Abstract
Abstract
A series of new β-isatin aldehyde-N,N′-thiocarbohydrazone, bis-β-isatin thiocarbohydrazones, bis-β-isatin carbohydrazones was synthesized by condensation of 5-substituted isatin with thiocarbohydrazide or carbohydrazide. The chemical structures of the newly synthesized compounds were confirmed by FT-IR, 1H NMR, and mass spectral analysis. The synthesized compounds were evaluated for in vitro antiviral activity against various strains of DNA and RNA viruses, but exhibited moderate antiviral activity compared with the reference compounds. Among all the compounds 6c exhibited the highest chemoprevention activity in a two-stage mouse-skin carcinogenesis test.
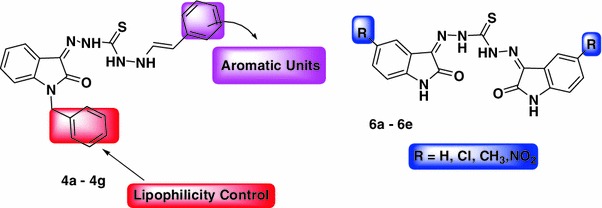
Graphical abstract
Keywords: Isatin, Thiocarbohydrazide, Carbohydrazide, Antiviral, Anti-influenza, Carcinogenesis
Introduction
Isatin is a versatile lead molecule for designing potential antiviral agents. Isatin derivatives display broad spectrum pharmacological properties, including cytotoxic (Reddy et al., 2012; Alcaide et al., 2012), antibacterial (Akhaja and Raval, 2011), antifungal (Reddy et al., 2011), antiviral (Kang et al., 2011; Bacani et al., 2011; Sin et al., 2009), anti-HIV (Bal et al., 2005), and antimalarial (Hans et al., 2011) activities. The first clinically approved antiviral agent, N-methylisatin-β-thiosemicarbazone (methisazone) was active against smallpox and vaccinia viruses (Bauer, 1985). N,N′-disubstituted thiosemicarbazone derivatives of isatin were inhibitory to HIV-1 replication (Teitz and Ronen, 1984). N-methylisatin-β-thiosemicarbazone is an inhibitor of Japanese encephalitis virus infection (Sebastain et al., 2008). The general configuration of the isatin molecule resembles that of the purines and also tryptophan and its derivatives, but there is no evidence available as to whether isatin-β-thiosemicarbazone acts as an antimetabolite to these compounds (Bauer and Sadler, 1960). Recent studies have shown that isatin could inhibit the protease, caspase, MAO and COX-2 enzymes (Medvedev et al., 2007).
Viral pathogens are responsible for many human diseases and examples of diseases caused by viruses include the common cold, smallpox, AIDS, cold sores, human herpes virus, papilloma virus, etc. (Prado-Prado et al., 2009). The worldwide market for antiviral drugs is estimated to be approximately 20 billion US dollars and is expected to grow rapidly as new therapies become available. The need for effective antiviral drugs is further emphasized by the lack of vaccines for most respiratory tract virus infections [adenovirus, rhinovirus, parainfluenza virus and respiratory syncytial virus (RSV), the widely occurring human papilloma viruses, and herpes simplex virus (HSV), varicella-zoster virus (VZV), Epstein–Barr virus, cytomegalovirus (CMV), and the vast array of hemorrhagic fever viruses (De Clercq, 2002)]. Millions of people worldwide are affected by infectious diseases caused by viruses. Further, widespread viral resistance has renewed the interest in the quest for new antiviral agents. Earlier work could clearly define the structural requirements necessary for the retention of antiviral activity by heterocyclic thiosemicarbazone in neurovaccinia infections in mice. Viral infections primarily affect the respiratory and gastrointestinal system; epithelium, mucous membranes and endothelium of skin, mouth and genitals; lymphoid tissue, liver and other organs; and the central nervous system (Bruce et al., 2007).
Recently, we have reported that β-isatin-N,N′-thiocarbohydrazone derivatives could have antimicrobial and antioxidant activity (Kiran et al., 2012a). Thiosemicarbazones were the first antiviral compounds recognized to possess broad-spectrum antiviral activity against a range of DNA and RNA viruses [Castro et al., 2011]. Earlier reports have described antiviral activity of isatin-β-thiosemicarbazone and isatin-β-semicarbohydrazone against different viral strains [Quenelle et al., 2006; Pandeya et al., 2005]. However, the biological activities of isatin-β-thiocarbohydrazone and isatin-β-carbohydrazone have not been evaluated against DNA and RNA viruses. In connection with our ongoing work on isatin (Kiran et al., 2012b), we are now reporting a simple and efficient method for the synthesis of some β-isatin-N,N′-thiocarbohydrazone (4a–g), bis-β-isatin thiocarbohydrazone, and bis-β-isatin thiocarbohydrazone derivatives (6a–e) as depicted in Schemes 1 and 2. These compounds were screened for in vitro antiviral activity and also in a two stage mouse-skin carcinogenesis test.
Scheme 1.
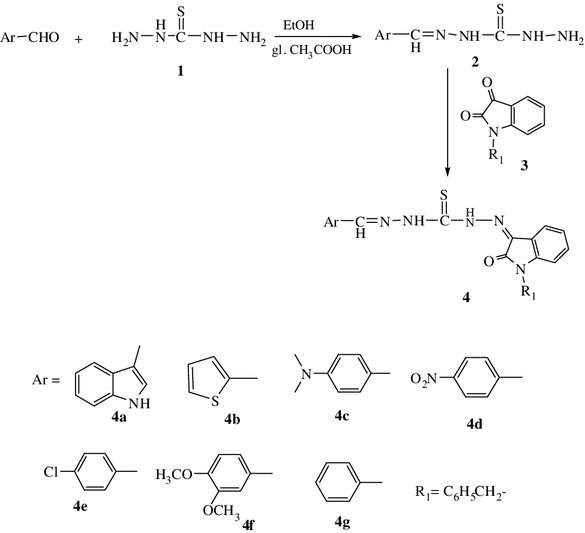
Schematic steps of β-isatin aldehyde-N,N′-thiocarbohydrazones derivatives synthesis
Scheme 2.
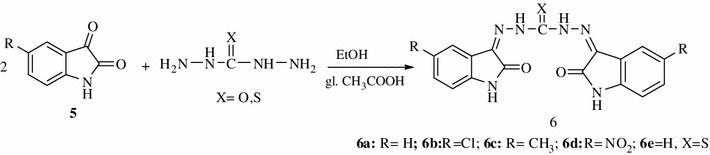
Schematic steps of Bis-isatin derivatives synthesis
Experimental
Materials and methods
Melting points (m.p.) were determined in open capillaries, using the Toshniwal melting point apparatus, expressed in °C and were uncorrected. FT-IR spectra (KBr) were recorded on a thermo Nicolet Nexus 670S series. NMR spectra were recorded on an Avance-300 MHz in DMSO-d 6 solvent using TMS as an internal standard (chemical shifts in δ, ppm). Mass spectra were obtained on a LC-MSD-Trap-SL. Reactions were monitored using thin layer chromatography (TLC) on aluminum-backed precoated silica gel 60 F254 plates (E Merck). The purity of the compounds was checked on silica gel-coated aluminum sheets by TLC. Column chromatography was performed by using Qualigen’s silica gel (60–120 mesh). All the solvents were AR grade and distilled before use. 5-Substituted isatins were purchased from Himedia (Mumbai, India). Indole-3-carboxaldehyde was obtained from E. Merck (India). All substituted aldehydes were purchased from Sd. Fine Chemicals.
General procedure
Synthesis of isatin derivatives
The synthesis of isatin derivatives was carried out using a modified Sandmeyer methodology (Henry and Blatt, 1964). N-benzyl isatin is prepared by a microwave method as reported in the literature (Shmidt et al., 2008). All the isatin derivatives exhibit same physical properties as reported in the literature.
Synthesis of thiocarbohydrazide (1)
The synthesis of thiocarbohydrazide was carried out by the Taguchi method. The physical data of the synthesized compound are comparable and show m.p 170–172 °C similar to that reported in the literature (Zhou et al., 2010).
Synthesis of monothiocarbohydrazones (2a–g)
An equimolar mixture of thiocarbohydrazide (0.01 mol), substituted aldehyde (0.01 mol), and a few drops of glacial acetic acid were taken in 30 ml of ethanol in 250 ml conical flask. The resulting mixture was heated under reflux for 1 h. Then the reaction mixture was cooled overnight and the precipitate was collected by filtration. Further it was purified by recrystallization with ethanol. The synthesized compounds were comparable with the reported literature (Mohamed et al., 1991).
Synthesis of β-isatin aldehyde-N,N′-thiocarbohydrazones (4a–g)
To a solution of monothiocarbohydrazone (2a–g, 0.01 mol) and substituted isatin (3, 0.01 mol) in ethanol, a few drops of glacial acetic acid were added to initiate the reaction. The progress of the reaction was monitored by TLC. The residue was cooled, kept overnight and the precipitate was collected by filtration. The solid was purified by column chromatography, and subsequently by recrystallization with ethanol.
Synthesis of bis-isatin derivatives (6a–e)
A mixture of thiocarbohydrazide or carbohydrazide (0.01 mol) was mixed with appropriate substituted isatin derivatives (0.02 mol) in ethanol–acetic acid (1:1). The reaction mixture was refluxed for 2 h. Then the reaction mixture was cooled, kept overnight and the precipitate was collected by filtration. The resulting solid was purified by column chromatography and subsequently by recrystallization with ethanol.
Spectral data of the synthesized compounds
3-[(1H-indol-3-ylmethylidene)amino]-1-{[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino}thiourea (4a)
IR (ν cm−1): 3226 (br, N–H, lactam), 3138, 3070 (w, C–H, Ar), 1705 (s, C=O, lactam), 1337 (s, C=S), 1538 (s, C=N), 1463 (s, C=C). 1H-NMR (DMSO-d 6) δ ppm: 14.1 (s, 1H, NH), 12.2 (s, 1H, NH), 11.7 (s, 1H, NH), 11.3 (s, 1H, NH), 8.67 (1H, =CH–), 8.47 (1H, N=CH), 7.87 (dd, J = 7.4, 1.6 Hz, 1H), 7.64–7.52 (m, 3H), 7.49–7.40 (m, 2H), 7.34 (td, J = 7.4, 1.5 Hz, 1H), 6.59 (d, J = 7.5 Hz, 1H). 13C NMR (DMSO-d 6) δ ppm: 173.9 (C=S), 162 (C=O), 143 (C=N), 110–137 (Ar–C); mass (ESI–MS): m/z 363 (M+1, 100 %), 385 (M+Na, 80 %). Elemental analysis for C18H14N6OS: calculated (%) C: 59.65; H: 3.89; N: 23.19; found: C: 59.29; H: 3.24; N: 23.45.
3-{[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino}-1-[thiophen-2-ylmethylidene)amino]thiourea (4b)
IR (ν cm−1): 3316 (N–H), 3026 (w, C–H, Ar), 1708 (s, C=O, lactam), 1368 (s, C=S), 1395 (s, C=N), 1528 (s, CH=N). 1H-NMR (DMSO-d 6) δ ppm: 14.7 (s, 1H, NH), 13.3 (s, 1H, –NH), 11.9 (s, 1H, –NH), 8.90 (s, 1H), 7.65–7.59 (m, 2H), 7.57–7.45 (m, 2H), 7.31 (dd, J = 7.5, 2.8 Hz, 1H), 7.27–7.20 (m, 1H), 6.96 (dd, J = 7.5, 1.5 Hz, 1H); mass (ESI–MS): m/z 330 (M+1, 100 %). Elemental analysis for C14H11N5OS2: calculated (%) C: 51.05; H: 3.37; N: 21.26; found: C: 51.02; H: 3.34; N: 21.18.
1-({[4-(dimethylamino)phenyl]methylidene}amino)-3-{[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino}thiourea (4c)
IR (ν cm−1): 3218 (–NH), 3016 (w, C–H, Ar), 2700 (C–H, str), 1702 (s, C=O, lactam), 1358 (s, C=S), 1528 (s, C=N), 1528 (s, CH=N). 1H-NMR (DMSO- d 6) δ ppm: 14.9 (s, 1H, –NH), 14.5 (s, 1H, –NH), 13.0 (s, 1H, –NH), 8.06 (s, 1H), 7.76 (dd, J = 7.5, 1.5 Hz, 1H), 7.61 (dd, J = 7.5, 1.7 Hz, 1H), 7.53–7.46 (m, 3H), 7.28–7.20 (m, 1H), 6.85–6.79 (m, 2H), 3.02 (s, 6H); mass (ESI–MS): m/z 367 (M+1, 100 %), 389 (M+Na, 40 %). Elemental analysis for C18H18N6OS: calculated (%) C: 59.00; H: 4.95; N: 22.93; found: C: 59.02; H: 4.86; N: 22.78.
1-{[(4-Nitrophenyl)methylidene]amino}-3-{[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino}thiourea (4d)
IR (ν cm−1): 3120 (–NH), 3006 (w, C–H, Ar), 1690 (s, C=O, lactam), 1358 (s, C=S), 1528 (s, C=N), 1528 (s, CH=N). 1H-NMR (DMSO-d 6) δ ppm: 14.2 (s, 1H,–NH), 13.6 (s, 1H, –NH), 12.0 (s, 1H, –NH), 8.06 (s, 1H), 7.64 (dd, J = 7.5, 1.5 Hz, 1H), 7.64 (dd, J = 7.5, 1.7 Hz, 1H), 7.42–7.26 (m, 3H), 7.28–7.20 (m, 1H), 6.85–6.79 (m, 2H); mass (ESI–MS): m/z 369 (M+1, 100 %), 391 (M+Na, 30 %). Elemental analysis for C16H12N6O3S: calculated (%) C: 52.17; H: 3.28; N: 22.81 found: C: 52.12; H: 3.24; N: 22.76.
1-{[(4-Chlorophenyl)methylidene]amino}-3-{[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino}thiourea (4e)
IR (ν cm−1): 3345 (N–H), 3050 (C–H, Ar), 1630 (C=O, lactam), 900–690 (Ar–H), 785 (C–Cl); 1H-NMR (DMSO- d 6) δ ppm; 14.7 (s, 1H), 13.6 (s, 1H), δ 11.2 (s, 1H), 7.93 (s, 1H), 7.85–7.79 (m, 2H), 7.68 (dd, J = 7.5, 1.6 Hz, 1H), 7.60 (dd, J = 7.4, 1.6 Hz, 1H), 7.48 (td, J = 7.4, 1.5 Hz, 3H), 7.27–7.20 (m, 1H); mass (ESI–MS): m/z 357 (M+, 100 %), 359 (M+2, 38 %). Elemental analysis for C16H12N6O3S: calculated (%) C: 53.71; H: 3.38; N: 19.57; found: C: 53.68; H: 3.42; N: 19.76.
1-{[(3,4-Dimethoxyphenyl)methylidene]amino}-3-{[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino}thiourea (4f)
IR (ν cm−1): 3348 (N–H), 3020 (C–H, Ar), 1648 (C=O), 1313 (C=S); 1H-NMR (DMSO-d 6) δ ppm; 14.7 (s, 1H), 13.1 (s, 1H), δ 10.9 (s, 1H), 7.93 (s, 1H), 7.71–7.57 (m, 4H), 7.48 (td, J = 7.5, 1.5 Hz, 1H), 7.14–7.08 (m, 2H), 3.79 (s, 6H); mass (ESI–MS): m/z 384 (M+1, 100 %). Elemental analysis for C24H21N5OS: calculated (%) C: 56.38; H, 4.47; N, 18.27; found: C: 56.34; H: 4.46; N: 18.23.
3-{[(3Z)-1-benzyl-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino}-1-[(phenylmethylidene)amino]thiourea (4g)
IR (ν cm−1): 3360 (N–H), 3050 (C–H, Ar), 1630 (C=O, lactam), 900–690 (Ar, oop); 1H-NMR (DMSO-d 6) δ ppm; 14.7 (s, 1H), 13.6 (s, 1H), δ 11.2 (s, 1H), 7.93 (s, 1H), 6.8–7.5 (Ar–H), 3.2 (s, –CH2, 2H); mass (ESI–MS): m/z 428 (M+, 100 %), 450 (M+Na, 38 %). Elemental analysis for C18H17N5O3S: calculated (%) C: 66.81; H: 4.63; N: 16.94; found: C: 66.78; H: 4.58; N: 16.78.
1,3-Bis({[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino})urea (6a)
IR (ν cm−1): 3350–3050 (NH, NH), 3070 (C–H, Ar), 1742 (s, C=O, lactam), 1608, 1472 (C=C, Ar), 1650 (C=O), 1610 (C=N). 1H-NMR (DMSO-d 6) ppm; δ 13.2 (s, 2H), 7.93 (s, 2H), 7.15–7.79 (m, 6H); mass (ESI–MS): m/z 349 (M+1, 100 %), 371 (M+Na, 52 %). Elemental analysis for C17H12N6O3: calculated (%) C:58.62; H:3.47; N:24.13; found: C: 58.58; H: 3.46; N: 24.20.
1,3-Bis({[(3Z)-5-chloro-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino})urea (6b)
IR (ν cm−1): 3250–3050 (NH, NH), 3010 (C–H, Ar), 1642 (s, C=O, lactam), 1608, 1472 (C=C, Ar), 1650 (C=O), 1610 (C=N). 1H-NMR (DMSO-d 6) ppm; δ 13.2 (s, 2H), 7.93 (s, 2H), 7.15–7.79 (m, 6H); mass (ESI–MS): m/z 417 (M+1, 100 %), 439 (M+Na, 46 %).Elemental analysis for C17H10Cl2N6O3: calculated (%) C:48.94; H:2.42;N: 20.14; found: C: 48.89; H: 2.46; N: 20.20.
1,3-Bis({[(3Z)-5-methyl-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino})urea (6c)
IR (ν cm−1) 3198 (NH), 3010 (C–H, Ar), 2980 (-CH str), 1730 (C=O), 1680 (s, C=O, lactam), 1608, 1472 (C=C, Ar), 1620 (C=N). 1H-NMR (DMSO-d 6) ppm; δ 11.2 (s, 2H), 10.2 (s, 2H), 7.15–7.79 (m, 6H) 2.2 (s, –CH3); mass (ESI–MS): m/z 377 (M+1, 100 %), 386 (M+Na, 51 %). Elemental analysis for C19H16 N6O3: calculated (%) C: 60.63; H: 4.28; N: 22.33; found: C: 60.69; H: 4.26; N: 22.32.
1,3-Bis({[(3Z)-5-nitro-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino})urea (6d)
IR (ν cm−1): 3097 (NH), 3050 (C–H, Ar), 1702 (C=O), 1618 (s, C=O, lactam), 1608, 1472 (C=C, Ar), 1626 (C=N) 1355 (–NO2). 1H-NMR (DMSO-d 6) ppm; δ 13.5 (s, 2H), 11.5 (s, 2H), 7.15–7.79 (m, 6H); mass (ESI–MS): m/z 439 (M+1, 100 %). Elemental analysis for C17H10 N8O7: calculated (%) C: 46.58; H: 2.30; N: 25.56; found: C: 46.53; H: 2.26; N: 25.54.
1,3-Bis({[(3Z)-2-oxo-2,3-dihydro-1H-indol-3-ylidene]amino})thiourea (6e)
IR (ν cm−1): 3150, 3010 (NH, NH) 1650 (C=O), 1610 (C=N), 1350 (NCSN). 1H-NMR (DMSO-d 6) δ ppm; δ 13.5 (s, 2H), 7.93 (s, 2H), 7.15–7.79 (m, 6H); mass (ESI–MS): m/z 365 (M+1, 100 %). Elemental analysis for C17H12 N6O2S: calculated (%) C: 56.04; H: 3.32; N: 23.06; found: C: 56.03; H: 3.36; N: 23.04.
Biological activities
Antiviral activity assays
The synthesized compounds were evaluated for antiviral activity according to well-established procedures by De Clercq (1981, 1986). The compounds were evaluated for antiviral activity by using the following viruses: human cytomegalovirus (HCMV) strains AD-169 and Davis, herpes simplex virus type 1 (HSV-1) strain KOS, thymidine kinase-deficient (TK-), HSV-1 KOS strain resistant to ACV (ACVr), herpes simplex virus type 2 (HSV-2) strain G, vaccinia virus, vesicular stomatitis virus (VSV), VZV strain Oka, TK- VZV strain 07-1, RSV strain Long, VSV, coxsackie B4, parainfluenza 3, Reovirus-1, Sindbis, Punta Toro, feline coronavirus (FIPV: feline infectious peritonitis virus), influenza A virus subtypes H1N1 and H3N2, and influenza B virus. Antiviral assays were carried out in Crandell–Rees feline kidney cells (feline corona virus and feline herpes virus), HeLa cell cultures (vesicular stomatitis virus, coxsackie virus B4, and RSV), human embryonic lung (HEL) cell cultures [HSV-1 (KOS), HSV-2 (G), vaccinia virus, vesicular stomatitis virus and HSV-1 TK- KOS ACVr], Madin Darby canine kidney (MDCK) cells (influenza A H1N1 subtype, influenza A H3N2 subtype, and influenza B) and Vero cell cultures (parainfluenza-3 virus, reovirus-1, sindbis virus, coxsackie virus B4, and Punta Toro virus). The HEL, Vero, and HeLa cell lines used in this study were monitored for mycoplasma contamination and were found to be mycoplasma-free.
Screening for inhibition of virus-induced cytopathic effect in vitro
Confluent cell cultures in microtiter 96-well plates were inoculated with 100 CCID50 of virus (1 CCID50 being the virus dose to infect 50 % of the cell cultures) or with 20 plaque forming units (PFU) (for VZV) and the cell cultures were incubated in the presence of varying concentrations of the test compounds. Viral cytopathicity or plaque formation (VZV) was recorded as soon as it reached completion in the control virus-infected cell cultures that were not treated with the test compounds. Antiviral activity was expressed as the EC50 or compound concentration required to reduce virus-induced cytopathicity or viral plaque formation by 50 %.
Cytotoxicity assays
Cytostatic activity were based on the inhibition of HEL cell growth. HEL cells were seeded at 5 × 103 cells/well into 96-well microtiter plates and allowed to proliferate for 24 h. Then, medium containing different concentrations of the test compounds was added. After 3 days of incubation at 37 °C, the cell number was determined with a Coulter counter. The cytostatic concentration was calculated as CC50 (the compound concentration required to reduce cell growth by 50 % relative to the number of cells in the untreated controls). CC50 values were estimated from graphic plots of the number of cells (percentage of control) as a function of the concentration of the test compounds. Cytotoxicity was expressed as minimum cytotoxic concentration (MCC) or the compound concentration that causes a microscopically detectable alteration of cell morphology.
Anti-influenza virus activity
The synthesized compounds were evaluated for their antiviral activity against three influenza virus subtypes [A/Puerto Rico/8/34 (H1N1); A/Hong Kong/7/87 (H3N2), and B/Hong Kong/5/72]. Antiviral activity was estimated from the inhibitory effect on virus-induced cytopathic effect, as determined by microscopical examination and/or the formazan-based MTS cell viability test. The EC50 (50 % Effective concentration), or concentration producing 50 % inhibition of virus-induced cytopathic effect, was determined by visual scoring of the CPE, or by measuring the cell viability with the colorimetric formazan-based MTS assay. Cytotoxicity of the test compounds was expressed as the compound concentration causing minimal changes in cell morphology (MCC), or the concentration causing 50 % cytotoxicity (CC50), as determined by the MTS assay.
Two-stage mouse-skin carcinogenesis test
Specific pathogen-free female ICR mice (6 weeks old, body weight approx. 30 g) were obtained from Japan SLC Inc., Shizuoka, Japan, and the animals were housed, five per polycarbonate cage, in a temperature-controlled room at 24 ± 2 °C and given food and water ad libitum throughout the experiment. Animals were divided into three experimental groups containing 15 mice each. The back (2 × 8 cm2) of each mouse was shaved with surgical clippers, and the mice were topically treated with 7,12-dimethyl benz[a]anthracene (DMBA) (100 μg, 390 nmol) in acetone (0.1 ml) an initiating treatment. One week after the initiation, papilloma formation was promoted twice weekly by the application of 12-O-tetradecanoylphorbol-13-acetate (TPA) (1 μg, 1.7 nmol) in acetone (0.1 ml) to the skin (Fig. 1). One hour before each treatment with TPA, the mice were treated with the samples (85 nmol) in acetone (0.1 ml). The incidence of papillomas was examined weekly over a period of 20 weeks (Tanaka et al., 2001), the percentages of mice bearing papillomas (Fig. 2a) and the average number of papillomas per mouse (Fig. 2b) were recorded.
Fig. 1.
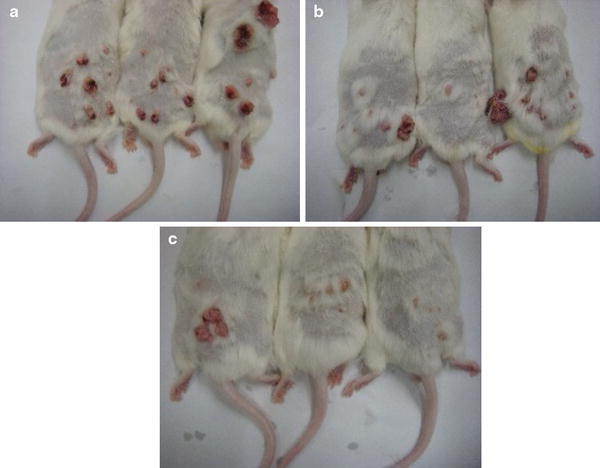
Inhibitory effects of compounds 6b and 6c on mouse-skin carcinogenesis induced by DMBA and TPA. a Positive control [DMBA (390 nmol) + TPA (1.7 nmol)]; b TPA + 85 nmol of 6b; c TPA + 85 nmol of 6c
Fig. 2.
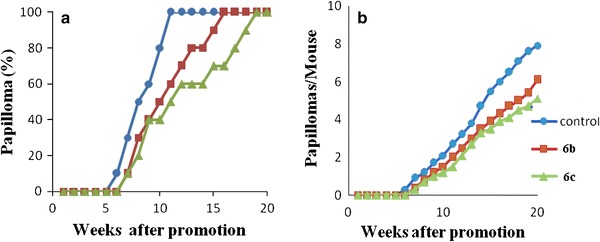
Inhibition effects of compounds 6b and 6c on DMBA–TPA-induced carcinogenesis. Tumor formation in all mice was initiated with DMBA (390 nmol) and promoted with TPA (1.7 nmol) twice weekly, 1 week after initiation. a Percentage of mice with papillomas. b Average number of papillomas/mouse. Circle control [DMBA (390 nmol) + TPA (1.7 nmol)]; filled square TPA + 85 nmol of 6b; triangle TPA + 85 nmol of 6c
Results and discussion
A series of new β-isatin aldehyde-N,N′-thiocarbohydrazone, bis-β-isatin thiocarbohydrazones, and bis-β-isatin carbohydrazones derivatives was synthesized by microwave-oriented reaction by two-step procedure as depicted in Schemes 1 and 2. The synthesized compounds were purified by column chromatography. All of the derivatives were characterized by FT-IR, 1H NMR, and mass spectral data. The FT-IR spectra of the compounds revealed absorption bands in the region 1,509–1,610 cm−1 corresponding to C=N stretching bands. Absence of carbonyl (C=O) peak around 1,715 cm−1 revealed the formation of Schiff bases. The 1H NMR spectrum of the synthesized compounds showed only one set of signals for the aromatic protons around 6.73–7.80 ppm, while the –NH of the isatin and –NH of hydrazones gave rise to two different signals in the 11–14 ppm range.
Antiviral activity
The novel β-isatin aldehyde-N,N′-thiocarbohydrazones (4a–g) and bis-isatin (6a–e) were evaluated against various strains of DNA viruses (i.e., human cytomegalovirus (HCMV), vaccinia virus (VACV), HSV type 1 (HSV-1) and type 2 (HSV-2), acyclovir-resistant, ACVr), VZV (Table 1). The test compounds were also evaluated against several RNA viruses (i.e., VSV, coxsackie B4 virus, RSV, parainfluenza virus type 3, reovirus-1, sindbis virus and Punta Toro virus (Table 2). The EC50 was calculated as the effective concentration of compound that decreased the percentage of formazan production in compound treated, virus-infected cells to 50 % of that produced by compound-free uninfected cells. The 50 % cytostatic concentration (CC50) was calculated as the concentration required to reduce cell growth by 50 %. MCC is the minimum cytotoxic concentration that causes a microscopically detectable alteration of cell morphology. The HEL, Vero, and HeLa cell lines used in this study were regularly monitored for mycoplasma contamination and found to be mycoplasma-free. The antiviral activity was measured for twelve isatin derivatives using a cell-protection assay. The data are recorded in Tables 1, 2, 3, and 4.
Table 1.
Inhibitory activity of synthesized isatin derivatives against DNA viruses
| S. no. | Compounds | Human embryonic cell culture (HEL) ECa50 (μM) | Crandell–Rees feline kidney cell culture (CRFK) | Human embryonic cell culture (HEL) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cytomegalovirus | Herpes simplex virus-1 (KOS) | Herpes simplex virus-2 (G) | Vaccinia virus | Vesicular stomatitis virus | Herpes simplex virus-1TK-KOS ACVr | Feline corona virus | Feline herpes virus | Varicella-zoster virus (VZV) | ||||
| AD-169 strain | Davis strain | TK + VZV strain | TK-VZV strain | |||||||||
| 1 | 4a | 12 ± 3.5 | 15 ± 0.4 | >20 | >20 | >20 | >20 | >20 | >20 | >20 | >4 | 7.4 |
| 2 | 4b | 16 ± 3.7 | 11.32 ± 0.08 | >20 | >20 | >20 | >20 | >20 | >20 | >20 | >20 | >20 |
| 3 | 4c | >20 | >20 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 4 | 4d | >20 | >20 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >20 | >20 |
| 5 | 4e | >20 | >20 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >20 | >20 |
| 6 | 4f | >20 | >20 | >20 | >20 | >20 | >20 | >20 | >100 | >100 | >20 | >20 |
| 7 | 4g | >20 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >20 |
| 8 | 6a | >20 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >20 | >100 |
| 9 | 6b | >20 | >20 | >100 | >100 | >100 | >100 | >100 | >100 | 19.7 | >20 | >20 |
| 10 | 6c | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | 55.1 | >100 | >100 |
| 11 | 6d | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >20 | >20 |
| 12 | 6e | >20 | >20 | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >20 | >20 |
| 13 | Ganciclovir | 8.1 ± 0.2 | 5.5 ± 2.36 | 0.02 | 0.01 | >100 | >100 | 4 | >100 | 1.4 | – | – |
| 14 | Cidofovir | 1.0 ± 0.05 | 0.78 ± 0.49 | 2 | 1 | 22 | >250 | 0.9 | – | – | – | – |
| 15 | Brivudin | – | – | 0.04 | 112 | 4 | >250 | 50 | – | – | 2.1 | 143 |
| 16 | Acyclovir | – | – | 0.4 | 0.2 | >250 | >250 | 22 | – | – | 0.019 | 104.5 |
| 17 | HHA (μg ml−1) | – | – | – | – | – | – | – | 4.2 | 11.0 | – | – |
| 18 | UDA (μg ml−1) | – | – | – | – | – | – | – | 1.6 | 1.2 | – | – |
“–” not performed
aRequired to reduce virus-induced cytopathogenicity by 50 %
Table 2.
Inhibitory activity of synthesized isatin derivatives against RNA Viruses
| S. no. | Compound | Antiviral activity ECa50 (μM) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HeLa cell cultures | Vero cell cultures | ||||||||
| Vesicular stomatitis virus | Coxsackie virus B4 | Respiratory syncytial virus | Para-influenza-3 virus | Reovirus-1 | Sindbis virus | Coxsackie virus B4 | Punta Toro virus | ||
| 1 | 4a | >20 | >20 | >20 | >20 | >20 | >20 | >20 | >20 |
| 2 | 4b | >4 | >4 | >4 | >20 | >20 | >20 | >20 | >20 |
| 3 | 4c | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 4 | 4d | >100 | >100 | >100 | >20 | >20 | >20 | >20 | >20 |
| 5 | 4e | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 6 | 4f | >100 | >100 | >100 | >20 | >20 | >20 | >20 | >20 |
| 7 | 4g | >20 | >20 | >20 | >100 | >100 | >100 | >100 | >100 |
| 8 | 6a | >100 | >100 | >100 | >20 | >20 | >20 | >20 | >20 |
| 9 | 6b | >100 | >100 | >100 | >20 | >20 | >20 | >20 | >20 |
| 10 | 6c | >100 | >100 | >100 | >20 | >20 | >20 | >20 | >20 |
| 11 | 6d | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 12 | 6e | >100 | >100 | >100 | >20 | >20 | >20 | >20 | >20 |
| 13 | DS—5,000 (μg ml−1) | 1 | >100 | 0.8 | >100 | >100 | 100 | >100 | >100 |
| 14 | (S)-DHPA | >250 | >250 | >250 | >250 | >250 | >250 | >250 | >250 |
| 15 | Ribavirin | 4 | 112 | 4 | 85 | 146 | >250 | 250 | 25 |
aRequired to reduce virus-induced cytopathogenicity by 50 %
Table 3.
Anti-influenza virus activity and cytotoxicity of compounds in MDCK cell cultures
| Compound | Cytotoxicity | Antiviral ECc50 (μM) | ||||||
|---|---|---|---|---|---|---|---|---|
| CCa50(μM) | Minimum cytotoxic concentrationb | Influenza A H1N1 subtype | Influenza A H3N2 subtype | Influenza B | ||||
| Visual CPE score | MTS | Visual CPE score | MTS | Visual CPE score | MTS | |||
| 4a | 51 | 20 | >4 | >4 | >4 | >4 | >4 | >4 |
| 4b | 46 | 20 | >4 | >4 | >4 | >4 | >4 | >4 |
| 4c | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 4d | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 4e | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 4f | >100 | >100 | 39 ± 5.5 | 37 ± 25 | 27 ± 7.0 | 27 ± 7.3 | 45 ± 0.0 | 37 ± 8.75 |
| 4g | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 6a | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 6b | >100 | >100 | >100 | >100 | >100 | >100 | >100 | >100 |
| 6c | 46 | ≥20 | >20 | >20 | >20 | >20 | >20 | >20 |
| 6d | >100 | >100 | 47 ± 2.5 | 55 ± 26 | 72 ± 27 | 33 ± 1.7 | 47 ± 2.5 | 38 ± 1.3 |
| 6e | >100 | >100 | 72 ± 27 | 61 ± 32 | 72 ± 27 | 34 ± 9.5 | 39 ± 5.5 | 48 ± 31 |
| Oseltamivir carboxylate | >100 | >100 | 0.4 ± 0.0 | 0.35 ± 0.2 | 10.25 ± 9.7 | 5.45 ± 4.05 | 6.7 ± 5.3 | 2.5 ± 0.7 |
| Ribavirin | >100 | >100 | 2.5 ± 0.5 | 2.8 ± 0.25 | 3 ± 1.0 | 2 ± 0.2 | 2.4 ± 1.6 | 2.45 ± 0.25 |
| Amantadine | >200 | >200 | 5 | 3.2 | 0.9 | 0.8 | >200 | >200 |
| Rimantadine | >200 | >200 | >200 | >200 | 0.4 | 0.6 | >200 | >200 |
MDCK cells Madin Darby canine kidney cells
a50 % Cytotoxic concentration, as determined by measuring the cell viability with the colorimetric formazan-based MTS assay
bMinimum compound concentration that causes a microscopically detectable alteration of normal cell morphology
c50 % Effective concentration, or concentration producing 50 % inhibition of virus-induced cytopathic effect, as determined by visual scoring of the CPE, or by measuring the cell viability with the colorimetric formazan-based MTS assay
Table 4.
Cytotoxicity for synthesized isatin derivatives in different cell cultures
| S.no | Compound | Human embryonic lung cell cultures | Crandell-Rees feline kidney cells | HeLa cell cultures | Vero cell cultures |
|---|---|---|---|---|---|
| Minimum cytotoxic concentrationa (μM) | Minimum cytotoxic concentrationa (μM) | Minimum cytotoxic concentrationa (μM) | Minimum cytotoxic concentrationa (μM) | ||
| 1 | 4a | 60 | 86 | ≥20 | 100 |
| 2 | 4b | 100 | 63 | 20 | 100 |
| 3 | 4c | ≥100 | >100 | >100 | >100 |
| 4 | 4d | 100 | >100 | >100 | 100 |
| 5 | 4e | 100 | >100 | >100 | >100 |
| 6 | 4f | 100 | 100 | >100 | ≥20 |
| 7 | 4g | ≥100 | ≥100 | 100 | >100 |
| 8 | 6a | ≥100 | >100 | >100 | 100 |
| 9 | 6b | 100 | >100 | >100 | 100 |
| 10 | 6c | >100 | >100 | >100 | 100 |
| 11 | 6d | ≥100 | >100 | >100 | >100 |
| 12 | 6e | 100 | >100 | >100 | 100 |
| 13 | Acyclovir | >400 | – | – | – |
| 14 | Brivudin | >300 | – | – | – |
| 15 | Ganciclovir | >350 | >100 | – | – |
| 16 | Cidofovir | >300 | – | – | – |
| 17 | DS-5000 (μg ml) | – | – | >100 | >100 |
| 18 | (S)-DHPA | – | – | >250 | >250 |
| 19 | Ribavirin | – | – | >250 | >250 |
aMinimum cytotoxic concentration that causes a microscopically detectable alteration of normal cell morphology
There was only moderate activity of the 4a and 4b compounds against both strains of HCMV. Although at concentrations close to their toxicity levels, no specific antiviral effects were noted with the evaluated compounds against HSV-1, (HSV-1 strain KOS), HSV-2 (HSV-2 strain G), HSV-1 (ACV resistant KOS strain), vaccinia virus, vesicular stomatitis virus, coxsackie virus B4, respiratory syncytial virus, parainfluenza-3 virus, reovirus-1, sindbis virus, and Punta Toro virus. None of the compounds exhibited specific antiviral effects (i.e., minimal antiviral effective concentration ≥ fivefold lower than minimal cytotoxic concentration) against any of the viruses evaluated.
Anti-influenza virus activity
The anti-influenza virus activities of a series of isatin derivatives were determined by measuring their inhibitory effects on virus replication in MDCK cells using three strains of the influenza subtype. The antiviral data obtained by microscopic evaluation of the virus-induced CPE were confirmed by the MTS cell viability assay and were expressed as the EC50. The cytotoxicities of the compounds were expressed as the MCC (the compound concentration causing minimal alterations in cell morphology as estimated by microscopy) or the CC50 (the compound concentration causing 50 % reduction in cell viability based on the MTS assay).
None of the twelve analogs were able to inhibit the cytopathic effects of three influenza virus subtypes i.e., H1N1, H3N2, and influenza B (Table 3), except 4f, 6d, and 6e that showed some activity below the non-toxic concentration of 100 µM.
Two-stage mouse-skin carcinogenesis test
In the present study, we selected two compounds 6b and 6c among the ten compounds to examine their effects on in vivo two-stage carcinogenesis using mouse-skin papillomas induced by DMBA as an initiator and TPA as a promoter. During the test, no significant toxic effects, such as inflammation and lesional damage (edema, erosion, and ulcer), were observed on the areas of mouse skin topically treated with test compounds. In our experiment, the body weight of the animals was not affected by the treatment with test compounds. As shown in Fig. 2a, the positive control (DMBA and TPA) group in papilloma-bearing mice appears rapidly from week 6, and reached 100 % within 10 weeks of promotion. On the other hand, treatment with compound 6c (85 nmol) along with DMBA/TPA reduced the percentage of papilloma-bearing mice to 40–70 % during weeks 10–15, and thereafter 90 % during week 18 and reached 100 % at week 20. As shown in Fig. 2b, in the positive control group, the number of papillomas per mouse formed increased rapidly after week 6 and reached 7.9 papillomas/mouse at week 20. On the other hand, mice treated with compound 6c bore only 5.1 papillomas/mouse over the period of week 20. A moderate protection is observed for the compound 6b. The percentage of papillomas increased rapidly from week 7 and reached 100 % after week 17, and in this group only 1.2, 3.9, and 6.1 papillomas were formed per mouse at 10, 15, and 20 weeks of promotion. From these results, the inhibitory effects of compound 6c on mouse two-stage carcinogenesis induced by DMBA and TPA were apparently more potent than those of compound 6b. Thus, as demonstrated above, the in vivo anti-tumor promoting activity of compound 6c showed stronger chemoprevention activity than that of compound 6b. These results suggest that isatin lead molecules may be useful as cancer chemopreventive agents.
Conclusion
We have synthesized twelve compounds by reacting substituted/unsubstituted 2,3-dihydro-2,3-dioxindole and thiocarbohydrazide/carbohydrazide in alcohol in the presence of glacial acetic acid. All synthesized compounds were characterized by FT-IR, NMR, and mass spectra. All the compounds were screened for antiviral activity against a various strains of DNA and RNA viruses and some of them, exhibited moderate antiviral activity compared with the reference compounds. Further, the anti-carcinogenic activity of compounds 6b and 6c was examined by a two stage-carcinogenesis test using DMBA as initiator and TPA as a promoter. The data suggested that compound 6c exhibited stronger chemoprevention activity than compound 6b. Thus these results suggest that isatin lead molecules could also be useful as cancer chemopreventive agents.
Acknowledgments
The authors are very much thankful to M. Sadalaxmi, President, Kakatiya Institute of Pharmaceutical Sciences, for providing the laboratory facilities. The antiviral research was performed by grants of the KU Leuven (GOA 10/14). The authors thank Leentje Persoons, Frieda De Meyer, Anita Camps, Lies Van den Heurck and Steven Carmans for excellent technical assistance.
References
- Akhaja TN, Raval JP. 1,3-dihydro-2H-indol-2-ones derivatives: design, synthesis, in vitro antibacterial, antifungal and antitubercular study. Eur J Med Chem. 2011;46:5573–5579. doi: 10.1016/j.ejmech.2011.09.023. [DOI] [PubMed] [Google Scholar]
- Alcaide B, Almendros P, Aragoncillo C, Campillos GG, Arnó M, Domingo LR. Scandium-catalyzed preparation of cytotoxic 3-functionalized quinolin-2-ones: regioselective ring enlargement of isatins or imino isatins. ChemPlusChem. 2012;77:563–569. doi: 10.1002/cplu.201200090. [DOI] [Google Scholar]
- Bacani PMC, Reis MB, Serpeloni JM, Calvo TR, Vilegas W, Varanda EA, Cólus IMS. Mutagenicity and genotoxicity of isatin in mammalian cells in vivo. Mutat Res. 2011;719:47–51. doi: 10.1016/j.mrgentox.2010.11.006. [DOI] [PubMed] [Google Scholar]
- Bal TR, Anand B, Yogeeswari P, Sriram D. Synthesis and evaluation of anti-HIV activity of isatin beta-thiosemicarbazone derivatives. Bioorg Med Chem Lett. 2005;15:4451–4455. doi: 10.1016/j.bmcl.2005.07.046. [DOI] [PubMed] [Google Scholar]
- Bauer DJ. A history of the discovery and clinical application of antiviral drugs. Br Med Bull. 1985;41:309–314. doi: 10.1093/oxfordjournals.bmb.a072069. [DOI] [PubMed] [Google Scholar]
- Bauer DJ, Sadler PW. New antiviral chemotherapeutic agent active against smallpox infection. Lancet. 1960;21:1110–1101. doi: 10.1016/s0140-6736(60)90990-9. [DOI] [PubMed] [Google Scholar]
- Bruce F, Richard HP, Pamela CC (2007) Lippincott’s illustrated reviews: microbiology. Lippincott Williams & Wilkins, Hagertown, pp 47–51
- Castro EF, Fabian LE, Caputto ME, Gagey D, Finkielsztein LM, Moltrasio GY, Moglioni AG, Campos RH, Cavallaro LV. Inhibition of bovine viral diarrhea virus RNA synthesis by thiosemicarbazone derived from 5,6-dimethoxy-1-indanone. J Virol. 2011;85:5436–5445. doi: 10.1128/JVI.00859-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clercq E. Strategies in the design of antiviral drugs. Nat Rev Drug Discov. 2002;1:13–25. doi: 10.1038/nrd703. [DOI] [PubMed] [Google Scholar]
- DeClercq E, Balzarini J, Torrence PF, Mertes MP, Schmidt CL, Shugar D, Barr PJ, Jones AS, Verhelst G, Walker RT. Thymidylate synthetase as target enzyme for the inhibitory activity of 5-substituted 2′-deoxyuridines on mouse leukemia L1210 cell growth. Mol Pharmacol. 1981;19:321. [PubMed] [Google Scholar]
- DeClercq E, Holý A, Rosenberg I, Sakuma T, Balzarini J, Maudgal PC. A novel selective broad-spectrum anti-DNA virus agent. Nature. 1986;323:464–467. doi: 10.1038/323464a0. [DOI] [PubMed] [Google Scholar]
- Hans RH, Wiid IJF, Helden PDV, Wan B, Frazblau SG, Gut J, Rosenthal PJ, Chilbale K. Novel thiolactone–isatin hybrids as potential antimalarial and antitubercular agents. Bioorg Med Chem Lett. 2011;21(7):2055–2058. doi: 10.1016/j.bmcl.2011.02.008. [DOI] [PubMed] [Google Scholar]
- Henry G, Blatt AH. Organic synthesis collective. 2. New York: Wiley; 1964. pp. 327–334. [Google Scholar]
- Kang IJ, Wang LW, Hsu TA, Yueh A, Lee CC, Lee YC, Lee CY, Chao YS, Shih SR, Chern JH. Isatin-β-thiosemicarbazones as potent herpes simplex virus inhibitors. Bioorg Med Chem Lett. 2011;21:1948–1952. doi: 10.1016/j.bmcl.2011.02.037. [DOI] [PubMed] [Google Scholar]
- Kiran G, Maneshwar T, Rajeshwar Y, Sarangapani M. Microwave-assisted synthesis, characterization, antimicrobial and antioxidant activity of some new isatin derivatives. J Chem. 2012;2013:1–7. doi: 10.1155/2013/192039. [DOI] [Google Scholar]
- Kiran G, Sarangapani M, Rajeshwar Y, Karki SS, Balzarini J, De Clercq E, Tokuda H. Microwave assisted synthesis, characterization of some new isatin and thiophene derivatives as cytotoxic and chemopreventive agents. Lett Drug Des Discov. 2012;9:934–941. doi: 10.2174/157018012804586950. [DOI] [Google Scholar]
- Medvedev AE, Buneeva O, Glover V. Biological targets for isatin and its analogues: implications for therapy. Biologics. 2007;1:151–162. [PMC free article] [PubMed] [Google Scholar]
- Mohamed A, Badawy A, Sayed A, Hady A. Reaction of isatin with thiocarbohydrazide: a correction. Arch Pharm (Weinheim) 1991;324:349–351. doi: 10.1002/ardp.19913240605. [DOI] [PubMed] [Google Scholar]
- Pandeya SN, Smitha S, Jyoti M, Sridhar SK. Biological activities of isatin and its derivatives. Acta Pharm. 2005;55:27–46. [PubMed] [Google Scholar]
- Prado-Prado FJ, de la Vega OM, Uriarte E, Ubeira FM, Chou KC, González-Díaz H. Unified QSAR approach to antimicrobials. 4. Multi-target QSAR modeling and comparative multi-distance study of the giant components of antiviral drug–drug complex networks. Bioorg Med Chem. 2009;17:569–575. doi: 10.1016/j.bmc.2008.11.075. [DOI] [PubMed] [Google Scholar]
- Quenelle DC, Keith KA, Kern ER. In vitro and in vivo evaluation of isatin-beta-thiosemicarbazone and marboran against vaccinia and cowpox virus infections. Antiviral Res. 2006;71:24–30. doi: 10.1016/j.antiviral.2006.02.010. [DOI] [PubMed] [Google Scholar]
- Reddy BVS, Rajeswari N, Sarangapani M, Reddy GR, Madan Ch, Kumar KP, Rao MS. Iodine-catalyzed conjugate addition of indoles onto en-1,4-dione: a novel synthesis of 3-(1-(1H-indol-3-yl)-2-oxo-2-phenylethyl)indolin-2-ones as antibacterial and antifungal agents. Bioorg Med Chem Lett. 2011;21(21):6510–6514. doi: 10.1016/j.bmcl.2011.08.075. [DOI] [PubMed] [Google Scholar]
- Reddy BVS, Rajeswari N, Sarangapani M, Prashanthi Y, Jones GR, Anthony A. Iodine-catalyzed condensation of isatin with indoles: a facile synthesis of di(indolyl)indolin-2-ones and evaluation of their cytotoxicity. Bioorg Med Chem. 2012;22:2460–2463. doi: 10.1016/j.bmcl.2012.02.011. [DOI] [PubMed] [Google Scholar]
- Sebastain L, Desai A, Shampur MN, Permul Y, Vasanthapuram R. N-methylisatin-beta-thiosemicarbazone derivative (SCH 16) is an inhibitor of Japanese encephalitis virus infection in vitro and in vivo. Virol J. 2008;22(5):64. doi: 10.1186/1743-422X-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmidt MS, Reverdito AM, Kremenchuzky L, Perillo IA, Blanco MM. Simple and efficient microwave assisted N-alkylation of isatin. Molecules. 2008;13:831–840. doi: 10.3390/molecules13040831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin N, Venables SNBL, Combrink KD, Gulqeze HB, Yu KL, Civiello RL, Thuring J, Wang XA, Yang Z, Zadjura L, Marino A, Kadow KF, Cianci CW, Clarke J, Genovesi ESV, Medina I, Lamb L, Krystal M, Meanwell NA. Respiratory syncytial virus fusion inhibitors. Part 7: structure–activity relationships associated with a series of isatin oximes that demonstrate antiviral activity in vivo. Bioorg Med Chem Lett. 2009;19:4857–4862. doi: 10.1016/j.bmcl.2009.06.030. [DOI] [PubMed] [Google Scholar]
- Tanaka R, Minami T, Tsujimoto K, Matsunga S, Tokuda H, Nishino H, Terada Y, Yoshitake A. Cancer chemopreventive agents, serratane-type triterpenoids from Picea jezoensis. Cancer Lett. 2001;172:119–126. doi: 10.1016/S0304-3835(01)00650-4. [DOI] [PubMed] [Google Scholar]
- Teitz Y, Ronen D. Inhibition of the synthesis of Moloney leukemia virus structural proteins by N-methylisatin-beta-4′,4′-diethylthiosemicarbazone. Antimicrob Agents Chemother. 1984;26:913–916. doi: 10.1128/AAC.26.6.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J, Wu D, Gou J. Optimization of the production of thiocarbohydrazide using the Taguchi method. Chem Technol Biotechnol. 2010;85:1402–1406. doi: 10.1002/jctb.2446. [DOI] [Google Scholar]


