Sir: Corticosteroid has been generally considered beneficial for patients with severe acute respiratory syndrome (SARS), but the standard treatment protocol is still uncertain [1]. We describe a SARS patient who twice experienced relapse of SARS which was complicated with shock and acute disseminated intravascular coagulopathy (DIC) during stepping down the corticosteroid dose.
A 56-year-old woman experiencing fever and progressive dyspnea visited our emergency service on the 5th day of fever. Hypoxia was noted and chest radiography showed bilateral lung infiltrates. Mechanical ventilatory support was given and she was admitted to an isolated room. Nasopharyngeal aspirates were positive for SARS-CoV RNA by RT-PCR assay and oral ribavirin (2,000 mg stat, then 1,000 mg daily for 7 days), moxifloxacin (400 mg daily), and intravenous methylprednisolone (2 mg·kg·day) were given from admission onwards (5th day of fever).
Because fever subsided and oxygenation improved, corticosteroid was tapered to oral prednisolone 0.5 mg·kg·day during the 8th to 16th day of fever (Fig. 1). Unfortunately, fever and hypoxia recurred on the 16th day of fever and intravenous methylprednisolone 2 mg·kg·day were reinstituted, with subsequent improvement in fever and hypoxia.
Fig. 1.
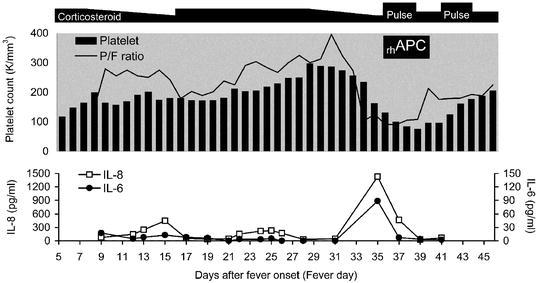
Time-course evolution of platelet count (middle panel, bar), P/F ratio (middle panel, solid line), and pro-inflammatory cytokines (bottom panel) in a SARS patient. Top panel denotes the dosage of corticosteroid. [Pulse high-dose pulse corticosteroid, rhAPC recombinant human activated protein C, P/F ratio PaO2/FiO2, IL-8 interleukin 8 (open square), IL-6 interleukin 6 (solid circle)]
The corticosteroid dose was reduced again from the 28th day of fever and the patient was weaned from ventilatory support on the 33rd day of fever. However, severe hypoxemia with profuse lung infiltrates occurred on the next day. Even under broad-spectrum empirical antibiotics (imipenem with cilastatin sodium and vancomycin), she still developed signs of multiple organ dysfunction syndrome (MODS): persistent shock, hypoxemia, and acute DIC (D-dimer 5510 ng/ml, prothrombin time (PT) 15.5 s, activated partial thromboplastin time (aPTT) 50.3 s). A surge in serum concentrations of interleukin-6 (IL-6) and interleukin-8 (IL-8) was also observed. A combination therapy of recombinant human activated protein C (rhAPC, 24 μg·kg·h continuous IV for 96 h) and pulsed methylprednisolone (500 mg daily IV for 3 days) was administered. The levels of cytokines reduced rapidly and oxygenation and, thrombocytopenia improved from the 72nd h of therapy onwards. Of particular note, coagulopathy improved within 48 h after initiating therapy and returned to normal range 48 h after therapy completion (PT 12.2 s, aPTT 30.9 s). Finally, the analysis of sputum, urine, catheter tips, blood, and serologic tests for common and atypical pathogens during these episodes were all negative. Without residual organ-system dysfunction, she was discharged from hospital 2 months later.
The most important finding of this case is that the recurrent relapses of SARS were closely associated with repeated attempts to taper the dose of corticosteroid. Although corticosteroid has been cited as an important therapy for SARS [2], some SARS patients experienced rebound of fever during step-down of corticosteroid and required subsequent rescue pulse steroid therapy [3, 4]. Cytokine overproduction has been known to induce tissue damage, acute DIC, MODS, and death [5]. In this patient, hypercytokinemia was associated with the relapse of SARS upon tapering corticosteroid. Although in this particular patient we successfully reversed acute DIC-associated MODS using a combination of pulse corticosteroid and a novel drug with immunomodulatory and anticoagulant effects, rhAPC, further controlled trials are strongly recommended to clarify the standard of care for avoiding disease relapse and associated catastrophic complications.
References
- 1.Peiris N Engl J Med. 2003;349:2431. doi: 10.1056/NEJMra032498. [DOI] [PubMed] [Google Scholar]
- 2.Nicholls Lancet. 2003;361:1773. doi: 10.1016/S0140-6736(03)13413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.So Lancet. 2003;361:1615. doi: 10.1016/S0140-6736(03)13265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ho Am J Respir Crit Care Med. 2003;168:1449. doi: 10.1164/rccm.200306-766OC. [DOI] [PubMed] [Google Scholar]
- 5.Bernard N Engl J Med. 2001;344:699. doi: 10.1056/NEJM200103083441001. [DOI] [PubMed] [Google Scholar]


