Abstract
Objective
To determine the correlation between hospital 30‐day risk‐standardized readmission rates (RSRRs) in elderly adults and those in nonelderly adults and children.
Data Sources/Study Setting
US hospitals (n = 1760 hospitals admitting adult patients and 235 hospitals admitting both adult and pediatric patients) in the 2013‐2014 Nationwide Readmissions Database.
Study Design
Cross‐sectional analysis comparing 30‐day RSRRs for elderly adult (≥65 years), middle‐aged adult (40‐64 years), young adult (18‐39 years), and pediatric (1‐17 years) patients.
Principal Findings
Hospital elderly adult RSRRs were strongly correlated with middle‐aged adult RSRRs (Pearson R 2 .69 [95% confidence interval (CI) 0.66‐0.71]), moderately correlated with young adult RSRRs (Pearson R 2 .44 [95% CI 0.40‐0.47]), and weakly correlated with pediatric RSRRs (Pearson R 2 .28 [95% CI 0.17‐0.38]). Nearly identical findings were observed with measures of interquartile agreement and Kappa statistics. This stepwise relationship between age and strength of correlation was consistent across every hospital characteristic.
Conclusions
Hospital readmission rates in elderly adults, which are currently used for public reporting and hospital comparisons, may reflect broader hospital readmission performance in middle‐aged and young adult populations; however, they are not reflective of hospital performance in pediatric populations.
Keywords: age, readmission
What this study adds.
Initiatives to reduce readmissions have focused predominately on elderly adult patients insured by Medicare; however, these patients account for only about one‐third of all hospital admissions.
Little is known about the relationship between elderly adult readmission rates with non‐elderly adult and pediatric readmission rates or the suitability of publicly reported readmission rates for profiling hospital performance in other age groups.
In this nationally representative sample of U.S. inpatient hospitalizations, hospital elderly adult RSRRs were strongly correlated with middle‐aged adult RSRRs, moderately correlated with young adult RSRRs, and not correlated with pediatric RSRRs.
Hospital readmission rates in elderly adults may reflect broader hospital readmission performance in other adult populations; however, they are not reflective of hospital performance in pediatric populations.
1. INTRODUCTION
Hospital readmissions are a priority for hospitals and policy makers, given their prevalence and cost.1 In October 2012, the Centers for Medicare & Medicaid Services (CMS) launched the Hospital Readmissions Reduction Program (HRRP),2, 3 which imposed financial penalties for hospitals with higher‐than‐expected Medicare readmissions for target conditions. This initiative and others have prompted hospitals to prioritize readmission reduction efforts among Medicare beneficiaries. In contrast, other adult and pediatric readmissions have been largely exempt from HRRP's public reporting and financial penalties but may benefit from a spillover effect of hospital efforts to address Medicare readmissions.4 Despite an abundance of research evaluating hospital readmissions in Medicare beneficiaries,5, 6, 7, 8, 9, 10, 11, 12, 13 adults ≥65 years of age account for only 35 percent of all hospital admissions, with young and middle‐aged adults accounting for half of total hospital admissions and pediatric admissions accounting for the remainder (15 percent).14 Little is known about the relationship between elderly readmission rates and nonelderly adult or pediatric rates.
Such information is important for understanding the application and limitations of readmission measures. Medicare readmission measures have been widely used to measure the quality of care delivered in US hospitals.15, 16 Although such measures control for age and patient comorbidities to account for differences in case mix within and across hospitals in elderly adults, it is unclear whether risk‐adjusted readmission rates in this cohort are reflective of hospital performance more globally across all age‐group cohorts. If readmission rates are highly correlated across elderly vs other age‐groups within hospitals, then publicly reported readmission rates may reflect broader hospital quality or an organizational structure that promotes quality improvement. Similarly, understanding how readmission rates correlate within a hospital across patient populations may provide insight into how readmission reduction efforts are being implemented. Nonelderly adult and pediatric patients may benefit from positive spillover effects from system‐wide readmission reduction efforts targeting elderly Medicare populations. Alternatively, no relationship between age‐specific readmission rates might suggest that departments operate in silos such that elderly readmission reduction efforts do not extend to younger patients. Finally, as Medicaid and private insurers that serve many younger individuals start to implement readmission measures, such as the Pediatric All‐Condition Readmission measure, it is important to understand the suitability and limitations of current measures for assessing hospital‐wide readmission performance.17, 18
This study evaluated the association between hospital‐level risk‐standardized middle‐aged adult, young adult, and pediatric readmission rates with elderly adult rates. Correlations and agreement between age‐specific 30‐day RSRRs were determined overall and across hospital characteristics to identify whether age‐specific RSRRs were more strongly correlated in certain types of hospitals.
2. METHODS
2.1. Data source
We used data from the 2014 Healthcare Cost and Utilization Project (HCUP) Nationwide Readmissions Database (NRD) to identify hospitals that treat both adult and pediatric patients. The NRD is a nationally representative, all‐payer database of hospital inpatient visits for all ages. It contains ~15 million discharges from 2048 hospitals across 22 geographically dispersed states with patient identifiers to link individuals across hospitalizations within state hospitals. Details appear elsewhere.19, 20
2.2. Hospital sample
The analytic steps are outlined in Figure S1. Two separate samples of hospitals were used to maximize the number of hospitals in analyses of readmission rates in adult populations and pediatric populations. The adult sample included all nonspecialty hospitals with ≥100 elderly adult (≥65 years old) index admissions and was used to calculate readmission rates for young, middle‐aged, and elderly adult patients (Figure S2). To remove specialty hospitals, we excluded hospitals with >50 percent of all primary diagnoses categorized as orthopedic (n = 24), oncologic (n = 1), psychiatric (n = 18), or obstetric (n = 8) conditions or >70 percent of all primary diagnoses categorized as surgical conditions (n = 14). Fifty‐seven specialty hospitals (3 percent) were excluded. Although such hospitals could treat patients for other diagnoses, they appeared unlikely to represent general hospitals with an array of subspecialty services or a diversity of patients.
The pediatric/adult sample was a subset of the adult sample and was used to calculate readmission rates for pediatric (1‐17 years) patients and elderly (≥65 years) adult patients for comparison. It included all nonspecialty hospitals with ≥100 pediatric index admissions. We chose ≥100 to increase the likelihood that hospitals had a pediatric service and to ensure adequate sample size for readmission rate calculations. Additionally, we excluded hospitals with <2 percent of all index admissions <18 years old to remove hospitals with very small relative pediatric volumes and with >80 percent of all pediatric admissions 13‐17 years old to remove hospitals that care for predominately adolescent patients. Finally, to remove specialty hospitals, we excluded hospitals with >50 percent of all pediatric primary diagnoses categorized as orthopedic (n = 2), oncologic (n = 0), or psychiatric (n = 29) conditions or >70 percent of all pediatric primary diagnoses categorized as surgical conditions. A total of 32 pediatric specialty hospitals (11 percent) of the sample were excluded. Of note, we excluded infants <1‐year‐old from our analyses to avoid including hospitals with obstetric services that do not otherwise treat pediatric patients and because NRD excludes records for patients <1 for about half the states.20
2.3. Within‐hospital patient sample
All index admissions to hospitals in the adult and pediatric/adult samples between 1/1/14 and 11/30/14 were identified to allow for a full 30‐day readmission window. In accordance with the National Quality Forum (NQF)‐endorsed hospital all‐condition readmission measures, we excluded index admissions for patients who died, left against medical advice, were discharged to another short‐term acute hospital setting, or were admitted for psychiatric or obstetric causes. Index admissions were divided by age into pediatric (1‐17), young adult (18‐39), middle‐aged adult (40‐64), and elderly adult (≥65) cohorts.
2.4. Patient and hospital characteristics
We assessed characteristics of the index admissions including age, gender, payer, number of chronic conditions, and top discharge diagnoses. NRD defines chronic conditions as lasting ≥12 months and either causing disability/impairments or resulting in the need for ongoing medical interventions. Discharge diagnoses were grouped using the AHRQ condition categories(https://meps.ahrq.gov/data_stats/conditions.shtml) for comparison across age‐groups; these are 63 distinct categories of conditions or body systems in the Clinical Classifications Software (CCS) to group diagnostic or procedure codes into clinically meaningful categories.
Hospital characteristics were drawn from available NRD variables originally collected from the American Hospital Association (AHA) Annual Survey19: hospital ownership, location and teaching status, and bed size. Bed size categories were based on number of hospital beds across all ages. Definitions of small, medium, and large vary by region and urban vs rural setting. Teaching status was defined by the presence of an AMA‐approved residency program or Council of Teaching Hospitals membership. Because nonmetropolitan teaching hospitals are rare, hospitals were divided into metropolitan nonteaching, metropolitan teaching, and nonmetropolitan categories. In addition, we calculated the percentage of hospital stays for patients aged <65 years old paid for by Medicaid to identify hospitals that disproportionately treat lower income patients.
2.5. Outcome
The primary outcome was all‐cause unplanned readmission to any hospital within 30 days of discharge. To align our estimates with those of the Pediatric All‐Condition Readmission Measure and the CMS risk‐standardized readmission measures, only the first readmission within 30 days was considered.21, 22 Subsequent admissions after 30 days from discharge were evaluated as another index hospitalization. Readmission hospitalizations within 30 days of a prior discharge were not categorized as index hospitalizations. We excluded readmissions for planned procedures as defined by the CMS Hospital‐wide All‐Cause Readmission Measure for the adult cohorts or the Pediatric All‐Condition Readmission Measure for the pediatric cohort.18, 21, 22
Hospital 30‐day RSRRs were calculated for the four cohorts separately within each hospital. For patients ≥18 (ie, young adult, middle‐aged adult, and elderly adult cohorts) in both the adult and pediatric/adult samples, we used the CMS Hospital‐wide All‐Cause Readmission Measure, described previously,21, 22 with two modifications. First, due to small sample size at some hospitals, we did not divide the sample into condition cohorts. Instead, we analyzed all admissions within a given hospital together. Second, because we lacked data on the year prior to admission, only diagnoses on that hospital record were included in the risk adjustment model. Risk adjustment was performed in an identical fashion to the CMS model using hierarchical logistic regression with a random hospital intercept to adjust for age, 31 risk factors, and the principal diagnosis grouped by AHRQ CCS codes.
For patients < 18 years in the pediatric/adult sample, RSRR calculations were performed using the Pediatric All‐Condition Readmission Measure developed by the Boston Children's Hospital Center of Excellence for Pediatric Quality Measurement.18 Briefly, it uses a hierarchical logistic regression model with a random hospital intercept that included age, gender, presence of 17 chronic condition body system indicators, and number of body systems affected by chronic conditions.
For both risk‐adjusted models, 30‐day RSRRs for each hospital were calculated as the ratio of “predicted” number of readmissions (from the model with the hospital‐specific effect) to “expected” number of readmissions (from the model applying the average effect among hospitals) multiplied by the national observed readmission rate.
2.6. Statistical analyses
Hospital characteristics were summarized across the adult and the adult/pediatric samples separately. Admission characteristics were summarized across the four age cohorts separately.
To assess the degree of association within hospitals’ age cohort‐specific RSRRs, we calculated Pearson correlation coefficients between pediatric, young adult, and middle‐aged adult RSRRs with elderly adult RSRRs. We compared each age cohort‐specific RSRR to elderly adult RSRRs because the latter are used by CMS for public reporting. In the adult hospital sample (n = 1760), we compared young adult and middle‐aged adult RSRRs against elderly adult RSRRs; in the pediatric/adult sample of hospitals (n = 235), we compared pediatric and elderly adult RSRRs.
We then divided hospitals into performance quartiles based on age cohort‐specific RSRRs and assessed the degree of agreement across quartiles using weighted Cohen's kappa statistics. We used a linear set of weights to account for greater magnitude of disagreement across quartiles. For each age‐specific group of RSRRs, we calculated the percentage of hospitals in the same quartile of performance, the same top or bottom quartile of performance, and the opposite quartile of performance (top or bottom) as elderly adult RSRRs.
We repeated analyses in subgroups of hospitals stratified by size, ownership, and teaching status to determine whether age‐specific readmission rates were more strongly correlated in certain hospitals. To compare differences in the strength of the correlations across hospital characteristics, we transformed Pearson correlation coefficients using Fisher's R‐to‐z transformation and then compared z‐scores between hospital categories for given age‐group pairs with a standard normal procedure.23 P‐values < .05 were considered statistically significant.
To determine the consistency of the association of age with 30‐day RSRRs, we repeated the RSRR calculations for smaller age cohorts from 1‐9, through each ten years, to ≥ 70 years and compared all age cohorts to the ≥70‐year‐old cohort using Pearson coefficients and weighted Kappa statistics. All analyses were performed using SAS 9.4. This analysis received IRB exemption.
2.7. Sensitivity analyses
We performed five sensitivity analyses. First, we repeated all analyses comparing elderly and nonelderly adults in the pediatric/adult sample to ensure that the observed differences across age categories were not related to the use of two separate hospital samples. Second, we repeated all 30‐day RSRR calculations using the pediatric risk adjustment algorithm to determine whether differences in the strength of RSRR correlations across age cohorts persisted irrespective of risk adjustment methodology. We used the pediatric algorithm because it adjusts for body system indicators rather than individual discharge diagnoses and can be more generally applied to other populations. Third, we repeated our analyses reincluding specialty hospitals given the potential for misclassification of hospitals as specialty hospitals based on primary diagnosis codes alone. Fourth, we repeated the analyses in the 2013 NRD database in order to test the external validity of our findings by confirming them in another population. Finally, we repeated the analyses for only patients admitted for infections in order to determine whether the stronger correlations observed between elderly and middle‐aged adults were due to similarity in discharge diagnoses. We chose infection (sepsis, bacteremia, viral infections, CNS infections, pericarditis/myocarditis, pneumonia, influenza, upper respiratory infections, urinary tract infections, and skin and soft tissue infections) diagnoses common across all ages. We required a minimum of 15 admissions each among young, middle‐aged, and elderly adults for infection.
3. RESULTS
The adult sample included 8,749,088 adult index admissions from 1760 nonspecialty hospitals; the pediatric/adult sample included 206 047 pediatric and 2 614 622 adult admissions from 235 nonspecialty hospitals (Figure S2). The percentage of nonelderly patients per hospital ranged from 8.2 percent to 89.4 percent in the adult sample and 2.0 percent to 23.4 percent for pediatric patients in the pediatric/adult sample (Figure S3). Most hospitals in the adult sample were small or medium (68 percent) or nonteaching hospitals (69 percent); most in the pediatric/adult sample were larger (67 percent) or teaching hospitals (68 percent; Table 1). Pediatric/adult sample hospitals treated a greater percentage of Medicaid patients than adult sample hospitals (highest Medicaid tertile 38 percent vs 33 percent) likely due to the inclusion of pediatric patients, who were more likely to be covered by Medicaid. Admission characteristics and the top 5 discharge diagnoses for the four age cohorts are presented in Table 2.
Table 1.
Hospital characteristics
| Adult sample (N = 1760) | Adult/pediatric sample (N = 235) | |
|---|---|---|
| Hospital ownership, n (%) | ||
| Public | 342 (19.4) | 53 (22.6) |
| Private, not‐for‐profit | 1100 (62.5) | 151 (64.3) |
| Private, for‐profit | 318 (18.1) | 31 (13.2) |
| Location/teaching status, n (%) | ||
| Metropolitan teaching | 553 (31.4) | 160 (68.1) |
| Metropolitan, nonteaching | 645 (36.7) | 49 (20.9) |
| Nonmetropolitan | 562 (31.9) | 26 (11.1) |
| Hospital bed size, n (%) | ||
| Small/Medium | 1198 (68.1) | 78 (33.2) |
| Large | 562 (31.9) | 157 (66.8) |
| Medicaid tertile, % | ||
| Lowest | <21.4% | <24.8% |
| Middle | 23.4%‐32.6% | 24.8%‐38.1% |
| Highest | ≥32.7% | ≥38.2% |
Table 2.
Admission characteristics and top diagnoses by age‐group
|
Pediatric index admissions (1‐17 y) (n = 206 047)a |
Young adult admissions (18‐39 y) (n = 997 569) |
Middle‐aged admissions (40‐64 y) (n = 3 227 664) |
Elderly admissions (65+ y) (n = 4 523 855) |
|
|---|---|---|---|---|
| Age, mean (SD) | 8.1 (5.4) | 30.0 (6.1) | 53.5 (6.5) | 77.2 (7.9) |
| Female gender, N (%) | 94 270 (45.8) | 534 353 (53.6) | 1 638 091 (50.8) | 2 519 381 (55.7) |
| Payer, N (%) | ||||
| None | 4722 (2.3) | 120 592 (12.1) | 210 296 (6.5) | 16 623 (0.4) |
| Medicare | 56 (0.3) | 83 591 (8.4) | 702 867 (21.8) | 4 088 077 (904) |
| Medicaid | 115 641 (56.1) | 324 205 (32.5) | 683 600 (21.2) | 67 675 (1.5) |
| Private insurance | 76 124 (36.9) | 397 277 (39.8) | 1 430 938 (44.3) | 291 520 (6.4) |
| Self‐pay/other | 8720 (4.2) | 69 132 (6.9) | 192 956 (6.0) | 56 194 (1.2) |
| No. of chronic conditions, N (%) | ||||
| 0 | 59 280 (28.8) | 142 946 (14.3) | 108 399 (3.4) | 28 501 (0.6) |
| 1 | 66 466 (32.3) | 188 480 (18.9) | 245 652 (7.6) | 106 276 (2.4) |
| 2‐3 | 51 570 (25.0) | 323 571 (32.4) | 732 414 (22.7) | 582 543 (12.9) |
| ≥4 | 28 731 (13.9) | 342 572 (34.3) | 2 141 199 (66.3) | 3 806 535 (84.1) |
| Top 5 discharge diagnoses (%) | Asthma (10.7) | Trauma (10.1) | Heart condition (13.1)b | Heart condition (16.9)b |
| Trauma (8.9) | Gallbladder/liver disease (6.9) | Osteoarthritis/joint disease (6.0) | Trauma (6.9) | |
| Epilepsy/seizures (6.4) | Systemic infection (6.3) | Systemic infection (5.8) | Systemic infection (6.8) | |
| Pneumonia (6.2) | Skin disorders (4.8) | Cancer (5.8) | Osteoarthritis/joint disease (6.4) | |
| Appendicitis (4.6) | Heart condition (4.5)b | COPD/pulmonary disease (4.7) | COPD/pulmonary disease (6.2) | |
Admission characteristics for pediatric patients hospitalized in a subset of 235 nonspecialty hospitals treating both pediatric and adult patients.
Heart condition includes myocardial infarction, angina, heart failure, conduction disorders, cardiomyopathy, and valve disorders.
The median hospital 30‐day RSRRs (interquartile range) for pediatric, young adult, middle‐aged adult, and elderly adult cohorts overall were 6.2 percent (5.4 percent‐7.6 percent), 9.5 percent (9.0 percent‐10.1 percent), 11.0 percent (10.2 percent‐11.9 percent), and 13.0 percent (11.9 percent‐14.1 percent), respectively. Elderly adult RSRRs were strongly correlated with middle‐aged adult RSRRs (Pearson R 2 .67 [95% confidence interval (CI) 0.63‐0.68]), moderately correlated with young adult RSRRs (Pearson R 2 .38 [95% CI 0.34‐0.42]), and not correlated with pediatric RSRRs (Pearson R 2 0.10 [95% CI −0.03‐0.23]) (Figures 1 and S4). This stepwise relationship between age and correlation strength was consistent across every hospital characteristic (Table 3). RSRRs were more strongly correlated in large hospitals and teaching hospitals in all comparisons (P < .05). There were no consistent differences in the strength of RSRR correlations by hospital ownership or across Medicaid tertiles.
Figure 1.
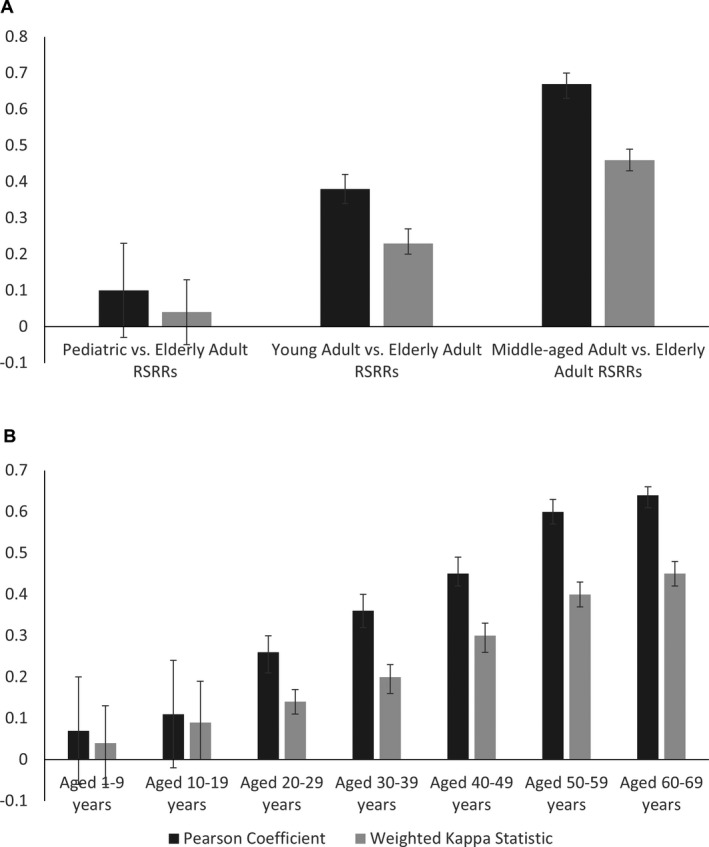
Pearson correlation coefficients and weight Cohen's kappa statistics comparing (A) pediatric, young adult, and middle‐aged adult RSRRs to elderly adult RSRRs, and (B) age decile RSRRs to age ≥70 y RSRRs. Comparisons between pediatric and elderly adult RSRRs in (A) and between RSRRs for patients aged 1‐9 y and 10‐19 y with RSRRs for patients aged ≥70 y in (B) are performed in pediatric/adult sample (n = 287 hospitals). All other comparisons were performed in adult sample (n = 1760)
Table 3.
Pearson correlation coefficients for middle‐aged adult, young adult, and pediatric RSRRs compared with elderly adult RSRRs by hospital characteristics
|
Pediatric (1‐17 y) vs elderly adults (≥65 y) RSRRs |
Young adults (18‐39 y) vs elderly adults (≥65 y) RSRRs (n = 1760)b |
Middle‐aged adults (40‐64 y) vs elderly adults (≥65 y) RSRRs (n = 1760)b | |||||||
|---|---|---|---|---|---|---|---|---|---|
| R 2 (95% CI) | P c | P d | R 2 (95% CI) | P c | P d | R 2 (95% CI) | P c | P d | |
| All | .10 (−0.03, 0.23) | — | — | .38 (0.34, 0.42) | — | — | .67 (0.63, 0.68) | — | — |
| Hospital ownership | |||||||||
| Public (A) | .11 (−0.16, 0.37) | — | — | .43 (0.33, 0.51) | — | — | .68 (0.62, 0.74) | — | — |
| Private, not‐for‐profit (B) | .14 (−0.02, 0.29) | .85 | — | .34 (0.28, 0.39) | .09 | — | .61 (0.57, 0.65) | .05 | — |
| Private, for‐profit | −.05 (−0.40, 0.31) | .50 | .35 | .41 (0.32, 0.50) | .76 | .20 | .71 (0.65, 0.76) | .46 | .005 |
| Location/Teaching status | |||||||||
| Metropolitan teaching (A) | .13 (−0.02, 0.28) | — | — | .52 (0.46, 0.58) | — | — | .79 (0.76, 0.82) | — | — |
| Metropolitan, nonteaching (B) | −.01 (−0.29, 0.27) | .40 | — | .38 (0.31, 0.44) | .002 | — | .71 (0.67, 0.74) | .002 | — |
| Nonmetropolitan | −.03 (−0.41, 0.36) | .47 | .94 | .25 (0.17, 0.33) | <.001 | .01 | .50 (0.44, 0.56) | <.001 | <.001 |
| Bed size | |||||||||
| Small/medium (A) | −.08 (−0.29, 0.15) | — | — | .30 (0.25, 0.35) | — | — | .61 (0.58, 0.65) | — | — |
| Large | .19 (0.03, 0.34) | .05 | — | .55 (0.49, 0.61) | <.001 | — | .77 (0.74, 0.80) | <.001 | — |
| % Medicaid, tertile | |||||||||
| Lowest (A) | .29 (0.08, 0.49) | — | — | .33 (0.26, 0.40) | — | — | .58 (0.52, 0.63) | — | — |
| Middle (B) | .06 (−0.16, 0.27) | .14 | — | .40 (0.33, 0.46) | .17 | — | .68 (0.64, 0.72) | .004 | — |
| Highest | .06 (−0.17, 0.28) | .14 | 1.00 | .41 (0.34, 0.48) | .11 | .84 | .72 (0.68, 0.76) | <.001 | .18 |
Abbreviations: CI, confidence interval; IQR, interquartile range; RSRR, risk‐standardized readmission rate.
Pediatric vs elderly adult RSRR comparisons performed in subset of 235 nonspecialty hospitals treating both pediatric and adult patients.
Median RSRR (IQR) for pediatric, young adult, middle‐aged adult, and elderly adult cohorts overall was 6.2% (5.4%, 7.6%), 9.5% (9.0%, 10.1%), 11.0% (10.2%, 11.9%), and 13.0% (11.9%, 14.1%), respectively.
P‐value for comparison with reference category (A).
P‐value for comparison with reference category (B).
Nearly identical findings were observed with measures of interquartile agreement and Kappa statistics (Table 4). Nearly half of hospitals were in the same quartile of performance for middle‐aged and elderly adult RSRRs compared with only 20 percent‐30 percent of hospitals when comparing pediatric and elderly adult RSRRs. Weighted Kappa statistics were consistently highest for middle‐aged vs elderly adult RSRRs (Kappa statistic range: 0.33‐0.57) and lowest for pediatric vs elderly adult RSRRs (Kappa statistic range: −0.10‐0.19) overall and across all hospital characteristics.
Table 4.
Weighted kappa statistics for middle‐aged adult, young adult, and pediatric RSRRs compared with elderly adult RSRRs by hospital characteristics
| Pediatric (1‐17 y) vs elderly adults (≥65 y) RSRRs (n = 235)a | Young adults (18‐39 y) vs elderly adults (≥65 y) RSRRs (n = 1760) | Middle‐aged adults (40‐64 y) vs elderly adults (≥65 y) RSRRs (n = 1760) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Same quartile (Q1‐Q4) n (%) |
Same quartile (Q1 or Q4) n (%) |
Opposite quartile (Q1 and Q4) n (%) |
Weighted Kappa (95% CI) |
Same quartile (Q1‐Q4) n (%) |
Same quartile (Q1 or Q4) n (%) |
Opposite quartile (Q1 and Q4) n (%) |
Weighted Kappa (95% CI) |
Same quartile (Q1‐Q4) n (%) |
Same quartile (Q1 or Q4) n (%) |
Opposite quartile (Q1 and Q4) n (%) |
Weighted Kappa (95% CI) |
|
| All | 62 (26.4) | 29 (16.5) | 27 (15.3) | 0.04 (−0.05, 0.13) | 627 (35.6) | 377 (29.5) | 103 (8.1) | 0.23 (0.20, 0.27) | 833 (47.3) | 526 (43.8) | 33 (2.8) | 0.46 (0.43, 0.49) |
| Hospital ownership | ||||||||||||
| Public | 21 (39.6) | 11 (29.0) | 5 (13.2) | 0.19 (−0.02, 0.40) | 113 (33.0) | 73 (29.2) | 19 (7.6) | 0.22 (0.14, 0.30) | 154 (45.0) | 103 (44.2) | 7 (3.0) | 0.45 (0.38, 0.51) |
| Private, not‐for‐profit | 36 (23.8) | 20 (17.2) | 13 (11.2) | 0.04 (−0.07, 0.15) | 367 (33.4) | 215 (26.5) | 73 (9.0) | 0.20 (0.16, 0.25) | 498 (45.3) | 312 (40.9) | 26 (3.4) | 0.44 (0.40, 0.48) |
| Private, for‐profit | 6 (19.4) | 1 (4.4) | 5 (21.7) | −0.06 (−0.27, 0.15) | 122 (38.4) | 68 (30.4) | 24 (10.7) | 0.26 (0.18, 0.34) | 154 (48.4) | 90 (40.9) | 6 (2.7) | 0.49 (0.42, 0.56) |
| Location/Teaching Status | ||||||||||||
| Metropolitan teaching | 40 (25.0) | 20 (16.3) | 17 (13.8) | 0.07 (−0.04, 0.18) | 217 (39.2) | 132 (33.3) | 25 (6.3) | 0.33 (0.27, 0.39) | 298 (53.9) | 187 (51.7) | 6 (1.7) | 0.56 (0.52, 0.61) |
| Metropolitan, nonteaching | 13 (26.5) | 6 (16.2) | 7 (18.9) | 0.04 (−0.15, 0.24) | 213 (33.0) | 129 (26.8) | 36 (7.5) | 0.20 (0.15, 0.26) | 302 (46.8) | 189 (42.2) | 7 (1.6) | 0.47 (0.42, 0.51) |
| Nonmetropolitan | 9 (34.6) | 4 (21.1) | 3 (15.8) | 0.14 (−0.14, 0.42) | 188 (33.5) | 105 (26.1) | 52 (12.9) | 0.15 (0.08, 0.21) | 223 (39.7) | 137 (34.1) | 21 (5.2) | 0.33 (0.27, 0.39) |
| Bed size | ||||||||||||
| Small/medium | 19 (24.4) | 7 (12.7) | 14 (25.5) | −0.10 (−0.26, 0.06) | 389 (32.5) | 228 (25.9) | 88 (10.0 | 0.17 (0.13, 0.22) | 544 (45.4) | 338 (40.8) | 31 (3.7) | 0.43 (0.39, 0.47) |
| Large | 45 (28.7) | 25 (21.9) | 17 (14.9) | 0.12 (0.01, 0.23) | 225 (40.0) | 143 (35.7) | 18 (4.5) | 0.35 (0.29, 0.41) | 317 (56.4) | 195 (53.6) | 4 (1.1) | 0.57 (0.52, 0.62) |
| % Medicaid, tertile | ||||||||||||
| Lowest | 21 (27.3) | 12 (19.7) | 7 (11.5) | 0.14 (−0.01, 0.30) | 196 (33.6) | 115 (26.9) | 39 (9.1) | 0.20 (0.14, 0.25) | 269 (46.1) | 169 (42.3) | 15 (3.8) | 0.45 (0.40, 0.50) |
| Middle | 16 (20.0) | 10 (15.4) | 8 (12.3) | −0.02 (−0.17, 0.13) | 213 (35.7) | 127 (29.2) | 34 (7.8) | 0.23 (0.17, 0.29) | 274 (46.0) | 175 (42.6) | 10 (2.4) | 0.44 (0.39, 0.50) |
| Highest | 20 (26.0) | 10 (17.2) | 9 (15.5) | 0.04 (−0.12, 0.20) | 209 (36.0) | 125 (30.1) | 39 (9.4) | 0.26 (0.20, 0.31) | 294 (50.7) | 180 (46.2) | 10 (2.6) | 0.52 (0.46, 0.56) |
Abbreviations: CI, confidence interval; IQR, interquartile range; RSRR, risk‐standardized readmission rate.
Pediatric vs elderly adult RSRR comparisons performed in subset of 235 nonspecialty hospitals treating both pediatric and adult patients.
When age cohorts were divided into smaller age deciles, there was again a stepwise relationship between correlation coefficients and weighted Kappa statistics for age‐specific RSRRs compared with RSRRs for patients aged ≥70 years old (Figures 1 and S5). The strongest associations between RSRRs were observed among the older age cohorts, and associations among the younger pediatric cohorts compared with patients aged ≥70 years were nonsignificant (Table S1).
In sensitivity analyses, replication of the adult analyses in the pediatric/adult sample or with the pediatric algorithm did not substantively change the results (Table S2). Similarly, when we repeated the analyses with reinclusion of the 57 and 32 specialty hospitals in the adult and pediatric/adult samples, respectively, and with the 2013 NRD database, the results were nearly identical. The strongest associations between RSRRs were observed again between middle‐aged vs elderly adult patients and the weakest associations between pediatric vs elderly adult patients. Analyses limited to index admissions for primary infections showed a similar pattern with comparable Pearson coefficient and weighted Cohen's Kappa statistic magnitudes.
4. DISCUSSION
In this large, national, all‐payer sample of patients of all ages, we found that 30‐day RSRRs for elderly adult patients were strongly correlated with middle‐aged adult RSRRs, moderately correlated with young adult ones, and not correlated with pediatric ones. This direct relationship between age and RSRR correlation strength was consistent across all hospital characteristics and when we used smaller age increments. Thirty‐day RSRRs were more strongly correlated in large hospitals and teaching hospitals. Our findings suggest that hospital all‐condition 30‐day RSRRs for elderly adult patients may capture broader aspects of hospital performance in other adult patients but may be less reflective of performance among pediatric patients.
There are several potential explanations for the high correlation between elderly adult and middle‐aged adult RSRRs. First, hospital efforts to avoid condition‐specific penalties for Medicare patients in the HRRP may have led to hospital‐wide improvements with positive effects for other populations. For instance, one study found improvements in both Medicare and Medicaid readmissions after implementation of the HRRP.24 Readmission processes such as discharge planning, care coordination, and medication reconciliation tend to be implemented at a hospital level across all adult patients, and thus, younger adult patients may benefit from hospital readmission reduction efforts aimed at Medicare patients.23 Indeed, qualitative studies of hospital quality officers have repeatedly identified system‐level readmission reduction efforts being implemented in US hospitals.25, 26, 27, 28 Examples of hospital‐wide strategies include investing in better health information technology, recruiting pharmacists for medication reconciliation and social workers to help with care transitions,29 leveraging electronic health records to share discharge summaries with community providers,30 and creating a hospital‐based, postdischarge clinic for patients to follow‐up in a timely manner.31 Even in the absence of hospital‐wide readmission reduction efforts, similar teams and services care for adult patients of different ages, presumably delivering similar quality of care to all patients regardless of age or condition. Prime examples of rotating teams are resident house staff and nurses who move between services, adapting new structures and processes to apply to other patient populations. In fact, this may explain why in our study the correlation between adult RSRRs was strongest in large, teaching hospitals, where residents play a critical role in patient care. Notably, hospital ownership or payer did not seem to affect correlation between RSRRs across age cohorts, suggesting that these hospital factors are less likely to explain age cohort differences. Moreover, there may be factors extrinsic to the hospital (eg, community resources) that facilitate access to outpatient services or home health care, improve health literacy, or address other social determinants of health such as housing, food, and transportation.32
An alternative explanation for the strong correlation between middle‐aged and elderly adult RSRRs but moderate correlation between young and elderly adult RSRRs stems from the similarity in discharge diagnoses between middle‐aged and elderly adult patients. The most common discharge diagnoses for middle‐aged adults closely mirrored those of elderly adults; however, there was minimal overlap in discharge diagnoses between young and elderly adults (Table 2). When we limited analyses to a subgroup of infection discharge diagnoses, the magnitude of the Pearson correlation coefficients and weighted Cohen's Kappa statistics was comparable to those for the overall sample, suggesting that differences in discharge diagnoses across age cohorts do not solely explain the findings. We chose infections because they are common across all age‐groups; however, it is possible that we might see stronger correlations between age‐specific RSRRs for conditions penalized under the HRRP if hospitals implement readmission reduction efforts specific to these conditions.33, 34
In contrast, the absent association between pediatric and elderly adult RSRRs is likely explained by the financial and administrative separation of pediatric and adult departments at most hospitals. There are a few examples of quality improvement initiatives that transcend both pediatric and adult care,35, 36, 37, 38 but most pediatric and adult services operate in silos with little cross‐pollination of house staff, clinicians, or resources.39 As a result, interventions such as discharge phone calls or home nursing visits may not be implemented across adult and pediatric populations. Although there are meaningful distinctions between adult and pediatric health systems (eg, lower prevalence of chronic illness in children, key role of family in child health, and higher percentage of children insured by Medicaid), there are also many similarities between health systems that suggest that lessons learned about readmissions in adults can apply to efforts to improve children's health care.35 In fact, readmission reduction efforts in pediatric and adult hospitals have focused on the same areas of care coordination, medication reconciliation, communication between providers, home visits, and allocation of resources for patients with psychosocial needs.27, 28
Our results on the suitability and limitations of readmission measures for profiling hospital performance in other patient populations have policy implications. Our data suggest that the current publicly reported CMS hospital‐wide readmission measure may not be a good surrogate for overall hospital quality among all patient populations, especially for hospitals with a substantial proportion of pediatric patients. This is in accordance with another study that found nonconcordance between hospital performance on readmissions for patients with CMS‐penalized conditions and for other patient populations.40, 41 Since the passage of the HRRP, Medicaid and private insurers have been incorporating readmission measures into quality assessments and provider profiling.17, 42, 43, 44 Currently, all states are required to report Medicaid readmission rates for patients ≥18, but they use different algorithms for reporting rates. As readmission measures expand to other insurers and patient populations, we demonstrate that the readmission rates in one patient population do not reflect hospital performance on readmissions across all patient populations. For instance, the pediatric readmission measure may be a better marker of quality than the CMS hospital‐wide measure in hospitals with a large percentage of pediatric patients. Attempts to characterize readmissions across all age‐groups will likely require multiple age‐specific calculations for hospital comparisons.
This study has several limitations. First, the pediatric/adult sample included mostly larger, teaching hospitals. Although we repeated the analyses stratified by hospital characteristics, our findings comparing pediatric and adult readmission rates may not be generalizable to all hospitals. Likewise, we included many small‐volume hospitals in the adult sample. Readmission estimates in small‐volume hospitals are less reliable than in large‐volume hospitals, which may limit our ability to detect correlations in this group. Second, we adjusted for a subset of patient characteristics in risk‐standardized measures and therefore may be omitting other measures of patient severity that account for differences in hospital readmission rates. Specifically, we used the all‐condition readmission measure developed for use in Medicare populations to calculate RSRRs for younger patients. Although there is significant overlap in diagnoses among adult patients, particularly middle‐aged and elderly adults, the Medicare model may not adjust for all relevant patient characteristics in younger adult populations. Third, unlike the Medicare all‐condition readmission model, we adjusted for diagnoses on the index hospitalization only rather than including diagnoses from the year prior because we lacked multiple years of data. Although additional NRD years are available, individual patients are not linkable across years. Finally, it is possible that the correlations for readmission across age‐groups are attributable to hospital characteristics not related to quality, such as coding practices, distribution of payers, or interhospital transfer rates.
Overall, we found that although hospital readmission rates for elderly adults, currently used for public reporting and hospital comparisons, may reflect broader hospital performance in middle‐aged and young adult populations, they are less indicative of hospital performance in pediatric populations. The robustness of our findings across hospital characteristics and smaller age categories suggests that this relationship is widespread. Further work is needed to understand the current state of readmission reduction efforts across hospital departments and how to best target these efforts in all age‐groups—particularly as we continue to expand readmission measures to other conditions and populations and as insurers move further toward accountable care organizations and bundled payments.
Supporting information
ACKNOWLEDGMENT
Joint Acknowledgment/Disclosure Statement: Dr. Mark Schuster and Dr. Sara Toomey are supported by the U.S. Department of Health and Human Services Agency for Healthcare Research and Quality and Centers for Medicare and Medicaid Services, CHIPRA Pediatric Quality Measures Program Centers of Excellence under grant numbers U18 HS 020513 (principal investigator: Dr. Schuster) and U18 HS 025299 (principal investigator: Dr. Toomey). The content is solely the responsibility of the authors and does not represent the official views of the Agency for Healthcare Research and Quality. No other disclosures.
Bucholz EM, Toomey SL, Butala NM, Chien AT, Yeh RW, Schuster MA. Suitability of elderly adult hospital readmission rates for profiling readmissions in younger adult and pediatric populations. Health Serv Res. 2020;55:277–287. 10.1111/1475-6773.13269
REFERENCES
- 1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360:1418‐1428. [DOI] [PubMed] [Google Scholar]
- 2. Joynt KE, Jha AK. A path forward on Medicare readmissions. N Engl J Med. 2013;368:1175‐1177. [DOI] [PubMed] [Google Scholar]
- 3. Centers for Medicare and Medicaid Services . Hospital compare. 2016. https://www.medicare.gov/hospitalcompare/search.html.Accessed April 12, 2017.
- 4. Srivastava R, Keren R. Pediatric readmissions as a hospital quality measure. JAMA. 2013;309:396‐398. [DOI] [PubMed] [Google Scholar]
- 5. Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30‐day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355‐363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Krumholz HM, Hsieh A, Dreyer RP, Welsh J, Desai NR, Dharmarajan K. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS ONE. 2016;11:e0160492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30‐day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407‐413. [DOI] [PubMed] [Google Scholar]
- 8. Lindenauer PK, Bernheim SM, Grady JN, et al. The performance of US hospitals as reflected in risk‐standardized 30‐day mortality and readmission rates for Medicare beneficiaries with pneumonia. J Hosp Med. 2010;5:e12‐e18. [DOI] [PubMed] [Google Scholar]
- 9. Zuckerman RB, Sheingold SH, Epstein AM. The Hospital readmissions reduction program. N Engl J Med. 2016;375:494. [DOI] [PubMed] [Google Scholar]
- 10. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374:1543‐1551. [DOI] [PubMed] [Google Scholar]
- 11. Wasfy JH, Zigler CM, Choirat C, Wang Y, Dominici F, Yeh RW. Readmission rates after passage of the Hospital Readmissions Reduction Program: a pre‐post analysis. Ann Intern Med. 2017;166:324‐331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Campione JR, Smith SA, Mardon RE. Hospital‐level factors related to 30‐day readmission rates. Am J Med Qual. 2017;32:48‐57. [DOI] [PubMed] [Google Scholar]
- 13. Mellor J, Daly M, Smith M. Does it pay to penalize hospitals for excess readmissions? Intended and unintended consequences of Medicare's Hospital Readmissions Reductions Program. Health Econ. 2017;26:1037‐1051. [DOI] [PubMed] [Google Scholar]
- 14. Weiss AJ, Elixhauser A. Overview of Hospital Stays in the United States, 2012: Statistical Brief #180. Rockville, MD: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs; 2014. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb180-Hospitalizations-United-States-2012.pdf. Accessed March 20, 2017. [Google Scholar]
- 15. Fischer C, Lingsma HF, Marang‐van de Mheen PJ, Kringos DS, Klazinga NS, Steyerberg EW. Is the readmission rate a valid quality indicator? A review of the evidence. PLoS ONE. 2014;9:e112282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jha AK.The 30‐day readmission rate: Not a quality measure but an accountability measure. An ounce of evidence. 2013. https://blogs.sph.harvard.edu/ashish-jha/2013/02/14/the-30-day-readmission-rate-not-a-quality-measure-but-an-accountability-measure.Accessed March 20, 2017.
- 17. Core set of adult health care quality measures for Medicaid (adult core set): technical specifications and resource manual for federal fiscal year 2017 reporting. Centers for Medicare and Medicaid Services; 2017. https://www.medicaid.gov/medicaid/quality-of-care/downloads/medicaid-adult-core-set-manual.pdf. Accessed September 9, 2017.
- 18. Boston Children's Hospital . Readmissions. 2016. http://www.childrenshospital.org/research-and-innovation/research/centers/center-of-excellence-for-pediatric-quality-measurement-cepqm/cepqm-measures/pediatric-readmissions.Accessed May 15, 2017.
- 19. Introduction to the HCUP Nationwide Readmissions Database (NRD) 2014. Rockville, MD: Agency for Healthcare Research and Quality; 2016. https://www.hcup-us.ahrq.gov/db/nation/nrd/NRD_Introduction_2014.jsp. Accessed February 17, 2017 [Google Scholar]
- 20. Nationwide Readmissions Database Known Data Issues, 2010‐2014. Rockville, MD: Agency for Healthcare Research and Quality; 2013. https://www.hcup-us.ahrq.gov/db/nation/nrd/NRDKnownDataIssues.pdf. Accessed February 17, 2017. [Google Scholar]
- 21. Horwitz LI, Partovian C, Lin Z, et al. Development and use of an administrative claims measure for profiling hospital‐wide performance on 30‐day unplanned readmission. Ann Intern Med. 2014;161:S266‐S275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Horwitz L, Partovian C, Lin Z, et al. Hospital‐wide (all‐condition) 30‐day risk‐standardized readmission measure. Centers for Medicare and Medicaid Services; 2013. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed February 17, 2017.
- 23. Fisher RA. On the ‘probable error’ of a coefficient of correlation deduced from a small sample. Metron. 1921;1:3‐32. [Google Scholar]
- 24. Ferro EG, Secemsky EA, Wadhera RK, et al. Patient readmission rates for all insurance types after implementation of the hospital readmissions reduction program. Health Aff (Millwood). 2019;38:585‐593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155:520‐528. [DOI] [PubMed] [Google Scholar]
- 26. Ahmad FS, Metlay JP, Barg FK, Henderson RR, Werner RM. Identifying hospital organizational strategies to reduce readmissions. Am J Med Qual. 2013;28:278‐285. [DOI] [PubMed] [Google Scholar]
- 27. Silow‐Carroll S, Edwards JN, Lashbrook A. Reducing hospital readmissions: lessons from top‐performing hospitals. The Commonwealth Fund; 2011. http://www.commonwealthfund.org/publications/case-studies/2011/apr/reducing-hospital-readmissions. Accessed June 24, 2017.
- 28. Kanaan SB.Homeward bound: nine patient‐centered programs cut readmissions. California Healthcare Foundation; 2009. http://www.chcf.org/publications/2009/09/homeward-bound-nine-patientcentered-programs-cut-readmissions. Accessed June 24, 2017.
- 29. Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital‐based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172:1057‐1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157:417‐428. [DOI] [PubMed] [Google Scholar]
- 31. Rennke S, Nguyen OK, Shoeb MH, Magan Y, Wachter RM, Ranji SR. Hospital‐initiated transitional care interventions as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:433‐440. [DOI] [PubMed] [Google Scholar]
- 32. Herrin J, St Andre J, Kenward K, Joshi MS, Audet AM, Hines SC. Community factors and hospital readmission rates. Health Serv Res. 2015;50:20‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bradley EH, Curry L, Horwitz LI, et al. Hospital strategies associated with 30‐day readmission rates for patients with heart failure. Circ Cardiovasc Qual Outcomes. 2013;6:444‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Dharmarajan K, Krumholz HM. Strategies to reduce 30‐day readmissions in older patients hospitalized with heart failure and acute myocardial infarction. Curr Geriatr Rep. 2014;3:306‐315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Starmer AJ, O'Toole JK, Rosenbluth G, et al. Development, implementation, and dissemination of the I‐PASS handoff curriculum: a multisite educational intervention to improve patient handoffs. Acad Med. 2014;89:876‐884. [DOI] [PubMed] [Google Scholar]
- 36. Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371:1803‐1812. [DOI] [PubMed] [Google Scholar]
- 37. The Breakthrough Series: IHI's Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper. Boston: Institute for Healthcare Improvement, 2003. http://www.IHI.org. Accessed June 24, 2017.
- 38. Homer CJ, Kleinman LC, Goldman DA. Improving the quality of care for children in health systems. Health Serv Res. 1998;33:1091‐1109. [PMC free article] [PubMed] [Google Scholar]
- 39. Berenson RA, Bodenheimer T, Pham HH. Specialty‐service lines: salvos in the new medical arms race. Health Aff (Millwood). 2006;25:337‐343. [DOI] [PubMed] [Google Scholar]
- 40. Butala NM, Kramer DB, Shen C, et al. Applicability of publicly reported hospital readmission measures to unreported conditions and other patient populations: a cross‐sectional all‐payer study. Ann Intern Med. 2018;168:631‐639. [DOI] [PubMed] [Google Scholar]
- 41. Hoffert D, Pavich P.Measurement year 2016: hospital pay‐for‐performance guide. Bureau of Fiscal Management, Division of Healthcare Access and Accountability; 2015. https://www.forwardhealth.wi.gov/WIPortal/content/provider/medicaid/hospital/P4P_MY2016_040115.pdf. Accessed September 9, 2017.
- 42. Reducing Medicaid Readmissions in Illinois: Moving Forward Together. Naperville, IL: The Institute for Innovations in Care and Quality; 2015. http://www.ihatoday.org/uploadDocs/1/reducingmedicaidreadmissions4-9-15.pdf. Accessed September 9, 2017. [Google Scholar]
- 43. Colorado Department of Health Care Policy and Financing .HQIP 30‐day all cause readmission. 2016. https://www.colorado.gov/pacific/sites/default/files/2016%2520March%2520HQIP%252030-day%2520all-cause%2520readmission%2520measure.pdf.Accessed September 9, 2017.
- 44. New York State Department of Health Medicaid Redesign Team .Delivery system reform incentive payment (DSRIP): measure specification and reporting manual. 2016. https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/2016/docs/2016-07-25_measure_specific_rpting_manual.pdf.Accessed September 9, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


