Abstract
Aims
The risk of potential harms prompted the UK government to introduce the Psychoactive Substances Act in 2016. The aim of the present study was to evaluate the impact and effectiveness of this new legislation on patterns of novel psychoactive substance (NPS) awareness, use, experiences and risk awareness in a self‐selected sample of UK consumers to inform education and policy.
Methods
The Bristol Online Survey was advertised on the Bluelight drug forum and social media Facebook pages and University email between 7 January and 7 February 2015 (168 responses) and 9 March to 18 September 2017 (726 responses). UK country of residence responses were extracted for analysis (SPSS).
Results
In a predominantly university‐educated, young (< 25 years) self‐selecting sample, 1 year after introduction of the legislation, NPS use (in males, under 18s, those educated to school/college level, P < .001) has increased, whilst health risk awareness has not changed and remains poor. Users are switching to sourcing NPSs via street dealers (49%) and the darknet (31%) and showing an increase in preference for the herbal NPS Salvia divinorum (P < .05). The main reasons for NPS use remain the influence of friends (69%) in a social setting and to get high (76%) usually in combination with alcohol, cannabis or ecstasy.
Conclusion
Regulation alone, so far, has not impacted on health risk awareness, NPS drug demand and culture in our UK survey sample. Alongside regulation, NPS health promotion education (particularly in schools, colleges) is needed that addresses resilience and both the risks and beneficial effects of NPS.
Keywords: novel psychoactive substances, online survey, policy, psychoactive effects, Psychoactive Substances Act 2016, recreational use
What is already known about this subject
Government evaluation review of its 2016 Psychoactive Substances Act shows indications of reduced UK NPS use in the general population.
No systematic evaluation of the impact and effectiveness of the UK 2016 Psychoactive Substances Act on patterns of NPS use, experiences and health risk perception has been undertaken in vulnerable user groups.
What this study adds
UK NPS use in under 18, school/college educated males has increased, whilst reasons, motivations and health risk perceptions of NPS have not changed.
There is a shift to sourcing NPS from street dealers and the darknet and an increase in the harder to regulate herb Salvia dinivorium.
Statutory drug education programmes in schools providing resilience and risk management skills on drug use are needed alongside policy.
1. INTRODUCTION
The emergence of novel psychoactive substances (NPSs) has created a challenge for drug policy‐makers worldwide and a substantial global threat for public health. NPSs vary widely with inconsistent composition and potency often being significant factors in the health risks they pose. Up to 2017, over 60 countries have implemented legal responses to control NPS.1 The European Union (EU) Early Warning System currently monitors over 670 NPS.2 Various laws and controls have been created to tackle NPS diffusion across Europe3 and even though there is no uniform consensus, two trends are identifiable. First, in line with public opinion, there appears to be a general move towards the use of the threat of prison to deter suppliers4 and, second, it seems that countries are choosing not to use criminal sanctions for those possessing a new psychoactive substance for personal use.5
The UK is one of the biggest consumers of NPSs in Europe with frequent reports of serious clinical and public health issues, particularly for vulnerable groups (prisoners, teenagers, homeless).6 Although NPSs account for a small share of drug‐related harms in the UK, compared with traditional drugs,7, 8, 9 the management10 and severity of harms e.g. long‐term health issues prompted the UK government to bring in the Psychoactive Substances Act (PSA) 2016 banning the production, supply, importation and exportation of NPSs, but permitting possession (with some exemptions).11
The PSA 2016 does appear to have reduced UK‐based online NPS stores and offline retail headshops.7, 12 Furthermore during 2017, 51 new NPSs were detected in Europe,2 fewer than the previous 3 years, which may, in part, be due to measures taken by some national governments in Europe, such as the UK, to target producers and retailers of NPSs by prohibiting their open sale as legal highs. Despite this encouraging decline the overall number of NPSs available on the market continues to grow and there is evidence that high potency substances are increasing7, 13 and that legal markets are being displaced by alternative routes, such as street‐level drug dealing or crypto‐markets.7, 14 Prohibition will not address supply of NPSs via the largely untraceable area of the internet, especially the darknet, nor will it address drug demand—the basic human desire for seeking pleasure and altered states of consciousness. Worryingly, since 2014, the number of UK drug users who have bought their drugs from crypto markets has risen from 12 to 25%.15
Despite legislation being one of the primary means used to tackle NPS availability, no systematic evaluation of the impact and effectiveness of this UK ban on patterns of NPS use has been undertaken. Evidence of the impact and effectiveness of drugs policy enactment is captured by the number of drug‐related deaths and offences, drug seizures, forensics, clinical case reports, and emergency department presentations. Alongside these sources, surveying users helps build an in‐depth picture on the patterns of NPS use. However, few surveys capture NPSs users' perceptions of safety,16, 17 their motivations,18, 19, 20 preferences and settings for NPS use and importantly their educational background. The search for pleasure is what drives consumer markets for psychoactive drugs, both legal and illegal, but, at present, public policy gives no weight to preferences. For example, preferences for NPSs differ across European (prefer stimulants) and US (prefer cannabimimetics) markets.21 Understanding consumer reasons and motivations for NPS use would enhance government‐targeted prevention interventions to the appropriate target groups.18
It is, therefore, important that reliable and up‐to‐date survey data are available to inform education and policy in this area. We recently reported that public awareness of NPS and, importantly, perceptions of the potential health risks associated with NPS use was lacking in a small sample of predominantly university‐educated young people, mainly from the UK and Greece22 highlighting a need for governments to take responsibility for educating their own consumer markets, as well as protecting them with legislation. Our online survey presented in this paper was designed and ran in 2015 and then again in 2017 with two aims: first to provide data on the impact of the PSA 2016 Act on UK consumer awareness and use of NPSs; and second to provide data on UK consumer NPSs preferences, motivations, experiences and health perceptions. Some of these survey findings were presented at the VI International Novel Psychoactive Substances conference.23
2. METHODS
Following our previous study available online between 7 January and 7 February 2015 (168 responses obtained)22 our survey was updated to capture sourcing and setting for NPS use and relaunched online between 9 March and 18 September 2017 (726 responses). UK country of residence responses were extracted for analysis and comparison of NPS awareness and use in 2015 and 2017, 1 year before and 1 year after the introduction of the UK PSA 2016.
To elicit the views of individuals and to get a wide range of views in a short time, an online survey was considered the most appropriate method, having been previously used by the authors in order to obtain information on NPS.22 The survey was developed using Bristol Online Survey (www. http://survey.bris.ac.uk), a Web survey development service with wide readership. This product was used as it is freely available to the University of Hertfordshire, provides analytical tools, and is easy to use. The survey instrument was designed to capture patterns of NPS awareness (had they heard of NPS or legal highs), use, preference, motivations, experiences and health risk perceptions.
In the updated 2017 survey there were 38 structured questions split into 4 sections. The first 2 sections were mandatory (11 questions on demographics and NPS awareness, use, and perceived harms). Respondents were informed that they should only complete the third section if they had taken an NPS on at least 1 occasion in the past. Finally, the fourth section was specific to those that had taken https://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=4233 on at least 1 occasion in the past. A copy of the survey will be provided upon request.
The survey was in English and advertised on DS Daily News, the Bluelight drug forum (http://www.bluelight.org) and promoted using University email, social media Facebook pages (including UKC Psychedelics Society, University of Hertfordshire Bioscience society, Life and Medical Sciences international students, Psychedelic Experience). The survey was anonymous, took 15 minutes to complete and comprised questions requiring both restricted/categorical and/or open responses. Social media enabled easy and fast distribution of the survey through personal accounts and university groups. The drug forum was an important source for targeting drug users, but also individuals with an interest in drug‐related issues.
The inclusion criteria were the following: (i) no restriction in terms of age, gender, sexual orientation or region of participants; (ii) non‐users and users of NPS could take part in the research; and (iii) a good understanding of English was required for participants.
Descriptive statistics were performed to describe the basic features of data using the Bristol Online Survey tool. Chi‐square tests were used to assess whether changes in demographics (age, gender, sexual orientation, educational background and employment status) affected NPS awareness and use in 2015 and 2017. The significance level was set to *P < .05 after a Bonferroni correction. IBM SPSS Statistics (version 24) for MacOS Sierra 10.12.3 was used. A t test for independent proportions (z‐test) was used to compare the population proportional differences between the 2015 and 2017 independent samples and assess whether NPS awareness and use changed between 2015 and 2017. The significance level was set to # P < .05.
The study was approved by the University of Hertfordshire's Health and Human Sciences Research Institute Ethics Committee (PHAEC/1042 (02). Informed consent was assumed by individuals agreeing to proceed with the survey.
2.1. Nomenclature of targets and ligands
Key protein targets and ligands in this article are hyperlinked to corresponding entries in http://www.guidetopharmacology.org, the common portal for data from the IUPHAR/BPS Guide to PHARMACOLOGY.
3. RESULTS
The 2015 survey was completed by 168 respondents from 17 countries internationally over the 1‐month period it was online. The 2017 survey was completed by 726 respondents from 44 countries internationally during the 6‐month period that it was online. The responses from UK residents were extracted for our analysis.
3.1. Demographics of UK respondents
In the 2017 survey there were 500 UK (69%) respondents mainly from England (95%), a few from Scotland (2.8%) and Wales (2.2%); whilst in 2015 there were 58% UK respondents with no definition of specific regions. Despite the lower numbers of respondents in the 1‐month 2015 survey the demographics of both survey samples are largely the same (P > .05, Table 1), with the exception of significantly less respondents in the 18–25 aged group (54%) in 2017 sample compared with the 2015 sample (89%, P < .05), enabling comparison across the survey samples. The UK respondents in both samples (Table 1) are typically female, young (under 25 y), heterosexual and educated to higher education level. Further, the self‐selected subset of UK respondents is similar for each survey sample identified from University of Hertfordshire sources (2015, 51%; 2017, 63%) and social media sources (2015, 49%; 2017 31%), with few identified from specialised social media (e.g. DS Daily, 2015, 0%; 2017, 2%) and drug fora (2015, 0%; 2017, 4%).
Table 1.
Demographics of UK respondents (absolute n number and %) in the 2015 and 2017 survey sample
| Characteristics | 2015 | 2017 | P value (z‐test, 2015 vs 2017) | ||
|---|---|---|---|---|---|
| Total respondents (n = 98) | Total respondents (n = 500) | ||||
| n | % | n | % | ||
| Sex | |||||
| Male | 34 | 34.7 | 197 | 39.4 | >.05 |
| Female | 64 | 65.3 | 303 | 60.6 | >.05 |
| Age (y) | |||||
| <18 | 1 | 1 | 13 | 2.6 | >.05 |
| 18–25 | 87 | 88.8 | 269 | 53.8 | #<.05 |
| 26–35 | 5 | 5.1 | 90 | 18 | >.05 |
| 36–50 | 5 | 5.1 | 73 | 14.6 | >.05 |
| >50 | 0 | 0 | 55 | 11 | >.05 |
| < 25 combined | 88 | 89.8 | 282 | 56.4 | #< .05 |
| Sexual orientation | |||||
| Straight/heterosexual | 88 | 89.8 | 447 | 89.4 | >.05 |
| Homosexual | 5 | 5.1 | 20 | 4 | >.05 |
| Bisexual | 5 | 5.1 | 29 | 5.8 | >.05 |
| Other | 0 | 0 | 4 | 0.8 | >.05 |
| Highest level of education | |||||
| High school | 4 | 4.1 | 31 | 6.2 | >.05 |
| College | 9 | 9.2 | 63 | 12.6 | >.05 |
| Undergraduate studies | 71 | 72.4 | 266 | 53.2 | >.05 |
| Postgraduate studies | 13 | 13.3 | 137 | 27.4 | >.05 |
| Combined HE | 84 | 85.7 | 403 | 80.6 | >.05 |
Other denotes asexual, asexual, pansexual or preferred not to say. Significant population proportional difference
P < .05 (z‐test) in <25 and 18–25 age group between 2015 and 2017 survey sample.
3.2. Awareness of NPS
Gender, age and sexual orientation did not alter NPS awareness in both surveys (Table 2). The level of education influenced NPS awareness in 2015, where high school (75%) and undergraduates (80%) were more aware than college level (44%) and postgraduates (46%, P < .05). This was not the case in 2017 (P > .05), which reflects a significant increase in NPS awareness in postgraduate (83%) and college level (92%) respondents in 2017, compared with 2015 (P < .05, z‐test), although differences may reflect the lower numbers of respondents in the 2015 groups. Similarly, employment impacted NPS awareness in 2015, which was not the case in the larger 2017 groups, where the unemployed and employed were equally aware, although there was a trend to less NPS awareness in the unemployed group seeking work (77%, P = .07).
Table 2.
Novel psychoactive substance awareness (absolute number and %) of 2015 and 2017 UK survey respondents
| Novel psychoactive substance awareness | |||||||
|---|---|---|---|---|---|---|---|
| 2015 | 2017 | ||||||
| Number of responses (%) | P value (χ2) | Number of responses (%) | P value (χ2) | P value (z‐test, 2015 vs 2017) | |||
| Yes | No | Yes | No | ||||
| 71 (72%) | 27 (28%) | 434 (87%) | 66 (13%) | >.05 | |||
| Demographics | |||||||
| Sex | .637 | .223 | |||||
| Male | 26 (76%) | 8 (24%) | 176 (89%) | 21 (11%) | >.05 | ||
| Female | 45 (70%) | 19 (30%) | 258 (85%) | 45 (15%) | >.05 | ||
| Sexual orientation | .33 | .626 | |||||
| Straight/heterosexual | 62 (70%) | 26 (30%) | 386 (86%) | 61 (14%) | >.05 | ||
| Homosexual | 4 (80%) | 1 (20%) | 18 (90%) | 2 (10%) | >.05 | ||
| Bisexual | 5 (100%) | 0 (0%) | 27 (93%) | 2 (7%) | >.05 | ||
| Other | ‐ | ‐ | 3 (75%) | 1 (25%) | nd | ||
| Employment | *.031 | .076 | |||||
| Full time | 19 (90%) | 2 (10%) | 169 (86%) | 28 (14%) | >.05 | ||
| Part time | 22 (71%) | 9 (29%) | 134 (91%) | 13 (9%) | >.05 | ||
| Not employed (looking for work) | 9 (50%) | 9 (50%) | 37 (77%) | 11 (23%) | >.05 | ||
| Not employed (not looking for work) | 16 (84%) | 3 (16%) | 72 (85%) | 13 (15%) | >.05 | ||
| Other | 5 (56%) | 4 (44%) | 22 (96%) | 1 (4%) | # <.05 | ||
| Education | *.031 | .176 | |||||
| High school | 3 (75%) | 1 (25%) | 30 (97%) | 1 (3%) | >.05 | ||
| College | 4 (44%) | 5 (56%) | 58 (92%) | 5 (8%) | ##.01 | ||
| Undergraduate studies | 57 (80%) | 14 (20%) | 229 (86%) | 37 (14%) | >.05 | ||
| Postgraduate studies | 6 (46%) | 7 (54%) | 114 (83%) | 23 (17%) | # <.05 | ||
| Combined high school/college | 7 (54%) | 6 (46%) | 88 (94%) | 6 (6%) | ##.01 | ||
| Other | 1 (100%) | 0 (0%) | 3 (100%) | 0 (0%) | >.05 | ||
| Age | .131 | .191 | |||||
| <under 18 | 0 (0%) | 1 (100%) | 13 (100%) | 0 (0%) | ### <.001 | ||
| 18–25 | 65 (75%) | 22 (25%) | 228 (85%) | 41 (15%) | >.05 | ||
| 26–35 | 2 (40%) | 3 (60%) | 81 (90%) | 9 (10%) | # <.05 | ||
| 36–50 | 4 (80%) | 1 (20%) | 61 (84%) | 12 (16%) | >.05 | ||
| >over 50 | ‐ | ‐ | 51 (93%) | 4 (7%) | nd | ||
Other refers to: Sexual orientation: asexual, pansexual, preferred not to say; Employment: semi voluntary, freelancer, out of work due to injury, disabled, long‐term sick, study‐based practice; Education: qualified accountant ACCA, diploma, vendor qualifications. Significant difference
P < .05 χ2 test;
P < .05;
P < .01;
P < .001 population proportional difference between 2015 and 2017 (z‐test).
Overall NPS awareness was not significantly higher following the legislation (2015, 72% vs 2017, 87%, P > .05, z‐test), although the under 18 (2015, 0% vs 2017, 100%, P < .001) and 26–35 (2015, 40% vs 2017, 90%, P = .01) age groups and those educated to postgraduate (2015, 46% vs 2017, 83%, P < .05) and high school/college level (2015, 54% vs 2017, 94%, P = .01) educated were significantly more aware of NPS following the ban.
3.3. Use of NPS
In both surveys NPS use was higher in males (Table 3) despite males and females being equally NPS aware (Table 2). Forty‐eight percent of males vs only 13% females used NPSs in 2017 (P < .001) compared with 24% males vs 14% females in 2015 (P > .05). Sexual orientation did not alter NPS use (P > .05) whereas employment status significantly impacted NPS use in both surveys (P < .01). High school and college educated respondents reported significantly higher use of NPS in 2017 (58 and 52% respectively) compared with the higher educated groups of undergraduates (23%) and postgraduates (15%; P < .001). Despite a similar higher education demographic in both surveys, NPS use was not altered across different educational groups in 2015, which is likely to reflect the low number of high school and college educated respondents in the 2015 survey. Similarly, the significant effect of age on NPS use in 2017 (not seen in 2015) probably reflects the low number of respondents in the under 18 age group. In both surveys this age group had the smallest number of respondents (2015, 1%; 2017, 2.6%), which will skew the % of NPS use and awareness. In 2017 NPS use correlated with age, i.e. the highest proportion of NPS users was the 100% NPS aware under 18s (62%), followed by 26–35 age group (39%), 18–25 (25%), 36–50 (25%) and over 50 (13%; P < .001). Given the low numbers of respondents in the under 18 group when combined with the 18–25 age group NPS use of the under 25 s was comparable with the overall NPS use trend (2015, 18% vs 2017, 26%, P > .05). Although there was no significant change in overall NPS use since the legislation (2015, 17% 2017, 27%, P = .2, z‐test) there was an increased trend in overall NPS use in males (P = .12, 24–48%), under 18s (P = .11, 0–62%) and those educated to high school/college level (P = .12, 23–54%).
Table 3.
Novel psychoactive substance use (absolute number and %) of 2015 and 2017 UK survey respondents
| Novel psychoactive substance use | |||||||
|---|---|---|---|---|---|---|---|
| 2015 | 2017 | ||||||
| Number of responses (%) | P value (χ2) | Number of responses (%) | P value (χ2) | P value (z‐test, 2015 vs 2017) | |||
| Yes | No | Yes | No | ||||
| 17 (17%) | 81 (83%) | 134 (27%) | 366 (73%) | 0.248 | |||
| Demographics | |||||||
| Sex | .27 | *** < .001 | |||||
| Male | 8 (24%) | 26 (76%) | 95 (48%) | 102 (52%) | .12 | ||
| Female | 9 (14%) | 55 (86%) | 39 (13%) | 264 (87%) | >.05 | ||
| Sexual orientation | .572 | .319 | |||||
| Straight/heterosexual | 16 (18%) | 72 (82%) | 115 (26%) | 332 (74%) | >.05 | ||
| Homosexual | 0 | 5 (100%) | 6 (30%) | 14 (70%) | >.05 | ||
| Bisexual | 1 (20%) | 4 (80%) | 12 (41%) | 17 (59%) | >.05 | ||
| Other | 0 | 0 | 1 (25%) | 3 (75%) | >.05 | ||
| Employment | *.008 | ** < .01 | |||||
| Full time | 9 (43%) | 12 (57%) | 56 (28%) | 141 (72%) | >.05 | ||
| Part time | 5 (16%) | 26 (84%) | 28 (19%) | 119 (81%) | >.05 | ||
| Not employed (looking for work) | 1 (6%) | 17 (94%) | 16 (33%) | 32 (67%) | >.05 | ||
| Not employed (not looking for work) | 2 (11%) | 17 (89%) | 22 (26%) | 63 (74%) | >.05 | ||
| Other | 0 (0%) | 9 (100%) | 12 (52%) | 11 (48%) | # <.05 | ||
| Education | .473 | *** < .001 | |||||
| High school | 1 (25%) | 3 (75%) | 18 (58%) | 13 (42%) | >.05 | ||
| College | 2 (22%) | 7 (78%) | 33 (52%) | 30 (48%) | .15 | ||
| Undergraduate studies | 14 (20%) | 57 (80%) | 62 (23%) | 204 (77%) | >.05 | ||
| Postgraduate studies | 0 (0%) | 13 (100%) | 20 (15%) | 117 (85%) | >.05 | ||
| Combined high school/college | 3 (23%) | 10 (77%) | 51 (54%) | 43 (46%) | .13 | ||
| Other | 0 (0%) | 1 (100%) | 1 (33%) | 2 (67%) | >.05 | ||
| Age | .717 | *** < .001 | |||||
| <under 18 | 0 (0%) | 1 (100%) | 8 (62%) | 5 (38%) | .11 | ||
| 18–25 | 16 (18%) | 71 (82%) | 66 (25%) | 203 (75%) | >.05 | ||
| 26–35 | 1 (20%) | 4 (80%) | 35 (39%) | 55 (61%) | >.05 | ||
| 36–50 | 0 (0%) | 5 (100%) | 18 (25%) | 55 (75%) | >.05 | ||
| >over 50 | 0 | 0 | 7 (13%) | 48 (87%) | >.05 | ||
| Combined <25 | 16 (18%) | 72 (82%) | 74 (26%) | 208 (73%) | >.05 | ||
Other refers to: Sexual orientation: asexual, pansexual, preferred not to say; Employment: semi voluntary, freelancer, out of work due to injury, disabled, long‐term sick, study‐based practice; Education: qualified accountant ACCA, diploma, vendor qualifications. Significant difference
P < .05;
P < .01;
P < .001, χ2 test;
P < .05 population proportional difference between 2015 and 2017 (z‐test).
3.4. Reasons and motivations for NPS use
The main reasons for using NPSs in the 2015 and 2017 respondents was their friends had taken them (2015, 82.4%; 2017, 68.7% Table 4) and being able to buy them online (2015, 47%; 2017, 43%). Cost remained a significant reason with just over 1/3 of 2015 and 2017 respondents citing the fact they are cheaper than other drugs. As expected, fewer 2017 NPS users stated the reason for using NPS was because they were not against the law (2017, 26.9%) compared with before the ban (2015, 41.2%, P > .05) reflecting some awareness of the PSA 2016 by users. The main motivation for UK NPS use was to get high (2015, 58.8%; 2017, 76.1%).
Table 4.
Reasons and motivations for novel psychoactive substance use (absolute n number of responses and %) of 2015 and 2017 UK survey respondents
| 2015 | 2017 | ||||
|---|---|---|---|---|---|
| Total responses (n = 54) | Total users (n = 17) | Total responses (n = 481) | Total users (n = 134) | P value (2015 vs 2017) | |
| Reasons | n | % of user | n | % of user | |
| Friends have taken them | 14 | 82.4 | 92 | 68.7 | >.05 |
| I was able to buy them online | 8 | 47.1 | 57 | 42.5 | >.05 |
| I know I was not against the law | 7 | 41.2 | 36 | 26.9 | >.05 |
| They are cheaper than other drugs | 6 | 35.3 | 47 | 35.1 | >.05 |
| I was able to buy them easily in head shops (stores that specialize in paraphernalia) | ‐ | ‐ | 36 | 26.9 | nd |
| They are safer than other illegal drugs | ‐ | ‐ | 18 | 13.4 | nd |
| Motivations | |||||
| Give me a good high | 10 | 58.8 | 102 | 76.1 | >.05 |
| Make a night out much better | 6 | 35.3 | 51 | 38.1 | >.05 |
| Make me more confident to socialise | 3 | 17.6 | 42 | 31.3 | >.05 |
3.5. Source and setting of NPS use
Following the legislation, 2017 users most commonly purchased NPS by illegal routes (friends, street dealers and surface internet (23, 24 and 22% frequency response; Figure 1a). Worryingly 31% of our NPS UK users (15% frequency response) purchased NPSs via the untraceable darknet indicating that legal markets (headshops, 13% frequency response) are being displaced by alternative routes, such as street‐level drug dealing or crypto‐markets.
Figure 1.
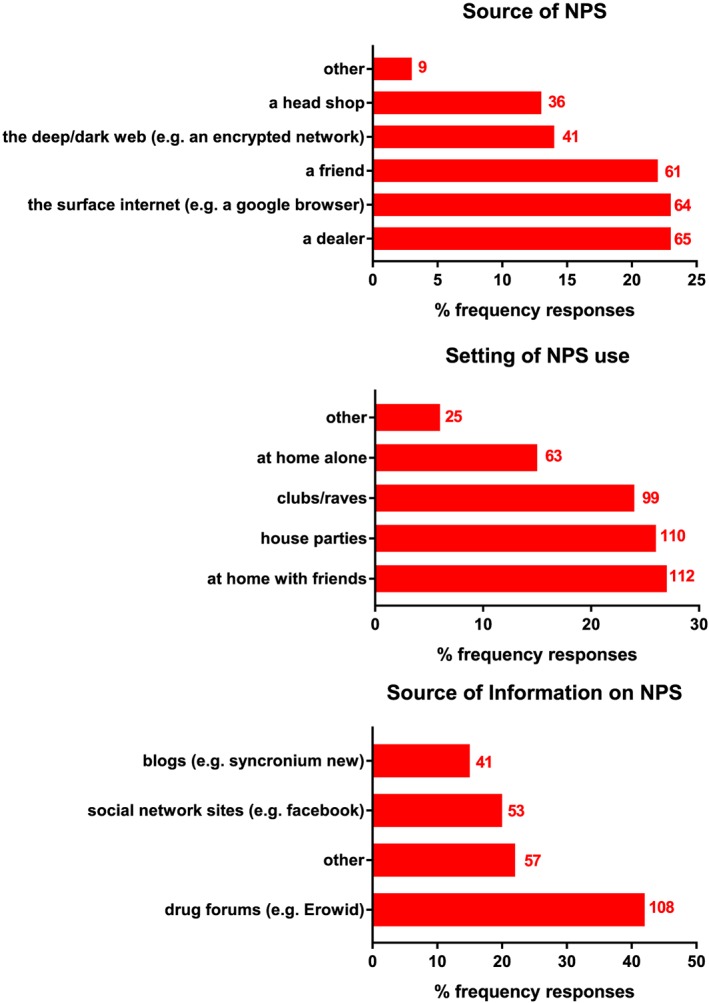
Source of novel psychoactive substance (NPS; A), setting of NPS use (B) and NPS information (C) in 2017 UK survey respondents. Data are expressed as % frequency responses of the 134 UK 2017 users. Absolute n number of responses denoted on histobar. Other sources of information on NPS (C) included friends, PubMed, ScienceDirect, medical case reports or simply trying them
The UK 2017 NPS users (typically in their 20s and 30s) preferred to take NPS in a social setting at parties and clubs or at home with friends (27, 24 and 27% frequency response) rather than alone (15%, Figure 1b) which fits with their demographic and main reasons for taking NPSs, which is with friends (Table 4). The 2017 NPS users most commonly sourced their information on NPSs from drug fora (42%) followed by social network sites (21%) and other (22%; Figure 1c).
3.6. Types of NPS used
The total number of responses to types of NPS was higher in 2017 users (3–4 NPS per user) compared with 2015 users (1–2 NPS per user) reflected by an increased range of other NPS used in 2017 (Figure 2). There was a significant increase in Salvia divinorum use (2017, 45%; 2015, 6%, P < .05) and an increased trend in all types of NPS used by 2017 users (% response) since the legislation, except aerosols, methoxphenidine and diphenidine. Ketamine use was high in both surveys (2015, 77%; 2017, 94%), which will have reflected a preference for the ketamine derivative e.g. methoxetamine in both surveys.
Figure 2.
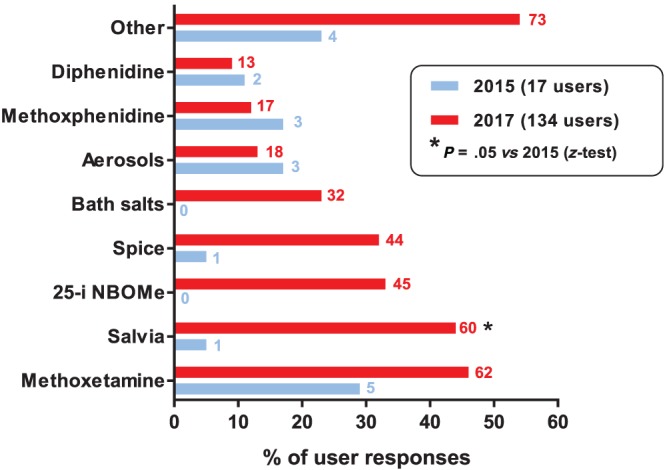
Types of novel psychoactive substance (NPS) used by 2015 and 2017 UK survey respondents. Data is expressed as absolute number of responses (on histobar) and % of user responses. Significant population proportional change *P < .05 (z‐test). The total number of responses is higher in 2017 users (354 responses, 3–4 NPS per user) compared with 2015 users (19 responses, 1–2 NPS per user). Other NPS reported included stimulants, hallucinogens, dissociatives, sedatives and opioids. 2017 other included kratom, 'shrooms, 5‐MeO‐dimethyltryptamine, dimethyltryptamine, etizolam, pyrazolam, mescaline, butyr‐fentanyl, furanyl‐fentanyl, diclazepam, ephenidine, clonazolam, diclazepam, methiopropamine, thiopropamine and entheogens. 2015 other included kratom, α‐methyl‐tryptamine, methylphenidate
3.7. Preference for other drugs used in combination with NPS
There were similar patterns in use and preference of other drugs (legal and illegal) in combination with NPS, before and after the legislation, with highest preference being for alcohol (2017, 73%; 2015, 88%), cannabis (2017, 63%; 2015, 65%) followed by ecstasy (2017, 53%; 2015, 47%; Figure 3). Polydrug use was also similar in both survey samples where approximately 3 to 4 drugs were used per user even though 2017 users used a wider range of NPS (Figure 2). There was a significantly lower use for mephedrone since the legislation (2017, 11%; 2015, 41% P < .05).
Figure 3.
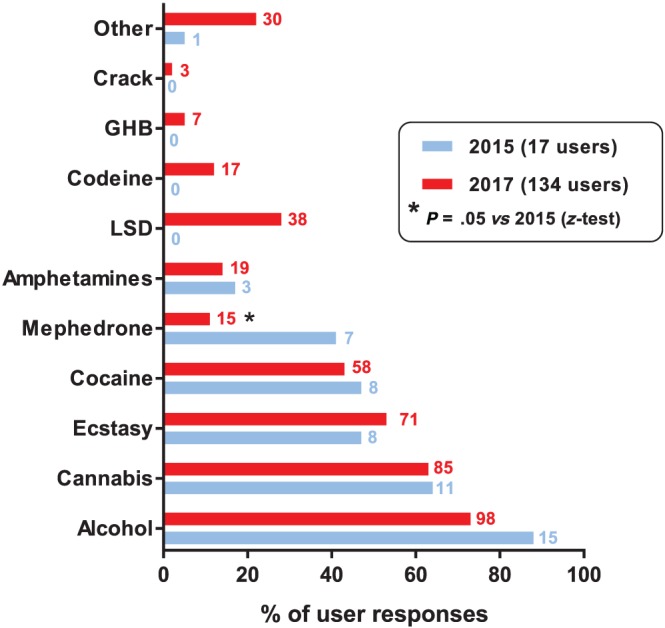
Preference for other substances used in combination with novel psychoactive substance in UK 2017 and 2015 respondents. Data is expressed as absolute number of responses (on histobar) and % of user responses. Significant population proportional change *P < .05 (z‐test). Polydrug use is similar in both survey samples (2017, 441 total responses, 3–4 drug per user; 2015, 54 total responses, 3–4 drug per user)
3.8. Subjective effects of NPS used
There were similar patterns in the subjective effects of the NPS used by 2015 and 2017 respondents (Figure 4). The main positive effects noted by NPS users (2015 and 2017 survey respectively) was feeling relaxed (65 and 90%) and experiencing hallucinations (41 and 69%). Many users also reported anxiety (29 and 53%), lower inhibitions (24 and 50%) or a faster heart rate (29 and 58%) after use of NPSs.
Figure 4.
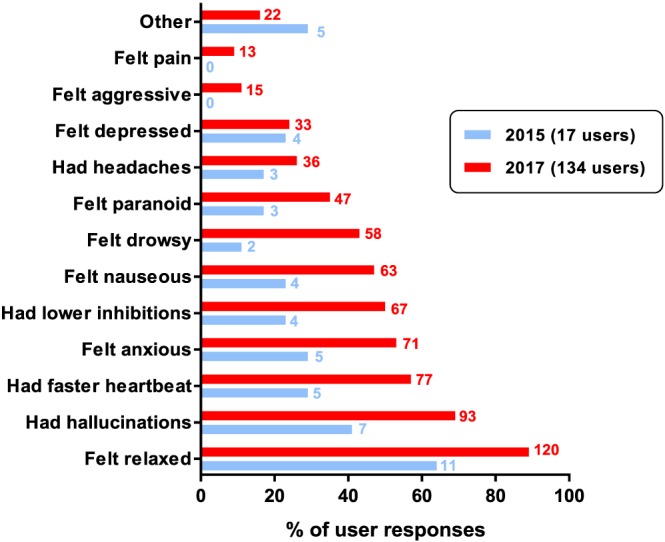
Subjective effects of novel psychoactive substance use. Data is expressed as absolute number of responses (on histobar) and % of user responses. Similar trends in subjective effects of novel psychoactive substance use in both survey samples (P > .05, z‐test)
3.9. User perception of health risks associated with NPS use
Only 17% of 2017 users considered NPS use as high risk compared with 35% of 2015 users (P = .18, Figure 5a). Further, nearly half of 2017 users (47%) considered NPS use carried a low risk, no risk or did not know if they carry a risk, compared with 35% of 2015 NPS users. Furthermore, the age of the 2017 users did not alter their perception of the health risks associated with NPS use, as the lack of risk awareness (> 40%) was seen across all age groups (P > .05 age effect, Figure 5b).
Figure 5.
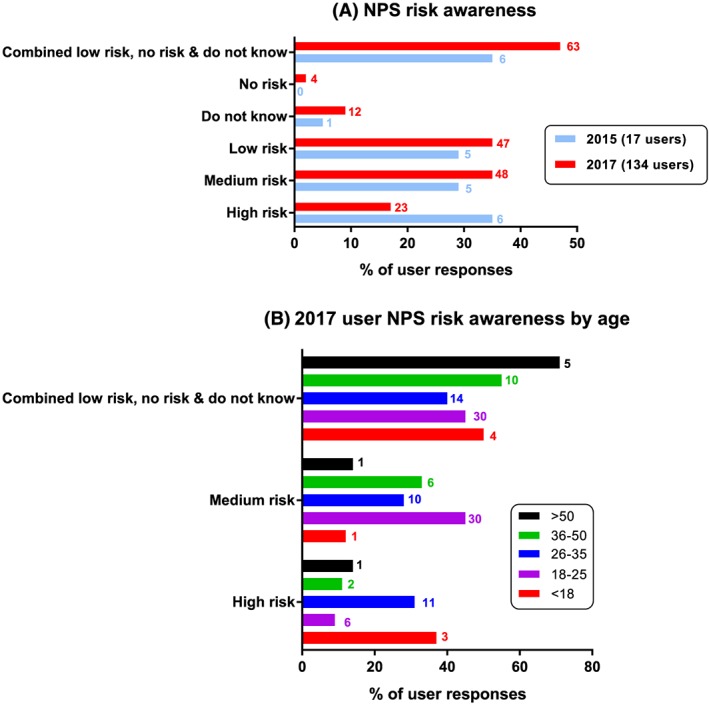
(A) User perception of health risks associated with novel psychoactive substance (NPS) use and (B) 2017 user risk awareness by age. Data expressed as absolute number of responses (on histobar) and % of user respondents. There is a decreased trend (P > .05) in health risk perception in 2017 survey sample compared with 2015 sample. There is no age group effect on risk awareness of the 2017 NPS users (P > .05)
4. DISCUSSION
To the best of our knowledge this is the first report to assess UK NPS awareness, use, experiences and knowledge of potential associated health risks before and after implementation of the PSA 2016.
5.1 Increase in NPS awareness in UK residents educated to postgraduate and high school/college level.
Although UK NPS awareness is not significantly higher following the PSA 2016 (P = .07) only 13% remain unaware in 2017, compared with 28% in 2015. This is also higher than a UK student sample where 18% of the 446 students were unaware of NPS in 201417 demonstrating the new UK legislation has increased awareness. A significant increase in NPS awareness was seen in those UK residents educated to postgraduate and high school/college level and corresponding age groups indicating more young UK residents are informed about NPS.
5.2 Increase in NPS use in male UK residents educated to school/college level and under 18s.
Since the introduction of the PSA 2016 there is an increased trend in UK NPS use from 17% to 27% (Table 3, P > .05) which is higher than 11.5% NPS use reported in England by GDS15 and 0.4% NPS use reported by UK 2017/18 Crime Survey,24 although the Crime Survey covers residential households, and not drug‐using subcultures such as students, in contrast to our survey. NPS use varies considerably depending on the demographic of respondents. A Eurobarometer survey4 revealed that the lifetime experience of NPS use was 8% among European youth compared with 65.8% among a targeted population of nightclub visitors.25 As our surveys were largely promoted through university email, many respondents were aged <35 years and in higher education. The high 27% 2017 NPS use is in line with 31.4% NPS use sampled from 446 UK students aged 17–34 years.17 A drug culture survey of 1401 students has also reported that nearly 1 in 5 (17%) students at British universities admitted to having taken NPS.26
The significantly higher use by males in 2017 (P < .001) is supported by a previous survey carried out among young people in UK, where male respondents were significantly more likely than female users to have taken NPS17 and the 2018 GDS15 indicates that males (6.7%) were more than twice as likely to have used NPS in the last year than females (2.6%). Worryingly, the presence of NPS in drug‐related deaths is becoming more common in the UK and males made up almost 3/4 of drug‐related deaths cases in 2015 and 2017.27 Many studies have shown that the use of NPS occurs in nearly all age groups, although the majority of users are believed to be young males.19, 28 Our 2017 survey shows a highly significant effect of age on NPS use (P < .001) where use was highest in the 100% aware under 18 group. Although this group had the smallest number of respondents the high NPS use correlates with the most represented age of 140 UK NPS users being 17 years.17 Further, high school and college educated respondents had significantly higher NPS use compared with those educated at university in 2017, but not in 2015, which is likely to reflect sampling differences as the response level in college and school educated groups in 2015 was low. The fact that those educated to college or school level are more likely to use NPS in 2017 (P < .001, Table 3; and not 2015), despite an increase in NPS awareness, indicates a need for improved drugs education in schools and colleges. A small study in North London recently demonstrated that 17% of 12–18‐year‐olds admitted using NPS and none had received teaching specifically about NPS.29
5.3 Reasons, motivations, experiences, preferences and health risk perception of UK NPS use remain unchanged.
NPS‐specific studies that take reason into account often emphasise external circumstances such as price, legal status and availability as crucial reasons for NPS use.18 The main reasons cited by our users, before and after the legislation, were their friends taking NPS and being able to buy them online, followed by price, in line with other studies.17, 30 The influence of friends fits with preference to take NPSs in a social setting and sourcing NPSs from a friend. The European Commission Eurobarometer (2014) survey of over 13 000 young people noted that in the UK (before the ban) the most popular route for sourcing NPS was from a friend.4 Worryingly, our survey demonstrates that, since the ban, NPSs are commonly purchased by illegal routes (friends 45%, street dealers 49% and internet, 49%) in line with the 2017/2018 Crime Survey.7 Other surveys also show a shift towards a greater reliance on real‐world interactions (friends, dealers) occurs when an NPS is banned,16, 19, 31 which indicates that an overlapping between the traditional and novel markets is taking place. Predictably, our data indicate that purchasing NPS from the previously legal headshops (26%) is being displaced by alternative illegal routes such as the darknet (31%), in line with recent GDS surveys15, 32 that show the UK is leading the world in the rise of purchasing drugs on the darknet where 1 in 4 (25%) of those who had used drugs in the past year had bought their drugs in this way. It is concerning that 1/3 of our knowledgeable UK NPS users have purchased NPS by this covert route.
The majority of our UK NPS users, before and after the legislation, were intrinsically motivated to get high with their friends and make a night out much better, revealing a culture and desire to experience social and reciprocal sharing fitting with the demographic profile of our users being predominantly young students. Other studies surveying NPS users with similar demographic profiles also suggest that NPS users are driven by enhancement of social situations, the enjoyable effects, and a desire to get high.17, 20, 33 Importantly, the majority of our NPS users indicated they were in control and would probably stop using NPSs if they had changes to extrinsic factors e.g. social demands and responsibilities. Further, our users did not cite using NPSs to cope with life problems or addiction and dependency, which is more likely to lead to abuse and harm potential, also supported by that fact that only 6% (2015) and 18% (2017) of users took NPSs more than once a week. It is also important to note that the distribution of this survey via University and drug fora makes for a selection of knowledgeable education seeking NPS users and not NPS users who are living under poor conditions, where they are unlikely to have access to discussion fora and the internet. Eighty percent of our 2017 NPS users sourced drugs information from drug fora and 43% cited other peer reviewed sources indicating that many users gain some scientific knowledge that might inform their NPS drug taking.
Previous studies have revealed that reasons and motivations for different types of NPS use can vary considerably.18, 19, 34, 35 These studies indicate that use of novel stimulants and hallucinogens is mainly motivated by self‐exploration, facilitation of social situations, euphoria (get high) and insignificantly associated with dependency. In line with the motivation to get high and feel relaxed our UK users (before and after the ban) preferred hallucinogenic dissociatives (e.g. methoxetamine) and psychedelics (e.g. S. divinorum). Many NPS users also took ketamine (2015, 77%; 2017, 94%), which will have reflected their preference for the ketamine derivative methoxetamine reported to produce more intense and longer lasting dissociative effects than ketamine.36 The increased use of the natural NPS, S. divinorum (P < .05), may, in part, be because it is harder to control under the PSA 2016. Preference for S. divinorum (20 and 39%) has been previously reported by UK students17, 26 and can lead to de‐realisation and medical and psychopathological risks.37, 38 There was an increase in the use of the synthetic cannabinoid spice following the legislation (32.8 vs 5.8%, P > .05), which can produce a state of relaxation and of feeling stoned,39 even though use of cannabis remained the same. This increase between 2015 and 2017 in our UK users may reflect the significant global rise in synthetic cannabinoid use that has occurred in the world of NPS over this time,6, 15, 32 demonstrating that regularly monitoring of NPS use is important in such a fast‐paced scene.
Polydrug use was similar (before and after the legislation) even though 2017 users took a wider range of NPS. The consumption of NPS was combined with alcohol, cannabis and ecstasy for the majority of users, in line with European drug use in young adults.40 Under‐18 NPS users in our survey reported taking cannabis and stimulants, including https://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=4804, https://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=2286, https://www.guidetopharmacology.org/GRAC/LigandDisplayForward?ligandId=17 and ecstasy. Cannabis remains the most commonly used illicit drug in the UK and the second most prevalent drug overall after alcohol, whilst ecstasy is the next most commonly reported illicit drug used in the UK.24 Since the legislation, preference for mephedrone significantly reduced to 11.1% (P < .05) in line with a recent report of the decline in mephedrone use in the UK among 16–34‐year‐olds24 and the recent global decline in synthetic cathinone use.6, 15, 32 The increased range of NPS hallucinogen dissociatives and psychedelics taken by 2017 UK users, many of which have stimulant properties, will account for the increased report of acute positive (relaxed, hallucinations) and negative (anxious, faster heart beating, aggression, nausea) subjective effects. As well as a subjective effect of feeling stoned, spice can be both stimulating and sedating, anxiogenic and anxiolytic41 and unlike cannabis, can produce a hangover state, which may correspond with reports of headaches. Polydrug use of alcohol, cannabis, ecstasy and cocaine may well contribute to the reported subjective effects.
Despite the increase in NPS awareness, we see a decreased trend in the perception of health risks associated with NPS use, where 1 in 5 users considered NPS use as high risk compared with 1 in 3 before the ban. Moreover, nearly half of 2017 users considered NPS use carried a low risk, no risk or did not know if they carry a risk, compared with 1/3 in 2015. The fact that >80% of our NPS users are typically well educated and well informed is surprising given that there is a significant knowledge gap on the health risks of NPS use across all age groups. Given that the main motivation for NPS use in our surveys is to get high the unknown high‐risk aspect of NPS may be an attractive feature for many users42 particularly younger adolescents happy to take risks to attain novel psychoactive experiences from NPS (age group with the highest NPS use). This may explain why our younger NPS users continue to use NPS even though they do not know the risks or believe they are high risk. Notably, significantly more of the 2015 NPS users were under 25 and twice as many considered NPS as high risk, compared with the 2017 NPS users. A recent qualitative study20 emphasised that the development of appropriate harm reduction policies should incorporate an understanding of the relationship between the risks and the beneficial effects of NPS to better resonate with young drug users.43
The high rate of NPS use in our surveys will, in part, reflect the demographic of the self‐selecting samples being young (typically 20s and 30s), risk takers with a greater interest in drugs and more likely to go clubbing and to parties, than the general population. Moreover, these self‐selecting subpopulations may be more resistant to change, hence extrapolation to the wider UK population needs to be carefully considered. However, high UK NPS use in males, in the under 18s and those educated to a school and college level in our 2017 sample, highlights the current need for statutory universal drugs education in UK schools and colleges as part of the national curriculum. This education needs to address the risks and benefits of drug taking and importantly resilience to risk factors (e.g. peer pressure), social and emotional skills.44, 45, 46 This will not only educate but build resilience and empower young people to help them make positive choices for their health, including drugs choices when in peer‐pressure situations.
In conclusion, our surveys demonstrate that regulation alone, so far, has not impacted on risk awareness and reasons and motivations for UK NPS use (drug demand and culture) and that determining the type of motivation in our NPS consumer groups (in this case mainly UK students) is essential for effective prevention policies and reduction of NPS‐related harms.
COMPETING INTERESTS
No conflicts of interest are declared here that may have influenced the interpretation of present data. Please note the following: F.S. is an editor of this special issue of Brain Science, was a full member of the UK Advisory Council on the Use of Drugs (ACMD) and a member of the ACMD's NPS and Technical Committees; J.C. is also a co‐opted member of the NPS and Technical Committees. The views expressed here are solely those of the authors and do not necessarily reflect those of the Home Office or the ACMD.
6. CONTRIBUTORS
E.D., O.D. and L.A.L conceptualized the online surveys, methodology and extracted and analysed the data. E.D. and L.A.L wrote the first draft of the paper; E.D., F.S., J.M.C. and L.A.L then critically revised subsequent drafts.
5. ACKNOWLEDGEMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors. The views expressed here reflect only the authors' views. The authors would like to acknowledge the help of Dr Richard Szydlo from the Faculty of Medicine at Imperial College for assisting with statistical analyses, the survey respondents for contributing their time to this research and http://www.bluelight.ru for their help in advertising the survey.
Deligianni E, Daniel OJ, Corkery JM, Schifano F, Lione LA. Impact of the UK Psychoactive Substances Act on awareness, use, experiences and knowledge of potential associated health risks of novel psychoactive substances. Br J Clin Pharmacol. 2020;86:505–516. 10.1111/bcp.14123
Dr Lisa A. Lione is the Principal Investigator. No interventions were performed with human subjects/patients and or substances administered.
DATA AVAILABILITY STATEMENT
Research data are not shared. The data are not publicly available due to privacy/ethical restrictions.
REFERENCES
- 1. United Nations Office for Drugs and Crime (UNODC) . Early Warning Advisory on New Psychoactive Substances. 2018. Accessed 10th August 2018. https://www.unodc.org/LSS/Page/NPS
- 2. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA‐Europol) . Annual Report on the implementation of Council Decision 2005/387/JHA. 2017. Accessed 18th October 2018. http://www.emcdda.europa.eu/publications/implementation-reports/2017_en
- 3. Beltgens MT. Legislative Measures' Impact on the New Psychoactive Substances Market In: Savona E, Kleiman M, Calderoni F, eds. Dual Markets. Cham: Springer; 2017. [Google Scholar]
- 4. European Commission Report: Flash Eurobarometer 401: Young people and drugs. Luxembourg: TNS Political & Social. 2014. Accessed 18th October 2018. http://ec.europa.eu/public_opinion/flash/fl_401_present_en.pdf
- 5. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) Legal approaches to controlling new psychoactive substances. 2014. Accessed 18th October 2018. http://www.emcdda.europa.eu/topics/pods/controlling-new-psychoactive-substances
- 6. Global Drug Survey 2016. Accessed on 10th August 2018. https://www.globaldrugsurvey.com/past-findings/the-global-drug-survey-2016-findings/
- 7. Home Office Review of Psychoactive Substances Act. 2018. Accessed on 15th May 2019. https://www.gov.uk/government/publications/review-of-the-psychoactive-substances-act-2016
- 8. Office of National statistics . Deaths related to drug poisoning in England and Wales. 2013. Accessed on 15th May 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/2014-09-03
- 9. Office for National Statistics . Deaths related to drug poisoning in England and Wales: 2017 registrations. from https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/2017registrations
- 10. Wood DM, Ceronie B, Dargan PI. Healthcare professionals are less confident in managing acute toxicity related to the use of new psychoactive substances (NPS) compared with classical recreational drugs. QJM. 2016;109(8):527‐529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Home Office Psychoactive Substances Act 2016, The Stationery Office Limited, 2016. http://services.parliament.uk/bills/2015-16/psychoactivesubstances.html
- 12. Wadsworth E, Drummond C, Deluca P. The adherence to UK legislation by online shops selling new psychoactive substances. Drugs Educ Prev Policy. 2018;25(1):97‐100. [Google Scholar]
- 13. Acreman DJ, Smith JC. Increased prevalence of high potency substances – an inadvertent effect of legislative control. Vth NPS conference 2017.
- 14. Van Buskirk J, Griffiths P, Farrell M, Degenhardt L. Trends in new psychoactive substances from surface and “dark” net monitoring. Lancet Psychiatry. 2017;4(1):16‐18. [DOI] [PubMed] [Google Scholar]
- 15.August, authors. Global drug survey 2018. Accessed on 10th. 2018. https://www.globaldrugsurvey.com/gds-2018/ [Google Scholar]
- 16. McElrath K, O'Neill C. Experiences with mephedrone pre‐ and post‐legislative controls: perceptions of safety and sources of supply. Int J Drug Policy. 2011;22(2):120‐127. [DOI] [PubMed] [Google Scholar]
- 17. Corazza O, Simonato P, Corkery JM, Trincas G, Schifano F. “Legal highs”: safe and legal “heavens”? A study on the diffusion, knowledge and risk awareness of novel psychoactive drugs among students in the UK. Riv Psichiatr. 2014;49(2):89‐94. [DOI] [PubMed] [Google Scholar]
- 18. Sutherland R, Bruno R, Peacoc A, et al. Motivations for new psychoactive substance use among regular psychostimulant users in Australia. Int J Drug Policy. 2017;43:23‐32. [DOI] [PubMed] [Google Scholar]
- 19. Soussan C, Kjellgren A. The users of novel psychoactive substances: online survey about their characteristics, attitudes and motivations. Int J Drug Policy. 2016;32:77‐84. [DOI] [PubMed] [Google Scholar]
- 20. Soussan C, Andersson M, Kiellgren A. The diverse reasons for using novel psychoactive substances ‐ a qualitative study of the users' own perspectives. Int J Drug Policy. 2018;52:71‐78. [DOI] [PubMed] [Google Scholar]
- 21. King LA. New phenethylamines in Europe. DTA Drug Test Anal. 2014. 2014;6(7–8):808‐818. [DOI] [PubMed] [Google Scholar]
- 22. Deligianni E, Corkery JM, Schifano F, Lione LA. An international survey on the awareness, use, preference, and health perception of novel psychoactive substances (NPS). Hum Psychopharmacol. 2017;32(3): e2581. [DOI] [PubMed] [Google Scholar]
- 23. Deligianni E, Corkery JM, Schifano F, Lione LA. Impact of the UK psychoactive substances act on awareness, use, experiences and knowledge of potential associated health risks of NPS. VIth NPS conference. Res Adv Psychiatry. 2019;6(1):1‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Home Office Drug Misuse: Findings from the 2017/18 Crime Survey for England and Wales London: Home Office. https://www.gov.uk/government/statistics/drug-misuse-findings-from-the-2017-to-2018-csew
- 25. Wood DM, Hunter L, Measham F, Dargan PI. Limited use of novel psychoactive substances in South London nightclubs. QJM. 2012;105(10):959‐964. [DOI] [PubMed] [Google Scholar]
- 26. The Student Beans survey . Drug culture at UK universities. 2012; https://www.theguardian.com/education/interactive/2012/oct/12/university-drug-culture-survey
- 27. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) (2018) UK Drug Report. 2018. Accessed 18th October 2018. http://www.emcdda.europa.eu/system/files/publications/8894/united-kingdom-cdr-2018-with-numbers.pdf
- 28. Barratt MJ, Cakic V, Lenton S. Patterns of synthetic cannabinoid use in Australia. Drug Alcohol Rev. 2013;32(2):141‐146. [DOI] [PubMed] [Google Scholar]
- 29. Lloyd AK, Shafi A, Mitchell K, Mayordomoaranda A, Martinotti G, Corazza O. NPS misuse in children and adolescents: a study among a sample population in North London accessing acute and community mental health services. Vth NPS conference, 2017.
- 30. Ramsey J, Dargan PI, Smyllie M, et al. Buying 'legal' recreational drugs does not mean that you are not breaking the law. QJM. 2010;103(10):777‐783. [DOI] [PubMed] [Google Scholar]
- 31. Sande M. Characteristics of the use of 3‐MMC and other new psychoactive drugs in Slovenia, and the perceived problems experienced by users. Int J Drug Policy. 2016;27:65‐73. [DOI] [PubMed] [Google Scholar]
- 32. Global Drug Survey 2017. Accessed on 10th August 2018. https://www.globaldrugsurvey.com/gds2017-launch/results-released/
- 33. Home Office New psychoactive substances review: Report of the expert panel. London: 2014. Accessed on 10th August 2018. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/368583/NPSexpertReviewPanelReport.pdf
- 34. Beharry S, Gibbons S. An overview of emerging and new psychoactive substances in the United Kingdom. Forensic Sci Int. 2016;267:25‐34. [DOI] [PubMed] [Google Scholar]
- 35. Zawilska JB. "legal highs"‐‐an emerging epidemic of novel psychoactive substances. Int Rev Neurobiol. 2015;120:273‐300. [DOI] [PubMed] [Google Scholar]
- 36. Corazza O, Schifano F, Simonato P, et al. Phenomenon of new drugs on the internet:the case of ketamine derivative methoxetamine. Hum Psychopharmacol. 2012;27(2):145‐149. [DOI] [PubMed] [Google Scholar]
- 37. Singh S. Adolescent salvia substance abuse. Addiction. 2007;102(5):823‐4. 24. [DOI] [PubMed] [Google Scholar]
- 38. González D, Riba J, Bouso JC, Gómez‐Jarabo G, Barbanoj MJ. Pattern of use and subjective effects of Salvia divinorum among recreational users. Drug Alcohol Depend. 2006;85(2):157‐162. [DOI] [PubMed] [Google Scholar]
- 39. Tracy DK, Wood DM, Baumeister D. Novel psychoactive substances: identifying and managing acute and chronic harmful use. BMJ; 2007; 356:i6814. [DOI] [PubMed] [Google Scholar]
- 40. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) . European Drug Report. Trends and Developments; EMCDDA: Lisbon, Portugal, 2017. Accessed 18th October 2018. http://www.emcdda.europa.eu/system/
- 41. Papanti D, Schifano F, Botteon G, et al. “Spiceophrenia”: a systematic overview of “spice”‐related psychopathological issues and a case report. Hum Psychopharmacol. 2013;28:379‐389. [DOI] [PubMed] [Google Scholar]
- 42. Reuter P, Pardo B. New psychoactive substances: are there any good options for regulating new psychoactive substances? Int J Drug Policy. 2017;40:117‐122. [DOI] [PubMed] [Google Scholar]
- 43. Penney J, Dargan PI, Padmore J, Wood DM, Norman IJ. Epidemiology of adolescent substance use in London schools. QJM. 2016;109(6):405‐409. [DOI] [PubMed] [Google Scholar]
- 44. DfE and ACPO drug advice for schools: Advice for local authorities, headteachers, school staff and governing bodies. London: Department for Education. 2012. Accessed 18th October 2018. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/270169/drug_advice_for_schools
- 45. Hargreaves P. School‐based drug education and prevention: the impact of inspection and curriculum provision. Drugs and Alcohol Today. 2016;16(2):131‐141. [Google Scholar]
- 46. Home Office New Psychoactive Substances (NPS) Resource pack for informal educators and practitioners. 2017. Accessed 18th October 2018. https://www.gov.uk/government/publications/new-psychoactive-substances-nps-resource-pack
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared. The data are not publicly available due to privacy/ethical restrictions.


