Abstract
Purpose
Sepsis is a leading cause of hospital deaths. Inter-hospital transfer is frequent in sepsis and is associated with increased mortality. Some sepsis patients undergo two inter-hospital transfers (double transfer). This study assessed the (1) prevalence, (2) associated risk factors, (3) associated mortality, and (4) hospital length-of-stay and costs of double-transfer of sepsis patients.
Materials and Methods
Retrospective cohort study using 2005-2014 administrative claims data in Iowa. Multivariable generalized estimating equations adjusted for potential confounding variables, with a primary outcome of mortality. Secondary outcomes included hospital length-of-stay and costs. Hospital-specific cost-to-charge ratios estimated hospital costs. Hospitals were categorized into quintiles based on sepsis-volume.
Results
Of 15,182 sepsis subjects, there were 45.2% non-transfers and 2.1% double-transfers. Double-transfers had worse mortality than non-transfers but not single-transfers. Of the non-transfers, 44.9% presented to a top sepsis-volume hospital compared to 22.8% of double-transfers and 25.1% of single-transfers. After transfer from first to second hospital, 93.4% of the single-transfers and 92.2% of the double-transfers were at a top sepsis-volume hospital. Double-transfers had longer length-of-stay and more in total hospital costs than single-transfers.
Conclusions
Double-transfer occurs in 2.1% of Iowa sepsis patients. Double-transfers had similar mortality and increased length of stay and costs compared to single-transfers.
Keywords: Sepsis, Critical Care, Patient Transfer, Delivery of Health Care, Emergency Medicine
BACKGROUND
Sepsis is a leading cause of death in U.S. hospitals [1, 2] with a mortality rate more than 25%.[2-7] Hospitals managing higher volumes of sepsis cases have been associated with lower sepsis mortality rates.[6, 8-12] Inter-hospital transfer is one strategy used to move sepsis patients to high-volume centers.[13-16] However, most studies demonstrating this volume-mortality association exclude transferred patients.[5, 6, 8-12] Paradoxically, several studies suggest that sepsis patients undergoing inter-hospital transfer have higher mortality than those who were not transferred.[5, 14, 15, 17-20]
In inter-hospital transfer, a principal concern is delayed treatment, [8, 14, 15, 17, 20-25] since treatment delays significantly worsen sepsis prognosis.[8, 14, 21-23] Previously, we found most sepsis patients in a midwestern state were transferred.[14] Notably, some patients underwent a second inter-hospital transfer (double-transfer).[14] Double-transfer increases exposure to inter-hospital transfer risks from the repeat transfer, multiple handoffs, and family burden of higher hospital cost and often further distance from home.[19] The presence of double-transfer exemplified another main concern in inter-hospital transfer—whether the current transfer process in sepsis is able to systematically route patients to hospitals with higher quality sepsis care.[26] Selection of an optimal level of care is not well described in sepsis, [15, 26-29] and inappropriate initial selection of a hospital without resources to meet the patients’ care needs may lead to double-transfer.
This study is the first study to analyze double-transfer transfer in sepsis care. The objectives of this study were to assess (1) the prevalence of double-transfer in patients diagnosed with sepsis in a Midwestern state (2) risk factors associated with double-transfer, and (3) the association between double-transfer and mortality, hospital length-of-stay, and hospital costs. We hypothesize that double-transfer patients will have worse mortality, increased hospital length-of-stay, and increased hospital costs.
METHODS
Study Design, Setting, and Selection of Participants
This study is a retrospective cohort analysis of adult sepsis patients in Iowa. Cases of sepsis were obtained from administrative claims data between January 1, 2005 and December 31, 2014. The majority of hospitals are located in rural areas (80%), do not have a dedicated critical care physician (25%), have a sepsis protocol, order set, or care plan (89%), and do not have written or unwritten criteria in place for transfer of sepsis patients (44%).[30] Those without a diagnosed infection at hospital arrival and those whose final transfer was more than one week after initial presentation were excluded. Under waiver of informed consent, the local Institutional Review Board approved this study. Reporting of this project adhered to Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines.[31]
As previously described, a probabilistic linkage algorithm was used to identify transferred subjects.[14] Utilizing sequential matching, the algorithm considered date of visit, subject birthdate, sex, zip code and county of residence. Social security number broke nonmatching linkages. Visits separated by one day were included if the discharge disposition indicated inter-hospital transfer, since this likely represented transfer that crossed midnight. Records (10%) were checked manually to verify the algorithm’s ability to detect linkages.[14]
Methods and Measurements
Definitions
Sepsis and Source of Infection were identified by the associated International Classification of Diseases, 9th edition, Clinical Modification (ICD-9-CM) discharge diagnosis codes.[3] Sepsis was defined using the previously described, prospectively validated Angus method which uses criteria based on the ICD-9-CM diagnostic codes.[1, 3, 32] This sepsis definition identifies subjects diagnosed with concomitant infection and organ failure during the same hospitalization and additionally were diagnosed with infection in the emergency department.[3, 14] Comorbidities were defined as 29 diseases included in the Elixhauser index, identified by the associated ICD-9-CM diagnoses. The Elixhauser method has been widely accepted as a tool using dichotomous variables of comorbidity presence to adjust for comorbidity burden.[33, 34] To describe the hospitals in which subjects were seen, the first, second, and third hospitals were referred to as Index hospital, Second hospital, and Final hospital respectively. Transfer order was determined by date of admission and disposition codes. Sepsis-volume was determined by the annual number of sepsis patients admitted to the hospital. Hospitals were categorized into quintiles based on sepsis-volume; if in the highest quintile, the site is a top sepsis-volume hospital. Emergency Department volume was similarly determined based on overall volume of patients seen, and hospitals were again categorized into quintiles. Rurality of a subject’s residence was based on the classification of the zip code of residence by the Rural Urban Commuting Area codes.[35] Medically Underserved Area is a designation given to the area a subject listed as their residence based on data from the US Census and Department of Health and Human Services. The medically underserved area designation is based on the number of primary care physicians, residents with income below the poverty level, elderly residents ( ≥ 65 years), and the infant mortality rate.[36] Critical Access Hospital is a designation given by the Center for Medicare and Medicaid services to hospitals serving rural communities. Procedures at each hospital were identified using Current Procedural Terminology© codes and dichotomized (procedure/no procedure) for each hospital. Surgery was classified using the Surgery Flag software, developed by the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project. This classification program uses Current Procedural Terminology© and ICD-9 -CM codes to identify surgical procedures; the Broad definition was used.[37]
Exposure
The primary exposure of interest was number of inter-hospital transfers. Subjects were divided into three categories based on the number of hospital transfers: (1) non-transfer, (2) single-transfer, and (3) double-transfer. For this study, double-transfer subjects were considered the exposed group, and single-transfer subjects were the comparison group. Single-transfer was defined by a disposition code describing discharge with transfer to a separate institution that could then be linked to an inpatient visit at the receiving hospital. Double-transfer was similarly defined as subjects with two distinct discharge codes each with transfer to another hospital and two subsequent inpatient visits at both receiving hospitals.
Outcomes
The primary outcome of this study was in-hospital mortality. In-hospital mortality included mortality in any hospital prior to discharge from the final hospital. Secondary outcomes were total length-of-stay (from initial visit to final discharge) and total healthcare costs.
Mapping
Distances were calculated using a previously described method utilizing GoogleMaps Application Programming Interface. [14] Briefly, driving distance was estimated from subject residence, defined as geographic centroid of the Zip Code Tabulation Area, to hospital location(s).
Costs
Healthcare costs were estimated using cost-to-charge ratios.[14] Similar to the Healthcare Research and Quality Healthcare Cost and Utilization Project, cost-to-charge ratios were estimated for each hospital based on annual financial statements, adjusted for inflation (according to inflation rates of the Consumer Price Index for medical costs). Total costs included all medical costs. Costs are reported in USD$2010.
Availability of Data and Materials
The data set analyzed in this study is not publicly available, because of protected health information, the data use agreement requirements for this dataset, and the possibility of subject identification in rural communities.
Analysis
Descriptive statistics were calculated by number of transfers and total study cohort. Univariate tests, chi-square and Wilcoxon-Mann-Whitney, were used to compare demographic and facility characteristics by exposure status.
Identification of Risk Factors for Double-Transfer.
A generalized logit model (binomial distribution, logit link) was used to identify subject and facility characteristics associated with double-transfer compared to a referent group of single-transfer (α <0.20). Candidate risk factors, identified in univariate regression, were included in a multivariable generalized logit model to estimate magnitude of risk, adjusting for other risk factors. Robust standard errors were used with clustering on the index hospital.
Association between Transfer Status and Outcomes.
Generalized estimating equations (binomial distribution and logit link) with robust standard errors clustered on index hospital were used to estimate the association between double-transfer status and hospital mortality. Unadjusted associations were presented. Then, multivariable models were constructed using the following criteria: (1) hypothesized association of covariate based on clinical reasoning and previous literature, (2) association of covariate and outcome (α <0.20), and (3) minimization of Akaike Information Criterion (AIC). Collinearity and statistical interactions were assessed for each outcome. For the secondary outcomes of cost and length-of-stay, generalized estimating equations models with a linear model and a log-transformed model were used (identity link with exchangeable correlation matrix). If estimates of the linear and log-transformed models were similar in direction and significance, an a priori decision was made to use the linear model, as it maximized interpretability of coefficients.
Sensitivity Analyses.
Two sensitivity analyses were performed to test the robustness of the results to the study population. The first sensitivity analysis reviewed the entire sepsis population (including those with infections that were not present on admission and late transfers). The second sensitivity analysis included the subset of subjects with infections that were not present on admission (while still excluding late transfers).
All statistical analyses were completed using SAS (version 9.4; SAS Institute, Inc., Cary, NC).
RESULTS
Characteristics of the Study Subjects
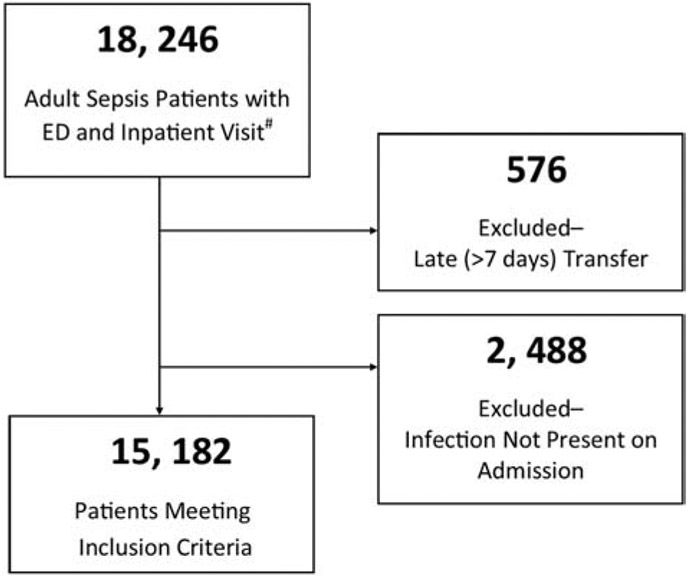
Over the ten-year study period, 23,067 adult severe sepsis or septic shock cases were identified. The majority of cases were successfully linked (79%, n= 18,246). Most failed linkages were cases that were likely transferred out of Iowa, as they presented at hospitals near state borders with neighboring large urban areas. Subjects with more than seven days elapsed between the initial encounter and the final transfer date, “late transfers,” (n=576) and subjects who did not have infection present on admission (n=2,488) were excluded (Figure 1). “Late transfers” might have been transferred for a non-sepsis related concern or care complication. Of the final study cohort (n=15,182), females compromised 50.3% and patients were predominately white (91.6%) and resided in a rural area (78.1%).
Figure 1.
Flowchart of Study Subjects.
#Cohort formation previously reported.14
Late transfer indicates greater than seven days between initial admit and final transfer date. Infection present on admission defined using Angus definition.
Main Results
Descriptive Analysis.
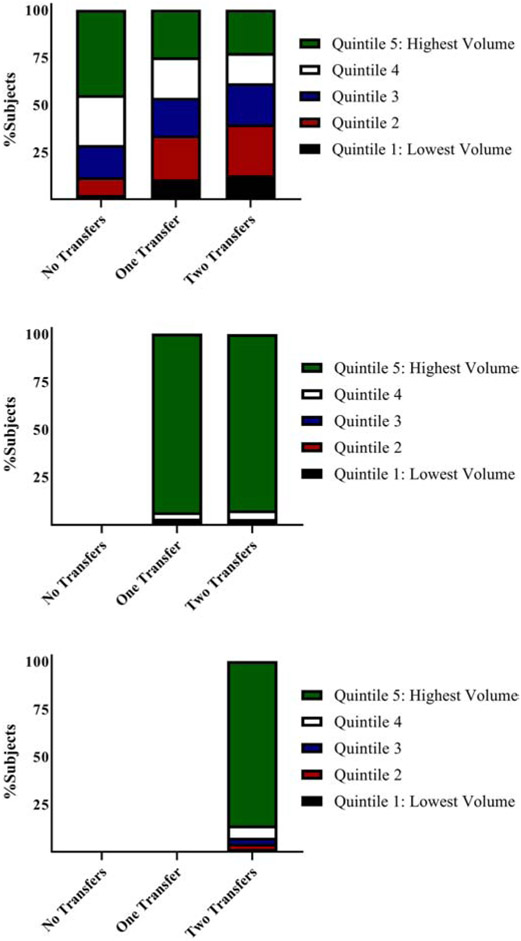
Overall, 54.8% (n= 8,325) of the cohort underwent inter-hospital transfer, 52.7% (n= 8,001) were single-transfer, and 2.1% (n= 324) were double-transfer (Table 1). A majority, 93.0% (n= 7,745) of all inter-hospital transfer subjects, were ultimately admitted at a top quintile sepsis-volume hospital (Figure 2). Of the non-transfer group, 44.9% presented to a top quintile sepsis-volume hospital. Initially, 25.1% of single-transfer and 22.8% of double-transfer subjects presented to a top quintile sepsis-volume hospital (Table 1 & Figure 2). After one transfer, 93.4% of single-transfer and 92.2% double-transfer subjects were at a top quintile sepsis-volume hospital however, double-transfer subjects underwent transfer once more. After the second transfer, most double-transfer subjects (86.1%) were at a top quintile sepsis-volume hospital as their final hospital.
Table 1.
Demographics of Study Participants by Transfer Frequency
| All | No Transfer |
Single Transfer |
Double Transfers |
|||||
|---|---|---|---|---|---|---|---|---|
| N (%) | 15 182 (100%) | 6 857 | (45.2) | 8 001 | (52.7) | 324 | (2.1) | |
| Age, n (%) | <0.001 | |||||||
| Median (IQR) | 74.0 (61.0 – 84.0) | 80.0 | (70.0 – 87.0) | 68.0 | (56.0 – 78.0) | 64.0 | (52.0 – 77.0) | |
| 18 – 50 years | 1 807 (11.9) | 463 | (6.8) | 1 271 | (15.9) | 73 | (22.5) | |
| 51 – 69 years | 4 291 (28.3) | 1 154 | (16.8) | 3 012 | (37.7) | 125 | (38.6) | |
| 70 – 81 years | 4 401 (28.3) | 2 063 | (30.1) | 2 259 | (28.2) | 79 | (24.4) | |
| 82+ years | 4 683 (30.9) | 3 177 | (46.3) | 1 459 | (18.2) | 47 | (14.5) | |
| Sex, n (%) | <0.001 | |||||||
| Female | 7 629 (50.3) | 3 611 | (52.7) | 3 863 | (48.3) | 155 | (47.8) | |
| Male | 7 553 (49.8) | 3 246 | (47.3) | 4 138 | (51.7) | 169 | (52.2) | |
| Race/Ethnicity, n (%) | <0.001 | |||||||
| African | 134 | (1.7) | 6 | (1.9) | ||||
| American/Black | 200 (1.3) | 60 | (0.9) | |||||
| White | 13 905 (91.6) | 6 404 | (93.4) | 7 198 | (90.0) | 304 | (93.8) | |
| Other/Missing | 1 077 (7.1) | 393 | (5.8) | 669 | (8.3) | 14 | (4.3) | |
| Insurance Type, n (%) | <.0001 | |||||||
| Public | 12 765 (84.1) | 6 266 | (91.4) | 6 236 | (77.9) | 263 | (81.2) | |
| Commercial | 1 893 (12.5) | 486 | (7.1) | 1 361 | (17.0) | 46 | (14.2) | |
| Uninsured/Self-Pay | 499 (3.3) | 96 | (1.4) | 389 | (4.9) | 14 | (4.3) | |
| Year, n (%) | <.0001 | |||||||
| 2005 | 787 (5.2) | 478 | (7.0) | 279 | (3.5) | 30 | (9.3) | |
| 2006 | 1 023 (6.7) | 611 | (8.9) | 373 | (4.7) | 39 | (12.0) | |
| 2007 | 1 244 (8.2) | 671 | (9.8) | 522 | (6.5) | 51 | (15.7) | |
| 2008 | 1 477 (9.7) | 724 | (10.6) | 728 | (9.1) | 25 | (7.7) | |
| 2009 | 1 609 (10.6) | 728 | (10.6) | 860 | (10.8) | 21 | (6.5) | |
| 2010 | 1 828 (12.0) | 898 | (13.1) | 900 | (11.3) | 30 | (9.3) | |
| 2011 | 1 927 (12.7) | 830 | (12.1) | 1 065 | (13.3) | 32 | (9.9) | |
| 2012 | 2 010 (13.2) | 792 | (11.6) | 1 183 | (14.8) | 35 | (10.8) | |
| 2013 | 2 094 (13.8) | 910 | (13.3) | 1 150 | (14.4) | 34 | (10.5) | |
| 2014 | 1 183 (7.8) | 215 | (3.1) | 941 | (11.8) | 27 | (8.3) | |
| Patient Rurality1 | <.0001 | |||||||
| Urban | 3 337 (22.0) | 1 630 | (23.8) | 1 650 | (20.6) | 57 | (17.6) | |
| Large Rural | 2 425 (16.0) | 622 | (9.1) | 1 737 | (21.7) | 66 | (20.4) | |
| Small Rural | 5 428 (35.8) | 2 668 | (38.9) | 2 654 | (33.2) | 106 | (32.7) | |
| Isolated Rural | 3 989 (26.3) | 1 934 | (28.2) | 1 960 | (24.5) | 95 | (29.3) | |
| Medically Underserved Area (MUA) | <.0001 | |||||||
| Yes | 4 260 (28.1) | 2 203 | (32.1) | 1 978 | (24.7) | 79 | (24.4) | |
| No | 9 384 (61.8) | 4 278 | (62.4) | 4 899 | (61.2) | 207 | (63.9) | |
| Unknown | 1 538 (10.1) | 376 | (5.5) | 1 124 | (14.1) | 38 | (11.7) | |
| Distance (mi.), Median (IQR) | ||||||||
| Index Hospital | 2.8 (0.9 – 13.6) | 2.7 | (0.7 – 13.7) | 2.8 | (1.0 – 12.8) | 14.6 | (1.6 – 50.5) | <.0001 |
| Final admitting Hospital | 26.7 (3.1 – 57.9) | 2.9 | (0.8 – 13.4) | 53.6 | (36.0 – 80.2) | 65.4 | (36.7 – 90.1) | <.0001 |
| Top-Decile Sepsis Hospital | 40.0 (25.7 – 65.6) | 44.1 | (25.2 – 72.4) | 39.2 | (26.3 – 57.9) | 40.0 | (28.6 – 57.9) | <.0001 |
| Total Transfer Distance (miles) | 22.9 (0.0 – 59.7) | 0 | (0 – 0) | 53.8 | (35.9 – 81.9) | 119.3 | (85.7 – 175.2) | <.0001 |
| First ED Cost (USD2010), Median (IQR) | $1,432 (926 – 2,200) | 1,287 | (859 – 1,962) | 1,562 | (994 – 2,404) | 1,502 | (1,050 – 2,303) | <.0001 |
| Source of Infection | ||||||||
| Abdominal | 838 (5.5) | 248 | (3.6) | 566 | (7.1) | 24 | (7.4) | <.0001 |
| Bloodstream | 1 107 (7.3) | 322 | (4.7) | 735 | (9.2) | 50 | (15.4) | <.0001 |
| Cellulitis/Soft Tissue | 1 265 (8.3) | 528 | (7.7) | 703 | (8.8) | 34 | (10.5) | 0.021 |
| Ear, Nose, Throat | 100 (0.7) | 41 | (0.6) | 54 | (0.7) | 5 | (1.5) | 0.117 |
| Gastroenteritis | 479 (3.2) | 229 | (3.3) | 242 | (3.0) | 8 | (2.5) | 0.426 |
| Meningitis | 100 (0.7) | 11 | (0.2) | 82 | (1.0) | 7 | (2.2) | <.0001 |
| Other | 6 791 (44.7) | 1 950 | (28.4) | 4 661 | (58.3) | 180 | (55.6) | <.0001 |
| Pneumonia | 5 808 (38.3) | 3 013 | (43.9) | 2 685 | (33.6) | 110 | (34.0) | <<.0001 |
| Osteomyelitis | 204 (1.3) | 39 | (0.6) | 157 | (2.0) | 8 | (2.5) | <<.0001 |
| UTI | 4 010 (26.4) | 2 361 | (34.4) | 1 578 | (19.7) | 71 | (21.9) | <.0001 |
| Surgical | 273 (1.8) | 55 | (0.8) | 205 | (2.6) | 13 | (4.0) | <.0001 |
| Co-morbidities (Elixhauser) | ||||||||
| Congestive Heart Failure | 3 690 (24.3) | 1 586 | (23.1) | 2 014 | (25.2) | 90 | (27.8) | 0.005 |
| Valvular Heart Disease | 1 031 (6.8) | 349 | (5.1) | 643 | (8.0) | 39 | (12.0) | <.0001 |
| Peripheral Vascular Disease | 1 379 (9.1) | 420 | (6.1) | 913 | (11.4) | 46 | (14.2) | <.0001 |
| Hypertension (complicated & uncomplicated) | 8 319 (54.8) | 3 414 | (49.8) | 4 709 | (58.9) | 196 | (60.5) | <.0001 |
| Paralysis | 522 (3.4) | 191 | (2.8) | 311 | (3.9) | 20 | (6.2) | <.0001 |
| Other Neurologic Disorders | 1 924 (12.7) | 974 | (14.2) | 915 | (11.4) | 35 | (10.8) | <.0001 |
| Diabetes Mellitus without Chronic Complications | 4 031 (26.6) | 1 639 | (23.9) | 2 291 | (28.6) | 101 | (31.2) | <.0001 |
| Diabetes Mellitus with Chronic Complications | 3 328 (21.9) | 1 242 | (18.1) | 2 009 | (25.1) | 77 | (23.8) | <.0001 |
| Liver Disease | 760 (5.0) | 174 | (2.5) | 560 | (7.0) | 26 | (8.0) | <.0001 |
| Lymphoma | 257 (1.7) | 81 | (1.2) | 168 | (2.1) | 8 | (2.5) | <.0001 |
| Metastatic Cancer | 480 (3.2) | 176 | (2.6) | 291 | (3.6) | 13 | (4.0) | 0.0007 |
| Solid Tumor without Metastasis | 605 (4.0) | 231 | (3.4) | 355 | (4.4) | 19 | (5.9) | 0.0009 |
| Rheumatoid arthritis/collagen vascular diseases | 576 (3.8) | 232 | (3.4) | 324 | (4.1) | 20 | (6.2) | 0.008 |
| Weight loss | 1 681 (11.1) | 386 | (5.6) | 1 246 | (15.6) | 49 | (15.1) | <.0001 |
| Fluid and electrolyte disorders | 8 658 (57.0) | 3 111 | (45.4) | 5 329 | (66.6) | 218 | (67.3) | <.0001 |
| Blood loss anemia | 240 (1.6) | 91 | (1.3) | 140 | (1.8) | 9 | (2.8) | 0.026 |
| Deficiency anemias | 4 824 (31.8) | 1 981 | (28.9) | 2 715 | (33.9) | 128 | (39.5) | <.0001 |
| Alcohol abuse | 582 (3.8) | 113 | (1.7) | 455 | (5.7) | 14 | (4.3) | <.0001 |
| Drug abuse | 216 (1.4) | 41 | (0.6) | 159 | (2.0) | 16 | (4.9) | <.0001 |
| Psychoses | 759 (5.0) | 338 | (4.9) | 405 | (5.1) | 16 | (4.9) | 0.933 |
| Depression | 2 015 (13.3) | 865 | (12.6) | 1 098 | (13.7) | 52 | (16.1) | 0.046 |
| Surgery during Hospital (Broad definition), n (%) | 3 476 (22.9) | 693 | (10.1) | 2 636 | (33.0) | 147 | (45.4) | <.0001 |
| Procedures | ||||||||
| First Hospital | 1 229 (8.1) | 475 | (6.9) | 724 | (9.1) | 30 | (9.3) | <.0001 |
| Second Hospital | 5 090 (61.1) | - | - | 4 989 | (62.4) | 101 | (31.2) | <.0001 |
| Third Hospital | 202 (62.4) | - | - | - | - | 202 | (62.4) | - |
| Total Length of Stay (days), Median (IQR) | 6.0 (3.0 – 10.0) | 4.0 | (3.0 – 6.0) | 8.0 | (5.0 – 13.0) | 10.0 | (7.0 – 16.0) | <.0001 |
| ED Volume – First ED | <.0001 | |||||||
| <20% | 1 318 (8.7) | 664 | (9.7) | 618 | (7.7) | 36 | (11.1) | |
| 20 – 39% | 2 488 (16.4) | 1 212 | (17.7) | 1 220 | (15.3) | 56 | (17.3) | |
| 40 – 59% | 3 588 (23.6) | 1 786 | (26.1) | 1 751 | (21.9) | 51 | (15.7) | |
| 60 – 79% | 3 860 (25.4) | 1 556 | (22.7) | 2 215 | (27.7) | 89 | (27.5) | |
| 80 – 89% | 1 494 (9.8) | 328 | (4.8) | 1 124 | (14.1) | 42 | (13.0) | |
| >90% | 2 434 (16.0) | 1 311 | (19.1) | 1 073 | (13.4) | 50 | (15.4) | |
| ED Volume – Second ED | <.0001 | |||||||
| <20% | 664 | (9.7) | * | * | * | * | ||
| 20 – 39% | 1 212 | (17.7) | * | * | * | * | ||
| 40 – 59% | 1 786 | (26.1) | * | * | * | * | ||
| 60 – 79% | 1 556 | (22.7) | 118 | (1.5) | 9 | (2.8) | ||
| 80 – 89% | 328 | (4.8) | 914 | (11.4) | 45 | (13.9) | ||
| >90% | 1 311 | (19.1) | 6896 | (86.2) | 169 | (83.0) | ||
| ED Volume – Last ED | <.0001 | |||||||
| <20% | 677 (4.5) | 664 | (9.7) | * | * | * | * | |
| 20 – 39% | 1 253 (8.3) | 1 212 | (17.7) | 31 | (0.4) | 10 | (3.1) | |
| 40 – 59% | 1 823 (12.0) | 1 786 | (26.1) | * | * | * | * | |
| 60 – 79% | 1 687 (11.1) | 1 556 | (22.7) | 118 | (1.5) | 13 | (4.0) | |
| 80 – 89% | 1 262 (8.3) | 328 | (4.8) | 914 | (11.4) | 20 | (6.2) | |
| >90% | 8 480 (55.9) | 1 311 | (19.1) | 6896 | (86.2) | 273 | (84.3) | |
| Critical Access Hospital – First Hospital | 10 254 (67.5) | 5 138 | (74.9) | 4 923 | (61.5) | 193 | (59.6) | <.0001 |
| Inpatient Sepsis Volume at first IP Hospital | <.0001 | |||||||
| <20% | 1 040 (6.9) | 158 | (2.3) | 842 | (10.5) | 41 | (12.7) | |
| 20 – 39% | 2 574 (17.0) | 636 | (9.3) | 1 851 | (23.2) | 87 | (26.9) | |
| 40 – 59% | 2 832 (18.7) | 1 174 | (17.1) | 1 588 | (19.9) | 70 | (21.6) | |
| 60 – 79% | 3 575 (23.6) | 1 812 | (26.4) | 1 711 | (21.4) | 52 | (16.1) | |
| 80 – 89% | 2 520 (16.6) | 1 411 | (20.6) | 1 084 | (13.6) | 25 | (7.7) | |
| >90% | 2 634 (17.4) | 1 666 | (24.3) | 919 | (11.5) | 49 | (15.1) | |
| Inpatient Sepsis Volume at 2nd IP Hospital | <.0001 | |||||||
| <20% | 158 | (2.3) | 73 | (0.9) | 7 | (2.2) | ||
| 20 – 39% | 636 | (9.3) | * | * | * | * | ||
| 40 – 59% | 1 174 | (17.1) | * | * | * | * | ||
| 60 – 79% | 1 812 | (26.4) | 274 | (3.4) | 15 | (4.6) | ||
| 80 – 89% | 1 411 | (20.6) | 564 | (7.1) | 28 | (8.6) | ||
| >90% | 1 666 | (24.3) | 6 902 | (86.3) | 271 | (83.6) | ||
| Inpatient Sepsis Volume at last IP Hospital | <.0001 | |||||||
| <20% | 236 (1.6) | 158 | (2.3) | 73 | (0.9) | 5 | (1.5) | |
| 20 – 39% | 739 (4.9) | 636 | (9.3) | 94 | (1.2) | 9 | (2.8) | |
| 40 – 59% | 1 277 (8.4) | 1 174 | (17.1) | 93 | (1.2) | 10 | (3.1) | |
| 60 – 79% | 2 107 (13.9) | 1 812 | (26.4) | 274 | (3.4) | 21 | (6.5) | |
| 80 – 89% | 1 988 (13.1) | 1 411 | (20.6) | 564 | (7.1) | 13 | (4.0) | |
| >90% | 8 834 (58.2) | 1 666 | (24.3) | 6 902 | (86.3) | 266 | (82.1) | |
| Inpatient-to-Inpatient Transfer (yes/no) (Only includes transferred subjects) | 2 628 (31.6) | - | - | 2 486 | (31.1) | 142 | (43.8) | <.0001 |
Patient rurality is based on the four category Rural Urban Commuting Area using the four-category classification.
Figure 2.
Inpatient Sepsis Volume of Hospitals by Transfer Status
Inpatient Sepsis Volume at First Hospital (Top); Second Hospital (Middle); Third Volume (Bottom).
Risk Factors for Double-transfer.
Table 2 describes patient and facility characteristics associated with increased odds of double-transfer compared to single-transfer. In an adjusted model controlling for other risk factors, younger age (18-50 years vs. 82+ years) (aOR 2.17 [95%CI 1.42 – 3.31]), procedure(s) at the second hospital (aOR 7.04 [95%CI 5.32 – 9.33]), and earlier year of encounter were the strongest risk factors for double-transfer compared to single-transfer (Table 2). The five most common procedures overall were: venous catheterization (ICD-9 code 3893), red blood cell transfusion (code 9904), continuous invasive mechanical ventilation < 96 hours (code 9671), insertion of endotracheal tube (code 9604), and diagnostic ultrasound of the heart (code 8872).
Table 2.
Risk Factors for Two Inter-Facility Transfers Compared to Single Transfers
| Unadjusted |
Adjusted |
|||||
|---|---|---|---|---|---|---|
| uOR | 95%CI | uOR | aOR | 95%CI | p-value | |
| Age, n (%) | ||||||
| 18 – 50 years | 1.84 | 1.25 – 2.69 | 0.002 | 2.17 | 1.42 – 3.31 | <0.001 |
| 51 – 69 years | 1.31 | 0.92 – 1.85 | 0.129 | 1.55 | 1.07 – 2.23 | 0.019 |
| 70 – 81 years | 1.11 | 0.77 – 1.61 | 0.571 | 1.11 | 0.76 – 1.63 | 0.586 |
| 82+ years (ref.) | 1.00 | - | - | 1.00 | - | - |
| Sex, n (%) | ||||||
| Female | 0.98 | 0.79 – 1.23 | 0.886 | - | ||
| Male (ref.) | 1.00 | - | - | - | ||
| Race/Ethnicity, n (%) | ||||||
| African American/Black | 1.02 | 0.44 – 2.36 | 0.955 | 0.92 | 0.38 – 2.23 | 0.849 |
| Hispanic/Latino (any race) | 0.89 | 0.12 – 6.63 | 0.912 | 1.42 | 0.16 – 12.50 | 0.749 |
| White (ref.) | 1.00 | - | - | 1.00 | - | - |
| Other/Missing | 0.52 | 0.30 – 0.90 | 0.019 | 0.32 | 0.18 – 0.58 | <0.001 |
| Insurance Type, n (%) | ||||||
| Public (ref.) | 1.00 | - | - | - | ||
| Commercial | 0.81 | 0.58 – 1.11 | 0.190 | - | ||
| Uninsured/Self-Pay | 0.87 | 0.50 – 1.51 | 0.623 | - | ||
| Other | 1.51 | 0.20 – 11.57 | 0.690 | - | ||
| Year, n (%) | ||||||
| 2005 (ref.) | 1.00 | - | - | 1.00 | - | - |
| 2006 | 0.96 | 0.58 – 1.60 | 0.884 | 0.83 | 0.48 – 1.49 | 0.502 |
| 2007 | 0.90 | 0.55 – 1.45 | 0.656 | 0.80 | 0.48 – 1.34 | 0.391 |
| 2008 | 0.31 | 0.18 – 0.55 | <0.001 | 0.34 | 0.19 – 0.61 | <0.001 |
| 2009 | 0.22 | 0.13 – 0.40 | <0.001 | 0.23 | 0.12 – 0.42 | <0.001 |
| 2010 | 0.30 | 0.18 – 0.52 | <0.001 | 0.34 | 0.19 – 0.60 | <0.001 |
| 2011 | 0.28 | 0.16 – 0.47 | <0.001 | 0.29 | 0.16 – 0.50 | <0.001 |
| 2012 | 0.27 | 0.16 – 0.45 | <0.001 | 0.28 | 0.16 – 0.49 | <0.001 |
| 2013 | 0.26 | 0.16 – 0.44 | <0.001 | 0.25 | 0.15 – 0.44 | <0.001 |
| 2014 | 0.26 | 0.15 – 0.47 | <0.001 | 0.14 | 0.08 – 0.25 | <0.001 |
| Patient Rurality1 | ||||||
| Urban (ref.) | 1.00 | - | - | 1.00 | - | - |
| Large Rural | 1.28 | 0.84 – 1.95 | 0.254 | 1.36 | 0.85 – 2.18 | 0.198 |
| Small Rural | 1.27 | 0.88 – 1.84 | 0.201 | 1.56 | 0.99 – 2.46 | 0.053 |
| Isolated Rural | 1.51 | 1.04 – 2.19 | 0.030 | 1.55 | 0.98 – 2.46 | 0.061 |
| Medically Underserved Area (MUA) | ||||||
| Yes | 1.03 | 0.77 – 1.38 | 0.849 | - | ||
| No (ref.) | 1.00 | - | - | - | ||
| Source of Infection | ||||||
| Abdominal | 0.85 | 0.52 – 1.41 | 0.537 | 0.64 | 0.38 – 1.11 | 0.111 |
| Bloodstream | 1.34 | 0.86 – 2.09 | 0.195 | 1.38 | 0.85 – 2.24 | 0.190 |
| Cellulitis/Soft Tissue | 1.24 | 0.82 – 1.88 | 0.310 | 1.15 | 0.74 – 1.80 | 0.528 |
| Ear, Nose, Throat | 0.68 | 0.09 – 5.01 | 0.704 | 0.60 | 0.07 – 5.23 | 0.641 |
| Gastroenteritis | 0.51 | 0.12 – 2.11 | 0.356 | 0.59 | 0.14 – 2.50 | 0.475 |
| Meningitis | 2.12 | 0.95 – 4.74 | 0.068 | 1.76 | 0.72 – 4.29 | 0.214 |
| Other | 0.68 | 049 – 0.93 | 0.015 | 0.77 | 0.55 – 1.09 | 0.139 |
| Pneumonia (ref.) | 1.00 | - | - | 1.00 | - | - |
| Osteomyelitis | 1.12 | 0.34 – 3.64 | 0.853 | 0.77 | 0.21 – 2.73 | 0.681 |
| UTI | 0.94 | 0.66 – 1.34 | 0.732 | 0.92 | 0.63 – 1.32 | 0.640 |
| Surgical | 0.94 | 0.66 – 1.34 | 0.732 | 1.18 | 0.61 – 2.26 | 0.629 |
| Co-morbidities (Elixhauser) | ||||||
| Congestive Heart Failure | 1.15 | 0.89 – 1.47 | 0.284 | - | ||
| Valvular Heart Disease | 1.59 | 1.12 – 2.24 | 0.009 | 1.59 | 1.10 – 2.30 | 0.014 |
| Peripheral Vascular Disease | 1.31 | 0.95 – 1.80 | 0.101 | 1.31 | 0.93 – 1.83 | 0.125 |
| Hypertension (complicated & uncomplicated) | 1.09 | 0.86 – 1.36 | 0.482 | - | ||
| Paralysis | 1.61 | 1.01 – 2.58 | 0.046 | 1.66 | 1.01 – 2.72 | 0.044 |
| Other Neurologic Disorders | 0.96 | 0.67 – 1.37 | 0.806 | - | ||
| Diabetes Mellitus without Chronic Complications | 1.13 | 0.88 – 1.43 | 0.335 | - | ||
| Diabetes Mellitus with Chronic Complications | 0.94 | 0.73 – 1.23 | 0.666 | - | ||
| Liver Disease | 1.13 | 0.75 – 1.72 | 0.549 | - | ||
| Lymphoma | 1.19 | 0.58 – 2.44 | 0.641 | - | ||
| Metastatic Cancer | 1.09 | 0.62 – 1.93 | 0.768 | - | ||
| Solid Tumor without Metastasis | 1.35 | 0.84 – 2.18 | 0.218 | - | ||
| Rheumatoid arthritis/collagen vascular diseases | 1.52 | 0.95 – 2.43 | 0.078 | 1.55 | 0.95 – 2.55 | 0.080 |
| Weight loss | 0.98 | 0.72 – 1.34 | 0.888 | - | ||
| Fluid and electrolyte disorders | 1.02 | 0.80 – 1.30 | 0.870 | - | ||
| Blood loss anemia | 1.60 | 0.81 – 3.18 | 0.177 | 1.70 | 0.81 – 3.57 | 0.160 |
| Deficiency anemias | 1.27 | 1.01 – 1.59 | 0.043 | 1.43 | 1.12 – 1.82 | 0.004 |
| Alcohol abuse | 0.74 | 0.43 – 1.29 | 0.291 | - | ||
| Drug abuse | 2.61 | 1.53 – 4.45 | <0.001 | 1.96 | 1.07 – 3.59 | 0.029 |
| Depression | 1.20 | 0.89 – 1.63 | 0.232 | - | ||
| Surgery during Hospital (Broad definition), n (%) | 1.70 | 1.36 – 2.13 | <0.001 | 2.35 | 1.79 – 3.07 | <0.001 |
| Procedures | ||||||
| First Hospital | 1.02 | 0.68 – 1.53 | 0.919 | - | ||
| Second Hospital | 3.91 | 3.06 – 5.00 | <0.001 | 7.04 | 5.32 – 9.33 | <0.001 |
| ED Volume – First ED | ||||||
| <20% | 1.28 | 0.75 – 2.20 | 0.371 | 1.07 | 0.27 – 4.31 | 0.922 |
| 20 – 39% | 0.97 | 0.59 – 1.59 | 0.905 | 0.97 | 0.26 – 3.68 | 0.970 |
| 40 – 59% | 0.59 | 0.35 – 0.97 | 0.039 | 0.62 | 0.18 – 2.19 | 0.458 |
| 60 – 79% | 0.83 | 0.52 – 1.32 | 0.425 | 1.00 | 0.37 – 2.69 | 0.998 |
| 80 – 89% | 0.88 | 0.51 – 1.54 | 0.658 | 1.08 | 0.48 – 2.43 | 0.854 |
| >90% (ref.) | 1.00 | - | - | 1.00 | - | - |
| Inpatient Sepsis Volume at first IP Hospital | ||||||
| <20% | 0.86 | 0.51 – 1.44 | 0.562 | 0.96 | 0.37 – 2.51 | 0.935 |
| 20 – 39% | 0.91 | 0.58 – 1.43 | 0.686 | 0.95 | 0.41 – 2.22 | 0.904 |
| 40 – 59% | 0.77 | 0.48 – 1.22 | 0.264 | 0.82 | 0.36 – 1.87 | 0.641 |
| 60 – 79% | 0.55 | 0.34 – 0.89 | 0.016 | 0.65 | 0.30 – 1.39 | 0.265 |
| 80 – 89% | 0.41 | 0.23 – 0.74 | 0.003 | 0.45 | 0.20 – 1.02 | 0.057 |
| >90% (ref.) | 1.00 | - | - | 1.00 | - | - |
| Critical Access Hospital | 0.34 | 0.20 – 0.58 | <0.001 | 0.86 | 0.38 – 1.97 | 0.724 |
This is a generalized logit model with a multinomial distribution clustered at the first hospital. The odds ratios can be interpreted as the odds of two transfer compared to one transfer (first column). (For example, in the unadjusted comparison, the odds of two or more transfers versus one transfer is 3.91 times greater for subjects undergoing procedure(s) at the second hospital compared to those that did not undergo a procedure at the second hospital.)
Double-transfer and Mortality, Length-of-Stay, and Costs
During the total hospital encounter, 13.8 % (n=2,089) subjects died. Among inter-hospital transfer subjects, 16.9% of single-transfer subjects died and 18.5% of double-transfer subjects died. Length of stay was higher for double-transfer subjects compared to single-transfer subjects (mean difference 2.97 days [95%CI 1.76 – 4.18]). Additionally, total encounter cost was higher for double-transfer compared to single-transfer subjects (mean difference $723 [95%CI 485 – 962]).
Double-transfer was not associated with higher hospital mortality when compared to single-transfer, even after adjustment for differences in risk and patient populations (aOR 1.23 [95%CI 0.95 – 1.61]) (Table 3). For the secondary outcomes, the log-transformed results were similar in direction and significance to linear model coefficients, so the linear models were reported (Table 3). After adjustment, double-transfer was associated with an average $10,691 (95%CI $5,737 – $15,646) greater total costs and increased length-of-stay of 2.86 days (95%CI 1.37 – 4.35) compared to single-transfer (Table 3).
Table 3.
Mortality, Cost, and Length of Stay for Double Transfer compared to Single Transfer
| B | 95%CI | p-value | B (adj)* | 95%CI | p-value | |
|---|---|---|---|---|---|---|
| Mortality | 1.11 | 0.86 – 1.44 | 0.408 | 1.23 | 0.95 – 1.61 | 0.155 |
| Total Cost (USD2010) | $8,840 | (3,345 – 14,335) | 0.002 | $10,691 | (5,737 – 15,646) | <0.001 |
| Log Total Cost# | 0.28 | (0.20 – 0.37) | <0.001 | 0.36 | (0.30 – 0.42) | <0.001 |
| Total LOS | 2.91 | 1.34 – 4.479 | <0.001 | 2.86 | 1.37 – 4.35 | 0.001 |
| Log Total LOS# | 1.27 | 1.16 – 1.39 | <0.001 | 1.27 | 1.18 – 1.38 | <0.001 |
Adjusted for: age (18-50, 51-69, 70-81, 82+), sex, year, rurality and medically underserved area (county level), source of infection, co-morbidities(alcohol use disorder, deficiency anemia, blood loss anemia, congestive heart failure, depression, diabetes mellitus without complications, diabetes mellitus with complications, hypertension, liver disease, lymphoma, electrolyte disorders, metastatic cancer, other neurologic disorders, peripheral vascular disease, tumor without metastasis, and weight loss), inpatient-to-inpatient transfer, initial ED costs (log-transformed), first hospital inpatient sepsis volume quintile, procedure at first hospital (y/n), and procedure at second hospital (y/n).
Coefficients are relative costs of twice-transfer compared to single transfer. For example, in the adjusted model, total costs of twice transferred patients are, on average, 1.43 greater than once transferred patients.
Sensitivity Analyses.
No association between double-transfer status and hospital mortality was observed when including late transfer subjects and subjects without infection present on admission (aOR 0.95 [95%CI 0.78 – 1.17]; p = 0.659). Results also did not change when including subjects without infection present on admission but who subsequently developed infection during the encounter (aOR 0.97 [95%CI 0.77 – 1.22]; p = 0.786) (Table S1).
DISCUSSION
Double-transfer occurs in 2.1% of sepsis patients in a Midwestern state. No difference in mortality was found between double-transfer and single-transfer patients, although double-transfer patients had longer length-of-stay and higher hospital costs. These findings highlight that patient-relevant outcomes may be worse in patients who undergo double-transfer than those whose care can be provided at the hospital they are transferred to initially.
Regarding double-transfer subjects, two sequences were observed in the second transfer: (1) the second transfer occurred between high-volume hospitals (amongst top-quintile or from top to 4th highest quintile hospitals), or (2) a small group of double-transfer patients (7.1%, n=23) were transferred from a top-quintile sepsis hospital to a hospital in the 3rd or lower sepsis-volume quintiles (e.g. back-transfer). Some sepsis patients in the double-transfer cohort (7.5%) were initially transferred to hospitals that were not high-volume hospitals, suggesting that inadequate resources were available at the first destination for comprehensive care. We hypothesize that a double-transfer patient is actually a patient who may have been inaccurately triaged at the time of the first hospital transfer.
Little guidance is provided on selecting the destination for inter-hospital transfer for sepsis patients.[38] Providers may rely on hospital volume as an indicator of sepsis capability, although outcomes and resources may still vary widely between top-volume institutions.[27] Some specialized services, such as hepatology, interventional radiology, or inpatient surgical specialties may not be available even in high volume hospitals, so if patients develop the need for these services they may require a second transfer. The relative success of regionalized networks, such as for trauma [39], and established associations between higher hospital volume and lower mortality [6, 8-12] reinforce that transferring to high volume hospitals will lead to improved outcomes[15, 26, 28, 40, 41], but hospital-specific capabilities are heterogeneous and contribute significantly to transfer-decision-making.[30] While hospital volume- sepsis mortality relationships are present, it is unclear whether transfer itself is associated with improved mortality, other than for resuscitated patients who have specific procedural or consultation needs.[5, 6, 8-12] [14, 15]
Regionalization networks are increasingly well established for high-mortality conditions such as trauma (hospital trauma level designations) and myocardial infarction.[42, 43] In myocardial infarction, a 9.4% reduction in 30-day mortality was found when double-transfer was prevented by avoiding initial transfer to an under-resourced hospital (i.e. without catheterization capability).[27] Trauma, stroke, critical care, and burn designations recognize that rapidly identifying patients who will benefit from the most comprehensive care can improve outcomes, and that risk stratifying both patients and hospital capabilities is a powerful strategy to better match patients with care facilities. Sepsis has a higher mortality rate than myocardial infarction,[44] but similar easily accessible sepsis hospital designations do not exist in the US. Double-transfer may occur due to the lack of sepsis-specific information to guide appropriate hospital selection and incomplete insight in the services that will be required for definitive care. An Interhospital Sepsis Code, a formal regionalization network, in Catalonia, Spain has developed a system of designated sepsis centers based on resources and capabilities to inform triage of sepsis patients.[45] In the US, formal regionalization networks and transfer protocols for sepsis care could reduce double-transfer by optimizing initial transfer triage for sepsis patients.
The largest risk factor for double-transfer was a procedure at the 2nd hospital. This could also demonstrate how double-transfer may occur due to the heterogenous presentation and management of sepsis. Providers may believe the benefit of transfer to another institution where specialists were more likely available would outweigh the risks of transfer especially when a patient’s management was complicated by factors such as procedural intervention. As the patient progressed and a procedure (such as surgical intervention or central line placement)[46] was considered, secondary transfer was performed.
Targeted approaches that could simplify transfer destination decisions and reduce unnecessary transfers include: (1) establishing easily accessible hospital data on sepsis-related resources (e.g. intensivist availability, ability to complete procedures such as a central line[46] through which “sepsis-capable hospitals” can be identified, (2) creating sepsis regionalization networks, or regional sepsis codes, (3) emphasizing the need to complete time sensitive interventions prior to transfer[5, 14, 24] (i.e. during the time at the referring facility which accounts for a large proportion of the transfer delay[24]) which may prevent patient deterioration that later requires repeat transfer to a higher capability hospital, and (4) identifying facility-level interventions (e.g. telemedicine) to close the outcome gap between higher and lower volume hospitals to allow more patients to be treated locally.[9, 47, 48]
Telemedicine has improved decision making with regards to appropriate patient and hospital selection in inter-hospital transfer, improved best practices adherence, and decreased complication rates.[21, 25, 49-51] Telemedicine could provide the bedside expertise of a specialist without exposing the patient to transfer but it may also be used to improve outcomes through improved triage or improved early care, even when transfer is indicated. Further, the volume-outcome relationship in sepsis has been hypothesized to be a surrogate indicator for best practice guideline adherence; local hospitals could improve adherence through telemedicine and the volume-outcome association may lessen.[9] Patients and families could stay closer to home [14, 50-52] health care resources would be better utilized, and local providers would increase their experience with diagnosis and treatment of sepsis.
This study has limitations. First, there may be residual confounding since our data was limited to administrative claims data utilized for billing purposes. Notably, severity of illness could not be included in our analysis due to the lack of physiological and clinical data (e.g. time to sepsis bundle component initiation, vasopressor dose, mechanical ventilation).[14] However, double-transfer subjects may have lived longer or were more stable and therefore were able to undergo double-transfer. That improved health status could contribute to a survival bias. To minimize this risk of bias, we adjusted for proxies of severity of illness by using a validated comorbidity index. Selection bias is a major concern in most studies of inter-hospital transfer in sepsis, as there is a possibility that the inter-hospital transfer group had increased severity of illness. In this study, our main comparison was between double-transfer and single-transfer subjects; both cohorts were composed of subjects chosen for transfer. Therefore, the risk of selection bias is greatly reduced, as both groups likely had a range of illness severities necessitating transfer to an outside hospital. -Further, single-transfer was used as a comparison group, as this population is likely to have fewer differences in unmeasured covariates with the double-transfer group than the population that was not transferred. Second, inaccurate coding practices allow the possibility of ascertainment bias, or inaccurately estimating incidence.[1] We used a validated method of identifying sepsis from ICD-9-CM codes to minimize this effect.[1, 3, 32] Although the term severe sepsis is not used currently, we mention this diagnosis as it is was used for coding purposes in IC9-CM. Third, another limitation comes from the use of all-cause mortality and transfer. The data did not indicate whether death or transfer was sepsis-specific. To limit the inclusion of deaths and transfers unrelated to sepsis, subjects were only included if their final transfers occurred within one week of the initial hospital presentation making it more likely that both transfer and mortality were sepsis-related. Fourth, it is possible that the power to detect a difference in mortality was limited for this study and may be susceptible to Type II error. Finally, our data was from one primarily rural Midwestern state, and outcomes may vary in other regions with different healthcare systems and case mixes.
CONCLUSION
Double-transfer occurs in 2.1% of severe sepsis and septic shock patients. Minimizing double-transfer through improved triage decision-making could be an opportunity to reduce cost, decrease length-of-stay, and limit exposure to transfer risks, including mortality. While transfer may ultimately be the best option for a specific patient, routing decisions (particularly those made at the initial hospital) should minimize unnecessary transfers. Future studies should assess decision making in double-transfer (including patient selection and hospital destination), double-transfer prevalence and patterns in other settings, and the effect of interventions such as telemedicine and sepsis regionalization networks on double-transfer.
Supplementary Material
Highlights:
Double-transfer occurs in 2.1% of severe sepsis and septic shock patients
No mortality differences were observed between double-and single-transfer
Higher healthcare costs and length-of-stay were observed in double-transfer
Minimizing double-transfer could reduce the health care burden of sepsis
Acknowledgements
The authors would like to acknowledge Karisa K Harland PhD, MPH for her assistance with data management and interpretation and Kelli Wallace MS, CCRC for her assistance with manuscript review.
Funding: This work was supported by the Emergency Medicine Foundation; by the University of Iowa Department of Emergency Medicine; and by the Institute for Clinical and Translational Science at the University of Iowa, which is supported by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant U54TR001356. Dr. Mohr is additionally supported by funding from the Agency for Healthcare Research and Quality (grant K08HS025753). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
List of Abbreviations
- 95%CI
95% confidence interval
- aOR
Adjusted odds ratios
- ICD-9-CM
International Classification of Diseases, 9th edition, Clinical Modification
Footnotes
Competing Interests: The authors have no competing interests to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Gaieski DF, Edwards JM, Kallan MJ, Carr BG. Benchmarking the incidence and mortality of severe sepsis in the United States. Critical care medicine 2013;41(5):1167–74. [DOI] [PubMed] [Google Scholar]
- [2].Doshi PB, Park AY, Banuelos RC, Akkanti BH, Darger BF, Macaluso A, et al. The Incidence and Outcome Differences in Severe Sepsis with and without Lactic Acidosis. J Emerg Trauma Shock 2018;11(3):165–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001;29(7):1303–10. [DOI] [PubMed] [Google Scholar]
- [4].Liu V, Escobar GJ, Greene JD, Soule J, Whippy A, Angus DC, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. Jama 2014;312(1):90–2. [DOI] [PubMed] [Google Scholar]
- [5].Ofoma UR, Dahdah J, Kethireddy S, Maeng D, Walkey AJ. Case Volume-Outcomes Associations Among Patients With Severe Sepsis Who Underwent Interhospital Transfer. Critical care medicine 2017;45(4):615–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Walkey AJ, Wiener RS. Hospital case volume and outcomes among patients hospitalized with severe sepsis. American journal of respiratory and critical care medicine 2014;189(5):548–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, Mcginley E, et al. Nationwide trends of severe sepsis in the 21st century (2000-2007). Chest 2011;140(5):1223–31. [DOI] [PubMed] [Google Scholar]
- [8].Gaieski DF, Edwards JM, Kallan MJ, Mikkelsen ME, Goyal M, Carr BG. The relationship between hospital volume and mortality in severe sepsis. Am J Respir Crit Care Med 2014;190(6):665–74. [DOI] [PubMed] [Google Scholar]
- [9].Goodwin AJ, Simpson KN, Ford DW. Volume-Mortality Relationships during Hospitalization with Severe Sepsis Exist Only at Low Case Volumes. Ann Am Thorac Soc 2015;12(8):1177–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kocher KE, Haggins AN, Sabbatini AK, Sauser K, Sharp AL. Emergency department hospitalization volume and mortality in the United States. Ann Emerg Med 2014;64(5):446–57 e6. [DOI] [PubMed] [Google Scholar]
- [11].Powell ES, Khare RK, Courtney DM, Feinglass J. Volume of emergency department admissions for sepsis is related to inpatient mortality: results of a nationwide cross-sectional analysis. Critical care medicine 2010;38(11):2161–8. [DOI] [PubMed] [Google Scholar]
- [12].Shahul S, Hacker MR, Novack V, Mueller A, Shaefi S, Mahmood B, et al. The Effect of Hospital Volume on Mortality in Patients Admitted with Severe Sepsis. PloS one 2014;9(9):e108754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Feazel L, Schlichting AB, Bell GR, Shane DM, Ahmed A, Faine B, et al. Achieving regionalization through rural interhospital transfer. The American journal of emergency medicine 2015;33(9):1288–96. [DOI] [PubMed] [Google Scholar]
- [14].Mohr NM, Harland KK, Shane DM, Ahmed A, Fuller BM, Torner JC. Inter-hospital transfer is associated with increased mortality and costs in severe sepsis and septic shock: An instrumental variables approach. J Crit Care 2016;36:187–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Rush B, Tyler PD, Stone DJ, Geisler BP, Walley KR, Celi LA. Outcomes of Ventilated Patients With Sepsis Who Undergo Interhospital Transfer: A Nationwide Linked Analysis. Critical care medicine 2018;46(1):e81–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Simpson SQ. Surviving Transfer for Sepsis: Size Matters-Or Does It? Critical care medicine 2017;45(4):749–50. [DOI] [PubMed] [Google Scholar]
- [17].Flabouris A, Hart GK, George C. Outcomes of patients admitted to tertiary intensive care units after interhospital transfer: comparison with patients admitted from emergency departments. Crit Care Resusc 2008;10(2):97–105. [PubMed] [Google Scholar]
- [18].Kozubal D, Liu A, Rinaldi J, Martin R, Healy M. Sepsis Patients Admitted From Limited Service Hospital ED To Tertiary ICU Are Twice As Likely To Die. Journal of Emergency Medicine 2016;50(6):925–6. [Google Scholar]
- [19].Mohr NM, Harland KK, Shane DM, Miller SL, Torner JC. Potentially Avoidable Pediatric Interfacility Transfer Is a Costly Burden for Rural Families: A Cohort Study. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 2016;23(8):885–94. [DOI] [PubMed] [Google Scholar]
- [20].Motzkus CA, Chrysanthopoulou SA, Luckmann R, Rincon TA, Lapane KL, Lilly CM. ICU Admission Source as a Predictor of Mortality for Patients With Sepsis. Journal of intensive care medicine 2018;33(9):510–6. [DOI] [PubMed] [Google Scholar]
- [21].Lilly CM, Cody S, Zhao H, Landry K, Baker SP, Mcilwaine J, et al. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. Jama 2011;305(21):2175–83. [DOI] [PubMed] [Google Scholar]
- [22].Pruinelli L, Westra BL, Yadav P, Hoff A, Steinbach M, Kumar V, et al. Delay Within the 3-Hour Surviving Sepsis Campaign Guideline on Mortality for Patients With Severe Sepsis and Septic Shock. Crit Care Med 2018;46(4):500–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Zilberberg MD, Shorr AF. Appropriate Antibiotic Treatment in Severe Sepsis and Septic Shock: Timing Is Everything. Crit Care Med 2015;43(10):2258–9. [DOI] [PubMed] [Google Scholar]
- [24].Faine BA, Noack JM, Wong T, Messerly JT, Ahmed A, Fuller BM, et al. Interhospital Transfer Delays Appropriate Treatment for Patients With Severe Sepsis and Septic Shock: A Retrospective Cohort Study. Crit Care Med 2015;43(12):2589–96. [DOI] [PubMed] [Google Scholar]
- [25].Campbell K VP, Wittrock a, Bell M, Skow B, Faine B, Harland K, Mohr N. Telemedicine Improves Timeliness and Appropriateness of Antibiotics in Rural Emergency Departments Medical Student Research Conference. University of Iowa Roy J. & Lucille A. Carver College of Medicine; 2017. [Google Scholar]
- [26].Iwashyna TJ, Christie JD, Moody J, Kahn JM, Asch DA. The structure of critical care transfer networks. Med Care 2009;47(7):787–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Critical care medicine 2012;40(8):2470–8. [DOI] [PubMed] [Google Scholar]
- [28].Kahn JM, Branas CC, Schwab CW, Asch DA. Regionalization of medical critical care: what can we learn from the trauma experience? Critical care medicine 2008;36(11):3085–8. [DOI] [PubMed] [Google Scholar]
- [29].Wedel SK, Orr RA, Frakes MA, Conn AK. Improving the incomplete infrastructure for interhospital patient transfer. Critical care medicine 2013;41(2):e21–2. [DOI] [PubMed] [Google Scholar]
- [30].Ilko SA, Vakkalanka JP, Ahmed A, Harland KK, Mohr NM. Central Venous Access Capability and Critical Care Telemedicine Decreases Inter-Hospital Transfer Among Severe Sepsis Patients: A Mixed Methods Design. Crit Care Med 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61(4):344–9. [DOI] [PubMed] [Google Scholar]
- [32].Iwashyna TJ, Odden A, Rohde J, Bonham C, Kuhn L, Malani P, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the angus implementation of the international consensus conference definition of severe sepsis. Med Care 2014;52(6):e39–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Austin SR, Wong Y-N, Uzzo RG, Beck JR, Egleston BL. Why Summary Comorbidity Measures Such As the Charlson Comorbidity Index and Elixhauser Score Work. Medical care 2015;53(9):e65–e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo Methods of Comorbidity Measurement in Administrative Data. Medical Care 2004;42(4):355–60. [DOI] [PubMed] [Google Scholar]
- [35].E.R.S. U.S. Department of Agriculture. ERS/USDA Briefing Room: Measuring Rurality: Rural-Urban Commuting Area Codes, http://www.ers.usda.gov/briefing/Rurality/RuralUrbanCommutingAreas/; 2010. [accessed 15 October 2017.
- [36].Goodwin AJ, Nadig NR, Mcelligott JT, Simpson KN, Ford DW. Where You Live Matters: The Impact of Place of Residence on Severe Sepsis Incidence and Mortality. CHEST 2016;150(4):829–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Surgery Flag Software, https://www.hcup-us.ahrq.gov/toolssoftware/surgflags/surgeryflags.jsp.
- [38].Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Jama 2016;315(8):801–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Mackenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 2006;354(4):366–78. [DOI] [PubMed] [Google Scholar]
- [40].Clay Mann N, Mullins RJ, Hedges JR, Rowland D, Arthur M, Zechnich AD. Mortality among seriously injured patients treated in remote rural trauma centers before and after implementation of a statewide trauma system. Med Care 2001;39(7):643–53. [DOI] [PubMed] [Google Scholar]
- [41].Esposito TJ, Sanddal TL, Reynolds SA, Sanddal ND. Effect of a voluntary trauma system on preventable death and inappropriate care in a rural state. J Trauma 2003;54(4):663–9; discussion 9-70. [DOI] [PubMed] [Google Scholar]
- [42].Mackenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A National Evaluation of the Effect of Trauma-Center Care on Mortality. New England Journal of Medicine 2006;354(4):366–78. [DOI] [PubMed] [Google Scholar]
- [43].Concannon TW, Nelson J, Goetz J, Griffith JL. A percutaneous coronary intervention lab in every hospital? Circ Cardiovasc Qual Outcomes 2012;5(1):14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006;34(6):1589–96. [DOI] [PubMed] [Google Scholar]
- [45].Yébenes JC, Lorencio C, Esteban E, Espinosa L, Badia JM, Capdevila JA, et al. Código Sepsis Interhospitalario en Catalunya: modelo organizativo territorial para la atención inicial al paciente con sepsis. Medicina Intensiva 2019. [DOI] [PubMed] [Google Scholar]
- [46].Ilko SA, Vakkalanka JP, Ahmed A, Harland KK, Mohr NM. Central Venous Access Capability and Critical Care Telemedicine Decreases Inter-Hospital Transfer Among Severe Sepsis Patients: A Mixed Methods Design. Critical care medicine 2019;47(5):659–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Djogovic D, Green R, Keyes R, Gray S, Stenstrom R, Sweet D, et al. Canadian Association of Emergency Physicians sepsis treatment checklist: optimizing sepsis care in Canadian emergency departments. Cjem 2012;14(1):36–9. [DOI] [PubMed] [Google Scholar]
- [48].O'shea AMJ, Fortis S, Vaughan Sarrazin M, Moeckli J, Yarbrough WC, Schacht Reisinger H. Outcomes comparison in patients admitted to low complexity rural and urban intensive care units in the Veterans Health Administration. Journal of critical care 2019;49:64–9. [DOI] [PubMed] [Google Scholar]
- [49].Damiani E, Donati A, Serafini G, Rinaldi L, Adrario E, Pelaia P, et al. Effect of performance improvement programs on compliance with sepsis bundles and mortality: a systematic review and meta-analysis of observational studies. PLoS One 2015;10(5):e0125827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Thorpe C, Vaughan L. Specialist not tertiary: Providing intensive care medicine in a district general hospital. Journal of the Intensive Care Society 2018;19(2):92–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Udeh C, Udeh B, Rahman N, Canfield C, Campbell J, Hata JS. Telemedicine/Virtual ICU: Where Are We and Where Are We Going? Methodist DeBakey cardiovascular journal 2018;14(2):126–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Bosk EA, Veinot T, Iwashyna TJ. Which patients and where: a qualitative study of patient transfers from community hospitals. Med Care 2011;49(6):592–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data set analyzed in this study is not publicly available, because of protected health information, the data use agreement requirements for this dataset, and the possibility of subject identification in rural communities.