Epidemiology
Middle East respiratory syndrome (MERS) is due to RNA betacoronavirus (MERS-CoV) infection. By February 2014, the World Health Organization (WHO) had received reports of 181 laboratory-confirmed cases in the Middle East, Europe and Northern Africa, with all having connections to the Middle East. The median age is 52 years, with male predominance (64.5 %) [1]. Severe cases deteriorate rapidly: median time from symptom onset to ICU admission is 2 days and to intubation is 4.5–6 days, with an ICU admission rate of 51.6 % [2, 3]. Mortality amongst critically ill ventilated patients is high with a 28-day mortality of 42 % and a 90-day mortality of 58 %. The median ICU stay is 30 days [2].
The apparent epidemiology may be biased by selective reporting of more severe cases and the small total number of patients makes it susceptible to distortion by individual outbreaks. For example, 23 of the 181 cases were in a single outbreak involving three healthcare facilities, including a haemodialysis unit [4], and more than half of all secondary cases have been nosocomial [5], increasing the prevalence of co-morbidity (75.8 %).
Bats [6] and camels [7] have been implicated as primary animal hosts; however, the data are not conclusive. Human to human transmission occurs with a relatively low basic reproductive number (R 0) of 0.42–1.5 [8, 9] and an incubation period of approximately 5 days [3, 10] but up to 15 days [4]. The mode of transmission is unknown, but relatively simple infection control measures effectively controlled a nosocomial outbreak [4].
Pathogenesis
In an ex vivo model MERS-CoV rapidly achieved a high viral load, infecting type I and II alveolar cells. Cell entry appears to be via proline exopeptidase (DPP4) receptors, which are expressed in lung and kidney. Histological changes include detachment of type II cells from basement membrane, disruption of alveolar tight junctions and changes consistent with apoptosis [10]. Viral nucleic acid in patients’ faeces and urine suggests direct involvement of gastrointestinal and urinary tracts [11].
Clinical features
The presentation is non-specific with fever, chills, sore throat, myalgia, arthralgia and dyspnoea. Vomiting and diarrhoea are common. Chest X-ray changes are consistent with viral pneumonitis and acute respiratory distress syndrome. Clinical suspicion, therefore, depends on vigilance and, for the present time, on a history of travel to the Middle East or contact with a patient with respiratory disease and an appropriate travel history [11].
The prevalence of organ failure is difficult to determine owing to reporting of limited ICU data and possible duplicate reporting of cases [2, 4]. However, almost all ICU admissions required mechanical ventilation [2–4, 11].
A recent case series reported 11 critically ill patients with confirmed MERS and one with probable MERS [2]. All required invasive mechanical ventilation. The median (range) P/F ratio on day 1 was 88 (76–413). Six patients required high frequency oscillation, nitric oxide or prone ventilation with four requiring a combination. Median duration of ventilation was 16 days. Five received non-invasive ventilation but all progressed to invasive ventilation, in keeping with other reports [4, 11, 12].
Acute kidney injury was common, with 7/12 critically ill patients requiring renal replacement therapy [2], consistent with other reports [11, 12]. Shock developed in 11/12 patients and appeared to be moderately severe [2].
Investigations
Routine investigations are neither specific nor sensitive. Lymphopenia and thrombocytopaenia occur in about one-third of patients, but approximately 10 % have lymphocytosis. Lactate dehydrogenase is raised in about half and hepatic transaminases in 10–15 % [3].
Lower respiratory tract specimens (preferably, due to higher viral load) and oropharyngeal and nasopharyngeal samples should be obtained [11]. Viral shedding may vary with time and repeated sampling is recommended for patients with high suspicion of MERS-CoV infection, even if initial results are negative [11] or other organisms are identified [2]. Blood, urine and stool specimens tested by real-time reverse-transcription polymerase chain reaction for MERS-CoV RNA targets, along with conjunctival swabs and cerebral spinal fluid if conjunctivitis or encephalitis are suspected.
Treatment
There is no effective disease-specific treatment or vaccine. Early ribavirin and interferon reduced severity of respiratory symptoms, radiology, inflammatory markers and viral load in rhesus macaque monkeys but was ineffective in humans with MERS and ARDS. However this may be due to late administration and severity of disease [13]. There is no evidence of benefit from high dose steroid [1] and SARS data indicate a significant risk of harm [14]. A management algorithm is given in Fig. 1.
Fig. 1.
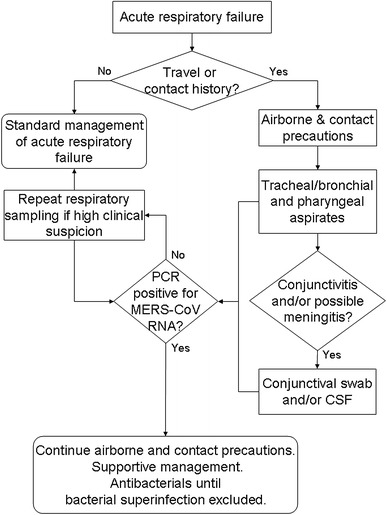
Algorithm for the isolation, investigation and management of patients who may have MERS
Implications for intensive care
Currently, the epidemic or pandemic risk appears to low. The estimated R 0 (the number of secondary infections generated by a primary infection in a susceptible population) ranges from 0.42 to 1.5. If this number is less than 1, then transmission is guaranteed to fade away. If greater than 1, there is a risk of an epidemic; but if it is only a little over 1 (i.e. 1–1.5), then transmission may fade away anyway [15]. However, there are a number of caveats. Firstly, R 0 is difficult to estimate [15]. Secondly, coronaviruses rapidly adapt to new hosts and in the process may become more infectious. Thirdly, the existence of mild, perhaps unidentified, cases makes infection control measures less likely to be effective. Approximately 60 % of MERS cases may have been undiagnosed [8]. Fourthly, a significant epidemic will pose a major challenge to intensive care, owing to the prolonged duration of mechanical ventilation and high requirement for renal replacement therapy. Non-invasive ventilation does not appear to be useful, except possibly to delay intubation, and may increase disease transmission and risk undue delay in intubation: four patients who received CPAP suffered six cardiac arrests [4].
As the mode of transmission is unknown implement airborne and contact precautions until proved unnecessary [11]. Personal protective equipment against airborne transmission includes a fit-tested FFP2 (or equivalent) face mask. Fit testing is time-consuming and should be carried out in advance of hospital admission of a patient with MERS as the delay between onset of symptoms and ICU admission [2] is very short. Visiting without full personal protective equipment has been associated with nosocomial transmission [11] and visitors should also be fit-tested.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- 1.The WHO MERS-CoV Research Group (2013) State of knowledge and data gaps of Middle East respiratory syndrome coronavirus (MERS-CoV) in humans. PLoS Curr 5. pii: ecurrents.outbreaks.0bf719e352e7478f8ad85fa30127ddb8 [DOI] [PMC free article] [PubMed]
- 2.Arabi YM, Arifi AA, Balkhy HH, Najm H, Aldawood AS, Ghabashi A, Hawa H, Alothman A, Khaldi A, Al Raly B (2014) Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med 160(6):389–397 [DOI] [PubMed]
- 3.Assiri A, Al Tawfiq JA, Al Rabeeah AA, Al Rabiah FA, Al Hajjar S, Al Barrak A, Flemban H, Al Nassir WN, Balkhy HH, Al Hakeem RF, Makhdoom HQ, Zumla AI, Memish ZA. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13:752–761. doi: 10.1016/S1473-3099(13)70204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DAT, Alabdullatif ZN, Assad M, Almulhim A, Makhdoom H, Madani H, Alhakeem R, Al Tawfiq JA, Cotten M, Watson SJ, Kellam P, Zumla AI, Memish ZA. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med. 2013;369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO (2014) Middle East respiratory syndrome coronavirus (MERS-CoV) summary and literature update—as of 20 January 2014. http://www.who.int/csr/disease/coronavirus_infections/archive_updates/en/. Accessed 5 Mar 2014
- 6.Memish ZA, Mishra N, Olival KJ, Fagbo SF, Kapoor V, Epstein JH, Alhakeem R, Durosinloun A, Al Asmari M, Islam A, Kapoor A, Briese T, Daszak P, Al Rabeeah AA, Lipkin WI. Middle East respiratory syndrome coronavirus in bats, Saudi Arabia. Emerg Infect Dis. 2013;19:1819–1823. doi: 10.3201/eid1911.131172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chu DKW, Poon LLM, Gomaa MM, Shehata MM, Perera RAPM, Abu Zeid D, El Rifay AS, Siu LY, Guan Y, Webby RJ, Ali MA, Peiris M, Kayali G (2014) MERS coronaviruses in dromedary camels, Egypt. Emerg Infect Dis. doi:10.3201/eid2006.140299 [DOI] [PMC free article] [PubMed]
- 8.Cauchemez S, Fraser C, Van Kerkhove MD, Donnelly CA, Riley S, Rambaut A, Enouf V, van der Werf S, Ferguson NM. Middle East respiratory syndrome coronavirus: quantification of the extent of the epidemic, surveillance biases, and transmissibility. Lancet Infect Dis. 2014;14:50–56. doi: 10.1016/S1473-3099(13)70304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Breban R, Riou J, Fontanet A. Interhuman transmissibility of Middle East respiratory syndrome coronavirus: estimation of pandemic risk. Lancet. 2013;382:694–699. doi: 10.1016/S0140-6736(13)61492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hocke AC, Becher A, Knepper J, Peter A, Holland G, Tönnies M, Bauer TT, Schneider P, Neudecker J, Muth D, Wendtner CM, Rückert JC, Drosten C, Gruber AD, Laue M, Suttorp N, Hippenstiel S, Wolff T. Emerging human Middle East respiratory syndrome coronavirus causes widespread infection and alveolar damage in human lungs. Am J Respir Crit Care Med. 2013;188:882–886. doi: 10.1164/rccm.201305-0954LE. [DOI] [PubMed] [Google Scholar]
- 11.Gomersall CD, Joynt GM. Middle East respiratory syndrome: new disease, old lessons. Lancet. 2013;381(9885):2229–2230. doi: 10.1016/S0140-6736(13)61412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drosten C, Seilmaier M, Corman VM, Hartmann W, Scheible G, Sack S, Guggemos W, Kallies R, Muth D, Junglen S, Muller MA, Haas W, Guberina H, Rohnisch T, Schmid-Wendtner M, Aldabbagh S, Dittmer U, Gold H, Graf P, Bonin F, Rambaut A, Wendtner CM. Clinical features and virological analysis of a case of Middle East respiratory syndrome coronavirus infection. Lancet Infect Dis. 2013;13:745–751. doi: 10.1016/S1473-3099(13)70154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al Tawfiq JA, Momattin H, Dib J, Memish ZA. Ribavirin and interferon therapy in patients infected with the Middle East respiratory syndrome coronavirus: an observational study. Int J Infect Dis. 2014;20:42–46. doi: 10.1016/j.ijid.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Griffith JF, Antonio GE, Kumta SM, Hui DSC, Wong JKT, Joynt GM, Wu AKL, Cheung AYK, Chiu KH, Chan KM, Leung PC, Ahuja AT. Osteonecrosis of hip and knee in patients with severe acute respiratory syndrome treated with steroids. Radiology. 2005;235:168–175. doi: 10.1148/radiol.2351040100. [DOI] [PubMed] [Google Scholar]
- 15.Bauch CT, Oraby T. Assessing the pandemic potential of MERS-CoV. Lancet. 1924;382:662–664. doi: 10.1016/S0140-6736(13)61504-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


