or influenced by external agents | Where there is certainty that an action of the person or a feeling is caused not by themselves but by some others or other force. | "The CIA controlled my arm." |
2. ICD‐10 criteria for schizophrenia.
| Although no strictly pathognomonic symptoms can be identified, for practical purposes it is useful to divide symptoms into groups that have special importance for the diagnosis and often occur together, such as: |
| a) thought echo, thought insertion or withdrawal, and thought broadcasting; |
| b) delusions of control, influence, or passivity, clearly referred to body or limb movements or specific thoughts, actions, or sensations; delusional perception; |
| c) hallucinatory voices giving a running commentary on the patient's behaviour, or discussing the patient among themselves, or other types of hallucinatory voices coming from some part of the body; |
| d) persistent delusions of other kinds that are culturally inappropriate and completely impossible, such as religious or political identity, or superhuman powers and abilities (e.g. being able to control the weather, or being in communication with aliens from another world); |
| e) persistent hallucinations in any modality, when accompanied either by fleeting or half‐formed delusions without clear affective content, or by persistent over‐valued ideas, or when occurring every day for weeks or months on end; |
| f) breaks or interpolations in the train of thought, resulting in incoherence or irrelevant speech, or neologisms; |
| g) catatonic behaviour, such as excitement, posturing, or waxy flexibility, negativism, mutism, and stupor; |
| h) "negative" symptoms such as marked apathy, paucity of speech, and blunting or incongruity of emotional responses, usually resulting in social withdrawal and lowering of social performance; it must be clear that these are not due to depression or to neuroleptic medication; |
| i) a significant and consistent change in the overall quality of some aspects of personal behaviour, manifest as loss of interest, aimlessness, idleness, a self‐absorbed attitude, and social withdrawal. |
| The normal requirement for a diagnosis of schizophrenia is that a minimum of one very clear symptom (and usually two or more if less clear‐cut) belonging to any one of the groups listed as (a) to (d) above, or symptoms from at least two of the groups referred to as (e) to (h), should have been clearly present for most of the time during a period of 1 month or more. Conditions meeting such symptomatic requirements but of duration less than 1 month (whether treated or not) should be diagnosed in the first instance as acute schizophrenia‐like psychotic disorder and are classified as schizophrenia if the symptoms persist for longer periods. |
ICD: International Statistical Classification of Diseases
3. DSM‐IV criteria for schizophrenia.
| A* |
Characteristic symptoms: Two or more of the following, each present for a significant portion of time during a one‐month period:
|
| B | Social/occupational dysfunction: Since the onset of the disturbance, one or more major areas of functioning, such as work, interpersonal relations, or self‐care, are markedly below the level previously achieved. |
| C | Duration: Continuous signs of the disturbance persist for at least six months. This six‐month period must include at least one month of symptoms (or less if successfully treated) that meet Criterion A. |
| D | Exclusion of schizoaffective disorder and mood disorder with psychotic features. |
| E | Substance/general medical condition exclusion: the disturbance is not due to the direct physiological effects of a substance (e.g. a drug of abuse, a medication) or a general medical condition. |
| F | Relationship to a pervasive developmental disorder: If there is a history of autistic disorder or another pervasive development disorder, the diagnosis of schizophrenia is made only if prominent delusions or hallucinations are also present for at least a month (or less if successfully treated). |
| * Only one Criterion A symptom is required if delusions are bizarre or hallucinations consist of a voice keeping up a running commentary on the person's behaviour or thoughts, or two or more voices conversing with each other. | |
DSM: Diagnostic and Statistical Manual of Mental Disorder
The presence of even one of these first rank symptoms is said to be strongly suggestive of schizophrenia (Schneider 1959) and it is postulated that this may be symptomatically sufficient for a diagnosis of schizophrenia. As such, these signs or symptoms are often not difficult to illicit by healthcare professionals with some minimal training. They are low technology and, potentially, high utility. If of diagnostic value, they could be employed world‐wide.
We examined whether the presence of any one FRS or multiple FRSs, are a useful diagnostic tool to differentiate schizophrenia from other psychotic disorders. FRS, however, have been described in subsequent studies in people with other psychiatric diagnoses such as mood disorders with psychotic symptoms, thus raising doubts about their specificity for schizophrenia (Koehler 1978; Koehler 1979).
Clinical pathway
For someone with psychotic symptoms, if it is the first time they have experienced delusions or hallucinations, they would be considered to have 'first episode psychosis'. People typically present to primary care or emergency services from where they are referred to specialists ‐ Early Intervention Teams in the UK and similar secondary care services elsewhere. A specific diagnosis of 'schizophrenia' is made only after several months of longitudinal observation using widely accepted nosological criteria (ICD or DSM). Once someone has received such a diagnosis this has major treatment, psychological and social implications. People may be treated with antipsychotic medications, which carry risk of serious adverse effects, may be treated for long periods, and a person's life course may alter. A diagnosis of schizophrenia is thought to be useful ‐ swiftly communicating much information about the person's condition ‐ but it carries with it a stigma. Accurate diagnosis is important.
The onset of schizophrenia is usually in adolescence or early adulthood and around seven people out of 1000 will be affected during their lifetime (McGrath 2008); the lifetime prevalence of the illness is around 0.5% to 1%. Confirmation of diagnosis is largely determined by symptom stability (of psychosis and of FRS) and, at least in a majority of cases, a deteriorating course (i.e. not reaching pre‐morbid levels of functioning). Five subtypes of schizophrenia have been described: paranoid, disorganised, catatonic, undifferentiated and residual type but none are clearly discrete nor allow confident prediction of the long‐term course of the disease. However, insidious slow onset of illness lasting for several months is associated with a poor prognosis when compared with acute onset linked to stress and lasting only a few weeks (Lawrie 2004). Within five years of the initial episode the clinical pathway tends to be clear. Around 20% of those with clear symptoms of schizophrenia at initial diagnosis recover and do not have relapses. Another 20% have a chronic and unremitting course. The remainder have a relapsing illness the pattern of which tends to be set within the first five years of illness, with reasonable recovery in between. Approximately five per cent of patients will end their own lives ‐ often early in the illness (Hor 2010).
Prior test(s)
It is unlikely that an individual would have had any other test before being examined using FRS.
Role of index test(s)
Schneider's efforts helped make diagnoses more operational, although use of the checklist was never free of criticism because of concerns regarding false positive diagnoses (Koehler 1978) and, therefore, potentially damaging miss‐labelling (Koehler 1979). Although the ICD and DSM operational criteria have superseded Schneider's list in many areas, the simple Schneider checklist needs more careful consideration of patient history to apply, and it is therefore of value. Furthermore, the Schneiderian list still forms a core of psychopathological training worldwide. This is particularly true in regions where health care workers are not highly trained and where access to specialists is limited. In these situations, FRS can certainly be used to triage the seriously mentally ill for further consideration by more specialised services.
Alternative test(s)
Alternative tests for schizophrenia include operational criteria: the International Statistical Classification of Diseases (ICD‐9 or ICD‐10) (Table 3); Diagnostic and Statistical Manual of Mental Disorder (DSM‐III or DSM‐IV) (Table 4); Feighner (Feighner 1972); Research Diagnostic Criteria (Spitzer 1978); Carpenter criteria (Carpenter 1973); New Haven (Astrachan 1974); Taylor Abrams (Taylor 1978); Bleulerian (Bleuler 1950) and/or ego function (Bellak 1973).
Largely, these operational criteria have superseded Schneider's list and confirm diagnosis of schizophrenia by determining symptom stability (of psychosis and of FRS) and (at least in a majority) a deteriorating course (not reaching pre‐morbid levels of functioning). These operational criteria that incorporate FRS whilst confirming longitudinally are also likely to be the current reference standard. The new DSM‐5, however, is moving away from special treatment of Schneiderian first rank symptoms (Tandon 2013) to very diagnostic stipulations, "raising the symptom threshold" and necessitating considerably more skill to elicit than the relatively simple FRS.
Rationale
Early and accurate diagnosis and treatment of schizophrenia may have long‐term advantages for the patient (De Haan 2003); there is also evidence that the longer psychosis goes unnoticed and untreated the more severe the repercussions for relapse and recovery (Bottlender 2003). If schizophrenia is not really the diagnosis, embarking on a schizophrenia treatment path could be very deleterious, due to the stigma associated with a diagnosis of schizophrenia and having intrusive treatment with considerable physical, social and psychological adverse effects. Furthermore, if the correct diagnosis is another psychotic disorder with some symptoms similar to schizophrenia ‐ the most likely being bipolar disorder – treatment tailored to schizophrenia may cause symptoms to be ignored and appropriate treatment delayed, with possible severe repercussions for the person involved and their family.
There is widespread uncertainty about the diagnostic specificity and sensitivity of the ubiquitous FRS; therefore, we determined to examine whether they are a useful diagnostic tool to help triage which patients need to be assessed by a qualified professional. This would be particularly relevant in settings where healthcare workers are not highly trained and where access to specialists is limited.
This review is part of a series of Cochrane reviews using the same methodology to assess the diagnostic accuracy of tests for schizophrenia, such as the Operational Criteria Checklist for Psychotic Illness and Affective Illness (OPCRIT+) (Bergman 2014) and the brain imaging analysis technique voxel‐based morphometry (Palaniyappan 2014).
Objectives
To determine the diagnostic accuracy of one or multiple FRS for diagnosing schizophrenia, verified by clinical history and examination by a qualified professional (e.g. psychiatrists, nurses, social workers), with or without the use of operational criteria and checklists, in people thought to have non‐organic psychotic symptoms.
Methods
Criteria for considering studies for this review
Types of studies
We included both retrospective and prospective studies, which consecutively or randomly selected participants. We excluded case‐control studies that used healthy controls.
Studies were included that evaluated the diagnostic accuracy of First Rank Symptoms (one or multiple) for diagnosis of schizophrenia compared with a reference standard, irrespective of publication status and language.
Participants
We included adolescents and adults presenting with psychotic symptoms, which included symptoms such as, hallucinations, delusions, disordered thinking and speech, grossly disorganised or catatonic behaviour, or negative symptoms (i.e. affective flattening, alogia, or volition). We did not exclude on the grounds of co‐morbidities. In addition, if a study reported all admissions to a psychiatric ward instead of only people admitted with psychosis, the study, including those participants with non‐psychotic symptoms, was not excluded. We did exclude if participants had organic source of psychosis, such as that triggered by an existent physical disease or alcohol and drug abuse.
Particular attention was paid to history, current clinical state (acute, post‐acute or quiescent), stage of illness (prodromal, early, established, late), or if there were predominant clinical issues (negative or positive symptoms). In addition, setting and referral status of people in the study was noted. We recognise that people in psychiatric hospital have already experienced a considerable degree of prior testing compared with those in community settings. Also, for similar reasons, people referred to a specialist centre treating only those with schizophrenia may well be different to those in general care.
Index tests
Schneider First Rank Symptoms (Table 2). The presence of any one of these symptoms, or multiple symptoms, would be indicative of a diagnosis of schizophrenia. We consider this an acceptable variation in threshold as Kurt Schneider proposed that presence of any one of these symptoms was diagnostic of schizophrenia as long as the person was free of other organic causes such as substance misuse, epilepsy or tumours (Schneider 1959). The different value of one symptom over another is not the focus of this review.
Target conditions
All types of schizophrenia disorder regardless of descriptive subcategory (e.g. paranoid, disorganised, catatonic, undifferentiated and residual). Studies that reported results combined for diagnoses related to schizophrenia (e.g. schizoaffective and schizophreniform disorder) in which data could not be separated were included and we investigated potential heterogeneity.
Reference standards
The reference standard is history and clinical examination collected by a qualified professional (e.g., psychiatrists, nurses, social workers), which may or may not involve the use of operational criteria or checklists of symptoms such as:
International Statistical Classification of Diseases (ICD‐9 or ICD‐10) (Table 3);
Diagnostic and Statistical Manual of Mental Disorder (DSM‐III or DSM‐IV) (Table 4);
Feighner (Feighner 1972);
Research Diagnostic Criteria (Spitzer 1978);
Carpenter criteria (Carpenter 1973);
New Haven (Astrachan 1974);
Taylor Abrams (Taylor 1978);
Bleulerian (Bleuler 1950) and/or ego function (Bellak 1973).
The more modern of these criteria involve some degree of follow‐up.
Ideally, in order to avoid incorporation bias the reference standard and the diagnostic test under consideration should be entirely independent of one another (Worster 2008). We were not be able to avoid incorporation bias with this review, as in most cases the reference standard incorporated FRS and hence the diagnostic accuracy may potentially be overestimated (Worster 2008). Also, in many cases using FRS also included taking a history and clinical examination, again contaminating the uniqueness of either approach. Differences between FRS and the reference standard lies in utilisation of:
a longitudinal frame work in addition to the cross sectional assessment of specific symptoms of psychosis such as FRS (reflecting limbic system abnormalities); and
less specific symptoms of psychosis such as the consequences of having acute psychotic symptoms and the deleterious effects of psychosis.
Heterogeneity due to whether FRSs or any operational criteria were used as part of the reference standard was investigated.
Search methods for identification of studies
Electronic searches
We conducted searches in MEDLINE, EMBASE, and PsycInfo using OvidSP (see Table 5 for full details of the peer‐reviewed search strategies) in April, June, July 2011 and December 2012. We also searched MEDION in December 2013. At the time of writing the protocol for this review there was no verified method of developing search strategies for DTA reviews. We decided to carry out our searches in phases while developing the search strategies with guidance from the Cochrane DTA Group. As there was a time lag between the phases and we did not want to miss any potentially relevant references, we did not apply any time limitation for the later phases. For the later phases of each database search, de‐duplication was carried out against the previous search phases before screening commenced.
4. Search strategies.
| Database | Phase and date | Search strategy |
| MEDLINE (OvidSP) | Phase I Date: 13‐04‐11 |
1 first‐rank.mp. 2 first rank.mp. 3 first?rank.mp. 4 FRS$.mp. 5 Schneiderian.mp 6 1 or 2 or 3 or 4 or 5 (2137) |
| Phase II Date: 01‐06‐11 |
1 exp "International Classification of Diseases"/ (3305) 2 exp "Diagnostic and Statistical Manual of Mental Disorders"/ (9349) 3 "Research Diagnostic Criteria".mp. (1325) 4 Feighner.mp. (147) 5 ICD.mp. (13774) 6 DSM.mp. (29660) 7 RDC.mp. (1143) 8 schneider.mp. (1529) 9 bleuler.mp. (215) 10 kraepelin.mp. (495) 11 "international pilot study of schizophrenia".mp. (47) 12 IPSS.mp. (1436) 13 "new haven schizophrenia index".mp. (13) 14 NHSI.mp. (14) 15 "present state examination".mp. (412) 16 PSE.mp. (1394) 17 "operational criteria".mp. (431) 18 (operation$ adj3 criteri$).mp. [mp=protocol supplementary concept, rare disease supplementary concept, title, original title, abstract, name of substance word, subject heading word, unique identifier] (1077) 19 "Sensitivity and Specificity"/ (233760) 20 Diagnosis/ (15703) 21 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (303793) 22 exp Schizophrenia/ (74720) 23 schizophren$.mp. (93319) 24 22 or 23 (93528) 25 21 and 24 (7401) 26 (animals not (humans and animals)).sh. (3503422) 27 25 not 26 (7398) |
|
| Phase III Date: 17‐07‐11 |
1 *schizophrenia/di [Diagnosis] (16918) | |
| EMBASE (OvidSP) | Phase I Date: 13‐04‐11 |
1 first‐rank.mp. 2 first rank.mp. 3 first?rank.mp. 4 FRS$.mp. 5 Schneiderian.mp 6 1 or 2 or 3 or 4 or 5 (456) |
| Phase II Date: 01‐06‐11 |
1 exp "International Classification of Diseases"/ (5070) 2 exp "Diagnostic and Statistical Manual of Mental Disorders"/ (17196) 3 "Research Diagnostic Criteria".mp. (1436) 4 Feighner.mp. (161) 5 ICD.mp. (20919) 6 DSM.mp. (38725) 7 RDC.mp. (1310) 8 schneider.mp. (2302) 9 bleuler.mp. (293) 10 kraepelin.mp. (661) 11 "international pilot study of schizophrenia".mp. (40) 12 IPSS.mp. (2881) 13 "new haven schizophrenia index".mp. (12) 14 NHSI.mp. (22) 15 "present state examination".mp. (447) 16 PSE.mp. (1625) 17 "operational criteria".mp. (557) 18 (operation$ adj3 criteri$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword] (1358) 19 "Sensitivity and Specificity"/ (139513) 20 Diagnosis/ (544275) 21 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (755543) 22 exp Schizophrenia/ (110049) 23 schizophren$.mp. (120515) 24 22 or 23 (121863) 25 21 and 24 (12378) 26 Human/ (12332237) 27 nonhuman/ (3642333) 28 26 and 27 (656673) 29 27 not 28 (2985660) 30 25 not 29 (12368) |
|
| Phase III Date: 17‐07‐11 |
1 *schizophrenia/di [Diagnosis] (12453) | |
| PsycINFO (OvidSP) | Phase I Date: 13‐04‐11 |
1 first‐rank.mp. 2 first rank.mp. 3 first?rank.mp. 4 FRS$.mp. 5 Schneiderian.mp 6 1 or 2 or 3 or 4 or 5 (588) |
| Phase II Date: 01‐06‐11 |
1 exp "International Classification of Diseases"/ (747) 2 "Research Diagnostic Criteria".mp. (1393) 3 Feighner.mp. (169) 4 ICD.mp. (4427) 5 DSM.mp. (42426) 6 RDC.mp. (392) 7 schneider.mp. (1283) 8 bleuler.mp. (464) 9 kraepelin.mp. (736) 10 "international pilot study of schizophrenia".mp. (68) 11 IPSS.mp. (53) 12 "new haven schizophrenia index".mp. (20) 13 NHSI.mp. (7) 14 "present state examination".mp. (811) 15 PSE.mp. (440) 16 "operational criteria".mp. (462) 17 (operation$ adj3 criteri$).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures] (810) 18 Diagnosis/ (25820) 19 "Research Diagnostic Criteria".mp. (1393) 20 exp "Diagnostic and Statistical Manual"/ (4184) 21 exp Research Diagnostic Criteria/ (122) 22 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 (72691) 23 exp SCHIZOPHRENIA/ (62498) 24 schizophren$.mp. (88734) 25 23 or 24 (88734) 26 22 and 25 (10364) 27 limit 26 to human (10180) |
|
| MEDION | Date: 24‐02‐11 02‐12‐13 |
(schizophrenia or schizophrenic or schizophreniform in title or abstract) or (psychosis or psychoses or psychotic in title or abstract) (11) |
All databases searched from inception.
All searches were undertaken, added to a common database and duplicates deleted.
We did not apply any restrictions based on language or type of document in the search. We used the 'multiple fields' search command for the OvidSP interface (.mp.) to search both text and database subject heading fields. To capture variations in suffix endings, the truncation operator ‘$’ was used.
The Cochrane Register of Diagnostic Test Accuracy Studies was not searched as the content had been covered by the other databases searched in this review, and because this resource was out of date at the time of the searches.
Searching other resources
Additional references were identified by manually searching references of included studies.
Data collection and analysis
Selection of studies
Review authors independently screened all titles and abstracts for eligibility. As there were 35,410 references to screen from the search, the screening was done by a team of review authors, see Contributions of authors and Acknowledgements for details. We retrieved full papers of potentially relevant studies, as well as review articles, if relevant, for manual reference search. NM and KSW independently reviewed full papers for eligibility according to the inclusion criteria detailed above. Abstracts, in the absence of a full publication, were included if sufficient data were provided for analysis. Any disagreements were resolved by discussion between NM and KSW and all decisions documented. If a consensus could not be reached, CEA or CD made the final decision regarding these studies.
Data extraction and management
Data extraction forms were developed using a web‐based software and piloted on a small selection of studies. NM and KSW, again working independently, completed data extraction forms for all included studies. Agreements and disagreements were recorded and resolved by discussion between NM and KSW. If a consensus could not be reached, CEA made the final decision regarding these studies.
We extracted the information on study characteristics listed in Table 6.
5. Study characteristics.
| Study Details | First author, year, publication status, country, aim of study |
| Patient characteristics and setting | Number of participants included in study and number in analysis Description of participants in the study (age, gender, ethnicity, comorbid disorders, duration of symptoms, and concurrent medications used) Predefined inclusion and exclusion criteria Study aim Previous treatment for schizophrenia Clinical setting Country |
| Index test | Description of FRS used Professionals performing test Resolution of discrepancies How FRS used in study |
| Target condition and reference standard(s) | Reference standard Target condition(s) Professionals performing test Resolution of discrepancies |
| Flow and timing | Study process Follow‐up |
FRS: first rank symptoms
We recorded the number of true positive (TP), true negative (TN), false positive (FP), false negative (FN) to construct a 2 x 2 table for each study for differentiating schizophrenia from other diagnoses, from other psychotic diagnoses and from non‐psychotic diagnoses. If such data were not available, we attempted to derive them from summary statistics such as sensitivity, specificity, and/or likelihood ratios if reported. We treated data as dichotomous. Where data were available for one and/or multiple FRS, or at several time points, we recorded these.
Assessment of methodological quality
We used QUADAS‐2 (Quality Assessment of Diagnostic Accuracy Studies), an updated version of the original QUADAS tool for the assessment of quality in systematic reviews of diagnostic accuracy studies (Whiting 2011). The QUADAS‐2 tool is made up of four domains: patient selection, index test, reference standard, and flow and timing. We tailored the tool to our review, which was used to judge the risk of bias and applicability of included studies. Included studies were assessed by NM and KSW, working independently using a form that we piloted on a small selection of studies. The inter‐rater agreement was then measured and the form adapted (see Appendix 1). It was then applied to the other included studies. Any disagreements were resolved by consensus with CEA and CD.
The results of the quality assessment were used to describe the internal validity and external validity (applicability)of the included studies. The results were also used to make recommendations for the design of future studies. We are aware that quality rating is important but also that it is problematic to pre‐define cut‐off points beyond which inclusion of data would be contraindicated. We, therefore, did not use QUADAS‐2 other than to help the qualitative commentary.
Statistical analysis and data synthesis
Estimates of sensitivity and specificity from each study were plotted in receiver operating characteristic (ROC) space and forest plots for visual assessment of variation in test accuracy were constructed. Meta‐analyses were performed using the SAS (SAS Institute Inc., Cary, NC, USA) program MetaDAS to fit the bivariate model, which was developed by Takwoingi (Takwoingi 2010) adapting program codes by Macaskill (Macaskill 2004). The program incorporates the precision by which sensitivity and specificity have been measured in each study (Reitsma 2005) and fits the model based on the generalised linear mixed model approach proposed by Chu and Cole (Chu 2006), allowing the automated fitting of bivariate and HSROC models. The bivariate model was used based on that all the included studies had a common test threshold.
Summary estimates were obtained for sensitivity and specificity of differential diagnosis of schizophrenia using FRS and diagnosis by a psychiatrist. Where the bivariate model failed to converge in SAS, we refitted the model using xtmelogit in Stata 12 (StataCorp, College Station, Texas). Parameter estimates were entered into RevMan for generation of SROC plots. Additional plots were constructed using Stata 12.
Investigations of heterogeneity
Covariates and their subgroups were added into the bivariate model to investigate sources of heterogeneity by using the MetaDAS program. Assessment of the effect of covariate subgroups on sensitivity and/or specificity by comparing models with and without the covariate were performed using likelihood ratio tests to evaluate the statistical significance of differences in model fit.
We investigated the following possible sources of heterogeneity.
Whether operational criteria were used as part of the reference standard (abbreviated to ‘Criteria’)
Whether FRS were used as part of the reference standard (abbreviated to ‘FRS/RS’)
All psychotic and non‐psychotic admissions to a psychiatric ward or only people with psychoses (abbreviated to ‘Diagnosis’)
Whether the definition of schizophrenia in the study included schizoaffective and/or schizophreniform (abbreviated to ‘Psychosis’)
Test positivity threshold, i.e. number of FRS needed for a diagnosis of schizophrenia (abbreviated to ‘Number’)
Results were divided into the following diagnostic test types.
Schizophrenia from all other psychotic and non‐psychotic diagnoses
Schizophrenia from other types of psychosis
Schizophrenia from non‐psychotic disorders
Sensitivity analyses
Sensitivity analyses had been planned to investigate the impact of blinding when conducting the tests, but due to the limited number of studies that reported whether the testers were blinded, this was not possible and so could not be performed.
Assessment of reporting bias
It has previously been described that standard funnel plots and tests for publication bias are likely to be misleading for meta‐analysis of test accuracy studies (Deeks 2005), therefore no assessment of publication bias was carried out.
Results
Results of the search
We screened 32,755 potentially relevant references for inclusion. We excluded 32,127 references through title and abstract screening. An initial first round full text assessment of the remaining 628 references resulted in 507 references being excluded mainly because they were not diagnostic studies or FRSs were not being assessed. Following a second round of full text screening, a further 99 references were excluded (see Characteristics of excluded studies for details of reasons for exclusion). We included 21 studies (25 references; 4 were companion papers), and an additional study in German is awaiting assessment. See Figure 1 for an overview of the selection process.
1.
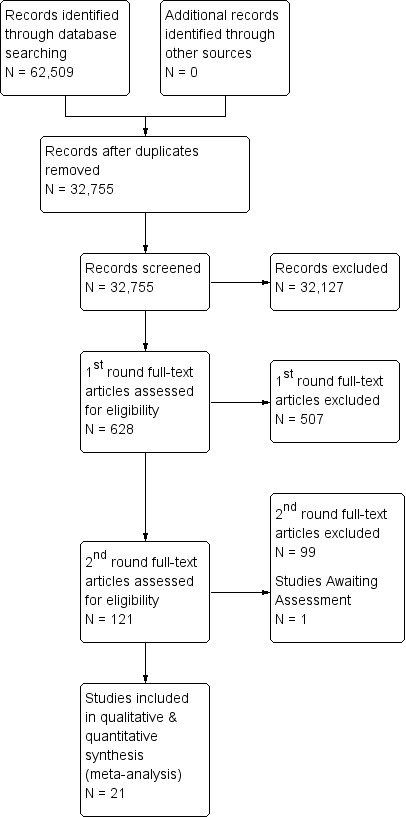
PRISMA flow diagram.
Included studies
1. Study Design
Seventeen studies were prospective and three studies were retrospective (Daradkeh 1995; Stephens 1980; Stephens 1982); Brockington 1978 included both a prospective sample and a retrospective sample of participants. Twelve studies consecutively enrolled participants, three randomly selected participants (Chandrasena 1987; Raguram 1985; Wu 1990); Stephens 1980 randomly selected participants from a previous study; Daradkeh 1995 also selected participants from a previous study, but did not report whether this was random;and four studies did not report how participants were enrolled (Brockington 1978; Rosen 2011; Salleh 1992; Tanenberg‐Karant 1995).
All included studies diagnosed participants with psychosis using an accepted reference standard, assessed the FRS of participants, and provided data that we could use to construct 2 x 2 tables. However, only five studies (Daradkeh 1995; Ihara 2009; Peralta 1999; Ramperti 2010l Salleh 1992) were specifically designed as diagnostic test accuracy studies. Seven studies aimed to investigate the utility of FRSs to diagnose participants, and eight measured the prevalence of FRSs in people diagnosed with schizophrenia. A single study (Preiser 1979) tested FRSs for assessing the prognosis of participants.
2. Setting
Sixteen studies were undertaken in inpatient settings, two in both inpatient and outpatient departments (Ihara 2009; Ramperti 2010), one in an outpatient setting (Raguram 1985); two studies did not report on setting (Daradkeh 1995; Rosen 2011).
Studies were conducted in the USA (six studies), UK (three studies), India (two studies), Spain (two studies), Australia, China, Ireland, Kenya, United Arab Emirates, and Malaysia. Carpenter 1974 was an international study including multiple sites (China (Taiwan), Colombia, Czechoslovakia, Denmark, India, Nigeria, USSR, UK, USA), and Chandrasena 1987 was a triple site study (Sri Lanka, UK, and Canada).
Studies were conducted from 1974 to 2011. Only four studies were conducted after 2000 (Gonzalez‐Pinto 2004; Ihara 2009; Ramperti 2010; Rosen 2011). Three studies were conducted in the 1970's (Brockington 1978; Carpenter 1974; Preiser 1979), eight in the 1980's (Chandrasena 1987; Chopra 1987; Ndetei 1983; Radhakrishnan 1983; Raguram 1985; Stephens 1980; Stephens 1982; Tandon 1987) and six in the 1990's (Daradkeh 1995; O'Grady 1990; Peralta 1999; Salleh 1992; Tanenberg‐Karant 1995; Wu 1990).
3. Participants
The included studies had a total of 6253 participants, although only 5515 were included in the analysis. Thirteen studies included only participants with psychosis. Seven studies included all admissions to psychiatric wards with psychotic and non‐psychotic symptoms (Ndetei 1983; O'Grady 1990; Preiser 1979; Radhakrishnan 1983; Stephens 1982; Tandon 1987; Wu 1990).
Six studies included people with first episode psychosis or first admissions to hospital (Gonzalez‐Pinto 2004;, Ihara 2009; Ndetei 1983; Ramperti 2010; Salleh 1992; Tanenberg‐Karant 1995); the duration of psychotic symptoms was not reported in the other 15 studies.
In 17 studies participants’ ages ranged from 16 to 89 years; four studies did not report on age. Thirteen studies included both males and females; this was not reported in the remaining studies. Most studies did not report details about participants’ ethnicity.
4. Index test
At least one FRS was needed to diagnose schizophrenia in 12 studies, and nine studies did not report the number of FRS needed for a diagnosis. For these studies we assumed the same threshold, at least one FRS.
Many studies did not specifically use FRSs to make a diagnosis of schizophrenia, but measured the prevalence of FRSs. For these studies, we assumed that the number of FRSs reported in the study was the number of FRSs needed to diagnose schizophrenia, e.g. if the prevalence was reported as number of people experiencing at least one FRS, we included this as at least one FRS to diagnose schizophrenia.
5. Reference standard
Four studies assessed patients' medical records to make a diagnosis (Brockington 1978; Ihara 2009; Stephens 1980; Stephens 1982), seven studies used both medical records and clinical interview, and nine studies used only clinical interview. Operational criteria were part of the reference standard in all studies apart from Brockington 1978 (See Characteristics of included studies for details). The reference standard included FRSs in 13 studies, and it was unclear in the remaining studies.
6. Target condition
Nine studies specified that their target condition was schizophrenia alone and did not include other schizophrenic‐like illnesses. Three studies also included schizoaffective and/or schizophreniform disorders in their definition of schizophrenia (Carpenter 1974; Ramperti 2010; Tanenberg‐Karant 1995). The remaining nine studies did not specify whether schizophrenia also included other types of schizophrenia‐like conditions.
Excluded studies
We excluded 99 reports, the majority for more than one reason: 50 studies were excluded because of insufficient data to construct 2 x 2 tables; 41 studies included only participants diagnosed with schizophrenia; 35 studies included participants who did not present with psychotic symptoms; 30 studies did not use the reference standard to separate those with schizophrenia from those without; 22 studies did not have FRS routinely performed on patients. See Characteristics of excluded studies for further details.
Awaiting assessment studies
Friedrich 1980 is in German and currently awaiting translation; see Characteristics of studies awaiting classification.
Ongoing studies
We found no ongoing studies.
Methodological quality of included studies
See also risk of bias and applicability concerns in Characteristics of included studies, Figure 2, and Figure 3for an overview of the assessment of risk of bias and applicability concerns for each of the 21 studies included in the review.
2.
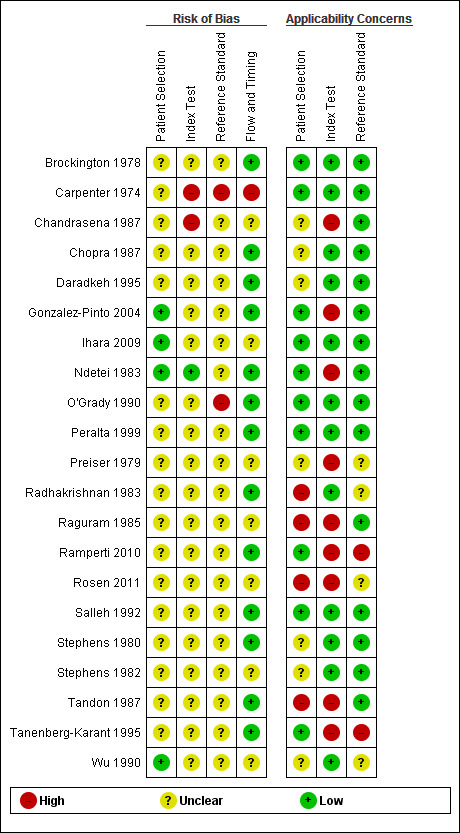
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study
3.
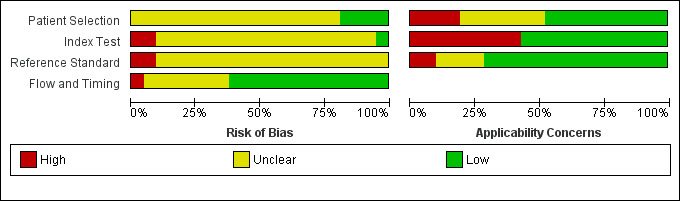
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies
1. Patient Selection
Twelve studies (57%) used a consecutive or random sample of patients; one study (Daradkeh 1995) selected participants from a previous study and in the remainder the method of selection of participants was unclear. Twelve studies (57%) did not use a case‐control design and nine studies (43%) either used a case‐control design or it was unclear whether this was the design. Eight studies (38%) avoided inappropriate exclusions and it was unclear how exclusions were managed in the remaining studies. As a result, 17 studies (81%) were considered as having an unclear risk of bias and four were low risk. In terms of applicability, we judged 10 included studies (48%) to be of low concern, four (19%) to be of high concern and the remaining to be of unclear applicability concerns.
2. Index test
Only seven studies (33%) reported that the index test results were interpreted without knowledge of the result of the reference standard, in one study (Carpenter 1974) the results were interpreted with knowledge of the reference standard, and in the remainder it was unclear. The number of FRSs required for a diagnosis of schizophrenia was only reported in seven studies (33%). As a result 17 studies (81%) were considered to be at unclear risk of bias, two (10%) to be high risk and only one low risk of bias. In terms of applicability, nine (43%) were judged as high concern because the aim of the studies was not to test FRSs specifically as a means of diagnosing schizophrenia, but to measure prevalence or to assess the prognosis of patients.
3. Reference standard
In 12 studies (57%), the reference standard was described and would correctly classify schizophrenia; nine studies (43%) did not clearly report what methods were used as the reference standard. Only three studies (14%) reported that the reference standard was interpreted without knowledge of the index test result, in four studies (19%) the person using the reference standard was unblinded to the results of the index test, and it was unclear in the remaining studies. As a result, all studies were rated as unclear or high risk of bias. In terms of applicability, six studies (29%) were considered as unclear or high concern as the target condition of schizophrenia as defined by the reference standard included schizophrenia‐like illnesses.
4. Flow and timing
We considered 13 studies (62%) to be of low concern for risk of bias since in most of these studies all participants received the same reference standard and the same index test, they accounted for all of their participants in the analysis, although 11 studies (52%) did not clearly report the interval between the reference standard and index test. One study was considered as high risk, as they did not apply the reference standard and index test to all participants and not all participants were included in the analysis. Seven studies (33%) had an unclear risk of bias on this domain due to insufficient reporting.
Findings
1. FRS to differentiate schizophrenia from all other psychotic and non‐psychotic diagnoses
Twenty studies (5079 participants) were included in the meta‐analysis. The median sample size was 146 (range 51 to 1119). Study sensitivities ranged from 27% to 78% and specificities from 39% to 94%. The summary sensitivity and specificity (95% CI) were 57.0% (50.4% to 63.3%) and 81.4% (74.0% to 87.1%) respectively (Data table 1; Figure 4).
1. Test.
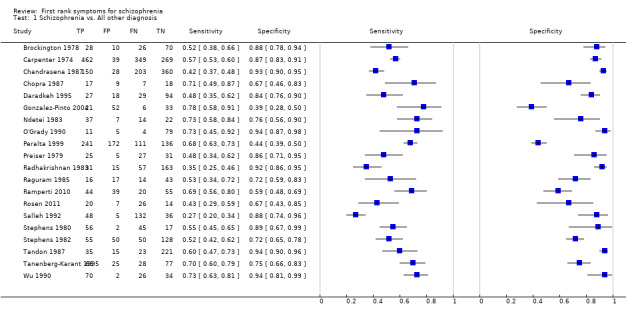
Schizophrenia vs. All other diagnosis.
4.
Summary ROC Plot of 1. FRS to differentiate schizophrenia from all other psychotic and non‐psychotic diagnoses
2. FRS to differentiate schizophrenia from other types of psychosis
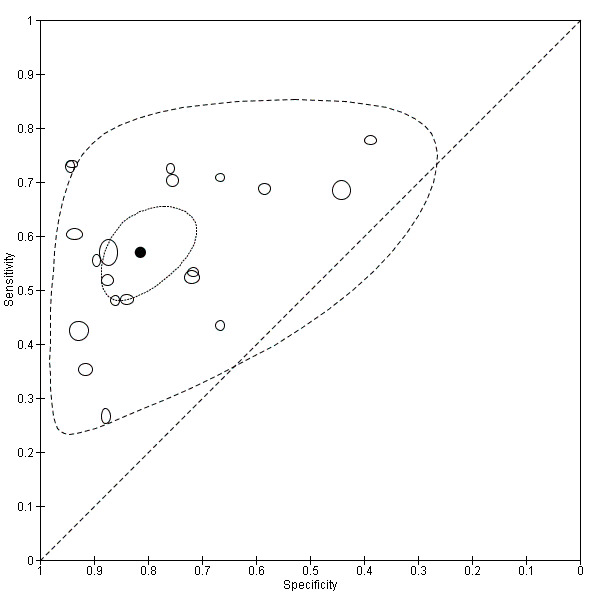
The meta‐analysis included 16 studies (4070 participants). The median sample size was 138 (range 30 to 996). Study sensitivities ranged from 27% to 78% and specificities from 33% to 93%. The summary sensitivity and specificity (95% CI) were 58.0% (50.3% to 65.3%) and 74.7% (65.2% to 82.3%) respectively (Data table 2; Figure 5).
2. Test.
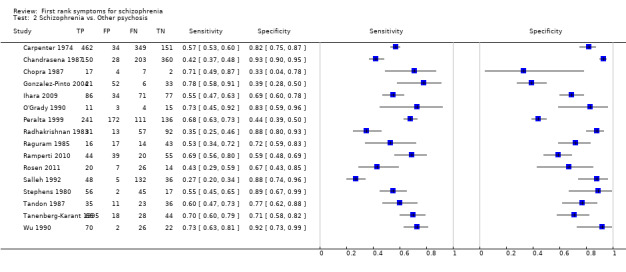
Schizophrenia vs. Other psychosis.
5.
Summary ROC Plot of 2. FRS to differentiate schizophrenia from other types of psychosis
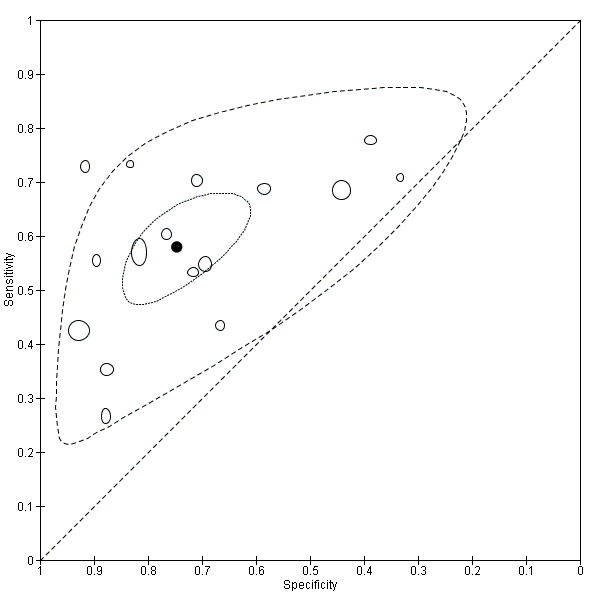
3. FRS to differentiate schizophrenia from non‐psychotic disorders
The meta‐analysis consisted of seven studies (1652 participants). The median sample size was 134 (range 45 to 934). Study sensitivities ranged from 35% to 73% and specificities ranges from 76% to 100%. The summary sensitivity and specificity (95% CI) were 61.8% (51.7% to 71.0%) and 94.1% (88.0% to 97.2%) respectively (Data table 3; Figure 6).
3. Test.
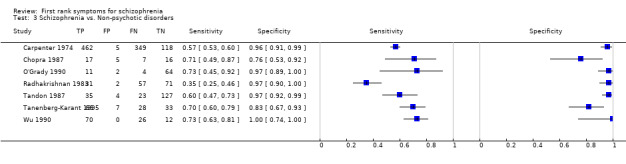
Schizophrenia vs. Non‐psychotic disorders.
6.
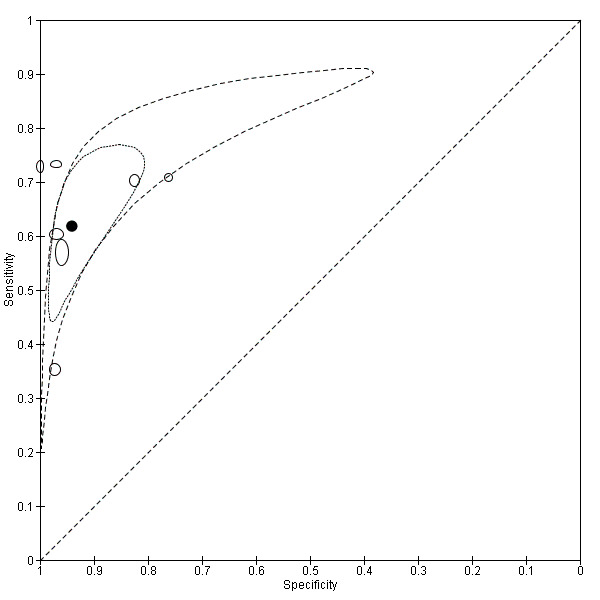
Summary ROC Plot of 3. FRS to differentiate schizophrenia from non‐psychotic disorders
Investigation of heterogeneity
We formally investigated the effect of the following covariates on sensitivity and specificity: operational criteria used as part of the reference standard; FRS used as part of the reference standard; all admissions to a psychiatric ward or with specific psychoses; if definition included schizoaffective and/or schizophreniform; and number of FRS needed for a diagnosis. Each covariate comprised of several subgroups, where adequate data allowed, these subgroups were investigated as sources of heterogeneity.
1. FRS to differentiate schizophrenia from all other psychotic and non‐psychotic diagnoses
The investigation of heterogeneity results for FRS to differentiate schizophrenia from all other psychotic and non‐psychotic diagnoses can be found in Table 7.
6. Investigations into heterogeneity between subgroups of tests using first rank symptoms to diagnose schizophrenia versus all other diagnoses.
| Schizophrenia versus all other diagnoses | Number of studies | Number of patients |
Summary of sensitivity % (95% CI) |
Summary of specificity % (95% CI) |
Likelihood Ratio Test1 (P‐value) |
|
| Operational criteria used as part of reference standard | DSM‐III | 4 | 1190 | 64.8 (54.3, 74.0) | 64.2 (52.8, 74.2) | 0.002 |
| ICD‐9 | 5 | 2515 | 42.0 (33.5, 51.0) | 89.8 (84.9, 93.2) | ||
| First rank symptoms used as part of reference standard | Unclear | 6 | 1629 | 60.9 (49.3, 71.4) | 85.3 (71.9, 93.0) | 0.3 |
| Yes | 13 | 3316 | 55.3 (47.2, 63.2) | 79.2 (69.2, 86.5) | ||
| All admissions to a psychiatric ward or with specific psychoses | All hospitalised | 8 | 1293 | 59.7 (49.2, 69.4) | 86.7 (77.3, 92.6) | 0.1 |
| Psychosis only | 12 | 3786 | 55.6 (47.3, 63.5) | 77.2 (66.9, 85.0) | ||
| If definition included schizoaffective and/or schizophreniform | Not reported | 9 | 1855 | 45.8 (38.4, 53.3) | 85.1 (75.1, 91.5) | 0.03 |
| Schizophrenic only | 7 | 1619 | 63.2 (54.4, 71.2) | 76.0 (60.6, 86.6) | ||
| Number of first rank symptoms needed for a diagnosis of schizophrenia | At least one | 10 | 3143 | 58.6 (49.5, 67.1) | 76.6 (65.0, 85.3) | 0.5 |
| Not reported | 9 | 1195 | 57.1 (47.1, 66.6) | 84.4 (74.2, 91.0) | ||
1Likelihood ratio test for model with and without covariate DSM: Diagnostic and Statistical Manual of Mental Disorder ICD: International Statistical Classification of Diseases
1.1 Covariate: “whether operational criteria were used as part of the reference standard” (Criteria)
This covariate contained 10 subgroups (Bleurian/ego (n = 1), Feighner's (n = 1), RDC (n = 3), DSM‐II (n = 1), DSM‐III (n = 4), DSM‐IV (n = 2), ICD (n = 5), 1984 Mt Huangshan (n = 1), New Haven (n = 1) and Not reported (n = 1)), however only two subgroups: ICD criteria (ICD‐8 n = 1, ICD‐9 n = 3 and ICD‐10 n = 1) and DSM‐III criteria (n = 4) had enough data to enable statistical analyses. There was a statistically significant difference (P = 0.002) in sensitivity and specificity for FRS to detect schizophrenia when studies used DSM‐III or ICD as reference standard. FRS to detect schizophrenia showed higher sensitivity but lower specificity when DSM‐III criteria were used as reference standard compared to when ICD criteria were used as reference standard. The summary sensitivity of FRS to detect schizophrenia was 64.8% (54.3% to 74.0%) with DSM‐III as reference standard and 42.0% (33.5% to 51.0%) with ICD as reference standard. The summary specificity of FRS to detect schizophrenia with DSM‐III as reference standard was 64.2% (52.8% to 74.2%) and with ICD as reference standard was 89.8% (84.9% to 93.2%).
1.2 Covariate: “whether FRS were used as part of the reference standard” (FRS/RS)
This covariate contained three subgroups (Yes, Unclear and Not reported) but only two of which, ‘yes’ (n = 13) and ‘unclear’ (n = 6) contained enough data to investigate heterogeneity. No statistical significance between these subgroups was detected (P = 0.3), indicating they are unlikely as a source of heterogeneity.
1.3 Covariate: “all psychotic and non‐psychotic admissions to a psychiatric ward or only people with psychoses” (Diagnosis)
This covariate contained two subgroups: ‘psychosis only’ (n = 12) and ‘all hospitalised’ (n = 8), both of which contained enough data to allow heterogeneity analysis. No statistical significance was found between these subgroups (P = 0.1), indicating these are unlikely as a source of heterogeneity.
1.4 Covariate: “whether the definition included schizoaffective and/or schizophreniform” (Psychosis)
This covariate contained four subgroups (Only schizophrenia, Schizophrenia plus others, Unclear and Not reported), but only two contained enough data to investigate heterogeneity: ‘not reported’ (n = 9) and ‘Schizophrenia only’ (n = 7). A statistically significant difference (P = 0.03) was found in sensitivity and specificity for FRS to detect schizophrenia when only schizophrenia was included in the definition for the diagnosis compared to when it was unclear what definition for the diagnosis was used. Findings indicated that when only schizophrenia was included in the diagnosis definition, sensitivity of FRS to diagnose schizophrenia increases but specificity decreases in comparison with tests where the definition used was not reported. The summary sensitivity was 45.8% (38.4% to 53.3%) for not reported definitions and 63.2% (54.4% to 71.2%) for the definition of schizophrenia only. The summary specificity was 85.1% (75.1% to 91.5%) for not reported definitions and 76.0% (60.6% to 86.6%) for a definition of schizophrenia only.
1.5 Covariate: “number of FRS needed for a diagnosis of Schizophrenia” (Number)
This covariate contained two subgroups: ‘at least 1’ (n = 8) and ‘not reported’ (n = 7). No statistical significance was found between these subgroups (P = 0.5), indicating these are unlikely as a source of heterogeneity.
2. FRS to differentiate schizophrenia from other types of psychosis
The investigation of heterogeneity results for FRS to differentiate schizophrenia from all other psychotic and non‐psychotic diagnoses can be found in Table 8.
7. Investigations of heterogeneity between subgroups of tests using first rank symptoms to diagnose schizophrenia versus other psychoses.
| Schizophrenia versus other psychoses | Number of studies | Number of patients | Summary sensitivity % (95% CI) |
Summary specificity % (95% CI) |
Likelihood Ratio Test[1] (P value) | |
| First rank symptoms used as part of reference standard: | Yes | 4 | 1326 | 60.9 (46.5, 736.) | 82.3 (65.0, 92.1) | 0.1 |
| Unclear | 12 | 2744 | 56.8 (48.1, 65.0) | 72.0 (60.6, 81.1) | ||
| All admissions to a psychiatric ward or with specific psychoses: | All hospitalised | 5 | 481 | 62.1 (47.8, 74.5) | 79.3 (62.0, 90.0) | 0.3 |
| Psychosis only | 11 | 3589 | 56.7 (47.7, 65.2) | 73.2 (61.1, 82.1) | ||
| If definition included schizoaffective and/or schizophreniform: | Not reported | 5 | 1312 | 39.6 (32.1, 47.6) | 85.3 (73.5, 92.4) | 0.004 |
| Schizophrenic only | 7 | 1328 | 63.3 (56.3, 69.9) | 63.6 (48.1, 76.7) | ||
| Number of first rank symptoms needed for a diagnosis of schizophrenia: | At least one | 8 | 2608 | 58.7 (48.0, 68.6) | 69.3 (56.9, 79.5) | 0.5 |
| Not reported | 7 | 721 | 59.8 (47.8, 70.8) | 76.6 (63.0, 86.3) | ||
1Likelihood ratio test for model with and without covariate
2.1 Covariate: “whether operational criteria were used as part of the reference standard” (Criteria)
This covariate contained seven subgroups (DSM‐II (n = 1), DSM‐III (n = 3), DSM‐IV (n = 3), Feighner's (n = 1), ICD (n = 5), RDC (n = 3) and 1984 Mt Huangshan (n = 1)). As only one subgroup had enough data points for analysis (ICD), no statistical testing for heterogeneity could be performed.
2.2 Covariate: “whether FRS were used as part of the reference standard” (FRS/RS)
This covariate contained two subgroups: ‘yes’ (n = 4) and ‘unclear’ (n = 12). No statistical significance was found between the subgroups (P = 0.1), indicating they unlikely as a source of heterogeneity.
2.3 Covariate: “all admissions to a psychiatric ward or people with specific psychosis” (Diagnosis)
This covariate contained two subgroups: ‘psychosis only’ (n = 11) and ‘all hospitalised’ (n = 5). No statistical significance was found between the subgroups (P = 0.3), indicating these subgroups are unlikely as a source of heterogeneity.
2.4 Covariate: “whether the definition included schizoaffective and/or schizophreniform” (Psychosis)
This covariate contained two subgroups: ‘not reported’ (n = 5) and ‘schizophrenic only’ (n = 7). There was a statistically significant difference (P = 0.004) in sensitivity and specificity for FRS to detect schizophrenia when only schizophrenia was included in the definition for the diagnosis compared to when it was unclear what definition for the diagnosis was used. Findings indicated that when only schizophrenia was included in the diagnosis definition, sensitivity of FRS to diagnose schizophrenia increases but specificity decreases in comparison with tests where the definition used was not reported. The summary sensitivity was 39.6% (32.1% to 47.6%) for not reported definitions and 63.3% (56.3% to 69.9%) for schizophrenia only as definition. The summary specificity was 85.3% (73.5% to 92.4%) for not reported definitions and 63.6% (48.1% to 76.7%) for schizophrenia only as definition.
2.5 Covariate: “number of FRS needed for a diagnosis of Schizophrenia” (Number)
This covariate had two subgroups: ‘at least one’ (n = 8) and ‘not reported’ (n = 7). No statistical significance was found between the subgroups (P = 0.5), indicating these are unlikely as a source of heterogeneity.
3. FRS to differentiate schizophrenia from non‐psychotic disorders
We planned to investigate sources of heterogeneity but due to the limited number of studies available for each covariate and their respective subgroups, but this was not possible.
Discussion
Summary of main results
This systematic review included a total of 21 studies evaluating the efficacy of FRS in diagnosing schizophrenia: 13 studies in people only with psychotic symptoms and eight studies in people with both psychotic and non‐psychotic symptoms who were admitted to a psychiatric ward. Only five studies were specifically designed as diagnostic test accuracy studies and the majority were based in a research rather than a clinical setting. The studies had a total of 6253 participants and 5515 were included in the analysis. Six studies included people with first episode psychosis or first admissions to hospital, although none reported the duration of symptoms. For the index test, just over half the studies diagnosed schizophrenia by the presence of at least one FRS, and the rest did not report the number of FRS needed for a diagnosis. The reference standard varied between studies and included clinical interview, medical records and operational criteria in various combinations. In nine studies, the target condition was schizophrenia alone, whereas three studies also included other schizophrenic‐like illnesses, and the remainder did not report this.
The quality assessments of the studies were mostly an unclear risk of bias regarding patient selection, use of index test and reference standard as important issues such as how patients were selected and the blinding of those conducting the tests were not reported. The reporting of the flow and timing of the studies was better and subsequently 62% were rated as a low risk of bias.
A summary of the results is given in Table 9, and details of the investigations of heterogeneity can be found in Table 7 and Table 8. Table 1 gives information on the quantity, quality and applicability of evidence as well as the accuracy of index test.
8. Summary sensitivity and specificity of first rank symptoms for diagnosis of schizophrenia.
| Test Comparison | Number of studies | Number of patients |
Summary sensitivity % (95% CI) |
Summary specificity % (95% CI) |
| Schizophrenia versus all other diagnoses | 20 | 5079 | 57.0 (50.4, 63.3) | 81.4 (74.0, 87.1) |
| Schizophrenia versus other types of psychosis | 16 | 4070 | 58.0 (50.3, 65.3) | 74.7 (85.2, 82.3) |
| Schizophrenia versus non‐psychotic disorders | 7 | 1652 | 61.8 (51.7, 71.0) | 94.1 (88.0, 97.2) |
1. FRS to differentiate schizophrenia from all other psychotic and non‐psychotic diagnoses
Twenty‐one studies reported results for diagnosing schizophrenia from all other diagnoses. The summary sensitivity was 57%, meaning that for every 100 people with schizophrenia the test will correctly identify 57 cases as positive for schizophrenia, therefore almost half of cases would be incorrectly diagnosed as not having schizophrenia. The summary specificity was better, at 81.4%, meaning that of 100 people without schizophrenia 81 would be found negative, but 19 would incorrectly receive a positive diagnosis for schizophrenia.
2. FRS to differentiate schizophrenia from other types of psychosis
Sixteen studies reported results for diagnosing schizophrenia from other types of psychosis. Results were very similar to schizophrenia from all other diagnoses, with the summary sensitivity slightly higher at 58%, meaning that for every 100 people with schizophrenia the test will find only 58 cases as positive for schizophrenia, therefore almost half of cases would be incorrectly diagnosed as not having schizophrenia. The results showed a slightly lower summary specificity of 76.7%, meaning that of 100 people without schizophrenia 77, would be found negative, but 23 would incorrectly receive a positive diagnosis for schizophrenia.
3. FRS to differentiate schizophrenia from non‐psychotic disorders
Seven studies reported results for diagnosing schizophrenia from non‐psychotic disorders. The results were only slightly better for summary sensitivity at 61.8%, meaning that for every 100 people with schizophrenia the test will find only 62 cases as positive for schizophrenia, and the remainder of cases would be incorrectly diagnosed as having a non‐psychotic disorder. The summary specificity was 94.1%, meaning that most people without schizophrenia would receive a negative schizophrenic diagnosis.
4. Investigations of heterogeneity
The investigations of heterogeneity between the subgroups showed no significant difference (P = 0.1) in sensitivity and specificity when admissions to a psychiatric ward was compared to those with specific psychoses, which might be expected, particularly in the studies conducted 20 to 30 years ago, in which most patients who were hospitalised would have psychotic symptoms or some severe mental health symptoms.
A significant difference (P = 0.002) was found when the reference standard including DSM‐III criteria were compared with reference standard including ICD (8, 9 and 10) criteria, with DSM‐III showing higher sensitivity but a lower specificity compared to the ICD criteria. Four out of the five ICD studies used ICD‐8 or ICD‐9, neither of which connect length of time to symptoms, whereas DSM‐III requires symptoms to have been present for at least six months. Furthermore, as only six studies included patients with a first psychotic episode, we cannot exclude the influence on diagnosis of patients having already been diagnosed with a chronic mental illness, and potentially previously received treatment. In addition, it is not possible to interpret the results for first rank symptoms used as part of reference standard and the number of first rank symptoms needed for a diagnosis of schizophrenia, as each subgroup was compared with studies that did not report this.
Strengths and weaknesses of the included studies
There were several limitations in the quality of included studies that may have lead to overestimation of test accuracy. The majority of included studies, although they provided useable data, were not designed to assess the diagnostic test accuracy of FRS. This meant that methodological details were often poorly reported, the enrolment of participants was not clearly stated and participants may have undergone some degree of selection to be included in the studies that does not reflect the range of patients that would present in clinical practice. The methodological quality of the studies was mostly rated as unclear due to these limitations, although the reporting for flow and timing was generally better with around half the studies rated as low risk of bias.
Primarily we were interested in studies that enrolled only participants with psychotic symptoms, although eight out of the 21 included studies enrolled all admissions to the psychiatric ward, meaning that other diagnoses were also present. However, subgroup analyses showed only a small difference in sensitivity and specificity when these studies were removed from the analysis.
There was a lack of consistency across the studies in the reporting of the reference standard and the type of reference standard when this was reported. Some studies reported that the reference standard was "medical records", and we had to presume that this meant a record of a clinical interview, which may have introduced bias.
Just over half the studies did not report the time interval between reference standard and index test. Out of the studies that did report the interval, only one retrospective study had an interval longer than four weeks.
A positive result for schizophrenia on the index test was defined as the presence of at least one FRS in 12 studies (57%). We assumed the same cut‐off for the remaining nine studies that did not report the number of FRSs required for a positive diagnosis of schizophrenia. There was no statistically significant difference between the studies that defined at least one and those that did not make a definition for how many FRS were required for a diagnosis (P = 0.5). Furthermore, eight studies were prevalence studies that reported the proportion of people with at least one FRS. For these studies we used "the proportion of people with at least one FRS" as a proxy for diagnosis of schizophrenia as it was the same cut‐off used in the diagnostic studies.
There were differences in what constituted a diagnosis of schizophrenia across studies, with three studies including schizoaffective and/or schizophreniform disorders and nine studies not reporting what was included.
Strengths and weaknesses of the review
The search strategy that we used was very wide and meant that we had over 35,000 references to screen. On the one hand, this meant that we feel certain that all possible studies were included, but on the other hand, the sheer volume of screening may have meant that some relevant studies may have been erroneously excluded. We have one article in German that is yet to be translated. There was some disagreement in selecting papers, as most of the eventually included studies were not specifically designed as diagnostic test accuracy studies, or included all admissions to the psychiatric ward as opposed to those with psychotic symptoms only, and therefore most of the final decisions to include studies took some discussion between review authors. We also found that the completion of QUADAS‐2 also involved discussion between review authors, mostly because the studies were again not designed as diagnostic test accuracy studies and many of the signalling questions were rated unclear due to lack of reporting of relevant details, which also made it difficult to judge the risk of bias of the QUADAS‐2 domains.
Although there was a large amount of heterogeneity of results across studies with wide ranges of sensitivity and specificity, the decision of pooling the results and obtaining a summary estimate was made to support those, particularly in low‐ and middle‐income countries, that might use FRS to triage patients. We caution, however, that in our investigations of heterogeneity, we identified significant sources of variability in the results, in particular, the variation in the reference standard used for the diagnosis (DSM‐III or ICD‐8, 9, or 10) (P = 0.002) and the variation in the spectrum of diseases evaluated together with schizophrenia (schizophrenia or schizophreniform and/or schizoaffective disorders) (P = 0.004). We also found that estimates of sensitivity were less precise than specificity because the number of those diagnosed positive was less than the number of those diagnosed negative. Further reasons may be the limited study quality and variation in the index test including its conduct and interpretation.
The diagnostic accuracies presented in this review may be overestimated as FRSs were part of the reference standard in at least 13 of the 21 included studies, However, there was no statistically significant difference (P = 0.3) between diagnostic accuracies for studies where FRSs were part of the reference standard and those where this was unclear. As no study specifically stated that FRSs were not part of the reference standard, this judgment is difficult to make.
Previous research
We know of no other reviews evaluating the diagnostic accuracy of FRSs.
Applicability of findings to the review question
Most (80%) of the 21 studies were conducted in the 1970's (three studies), 1980's (eight studies) and 1990's (six studies), and only four studies were conducted after the year 2000. We acknowledge that there could be an impact of time period on estimates of FRS sensitivity and specificity. This could be due to many reasons, including the change of reference standard, study population, and setting (please see Implications for research). However, when we crudely ordered data by time, there is little indication that this explains the heterogeneity (Figure not shown).
Most of the included studies were based in a research setting and most did not report how patients were selected for inclusion. The studies included both first episode psychosis patients and also those that already had a diagnosis. Only six studies (Gonzalez‐Pinto 2004; Ihara 2009; Ndetei 1983; Ramperti 2010; Salleh 1992; Tanenberg‐Karant 1995) exclusively included patients with first episode psychosis or first admissions, the population most likely to present for diagnostic evaluation in practice. These six studies found similar sensitivities and specificities of FRS to diagnose schizophrenia to the other studies that included a broader spectrum of psychoses (see, for instance, Figure 4).
For those studies that did report it, at least one FRS was used to diagnose schizophrenia. Although indicative of a serious mental disorder, it is not likely that in clinical practice the presence of one of these symptoms would be used to give a firm diagnosis of schizophrenia, and further diagnostic methods would be used.
The reference standard is representative of how schizophrenia is diagnosed, with studies using patient history, clinical interview and possibly operational criteria such as the DSM and ICD.
Authors' conclusions
Implications for practice.
The wide range of sensitivities and specificities makes summary estimates problematic. Routine use of FRS for triaging patients is likely to result in delayed treatment of some people with schizophrenia or unnecessary treatment of some others without the illness. However, clinical reality is such that in much of psychiatry practice in low‐ and middle‐income countries ‐ where 70% of the world's population live ‐ there are typical ratios of one psychiatrist to one million people (McKenzie 2004). In such situations FRS could remain a useful tool ‐ to help triage potential patients who need to be assessed by a qualified professional. The presence of FRS indicates schizophrenia as a possible diagnosis (as reflected in the inclusion of FRS in the DSM and ICD checklists), but does not exclude a possible diagnosis of other psychoses or non‐psychotic mental disorder.
FRS performs better at 'ruling out' rather than 'ruling in' schizophrenia. This review of FRS accuracy provides clinicians with valuable information to quantify the (moderate) performance of FRS for diagnosis of schizophrenia ‐ indicating the level of uncertainty that should be assigned to an FRS‐based provisional diagnosis. In reality, those with a positive diagnosis, including false positive, would undergo further assessment, even if this assessment, in situations of very limited health resources, was the passage of time. FRS, if used to triage, will identify ‐ to use broad figures related to our findings ‐ about five to 19 people per 100 as being 'FRS' schizophrenia and this will not turn out to be the case. However, it would seem that those five to 19 people, although not experiencing schizophrenia, would be quite disturbed in their behaviour and mental state and still merit some degree of specialist assessment and help.
For people who have schizophrenia, who have been misdiagnosed as not having schizophrenia (around 40%), they may experience a delay in treatment (again using a very broad figure related to our findings). A proportion will, because of disturbance (but not of the FRS type), nevertheless be offered assessment and, perhaps, treatment ‐ although neither may be offered with great confidence. Another group with what turns out to be the illness, if FRS triage is used thoughtlessly, could be discharged from the care from which they could benefit. Empathetic, considerate use of FRS as one diagnostic aid ‐ with known limitations ‐ should avoid a good proportion of this.
Implications for research.
Most studies were old, with 80% of the studies conducted in the 1970's, 1980's and 1990s', and most were not designed to investigate the accuracy of FRS in the diagnosis of schizophrenia. In any future update of this review, we would consider carrying out a regression analysis for time of publication and an investigation whether or not a diagnostic study design would contribute to any heterogeneity of results. Although we are confident that our extensive literature search was unlikely to have missed important studies for this review, and although FRS are highly prevalent in schizophrenia, we cannot recommend the use of FRS as a diagnostic test on its own for schizophrenia.
Arguably, the use of Schneider’s FRS to diagnose schizophrenia on its own, instead of part of another operational criteria, is unlikely to be practical or relevant. However, FRS could potentially still be utilised as a screening tool for serious mental health disorders in low‐income countries, where there is a need for simple, effective mental health screening tools. In many low‐income countries nurses are the first line of care; in some countries up to 90% of services, including diagnosing conditions and prescribing antipsychotic medication, is undertaken by nurses (WHO 2007), partly due to lack of trained psychiatrists (WHO 2007; WHO 2011). In Africa there are far fewer psychiatrists per capita with less than 0.05 per 10,000 people, compared to 1.1 psychiatrists per 10,000 people in Europe, with some countries, such as Eritrea, having no psychiatrists (WHO 2012). Future research could focus on the utility of FRS as an initial screening test by non‐psychiatrists in low‐resource settings as the presence of FRS indicate a serious mental disorder. In these settings we would recommend prospective diagnostic cohort studies in patients presenting to primary care or community health clinics with a first psychotic episode.
Acknowledgements
The authors would like to thank the support of the Diagnostic Test Accuracy Editorial Team throughout the protocol development, in particular to Yemisi Takwoingi for advise on statistical analysis methods.
We would also like to thank other members of the Enhance Review team who helped with screening and data extraction: Atoosa Khodabakhsh, Danielle Phoenix and Netta Weiser.
Appendices
Appendix 1. QUADAS 2
| DOMAIN 1: PATIENT SELECTION | |
| Risk of bias: Could the selection of patients have introduced bias? | |
| Signalling question | 1. Was a consecutive or random sample of patients enrolled? ‘Yes’ if a random sample of patients with suspected psychotic symptoms were included, or consecutive patients were enrolled ‘No’ if the patients were specifically selected (not random sample) to be included in the study ‘Unclear’ if insufficient information is provided |
| 2. Was a case‐control design avoided? ‘Yes’ participants did not have a specific diagnosis at entry to the study even if they had psychotic symptoms ‘No’ participants had a specific diagnosis at entry to the study ‘Unclear’ if insufficient information is provided | |
| 3. Did the study avoid inappropriate exclusions? ‘Yes’ the study explicitly states that there were no exclusions or there were no inappropriate exclusions ‘No’ some patients were inappropriately excluded e.g. if they were deemed “difficult‐to‐diagnose” patients ‘Unclear’ exclusions not explicitly reported in the study | |
| Applicability | |
| Signalling question | 1. Are there concerns that the included patients and setting do not match the review question? ‘No’ Included patients with psychosis but not a specific diagnosis ‘Yes’ Patients already had a specific diagnosis upon entry to study (e.g. inclusion criteria lists specific diagnoses) 'Unclear' Not enough information to decide |
| DOMAIN 2: INDEX TEST | |
| Risk of bias: Could the conduct or interpretation of the index test have introduced bias? | |
| Signalling question | 1. Were the index test results interpreted without knowledge of the results of the reference standard? ‘Yes’ if the index test was conducted before the reference standard, or if the person applying the index test was blinded to the results of the reference standard ‘No’ if the index test operator knew the results of the reference standard ‘Unclear’ if insufficient information is provided |
| 2. Did the study pre‐specify whether they were using one or multiple FRSs? ‘Yes’ if the study states the number of FRSs needed to be present to diagnose schizophrenia ‘No’ if the study does not state the number of FRSs they considered necessary to diagnose schizophrenia | |
| Applicability | |
| Signalling question | 1. Are there concerns that the index test, its conduct, or interpretation, differ from the review question? ‘No’ if FRSs are used for diagnosing schizophrenia ‘Yes’ if the study is not using FRSs for the diagnosis of schizophrenia, e.g. the prognosis of patients, or the prevalence of FRSs ‘Unclear’ if insufficient information is provided to judge the purpose of applying FRSs |
| DOMAIN 3: REFERENCE STANDARD | |
| Risk of bias: Could the reference standard, its conduct, or its interpretation have introduced bias? | |
| Signalling question | 1. Is the reference standard likely to correctly classify the target condition? ‘Yes’ if the history and clinical examination is conducted by a qualified professional (psychiatrist, nurse, social worker) ‘No’ if the history and clinical examination is conducted by insufficiently qualified individuals ‘Unclear’ if insufficient information is provided |
| 2. Were the reference standard results interpreted without knowledge of the results of the index test? ‘Yes’ if the reference standard was conducted before the index test, or if the person applying the reference standard was blinded to the results of the index test ‘No’ if the reference standard operator knew the results of the index test ‘Unclear’ if insufficient information is provided | |
| Applicability | |
| Signalling question | 1. Are there concerns that the target condition as defined by the reference standard does not match the question? ‘No’ if the paper specifically looks at diagnosing schizophrenia (regardless of subtypes) ‘Yes’ if the paper also includes schizophrenia‐like illnesses ‘Unclear’ if insufficient information is provided |
| DOMAIN 4: FLOW AND TIMING | |
| Risk of Bias: Could the patient flow have introduced bias? | |
| Signalling question | 1. Was there an appropriate interval between index test and reference standard? 'Yes' if reference standard and index text were applied in the same interview or within 4 weeks (applied more than once for chronic schizophrenia) 'No' if reference standard or index test were applied in different interviews beyond 4 weeks 'Unclear' if not enough information is given to assess whether there was an appropriate interval |
| 2. Did all patients receive a reference standard? 'Yes’ if all patients had details of history and clinical examination, with or without operational criteria ‘No’ if not all patients had a description of history and clinical examination ‘Unclear’ if insufficient information is provided | |
| 3. Did all patients receive the same reference standard? ‘Yes’ if all patients were diagnosed with history and clinical examination; and if any operational criteria were used, the same ones were applied to all patients and all received the same clinical follow up ‘No’ if all patients received history and clinical examination but only some received operational criteria, or different operational criteria ‘Unclear’ if insufficient information is provided | |
| 4. Were all patients included in the analysis? 'Yes' if there are no patients excluded from the analysis 'No' if there are patients excluded from the analysis 'Unclear' if not enough information is given to assess whether any patients were excluded from the analysis | |
Appendix 2. Graphical representations of covariate analyses
1. Schizophrenia vs all other diagnoses
a. Covariate ‐ Criteria
Figure 7
b. Covariate ‐ FRS/RS
Figure 8
c. Covariate ‐ Diagnosis
Figure 9
d. Covariate ‐ Psychosis
Figure 10
e. Covariate ‐ Number of FRS
Figure 11
2. Schizophrenia vs other diagnoses
a. Covariate ‐ FRS/RS
Figure 12
b. Covariate ‐ Diagnosis
Figure 13
c. Covariate ‐ Psychosis
Figure 14
d. Covariate ‐ Number of FRS
Figure 15
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
| Test | No. of studies | No. of participants |
|---|---|---|
| 1 Schizophrenia vs. All other diagnosis | 20 | 5079 |
| 2 Schizophrenia vs. Other psychosis | 16 | 4070 |
| 3 Schizophrenia vs. Non‐psychotic disorders | 7 | 1652 |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Brockington 1978.
| Study characteristics | |||
| Patient sampling | Retrospective, unclear patient selection. | ||
| Patient characteristics and setting |
N included in study: 134.
N in analysis: 134.
Age: Not reported.
Gender: Not reported.
Ethnicity: Not reported.
Comorbid disorders: Not reported.
Duration of symptoms: Not reported.
Concurrent medications used: Not reported. Inclusion criteria: Diagnosis of functional psychosis (schizophrenia, affective psychosis, paranoid state, or other/unspecified psychosis). Exclusion criteria: Children under 15 years, geriatric patients over 65 years and people suffering from addictions, neuroses or situational disturbances. Study aim: Compare 10 definitions of schizophrenia in respect of their reliability, concordance and prediction of outcome with two different samples of patients. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: UK. |
||
| Index tests |
Description of FRS used: The symptoms of first rank importance are: Audible thoughts, voices heard arguing, voices commenting on one's actions; the experience of influences playing on the body (somatic passivity experiences), thought withdrawal and other interferences with thought; diffusion of thought, delusional perception and all feelings, impulses (drives) and volitional acts that are experienced by the patient as the work or influence of others". Professionals performing test: Psychiatrists. Resolution of discrepancies: "Disagreements were resolved and an agreed verdict reached, so that, for each definition, each patient had a diagnosis made (schizophrenia present or absent) by agreement between 2 raters". How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: Final diagnosis comprised of original history, mental state schedules and follow‐up data reviewed to give a 'final' or lifetime' diagnosis. Target condition(s): Schizophrenia and non‐schizophrenia. Professionals performing test: 2 Psychiatrists. Resolution of discrepancies: Two raters worked together to decide on final diagnosis. |
||
| Flow and timing |
Study process: A sample of mixed first and subsequent admissions interviewed by the US/UK diagnostic team at that hospital and given a project diagnosis of some form of functional psychosis (schizophrenia, affective psychosis, paranoid state, or other/unspecified psychosis). The interviews, using the 7th edition of the Present State Examination, were carried out usually within 24 hours and always within 72 hours of admission. 12 diagnostic definitions* were applied by 2 raters working independently from observations made at a single mental state examination. Follow‐up interviews were done an average of 6.5 years after the index admission, and final diagnoses were made by 2 raters based on original history, mental state schedules and follow‐up data . Follow‐up: 6.5 years |
||
| Comparative | |||
| Notes | 2 samples were reported (Camberwell and Netherne), however we only refer to the Netherne sample since this is the only one to report the reference standard of 'final diagnosis'. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | No | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Carpenter 1974.
| Study characteristics | |||
| Patient sampling | Prospective, consecutive (unclear whether consecutive for patients with neurotic depression). | ||
| Patient characteristics and setting |
N with a clinical diagnosis of psychosis: 1202. N screened: 1119. Age: Not reported. Gender: Not reported. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Between the ages of 15 and 45. Had one of the following symptoms: delusions, other disordered thinking, hallucinations, inappropriate or bizarre behavior, gross psychomotor disorder, severe affect disorder, depersonalisation, self‐neglect, social withdrawal, overwhelming fear, or a diagnosis of psychosis on admission. The "aim of Phase 2 was for each Centre to collect at least 125 cases of functional psychosis" "In addition to the 125 cases of functional psychosis, it was decided that 10 cases of neurotic depression should also be included in order to provide extra material for differential diagnosis." Exclusion criteria: Evidence of organic disease, hospitalised for more than two or psychotic for more than three of the last five years. Study aim: The International Pilot Study of Schizophrenia (IPPS) was a long‐term epidemiological study funded by WHO with broader aims, among them to evaluate the prevalence and frequency of FRS in schizophrenia, and whether FRS are pathognomonic of schizophrenia in the absence of "organic psychosis". Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: China (Taiwan), Colombia, Czechoslovakia, Denmark, India, Nigeria, USSR, UK, USA. |
||
| Index tests |
Description of FRS used: PSE interview schedule used.
Nine of the 11 FRSs (delusional percept and somatic passivity omitted as not adequately defined in the PSE).
Two FRSs were not systematically assessed in US and were omitted from the analysis of American patients.
One PSE interview item covered both "made impulses" and "made feelings" so these two symptoms were grouped together in the analysis.
One or more FRSs needed for a diagnosis of schizophrenia. Only ratings indicating that a symptom was definitely present were considered positive, and all other ratings, including "questionably present" were considered negative. Professionals performing test: One psychiatrist. Resolution of discrepancies: Only one psychiatrist made each diagnosis. In order to check the reliability of their diagnoses, at least one interview was conducted each month with two psychiatrists rating. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: International Statistical Classification of Diseases (ICD‐8) using the PSE interview and a psychiatric history and a social description interview. In the USA subsample, diagnoses were made according to the Diagnostic and Statistical Manual (DSM‐II). Target condition(s): Schizophrenia, manic psychosis, neurosis and personality disorders. Professionals performing test: One psychiatrist. Resolution of discrepancies: Only one psychiatrist made each diagnosis. In order to check the reliability of their diagnoses, at least one interview was conducted each month with two psychiatrists rating. |
||
| Flow and timing |
Study process: All patients contacting each of the Field Research Centres were put through two screens, a demographic screen and a psychotic screen. Once included, they were given the PSE, past history was obtained, then a diagnosis was made using the ICD or DSM‐II (USA subsample). FRS were assessed in the PSE interview. Follow‐up: 2 years. |
||
| Comparative | |||
| Notes | [See page 8 of WHO report for details of methods.] Study part of the International Pilot Study of Schizophrenia (IPSS). |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | Yes | ||
| High | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| High | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Did all patients receive a reference standard? | No | ||
| Did all patients receive the same reference standard? | No | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | No | ||
| High | |||
Chandrasena 1987.
| Study characteristics | |||
| Patient sampling | Sri Lanka: prospective and randomly selected. UK and Canada: unclear how patients were sampled. | ||
| Patient characteristics and setting |
N with a clinical diagnosis of psychosis: 741. N screened: 741. Age: Not reported. Gender: Not reported. Ethnicity: Sri Lanka: (n = not reported). UK and Canada: Afro‐Craibbean immigrants n = 60, Asian immigrants n = 60, "Native" n = 64. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: not reported. Inclusion criteria: "Schizophrenics and non‐schizophrenics", no further details reported. Sri Lanka: all had “Functional Psychosis” as defined by the World Health Organization for the IPSS. Exclusion criteria: Not reported. Study aim: To investigate whether the prevalence of some individual FRS also vary with ethnicity and nationality. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: Sri Lanka, UK, and Canada. |
||
| Index tests |
Description of FRS used: FRSs were recorded using a modified version of the Present State Examination (PSE; translated standardised 9th version, modified to elicit and record all eleven FRS, since PSE reliably elicits only seven FRS). Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Prevalance. |
||
| Target condition and reference standard(s) |
Reference standard: Sri Lankan: the World Health Organization definitions for the IPSS. UK and Canada: ICD‐9. Target condition(s): Schizophrenia and non‐schizophrenia. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: Not reported. Follow‐up: Study carried out over 12 years. Exclusions: No exclusions reported. All participants included on the 2 x 2 tables. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| High | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Unclear | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Unclear | |||
Chopra 1987.
| Study characteristics | |||
| Patient sampling | Prospective and consecutive. | ||
| Patient characteristics and setting |
N included in study: 50. N in analysis: 50. Age: Mean not reported. Range 21‐86 years. Gender: M 23, F 27. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Not reported. "All the patients, irrespective of their diagnosis, were interviewed ... after admission" to the psychiatric hospital. Exclusion criteria: Not reported. Study aim: To evaluate the prevalence and diagnostic implications of FRS. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: Australia. |
||
| Index tests |
Description of FRS used: Questionnaire specially prepared for the study and based on Mellor's definitions of the FRS. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Prevalence and diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: DSM‐III. Target condition(s): Schizophrenic disorders, psychotic disorders not elsewhere classified (schizophreniform disorder, brief reactive psychosis, schizoaffective disorder, atypical psychosis‐schizophrenia onset after age 45), affective disorders (mania, major depression recurrent, atypical depression, dysthymic disorder), organic mental disorders, anxiety disorders, adjustment disorders and personality disorders. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. The second author confirmed all diagnoses. |
||
| Flow and timing |
Study process: All the patients, irrespective of their diagnosis, were interviewed by one of the authors (MG) for the presence of FRS as early as possible after admission. The patients were later seen by the first author (HDC) to confirm the findings and diagnosis. Diagnostic labels were given according to DSM‐III. Follow‐up: Not reported. Exclusions: Exclusions not explicitly reported in the study. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Unclear | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Daradkeh 1995.
| Study characteristics | |||
| Patient sampling | Retrospective, selected from a previous sample. | ||
| Patient characteristics and setting |
N included in study: 168. N in analysis: 168. Age: Mean age onset 26.8 years (SD = 9.3) Gender: M 108, F 60. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Patients with major mental illnesses. Exclusion criteria: Not reported. Study aim: Prevalence and diagnostic validity of FRS for schizophrenia.. Previous treatment for schizophrenia: Not reported. Clinical setting: Unclear. Country: United Arab Emirates. |
||
| Index tests |
Description of FRS used: FRS's assessed through OPCRIT. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Prevalence and diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: ICD‐10 through OPCRIT. Target condition(s): Schizophrenia. Professionals performing test: Pair of clinicians. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process:Patients selected from a larger previous trial of ICD‐10. Most patients assessed by pairs of clinicians and two thirds had diagnostic interviews applied. OPCRIT was used to generate diagnosis and FRSs. Follow‐up: Not reported. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | No | ||
| Was a case‐control design avoided? | Unclear | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Gonzalez‐Pinto 2004.
| Study characteristics | |||
| Patient sampling | Prospective, consecutive. | ||
| Patient characteristics and setting |
N with a clinical diagnosis of psychosis: 112. N screened: 112. Age: mean age 28.86 (SD 10.27), range 16‐61. Gender: M 75, F 37. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Presenting with first psychotic episode (FPE) and needing in‐patient psychiatric treatment. Aged 15–65 years. Exclusion criteria: Participants with mental retardation, organic brain disorders or drug abuse as a primary diagnosis. Study aim: To investigate the association between age and the occurrence of FRS in patients with a first psychotic episode (FPE) and to look for a linear relationship between age and number of FRS. Previous treatment for schizophrenia: None. Clinical setting: Inpatients. Country: Spain. |
||
| Index tests |
Description of FRS used: FRS using a checklist of 11 items: audible thoughts, voices arguing, voices commenting, delusional perception, somatic passivity, made thoughts, made impulses, made volition, made feelings, thought withdrawal and thought broadcasting. Professionals performing test: Two psychiatrists. Resolution of discrepancies: Not reported. How FRS used in study: Prevalence. |
||
| Target condition and reference standard(s) |
Reference standard: DSM‐IV using the Structured Clinical Interview for DSM Disorders (SCID‐1). Performed once a year over three years. Diagnosis made at three years considered the definitive diagnosis. If follow‐up not available, last diagnosis used. Also considered information from clinical records, family informants and staff observations. Target condition(s): 1. Schizophrenia. 2. Bipolar disorder (I or II). 3. Other diagnosis (includes schizophreniform disorder, schizoaffective disorder, delusional disorder, brief psychotic disorder, atypical psychosis, or major depressive disorder with psychotic symptoms (with no history of manic or hypomanic episode). Professionals performing test: Two psychiatrists. Resolution of discrepancies: Not reported. Kappa = 0.88 for inter‐rater reliability of SCID‐I diagnoses. |
||
| Flow and timing |
Study process: The day after admission, patients were assessed with a protocol that included SCID‐I and FRS. The evaluations were performed during a clinical interview lasting about 90 min and pertaining to the previous week.
Patients were evaluated by direct interview, with the same methodology, once a year over a period of 3 years. Follow‐up: 3 years. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Low | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | Yes | ||
| Unclear | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Ihara 2009.
| Study characteristics | |||
| Patient sampling | Prospective and consecutive. | ||
| Patient characteristics and setting |
N included in the study: 626. N included in the analysis: 426. Age: Mean 30.9 (SD 10.9), range 16‐64. Gender: M 251, F 175. Ethnicity: Black 46.2% (n = 197); White British 53.8% (n = 229). Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Age 16–64 years, resident within the 3 study areas (South East London, and Nottingham, Bristol), presence of hallucinations, delusions, thought disorder, bizarre or disturbed behavior, negative syndrome, mania or clinical suspicion of psychosis. Exclusion criteria: organic medical cause, or profound learning disability, previous contact with psychiatric services for psychotic symptoms. Study aim: To examine the prevalence of FRSs in a sample of first‐episode psychoses stratified by relevant demographic variable. Previous treatment for schizophrenia: None. Clinical setting: Inpatients and outpatients. Country: UK. |
||
| Index tests |
Description of FRS used: FRSs were assessed within a month after first contact with psychiatric services. FRSs were assessed by SCAN (refers to the previous 4 weeks) and IGC case notes. SCAN incorporates the Present State Examination Version 10.0, which captures FRSs. "For persons for whom SCAN data were not obtained, FRSs as well as passivity experiences were judged by whether item IG26 (delusion of control) in the IGC was positive or not, as other categories in the IGC like IG25 contain mixtures of FRSs". Professionals performing test: Certified psychiatrists or psychologists*. Resolution of discrepancies: Not Reported. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: Consensus diagnoses were made according to DSM‐IV and ICD‐10, using information obtained from the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) version 2.0 or the SCAN Item Group Checklist (IGC), which is scored from case notes. Target condition(s): All psychoses, schizophrenia, affective psychoses, non‐affective psychoses other than schizophrenia, and substance‐induced psychoses. Professionals performing test: Certified psychiatrists or psychologists* carried out the SCAN interviews and IGC scoring. A panel of clinicians received clinical information from the researcher who conducted the individual assessments and made a consensus diagnosis according to DSM‐IV and ICD‐10. Resolution of discrepancies: Not reported. "The inter‐rater reliability between the individual diagnosticians who were involved in the consensus diagnosis groups was good", no kappa score reported. |
||
| Flow and timing |
Study process: People presenting with their first psychosis at health centres over 2 years were screened for inclusion. Psychopathology was assessed using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN) version 2.0 or the SCAN Item Group Checklist (IGC), which is scored from case notes. FRSs were assessed within a month after first contact with psychiatric services using the SCAN and ICG case notes and SCAN refers to the previous 4 weeks. Consensius diagnoses were made according to DSM‐IV and ICD‐10 from the clinical information. Follow‐up: not reported. |
||
| Comparative | |||
| Notes | *Certified psychiatrists or psychologists who were trained in SCAN interviews at the Nottingham WHO training centre and had achieved acceptable item‐level agreement before certification. They also carried out the IGC scoring. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Did all patients receive a reference standard? | No | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | No | ||
| Did all patients receive the same index test? | Yes | ||
| Unclear | |||
Ndetei 1983.
| Study characteristics | |||
| Patient sampling | Prospecitve, consecutive. | ||
| Patient characteristics and setting |
N included in study: 82. N in analysis: 80. Age: Not reported. Gender: M 38, F 42. Ethnicity: African. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: All the recent “first ever admissions” to the professorial acute wards of Mathare Hospital in Nairobi (The National Psychiatric referral and teaching hospital) between the ages of 15‐ 65 years. In hospital between 7 days and 4 weeks. Exclusion criteria: Psychiatric illness complicated by a physical condition. Study aim: To ascertain the prevalence and frequency of FRS in Kenyan schizophrenic patients diagnosed using an objective schizophrenic screening index ‐ the New Haven Schizophrenic Index (NHSI), which does not include FRS in the diagnostic criteria for schizophrenia. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: Kenya. |
||
| Index tests |
Description of FRS used: FRS measured using the PSE. At least one FRS needed to be present. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Prevalence. |
||
| Target condition and reference standard(s) |
Reference standard: The New Haven Schizophrenic Index. Target condition(s): Schizophrenia. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: Patients were screened using the New Haven Schizophrenic Index. Before deciding whether the patient met the criteria for a diagnosis of schizophrenia each patient was then given a structured pre‐coded interview on their social‐demographic characteristics, followed by the Present State Examination (PSE) to measure FRS. Each symptom was rated as present only when the interviewer was convinced that any possible cultural interpretation or misunderstanding of the question had been excluded. The reference standard and index tests were applied in the same interview. Follow‐up: Not reported. Exclusions: Two patients were excluded from the analysis, because the interviews were not considered adequate and reliable. |
||
| Comparative | |||
| Notes | New Haven Schizophrenia Index used as it does not contain FRS. "It must, however, be pointed out that some or all of the NHSI negative patients in this study could have been regarded as schizophrenic by other diagnostic criteria" |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Low | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | Yes | ||
| Low | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
O'Grady 1990.
| Study characteristics | |||
| Patient sampling | Prospective, consecutive admissions over the 24 hours of the chosen research day, one day each week for one year. | ||
| Patient characteristics and setting |
N included in study: 109. N in analysis: 99. Age: Mean 40.6, range 18‐89 years. Gender: M 40, F 59. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Patients admitted to the acute admission wards, in hospital for a minimum of four days, but in practice, no patient was excluded by staying less than four days. Exclusion criteria: Patients admitted to psychogeriatric admission wards. Patients profoundly deaf or unable to speak English. Study aim: To find the frequencies of broadly and narrowly defined FRS in a sample of acute mental hospital admissions and find how they relate to diagnosis. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: UK. |
||
| Index tests |
Description of FRS used: A FRS questionnaire was added on to the SADS. The symptom questionnaire contained questions on all 11 first‐rank symptoms. Each symptom was rated using the dichotomy of wide versus narrow definitions proposed by Koehler (1979). The various definitions were drawn from Mellor (1970), Fish (1967), Wing et al (1974), and Taylor and Heissler (1971).The narrow definition was in all cases that of Mellor (1970). Professionals performing test: "Researcher" Resolution of discrepancies: Not reported. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: A semi‐structured interview, the Schedule for Affective Disorders and Schizophrenia (SADS), was used for each participant. Then diagnoses were assigned using the Research Diagnostic Criteria (RDC), Carpenter's Flexible System, and the New Haven Index. Target condition(s): Schizophrenia, schizoaffective manic, schizoaffective depressed, manic disorder, hypomanic disorder, major depressive disorder, minor depressive disorder, other (not specified). Professionals performing test: "Researcher". Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: Participants were interviewed on one day each week over a year, excluding breaks for holidays. All admissions over the 24 hours of the chosen research day were interviewed. Each participant was interviewed using the Schedule for Affective Disorders and Schizophrenia (SADS) with an additional FRS questionnaire. Diagnoses were then assigned using the Research Diagnostic Criteria (RDC), Carpenter's Flexible System, and the New Haven Index. The reference standard and index test were applied during the same interview. Follow‐up: Not reported. Exclusion: "Three [patients] refused to be interviewed and three interviews were not suitable for research purposes. In these six cases there was no evidence of first‐rank symptoms from interview or scrutiny of case notes. Four patients had organic brain disease and are not included in the main sample as they were not suitable for interview using the SADS." |
||
| Comparative | |||
| Notes | The SADS was used as it is specifically structured to provide RDC diagnoses. Carpenter's Flexible System and the New Haven Index were used as they do not heavily rely on first rank symptoms (FRS) to define schizophrenia. Only data from the RDC is usable in the analysis. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| High | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | No | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Peralta 1999.
| Study characteristics | |||
| Patient sampling | Prospective, consecutive. | ||
| Patient characteristics and setting |
N included in study: 660. N in analysis: 660. Age: Range of mean ages across diagnostic groups: 28.4 to 44.9 years. Gender: M 384, F 276. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Symptoms at admission: delusions, hallucinations,marked formal thought disorder, gross disorganised behaviour, severe negative symptoms, or catatonic symptoms. Exclusion criteria: Demonstrable brain disorders, drug misuse confounding diagnosis, mental retardation, serious medical disease or lack of reliable external sources of information. Study aim: Examine the diagnostic significance of FRSs for schizophrenia. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: Spain. |
||
| Index tests |
Description of FRS used: First‐rank symptoms were assessed by the authors through the Manual for the Assessment of Schizophrenia (MAS) interview assessing 12 FRS's, including "made feelings" symptoms. FRS rated with SAPS ( Scale for the Assessment of Positive Symptoms, 1984). Professionals performing test: Two authors, doctors in the psychiatric unit. Resolution of discrepancies: Not reported. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: Three sets of reference criteria were used: DSM‐III‐R narrow concept (i.e. DSM‐III‐R schizophrenia), a DSM‐III‐R broad concept (i.e. schizophrenia, schizophreniform disorder and schizoaffective disorder) and the Feighner* criteria for definite schizophrenia (Feighner et al, 1972). Target condition(s): Schizophrenia, schizophreniform disorder, schizoaffective disorder, mood disorder, delusional disorder, brief reactive psychosis, atypical psychosis. Professionals performing test: Two authors, doctors in the psychiatric unit.. Resolution of discrepancies: Consensus diagnoses were made by two authors after reviewing all the available information. Inter‐rater reliability for DSM‐111‐R and Feighner schizophrenia was 0.88 and 0.76, respectively. |
||
| Flow and timing |
Study process: Diagnoses were made using the reference standards at the end of the index admission. FRS assessed in clinical interviews conducted within the first five days of admission. Follow‐up: Not reported. Exclusions: Not explicitly reported. All patients included in the analysis. |
||
| Comparative | |||
| Notes | Part of the Pamplona Study on the phenomenology of functional psychotic disorders. *Feighner's definition was used as the 'gold standard' because it does not give particular diagnostic emphasis to FRSs |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Unclear | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | Yes | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Preiser 1979.
| Study characteristics | |||
| Patient sampling | Prospective, consecutive. | ||
| Patient characteristics and setting |
N included in study: 88. N in analysis: 88. Age: Not reported for whole sample. (Schizophrenic with FRS: mean 25.6 years. Schizophrenic without FRS: mean 23.3 years). Gender: Not reported for whole sample. (Schizophrenic with FRS: M13, F12. Schizophrenic without FRS: M14, F13). Ethnicity: Not reported for whole sample. (Schizophrenic with FRS: Black 14, White 7, Hispanic 4. Schizophrenic without FRS: Black 17, White 8, Hispanic 2). Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Majority of patients were on medication, medications not reported. Inclusion criteria: The study was conducted on a 24‐bed therapeutic community ward in a large municipal hospital. Patients were mostly referred from the acute wards of the psychiatric hospital, sample consisted of patients who were judged to need hospitalisation of at least 2 weeks duration and to have the potential to profit from the intensive therapeutic experience offered. Exclusion criteria: Not reported. Study aim: To investigate whether schizophrenics with FRS have more observable pathologic behaviour than schizophrenics without FRS and whether schizophrenics with FRS have a poorer response to an intensive short‐term treatment program than schizophrenics without FRS. Previous treatment for schizophrenia: Not reported, majority of patients were medicated and referred from the acute wards of the hospital. Clinical setting: Inpatients. Country: USA. |
||
| Index tests |
Description of FRS used: FRS as defined by Mellor. Professionals performing test: Each patient's therapist and corroborated by a senior attending psychiatrist. Resolution of discrepancies: Not reported. How FRS used in study: Prognosis. |
||
| Target condition and reference standard(s) |
Reference standard: Bleulerian and/or ego function criteria at discharge from the ward. Target condition(s): Schizophrenia and not schizophrenia (not defined in study). Professionals performing test: Individual therapist in consultation with the attending supervisor. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: During a 6‐month period all patients admitted to the ward were evaluated through a nurse completing Psychotic Inpatient Profile (PIP), and therapist's evaluation through a scale . FRS were assessed during patients time on the ward and diagnosis was decided at discharge. Maximum stay on the ward was 3 months and the average stay was 6 weeks. Follow‐up: Not reported. Exclusions: "Five patients not diagnosed schizophrenic also exhibited FRS. These patients were not included in any of the subsequent analyses reported in this study." |
||
| Comparative | |||
| Notes | Unclear whether all patients received the index test; 88 patients were included, "52 were given a discharge diagnosis of schizophrenia. Of these 52, 25 exhibited at least one Schneiderian first‐rank symptom, and 27 exhibited none. Five patients not diagnosed schizophrenic also exhibited FRS. These patients were not included in any of the subsequent analyses reported in this study." | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Unclear | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Unclear | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Unclear | |||
Radhakrishnan 1983.
| Study characteristics | |||
| Patient sampling | Prospecitve, consecutive. | ||
| Patient characteristics and setting |
N included in study: 266. N in analysis: 266. Age: Not reported. Gender: Not reported. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: All admissions over a period of 18 months. Exclusion criteria: Not reported. Study aim: To evaluate the prevalence of FRS and their diagnostic and prognostic implications. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: India. |
||
| Index tests |
Description of FRS used: Questions to establish the presence of FRS were asked according to the standardised interview schedule of the International Pilot Study of Schizophrenia. The patients were interviewed before starting on any medication. The first rank symptoms were rated as either present, or absent. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Prevalence, diagnosis, prognosis. |
||
| Target condition and reference standard(s) |
Reference standard: Diagnostic criteria used were according to the International Classification of Diseases: lCD 9. Only those patients who satisfied the criteria of Feighner for schizophrenia were included in the schizophrenia group. Target condition(s): Schizophrenia, affective disorders, hysterical psychosis, paranoid state, acute psychotic reaction, organic psychosis, neurotic disorders, personality disorders, and temporal lobe epilepsy. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: Not reported when patients were diagnosed and interviewed for FRS. Follow‐up: Not reported. Exclusion: Exclusions not explicitly reported. All participants received a diagnosis according to the reference standard, unclear whether all were evaluated for FRS. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Unclear | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | High | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Raguram 1985.
| Study characteristics | |||
| Patient sampling | Prospective, randomly selected. | ||
| Patient characteristics and setting |
N included in study: 90. N in analysis: 90. Age: Not reported. Gender: Not reported. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: The cases were selected from the outpatients attending the hospital for the first time. 30 cases in each diagnostic category (schizophrenia, affective psychosis and reactive psychosis) were randomly collected. Exclusion criteria: Not reported. Study aim: To study the occurrence of FRS in three major forms of functional psychosis (schizophrenia, affective psychosis and reactive psychosis). To explore the relationship between the occurrence of FRS and the presence of family history of schizophrenia, affective psychosis and reactive psychosis. Previous treatment for schizophrenia: Not reported. Clinical setting: Outpatients. Country: India. |
||
| Index tests |
Description of FRS used: FRS were evaluated using Mellor's check‐list. Professionals performing test: The investigator. Resolution of discrepancies: Not reported. How FRS used in study: Prevalence. |
||
| Target condition and reference standard(s) |
Reference standard: Feighner's (1972) diagnostic criteria were employed for making the diagnosis of schizophrenia and affective psychosis. For a diagnosis of reactive psychosis, the criteria used by Pandurangi and Kapur (1979) were employed. Target condition(s): Schizophrenia, affective psychosis and reactive psychosis. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: Outpatients attending the hospital for the first time were diagnosed using Feigner's diagnostic criteria before they were randomly selected for the study. 30 cases from each diagnosis (schizophrenia, affective psychosis and reactive psychosis) were randomly selected and were seen by the investigator in the out‐patient before they were started on medication. FRS were evaluated using Mellor's check‐list, the timing was not reported. FRS were evaluated after this, the timing is not reported. Follow‐up: Not reported. Exclusions: Exclusions not explicitly reported. All participants are included in the analysis. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | High | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | Yes | ||
| Unclear | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | No | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Unclear | |||
Ramperti 2010.
| Study characteristics | |||
| Patient sampling | Prospective, consecutive. | ||
| Patient characteristics and setting |
N included in study: 158. N in analysis: 158. Age: Mean 31.9 years (SD 11.2) Gender: M 99, F 59. Ethnicity: Not reported. Comorbid disorders: History of cannabis n = 14. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Between 16 and 65 years old, experiencing first episode of psychosis (affective and non‐affective). Current or previous history of alcohol and drug misuse were included. First episode of psychosis as the presence of any psychotic symptom for the first time in a person's life. Exclusion criteria: Organic brain disease and/or the patient being on antipsychotic medication for more than 30 days. Study aim: To establish the prevalence of FRS across the range of psychotic illnesses. Previous treatment for schizophrenia: No previous treatment. Clinical setting: Inpatients and outpatients. Country: Ireland. |
||
| Index tests |
Description of FRS used: FRS consistent with those described by Mellor.
Of these 11 items, 8 are represented in the SAPS (made feelings, impulses, and volitions are scored together). Symptoms in the SAPS are scored in a Likert Scale from "Not at all" to "severe" (0‐5). It was agreed between the assessors that due to the bizarre quality of the FRS ("questionable") should be used as a cut off point. The following 3 symptoms were not included as they are not clearly assessed in the SAPS or SCID: "audible thoughts," "Influence playing on the body or somatic passivity," and "delusional perception." Professionals performing test: Clinical fellows trained in the different rating scales. Resolution of discrepancies: Not reported. Inter‐rater reliability was achieved for the SAPS and SANS (kappa >0.7). The concordance for the SCID interview diagnosis ranged from 93% to 100% among raters. How FRS used in study: Prevalence. |
||
| Target condition and reference standard(s) |
Reference standard: DSM‐IV. Target condition(s): Schizophrenia, schizophreniform disorder, and schizoaffective disorder (1 case) were combined together to form a schizophrenia spectrum group. Professionals performing test: Clinical fellows trained in the different rating scales. Resolution of discrepancies: Not reported. The concordance for the SCID interview diagnosis ranged from 93% to 100% among raters. |
||
| Flow and timing |
Study process: Patients were contacted within 72 hours after the referral. All patients were assessed and diagnosed using the SCID‐Il. FRS were rated accordingly to the Scale for the Assessment of Positive Symptoms (SAPS). Clinical fellows trained in the different rating scales carried out the assessments. Diagnoses made using the DSM‐IV. Unclear when the tests were applied and the order. Follow‐up: Not reported. Exclusions: Not explicitly reported. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Rosen 2011.
| Study characteristics | |||
| Patient sampling | Prospective, unclear whether consecutive or random sample. | ||
| Patient characteristics and setting |
N included in study: 86. N in analysis: 78. Age: Mean age at testing, schizophrenia: 23 (SD 3.4), bipolar: 24 (SD 6.3). Gender: M 50, F 36. Ethnicity: White 5. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported for all time points. At the 20‐year follow‐up, 65% (n = 38) of schizophrenia patients were on psychiatric medications as were 58% (n = 15) bipolar patients. Of these, 55% (n = 32) of schizophrenia patients were on antipsychotic medications compared with 23% (n = 6) of bipolar patients. Inclusion criteria: Patients with schizophrenia and bipolar. Exclusion criteria: Not reported. Study aim: Prevalence and severity of first‐rank symptoms (FRS) during an extended period of time in patients with schizophrenia and bipolar disorder with psychosis. Previous treatment for schizophrenia: 64% of the total sample had one or fewer previous hopitalisations. There was no significant difference between patients with schizophrenia and bipolar disorder in the number of previous admissions. Clinical setting: Not reported. Country: USA. |
||
| Index tests |
Description of FRS used: At index hospitalisation, the following FRS were assessed: thought broadcasting, thought insertion, thought withdrawal, delusions of control, a voice keeping a running commentary, and voices conversing. We evaluated at index and at all 6 follow‐ups the 2 FRS in DSM‐IIIR/IV criterion A for schizophrenia, auditory hallucinations that consist of a voice keeping a running commentary and voices conversing. In addition, at each follow‐up, all 12 FRS were assessed. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Diagnosis and prognosis. |
||
| Target condition and reference standard(s) |
Reference standard: Research Diagnostic Criteria (RDC)* diagnoses at index hospitalisation were based on structured clinical interviews including the Schedule for Affective Disorders and Schizophrenia, and/or the Schizophrenia State Inventory and collateral information. Target condition(s): Schizophrenia and bipolar. Professionals performing test: Not reported. Interviewers performing follow‐up evaluations were not informed of diagnosis or the results of previous follow‐up evaluations. Resolution of discrepancies: Not reported. Diagnostic inter‐rater reliability was kappa = 0.88. |
||
| Flow and timing | Study process: This research follows a sample of patients with psychotic and mood disorders who were evaluated at index hospitalisation and then prospectively followed at 6 evaluations subsequently for 20 years. Follow‐up evaluations occurred at 2, 4.5, 7.5, 10, 15, and 20 after index hospitalisation. All 86 patients were assessed at the 20‐year follow‐up. First‐rank symptoms were individually evaluated at index hospitalisation and at each subsequent follow‐up. The assessment of FRS was based on the Schedule for Affective Disorders and Schizophrenia. Research Diagnostic Criteria (RDC) diagnoses at index hospitalisation were based on structured clinical interviews including the Schedule for Affective Disorders and Schizophrenia, and/or the Schizophrenia State Inventory and collateral information. Interviewers performing follow‐up evaluations were not informed of diagnosis or the results of previous follow‐up evaluations. Follow‐up: 20 years. Exclusions: Not clearly reported. Data on FRS at the 20‐year follow‐up were available for 73% of the original sample assessed. | ||
| Comparative | |||
| Notes | All patients were evaluated as part of the Harrow Chicago Follow‐up study. *The RDC were used for diagnosis because they provide diagnostic criteria that are independent of FRS, allowing diagnostic analyses that have not been confounded by the use of FRS as an inclusion criterion for schizophrenia. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Unclear | High | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | Yes | ||
| Unclear | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | No | ||
| Did all patients receive a reference standard? | Unclear | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Unclear | ||
| Did all patients receive the same index test? | Yes | ||
| Unclear | |||
Salleh 1992.
| Study characteristics | |||
| Patient sampling | Prospective, selection of patients not reported. | ||
| Patient characteristics and setting |
N included in study: 221. N in analysis: 221. Age: Not reported. Gender: Not reported. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: First visit adult Malay patients diagnosed as having functional psychosis and attending psychiatric facilities at the hospital. Exclusion criteria: Patients with doubtful organic status. Study aim: Prevalence of FRS in functional psychosis and utility of FRS as diagnostic tool. Previous treatment for schizophrenia: No previous treatment. Clinical setting: Inpatients. Country: Malaysia. |
||
| Index tests |
Description of FRS used: 11 FRS used. Patients interviewed based on a standard questionnaire*. Presence of FRS was rated as defined by Mellor but combining the three components of passivity phenomenon into one. Professionals performing test: Author or one of the three senior psychiatric house staff. Resolution of discrepancies: All discrepancies were settled with a consensus opinion. Interrater reliability established in a pilot study conducted prior to this was continuously checked by the author throughout the study. All cases initially seen by the house staff for instance were reviewed by the author within 48h of the initial interview. How FRS used in study: Prevalence and diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: ICD‐9. Target condition(s): Schizophrenia, affective psychoses, paranoid state, other non‐organic psychoses. Professionals performing test: Two psychiatrists. Resolution of discrepancies: Not reported. Diagnosis had to be agreed by two psychiatrists. |
||
| Flow and timing |
Study process: First visit adult patients attending psychiatric facilities entered into the study. Diagnoses made using the ICD‐9 criteria. Patients interviewed for FRS within 24 hours of admission by author or senior psychiatric house staff. All cases initially seen by the house staff reviewed by author within 48 hours of initial interview. Follow‐up: Not reported. Exclusions: Not explicitly reported. |
||
| Comparative | |||
| Notes | *Unclear whether FRS interview was PSE". | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Stephens 1980.
| Study characteristics | |||
| Patient sampling | Retrospective, randomly selected. | ||
| Patient characteristics and setting |
N included in study: 555. N in analysis: 120. Age: Mean age 35.4 (range 20‐57). Gender: M 60, F 60. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Phenothiazine alone and treatment with a phenothiazine combined with a tricyclic antidepressant or antianxiety drug. Inclusion criteria: Newly hospitalised patients who had participated in three drug studies between 1964 and 1966. Exclusion criteria: Patients with brain syndromes, major systemic diseases, mental deficiency, and alcoholism or drug abuse. Study aim: Prognostic implications of diagnostic criteria. Previous treatment for schizophrenia: Hospitalisation. Clinical setting: Inpatients. Country: USA. |
||
| Index tests |
Description of FRS used: Not reported. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: DSM‐II*. Target condition(s): Schizoprenia (chronic undifferentiated, paranoid, acute undifferentiated), schizoaffective, psychotic depression. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: 555 newly hospitalised patients admitted over 2 years were participants in previous drug studies. 120 participants were randomly selected. Retrospective diagnoses made by chart review using six sets of criteria including FRS. The seventh diagnosis was made at the time of hospitalisation using DSM‐II. Follow‐up: Mean 9.8 years Exclusion: All included participants in analyses. Followup data that is not relevant for this review was obtained for 82 participants, reasons for exclusions not provided. |
||
| Comparative | |||
| Notes | *Also reported diagnoses using the New York Research Diagnostic Criteria (RDC), the New Haven Schizophrenia Index (NHSI), the 12‐point “Flexible” criteria system developed by the Washington field center of the International Pilot Study of Schizophrenia (Carpenter et al., 1973) the St. Louis diagnostic criteria (Feighner et al., 1972) and the modification by Bland and Orn (1979) of the St. Louis criteria. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Unclear | Unclear | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Stephens 1982.
| Study characteristics | |||
| Patient sampling | Retrospective, consecutive. | ||
| Patient characteristics and setting |
N with a clinical diagnosis of psychosis: 283. N screened: 283. Age: Mean age at admission 28.7 years. Gender: M 119, F 164. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Have a diagnosis of schizophrenia, schizoaffective schizophrenia, or paranoid state (according to DSM‐I). First admissions to any hospital, had been hospitalised for at least 21 days, and had long‐term follow‐ups available. Exclusion criteria: Not reported. Study aim: To compare nine systems to diagnose schizophrenia. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatient. Country: USA. |
||
| Index tests |
Description of FRS used: FRS, evaluated though chart review, no further description reported. Professionals performing test: One of the authors. Resolution of discrepancies: Not applicable, only one person rated FRS. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: DSM III Target condition(s): Schizophrenia, schizoaffective, paranoid state. Professionals performing test: One of the authors. Resolution of discrepancies: Not applicable, only one person made diagnoses. |
||
| Flow and timing |
Study process: One author read charts and classified patients as "process" (expected to have unfavourable outcome) or "nonprocess" (expected to have a favourable outcome). All process patients were given a diagnosis according to Leonhard’s scheme as described by Leonhard (1979) and Astrup et al. (1962). Nonprocess patients were usually diagnosed reactive psychoses or cycloid psychoses. Retrospective diagnosis by chart review, diagnoses by six of the seven sets of criteria. Follow‐up: 5 to 16 years. |
||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Unclear | |||
Tandon 1987.
| Study characteristics | |||
| Patient sampling | Prospective, consecutive. | ||
| Patient characteristics and setting |
N included in study: 294. N screened: 294. Age: Not reported. Gender: Not reported. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: "Off all medication for at least 2 weeks." Inclusion criteria: Having "undergone a comprehensive SADS interview by a trained clinician in the course of the inpatient stay after having been off all medication for at least 2 weeks". Exclusion criteria: Not reported. Study aim: The prevalence of Schneiderian first‐rank symptoms (FRS) to their diagnostic distribution (SAD, RDC). Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: USA. |
||
| Index tests |
Description of FRS used: "Presence or absence of first‐rank symptoms was established on the basis of the standardized SADS interview."
"Patients with two or more FRS received a diagnosis of schizophrenia."
Only 9 FRS's reported (not predefined) in table, with Delusional perception as" not documented". Professionals performing test: SADS interview by a trained clinician. Resolution of discrepancies: Not reported. How FRS used in study:Prevalence. |
||
| Target condition and reference standard(s) |
Reference standard: Research Diagnostic Criteria (RDC). Target condition(s): Major depressive disorder, primary major depressive disorder (MDD), substance abuse with toxic psychosis with secondary MDD, schizophrenia, schizoaffective disorder, manic disorder, minor depressive disorder. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: "All admissions to a unit for affective disorders at the University of Michigan Medical Center" over 8 years were reviewed, and anyone who had "undergone a comprehensive SADS interview by a trained clinician in the course of the inpatient stay" was included.
These patients were screened for the presence of first‐rank symptoms at the time of the baseline evaluation through SADS. No details about when or how RDC diagnosis was assessed. Follow‐up: Not reported. Exclusions: Not reported. |
||
| Comparative | |||
| Notes | Unclear when Reference standard was assessed. FRS symptoms not pre‐defined. All patients with two or more FRS received a diagnosis of schizophrenia however no differentiation made between the diagnosis of more than 1 FRS. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | High | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | Yes | ||
| Unclear | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Tanenberg‐Karant 1995.
| Study characteristics | |||
| Patient sampling | Prospective, unclear whether consecutive or random selection. | ||
| Patient characteristics and setting |
N included in study: 196. N in analysis: 196. Age: Not reported. Gender: Not reported. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Aged 15 to 60 years. Experiencing first admission to inpatient facilities. Screened for the presence of psychotic symptoms. "This study focused on 196 hospitalized patients with a 6‐month longitudinal best‐estimate research diagnosis (see below) of schizophrenia, schizoaffective disorder, schizophreniform disorder, bipolar disorder with psychotic features, and major depressive disorder with psychotic features. Six additional patients in these diagnostic groups did not have delusions or hallucinations (i.e., they had, for example, thought disorder)." Exclusion criteria: First psychiatric hospitalisation more than 6 months before current admission, moderate or severe mental retardation, and non‐English‐speaking status. Study aim: To examine the prevalence and correlates of bizarre delusions and FRS in a first‐admission sample with psychosis. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: USA. |
||
| Index tests |
Description of FRS used: FRS evaluated using SCID interview, which included nine of 11 FRS delusions and hallucinations. It does not specifically ask about audible thoughts or delusional perception. These were only coded from information volunteered by the patient during the interview or mentioned by the clinician either in the discharge summary or the clinician interview.*
FRS decisions were based on definitions and examples provided by Mellor. Professionals performing test: Two project psychiatrists blind to the best‐estimate diagnosis. Resolution of discrepancies: For all but eight disagreements, consensus between the two psychiatrists was achieved after discussion. The inter‐rater agreement between pairs of psychiatrists was k = 0.861 for FRS. How FRS used in study: Prevalence. |
||
| Target condition and reference standard(s) |
Reference standard: 6‐month longitudinal best‐estimate research diagnosis based on DSM‐III‐R using SCID, discharge summaries, and other relevant information. Target condition(s): Schizophrenia, schizoaffective disorder, schizophreniform disorder, bipolar disorder with psychotic features, and major depressive disorder with psychotic features. Professionals performing test: Two project psychiatrists independently reviewed the SCIDs, discharge summaries, and other relevant information and arrived at a diagnosis. Each case was presented at a project psychiatrists' meeting and a best‐estimate diagnosis was determined. (SCID interviewers were master's‐level mental health professionals with considerable clinical experience and who were trained over a period of 3 to 6 months) Resolution of discrepancies: SCID: Not reported. Interrater reliability assessments were conducted on approximately every tenth interview, and mean K values for mood and psychosis sections were high. Diagnosis: Regardless of whether a consensus was reached by the two psychiatrists, each case was presented at a project psychiatrists' meeting and a best‐estimate diagnosis was determined. |
||
| Flow and timing | Study process: SCID interview at hospital before discharge and a 6‐month follow‐up interview typically took place in the patients' homes. After these interviews two psychiatrists reviewed the SCIDs, discharge summaries, and other relevant information and arrived at a diagnosis. Regardless of whether a consensus was reached by the two psychiatrists, each case was presented at a project psychiatrists' meeting and a best‐estimate diagnosis was determined. Follow‐up: 6 months. Exclusions: Not explicitly reported. | ||
| Comparative | |||
| Notes | *Determinations about delusions and hallucinations derive primarily from the interview, with supplementation from other informed sources (medical records, treating clinician, interview with significant other). | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | High | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Unclear | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Low | |||
Wu 1990.
| Study characteristics | |||
| Patient sampling | Prospective, randomly selected. | ||
| Patient characteristics and setting |
N with a clinical diagnosis of psychosis: 132. N screened: 132. Age: 15‐63 years old. Gender: M 78, F 54. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Not reported. Exclusions criteria: Not reported. Study aim: Diagnostic specificity by Schneider's first rank symptoms. Previous treatment for schizophrenia: Not reported. Clinical setting: Inpatients. Country: China. |
||
| Index tests |
Description of FRS used: "11 items of FRS and patients" . Professionals performing test: "Two experienced doctors". Resolution of discrepancies: Not reported. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: "standards set in the 1984 Mount Huangshan Conference". Target condition(s): Schizophrenia, Manic depression psychosis, Hysterical psychosis, Mental deficiency with mental disorder, Epileptic mental disorder, Traumatic mental disorder, Alcoholic psychosis. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: Patients were randomly selected from the inpatient ward. The diagnosis was based on the standards set in the 1984 Mount Huangshan Conference. According to the 11 items of FRS and patients’ medical history, two experienced doctors conducted psychiatric examination to determine the patients’ FRS symptoms. Follow‐up: Not reported. |
||
| Comparative | |||
| Notes | Reference standard, Mount Huanshan Conference is an early version of Chinese Classification and Diagnostic Criteria of Mental Disorders, CCMD. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Unclear | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Low | Unclear | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| Did the study pre‐specify whether they were using one or multiple FRSs? | No | ||
| Unclear | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Unclear | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Unclear | Unclear | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Unclear | ||
| Did all patients receive a reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Unclear | ||
| Did all patients receive an index test? | Yes | ||
| Did all patients receive the same index test? | Yes | ||
| Unclear | |||
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abrams 1973 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Abrams 1981 | Data insufficient to construct appropriate 2 x 2 table. |
| Ahmed 1984 | Participants did not present with psychotic symptoms. Data insufficient to construct appropriate 2 x 2 table. |
| Al‐Ansari 1989 | All participants had a diagnosis of schizophrenia. |
| Anselmetti 2007 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Asnis 1982 | All participants had a diagnosis of schizophrenia. |
| Basu 1999 | Assessors not blinded to diagnosis in a retrospective study. |
| Beckmann 1990 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Berner 1984 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. FRS not routinely performed on patients in study. |
| Berner 1986 | FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Berner 1986a | Data insufficient to construct appropriate 2 x 2 table. |
| Bland 1978 | All participants had a diagnosis of schizophrenia. |
| Bland 1979 | Participants did not present with psychotic symptoms. All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Botros 2006 | All participants had a diagnosis of schizophrenia. |
| Burbach 1984 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Cardno 2002 | Data insufficient to construct appropriate 2 x 2 table. |
| Ceccherini‐Nelli 2003 | All participants had a diagnosis of schizophrenia. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. Assessors not blinded to diagnosis in a retrospective study. |
| Cernovsky 1985 | All participants had a diagnosis of schizophrenia. |
| Chandrasena 1979 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Coffey 1993 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Assessors not blinded to diagnosis in a retrospective study. |
| Compton 2008 | Data insufficient to construct appropriate 2 x 2 table. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Conus 2004 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Cowell 1996 | All participants had a diagnosis of schizophrenia. |
| Craddock 1996 | Data insufficient to construct appropriate 2 x 2 table. FRS not routinely performed on patients in study. |
| Cuesta 2007 | Participants did not present with psychotic symptoms. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Deister 1993 | All participants had a diagnosis of schizophrenia. |
| Deister 1994 | Participants did not present with psychotic symptoms. All participants had a diagnosis of schizophrenia. FRS not routinely performed on patients in study. |
| Dollfus 1992 | Data insufficient to construct appropriate 2 x 2 table. |
| Dollfus 1993 | All participants had a diagnosis of schizophrenia. |
| Dollfus 1993a | Participants did not present with psychotic symptoms. Data insufficient to construct appropriate 2 x 2 table. FRS not routinely performed on patients in study. |
| Endicott 1982 | Data insufficient to construct appropriate 2 x 2 table. FRS not routinely performed on patients in study. |
| Endicott 1986 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Eva 1984 | All participants had a diagnosis of schizophrenia. |
| Evans 1981 | All participants had a diagnosis of schizophrenia. |
| Fanous 2012 | All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Fourneret 2001 | Participants did not present with psychotic symptoms. All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Franck 2002 | All participants had a diagnosis of schizophrenia. |
| Ganesan 2005 | Participants did not present with psychotic symptoms. All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Gharagozlou 1979 | Participants did not present with psychotic symptoms. |
| Gift 1980 | Participants did not present with psychotic symptoms. Data insufficient to construct appropriate 2 x 2 table. FRS not routinely performed on patients in study. |
| Glazer 1987 | Participants did not present with psychotic symptoms. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Gur 1994 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Gureje 1987 | All participants had a diagnosis of schizophrenia. |
| Hayashi 1998 | Participants did not present with psychotic symptoms. All participants had a diagnosis of schizophrenia. FRS not routinely performed on patients in study. |
| Helmes 1983 | Participants did not present with psychotic symptoms. Data insufficient to construct appropriate 2 x 2 table. |
| Hill 1996 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Idrees 2010 | All participants had a diagnosis of schizophrenia. |
| Jakobsen 2006 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. FRS not routinely performed on patients in study. |
| Kendell 1979 | Participants did not present with psychotic symptoms. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Klosterkotter 1992 | All participants had a diagnosis of schizophrenia. |
| Koehler 1976 | All participants had a diagnosis of schizophrenia. |
| Koehler 1978 | FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Kulhara 1988 | All participants had a diagnosis of schizophrenia. |
| Kulhara 1989 | All participants had a diagnosis of schizophrenia. |
| Landmark 1986 | Participants did not present with psychotic symptoms. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Landmark 1990 | All participants had a diagnosis of schizophrenia. |
| Lenz 1986 | Data insufficient to construct appropriate 2 x 2 table. |
| Lewine 1982 | All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Lewine 1984 | Participants did not present with psychotic symptoms. Data insufficient to construct appropriate 2 x 2 table. |
| Littlewood 1981 | Participants did not present with psychotic symptoms. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Loftus 2000 | All participants had a diagnosis of schizophrenia. |
| Maier 1986 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Makanjuola 1987 | All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Malik 1990 | All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Marneros 1984 | Participants did not present with psychotic symptoms. No index tests for comparison. Data insufficient to construct appropriate 2 x 2 table. |
| Mason 1997 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Matsuura 2004 | Participants did not present with psychotic symptoms. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Mauri 1992 | Data insufficient to construct appropriate 2 x 2 table. FRS not routinely performed on patients in study. |
| McGuffin 1984 | Data insufficient to construct appropriate 2 x 2 table. |
| McGuffin 1991 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Melges 1977 | Participants did not present with psychotic symptoms. Data insufficient to construct appropriate 2 x 2 table. |
| Mellor 1970 | All participants had a diagnosis of schizophrenia. |
| Menezes 1993 | Data insufficient to construct appropriate 2 x 2 table. |
| Modestin 2003 | All participants had a diagnosis of schizophrenia. |
| Munk‐Jorgensen 1989 | All participants had a diagnosis of schizophrenia. The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. FRS not routinely performed on patients in study. Data insufficient to construct appropriate 2 x 2 table. |
| Nakaya 2002 | All participants had a diagnosis of schizophrenia. |
| Ndetei 1984 | Data insufficient to construct appropriate 2 x 2 table. |
| Nordgaard 2008 | Participants did not present with psychotic symptoms. |
| Pela 1982 | Data insufficient to construct appropriate 2 x 2 table. |
| Peralta 1992 | Participants did not present with psychotic symptoms. Data insufficient to construct appropriate 2 x 2 table |
| Philipp 1986 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Philipp 1986a | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Pihlajamaa 2008 | All participants had a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Ross 1991 | Participants did not present with psychotic symptoms. |
| Salvatore 2011 | Participants did not present with psychotic symptoms. FRS not routinely performed on patients in study. |
| Schanda 1984 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Schiopu 2005 | All participants had a diagnosis of schizophrenia. |
| Serban 1979 | All participants had a diagnosis of schizophrenia. |
| Silverstein 1978 | All participants had a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Silverstein 1981 | Data insufficient to construct appropriate 2 x 2 table. |
| Sougey 1987 | All participants had a diagnosis of schizophrenia. |
| Taylor 1972 | All participants had a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Thorup 2007 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. |
| Vazquez‐Barquero 1995 | The reference standard was not used to separate those with a diagnosis of schizophrenia from the ones without a diagnosis of schizophrenia. |
| Vega 2006 | Participants did not present with psychotic symptoms. |
| Wciorka 1995 | Data insufficient to construct appropriate 2 x 2 table. |
| Wetterberg 1991 | Participants did not present with psychotic symptoms. FRS not routinely performed on patients in study. No index tests for comparison. Data insufficient to construct appropriate 2 x 2 table. |
| Young 1982 | All participants had a diagnosis of schizophrenia. Data insufficient to construct appropriate 2 x 2 table. FRS not routinely performed on patients in study. |
| Zarrouk 1978 | All participants had a diagnosis of schizophrenia. |
FRS: First Rank Symptoms
Characteristics of studies awaiting classification [ordered by study ID]
Friedrich 1980.
| Study characteristics | |||
| Patient sampling | Retropective. | ||
| Patient characteristics and setting |
N with a clinical diagnosis of psychosis: 28. N screened: 28. Age: Adolescence Gender: Not reported. Ethnicity: Not reported. Comorbid disorders: Not reported. Duration of symptoms: Not reported. Concurrent medications used: Not reported. Inclusion criteria: Not reported. Exclusion criteria: Not reported. Study aim: Diffrential diagnosis of Schneider's first rank symptoms for adolescents. Previous treatment for schizophrenia: Not reported. Clinical setting: Not reported. Country: Not reported. |
||
| Index tests |
Description of FRS used: Not reported. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. How FRS used in study: Diagnosis. |
||
| Target condition and reference standard(s) |
Reference standard: E. Blueler's (1975), and P. Berner's (1977) criteria. Target condition(s): Schizophrenia, schizoaffective, affective psychosis, borderline. Professionals performing test: Not reported. Resolution of discrepancies: Not reported. |
||
| Flow and timing |
Study process: Patients observed and supervised for up to 5 years. Follow‐up: Not reported. |
||
| Comparative | E. Blueler's (1975), K. Schneider's (1976), and P. Berner's (1977) criteria for the diagnosis of psychoses . | ||
| Notes | Awaiting translation‐ reported from English abstract. | ||
FRS: first rank symptoms
Contributions of authors
Karla Soares‐Weiser ‐ lead project, screening, data extraction, wrote the review.
Nicola Maayan ‐ screening, data extraction, wrote the review.
Hanna Bergman ‐ screening and wrote the review.
Clare Davenport ‐ helped guide and draft protocol, commented on final review.
Sarah Grabowski ‐ screening and data extraction.
Amanda Kirkham ‐ data analysis and statistical support.
Clive E Adams ‐ gained funding, helped draft protocol and review.
Sources of support
Internal sources
University of Nottingham, UK.
External sources
-
NIHR Cochrane Programme Grant 2011, UK.
Reference number: 10/4001/15, UK
Declarations of interest
Karla Soares‐Weiser ‐ currently works for Enhance Reviews Ltd, a company that carries out systematic reviews mostly for the public sector, it currently does not provide services for the pharmaceutical industry.
Nicola Maayan ‐ currently works for Enhance Reviews Ltd, a company that carries out systematic reviews mostly for the public sector, it currently do not provide services for the pharmaceutical industry.
Hanna Bergman ‐ currently works for Enhance Reviews Ltd, a company that carries out systematic reviews mostly for the public sector, it currently does not provide services for the pharmaceutical industry.
Clare Davenport ‐ none known.
Sarah Grabowski ‐ none known.
Amanda Kirkham ‐ none known.
Clive E Adams ‐ none known.
New
References
References to studies included in this review
Brockington 1978 {published data only}
- Brockington IF, Kendell RE, Leff JP. Definitions of schizophrenia: concordance and prediction of outcome. Psychological Medicine 1978; Vol. 8, issue 3:387‐98. [0033‐2917: (Print).] [DOI] [PubMed]
- Kendell RE, Brockington IF, Leff JP. Prognostic implications of six alternative definitions of schizophrenia. Archives of General Psychiatry 1979;36(1):25‐31. [DOI] [PubMed] [Google Scholar]
Carpenter 1974 {published data only}
- Carpenter WT Jr, Strauss JS, Muleh S. Are there pathognomonic symptoms in schizophrenia? An empiric investigation of Schneider's first‐rank symptoms. Archives of General Psychiatry 1973;28(6):847‐52. [DOI] [PubMed] [Google Scholar]
- Carpenter WT Jr, Strauss JS. Cross‐cultural evaluation of Schneider's first‐rank symptoms of schizophrenia: a report from the International Pilot Study of Schizophrenia. American Journal of Psychiatry 1974; Vol. 131, issue 6:682‐7. [0002‐953X] [DOI] [PubMed]
- Carpenter WT Jr, Strauss JS, Bartko JJ. The diagnosis and understanding of schizophrenia. Part I. Use of signs and symptoms for the identification of schizophrenic patients. Schizophrenia Bulletin 1974;11:37‐49. [0586‐7614: (Print)]. [DOI] [PubMed] [Google Scholar]
Chandrasena 1987 {published data only}
Chopra 1987 {published data only}
Daradkeh 1995 {published data only}
- Daradkeh TK, El‐Rufaie OEF, Younis YO, Ghubash R. The diagnostic stability of ICD‐10 psychiatric diagnoses in clinical practice. European Psychiatry 1997;12:136‐9. [DOI] [PubMed] [Google Scholar]
- Daradkeh TK, Hamdi E, Amin Y. Schneider's first‐rank symptoms of schizophrenia in an Arab patient population: Their prevalence and diagnostic validity. Arab Journal of Psychiatry 1995;6:39‐50. [Google Scholar]
Gonzalez‐Pinto 2004 {published data only}
Ihara 2009 {published data only}
- Ihara K, Morgan C, Fearon P, Dazzan P, Demjaha A, Lloyd T, et al. The prevalence, diagnostic significance and demographic characteristics of Schneiderian first‐rank symptoms in an epidemiological sample of first‐episode psychoses. Psychopathology 2009; Vol. 42, issue 2:81‐91. [0254‐4962] [DOI] [PubMed]
Ndetei 1983 {published data only}
O'Grady 1990 {published data only}
Peralta 1999 {published data only}
Preiser 1979 {published data only}
Radhakrishnan 1983 {published data only}
Raguram 1985 {published data only}
- Raguram R, Kapur R. A study of first rank symptoms of Schneider in functional psychoses. Indian Journal of Psychiatry 1985; Vol. 27, issue 2:111‐8. [0019‐5545] [PMC free article] [PubMed]
Ramperti 2010 {published data only}
Rosen 2011 {published data only}
- Rosen C, Grossman LS, Harrow M, Bonner‐Jackson A, Faull R. Diagnostic and prognostic significance of Schneiderian first‐rank symptoms: a 20‐year longitudinal study of schizophrenia and bipolar disorder. Comprehensive Psychiatry 2011; Vol. 52, issue 2:126‐31. [1532‐8384] [DOI] [PMC free article] [PubMed]
Salleh 1992 {published data only}
Stephens 1980 {published data only}
Stephens 1982 {published data only}
Tandon 1987 {published data only}
Tanenberg‐Karant 1995 {published data only}
Wu 1990 {published data only}
- Wu Y. Study of the diagnostic specificity by Schneider's first rank symptoms. [Chinese]. Zhonghua shen jing jing shen ke za zhi = Chinese Journal of Neurology and Psychiatry 1990; Vol. 23, issue 2:79‐80, 126. [0412‐4057] [PubMed]
References to studies excluded from this review
Abrams 1973 {published data only}
- Abrams R, Taylor M. First‐rank symptoms, severity of illness, and treatment response in schizophrenia. Comprehensive Psychiatry 1973;14:353‐5. [DOI] [PubMed] [Google Scholar]
Abrams 1981 {published data only}
- Abrams R, Taylor MA. Importance of schizophrenic symptoms in the diagnosis of mania. American Journal of Psychiatry 1981;138:658‐61. [DOI] [PubMed] [Google Scholar]
Ahmed 1984 {published data only}
- Ahmed S H, Naeem S. First rank symptoms and diagnosis of schizophrenia in developing countries. Psychopathology 1984;17:275‐9. [DOI] [PubMed] [Google Scholar]
Al‐Ansari 1989 {published data only}
- Al‐Ansari EA, Emara MM, Mirza IA, El‐Islam MF. Schizophrenia in ICD‐10: a field trial of suggested diagnostic guidelines. Comprehensive Psychiatry 1989;30:416‐9. [DOI] [PubMed] [Google Scholar]
Anselmetti 2007 {published data only}
- Anselmetti S, Cavallaro R, Bechi M, Angelone SM, Ermoli E, Cocchi F, et al. Psychopathological and neuropsychological correlates of source monitoring impairment in schizophrenia. Psychiatry Research 2007;150:51‐9. [DOI] [PubMed] [Google Scholar]
Asnis 1982 {published data only}
- Asnis L C, Baron M, Gruen R. Diagnostic overlap in schizophrenia research: relation to outcome predictors and family history. Psychiatry Research 1982;6:345‐53. [DOI] [PubMed] [Google Scholar]
Basu 1999 {published data only}
- Basu D, Malhotra A, Bhagat A, Varma VK. Cannabis psychosis and acute schizophrenia. a case‐control study from India. European Addiction Research 1999;5(2):71‐3. [DOI] [PubMed] [Google Scholar]
Beckmann 1990 {published data only}
- Beckmann H, Fritze J, Lanczik M. Prognostic validity of the cycloid psychoses. A prospective follow‐up study. Psychopathology 1990;23:205‐11. [DOI] [PubMed] [Google Scholar]
Berner 1984 {published data only}
- Berner P, Gabriel E, Kronberger ML, Kufferle B, Schanda H, Trappl R. Course and outcome of delusional psychoses. Psychopathology 1984;17:28‐36. [DOI] [PubMed] [Google Scholar]
Berner 1986 {published data only}
- Berner P, Katschnig H, Lenz C. The polydiagnostic approach in research on schizophrenia. Issues in Psychiatric Classification: Science, Practice, and Social Policy. New York: Human Sciences Press, 1986:70‐91. [Google Scholar]
Berner 1986a {published data only}
- Berner P, Katschnig H, Lenz G. First‐rank symptoms and Bleuler's basic symptoms. New results in applying the polydiagnostic approach. Psychopathology 1986;19:244‐52. [DOI] [PubMed] [Google Scholar]
Bland 1978 {published data only}
- Bland RC. Diagnosis of schizophrenia. Canadian Psychiatric Association Journal. 1978;23:291‐6. [DOI] [PubMed] [Google Scholar]
Bland 1979 {published data only}
- Bland RC, Orn H. Schizophrenia: diagnostic criteria and outcome. British Journal of Psychiatry 1979;134:34‐8. [DOI] [PubMed] [Google Scholar]
Botros 2006 {published data only}
- Botros MM, Atalla SF, El‐Islam M F. Schneiderian first rank symptoms in a sample of schizophrenic patients in Egypt. International Journal of Social Psychiatry 2006;52:424‐31. [DOI] [PubMed] [Google Scholar]
Burbach 1984 {published data only}
- Burbach DJ, Lewine RR, Meltzer HY. Diagnostic concordance for schizophrenia as a function of sex. Journal of Consulting and Clinical Psychology 1984;52:478‐9. [DOI] [PubMed] [Google Scholar]
Cardno 2002 {published data only}
- Cardno AG, Sham PC, Farmer AE, Murray RM, McGuffin P. Heritability of Schneider's first‐rank symptoms. British Journal of Psychiatry 2002;180:35‐8. [DOI] [PubMed] [Google Scholar]
Ceccherini‐Nelli 2003 {published data only}
- Ceccherini‐Nelli A, Crow TJ. Disintegration of the components of language as the path to a revision of Bleuler's and Schneider's concepts of schizophrenia: Linguistic disturbances compared with first‐rank symptoms in acute psychosis. British Journal of Psychiatry 2003; Vol. 182, issue MAR.:233‐40. [0007‐1250] [DOI] [PubMed]
Cernovsky 1985 {published data only}
- Cernovsky Z, Landmark J, Leslie B. Social and anamnestic correlates of consensus in diagnosing schizophrenia. Journal of Clinical Psychology 1985;41:614‐9. [DOI] [PubMed] [Google Scholar]
Chandrasena 1979 {published data only}
- Chandrasena R, Rodrigo A. Schneider's First Rank Symptoms: their prevalence and diagnostic implications in an Asian population. British Journal of Psychiatry 1979;135:348‐51. [DOI] [PubMed] [Google Scholar]
Coffey 1993 {published data only}
- Coffey GJ, Mackinnon A, Minas IH. Interethnic variations in the presence of Schneiderian first rank symptoms. Australian and New Zealand Journal of Psychiatry 1993;27:219‐27. [DOI] [PubMed] [Google Scholar]
Compton 2008 {published data only}
- Compton MT, Leiner AS, Bergner E, Chien VH, Franz L, Goulding SM, et al. Prevalence, factorial structure, and clinical correlates of first rank symptoms in urban, African‐American patients with first‐episode nonaffective psychosis. Clinical Schizophrenia and Related Psychoses 2008; Vol. 2, issue 1:59‐69. [1935‐1232]
Conus 2004 {published data only}
- Conus P, Abdel‐Baki A, Harrigan S, Lambert M, McGorry PD. Schneiderian first rank symptoms predict poor outcome within first episode manic psychosis. Journal of Affective Disorders 2004;81:259‐68. [DOI] [PubMed] [Google Scholar]
Cowell 1996 {published data only}
- Cowell PE, Kostianovsky DJ, Gur RC, Turetsky BI, Gur RE. Sex differences in neuroanatomical and clinical correlations in schizophrenia. The American Journal of Psychiatry 1996;153(6):799‐805. [DOI] [PubMed] [Google Scholar]
Craddock 1996 {published data only}
- Craddock M, Asherson P, Owen MJ, Williams J, McGuffin P, Farmer AE. Concurrent validity of the OPCRIT diagnostic system. Comparison of OPCRIT diagnoses with consensus best‐estimate lifetime diagnoses. British Journal of Psychiatry 1996;169:58‐63. [DOI] [PubMed] [Google Scholar]
Cuesta 2007 {published data only}
- Cuesta M J, Peralta V, Zarzuela A. Empirical validation of competing definitions of schizophrenia: a poly‐diagnostic study of cognitive impairment in non‐affective psychosis. Schizophrenia Research 2007;95:39‐47. [DOI] [PubMed] [Google Scholar]
Deister 1993 {published data only}
- Deister A, Marneros A. Subtypes in schizophrenic disorders: frequencies in long‐term course and premorbid features. Social Psychiatry and Psychiatric Epidemiology 1993;28:164‐71. [DOI] [PubMed] [Google Scholar]
Deister 1994 {published data only}
- Deister A, Marneros A. Prognostic value of initial subtype in schizophrenic disorders. Schizophrenia Research 1994;12:145‐57. [DOI] [PubMed] [Google Scholar]
Dollfus 1992 {published data only}
- Dollfus S, Petit M, Menard JF. The relationship between 'chronic hallucinatory psychosis' (CHP) and schizophrenia. European Psychiatry 1992; Vol. 7:271‐6.
Dollfus 1993 {published data only}
- Dollfus S, Petit M, Menard J, Lesieur P. Schizophrenia: Comparison of 13 diagnostic systems in a cross‐sectional study. European Psychiatry. 1993;8:7‐13. [Google Scholar]
Dollfus 1993a {published data only}
- Dollfus S, Petit M, Menard J F, Lesieur P. Symptomatic and diagnostic stability in schizophrenia: A one‐year follow‐up study. European Psychiatry. 1993;8:131‐7. [Google Scholar]
Endicott 1982 {published data only}
- Endicott J, Nee J, Fleiss, J, Cohen J, Williams JBW, Robert Simon R. Diagnostic criteria for schizophrenia: Reliabilities and agreement between systems. Archives of General Psychiatry 1982;39(8):884‐9. [DOI] [PubMed] [Google Scholar]
Endicott 1986 {published data only}
- Endicott J, Nee J, Cohen J, Fleiss JL, Simon R. Diagnosis of schizophrenia. Prediction of short‐term outcome. Archives of General Psychiatry 1986;43:13‐9. [DOI] [PubMed] [Google Scholar]
Eva 1984 {published data only}
- Eva P, Cabane J, Ruiz A. Schizophrenia: Diagnostic errors. Revista de Psiquiatria Clinica 1984;21:31‐7. [Google Scholar]
Evans 1981 {published data only}
- Evans JW, Elliott H. Screening criteria for the diagnosis of schizophrenia in deaf patients. Archives of General Psychiatry 1981;38:787‐90. [DOI] [PubMed] [Google Scholar]
Fanous 2012 {published data only}
- Fanous AH, Amdur RL, O'Neill FA, Walsh D, Kendler KS. Concordance between chart review and structured interview assessments of schizophrenic symptoms. Comprehensive Psychiatry 2012;53:275‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fourneret 2001 {published data only}
- Fourneret P, Franck N, Slachevsky A, Jeannerod M. Self‐monitoring in schizophrenia revisited. NeuroReport 2001;12:1203‐8. [DOI] [PubMed] [Google Scholar]
Franck 2002 {published data only}
- Franck N, O'Leary DS, Flaum M, Hichwa RD, Andreasen NC. Cerebral blood flow changes associated with Schneiderian first‐rank symptoms in schizophrenia. Journal of Neuropsychiatry and Clinical Neurosciences 2002;14:277‐82. [DOI] [PubMed] [Google Scholar]
Ganesan 2005 {published data only}
- Ganesan V, Hunter MD, Spence SA. Schneiderian first‐rank symptoms and right parietal hyperactivation: a replication using FMRI. American Journal of Psychiatry 2005;162(8):154‐5. [DOI] [PubMed] [Google Scholar]
Gharagozlou 1979 {published data only}
- Gharagozlou H, Behin M. Diagnostic evaluation of Schneider first rank symptoms of schizophrenia among three groups of Iranians. Comprehensive Psychiatry 1979;20(3):242‐5. [DOI] [PubMed] [Google Scholar]
Gift 1980 {published data only}
- Gift TE, Strauss JS, Ritzler BA. How diagnostic concepts of schizophrenia differ. Journal of Nervous and Mental Disease 1980;168:3‐8. [DOI] [PubMed] [Google Scholar]
Glazer 1987 {published data only}
- Glazer WM, Pino CD, Quinlan D. The reassessment of chronic patients previously diagnosed as schizophrenic. Journal of Clinical Psychiatry 1987;48:430‐4. [PubMed] [Google Scholar]
Gur 1994 {published data only}
- Gur RE, Mozley PD, Shtasel DL, Cannon TD, Gallacher F, Turetsky B, et al. Clinical subtypes of schizophrenia: differences in brain and CSF volume. American Journal of Psychiatry 1994;151:343‐50. [DOI] [PubMed] [Google Scholar]
Gureje 1987 {published data only}
- Gureje O, Bamgboye EA. A study of Schneider's first‐rank symptoms of schizophrenia in Nigerian patients. British Journal of Psychiatry 1987;150:867‐9. [DOI] [PubMed] [Google Scholar]
Hayashi 1998 {published data only}
- Hayashi T, Hotta N, Fukastu N, Suga H. Clinical and socio‐demographic studies of atypical psychoses using ICD‐ 10 criteria. Neurology Psychiatry and Brain Research. 1998;6:147‐54. [Google Scholar]
Helmes 1983 {published data only}
- Helmes E, Landmark J, Kazarian SS. Inter‐rater reliability of twelve diagnostic systems of schizophrenia. Journal of Nervous and Mental Disease 1983;171:307‐11. [PubMed] [Google Scholar]
Hill 1996 {published data only}
- Hill C, Keks N, Roberts S, Opeskin K, Dean B, MacKinnon A, et al. Problem of diagnosis in postmortem brain studies of schizophrenia. American Journal of Psychiatry 1996;153:533‐7. [DOI] [PubMed] [Google Scholar]
Idrees 2010 {published data only}
- Idrees M, Khan I, Irfan M, Sarwar R. First rank symptoms in the diagnosis of schizophrenia. JPMI ‐ Journal of Postgraduate Medical Institute 2010;24:323‐8. [Google Scholar]
Jakobsen 2006 {published data only}
- Jakobsen K, Frederiksen J, Parnas J, Werge T. Diagnostic agreement of schizophrenia spectrum disorders among chronic patients with functional psychoses. Psychopathology 2006;39(6):269‐76. [DOI] [PubMed] [Google Scholar]
Kendell 1979 {published data only}
- Kendell RE, Brockington IF, Leff JP. Prognostic implications of six alternative definitions of schizophrenia. Archives of General Psychiatry 1979;36:25‐31. [DOI] [PubMed] [Google Scholar]
Klosterkotter 1992 {published data only}
- Klosterkotter J. The meaning of basic symptoms for the development of schizophrenic psychoses. Neurology Psychiatry and Brain Research. 1992;1:30‐41. [Google Scholar]
Koehler 1976 {published data only}
- Koehler K, Guth W. Schneider‐oriented versus Conrad‐oriented psychiatric diagnosis in the same German clinic. British Journal of Psychiatry 1976;129:446‐51. [DOI] [PubMed] [Google Scholar]
Koehler 1978 {published data only}
- Koehler K, Seminario I. First rank schizophrenia and research diagnosable schizophrenic and affective illness. Comprehensive Psychiatry 1978;19(5):401‐6. [DOI] [PubMed] [Google Scholar]
Kulhara 1988 {published data only}
- Kulhara P, Chandiramani K. Outcome of schizophrenia in India using various diagnostic systems. Schizophrenia Research. 1988;1:339‐49. [DOI] [PubMed] [Google Scholar]
Kulhara 1989 {published data only}
- Kulhara P, Avasthi A, Chandiramani K. Prognostic variables in schizophrenia. Indian Journal of Psychiatry 1989;31:51‐62. [PMC free article] [PubMed] [Google Scholar]
Landmark 1986 {published data only}
- Landmark J, Cernovsky ZZ, Merskey H, Leslie B. Interrelationships of systems for diagnosing schizophrenia. Comprehensive Psychiatry 1986;27:343‐50. [DOI] [PubMed] [Google Scholar]
Landmark 1990 {published data only}
- Landmark J, Merskey H, Cernovsky Z, Helmes E. The positive triad of schizophrenic symptoms. Its statistical properties and its relationship to 13 traditional diagnostic systems. British Journal of Psychiatry 1990;156:388‐94. [DOI] [PubMed] [Google Scholar]
Lenz 1986 {published data only}
- Lenz G, Katschnig H, David H. Symptoms, diagnosis and time in hospital. A polydiagnostic study of schizophrenia. Psychopathology 1986;19:253‐8. [DOI] [PubMed] [Google Scholar]
Lewine 1982 {published data only}
- Lewine R, Renders R, Kirchhofer M, Monsour A, Watt N. The empirical heterogeneity of first rank symptoms in schizophrenia. British Journal of Psychiatry 1982;140:498‐502. [DOI] [PubMed] [Google Scholar]
Lewine 1984 {published data only}
- Lewine R, Burbach D, Meltzer HY. Effect of diagnostic criteria on the ratio of male to female schizophrenic patients. American Journal of Psychiatry 1984;141:84‐7. [DOI] [PubMed] [Google Scholar]
Littlewood 1981 {published data only}
- Littlewood R, Lipsedge M. Acute psychotic reactions in Caribbean‐born patients. Psychological Medicine 1981;11:303‐18. [DOI] [PubMed] [Google Scholar]
Loftus 2000 {published data only}
- Loftus J, Delisi LE, Crow TJ. Factor structure and familiality of first‐rank symptoms in sibling pairs with schizophrenia and schizoaffective disorder. British Journal of Psychiatry 2000;177:15‐9. [DOI] [PubMed] [Google Scholar]
Maier 1986 {published data only}
- Maier W, Philipp M, Schlegel S. Operational diagnoses for schizophrenic and schizoaffective disorders: I. Interrater reliability. Pharmacopsychiatry 1986;19:178‐9. [Google Scholar]
Makanjuola 1987 {published data only}
- Makanjuola RO, Adedapo SA. The DSM‐III concepts of schizophrenic disorder and schizophreniform disorder. A clinical and prognostic evaluation. British Journal of Psychiatry 1987;151:611‐8. [DOI] [PubMed] [Google Scholar]
Malik 1990 {published data only}
- Malik S, Ahmed M, Bashir A, Choudhry T. Schneider's first‐rank symptoms of schizophrenia: Prevalence and diagnostic use: A study from Pakistan. British Journal of Psychiatry 1990;156:109‐11. [DOI] [PubMed] [Google Scholar]
Marneros 1984 {published data only}
- Marneros A. The pathognomonic value of K. Schneider's First Rank symptoms. Psychiatria Fennica. 1984;15:99‐105. [Google Scholar]
Mason 1997 {published data only}
- Mason P, Harrison G, Croudace T, Glazebrook C, Medley I. The predictive validity of a diagnosis of schizophrenia. A report from the International Study of Schizophrenia (ISoS) coordinated by the World Health Organization and the Department of Psychiatry, University of Nottingham. British Journal of Psychiatry 1997;170:321‐7. [DOI] [PubMed] [Google Scholar]
Matsuura 2004 {published data only}
- Matsuura M, Adachi N, Oana Y, Okubo Y, Kato M, Nakano T, et al. A polydiagnostic and dimensional comparison of epileptic psychoses and schizophrenia spectrum disorders. Schizophrenia Research 2004;69:189‐201. [DOI] [PubMed] [Google Scholar]
Mauri 1992 {published data only}
- Mauri M, Borri C, Giannotti D, Zambotto S, Cassano G B, Akiskal HS. Psychotic symptom patterns and the diagnosis of schizophrenia. Psychopathology 1992;25:5‐10. [DOI] [PubMed] [Google Scholar]
McGuffin 1984 {published data only}
McGuffin 1991 {published data only}
- McGuffin P, Farmer A, Harvey I. A polydiagnostic application of operational criteria in studies of psychotic illness. Development and reliability of the OPCRIT system. Archives of General Psychiatry 1991;48:764‐70. [DOI] [PubMed] [Google Scholar]
Melges 1977 {published data only}
- Melges FT, Freeman AM 3rd. Temporal disorganization and inner‐outer confusion in acute mental illness. American Journal of Psychiatry 1977;134:874‐7. [DOI] [PubMed] [Google Scholar]
Mellor 1970 {published data only}
- Mellor CS. First rank symptoms of schizophrenia. I. The frequnncy in schizophrenics on admission to hospital. II. Differences between individual first rank symptoms. British Journal of Psychiatry. 1970;117:15‐23. [PubMed] [Google Scholar]
Menezes 1993 {published data only}
Modestin 2003 {published data only}
- Modestin J, Huber A, Satirli E, Malti T, Hell D. Long‐term course of schizophrenic illness: Bleuler's study reconsidered. American Journal of Psychiatry 2003;160:2202‐8. [DOI] [PubMed] [Google Scholar]
Munk‐Jorgensen 1989 {published data only}
Nakaya 2002 {published data only}
- Nakaya M, Kusumoto K, Okada T, Ohmori K. Bizarre delusions and DSM‐IV schizophrenia. Psychiatry and Clinical Neuroscience 2002;56:391‐5. [DOI] [PubMed] [Google Scholar]
Ndetei 1984 {published data only}
Nordgaard 2008 {published data only}
- Nordgaard J, Arnfred SM, Handest P, Parnas J. The diagnostic status of first‐rank symptoms. Schizophrenia Bulletin 2008;34:137‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pela 1982 {published data only}
Peralta 1992 {published data only}
- Peralta V, Cuesta MJ. A polydiagnostic approach to self‐perceived cognitive disorders in schizophrenia. Psychopathology 1992;25:232‐8. [DOI] [PubMed] [Google Scholar]
Philipp 1986 {published data only}
- Philipp M, Maier W. The polydiagnostic interview: a structured interview for the polydiagnostic classification of psychiatric patients. Psychopathology 1986;19:175‐85. [DOI] [PubMed] [Google Scholar]
Philipp 1986a {published data only}
- Philipp M, Maier W, Frommberger U. Operational diagnoses for schizophrenic and schizoaffective disorders: II. Agreement between systems. Pharmacopsychiatry 1986;19:180‐1. [Google Scholar]
Pihlajamaa 2008 {published data only}
- Pihlajamaa J, Suvisaari J, Henriksson M, Heila H, Karjalainen E, Koskela J, et al. The validity of schizophrenia diagnosis in the Finnish Hospital Discharge Register: findings from a 10‐year birth cohort sample. Nordic Journal of Psychiatry 2008;62:198‐203. [DOI] [PubMed] [Google Scholar]
Ross 1991 {published data only}
- Ross CA. Epidemiology of multiple personality disorder and dissociation. Psychiatric Clinics of North America 1991;14:503‐17. [PubMed] [Google Scholar]
Salvatore 2011 {published data only}
- Salvatore P, Baldessarini RJ, Tohen M, Khalsa HM, Sanchez‐Toledo JP, Zarate CA Jr, et al. McLean‐Harvard International First‐Episode Project: two‐year stability of ICD‐10 diagnoses in 500 first‐episode psychotic disorder patients. Journal of Clinical Psychiatry 2011;72:183‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schanda 1984 {published data only}
- Schanda H, Thau K, Kufferle B, Kieffer W, Berner P. Heterogeneity of delusional syndromes: diagnostic criteria and course prognosis. Psychopathology 1984;17:280‐9. [DOI] [PubMed] [Google Scholar]
Schiopu 2005 {published data only}
- Schiopu B, Nel M, Hiemstra LA, Latecki B. Relevance of Schneider's first‐rank symptoms in Zulu patients with paranoid schizophrenia. South African Family Practice 2005;47:55‐60. [Google Scholar]
Serban 1979 {published data only}
- Serban G, Gidynski CB. Relationship between cognitive defect, affect response and community adjustment in chronic schizophrenics. British Journal of Psychiatry 1979;134:602‐8. [DOI] [PubMed] [Google Scholar]
Silverstein 1978 {published data only}
Silverstein 1981 {published data only}
- Silverstein M L, Harrow M. Schneiderian first‐rank symptoms in schizophrenia. Archives of General Psychiatry 1981;38:288‐93. [DOI] [PubMed] [Google Scholar]
Sougey 1987 {published data only}
- Sougey EB, Carvalho TF, Bandin JM, Albuquerque JO. Frequency of Kurt Schneider's first rank symptoms in schizophrenics in Northeastern Brazil. Revista ABP APAL 1987;9:151‐6. [Google Scholar]
Taylor 1972 {published data only}
Thorup 2007 {published data only}
- Thorup A, Petersen L, Jeppesen P, Nordentoft M. Frequency and predictive values of first rank symptoms at baseline among 362 young adult patients with first‐episode schizophrenia Results from the Danish OPUS study. Schizophrenia Research. 2007;97:60‐7. [DOI] [PubMed] [Google Scholar]
Vazquez‐Barquero 1995 {published data only}
- Vazquez‐Barquero JL, Cuesta Nunez MJ, Varga M, Herrera Castanedo S, Gaite L, Arenal A. The Cantabria first episode schizophrenia study: a summary of general findings. Acta Psychiatrica Scandinavica 1995;91:156‐62. [DOI] [PubMed] [Google Scholar]
Vega 2006 {published data only}
- Vega WA, Sribney WM, Miskimen TM, Escobar JI, Aguilar‐Gaxiola S. Putative psychotic symptoms in the Mexican American population: prevalence and co‐occurrence with psychiatric disorders. Journal of Nervous and Mental Disease 2006;194:471‐7. [DOI] [PubMed] [Google Scholar]
Wciorka 1995 {published data only}
- Wciorka J, Anczewska M, Chojnowska A, Stanikowska I. Delusional psychoses during first hospitalization: Age of onset and diagnosis of schizophrenia by six diagnostic criteria. Psychiatria Polska 1995;29:133‐46. [PubMed] [Google Scholar]
Wetterberg 1991 {published data only}
- Wetterberg L, Farmer AE. Clinical polydiagnostic studies in a large Swedish pedigree with schizophrenia. European Archives of Psychiatry and Clinical Neuroscience 1991;240:188‐90. [DOI] [PubMed] [Google Scholar]
Young 1982 {published data only}
- Young MA, Tanner MA, Meltzer HY. Operational definitions of schizophrenia: What do they identify?. Journal of Nervous and Mental Disease 1982;170:443‐7. [DOI] [PubMed] [Google Scholar]
Zarrouk 1978 {published data only}
- Zarrouk ET. The usefulness of first‐rank symptoms in the diagnosis of schizophrenia in a Saudi Arabian population. British Journal of Psychiatry 1978;132:571‐3. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Friedrich 1980 {published data only}
- Friedrich M, Leixnering W. Differential diagnosis of schizophrenia in children and adolescents. Acta Paedopsychiatrica: International Journal of Child & Adolescent Psychiatry 1980;46:21‐30. [PubMed] [Google Scholar]
Additional references
Astrachan 1974
- Astrachan BM, Brauer L, Harrow M, Schwartz C. Symptomatic outcome in schizophrenia. Archives of General Psychiatry 1974;31:155‐63. [DOI] [PubMed] [Google Scholar]
Bellak 1973
- Bellak L, Hurvich M, Gediman HK. Ego Functions in Schizophrenics, Neurotics, and Normals: A Systematic Study of Conceptual, Diagnostic, and Therapeutic Aspects. Wiley New York, 1973. [Google Scholar]
Bergman 2014
- Bergman H, Khodabakhsh A, Maayan N, Kirkham AJ, Adams CE, Soares‐Weiser K. Operational Criteria Checklist for Psychotic Illness and Affective Illness (OPCRIT+) for diagnosing schizophrenia in people with psychotic symptoms. Cochrane Database of Systematic Reviews 2014, Issue 6. [DOI: 10.1002/14651858.CD011104] [DOI] [Google Scholar]
Bleuler 1950
- Bleuler E. Dementia Praecox or the Group of Schizophrenias. New York: International Universities Press, 1950. [Google Scholar]
Bottlender 2003
- Bottlender R, Sato T, Jager M, Wegener U, Wittmann J, Strauss A, et al. The impact of the duration of untreated psychosis prior to first psychiatric admission on the 15‐year outcome in schizophrenia. Schizophrenia Research 2003;62(1‐2):37‐44. [PUBMED: 12765741] [DOI] [PubMed] [Google Scholar]
Bustillo 2001
- Bustillo J, Lauriello J, Horan W, Keith S. The psychosocial treatment of schizophrenia: an update. American Journal of Psychiatry 2001;158(2):163‐75. [DOI] [PubMed] [Google Scholar]
Carpenter 1973
- Carpenter WT, Strauss JS, Bartko JJ. Flexible system for the diagnosis of schizophrenia: a report from the WHO pilot study of schizophrenia. Science 1973;182:1275. [DOI] [PubMed] [Google Scholar]
Chu 2006
- Chu H, Cole SR. Biavariate meta‐analysis of sensitivity and specificity with sparse data: a generalized mixed linear model approach. Journal of Clinical Epidemiology 2006;59(12):1331‐2. [DOI] [PubMed] [Google Scholar]
De Haan 2003
- Haan L, Linszen DH, Lenior ME, Win ED, Gorsira R. Duration of untreated psychosis and outcome of schizophrenia: delay in intensive psychosocial treatment versus delay in treatment with antipsychotic medication. Schizophrenia Bulletin 2003;29(2):341‐8. [PUBMED: 14552508] [DOI] [PubMed] [Google Scholar]
Deeks 2005
- Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. Journal of Clinical Epidemiology 2005;58:882‐93. [DOI] [PubMed] [Google Scholar]
Feighner 1972
- Feighner JP, Robins E, Guze SB, Woodruff RA Jr, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Archives of General Psychiatry 1972;26(1):57‐63. [DOI] [PubMed] [Google Scholar]
Hor 2010
- Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. Journal of Psychopharmacology 2010;24(4 supplement):81‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kane 2001
- Kane JM, Marder SR, Schooler NR, Wirshing WC, Umbricht D, Baker RW, et al. Clozapine and haloperidol in moderately refractory schizophrenia: a 6‐month randomized and double‐blind comparison. Archive of General Psychiatry 2001;58(10):965‐72. [DOI] [PubMed] [Google Scholar]
Koehler 1979
- Koehler K, Seminario I. Research diagnosable "schizo‐affective" disorder in Schneiderian "first rank" schizophrenia. Acta Psychiatrica Scandinavica 1979;60(4):347‐54. [DOI] [PubMed] [Google Scholar]
Lawrie 2004
- Lawrie SM, Johnstone EC. Schizophrenia and related disorders. Companion to Psychiatric Studies. London: Churchill Livingstone, 2004. [Google Scholar]
Macaskill 2004
- Macaskill P. Empirical Bayes estimates generated in a hierarchical summary ROC analysis agreed closely with those of a full Bayesian analysis. Journal of Clinical Epidemiology 2004;57(9):925‐32. [DOI] [PubMed] [Google Scholar]
Marshall 2011
- Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database of Systematic Reviews 2011, Issue 6. [DOI: 10.1002/14651858.CD004718.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
McGrath 2008
- McGrath J, Saha S, Chant D, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiologic Reviews 2008;30:67‐76. [DOI] [PubMed] [Google Scholar]
McKenzie 2004
- McKenzie K, Patel V, Araya R. Learning from low income countries: mental health. BMJ 2004 Nov 13;329(7475):1138‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Palaniyappan 2014
- Palaniyappan L, Maayan N, Kirkham AJ, Davenport C, Khodabakhsh A, Adams CE, et al. Voxel‐based morphometry for separation of schizophrenia from other types of psychosis in first‐episode psychosis. Cochrane Database of Systematic Reviews 2014, Issue 3. [DOI: 10.1002/14651858.CD011021] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reitsma 2005
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. Journal of Clinical Epidemiology 2005;58:982‐990. [DOI] [PubMed] [Google Scholar]
Schneider 1959
- Schneider K. Clinical Psychopathology. New York: Grune & Stratton, 1959. [Google Scholar]
Spitzer 1978
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry 1978;35(6):773‐82. [DOI] [PubMed] [Google Scholar]
Takwoingi 2010
- Takwoingi Y, Deeks JJ. METADAS: A SAS macro for meta‐analysis of diagnostic accuracy studies. User Guide Version 1.3. 2010 July. http://srdta.cochrane.org (accessed 7th June 2012).
Tandon 2013
- Tandon R. Schizophrenia and other psychotic disorders in DSM‐5. Clinical Schizophrenia & Related Psychoses 2013;7(1):16‐9. [DOI: 10.3371/CSRP.TA.032513] [DOI] [PubMed] [Google Scholar]
Taylor 1978
- Taylor MA, Abrams R. The prevalence of schizophrenia: a reassessment of using modern diagnostic criteria. American Journal of Psychiatry 1978;135:945‐8. [DOI] [PubMed] [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS‐2: A revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529‐36. [DOI] [PubMed] [Google Scholar]
WHO 2007
- WHO. Nurses in mental health. http://www.who.int/mental_health/evidence/nursing_atlas_2007.pdf (accessed on 12/12/13).
WHO 2011
- WHO. WHO highlights global under investment in mental health care. http://www.who.int/mediacentre/news/notes/2011/mental_health_20111007/en/index.html (accessed on 12/12/13).
WHO 2012
- WHO. World Health Statistics 2012. http://www.who.int/gho/publications/world_health_statistics/EN_WHS2012_Full.pdf (accessed on 19/12/13.
Worster 2008
- Worster A, Carpenter C. Incorporation bias in studies of diagnostic tests: how to avoid being biased about bias. CJEM 2008 Mar;10(2):174‐5. [DOI] [PubMed] [Google Scholar]


