Abstract
Background
In order to optimize the tenogenic differentiation of mesenchymal stem cells (MSCs), researchers should consider various factors. However, this requires testing numerous experimental settings, which is costly and time-consuming. We aimed to assess the differential effects of transforming growth factor beta-3 (TGF-β3) on the tenogenesis of tonsil-derived MSCs (T-MSCs) and bone marrow-derived MSCs (BM-MSCs) using response surface methodology (RSM).
Methods
Bone marrow and tonsillar tissue were collected from four patients; mononuclear cells were separated and treated with 5 or 10 ng/mL of TGF-β3. A full factorial experimental design with a categorical factor of 0 was employed to study the effect of tension based on T-MSCs. Eighty-four trials were fitted with RSM and then used to obtain mathematical prediction models.
Results
Exposure of T-MSCs and BM-MSCs to TGF-β3 increased the expression of scleraxis (SCX), tenomodulin (TNMD), decorin, collagen I, and tenascin C. Expression of most of these factors reached a maximum after 2–3 days of treatment. The model predicted that the values of the tenocyte lineage-related factors assessed would be significantly increased at 2.5 days of culture with 2.7 ng/mL of TGF-β3 for T-MSCs and at 2.3 days of culture regardless of TGF-β3 concentration for BM-MSCs.
Conclusions
This study demonstrated that the RSM prediction of the culture time necessary for the tenogenic differentiation of T-MSCs and BM-MSCs under TGF-β3 stimulation was similar to the experimentally determined time of peak expression of tenocyte-related mRNAs, suggesting the potential of using the RSM approach for optimization of the culture protocol for tenogenesis of MSCs.
Keywords: Tenocyte, Tonsil-derived mesenchymal stem cells, Bone marrow-derived mesenchymal stem cells, Design of experiments, Response surface methodology
Background
Tissue healing after tendon repair surgery is challenging [1] because tendons have limited self-healing potential given the scar tissue on the repaired tendon [2, 3]. Even after long periods, the structure and strength of the repaired tissue do not show full recovery, and the tissue does not return to the pre-injury state [4]. For these reasons, there have been various studies done on tendon repair using tissue engineering with mesenchymal stem cells (MSCs) [5–9].
Although bone marrow-derived, adipose tissue-derived, synovial membrane-derived, and human embryonic MSCs have all been used to differentiate into tenocytes [6, 9, 10], these stem cells are obtained through invasive procedures. Thus, there is usually a lack of an adequate number of MSCs for clinical use [11]. Tonsil-derived MSCs (T-MSCs) obtained from waste tissue after tonsillectomy represent a new source of progenitor cells [12, 13], and several studies have focused on T-MSCs as cellular therapeutic agents for various diseases [12–19]. A previous study reported that T-MSCs have a good potential of being suitable for clinical banking of stem cells [12]. This means that it might be possible to conduct tonsil tissue banking (after tonsillectomy) for autogenic MSCs grafts to be used in case of future injury or disease. In the United States, 68.7% of the patients who underwent tonsillectomy were children less than 15 years old [20]. The prevalence of tendinopathies such as rotator cuff tears increased with age [21]. Because the donor age may affect the differentiation potential of MSCs [22, 23], T-MSCs harvested when a patient is young could have an advantage in terms of tenogenic differentiation potential compared with BM-MSCs harvested at the time of treatment. If T-MSCs show non-inferior tenogenic differentiation potential compared with other cell sources, physicians can consider tonsils as a stem cell source for cellular therapeutic agents. However, protocols for tenogenic differentiation of T-MSCs have not been established, and there is a lack of studies comparing the tenogenic differentiation potential of T-MSCs with MSCs from other cell sources.
Researchers should consider various potential factors affecting tenogenic differentiation of MSCs, such as culture time and the dose of the stimulator; however, this requires numerous experimental settings whose optimization is associated with high cost and time. Response surface methodology (RSM), which is used as a part of the design of experiments (DoE), is gaining recognition as a powerful approach for optimizing conditions to produce industrially important products such as chemicals and enzymes. It allows for multiple input factors to be manipulated, determining their effect on the desired output. In the last few years, RSM has been applied to optimize and evaluate the interactive effects of independent factors in numerous chemical and biochemical processes [24]. Recently, DoE has been used to investigate the differentiation of MSCs [25]. The main advantages of this methodology are that it (1) avoids experimental bias and (2) reduces the number of experiments, leading to a rational understanding of what could be the most favorable factor combination [24, 26]. By manipulating multiple inputs at the same time, DoE can identify important interactions that may be missed when experimenting with one factor at a time.
In this study, we aimed to optimize the culture conditions for the tenogenesis of T-MSCs and bone marrow-derived MSCs (BM-MSCs) using TGF-β3, testing different concentrations and culture times.
Materials and methods
This experimental study was approved by the institutional review board of our institution. Informed consent was obtained from all the patients or patients’ legal guardians.
Isolation and cultivation of human MSCs
Bone marrow was collected from four patients (mean age 79.0 ± 2.2 years) and mononuclear cells were separated using the Ficoll-Paque Premium (GE Healthcare, Chicago, IL, USA) gradient method. The isolated cells were seeded at a density of 1 × 105 cells/cm2 in a growth medium consisting of low-glucose Dulbecco’s Modified Eagle’s Medium (DMEM-LG; Hyclone, South Logan, UT, USA), 10% fetal bovine serum (FBS; Corning, Corning, NY, USA), 100 U/mL penicillin, and 100 μg/mL streptomycin. The tonsillar tissues were collected from four patients (mean age 7.6 ± 0.6 years) and minced with surgical scissors, followed by enzymatic digestion using 210 U/mL collagenase type I (Sigma, St. Louis, MO, USA) and 90 KU/mL DNase (Sigma, St. Louis, MO, USA) in DMEM-LG for 30 min at 37 °C. After filtration through a 100-μm cell strainer (BD Bioscience, Franklin Lakes, NJ, USA), the cells were washed twice with Dulbecco’s phosphate-buffered saline (D-PBS; Chembio, Seoul, Korea). Mononuclear cells were separated using the Ficoll-Paque gradient method [13] and seeded at a density of 1 × 104 cells/cm2 in growth medium. MSCs were incubated in a 5% CO2 incubator with humidified air at 37 °C, and the medium was replaced every other day. After reaching 80% confluency, the cells were split at a ratio of 1:3 for BM-MSCs and 1:4 for T-MSCs. MSCs were used between passages two and four for further experiments. Cell surface antigen phenotyping was performed on BM-MSCs and T-MSCs at the second passage to characterize the immunophenotype of MSCs using BD Stemflow™ hMSC Analysis kit (BD Bioscience, Franklin Lakes, NJ, USA). The analysis kit contained pre-conjugated and pre-titrated cocktails of the International Society for Cellular Therapy-defined positive expression markers (CD105-PerCP-Cy™5.5/CD73-APC/CD90-FITC) and negative expression markers (CD45/CD34/CD11b/CD19/HLA-DR-PE). Mouse isotype antibodies served as control. Labeled cells (1 × 106) were analyzed using a BD FACS LSR II SORP system (Becton Dickinson).
Tenogenic differentiation of BM-MSCs and T-MSCs
BM-MSCs and T-MSCs were seeded at a density of 1 × 104 cells/cm2 into 24-well plates in growth medium. After 18 h, the growth medium was removed and replaced with tenogenic differentiation media, which consisted of DMEM-LG, 10% FBS, and 50 μg/mL L-ascorbate-2-phosphate with 5 or 10 ng/mL TGF-β3 (Sigma, St. Louis, MO, USA). MSC growth medium was added to the control group. The medium was replaced three times a week.
Isolation of RNA and quantitative real-time PCR
Total RNA was isolated daily for up to 7 days using the total RNA mini kit supplemented with DNase I (NucleoGen Biotechnology). First-strand cDNA was synthesized using SuperScript III first-strand cDNA synthesis kit (Invitrogen), and quantitative real-time PCR was performed with SensiFAST SYBR Hi-ROX kit (Bioline) using the QuantStudio 3 real-time PCR system (Applied Biosystem, Life Technologies). The relative expression level of each gene was normalized to that of 18S rRNA and calculated using the 2−ΔΔCt method. The data are presented as fold changes relative to controls. The following genes were analyzed: scleraxis (SCX), tenomodulin (TNMD), decorin, collagen I/III, and tenascin C. These genes have a crucial role in the tenogenesis of MSCs [27–29]. The primers used in this study are shown in Table 1.
Table 1.
Primers used in this study*
| Gene | Forward Primer (5'->3') | Reverse Primer (5'->3') | |
|---|---|---|---|
| Adipogenic | PPARγ | GAGGCAGCAGAGGTTAACAGA | CACCGAGGCGTAAAGTACCA |
| LPL | CCGCCGACCAAAGAAGAGAT | TAGCCACGGACTCTGCTACT | |
| FABP4 | TGGGCCAGGAATTTGACGAA | CACATGTACCAGGACACCCC | |
| Osteogenic | RUNX2 | CCTACCTGAGCCAGATGACG | ATGCTGGGTGGCCTGAAAT |
| ALP | GAATCTTCCCCAAGGGCCAA | CAGAATGTTCCACGGAGGCT | |
| BGLAP | TCCTTTGGGGTTTGGCCTAC | CCAGCCTCCAGCACTGTTTA | |
| Chondrogenic | SOX9 | AGGAAGTCGGTGAAGAACGG | AAGTCGATAGGGGGCTGTCT |
| COL2 | GCTCCTGCCGTTTCGCTG | ATTATACCTCTGCCCATCCTGC | |
| ACAN | CTTCCGCTGGTCAGATGGAC | CGTTTGTAGGTGGTGGCTGT | |
| Tenogenic | SCX | ACAGATCTGCACCTTCTGCC | GCCACCTCCTAACTGCGAAT |
| TNMD | TCCCTCAGGCTCTGGTATGA | AGGACTGAGAGACCACTGCT | |
| DCN | TGCCAAAGGATCTTCCCCCT | AGGTGTAAATGCTCCAGGACT | |
| COL1A1 | AGTGGTTTGGATGGTGCCAA | GCACCATCATTTCCACGAGC | |
| COL3A1 | TGGAGGATGGTTGCACGAAA | ACAGCCTTGCGTGTTCGATA | |
| TNC | ATGGGCAGACGCACCATTAG | TGTGCATCGACCTTCACAAGA | |
| Internal control | 18S rRNA | GTAACCCGTTGAACCCCATT | CCATCCAATCGGTAGTAGCG |
*NCBI/ Primer-BLAST: Finding primers specific to your PCR template (using Primer3 and BLAST). Available from: https://www.ncbi.nlm.nih.gov/tools/primer-blast/ (Assessed on 15 December 2017)
Experimental design
A full factorial experimental design with a categorical factor of 0 was employed to study the effect of tension in T-MSCs. The design comprised of three levels coded as −1, 0, and +1. In total, 18 runs were performed in duplicate to optimize the level of the chosen variables, such as the number of days in culture and amount of TGF-β3 added. For the purpose of statistical computation, two independent variables denoted as x1 and x2 were selected. The levels used in the computation were determined from preliminary experiments and are presented in Table 2.
Table 2.
ANOVA for response surface model
| MSCs | Source | Sum of squares | Mean square | F value | p value |
|---|---|---|---|---|---|
| T-MSCs | Days | 17.57867 | 5.859557 | 9.98 | < 0.001 |
| Concentration of TGF-β3 | 88.30324 | 29.43411 | 50.11 | < 0.001 | |
| BM-MSCs | Days | 37.2556 | 12.4185 | 3.68 | 0.013 |
| Concentration of TGF-β3 | 71.4878 | 23.8293 | 7.07 | < 0.001 |
MSCs mesenchymal stem cells, T-MSCs tonsil-derived mesenchymal stem cells, BM-MSCs bone marrow-derived mesenchymal stem cells
The results were analyzed via analysis of variance (ANOVA). Multi-level factorial designs were used to estimate the response, calculated according to the following second-degree polynomial equation (1):
| 1 |
where Y is the estimated response; βo, βi, βii,and βij are the regression coefficients for intercept, linearity, square, and interaction, respectively; and Xi and Xj(i, j = 1, 2, i ≠ j) are the different interaction coefficients between the predicted response and independent variables in the coded values according to Table 2.
In this study, RSM combined with a full factorial design was used to investigate MSCs in tissues. By using a multi-level two-factorial design and a full range of RSM, the following parameters were optimized: SCX, TNMD, decorin, collagen I/III ratio, and tenascin C. A second-order polynomial regression model was used to generate three-dimensional response surfaces of MSCs. The regression model would provide a good explanation of the relationship between the independent variables and responses [30].
Statistical analysis
The statistical significance among different concentrations and time points was analyzed by ANOVA, followed by Tukey’s multiple comparison test using SAS version 9.4.2 (SAS Institute, Cary, NC). All statistics were two-tailed, and p < 0.05 was considered significant.
Results
Immunophenotypic characterization of BM-MSCs and T-MSCs
Immunophenotypic surface marker analysis of BM-MSCs and T-MSCS showed the typical expression profile of human MSCs. Both MSC populations expressed CD73, CD90, and CD105, whereas they lacked expression of CD11b, CD19, CD34, CD45, and HLA-DR (Table 3). The T-MSCs used in this study showed stemness, meaning that they are at least able to differentiate into adipocytes, osteoblasts, and chondroblasts [31].
Table 3.
Immunophenotypic markers on the cell surface of T-MSCs and T-MSCs
| BM-MSCs | T-MSCs | ||
|---|---|---|---|
| Positive | CD73 | 99.9 ± 0.05 | 99.9 ± 0.03 |
| CD90 | 99.6 ± 0.00 | 97.7 ± 1.57 | |
| CD105 | 99.8 ± 0.10 | 99.9 ± 0.05 | |
| Negative | CD11b | 1.2 ± 1.00 | 0.23 ± 0.03 |
| CD19 | |||
| CD34 | |||
| CD45 | |||
| HLA-DR | |||
T-MSCs tonsil-derived mesenchymal stem cells, BM-MSCs bone marrow-derived mesenchymal stem cells
Expression of tenogenic genes in MSCs under TGF-β3 stimulation
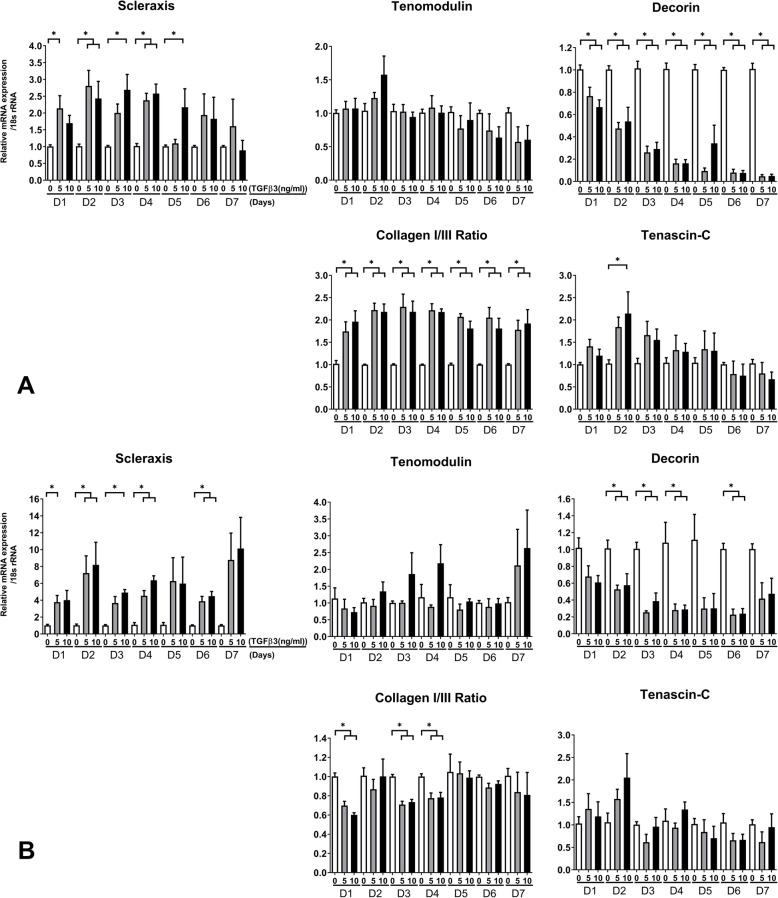
Exposure of T-MSCs and BM-MSCs to TGF-β3 resulted in increased expression of SCX, TNMD, and tenascin C, as well as increased collagen I/III ratio. The expression of decorin was lower in both T-MSCs and BM-MSCs than in untreated MSCs. The peak expression of each mRNA varied slightly according to the culture time and the concentration of TGF-β3 (Fig. 1).
Fig. 1.
Tenogenic mRNA expression of T-MBCs (a) and BM-MSCs (b) exposed to TGF-β3. The peak expression of each mRNA differed slightly according to the culture time and TGF-β3 concentration. The collagen I to III ratio of T-MSCs increased regardless of TGF-β3 concentration, whereas the ratio in BM-MSCs decreased. (*p < 0.05, analyzed by one-way analysis of variance, followed by Tukey’s multiple comparison test)
Optimization of tenocyte lineage-related factors from T-MSCs
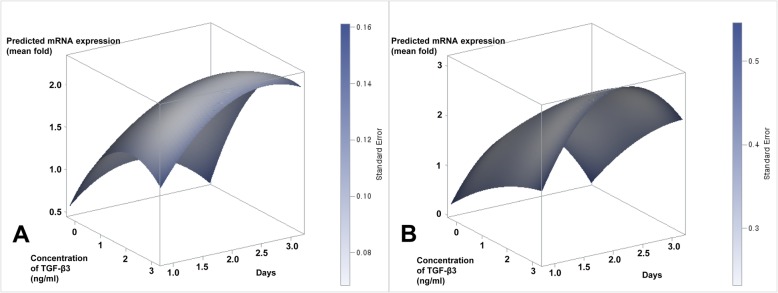
The DoE used in this study allowed for the optimization of tenocyte lineage-related factors from T-MSCs and BM-MSCs under different TGF-β3 concentrations and culture times. From the DoE approach, the predicted value of SCX from T-MSCs was significantly increased at 8.4 ng/mL TGF-β3 (p = 0.014) and 2.3 days (55.2 h) of culture (p = 0.040); the expression of collagen I showed the maximum increase at 8.1 ng/mL TGF-β3 (p < 0.001) at 2.7 days (64.8 h) of culture (p = 0.036); TNMD peaked at 2.5 days (60 h) of culture (p = 0.011), regardless of TGF-β3 concentration; and TGF-β3 concentration affected the peak expression of decorin (p < 0.001) and the ratio of collagen I to III (p < 0.001) regardless of culture time (Table 4). For all the tenocyte lineage-related mRNAs that were assessed, the predicted value of the factors was significantly increased at 2.7 ng/mL TGF-β3 (p < 0.001) at 2.5 days of culture (p = 0.001) (Fig. 2a).
Table 4.
Optimization of each tenocyte lineage-related factor from T-MSCs and BM-MSCs using response surface methodology
| Estimated value from T-MSCs | Estimated value from BM-MSCs | |||||||
|---|---|---|---|---|---|---|---|---|
| Time (day) | p value | Concentration | p value | Time (day) | p value | Concentration | p value | |
| Scleraxis | 2.3 | 0.040 | 8.4 | 0.014 | 2.1 | 0.014 | 3.6 | 0.133 |
| Tenomodulin | 2.5 | 0.011 | 31.2 | 0.528 | 2.9 | 0.872 | 0.6 | 0.034 |
| Decorin | 4.8 | 0.891 | 1.1 | < 0.001 | 0.6 | 0.599 | 2.0 | 0.004 |
| Collagen I/III | 2.8 | 0.376 | 7.8 | < 0.001 | 2.1 | 0.009 | 2.3 | 0.018 |
| Tenacin C | 2.2 | 0.038 | 7.6 | 0.075 | 1.9 | 0.019 | 0.2 | 0.805 |
TGF-β3 transforming growth factor-beta 3, T-MSCs tonsil-derived mesenchymal stem cells, BM-MSCs bone marrow-derived mesenchymal stem cells
Fig. 2.
Response surface for all tenocyte lineage-related mRNAs from T-MSCs (a) and BM-MSCs (b)
Optimization of tenocyte lineage-related factors from BM-MSCs
From the DoE approach, the predicted maximum ratio of collagen I to III in BM-MSCs was significantly increased at 2.3 ng/mL TGF-β3 (p = 0.018) and 2.1 days of culture (p = 0.009); the maximum expression of SCX, collagen I, and tenascin C was affected by culture time; the expression of TNMD and decorin peaked at 0.6 ng/mL (p = 0.036) and 2.0 ng/mL (p = 0.004) of TGF-β3, respectively, regardless of culture time for the predicted peak expression of TNMD (p = 0.872) and decorin (p = 0.599) (Table 4). For all the tenocyte lineage-related mRNAs that were assessed, the predicted value of the factors was significantly increased at 2.3 days of culture (p = 0.004) regardless of TGF-β3 concentration (Fig. 2b).
A full factorial design is a powerful tool for understanding complex processes of tenocyte lineage-related factors in multifactor systems because it includes all possible factor combinations for each of the factors. RSM is an empirical statistical technique employed for multiple regression analysis that uses quantitative data obtained from design experiments to solve multivariate equations simultaneously.
The quadratic equation for predicting the optimum point was obtained according to the data and input variables, and then the empirical relationship between the response and independent variables in the coded units was presented based on the experimental results as follows:
where Y is the T-MSCs, and X1 and X2 are the time in days and the concentration of TGF-β3, respectively (Table 5). The results of the ANOVA for the quadratic equation are tabulated in Table 5. The ANOVA shows whether the equation and actual relationship between response and significant variables represented by the equation are accurate. The significance of the coefficient term is determined by the values of F and p, and larger values of F and smaller values of p represent more significant terms.
Table 5.
ANOVA for response surface quadratic model
| MSCs | Source | Estimate | Standard error | F value | p value |
|---|---|---|---|---|---|
| T-MSCs | Intercept | 0.064 | 0.337 | 0.04 | 0.849 |
| X1 | 1.143 | 0.352 | 10.50 | 0.0013 | |
| X2 | 0.623 | 0.151 | 16.97 | <.0001 | |
| −0.288 | 0.058 | 11.29 | 0.0009 | ||
| −0.163 | 0.044 | 13.91 | 0.0002 | ||
| X1X2 | 0.105 | 0.039 | 7.08 | 0.0083 | |
| BM-MSCs | Intercept | −1.874 | 1.142 | 2.69 | 0.1029 |
| X1 | 3.534 | 1.195 | 8.76 | 0.0035 | |
| X2 | 0.442 | 0.513 | 0.74 | 0.3897 | |
| −0.895 | 0.290 | 9.48 | 0.0024 | ||
| −0.064 | 0.148 | 0.18 | 0.6671 | ||
| X1X2 | 0.117 | 0.134 | 0.76 | 0.3855 |
MSCs mesenchymal stem cells, T-MSCs tonsil-derived mesenchymal stem cells, BM-MSCs bone marrow-derived mesenchymal stem cells, X1, day; X2, concentration of TGF-β3
In the results, were highly significant factors. The analysis of equation (1) depicted that the variables, i.e., time in days and concentration of TGF-β3, have positive effects on T-MSCs. Synergistic interactions between time and concentration were highly significant (p < 0.05). The results also indicated that the selected quadratic model was adequate in assuming the response variables for the experimental data.
Three-dimensional response surface plot
Figure 2 depicts the three-dimensional response surface relationship between culture time and TGF-β3 concentration for T-MSCs and BM-MSCs. MSCs were sensitive to culture time and TGF-β3 concentration, which was consistent with the results presented in Table 5. These data indicate that the appropriate conditions would result in the highest mRNA concentration. Response surface plots as a function of two factors at a time, with the maintenance of all other factors at fixed levels, clarify both the main and interaction effects of the two factors. In the present study, the interaction effects of the variables and optimal levels of each variable were determined by the response surface graphs. The optimum values drawn from these figures were in close agreement with those obtained by optimizing the regression model equation (1).
Discussion
In this study, we aimed to assess the effects of TGF-β3 on the tenogenesis of T-MSCs and BM-MSCs using RSM. We found that tenocyte-like cells could be successfully differentiated from T-MSCs and BM-MSCs under TGF-β3 stimulation.
Traditionally, protocol optimization for the differentiation of T-MSCs would require the consideration of various factors that influence tenogenesis, making it a resource-intensive process. We conducted this study to optimize the culture conditions for tenogenesis of T-MSCs and BM-MSCs under TGF-β3 stimulation at different concentrations and culture times using DoE. This statistical method predicted that the expression of differentiation markers would be significantly induced after 2.5 and 2.3 days in culture for T-MSCs and BM-MSCs, respectively. We validated this prediction experimentally by exposing T-MSCs and BM-MSCs to various concentrations of TGF-β3, which resulted in an increase in the expression of the differentiation markers SCX, TNMD, decorin, collagen I, and tenascin C after 2–3 days of culture.
The statistical methods used in this study, RSM and DoE, might be unfamiliar to most physicians. Here is an example of their work: while doing the interior design of a new house, the final effect will depend on various factors such as color of the walls, lights, placement of various objects, and others. The final outcome can be impacted by variation in each factor alone, or a variation in a combination of these factors at the same time. Hence, in order to do an effective job, it is important to know how each of these factors impact the final outcome, which critical factors have the most impact, and which combinations have the most significant impact. To solve this problem, the interior designer can plan and conduct some experiments. DoE is a statistical method that helps solve complicated problems and save time and cost by reducing the number of required experiments. That is, the DoE is an efficient method for planning experiments that can be analyzed to yield valid and objective conclusions with less experimental effort. The choice of DoE depends on the objectives of the experiment and the number of factors to be investigated. RSM is used as a DoE tool, used to fit models and analyze problems in which several independent variables influence a dependent variable or response. RSM has been applied for developing mathematical models in the form of multiple regression equations [32]. Recently, DoE has been used in molecular biology and tissue engineering [25]. The present study represents the first stages of research regarding tenogenesis of MSCs, and we believe that the methodology used here can contribute to future studies.
We found that the expression of all examined molecules except for decorin tended to increase after exposure of T-MSCs and BM-MSCs to TGF-β3. Our results were similar to those of a previous study [29]. Although the peak expression of each gene for T-MSCs and BM-MSCs was analyzed using DoE, the optimal culture time and concentration of TGF-β3 varied for each gene. For instance, the expression of decorin decreased as the culture progressed, whereas the expression of TNMD peaked during the 7-day culture in BM-MSCs after TGF-β3 treatment. Since the expression levels of all genes that were analyzed in this study should increase for tenogenesis of MSCs, we could not determine the optimal culture time. Although the expression of TNMD did not change significantly (Fig. 1), we could not determine the expression of TNMD after exposure of MSCs to TGF-β3 owing to the small sample size and experimental settings.
There are certain limitations to this study. First, MSCs were stimulated only by a single chemical. Several other proteins can be stimulation candidates for MSCs, although we only referred to previous studies that used TGF-β for tenogenic differentiation of MSCs [8, 33]. Therefore, different approaches would be required for different chemical stimulators. Second, we did not consider the effect of mechanical stimulation on the tenogenesis of MSCs. Several studies showed that mechanical stretching stimulates MSCs to proliferate and differentiate into tenocytes [34, 35]. Further research focusing on mechanical stimulation of T-MSCs and BM-MSCs is needed.
In summary, we optimized a protocol for the tenogenic differentiation of T-MSCs and BM-MSCs using the DoE approach. This approach was less expensive than the standard experimentation-based optimization approach. In addition, our protocol was validated experimentally. This study suggests the potential of using the DoE approach for optimization of the culture protocol for tenogenesis of MSCs.
Acknowledgements
Not applicable.
Abbreviations
- ANOVA
Analysis of variance
- BM-MSCs
Bone marrow-derived mesenchymal stem cells
- DMEM-LG
Low-glucose Dulbecco’s Modified Eagle’s Medium
- DoE
Design of experiments
- D-PBS
Dulbecco’s phosphate-buffered saline
- FBS
Fetal bovine serum
- MSCs
Mesenchymal stem cells
- RSM
Response surface methodology
- SCX
Scleraxis
- T-MSCs
Tonsil-derived mesenchymal stem cells
- TNMD
Tenomodulin
Authors’ contributions
All authors on this manuscript (SYL, HK, S-JS, and S-SK) made significant contributions to the study design. SYL, HK, and S-JS were involved in the acquisition of data. SYL, S-JS, and S-SK were involved in the analysis and interpretation of data, as well as drafting the manuscript. All authors gave final approval of the version to be published.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (NRF-2019R1A2C2010150) and was partly supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (2017R1E1A1A03070345).
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the institutional board of Ewha Womans University Mokdong Hospital (IRB number: EUMC-06-048). Informed consent was obtained from all of the patients or patients’ legal guardians.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Soon-Sun Kwon, Email: qrio1010@gmail.com.
Hyang Kim, Email: hyang9252@gmail.com.
Sang-Jin Shin, Email: sjshin622@ewha.ac.kr.
Seung Yeol Lee, Email: kernels00@naver.com.
References
- 1.Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87(1):187–202. doi: 10.2106/JBJS.D.01850. [DOI] [PubMed] [Google Scholar]
- 2.Longo UG, Lamberti A, Maffulli N, Denaro V. Tissue engineered biological augmentation for tendon healing: a systematic review. Br Med Bull. 2011;98:31–59. doi: 10.1093/bmb/ldq030. [DOI] [PubMed] [Google Scholar]
- 3.Yao L, Bestwick CS, Bestwick LA, Maffulli N, Aspden RM. Phenotypic drift in human tenocyte culture. Tissue Eng. 2006;12(7):1843–1849. doi: 10.1089/ten.2006.12.1843. [DOI] [PubMed] [Google Scholar]
- 4.Omachi T, Sakai T, Hiraiwa H, Hamada T, Ono Y, Nakashima M, Ishizuka S, Matsukawa T, Oda T, Takamatsu A, et al. Expression of tenocyte lineage-related factors in regenerated tissue at sites of tendon defect. J Orthop Sci. 2015;20(2):380–389. doi: 10.1007/s00776-014-0684-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bullough R, Finnigan T, Kay A, Maffulli N, Forsyth NR. Tendon repair through stem cell intervention: cellular and molecular approaches. Disabil Rehabil. 2008;30(20-22):1746–1751. doi: 10.1080/09638280701788258. [DOI] [PubMed] [Google Scholar]
- 6.Awad HA, Butler DL, Boivin GP, Smith FN, Malaviya P, Huibregtse B, Caplan AI. Autologous mesenchymal stem cell-mediated repair of tendon. Tissue Eng. 1999;5(3):267–277. doi: 10.1089/ten.1999.5.267. [DOI] [PubMed] [Google Scholar]
- 7.Awad HA, Boivin GP, Dressler MR, Smith FN, Young RG, Butler DL. Repair of patellar tendon injuries using a cell-collagen composite. J Orthop Res. 2003;21(3):420–431. doi: 10.1016/S0736-0266(02)00163-8. [DOI] [PubMed] [Google Scholar]
- 8.Yu Y, Lee S, Yang E, Kim H, Jo I, Shin S. Expression of tenocyte lineage-related factors from tonsil-derived mesenchymal stem cells. Tissue Eng Regen Med. 2016;13(2):162–170. doi: 10.1007/s13770-016-9134-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SY, Kwon B, Lee K, Son YH, Chung SG. Therapeutic mechanisms of human adipose-derived mesenchymal stem cells in a rat tendon injury model. Am J Sports Med. 2017;45(6):1429–1439. doi: 10.1177/0363546517689874. [DOI] [PubMed] [Google Scholar]
- 10.Dai L, Hu X, Zhang X, Zhu J, Zhang J, Fu X, Duan X, Ao Y, Zhou C. Different tenogenic differentiation capacities of different mesenchymal stem cells in the presence of BMP-12. J Transl Med. 2015;13:200. doi: 10.1186/s12967-015-0560-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bagnaninchi PO, Yang Y, El Haj AJ, Maffulli N: Tissue engineering for tendon repair. Br J Sports Med 2007, 41(8):e10; discussion e10. [DOI] [PMC free article] [PubMed]
- 12.Ryu KH, Cho KA, Park HS, Kim JY, Woo SY, Jo I, Choi YH, Park YM, Jung SC, Chung SM, et al. Tonsil-derived mesenchymal stromal cells: evaluation of biologic, immunologic and genetic factors for successful banking. Cytotherapy. 2012;14(10):1193–1202. doi: 10.3109/14653249.2012.706708. [DOI] [PubMed] [Google Scholar]
- 13.Janjanin S, Djouad F, Shanti RM, Baksh D, Gollapudi K, Prgomet D, Rackwitz L, Joshi AS, Tuan RS. Human palatine tonsil: a new potential tissue source of multipotent mesenchymal progenitor cells. Arthritis Res Ther. 2008;10(4):R83. doi: 10.1186/ar2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim SY, Kim YR, Park WJ, Kim HS, Jung SC, Woo SY, Jo I, Ryu KH, Park JW. Characterisation of insulin-producing cells differentiated from tonsil derived mesenchymal stem cells. Differentiation. 2015;90(1-3):27–39. doi: 10.1016/j.diff.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Park YS, Kim HS, Jin YM, Yu Y, Kim HY, Park HS, Jung SC, Han KH, Park YJ, Ryu KH, et al. Differentiated tonsil-derived mesenchymal stem cells embedded in Matrigel restore parathyroid cell functions in rats with parathyroidectomy. Biomaterials. 2015;65:140–152. doi: 10.1016/j.biomaterials.2015.06.044. [DOI] [PubMed] [Google Scholar]
- 16.Park M, Kim YH, Woo SY, Lee HJ, Yu Y, Kim HS, Park YS, Jo I, Park JW, Jung SC, et al. Tonsil-derived mesenchymal stem cells ameliorate CCl4-induced liver fibrosis in mice via autophagy activation. Sci Rep. 2015;5:8616. doi: 10.1038/srep08616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu Y, Park YS, Kim HS, Kim HY, Jin YM, Jung SC, Ryu KH, Jo I. Characterization of long-term in vitro culture-related alterations of human tonsil-derived mesenchymal stem cells: role for CCN1 in replicative senescence-associated increase in osteogenic differentiation. J Anat. 2014;225(5):510–518. doi: 10.1111/joa.12229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryu KH, Kim SY, Kim YR, Woo SY, Sung SH, Kim HS, Jung SC, Jo I, Park JW. Tonsil-derived mesenchymal stem cells alleviate concanavalin A-induced acute liver injury. Exp Cell Res. 2014;326(1):143–154. doi: 10.1016/j.yexcr.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 19.Park YS, Hwang S, Jin YM, Yu Y, Jung SA, Jung SC, Ryu KH, Kim HS, Jo I. CCN1 secreted by tonsil-derived mesenchymal stem cells promotes endothelial cell angiogenesis via integrin alphav beta3 and AMPK. J Cell Physiol. 2015;230(1):140–149. doi: 10.1002/jcp.24690. [DOI] [PubMed] [Google Scholar]
- 20.Owings MF, Kozak LJ. Ambulatory and inpatient procedures in the United States. Vital Health Stat 13. 1996;1998(139):1–119. [PubMed] [Google Scholar]
- 21.Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg. 2010;19(1):116–120. doi: 10.1016/j.jse.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 22.Wagner W, Ho AD, Zenke M. Different facets of aging in human mesenchymal stem cells. Tissue Eng Part B Rev. 2010;16(4):445–453. doi: 10.1089/ten.teb.2009.0825. [DOI] [PubMed] [Google Scholar]
- 23.Zaim M, Karaman S, Cetin G, Isik S. Donor age and long-term culture affect differentiation and proliferation of human bone marrow mesenchymal stem cells. Ann Hematol. 2012;91(8):1175–1186. doi: 10.1007/s00277-012-1438-x. [DOI] [PubMed] [Google Scholar]
- 24.Flaherty P, Davis RW. Robust optimization of biological protocols. Technometrics. 2015;57(2):234–244. doi: 10.1080/00401706.2014.915890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendes LF, Tam WL, Chai YC, Geris L, Luyten FP, Roberts SJ. Combinatorial analysis of growth factors reveals the contribution of bone morphogenetic proteins to chondrogenic differentiation of human periosteal cells. Tissue Eng Part C Methods. 2016;22(5):473–486. doi: 10.1089/ten.tec.2015.0436. [DOI] [PubMed] [Google Scholar]
- 26.Mandenius CF, Brundin A. Bioprocess optimization using design-of-experiments methodology. Biotechnol Prog. 2008;24(6):1191–1203. doi: 10.1002/btpr.67. [DOI] [PubMed] [Google Scholar]
- 27.Farhat YM, Al-Maliki AA, Chen T, Juneja SC, Schwarz EM, O'Keefe RJ, Awad HA. Gene expression analysis of the pleiotropic effects of TGF-beta1 in an in vitro model of flexor tendon healing. PLoS One. 2012;7(12):e51411. doi: 10.1371/journal.pone.0051411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Docheva D, Muller SA, Majewski M, Evans CH. Biologics for tendon repair. Adv Drug Deliv Rev. 2015;84:222–239. doi: 10.1016/j.addr.2014.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bottagisio M, Lopa S, Granata V, Talo G, Bazzocchi C, Moretti M, Lovati AB. Different combinations of growth factors for the tenogenic differentiation of bone marrow mesenchymal stem cells in monolayer culture and in fibrin-based three-dimensional constructs. Differentiation. 2017;95:44–53. doi: 10.1016/j.diff.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 30.Bai Y, Saren G, Huo W. Response surface methodology (RSM) in evaluation of the vitamin C concentrations in microwave treated milk. J Food Sci Technol. 2015;52(7):4647–4651. doi: 10.1007/s13197-014-1505-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pascucci L, Curina G, Mercati F, Marini C, Dall'Aglio C, Paternesi B, Ceccarelli P. Flow cytometric characterization of culture expanded multipotent mesenchymal stromal cells (MSCs) from horse adipose tissue: towards the definition of minimal stemness criteria. Vet Immunol Immunopathol. 2011;144(3-4):499–506. doi: 10.1016/j.vetimm.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 32.Myers R, Montgomery D. Response surface methodology: process and product optimization using designed experiments. 4. New York: John Wiley & Sons Inc; 1995. [Google Scholar]
- 33.Pryce BA, Watson SS, Murchison ND, Staverosky JA, Dunker N, Schweitzer R. Recruitment and maintenance of tendon progenitors by TGFbeta signaling are essential for tendon formation. Development. 2009;136(8):1351–1361. doi: 10.1242/dev.027342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morita Y, Watanabe S, Ju Y, Xu B. Determination of optimal cyclic uniaxial stretches for stem cell-to-tenocyte differentiation under a wide range of mechanical stretch conditions by evaluating gene expression and protein synthesis levels. Acta Bioeng Biomech. 2013;15(3):71–79. [PubMed] [Google Scholar]
- 35.Chen YJ, Huang CH, Lee IC, Lee YT, Chen MH, Young TH. Effects of cyclic mechanical stretching on the mRNA expression of tendon/ligament-related and osteoblast-specific genes in human mesenchymal stem cells. Connect Tissue Res. 2008;49(1):7–14. doi: 10.1080/03008200701818561. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.