Abstract
Objective
To compare readmission rates as measured by the Centers for Medicare and Medicaid Services and the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) methods.
Data Sources
20 percent sample of national Medicare data for patients undergoing cystectomy, colectomy, abdominal aortic aneurysm (AAA) repair, and total knee arthroplasty (TKA) between 2010 and 2014.
Study Design
Retrospective cohort study comparing 30‐day readmission rates.
Data Collection/Extraction Methods
Patients undergoing cystectomy, colectomy, abdominal aortic aneurysm repair, and total knee arthroplasty between 2010 and 2014 were identified.
Principal Findings
Cystectomy had the highest and total knee arthroplasty had the lowest readmission rate. The NSQIP measure reported significantly lower rates for all procedures compared to the CMS measure, which reflects an immortal‐time bias.
Conclusions
We found significantly different readmission rates across all surgical procedures when comparing CMS and NSQIP measures. Longer length of stay exacerbated these differences. Uniform outcome measures are needed to eliminate ambiguity and synergize research and policy efforts.
Keywords: administrative data uses, health policy/politics/law/regulation, Medicare, program evaluation, quality of care/patient safety, surgery
What this study adds.
What was already known?
The Hospital Readmissions Reduction Program (HRRP) aims to improve quality.
HRRP initially targeted medical conditions for readmission benchmarking.
Under the HRRP, underperforming hospitals receive reduced payments.
Benchmarks exist for the rate of unplanned readmission after certain surgical procedures.
Readmission rate is subject to bias in the literature due to differences in measurement method.
An immortal‐time bias exists for one of two commonly used readmission measures.
What do we know now?
The American College of Surgeons National Surgical Quality Improvement Program method of measuring readmission underestimates the true readmission rate.
Immortal‐time bias is strengthened as the duration and variability of length of stay increase.
Reoperation rate or complication rate may be a more appropriate measure of quality for surgical procedures with relatively low or widely variable lengths of stay.
1. INTRODUCTION
Readmission following major surgery is common and costly, affecting 15 percent of patients within 30 days of discharge and averaging nearly $14 000 per episode.1 Though some readmissions are necessary, preventable readmissions are estimated to cost $25 million annually.2 As such, readmission has received significant attention from both researchers and policy makers.
The Hospital Readmissions Reduction Program (HRRP), a Centers for Medicare and Medicaid Services (CMS) policy, addresses excess readmission by penalizing underperforming hospitals.3 While initially targeting medical conditions, this policy expanded to include surgical discharges.4 Positive change has come from HRRP; however, these improvements have been recently found to be overstated.5 There is an ongoing nuanced discussion of readmission in health policy circles, but aspects of readmission measurement in the surgical literature present methodological concerns.6, 7
One such concern regards the inconsistency between CMS, which reports readmissions within 30 days of the index hospitalization discharge, and the American College of Surgeons National Surgical Quality Improvement Program (NSQIP), which reports readmission within 30 days of the index surgery.3, 8 In this letter, we demonstrate how this inconsistency is a particular concern across surgical procedures with disparate lengths of stay.
2. METHODS
Using a 20 percent sample of national Medicare data, we identified patients undergoing cystectomy, colectomy, abdominal aortic aneurysm (AAA) repair, and total knee arthroplasty (TKA) between 2010 and 2014. These procedures were chosen due to varying index lengths of stay and readmission rates. We included patients with continuous Medicare enrollment for one year prior to surgery and at least 30 days after discharge. We calculated 30‐day readmission using both the CMS and NSQIP methods and compared differences using t tests.
3. RESULTS
We identified 299 249 patients, whose characteristics are shown in Table 1. Median length of stay was 9 days for cystectomy and colectomy, 3 days for AAA repair, and 4 days for TKA. Regardless of measurement methodology, cystectomy had the highest 30‐day readmission rate and TKA had the lowest readmission rate (Figure 1). However, we found an absolute difference in the CMS and NSQIP measurement of readmission of 6.2 percent for cystectomy, 3.7 percent for colectomy, 2.5 percent for AAA repair, and 0.4 percent for TKA. These corresponded to a relative difference of 31 percent for cystectomy, 36 percent for colectomy, 28 percent for AAA repair, and 9 percent for TKA, with the NSQIP measure reporting significantly lower rates for all procedures (all P < .001).
Table 1.
Demographic characteristics of Medicare beneficiaries undergoing major surgery
| Characteristic | Cystectomy | Colectomy | AAA | TKR |
|---|---|---|---|---|
| n = 3544 | n = 70 608 | n = 20 065 | n = 205 032 | |
| Age, year (median, IQR) | 75 (71‐80) | 77 (71‐83) | 77 (72‐82) | 74 (70‐79) |
| Race/ethnicity, no. (%) | ||||
| White | 3276 (92) | 62 467 (89) | 18 660 (93) | 187 214 (91) |
| Black | 163 (5) | 5461 (8) | 853 (4) | 10 482 (5) |
| Hispanic | 26 (1) | 834 (1) | 117 (1) | 2288 (1) |
| Asian | 22 (1) | 703 (1) | 177 (1) | 1778 (1) |
| Other | 57 (2) | 1143 (2) | 258 (1) | 3270 (2) |
| Average number of HCCs (SD) | 2.1 (1.8) | 1.8 (2) | 2.1 (2) | 1.2 (1) |
| Socioeconomic class, no. (%) | ||||
| Low | 1144 (32) | 22 906 (32) | 6523 (33) | 65 558 (32) |
| Medium | 1136 (32) | 22 771 (32) | 6529 (33) | 65 777 (32) |
| High | 1165 (33) | 23 188 (33) | 6527 (33) | 68 487 (33) |
| Residential area, no. (%) | ||||
| Large metropolitan county | 1587 (45) | 31 617 (44) | 8255 (41) | 86 514 (42) |
| Smaller metropolitan county | 1165 (33) | 24 003 (34) | 6942 (35) | 73 006 (36) |
| Urban county | 697 (20) | 13 153 (19) | 4239 (21) | 39 744 (20) |
| Smaller urban or rural county | 92 (3) | 1763 (3) | 606 (3) | 5600 (3) |
| Length of stay, days (median, IQR) | 9 (8‐13) | 9 (6‐14) | 3 (2‐7) | 4 (4‐4) |
Percentages may not add to 100 due to rounding.
Abbreviations: AAA, abdominal aortic aneurysm; CMS, Centers for Medicare and Medicaid Services. HCC, hierarchical condition category; IQR, interquartile range; NSQIP, National Surgical Quality Improvement Program; SD, standard deviation; TKR, total knee replacement.
Figure 1.
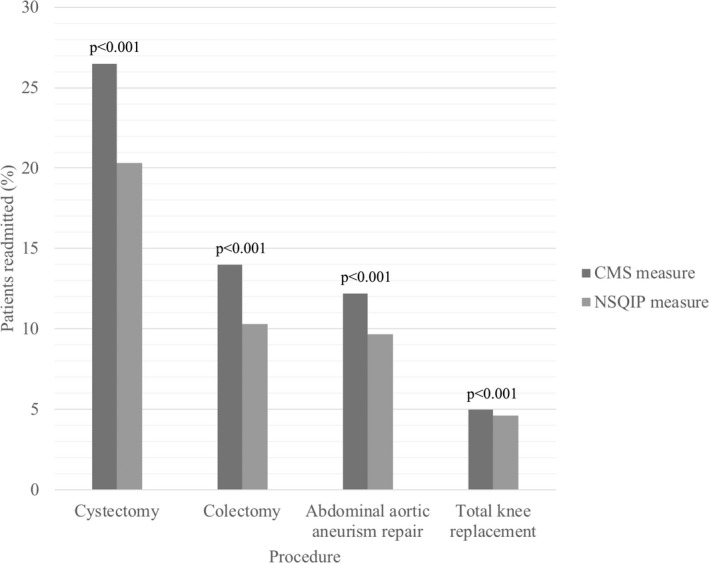
Comparison of CMS and NSQIP readmission measures in Medicare beneficiaries undergoing major surgery
Abbreviations: CMS, Centers for Medicare and Medicaid Services; and NSQIP, National Surgical Quality Improvement Program.
Note: Readmission measure definitions: CMS, 30 days from index hospitalization discharge date; and NSQIP, 30 days from index surgery date. P < .001 for readmission rate differences in all procedures.
4. DISCUSSION
We found significantly different readmission rates across all surgical procedures when comparing CMS and NSQIP measures. Longer lengths of stay exacerbated these differences. These findings demonstrate the need for uniformity across measurement methodologies to allow for more direct comparisons across studies that seek to examine the intended and unintended effects of changes to readmission policy.
Our findings result from an immortal‐time bias, defined as the span of time in the follow‐up period during which the outcome of interest could not possibly have occurred.9 When measuring readmission from the index surgical date, patients are considered “immortal” from readmission until discharge. In 2013, Lucas et.al. showed that longer lengths of stay strengthened immortal‐time bias.10 We show that immortal‐time bias is further emphasized across different procedures with disparate lengths of stay. For example, radical cystectomy is a morbid procedure with a longer and more variable length of stay. Estimated readmission rate in the literature ranges from 29 percent using CMS data to 20 percent using ACS NSQIP data.11, 12 The estimate closer to 30 percent is a more accurate reflection of the true readmission rate.
Not only does immortal‐time bias artificially lower 30‐day readmission rate, it minimizes other risk factors for readmission. These risk factors include complications that occur during index hospitalizations, postdischarge complications, and patient‐ and community‐level factors in the postdischarge environment.13, 14 Immortal‐time bias increasingly attenuates the effect of these risk factors as length of stay increases, by overlooking what occurs during the inpatient hospital stay and shortening the timeframe of potentially harmful postdischarge exposures.
Recognizing immortal‐time bias has important implications for surgical outcomes research and informing future health policy. For surgical outcomes research, our data show that the CMS definition more appropriately accounts for readmission risk factors while estimating a more accurate readmission rate. We believe the CMS measure should be uniformly adopted to measure readmission, especially if hypotheses or conclusions regard health policy. However, complication rate or 90‐day mortality may be more appropriate quality metrics for morbid procedures with long lengths of stay, such as cystectomy and colectomy. Likewise, measures such as reoperation rate or surgical site infection may facilitate more meaningful quality improvement for procedures with short lengths of stay like arthroplasty.
In conclusion, an immortal‐time bias is responsible for a 9 to 36 percent difference in readmission rate when CMS and NSQIP measurement methodologies are compared. This bias is strengthened as both the duration and variability of length of stay increase. As health services research and health policy become more enmeshed, uniform outcome measures are needed to eliminate ambiguity and synergize results across studies.
CONFLICTS OF INTEREST
There are no conflicts of interest to disclose.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: The views expressed in this article do not reflect the views of the federal government.
Hugar LA, Borza T, Oerline MK, Hollenbeck BK, Skolarus TA, Jacobs BL. Resurrecting immortal‐time bias in the study of readmissions. Health Serv Res. 2020;55:273–276. 10.1111/1475-6773.13252
Hugar and Borza contributed equally to this work.
REFERENCES
- 1. Qasim M, Andrews RM. Post‐Surgical Readmissions among Patients Living in the Poorest Communities, 2009: Statistical Brief #142. Healthcare Cost and Utilization Project. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb_readmission.jsp. Accessed April 20, 2018. [PubMed] [Google Scholar]
- 2. PricewaterhouseCoopers . The Price of Excess: Identifying Waste in Healthcare Spending; 2008. http://www.pwc.com/hri. Accessed February 19, 2018.
- 3. U.S. Centers for Medicare & Services Medicaid . Readmissions Reduction Program (HRRP). https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed May 5, 2018. [Google Scholar]
- 4. Medicare Payment Advisory Commission . Refining the hospital readmissions reduction program In: Report to the Congress: Medicare and the Health Care Delivery System. Washington: Medicare Payment Advisory Commission; 2013:91‐114. [Google Scholar]
- 5. Ody C, Msall L, Dafny LS, et al. Decrease in readmissions credited to medicare's program to reduce hospital readmissions have been overstated. Health Aff. 2019;38(1):36‐43. [DOI] [PubMed] [Google Scholar]
- 6. Berenson RA, Paulus RA, Kalman NS. Medicare's readmissions‐reduction program — a positive alternative. N Engl J Med. 2012;366(15):1364‐1366. [DOI] [PubMed] [Google Scholar]
- 7. Hechenbleikner EM, Makary MA, Samarov DV, et al. Hospital readmission by method of data collection. J Am Coll Surg. 2013;216:1150‐1158. [DOI] [PubMed] [Google Scholar]
- 8. American College of Surgeons . User Guide for the 2015 ACS NSQIP Participant Use Data File (PUF). https://www.facs.org/~/media/files/qualityprograms/nsqip/nsqip_puf_user_guide_2015.ashx. Accessed May 5, 2018. [Google Scholar]
- 9. Suissa S. Immortal time bias in pharmacoepidemiology. Am J Epidemiol. 2008;167(4):492‐499. [DOI] [PubMed] [Google Scholar]
- 10. Lucas DJ, Haider A, Haut E, et al. Assessing readmission after general, vascular, and thoracic surgery using ACS‐NSQIP. Ann Surg. 2013;258(3):430‐439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stitzenberg KB, Chang Y, Smith AB, et al. Exploring the burden of inpatient readmissions after major cancer surgery. J Clin Oncol. 2015;33(5):455‐464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gandaglia G, Varda B, Sood A, et al. Short‐term perioperative outcomes of patients treated with radical cystectomy for bladder cancer included in the National Surgical Quality Improvement Program (NSQIP) database. Can Urol Assoc J. 2014;8(9–10):E681‐E687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lawson EH, Hall BL, Louie R, Zingmond DS, Ko CY. Identification of modifiable factors for reducing readmission after colectomy: a national analysis. Surgery. 2014;155(5):754‐766. [DOI] [PubMed] [Google Scholar]
- 14. Joynt KE, Orav EJ, Jha AK. Thirty‐day readmission rates for medicare beneficiaries by race and site of care. J Am Med Assoc. 2011;305(7):675. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


