Abstract
Purpose
In this prospective, multicenter, 14-day inception cohort study, we investigated the epidemiology, patterns of infections, and outcome in patients admitted to the intensive care unit (ICU) as a result of severe acute respiratory infections (SARIs).
Methods
All patients admitted to one of 206 participating ICUs during two study weeks, one in November 2013 and the other in January 2014, were screened. SARI was defined as possible, probable, or microbiologically confirmed respiratory tract infection with recent onset dyspnea and/or fever. The primary outcome parameter was in-hospital mortality within 60 days of admission to the ICU.
Results
Among the 5550 patients admitted during the study periods, 663 (11.9 %) had SARI. On admission to the ICU, Gram-positive and Gram-negative bacteria were found in 29.6 and 26.2 % of SARI patients but rarely atypical bacteria (1.0 %); viruses were present in 7.7 % of patients. Organ failure occurred in 74.7 % of patients in the ICU, mostly respiratory (53.8 %), cardiovascular (44.5 %), and renal (44.6 %). ICU and in-hospital mortality rates in patients with SARI were 20.2 and 27.2 %, respectively. In multivariable analysis, older age, greater severity scores at ICU admission, and hematologic malignancy or liver disease were independently associated with an increased risk of in-hospital death, whereas influenza vaccination prior to ICU admission and adequate antibiotic administration on ICU admission were associated with a lower risk.
Conclusions
Admission to the ICU for SARI is common and associated with high morbidity and mortality rates. We identified several risk factors for in-hospital death that may be useful for risk stratification in these patients.
Electronic supplementary material
The online version of this article (doi:10.1007/s00134-015-4206-2) contains supplementary material, which is available to authorized users.
Keywords: Severe acute respiratory infections, Pneumonia, Outcome, Intensive care
Introduction
Recent outbreaks of severe acute respiratory syndrome (SARS) and H1N1 influenza infection [1–4] have stimulated an interest in the surveillance of patients with severe acute respiratory infection (SARI), defined by the World Health Organization as an acute respiratory illness of recent onset (within 7 days) that includes fever (≥38 °C), cough, and dyspnea requiring overnight hospitalization [5]. Whereas this definition of SARI may prove practical for surveillance systems, it provides little information for intensive care physicians regarding the nature of infections, the spectrum of severity, or the diagnostic and treatment strategies used for the subset of these patients that ultimately requires intensive care unit (ICU) admission. Indeed, only a subset of the patients with SARI will require ICU admission for oxygen therapy or mechanical ventilation; a smaller subset will develop acute respiratory distress syndrome and sepsis and an even smaller proportion will require adjunctive treatments [6–8].
Obtaining accurate information on the epidemiology of critically ill patients with SARI and how these patients are currently diagnosed and treated should help intensive care practitioners to understand the factors associated with progression from acute respiratory infection to more severe critical illness. Such information may also help identify high-risk populations and guide healthcare providers in resource allocation. It is also required to identify patients for future interventional studies and provide a framework to facilitate a rapid response of the ICU community to emerging epidemics.
We conducted a prospective, observational, inception cohort study to investigate the epidemiology and microbiological profiles of ICU-SARI, to document commonly used treatment and monitoring strategies, to measure current outcomes, and to identify risk factors for poor outcome in these patients.
Methods
The Intensive Care Global Study on Severe Acute Respiratory Infection (IC-GLOSSARI) study group was an initiative of the Trials Group of the European Society of Intensive Care Medicine (ESICM-TG). Participation was entirely voluntary, with no financial incentive. Institutional review board approval was obtained by the participating institutions according to local ethical regulations. Informed consent was not required because of the observational and anonymous nature of the data collection. A steering committee was nominated by the ESICM-TG and was responsible for the scientific conduct and consistency of the project. A list of contributing centers is provided in the “Appendix” and the electronic supplementary material (file ESM1).
Study design
The study was performed over 4 weeks, from 3 to 17 November 2013 and from 13 to 26 January 2014. Each center included patients for two 1-week periods, one in November and the other in January. These dates were arbitrarily chosen to capture the expected peaks of admissions due to SARI. The same centers participated in both periods. All adult (≥18 years) patients admitted to the participating ICUs during the study period (2 weeks per center) were screened. Patients admitted to the ICU due to SARI, defined as possible, probable, or microbiologically confirmed respiratory tract infection together with recent onset (within 7 days prior to ICU admission) dyspnea and/or fever (≥38 °C), were included in the study. Patients were excluded if they (1) were less than 18 years of age; (2) had had symptoms for more than 7 days; (3) were receiving invasive mechanical ventilation prior to admission for any reason other than general anesthesia for surgical procedures; and (4) had previously been included in the study during the same study period. As a result of the lack of data from similar studies on this specific population, it was not possible to estimate the sample size prior to inclusion. The study was purely observational and there was no study protocol for patient diagnosis or therapy. Patients were followed up for 60 days after admission to the ICU for in-hospital mortality.
Definitions
Infection was defined according to the definitions of the International Sepsis Forum (Table E1) [9]. Organ failure was defined as a sequential organ failure assessment (SOFA) score >2 for the organ in question. Hospital-acquired SARI was defined as the development of SARI 48 h or more after hospital admission [10]. The definition of healthcare-related infections is provided in Table E1 [10]. Patients were classified as having community-acquired SARI if they did not fit the criteria for healthcare-related or hospital-acquired SARI.
Antibiotic therapy was considered adequate if the results of microbiology confirmed in vitro sensitivity and/or if clinical improvement occurred with no need to change or escalate the antibiotic regimen within 7 days of the onset of therapy.
Data collection
Data were collected in individual centers on paper case record forms (CRFs) and were then transcribed by local investigators into a secure Internet-based platform. A minimal data set was recorded for all adult patients admitted to the participating ICUs during the two study weeks. This included the type of admission (surgical or not), use of mechanical ventilation on admission to the ICU and during the ICU stay, the ICU length of stay, and the ICU mortality. In patients with SARI, data collection on admission included demographic data, comorbid diseases, and the presenting signs and symptoms. Clinical and laboratory data to calculate the SAPS II score [11] were recorded as the worst values within 24 h after admission. Microbiologic and clinical infections were recorded daily as were the antibiotics administered. Organ function was evaluated daily using the SOFA score [12]. The daily data collection was performed for 28 days following admission to the ICU or until ICU discharge or death.
Data management and quality control
Detailed instructions were available for all participants before starting data collection and throughout the study period. Plausibility checks were performed for each variable and between variables. Data were further reviewed by the primary investigator (YS) for plausibility and availability of outcome parameters, and any doubts were clarified with the center in question. Any file with more than 20 % missing data was excluded from the study. The reliability of data collection was further analyzed using Kappa statistics on a randomly selected 2 % of the collected comorbidity and mortality data. Discordance was clarified through direct contact with the investigators and corrected in the final database. The Kappa coefficient ranged from 0.84 to 1.00 denoting very good agreement between collected data and the randomly recollected sample.
For single missing values of the SOFA score, the mean value of the results on either side of the absent result was imputed. When first or last values were missing, the nearest value was carried backward or forward, respectively. When more than one consecutive result was missing, it was considered as a missing value in the analysis. Missing data represented 6.7 % of the collected data and 1.5 % were replaced.
Outcome parameters
The primary outcome parameter in patients with SARI was in-hospital mortality within 60 days of admission to the ICU. Secondary outcome parameters included death in the ICU, ICU and hospital lengths of stay, and organ failure as assessed by the SOFA score.
Statistical analyses
Data were analyzed using IBM® SPSS® Statistics software, version 22 for Windows, R software, version 3.2.2 (CRAN project), and MLwiN v.2.28. The Kolmogorov–Smirnov test was used to verify the normality assumption of continuous variables. Difference testing between groups was performed using analysis of variance (ANOVA), Student’s t test, Mann–Whitney test, Chi square test, or Fisher’s exact test, as appropriate.
To identify the independent risk factors for in-hospital death in patients with SARI we used a three-level multilevel technique with in-hospital outcome as the dependent variable (Table E2). The explanatory variables considered in the model were
Individual-level factors: age, sex, ethnicity, SAPS II and SOFA scores on admission to the ICU, source of admission, comorbidities, mode of acquisition of SARI, prior vaccination against pneumococcus or influenza, antibiotic administration, adequacy and timing (in days) of the antibiotic therapy initiated on admission to the ICU, need for mechanical ventilation during the ICU stay, number of days in the hospital prior to ICU admission, and microorganisms retrieved at any time during the ICU stay
Hospital-level factors: type of hospital, level of care, number of staffed ICU beds
Country-level factors: for this level, a random intercept model was considered
Data are given as means with standard deviation, medians, and interquartile ranges (IQR), or numbers and percentages (n, %). All statistics were two-tailed and a p value less than 0.05 was considered as significant.
Results
Characteristics of study cohort
A total of 206 ICUs from 42 countries contributed to the study, mostly located in Western Europe (66.5 %, n = 137) (Table E3). During the study periods, 5550 patients were admitted to these units (Fig. 1). A total of 663 (11.9 %) patients were admitted because of SARI; 364 in the first and 299 in the second inclusion periods. The epidemiology of SARI in the different geographic regions is presented in Table E4.
Fig. 1.
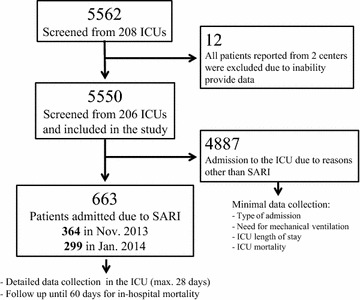
Flowchart of recruitment to and inclusion in the study. ICU intensive care unit, SARI severe acute respiratory infection
SARI admissions were more likely to be non-surgical and to require mechanical ventilation on admission to the ICU and at any time during the ICU stay than those who were admitted for reasons other than SARI (Table E5).
The characteristics of patients with SARI on admission to the ICU are presented in Table 1; these admissions were most commonly community-acquired (68.8 %). The most common comorbidities in the these patients were systemic hypertension (51.3 %) and chronic obstructive pulmonary disease (COPD, 31.1 %) (Table E6).
Table 1.
Characteristics of patients with severe acute respiratory infections (SARI) on admission to the ICU, stratified according to the inclusion periods
| All patients | Inclusion period | p value | ||
|---|---|---|---|---|
| November 2013 | January 2014 | |||
| N | 663 | 364 | 299 | |
| Age, years, mean ± SD | 63.9 ± 16 | 64.5 ± 15.9 | 63.1 ± 16.2 | 0.226 |
| Male, n (%) | 386 (58.7) | 216 (59.8) | 170 (57.2) | 0.501 |
| Healthcare worker, n (%) | 11 (1.7) | 5 (1.4) | 6 (2.0) | 0.798 |
| Ethnicity, n (%) | ||||
| White/Caucasian | 441 (67.7) | 246 (69.5) | 195 (71.3) | 0.392 |
| Asian | 49 (7.5) | 22 (6.2) | 27 (9.1) | |
| Latin American | 46 (6.9) | 24 (6.8) | 22 (7.4) | |
| South Asiana | 41 (6.2) | 23 (6.5) | 18 (6.1) | |
| Arab | 34 (5.2) | 19 (4.9) | 15 (5.1) | |
| Black | 24 (3.6) | 15 (4.2) | 9 (3.0) | |
| Others | 16 (2.5) | 5 (1.4) | 11 (3.7) | |
| Source of admission, n (%) | ||||
| Community | 194 (29.4) | 108 (29.9) | 36 (22.1) | 0.847 |
| Hospital ward | 183 (27.8) | 99 (27.4) | 64 (39.3) | |
| Emergency room | 165 (25.0) | 93 (25.8) | 34 (20.9) | |
| Other hospital | 58 (8.8) | 33 (9.1) | 25 (8.4) | |
| Long-term facility | 24 (3.6) | 10 (2.8) | 14 (4.7) | |
| Other ICU | 13 (2.0) | 2 (0.6) | 11 (3.7) | |
| Step-down/-up | 14 (2.1) | 10 (2.8) | 4 (1.3) | |
| Others | 8 (1.2) | 6 (1.7) | 2 (0.7) | |
| Severity scores | ||||
| SAPS II, mean ± SD | 50.4 ± 19.0 | 49.3 ± 18.2 | 51.7 ± 19.8 | 0.178 |
| SOFA score, median (IQR) | 5 (2–9) | 5 (2–9) | 5 (2–9) | 0.727 |
| Mode of acquisition, n (%) | ||||
| Community-acquired | 452 (68.2) | 246 (68.3) | 206 (69.4) | 0.059 |
| Healthcare-related | 76 (11.5) | 37 (10.3) | 39 (13.1) | |
| Nosocomial-acquired | 129 (19.5) | 77 (21.4) | 39 (17.5) | |
| Mechanical ventilation on admission to the ICU | ||||
| Invasive | 385 (58.1) | 208 (57.1) | 177 (59.2) | 0.594 |
| Non-invasive | 46 (6.9) | 28 (7.7) | 18 (6.0) | 0.399 |
| Influenza vaccine, n (%) | 67 (10.2) | 43 (11.9) | 24 (8.1) | 0.751 |
| Pneumococcal vaccine, n (%) | 49 (7.4) | 31 (8.6) | 18 (6.0) | 0.692 |
Missing values n = 2–12 (max 1.8 %), valid percentages are presented after exclusion of missing values
ICU intensive care unit, SAPS simplified acute physiology score, IQR interquartile range, SOFA sequential organ failure assessment score
aIndia, Pakistan, and Sri Lanka
Clinical manifestations, patterns of infection, and antimicrobial therapy in SARI patients
The first symptoms occurred at a median of 2 days (IQR 0–4) before admission to the ICU, most commonly dyspnea (92.8 %), cough (75.3 %), and fever (64.7 %). Less common symptoms included headache (18.3 %), nausea and vomiting (17.4 %), and diarrhea (7.3 %). A history of recent foreign travel was reported by 27 patients (4.1 %).
Prior antimicrobial therapy was initiated in 378 patients (57.0 %) (Table E7) and in 611 patients (96.5 %) a new antimicrobial agent was started on admission to the ICU, mostly empirically (88.6 %). The initial antimicrobial therapy was adequate in 80.6 % of cases. The antimicrobial regimen was changed in 209 patients (31.5 %) because of clinical deterioration (45.2 %), culture results (34.8 %), or in the context of de-escalation of therapy (19.9 %). Concomitant antimicrobials were used in 130 patients (19.6) for indications other than treatment of SARI.
Specimens were obtained for microbiological examination in 596 (89.9) patients and were positive for microorganisms in 62.7 % of patients (Table E8). Microbiological investigation on admission to the ICU revealed predominantly Gram-positive (29.6 %) or Gram-negative bacteria (26.2 %) but rarely atypical bacteria (1.0 %); 7.7 % of the microorganisms isolated on admission were viruses (Table 2). Overall, the most frequently isolated Gram-positive bacteria was Streptococcus pneumoniae (12.7 %); the most frequently isolated Gram-negative microorganism was Pseudomonas aeruginosa (14.4 %). Viruses were isolated in 13.7 % of positive cultures, atypical bacteria in 2.9 %, and fungi in 27.6 % of cases. In patients with hospital-acquired SARI, Gram-negative microorganisms (33.3 vs. 26.5 %, p = 0.002) and fungi (29.5 vs. 12.8 %, p = 0.001) were more frequently and viral infections less frequently (3.9 vs. 9.9 %, p = 0.006) isolated than in patients with community-acquired SARI (Fig. 2).
Table 2.
Isolated microorganisms (out of 416 patients with positive results)
| On admission to the ICU | After admission | Any time in the ICUa | |
|---|---|---|---|
| Gram-positive, n (%) | 123 (29.6) | 123 (29.6) | 205 (49.3) |
| Streptococcus pneumoniae | 41 (9.9) | 23 (5.5) | 53 (12.7) |
| Staphylococcus aureus sensitive to methicillin | 23 (5.5) | 27 (6.5) | 42 (10.1) |
| Staph. coag. neg. sensitive to methicillin | 15 (3.6) | 34 (8.2) | 45 (10.8) |
| S. aureus resistant to methicillin | 14 (3.4) | 13 (3.1) | 26 (6.3) |
| Staph. coag. neg. resistant to methicillin | 7 (1.7) | 14 (3.4) | 20 (4.8) |
| Streptococcus A, B, C, G group | 7 (1.7) | 5 (1.2) | 12 (2.9) |
| Streptococcus, others | 14 (3.3) | 26 (6.3) | 36 (8.6) |
| Other Gram-positive | 10 (2.4) | 16 (3.8) | 26 (6.3) |
| Gram-negative, n (%) | 109 (26.2) | 127 (30.5) | 201 (48.3) |
| Pseudomonas aeruginosa | 29 (7.0) | 40 (9.6) | 60 (14.4) |
| Klebsiella species | 27 (6.5) | 36 (8.7) | 57 (13.7) |
| Escherichia coli | 23 (5.5) | 26 (6.3) | 43 (10.3) |
| Acinetobacter species | 15 (3.6) | 25 (6.0) | 34 (8.2) |
| Enterobacter species | 10 (2.4) | 11 (2.6) | 21 (5.0) |
| Proteus species | 5 (1.2) | 7 (1.7) | 10 (2.4) |
| Citrobacter species | 5 (1.2) | 2 (0.5) | 6 (1.4) |
| Serratia species | 1 (0.2) | 5 (1.2) | 6 (1.4) |
| Stenotrophomonas maltophilia | 3 (0.7) | 5 (1.2) | 7 (1.7) |
| Haemophilus species | 7 (1.7) | 11 (2.6) | 18 (4.3) |
| Other Gram-negative | 4 (1.0 | 7 (1.7) | 11 (2.6) |
| Anaerobic, n (%) | 4 (1.0) | 3 (0.7) | 7 (1.7) |
| Clostridium species | 2 (0.5) | 3 (0.7) | 5 (1.2) |
| Bacteroides | 1 (0.2) | 0 (0.0) | 1 (0.2) |
| Anaerobe, others | 1 (0.2) | 0 (0.0) | 1 (0.2) |
| Atypical bacteria, (%) | 4 (1.0) | 8 (1.9) | 12 (2.9) |
| Mycobacteria | 1 (0.2) | 1 (0.2) | 2 (0.5) |
| Chlamydia species | 0 (0.0) | 3 (0.7) | 3 (0.7) |
| Mycoplasma | 0 (0.0) | 4 (1.0) | 4 (1.0) |
| Legionella pneumophila | 3 (0.7) | 2 (0.5) | 5 (1.2) |
| Fungi, n (%) | 45 (10.8) | 83 (20.0) | 115 (27.6) |
| Candida albicans | 36 (8.7) | 61 (14.7) | 87 (20.9) |
| Candida non-albicans | 7 (1.7) | 22 (5.3) | 28 (6.7) |
| Aspergillus species | 3 (0.7) | 7 (1.7) | 9 (2.2) |
| Other | 2 (0.5) | 9 (2.2) | 11 (2.6) |
| Viruses, n (%) | 32 (7.7) | 27 (6.5) | 57 (13.7) |
| Influenza A | 23 (5.5) | 16 (3.8) | 38 (9.1) |
| Influenza B | 3 (0.7) | 0 (0.0) | 3 (0.7) |
| HSV I or II | 0 (0.0) | 1 (0.2) | 1 (0.2) |
| CMV | 2 (0.5) | 5 (1.2) | 6 (1.4) |
| Other | 5 (1.2) | 6 (1.4) | 11 (2.6) |
| Parasites, n (%) | 2 (0.5) | 3 (0.7) | 5 (1.2) |
CMV cytomegalovirus, HSV herpes simplex virus
aMicroorganisms isolated both on admission to the ICU and during the ICU stay are counted once
Fig. 2.
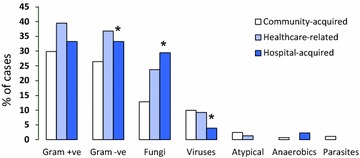
Microbiological isolates according to mode of acquisition of severe acute respiratory infection (SARI). *p < 0.05
Morbidity and mortality
Organ failure was present on admission to the ICU in 427 (64.4 %) of the patients with SARI and occurred during the entire ICU stay in 495 (74.7 %). Respiratory, cardiovascular, and renal failures were the most common organ failures (Table 3). The ICU and hospital mortality rates were 20.2 and 27.2 %, respectively.
Table 3.
Morbidity and mortality in patients with SARI (n = 663)
| Organ failure on admission to the ICU, n (%)a | |
| Respiratory | 205 (30.9) |
| Cardiovascular | 217 (32.7) |
| Renal | 180 (27.1) |
| CNS | 138 (20.8) |
| Hematologic | 54 (8.1) |
| Hepatic | 29 (4.4) |
| Organ failure at any time in the ICU, n (%)a | |
| Respiratory | 357 (53.8) |
| Cardiovascular | 295 (44.5) |
| Renal | 296 (44.6) |
| CNS | 216 (32.6) |
| Hematologic | 133 (20.1) |
| Hepatic | 50 (7.5) |
| Mortality rates, n (%) | |
| ICU | 123 (20.2) |
| In-hospital | 163 (27.2) |
| Length of stay, days, median (IQR) | |
| ICU | 5 (2–12) |
| Hospital | 12 (7–23) |
| Limitation of therapy in-hospital, n (%) | |
| DNR | 72 (11.9) |
| WH/WD | 57 (9.4) |
Missing values: 53 and 64 for ICU and hospital mortality, respectively. Valid percentages are displayed after exclusion of the missing values
CNS central nervous system, DNR do not resuscitate order, ICU intensive care unit, LOS length of stay, WD withdrawal of life-sustaining therapy (vasopressors, mechanical ventilation, and renal replacement therapy), WH withholding of life-sustaining measures
aDefined as a SOFA score >2 for the corresponding organ
The overall ICU mortality in all patients admitted to the contributing centers (n = 5550) was 13.1 % and the median ICU stay was 3 (IQR 2–8) days. Patients with SARI had higher ICU mortality (20.2 vs. 12.2 %, p < 0.001) and longer ICU lengths of stay [5 (2–12) vs. 3 (2–8)] days, p < 0.001) than those without SARI (Table E5).
Survivors were younger, more likely to be female, less likely to be admitted to the ICU from a hospital ward, had lower severity scores on admission to the ICU, and had a lower incidence of organ failure during the ICU stay (Tables E9, E10) than non-survivors. Survivors were more likely to have received pneumococcal or influenza vaccines than non-survivors. Arrhythmias, chronic renal failure, cancer, asthma, hematologic malignancies, organ or bone marrow transplantation, liver disease, immunosuppression, or chemotherapy prior to ICU admission were more frequent in non-survivors than in survivors (Table E7). The most common primary causes of in-hospital death were multiorgan failure (43.6 %) and pneumonia (31.9 %) (Table E11).
In multivariable analysis, older age, greater severity scores on admission to the ICU, hematologic malignancy, and liver disease were independently associated with an increased risk of in-hospital death. Influenza vaccination prior to ICU admission, and adequate antibiotic administration on admission to the ICU were associated with a lower risk of in-hospital death (Table E2).
Discussion
The main findings of our study were that (1) SARI was a common cause of admission to the ICU and was associated with considerable morbidity and high mortality rates; (2) these infections were predominantly due to Gram-positive or Gram-negative bacteria and rarely due to atypical bacteria or viruses; and (3) older age, greater severity scores, and comorbid conditions were independently associated with an increased risk of in-hospital death in these patients, whereas prior influenza vaccination and adequate initial antibiotic administration were associated with a lower risk.
Repeated outbreaks of SARI-related epidemics represent a major healthcare problem [1–4]. Several studies have investigated the epidemiology and clinical characteristics of SARI, with a special emphasis on viral etiology [13–17] or on the subset of patients admitted to the ICU with severe community-acquired pneumonia [17–22]. To the best of our knowledge, our study is the first to investigate this issue in a large prospective, multinational cohort of critically ill patients with SARI, providing a global view of this condition worldwide.
One in ten patients with SARI was treated empirically without any microbiologic sampling. Increased awareness of sepsis should be expected to improve compliance with early microbiologic sampling [23]. Nevertheless, the low index of suspicion in the absence of an ongoing epidemic may explain the relatively low rate of investigations aimed at detecting a viral etiology. In agreement with previous large epidemiologic studies in ICU patients with infections [24–26], pathogenic microorganisms were identified in only 62.7 % of patients. Lack of testing for all possible microorganisms during microbiological investigations, the relatively high rates of prior antibiotic administration with possible interference with culture results, and inappropriate sampling techniques may hinder microorganism identification.
Despite the relatively small number of microbiological investigations performed, antimicrobial agents were used generously in our cohort. Interestingly, antiviral and antifungal agents were initiated without microbiological evidence of these microorganisms in 6.9 and 4.0 % of cases, respectively. The relatively high incidence of comorbid conditions in our cohort, especially those related to immunosuppression, and the high predominance of life-threatening organ failure in these patients may explain the high use of antimicrobial agents.
The most commonly identified microorganisms were Gram-positive and Gram-negative bacteria. The reported microorganisms may have included, however, some non-pathogenic organisms that are not responsible for SARI. Interestingly, atypical microorganisms were less frequently identified. This observation raises questions regarding the frequent empirical use of macrolides in these patients. However, macrolides have been reported to have additional benefits in patients with community-acquired pneumonia, irrespective of their antimicrobial effects [27]. Moreover, diagnosis of infections with atypical bacteria is a considerable challenge, such that the occurrence of these infections may be underestimated [28].
Community-acquired infections were common in our cohort, explaining the frequent occurrence of infections with S. pneumoniae. The patterns of microbiologic isolates in our study may be useful to guide empirical antimicrobial therapy in patients with ICU-SARI. Although fungi were frequently isolated, only a small proportion of these patients received antifungal agents. This finding supports the common perception that fungal etiologies may not be relevant in all critically ill patients with respiratory infections [29].
Our data underscore the poor prognosis of critically ill patients with SARI. These patients had considerably higher mortality rates and longer lengths of stay compared to patients without SARI. The in-hospital mortality rate in our cohort was similar to rates reported in patients with severe community-acquired pneumonia in previous studies [17, 20, 30]. This can be explained by the frequent occurrence of organ failure in these patients.
We identified several risk factors for in-hospital mortality in the current cohort. These patterns may be useful in identifying patients at risk of poor prognosis. In agreement with the results of a meta-analysis of 70 large observational studies including 21,338 patients with sepsis [31], we found that adequate initial antibiotic administration was protective in terms of low risk of in-hospital death. This supports the early rigorous empiric use of wide-spectrum antibiotics in these patients, pending the results of microbiological investigations. Nonetheless, since the definition of appropriate antibiotic administration in the current study was based on both positive microbiologic isolates and clinical improvement, we cannot exclude a possible bias in patients who were judged only on the basis of clinical improvement.
Interestingly, prior seasonal influenza vaccination was independently associated with a favorable in-hospital outcome. Ortiz and collaborators [32] estimated that about 28,000 adults are hospitalized for influenza-associated critical illness in the USA annually. A recent bias-adjusted meta-analysis [33] confirmed that influenza vaccine was effective in preventing hospitalization from influenza and/or pneumonia and all-cause mortality in community-dwelling elderly. However, the evidence to support risk factors for influenza-related complications is still low and adequately powered studies are needed to address this issue [34, 35].
The study had several limitations. First, participation was voluntary and was concentrated in some countries in Western Europe, so that the results in this report may not be extrapolated to all ICU patients worldwide. Second, regional and seasonal differences may also occur and cannot be captured from our data. Third, some of the reported microorganisms may have represented respiratory colonization rather than infection. Fourth, the definitions of infection were not based on only the presence of microorganisms and we did not differentiate between possible and probable clinical infections. Nonetheless, defining infection according to the isolation of a pathogenic microorganism may also be subject to a certain bias because of possible interference from prior antibiotic administration, availability and the diagnostic performance of the serologic tests, and local practice concerning microbiologic investigations. Fifth, our data may not be extrapolated to all hospitalized patients with SARI. Finally, the study was purely observational and we did not apply standard protocols for diagnosis and therapy in patients with SARI; however, our aim was to report current practice in these patients.
Conclusions
SARI is a common cause of admission to the ICU and has associated high morbidity and mortality rates. Our data describe the current patterns of infections and therapy of this serious healthcare problem. This information may be particularly useful in resource allocation and risk stratification for clinical and research purposes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We would like to thank Dr. Hassane Nijimi (Free University of Brussels), the study statistician, for his efforts in data monitoring and analysis and Dr. Karen Pickett for editorial assistance with the manuscript.
Appendix 1. Alphabetical list of participating centers by region & country
Study coordinator
The trials group of the European Society of Intensive Care (ESICM): (G Francois)
Europe
Austria: General Hospital, Braunau (J Auer, G Schatzl); Krankenhaus Oberwart, Oberwart (K Mach, H Gruber)
Belgium: Ziekenhuis Oost-Limburg, Genk (E Schreurs, M Vander Laenen); Universitair Ziekenhuis, Leuven (H Ceunen, J Wauters); CHU Saint-Pierre, Brussels (P Deschamps); Cliniques Universitaires Saint-Luc UCL, Brussels (D Castanares); CHU Brugmann, Brussels (D Debels, C Pierrakos); Erasme University Hospital, Brussels (JL Vincent, F Taccone (national coordinator))
Czech Republic: University Hospital Motol, Prague (T Vymazal)
Croatia: University Hospital Centre Zagreb, Zagreb (I Gornik, A Vujiaklija Brajkovic)
Denmark: Holbaek Sygehus, Holbaek (R Medici); Rigshopitalet, Copenhagen (J Nielsen); Glostrup Sygehus, Glostrup (A Bendtsen, H Siegel)
Finland: Meilahti Hospital, Helsinki (T Suonsyrjä)
France: CHU Nord, Marseille (S Hraech), Hôpital Cochin, Paris (J-D Chiche, F Daviaux); CHRU Strasbourg-Hôpital de Hautepierre, Strasbourg (M Guillot, V Castelain); CHRU Nancy- Hôpital Brabois- Réanimation et soins continus chirurgicaux, Vandoeuvre-Les-Nancy (R-R Losser), CHRU Nancy- Hôpital Brabois- Réanimation médicale, Vandoeuvre-Les-Nancy (E Novy); Hôpital Bichat, Paris (J-F Timsit (national coordinator), L Bouadma); Groupe Hospitalier Paris Saint-Joseph, Paris (B Misset, F Philippart); Centre Hospitalier Dr Schaffner, Lens (J Mallat); CHU Amiens, Amiens (E Zogheib, M Miclo) Hôpital Bicêtre, Le Kremlin-Bicêtre Paris (J-L Teboul, N Anguel); CHU Saint-Etienne, Saint-Etienne (M Darmon); Hôpital Tenon, Paris (T Pham); CH Mulhouse-Hôpital Emile Muller, Mulhouse (G Barberet); Hôpital Victor Dupouy, Argenteuil (G Plantefeve); Hôpital Edouard Herriot, Hospices Civils de Lyon, Lyon (B Floccard)
Georgia: Georgian Critical Care Medicine Institute, Tbilissi (Z Kheladze)
Germany: Universitätsklinikum Jena, Jena (K Reinhart (national coordinator), Y Sakr, F Bloos); Klinikum Weiden, Weiden in der Oberpfalz (A Faltlhauser); Klinikum Luedenscheid, Luedenscheid (T Helmes); University Hospital Frankfurt, Frankfurt am ( K Zacharowski, P Meybohm); Klinikum Saarbrücken, Saarbrücken (K Schwarzkopf); Klinikum Nürnberg, Dept. of Emergency and Critical Care Medicine, Nurenberg (M Christ, M Baumgaertel); Klinikum Nürnberg, Nephrologische Intensivstation BU13, Nurenberg (S John, J Nentwich); Universitätsmedizin-Charité, Berlin (M Deja, A Goldmann); Diakoniekrankenhaus Friederikenstift, Hannover (A Gottschalk, F Honig); University Medical Center Freiburg, Freiburg (B Siepe, U Goebel); Vivantes Humboldt-Klinikum, Berlin ( J Lehmke, S Behrens); Oberschwabenklinik, Krankenhaus St. Elisabeth, Ravensburg (K Fiedler); Universitätsmedizin Mainz, Mainz (I Sagoschen); University Hospital, Tübingen (R Riessen, M Haap); University Hospital, Leipzig (Ph Simon,U Kaisers); Vivantes Klinikum Spandau, Berlin (S Behrens, M Niesen); Klinikum Augsburg, Augsburg (U Jaschinski); Universitätsklinikum des Saarlandes, Homburg (S Hoersch, A Jung); Robert-Bosch-Krankenhaus, Stuttgart (S Allgaeuer); Maria Hilf, Mönchengladbach (H Haake); Klinik Hennigsdorf der Oberhavel Kliniken, Hennigsdorf (A Lange)
Greece: Hippokrateion General Hospital, Athens (M Papanikolaou, M Balla); AHEPA University Hospital, Thessaloniki (M Giannakou, I Soultati); University Hospital of Ioannina, Ioannina (G Nikos, V Koulouras); Lamia General Hospital, Lamia (G Kyriazopoulos, D Gkika); General Hospital O Agios Dimitrios, Thessaloniki (G Vlachogianni, K Psaroulis); Hippokratio Hospital, Thessaloniki (E Mouloudi, E Massa)
Ireland: St Vincents University Hospital, Dublin (A Nichol, E Meany); Limerick University Hospital, Limerick (C Motherway)
Italy: San Gerardo Hospital, Monza (G Bellani); Pinetagrande Private Hospital, Castelvolturno (V Pota, V Schiavone); University Hospital of Modena, Modena (M Girardis, S Busani); Azienda Ospedaliera Desenzano, Desenzano (N Petrucci, R Di Pasquale); Ospedale Sandro Pertini, Rome (P Mazzini); IRCCS San Martino-IST, Genova (A Molin, G Pellerano); Arispedale Sant’Anna Hospital, Ferrara (C Volta, S Spadaro); Azienda Ospedaliero Universitaria Pisana, Pisa (F Guarracino); Fondazione IRCCS Ca’ Granda - Ospedale Maggiore Policlinico, Milan (M Savioli); Santa Maria degli Angeli Hospital, Pordenone (T Pellis, N Chinellato); Ospedale Ceccarini, Riccione (A Gatta, F Cecchini); Policlinico P. Giaccone, Palermo (S.M. Raineri, A Cortegiani)
Lithuania: Vilnius University Hospital Santariskiu Clinics, Vilnius (G Kekstas, V Karosas)
Macedonia: Special Hospital for surgery Fillip II, Skopje (T Anguseva, Z Mitrev)
Netherlands: Tjongerschans, Heerenveen (O Beck, N Cimic); Atrium Medisch Centrum Parkstad, Heerlen (G Janssen, L Bormans); Medical Center Leeuwarden, Leeuwarden (M Kuiper, K Koopmans); Spaarneziekenhuis, Hoofddorp (S Den Boer, M de Groot); Medical Centre Haaglanden, The Hague, P Dennesen); Reinier de Graaf Ziekenhuis, Delft (J van den Bosch); Slotervaartziekenhuis, Amsterdam (G Kluge)
Poland: Child Jesus Clinical Hospital of the Medical University of Warsaw, Warsaw (M Mikaszewska-Sokolewicz, T Lazowski); Szpital Praski, Warsaw (M Chruscikowski); Wroclaw University Hospital, Wroclaw (J Machon, B Adamik, A Kübler); Barlicki Clinical Hospital, Lodz (A Wieczorek)
Portugal: Hospital de S. José, Lisbon (S Afonso, R Matos (national coordinator)); Centro Hospitalar do Médio Tejo, Abrantes (N Catorze, A Araujo); Hospital de Santa Maria EPE (CHLN), Lisbon (Z Costa, A Pais-de-Lacerda); Centro Hospitalar Tondela-Viseu, Viseu (I Martins); Hospital Sao Francisco Xavier – CHLO, Lisbon (R Cardiga, L Fernandes); Hospital Pr Doutor Fernando Fonseca EPE, Amadora (I Serra, A Martinho)
Romania: Fundeni Clinical Institute, Bucharest (D Tomescu, M Popescu, E Scarlatescu); Institute of Pneumology, Bucharest (R Stoica, A Macri); Emergency Institute for Cardiovascular Diseases Prof. Dr. C.C. Iliescu, Bucharest (D Filipescu (national coordinator))
Slovenia: General Hospital Izola, Izola (E Rupnik); University Clinic of Respiratory and Allergic Diseases, Golnik (V Tomic, F Sifrer)
Spain: Hospital de Gran Canaria Dr Negrín, Las Palmas de Gran Canaria (J Sole Violan, J.M; Ferrer Agüero); Complejo Hospitalario de Navarra, UCI B, Pamplona (J Izura); Clinica Universidad de Navarra, UCI Adultos, Pamplona (P Monedero); Hospital de Torrejón, Torrejón de Ardoz (C Muños de Cabo); Hospital Clínico Universitario de Valencia, Cuidados intensivos quirurgicos, Valencia (G Aguilar, F.J. Belda); Hospital Clínico Universitario de Valencia, Cuidados Intensivos, Valencia (J Blanquer, E Nives Carbonell); Hospital Universitari Bellvitge, L’Hospitalet de Llobregat-Barcelona (J-C Lopez-Delgado); Hospital Regional Carlos Haya, Málaga (C Aragon, C Joya); Hospital Quirón Sagrado Corazón, Seville (C Ortiz-Leyba); Complejo Hospitalario Universitario de Ferrol, Ferrol (C.J Fernandez Gonzalez); Hospital Universitario Virgen de la Victoria, Málaga (M-V de la Torre-Prados, A Puerto-Morlan); Hospital Universitario Miguel Servet, Zaragoza (P Araujo Aguilar, J.I Tomás Marsilla); Hospital de la Santa Creu I Sant Pau, Barcelona (P Vera Aratcoz, A Olmo); Mutua Terrassa University Hospital, Terrasa (R Ferrer Roca (national coordinator)); Hospital General de Vic, Vic-Barcelona (R.M Catalan); Hospital General Universitario Gregorio Marañon, Madrid (P Garcia Olivares); Hospital de Mataró, Mataró (A Albis); Clinico San Carlos, Madrid
(M Alvarez); Hospital General Universitario de Albacete, Albacete (V Corcoles Gonzalez, J. M Gutierrez Rubio); Hospital Clínico Universitario Lozano Blesa, Zaragoza (R Montoiro Allue); Hospital Infanta Cristina, Badajoz (J Rubio Mateo-Sidron)
United Kingdom: Bronglais General Hospital, Aberystwyth (M Hobrok); St George’s Hospital, London (M Cecconi (national coordinator), N Di Tomasso); Barts Health NHS Trust, Whipps Cross Hospital, Leytonstone (A Raj); Royal Glamorgan Hospital, Llantrisant (T Szakmany, L Srinivasa); Alexandra Hospital, Redditch (S Mathew); Craigavon Area Hospital, Portadown (A Ferguson); The Great Western Hospital, Swindon (M Blahut-Zugaj, M Watters); Western Infirmary, Glasgow (S Henderson, M Sim); Wexham Park Hospital, Slough( P Csabi); Antrim Area Hospital, Antrim (O O’Neill, C Nutt); West Suffolk Hospital, Bury St Edmunds (S Humphreys, K Bhowmick); Altnagelvin Hospital, Derry (A Donnelly, S O’Kane); Ipswich Hospital NHS Trust, Ipswich (M Garfield); Barnet General Hospital, Barnet (R Jha, N Unni); Imperial College Healthcare NHS Trust-Charing Cross Hospital, London (A Gordon, F Rubulotta); Rotherham General Hospital, Rotherham (K Ravi, G Lunch); Chase Farm Hospital, Royal Free London Foundation Trust, Enfield (F Franco); Kent & Canterbury Hospital, Canterbury (D Higgs, G Strandvik); Pilgrim Hospital, Boston (A Jonas); King’s College Hospital, London (Ph Hopkins, T Hurst); Queen’s Hospital, Romford (A Bellini, O Balogun); St Thomas Hospital, London (R Srinivasan, M Ostermann); University Hospital of South Manchester, Manchester (P Alexander, K McCalman); Guy’s Hospital, London (J Bedford, M Fulop); Luton and Dunstable Hospital, Luton (G Brescia); John Radcliffe Hospital, Oxford (J Strachan, J Meyer); Imperial College Healthcare NHS Trust-St Mary’s Hospital, London (M Stotz), Imperial College Healthcare NHS Trust-Hammersmith Hospital, London (S Brett)
Middle East
Iran: Nemazee Hospital (AACCRC), Shiraz (F Zand, R Nikandish); Masih Daneshvari Hospital (NRITLD), Teheran (S Hashemian, H Jamaati);
Qatar: Hamad General Hospital, Doha (A.S. Alsheikhly)
Saudi Arabia: Prince Sultan Military Medical City (PSMMC), Riyadh (G Almekhlafi, M Albarrak); King Faisal Specialist Hospital, Riyadh (A Maghrabi, N Salahuddin); King Fahad Hospital, Baha (T Aisa)
Turkey: Atasehir Memorial Hospital, Istanbul (H. K Atalan); Erciyes Universitesi Tip Fakultesi, Kayseri (M Sungur);
United Arab Emirates: Sheikh Khalifa Medical City, Abu Dhabi (M Hegazi)
North America
United States: Mayo Clinic, Saint Mary’s Hospital, Rochester (P Bauer); Memorial Medical Center, Springfield (S Mukkera); Santa Barbara Cottage Hospital, Santa Barbara (J Fried, M Barger); John H Stroger Hospital of Cook County, Chicago (R Gueret)
South America
Argentina: Sanatorio Parque, Rosario (C Gonzalez, C Lovesio); Hospital Dr Julio C. Perrando, Resistencia (Ch Dellera, D Barrios)
Brazil: Hospital Universitario Lauro Wanderley, João Pessoa (C Leite Mendes, P Gottardo); Hospital Unimed, Vitória (E Caser, C Santos); UDI Hospital, São Luís (A Carvalho); Hospital Moinhos de Vento, Porto Alegre (C Teixeira)
Chile: Hospital del Trabajador, Santiago (W Samaniego, S Whittle)
Colombia: Clinica Universitaria Colombia, Bogota (D Molano, A Rojas); Clinica Medellín, Medellin (K Guerra)
Ecuador: Hospital Militar, Quito (B Villamagua); Clinica La Merced, Quito (E Salgado-Yepez); Hospital de los Valles, Quito (D Morocho, N Remache-Vargas)
Mexico: Instituto Nacional de Cancerologia, Mexico (S Ñamendys-Silva); Hospital civil de Guadalajara-Hospital Juan I Menchaca, Guadalajara (D Rodriguez); Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico (G Dominguez, G Barraza); Hospital Regional Leon ISSSTE, Mexico (E. Bermudez-Aceves); Hospital de Especialidades Antonio Fraga Mouret-Centro Medico Nacional La Raza IMSS, Mexico (L.A Sanchez-Hurtado, J. A Baltazar-Torres)
Peru: Hospital Nacional Dos de Mayo, Lima (R Quispe Sierra, R Ovalle Olmos); Hospital Regional Honorio Delgado, Arequipa (C Chavez)
Venezuela: Hospital Central Dr. Miguel Pérez Carreño, Caracas (I von Osten) ;
Oceania
Australia: Canberra Hospital, Canberra (C Van Haren (national coordinator)); Townsville Hospital, Douglas (N Smalley); Concord Hospital, Concord-West Sydney (M Kol, H Wong); St Vincent’s Hospital, Fitzroy-Melbourne (R Smith)
East and South-East Asia
China: Wuhan Central Hospital, Wuhan (L Yu, X Wu); The First People’s Hospital, Kunming (L Chao); Qilu Hospital of Shandong University, Jinan (Q Zhai, D Wu); Tenth People’s Hospital, Tongji University School of Medicine, Shanghai (X Zhang, X Jing);
Philippines: Chong Hua Hospital, Cebu (R Bigornia, Y Ikeda-Maquiling); The Medical City, Pasig (J Robles, J. E. Palo)
Vietnam: Bachmai Hospital, Hanoi (T Nguyen, C Dao)
South Asia
India: Sanjeevan Hospital, Pune (S Dixit), Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow (M Gurjar); Care Hospital, Hyderabad (P Reddy); Bombay Hospital Institute of Medical Sciences, Mumbai Maharashtra (A Pravin (national coordinator)); Hinduja Hospital, Mumbai (S Simran); Apollo Hospitals, Chennai (N Ramakrishnan); Manipal Hospital, Bangalore (R Shetty); Breach Candy Medical Research Centre, Mumbai (F Udwadia)
Pakistan: Shifa International Hospital, Islamabad (M Faraz)
Sri Lanka: Sri Jayewardenepura General Hospital, Nugegoda (K Indraratna, J Rajasinhe)
Compliance with ethical standards
Conflicts of interest
The authors declare that they do not have any conflict of interest in relation to the subject of this manuscript.
Funding
The study was supported by an unrestricted grant from the European Society of Intensive Care Medicine (ESICM), Rue Belliard, 19, 1040 Brussels, Belgium.
Footnotes
Take-home message: Admission to the ICU for SARI is common and associated with high morbidity and mortality rates. We identified several risk factors for in-hospital death that may be useful for risk stratification in these patients.
On behalf of the IC-GLOSSARI Investigators and the Trials Group of the European Society of Intensive Care (ESICM), Rue Belliard, 19, 1040 Brussels, Belgium. Email: research@esicm.org.
A complete list of IC-GLOSSARI investigators is provided in the “Appendix” and in the electronic supplementary material (file ESM2).
References
- 1.Webb SA, Seppelt IM. Pandemic (H1N1) 2009 influenza (“swine flu”) in Australian and New Zealand intensive care. Crit Care Resusc. 2009;11:170–172. [PubMed] [Google Scholar]
- 2.Rello J, Rodriguez A, Ibanez P, Socias L, Cebrian J, Marques A, Guerrero J, Ruiz-Santana S, Marquez E, Del Nogal-Saez F, Alvarez-Lerma F, Martinez S, Ferrer M, Avellanas M, Granada R, Maravi-Poma E, Albert P, Sierra R, Vidaur L, Ortiz P, Prieto DPI, Galvan B, Leon-Gil C, H1N1 SEMICYUC Working Group Intensive care adult patients with severe respiratory failure caused by Influenza A (H1N1)v in Spain. Crit Care. 2009;13:R148. doi: 10.1186/cc8044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, Stelfox T, Bagshaw S, Choong K, Lamontagne F, Turgeon AF, Lapinsky S, Ahern SP, Smith O, Siddiqui F, Jouvet P, Khwaja K, McIntyre L, Menon K, Hutchison J, Hornstein D, Joffe A, Lauzier F, Singh J, Karachi T, Wiebe K, Olafson K, Ramsey C, Sharma S, Dodek P, Meade M, Hall R, Fowler RA. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA. 2009;302:1872–1879. doi: 10.1001/jama.2009.1496. [DOI] [PubMed] [Google Scholar]
- 4.Martin-Loeches I, Diaz E, Vidaur L, Torres A, Laborda C, Granada R, Bonastre J, Martin M, Insausti J, Arenzana A, Guerrero JE, Navarrete I, Bermejo-Martin J, Suarez D, Rodriguez A. Pandemic and post-pandemic influenza A (H1N1) infection in critically ill patients. Crit Care. 2011;15:R286. doi: 10.1186/cc10573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Regional Office for Europe (2011) WHO Regional Office for Europe Guidance for Sentinal Influeza Surveillance in Humans. http://www.euro.who.int/__data/assets/pdf_file/0020/90443/E92738.pdf?ua=1. Accessed 1 Jan 2015
- 6.Fowler RA, Lapinsky SE, Hallett D, Detsky AS, Sibbald WJ, Slutsky AS, Stewart TE. Critically ill patients with severe acute respiratory syndrome. JAMA. 2003;290:367–373. doi: 10.1001/jama.290.3.367. [DOI] [PubMed] [Google Scholar]
- 7.Lew TW, Kwek TK, Tai D, Earnest A, Loo S, Singh K, Kwan KM, Chan Y, Yim CF, Bek SL, Kor AC, Yap WS, Chelliah YR, Lai YC, Goh SK. Acute respiratory distress syndrome in critically ill patients with severe acute respiratory syndrome. JAMA. 2003;290:374–380. doi: 10.1001/jama.290.3.374. [DOI] [PubMed] [Google Scholar]
- 8.Manocha S, Walley KR, Russell JA. Severe acute respiratory distress syndrome (SARS): a critical care perspective. Crit Care Med. 2003;31:2684–2692. doi: 10.1097/01.CCM.0000091929.51288.5F. [DOI] [PubMed] [Google Scholar]
- 9.Calandra T, Cohen J. The International Sepsis Forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med. 2005;33:1538–1548. doi: 10.1097/01.CCM.0000168253.91200.83. [DOI] [PubMed] [Google Scholar]
- 10.American Thoracic Society. Infectious Diseases Society of America Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416. doi: 10.1164/rccm.200405-644ST. [DOI] [PubMed] [Google Scholar]
- 11.Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–2963. doi: 10.1001/jama.1993.03510240069035. [DOI] [PubMed] [Google Scholar]
- 12.Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 13.Poulakou G, Perez M, Rello J. Severe acute respiratory infections in the postpandemic era of H1N1. Curr Opin Crit Care. 2012;18:441–450. doi: 10.1097/MCC.0b013e32835605f2. [DOI] [PubMed] [Google Scholar]
- 14.Jain S, Benoit SR, Skarbinski J, Bramley AM, Finelli L. Influenza-associated pneumonia among hospitalized patients with 2009 pandemic influenza A (H1N1) virus—United States, 2009. Clin Infect Dis. 2012;54:1221–1229. doi: 10.1093/cid/cis197. [DOI] [PubMed] [Google Scholar]
- 15.Martin-Loeches I, Sanchez-Corral A, Diaz E, Granada RM, Zaragoza R, Villavicencio C, Albaya A, Cerda E, Catalan RM, Luque P, Paredes A, Navarrete I, Rello J, Rodriguez A. Community-acquired respiratory coinfection in critically ill patients with pandemic 2009 influenza A(H1N1) virus. Chest. 2011;139:555–562. doi: 10.1378/chest.10-1396. [DOI] [PubMed] [Google Scholar]
- 16.Sandrock C, Stollenwerk N. Acute febrile respiratory illness in the ICU: reducing disease transmission. Chest. 2008;133:1221–1231. doi: 10.1378/chest.07-0778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bertolini G, Rossi C, Crespi D, Finazzi S, Morandotti M, Rossi S, Peta M, Langer M, Poole D. Is influenza A(H1N1) pneumonia more severe than other community-acquired pneumonias? Results of the GiViTI survey of 155 Italian ICUs. Intensive Care Med. 2011;37:1746–1755. doi: 10.1007/s00134-011-2339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cilloniz C, Ewig S, Ferrer M, Polverino E, Gabarrus A, de la Puig BJ, Mensa J, Torres A. Community-acquired polymicrobial pneumonia in the intensive care unit: aetiology and prognosis. Crit Care. 2011;15:R209. doi: 10.1186/cc10444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeong BH, Jeon EJ, Yoo H, Koh WJ, Suh GY, Chung MP, Kwon OJ, Jeon K. Comparison of severe healthcare-associated pneumonia with severe community-acquired pneumonia. Lung. 2014;192:313–320. doi: 10.1007/s00408-013-9541-x. [DOI] [PubMed] [Google Scholar]
- 20.Walden AP, Clarke GM, McKechnie S, Hutton P, Gordon AC, Rello J, Chiche JD, Stueber F, Garrard CS, Hinds CJ. Patients with community acquired pneumonia admitted to European intensive care units: an epidemiological survey of the GenOSept cohort. Crit Care. 2014;18:R58. doi: 10.1186/cc13812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mongardon N, Max A, Bougle A, Pene F, Lemiale V, Charpentier J, Cariou A, Chiche JD, Bedos JP, Mira JP. Epidemiology and outcome of severe pneumococcal pneumonia admitted to intensive care unit: a multicenter study. Crit Care. 2012;16:R155. doi: 10.1186/cc11471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Viasus D, Marinescu C, Villoslada A, Cordero E, Galvez-Acebal J, Farinas MC, Gracia-Ahufinger I, Fernandez-Navarro A, Niubo J, Ortega L, Munez-Rubio E, Romero-Gomez MP, Carratala J. Community-acquired pneumonia during the first post-pandemic influenza season: a prospective, multicentre cohort study. J Infect. 2013;67:185–193. doi: 10.1016/j.jinf.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb S, Beale RJ, Vincent JL, Moreno R. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34:344–353. doi: 10.1097/01.CCM.0000194725.48928.3A. [DOI] [PubMed] [Google Scholar]
- 25.Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302:2323–2329. doi: 10.1001/jama.2009.1754. [DOI] [PubMed] [Google Scholar]
- 26.Vincent JL, Marshall JC, Namendys-Silva SA, Francois B, Martin-Loeches I, Lipman J, Reinhart K, Antonelli M, Pickkers P, Njimi H, Jimenez E, Sakr Y. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380–386. doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
- 27.Feldman C, Anderson R. Community-acquired pneumonia: pathogenesis of acute cardiac events and potential adjunctive therapies. Chest. 2015;148:523–532. doi: 10.1378/chest.15-0484. [DOI] [PubMed] [Google Scholar]
- 28.Basarab M, Macrae MB, Curtis CM. Atypical pneumonia. Curr Opin Pulm Med. 2014;20:247–251. doi: 10.1097/MCP.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 29.Lamoth F, Alexander BD. Nonmolecular methods for the diagnosis of respiratory fungal infections. Clin Lab Med. 2014;34:315–336. doi: 10.1016/j.cll.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 30.Cavallazzi R, Wiemken T, Arnold FW, Luna CM, Bordon J, Kelley R, Feldman C, Chalmers JD, Torres A, Ramirez J. Outcomes in patients with community-acquired pneumonia admitted to the intensive care unit. Respir Med. 2015;109:743–750. doi: 10.1016/j.rmed.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 31.Paul M, Shani V, Muchtar E, Kariv G, Robenshtok E, Leibovici L. Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother. 2010;54:4851–4863. doi: 10.1128/AAC.00627-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ortiz JR, Neuzil KM, Shay DK, Rue TC, Neradilek MB, Zhou H, Seymour CW, Hooper LG, Cheng PY, Goss CH, Cooke CR. The burden of influenza-associated critical illness hospitalizations. Crit Care Med. 2014;42:2325–2332. doi: 10.1097/CCM.0000000000000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Darvishian M, Gefenaite G, Turner RM, Pechlivanoglou P, Van der Hoek W, Van den Heuvel ER, Hak E. After adjusting for bias in meta-analysis seasonal influenza vaccine remains effective in community-dwelling elderly. J Clin Epidemiol. 2014;67:734–744. doi: 10.1016/j.jclinepi.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 34.Mertz D, Kim TH, Johnstone J, Lam PP, Science M, Kuster SP, Fadel SA, Tran D, Fernandez E, Bhatnagar N, Loeb M. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ. 2013;347:f5061. doi: 10.1136/bmj.f5061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Darvishian M, Bijlsma MJ, Hak E, Van den Heuvel ER. Effectiveness of seasonal influenza vaccine in community-dwelling elderly people: a meta-analysis of test-negative design case-control studies. Lancet Infect Dis. 2014;14:1228–1239. doi: 10.1016/S1473-3099(14)70960-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


