Abstract
Background
Infection with COVID-19 is currently rare in children.
Objective
To describe chest CT findings in children with COVID-19.
Materials and methods
We studied children at a large tertiary-care hospital in China, during the period from 28 January 2019 to 8 February 2020, who had positive reverse transcriptase polymerase chain reaction (RT-PCR) for COVID-19. We recorded findings at any chest CT performed in the included children, along with core clinical observations.
Results
We included five children from 10 months to 6 years of age (mean 3.4 years). All had had at least one CT scan after admission. Three of these five had CT abnormality on the first CT scan (at 2 days, 4 days and 9 days, respectively, after onset of symptoms) in the form of patchy ground-glass opacities; all normalised during treatment.
Conclusion
Compared to reports in adults, we found similar but more modest lung abnormalities at CT in our small paediatric cohort.
Keywords: Child, Computed tomography, Coronavirus, COVID-19, Pneumonia, Viral
Introduction
On 31 December 2019, an “unknown viral pneumonia” was first reported in Wuhan, China; it was initially named the 2019 novel coronavirus (2019-nCoV) [1, 2]. On 11 February 2020, the International Committee on Taxonomy of Viruses referred to a new coronavirus capable of infecting humans as SARS-CoV-2 [3]. On the same day, the World Health Organization announced that the official name of the disease caused by this virus is COVID-19 [4]. As of 4 March 2020, there were 93,094 confirmed cases of COVID-19 in 77 countries, with 80,422 in China [5]. According to recently published literature, similar to previously reported coronavirus infections, the typical radiographic image of pulmonary involvement in COVID-19 is parenchymal destruction expressed as ground-glass opacities and consolidation [6]. It has been reported that the susceptible population to the virus is mainly older adults with low immunity, and there have been few reports of paediatric patients [7]. Our objective was to present preliminary findings of abnormalities at chest CT in children with proven COVID-19.
Materials and methods
The Fifth Affiliated Hospital of Sun Yat-sen University is a large-scale third-level comprehensive hospital integrating medical treatment, teaching and scientific research. It is also the only directly affiliated hospital of Sun Yat-sen University on the west bank of the Pearl River estuary. The hospital has 2,680 faculty members. It is the only treatment unit for COVID-19 in Zhuhai City, Guangdong Province. The hospital has 50 paediatric beds. About 1 million people are served by the institution, and in 2019 it had 4,203 paediatric admissions and 88,808 paediatric outpatient appointments.
We identified children who presented to the institution and were initially suspected to have COVID-19 infection during the period 28 January 2020 to 8 February 2020. Children who tested positive on a reverse transcriptase polymerase chain reaction test for COVID-19 were included in this study. We recorded the available clinical history, laboratory findings and any CT imaging in these children. We obtained informed consent from patients and our ethics committee approved this study.
Results
Five children were evaluated. Four tested positive on the first RT-PCR, and one tested positive on the sixth test. None of the children had a chest radiograph. All had a non-enhanced chest CT after admission. Among the five, three initially had abnormal lung CT with fairly modest patchy ground-glass opacities, all three with normal chest CT at follow-up (Figs. 1, 2 and 3). A summary of presentation, clinical course and imaging finding is given in Table 1.
Fig. 1.
Axial non-enhanced chest CT in a boy age 1 year 5 months (Patient 1 in Table 1). a Four days after admission there is patchy ground-glass opacification (arrowheads) of the right upper lobe. b Five days subsequently, during antiviral treatment, the appearances have normalised
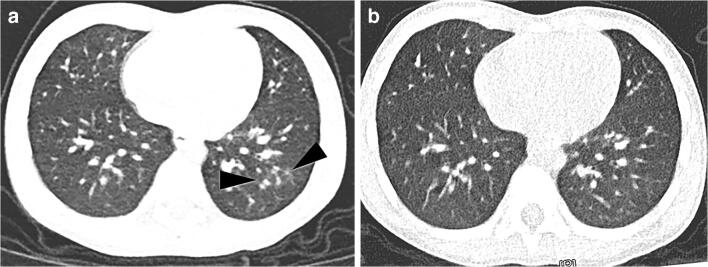
Fig. 2.
Axial non-enhanced chest CT in a 4-year-old boy (Patient 4 in Table 1). a Two days after admission there is patchy ground-glass opacification (arrowheads) of the left lower lobe. b Five days subsequently, during symptomatic and supportive treatment, the appearances have normalised
Fig. 3.
Axial non-enhanced chest CT in a 3-year-old boy (Patient 3 in Table 1). a Nine days after onset of symptoms, there is patchy ground-glass opacification (arrowheads) in the left lower lobe. b Seven days subsequently, during antiviral treatment, the appearances have normalised
Table 1.
Patient demographics, treatment and outcomes
| Patient | Age/gender | Presenting history | RT-PCR positive | CRP at presentation, mg/L (normal reference values 0–3) |
White blood cells, ×109/L (normal reference values 4.5–11) |
Initial chest CT | Treatment | Follow-up chest CT | Length of hospital stay | Outcomea | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Days from admission or onset of symptoms to scan | Findings | Days after initial CT | Findings | |||||||||
| 1 | 1 y 5 m/M | Asymptomatic, grandmother positive RT-PCR | 6th test | 9.4 | 9.2 | 4 | Patchy ground-glass opacities | Antiviral, anti-infective therapy, immunoglobulin therapy, interferon, Lianhua qingwen granules | 5 | Normal | Remains in hospital for observation; 24 days at time of writing | |
| 2 | 10 m/F | Asymptomatic, parents and grandparents positive RT-PCR | 1st test | 0.9 | 14.8 | 2 | Normal | Montelukast sodium chewable tablets, immunoglobulin therapy | Not performed | 14 days | Discharged home | |
| 3 | 3 y/M | Runny nose, cough, sputum, sore throat, fever after 3 days; father positive RT-PCR | 1st test | 0.7 | 15.0 | 9 | Patchy ground- glass opacities | Antiviral, anti-infective therapy, immunoglobulin therapy | 7 | Normal | 12 days | Discharged home |
| 4 | 4 y/M | Asymptomatic, father positive RT-PCR | 1st test | 0.2 | 6.6 | 2 | Patchy ground- glass opacities | Montelukast sodium chewable tablets, immunoglobulin therapy | 5 | Normal | 13 days | Discharged home |
| 5 | 6 y/M | Asymptomatic, travelled from high-endemic area (Wuhan) | 1st test | 0.6 | 5.3 | 3 | Normal | Interferon, Montelukast sodium chewable tablets, immunoglobulin therapy | Not performed | Remains in hospital for observation; 13 days at time of writing | ||
CRP C-reactive protein, CT computed tomography, F female, M male, m months, RT-PCR reverse transcriptase polymerase chain reaction test for COVID-19, y years
aRecovery defined as afebrile, improved respiratory symptoms, normalised chest CT, and two consecutive (24-h interval) RT-PCR tests negative
Discussion
Two children with confirmed COVID-19 infection had no sign of abnormality at chest CT. The remaining three showed characteristic but very modest radiologic abnormality before treatment in the form of patchy ground-glass opacification. The imaging changes disappeared during treatment.
Based on current diagnostic criteria, laboratory tests (such as swab tests) have become the standard and formative assessment for the diagnosis of COVID-19 infection. However, CT can be diagnostically helpful because current laboratory tests are time-consuming, sometimes return false-negative results, and do not always keep up with the needs of a growing number of infected people. Previous radiologic studies have shown that adults with COVID-19 infection have CT features of ground-glass opacities and consolidation, typically with peripheral distribution, and bilateral multifocal lower-lobe predominance [8]. Our observations were similar, but in our small cohort the CT findings were very modest.
Conclusion
Our preliminary observations in a small cohort of children with COVID-19 infection demonstrated rather moderate lung abnormality at CT with peripheral ground-glass lesions, similar to those seen in adults with COVID-19.
Compliance with ethical standards
Conflicts of interest
None
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wei Li and Huaqian Cui contributed equally to this work.
References
- 1.World Health Organization (2020) Coronavirus disease (COVID-19) outbreak. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 15 Feb 2020
- 2.World Health Organization (2020) Novel coronavirus — China. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. Accessed 15 Feb 2020
- 3.International Committee on Taxonomy Viruses (2020) Naming the 2019 coronavirus. https://talk.ictvonline.org/. Accessed 15 Feb 2020
- 4.World Health Organization (2020) Novel coronavirus (2019-nCoV) situation report – 22. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_2. Accessed 15 Feb 2020
- 5.World Health Organization (2020) Novel coronavirus (COVID-19) situation. https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd. Accessed 4 March 2020
- 6.Chung M, Bernheim A, Mei XY et al (2020) CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology. 10.1148/radiol.2020200230. Accessed 20 Feb 2020 [DOI] [PMC free article] [PubMed]
- 7.Xie XZ, Zhong Z, Zhao W et al (2020) Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 10.1148/radiol.2020200343. Accessed 20 Feb 2020 [DOI] [PMC free article] [PubMed]
- 8.Pan YY, Guan HX, Zhou SC et al (2020) Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 10.1007/s00330-020-06731-x. Accessed 20 Feb 2020 [DOI] [PMC free article] [PubMed]