Abstract
Aim
To identify trends in drug‐related deaths associated with fentanyl and its derivatives, including novel variants, in England, 1998–2017.
Methods
Case reports from the National Programme on Substance Abuse Deaths (NPSAD) where a pharmaceutical fentanyl or non‐pharmaceutical fentanyl derivative (NPFD) was found at post‐mortem and/or implicated in the death were extracted for analysis.
Results
NPSAD has received case reports detailing 298 deaths in England from 1998–2017 where a fentanyl was found at post‐mortem and/or implicated in the death. Hospital administered fentanyl is “very safe”, whereas pharmaceutical fentanyls in the community, procured either legitimately via prescription or illegitimately, carry high risk of unintentional death. Deaths involving NPFDs, which possess extreme potencies in comparison to morphine, have drastically risen over the past three years, and correlate with an increasing number of available compounds. Males, and those with existing opioid abuse disorders, are particularly susceptible to death related to NPFD intake.
Conclusions
The increasing availability of both pharmaceutical fentanyls and NPFDs represents a serious risk to public health. Unintentional misuse of these compounds in England is contributing to the exponential increase in fentanyl‐associated deaths that is being observed at the global scale.
Keywords: drug‐related deaths, fentanyl, novel psychoactive substance, opioid overdose, synthetic opioid
What is already known about this subject
Fentanyl is a highly potent synthetic opioid.
The structural flexibility of fentanyl has enabled the development of several pharmaceutical derivatives key for the delivery of modern medicine.
Extremely potent non‐pharmaceutical fentanyl derivatives (NPFDs) have also been synthesised and carry severe risk of death if administered.
What this study adds
Fentanyl‐related fatalities in England are on the rise.
Pharmaceutical fentanyl derivatives prescribed and self‐administered in an outpatient setting carry risk of unintentional death.
An increasing number of highly potent NPFDs have been detected and have contributed to the recent spike in fentanyl‐related fatalities.
1. INTRODUCTION
The naturally occurring alkaloids of the opium poppy, which famously include morphine, have long been sought clinically to induce anaesthesia, analgesia and sedation.1 Structural identification of these opiate alkaloids,1 and the receptors at which they act (https://www.guidetopharmacology.org/GRAC/ObjectDisplayForward?objectId=319, https://www.guidetopharmacology.org/GRAC/ObjectDisplayForward?objectId=318 and https://www.guidetopharmacology.org/GRAC/ObjectDisplayForward?objectId=317),2 has enabled the design and manufacture of several semi‐synthetic and synthetic opioids for clinical use.3
One such synthetic opioid is fentanyl, which possesses several advantageous pharmacodynamic properties: a higher therapeutic index than morphine, high potency (50–100 times that of morphine), fast onset due to high lipid solubility enabling rapid penetration of the blood–brain barrier, and relatively short duration of action.4 In addition, the flexibility of the core fentanyl structure has aided in the formulation of pharmaceutical fentanyl analogues, namely alfentanyl, remifentanyl and sufentanyl, with precise onset of action, duration and potency designed for use in specific clinical scenarios.5 In hospitals, fentanyl and its derivatives are intravenously administered for anaesthesia in operating theatres,6 and analgesia and sedation in intensive care units7 and emergency departments.8 In the community they can be delivered in patches, lozenges and sprays for chronic pain conditions,9, 10, 11 as infusions via syringe driver for palliative care patients,12 and as lollipops to military personnel in active deployment.13 Fentanyl analogue use also extends to veterinary medicine, where carfentanyl, possessing potencies 10,000 times that of morphine, is used for sedation of large animals.14 Access to pharmaceutical and veterinary fentanyls is therefore heavily restricted as their diversion for recreational use carries risk of overdose and death, commonly via respiratory arrest.4, 5
As both clinical and recreational demand has increased for these compounds,15, 16 the manufacturing processes have been improved to reduce costs and increase yields.17, 18 Easy access to this synthesis guidance via the internet, in combination with the structural flexibility of fentanyl, has enabled the development of a number of illicit non‐pharmaceutical fentanyl derivatives (NPFDs) in recent years.15, 19 These NPFDs often possess very high potencies (470–10,000 times that of morphine), so that they require only small batch manufacture and shipping, aiding concealment from authorities.20, 21, 22 However, this feature of NPFDs concomitantly makes risk of accidental overdose and subsequent death via respiratory arrest critically severe. Accordingly, NPFDs in the UK are controlled either by the Misuse of Drugs Act 1971 or banned by the Psychoactive Substances Act 2016.
In recent years, fentanyl‐related deaths have risen rapidly on a global scale,23 particularly in the US and Canada: in the US between 2013 and 2014 the age‐adjusted rate of deaths involving synthetic opioids increased by 80%23 and by 250% amongst younger people24; in Canada fentanyl and its analogues contributed to at least 1,516 deaths in 2016, with preliminary data for 2017 indicating a further increasing trend.25 In this article, we are able to provide evidence that fentanyl‐related deaths in England have increased at an astonishing rate in recent years, largely due to the introduction and misuse of NPFDs. We have extracted case reports from the National Programme on Substance Abuse Deaths where a fentanyl was found at post‐mortem and/or implicated in order to determine the source of pharmaceutical fentanyls involved in reported deaths, and the circumstances surrounding NPFD‐associated fatalities.
2. METHODS
2.1. National Programme on Substance Abuse Deaths (NPSAD)
NPSAD regularly receives information from Coroners on a voluntary basis on deaths related to drugs in both addicts and non‐addicts in England and Wales, Northern Ireland, the Channel Islands and the Isle of Man, as described previously.26 Reports were also received from the Scottish Crime and Drug Enforcement Agency between 2004 and 2011, and from the General Register Office for Northern Ireland since 2004. In total NPSAD has received over 34,000 deaths since 1997. If a death has an unknown cause, is violent or unnatural, sudden and unexplained, occurred during an operation or before the person came out of an anaesthetic, or may have been caused by an industrial disease or poisoning, then it is referred to a Coroner.27 Toxicology tests are requested at the discretion of the Coroner, and are dependent upon the circumstances of individual cases. Coroners voluntarily report a death to NPSAD if it features one or more of the following:
Presence of one or more psychoactive substance(s) directly implicated in death.
History of dependence or abuse of drugs.
Presence of controlled drugs at post‐mortem.
The Central Office for Research Ethics Committees (COREC), of the National Patient Safety Agency confirmed (February 2006) that the NPSAD Programme does not require NHS Research Ethics Committee review as the subjects of the research are deceased.
2.2. Case identification
A range of documents are contained in Coronial inquest files, although this varies from case to case. Typically, the Coroner has access to: statements from witnesses, family and friends; General Practitioner records (if the deceased is registered with one); reports from first responders (e.g. police, emergency services); hospital emergency departments and clinical ward reports; psychiatric and substance abuse team reports; as well as post‐mortem and toxicology reports.
A retrospective study design was employed to identify relevant cases from England associated with the use of pharmaceutical and non‐pharmaceutical fentanyl derivatives by searching the NPSAD database for the following terms: “fentanyl”, “alfentanyl”, “remifentanyl”, “acetylfentanyl”, “parafluorobutyrfentanyl”, “2‐fluorofentanyl”, “4‐fluorofentanyl”, “carfentanyl”, “butyrfentanyl”, “cyclopropylfentanyl”, “despropionylfentanyl”, “furanylfentanyl”, “methoxyacetylfentanyl”, “ocfentanyl”, and any variants in spelling. These search terms capture all deaths recorded in the database as fentanyl‐related. The fields searched on the database were those holding data on drugs present at post‐mortem, drugs implicated in death, cause(s) of death, verdict, accident details, prescribed drugs and “other relevant information”.
All cases reported here have confirmatory evidence that a fentanyl was (self‐)administered or the toxicology reports indicate the presence of these substances in the decedents' tissue(s). Fentanyl and its analogues are tested for using a variety of mass spectrometry and high‐pressure liquid chromatography methods, where they are identified by comparison against a routinely updated library of known fentanyl analogues, or deduced using advanced detection methods.28
2.3. Data analysis
Data entry and analysis were performed using IBM® SPSS™ Statistics for Windows version 25.
Cases where a pharmaceutical fentanyl (fentanyl, remifentanyl, alfentanyl, sufentanyl) was found at post‐mortem and/or implicated were categorised as having been prescribed, hospital administered, unlawfully obtained, or unknown in source based upon information provided in the NPSAD case reports. Cases were assigned to the prescribed category where data listing a pharmaceutical fentanyl as prescribed were provided. Cases were assigned to the hospital administered category based upon details given in the case background information and/or evidence that a general anaesthetic was administered. Cases were assigned as unlawfully obtained where it was explicitly detailed that they were not prescribed a pharmaceutical fentanyl or administered it in hospital, and/or where explicit details were given in the case background information that the pharmaceutical fentanyl had been unlawfully obtained. Cases were assigned as unknown in source when they could not be categorised as either prescribed, hospital administered or unlawfully obtained.
Stata®™ Version 15 for Windows was used to perform Poisson tests to indicate statistical significance.
2.4. Nomenclature of targets and ligands
Key protein targets and ligands in this article are hyperlinked to corresponding entries in http://www.guidetopharmacology.org, the common portal for data from the IUPHAR/BPS Guide to PHARMACOLOGY,29 and are permanently archived in the Concise Guide to PHARMACOLOGY 2017/18.30
3. RESULTS
A total of 298 people died in England between 1998–2017 with a fentanyl found at post‐mortem and/or implicated in the death, and were reported to NPSAD. Presence at post‐mortem indicates that the decedent died with fentanyl(s) in their system, with an implicated listing indicating that the (self‐)administered fentanyl(s) directly contributed to the death.
It is clear that reporting of fentanyl‐related fatalities in England has drastically risen in recent years (Figure 1A). Whilst there has been a steady increase from 2007 to 2017 in deaths involving a pharmaceutical fentanyl, it is those where an NPFD was detected that are responsible for the recent spike in reported deaths.
Figure 1.
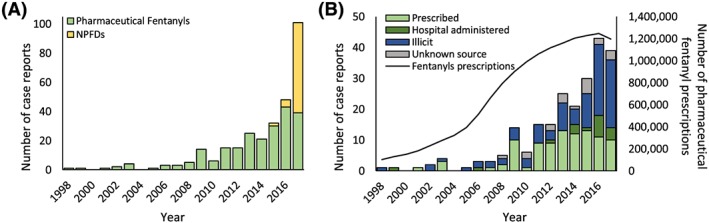
A, Total fentanyl‐associated fatalities in England 1998–2017. These fatalities comprise cases where only pharmaceutical fentanyls were found at post‐mortem and/or implicated (green), or NPFDs either alone or in combination with a pharmaceutical fentanyl (yellow). When normalised against total NPSAD reporting in England over the same time period, this increase in fentanyl‐associated deaths remains, demonstrating that there has been a proportional rise in the occurrence of fentanyl‐related deaths (data not shown) B, Sources of pharmaceutical fentanyls detected at post‐mortem and/or implicated. The prescription, verdict narrative and additional information fields were interrogated to determine case categorisation. Cases where the source of the pharmaceutical fentanyls was unclear were deemed “unknown”, and likely represent a mix of prescribed, hospital administered and unlawfully obtained sources. The secondary Y axis shows the number of General Practitioner prescriptions for pharmaceutical fentanyls in England by year (data from Peterson et al.24)
3.1. Pharmaceutical fentanyl‐associated deaths
A total of 229 cases where a pharmaceutical fentanyl was found at post‐mortem and/or implicated in England have been reported to NPSAD (Table 1). The pharmaceutical fentanyls specified in these cases include fentanyl, alfentanyl and remifentanyl. No cases involving sufentanyl were found. The steady increase in the number of reported cases from 2005 to 2017 correlates with the rate of fentanyl prescribing in England16 over the same time period (95% CI 0.99–1.16) (Figure 1B). When delineating the source of the pharmaceutical fentanyl, there has been a rise in case reports across all known categories (prescribed, hospital administered, unlawful obtainment). Self‐administration of pharmaceutical fentanyls without direct supervision from healthcare professionals appears to carry a higher risk that the fentanyl will be implicated in the death, irrespective of their source: pharmaceutical fentanyls were implicated in 93.7% of cases where they had been prescribed, and 84.5% of cases where they had been unlawfully obtained (Table 1). Furthermore, death was deemed unintentional in 85.3% of prescribed cases and 88.7% of cases where it had been unlawfully obtained. By comparison, only one death was reported over the 20‐year study period where a pharmaceutical fentanyl administered in a hospital, and therefore under direct supervision from healthcare professionals, was ruled by the Coroner to have directly contributed to the death. This patient was in renal failure and was receiving fentanyl via syringe driver infusion, likely as part of a palliative care programme. Death was deemed unintentional in all cases (64.9%; n = 63 out of 97) where the pharmaceutical fentanyl was administered in a hospital setting.
Table 1.
Type, source and rates of fentanyl implication in reported deaths
| Fentanyl type | Source | Implicated in death |
|---|---|---|
| Pharmaceutical | Hospital | 5.6% (n = 1/18) |
| Prescription | 93.7% (n = 89/95) | |
| Illicit | 84.5% (n = 82/97) | |
| Unknown | 73.7% (n = 14/19) | |
| Pharmaceutical & NPFD | Unknown & illicit | 100% (n = 29/29) |
| NPFD | Illicit | 97.5% (n = 39/40) |
Co‐administration of illicit substances was more likely to occur when the pharmaceutical fentanyl had been unlawfully obtained (44.3% of cases; n = 43 out of 97) as opposed to when it had been prescribed (15.8% cases; n = 15 out of 95). There was an even higher occurrence of co‐administered illicit substances in hospital‐administered fentanyl cases (55.6%; n = 10 out of 18). In all these cases a pharmaceutical fentanyl was administered as part of treatment to address adverse events that had occurred as a direct result of this illicit substance administration.
3.2. NPFD‐associated deaths
A total of 69 cases where an NPFD was found at post‐mortem and/or implicated in England have been reported to NPSAD (Table 1), with the first case occurring in 2015. There has been a subsequent sharp rise in deaths where an NPFD was found at post‐mortem and/or implicated (Figure 1A), along with an increasing number of identified NPFD compounds (Table 2A). NPFD administration was directly implicated in causing death in all but one case (n = 68 out of 69 NPFD cases; Table 1), from which there was only one instance where the NPFD was administered with the intention of suicide (n = 1 out of 68 NPFD‐implicated cases). Carfentanyl was the most commonly reported NPFD (whilst carfentanyl is licensed for use in veterinary medicine,14 it is not licensed for human use, and as such is classified as an NPFD), with its presence at post‐mortem and/or implication listed in 79.7% of NPFD cases (n = 55 out of 69 NPFD cases; Table 2B). Co‐administration of multiple fentanyls, either multiple NPFDs alone or in combination with a pharmaceutical fentanyl, was reported in 43.5% of NPFD cases (n = 30 out of 69 NPFD cases; Table 2C). Co‐administration with other, non‐fentanyl derivative substances was also a common occurrence, with heroin/morphine, benzodiazepines/Z‐drugs and cocaine being the most commonly co‐administered substances: 56.5% of cases (n = 39 out of 69 NPFD cases) had heroin/morphine and/or their metabolites detected at post‐mortem; 50.7% of cases (n = 35 out of 69 NPFD cases) had a benzodiazepine/Z‐drug and/or their metabolites detected at post‐mortem; 58.0% (n = 40 out of 69 NPFD cases) had cocaine and/or their metabolites detected at post‐mortem. (as diamorphine is rapidly metabolised to 6‐monoacetylmorphine and morphine after administration, it is impossible to ascertain whether heroin or morphine was ingested if diamorphine‐specific metabolites or common street heroin contaminants are not tested for. As such, heroin and morphine are combined in the NPSAD database.) Only 5 cases were reported (7.2%) where only an NPFD was found at post‐mortem.
Table 2A.
Year when each NPFD was first reported to NPSAD
| 2015 | 2016 | 2017 |
|---|---|---|
| Acetylfentanyl | 2‐Fluorofentanyl | Butyrfentanyl |
| Para‐Fluorobutyrfentanyla | 4‐Fluorofentanyl | Cyclopropylfentanyl |
| Carfentanyl | Despropionylfentanyl | |
| Furanylfentanyl | ||
| Methoxyacetylfentanyl | ||
| Ocfentanyl |
Para‐fluorobutyrfentanyl was also reported using its alternate name fluorobutryrylfentanyl: for analysis these cases have been merged and classified under the para‐fluorobutyrfentanyl term.
Table 2B.
Number of cases where each NPFD has been reported
| NPFD | Number of casesa |
|---|---|
| 2‐Fluorofentanyl | 2 |
| 4‐Fluorofentanyl | 1 |
| Acetylfentanyl | 5 |
| Butyrfentanyl | 6 |
| Carfentanyl | 55 |
| Cyclopropylfentanyl | 1 |
| Despropionylfentanyl | 2 |
| Furanylfentanyl | 2 |
| Methoxyacetylfentanyl | 1 |
| Ocfentanyl | 1 |
| Para‐Fluorobutyrfentanyl | 7 |
| Unknown Fluorofentanyl | 1 |
As there were instances where multiple NPFDs were found in a single case, the sum of the Number of Cases column will exceed 69 (total number of NPFD cases).
Table 2C.
Number of cases with NPFDs reported either alone or in combination with other NPFD(s) and/or pharmaceutical fentanyls
| Number of cases | |
|---|---|
| Cases with 1 NPFD | 39 |
| Cases with 1 NPFD & 1 pharmaceutical fentanyl | 22 |
| Cases with 2 NPFD | 0 |
| Cases with 2 NPFD & 1 pharmaceutical fentanyl | 1 |
| Cases with 3 NPFD | 1 |
| Cases with 3 NPFD & 1 pharmaceutical fentanyl | 6 |
3.3. Demographics
Whilst gender and age at time of death demographics for total fentanyl‐associated fatalities are comparable to those of all cases reported to NPSAD over the same time period (Table 3), there are clear differences in the demographics of decedents where a pharmaceutical fentanyl alone or NPFD(s) was found. Decedents where an NPFD was found at post‐mortem and/or implicated were majority male (90%) and were on average younger than male decedents where a pharmaceutical fentanyl alone was found. In contrast, a balanced gender split and older demographic is apparent where a pharmaceutical fentanyl alone was found and its procurement legitimate (prescribed or hospital administered).
Table 3.
Gender and age at time of death demographics for pharmaceutical fentanyl‐ and NPFD‐associated fatalities
| Fentanyl type | Source | % male | Mean age (±SEM) | % female | Mean age (±SEM) |
|---|---|---|---|---|---|
| Pharmaceutical | Hospital | 66.7% (n = 13) | 42.4 ± 3.8 | 33.3% (n = 6) | 42.7 ± 9.6 |
| Prescription | 49.5% (n = 47) | 49.3 ± 2.2 | 50.5% (n = 48) | 54.7 ± 2.2 | |
| Illicit | 75.3% (n = 73) | 40.3 ± 1.5 | 24.7% (n = 24) | 46.5 ± 4.5 | |
| Unknown | 78.9% (n = 15) | 43.6 ± 3.4 | 21.1% (n = 4) | 39.0 ± 3.5 | |
| Pharmaceutical & NPFD | Unknown & illicit | 90% (n = 26) | 37.3 ± 1.5 | 10% (n = 3) | 22.7 ± 2.7 |
| NPFD | Illicit | 90% (n = 36) | 36.9 ± 1.5 | 10% (n = 4) | 44.8 ± 1.5 |
| Total fentanyl cases | 70.5% (n = 210) | 41.5 ± 0.9 | 29.5% (n = 88) | 49.4 ± 1.7 | |
| All England NPSAD cases | 73.6% | 37.8 ± 0.1 | 26.4% | 43.9 ± 0.2 |
4. DISCUSSION
Fentanyl prescriptions in England have increased dramatically over the last decade.24 Alongside their legitimate uses in healthcare provision and research, fentanyl and its derivatives have an established history of illicit use as alternatives or additives for heroin and other controlled opioids.31 Since 2009 there have been 28 new fentanyl derivatives detected on Europe's illicit drug market—10 of which were reported for the first time in 2017.15, 31 This made new opioids the largest group of novel psychoactive substances to appear on the European drug market in 2017—an accolade previously dominated by the synthetic cannabinoids and cathinones.15 The recent increase in availability of fentanyl and its derivatives in a community setting, from both legitimate and illicit sources, is having a demonstrable impact on drug‐related deaths in England.
4.1. Clinician administration of fentanyls is “very safe”
Pharmaceutical fentanyls are key in the delivery of modern medicine,6, 7, 8, 9, 10, 11, 12, 13 with their use most widespread in the delivery of general anaesthesia: more than 3.5 million patients are treated in NHS hospitals by anaesthetists every year.32 A UK‐wide survey indicates general anaesthetics are associated with a low mortality rate of 1 in 100,000, with elderly or infirm patients, or those undergoing emergency surgery at greatest risk.32 The NPSAD data presented here complements this recent survey, corroborating it with a low rate of reported cases and a single instance of fentanyl implication in death occurring in an elderly and infirm patient likely receiving palliative care. When administered under the direct supervision of healthcare professionals, fentanyls are demonstrably “very safe”.33
4.2. Fentanyl prescriptions require tighter regulation
Fentanyls undergo extensive first pass hepatic metabolism, making oral doses less effective than direct delivery into the blood stream, or by transdermal, buccal or nasal absorption.34 Consequentially, pharmaceutical fentanyls are available via prescription in patch, lozenge and spray preparations due to their ease of administration for untrained members of the public in an outpatient setting.9, 10, 11, 13 The recent increase in pharmaceutical fentanyl prescriptions16 correlates with an increasing number of fentanyl‐related deaths reported to NPSAD, where there is a high rate of implication and unintentional fatal administration. Fentanyl prescriptions require tighter regulation, both in their criteria for distribution and how their proper use is communicated to patients.
Additional controls and more stringent safeguarding of fentanyl prescriptions will not only reduce the risk of self‐harm for patients prescribed these medications, but also reduce their diversion for non‐medical use. It is these outpatient‐appropriate dosage forms of pharmaceutical fentanyls that are most susceptible for diversion, with the transdermal patch preparations being the most commonly misused.23 As misuse of illicit substances was more prevalent in those who unlawfully obtained a pharmaceutical fentanyl, it is evident that these individuals are more susceptible to possess illicit substance‐seeking behaviours. Diversion methods reported include: theft from pharmacies; patients selling patches; patients using fraudulent prescriptions; illicit sale by healthcare professionals; unused patches sold by relatives; and collection from the waste of hospitals and palliative care units.23 Patch preparations can contain 1 mg of active material,35 and with a non‐medical fentanyl dose in the order of 0.1 mg9 each patch even used only once can contain a number of doses viable for misuse.36 Once obtained, fentanyls are extracted from these patches and administered in a variety of ways: the fentanyl can be siphoned using a syringe and then injected; patches can be placed in a sealed container, heated and the fumes then inhaled; they can be smoked on foil; reused on the skin; and cut into pieces and placed in the mouth where they are sucked or swallowed.23 Cases reported to NPSAD where a pharmaceutical fentanyl was unlawfully obtained almost equal the number of cases reported where the pharmaceutical fentanyl was prescribed, and in these cases users will have received no guidance as to their proper use (e.g. dosages, length of administration) or warnings pertaining to contraindications or side‐effects from healthcare professionals. Indeed, the implication and unintentional death rates suggest ill‐ (or nil‐) informed fentanyl use. Increased availability in the community as a result of increases in fentanyl prescriptions16 facilitate diversion, and steps must be taken to tackle this ever‐increasing problem. However, previous attempts to address pharmaceutical fentanyl diversion have had varied success. The introduction of the matrix patch, where the fentanyl is impregnated into a mesh as a replacement for the gel reservoir formulation,36 prevents misuse via the syringe method, but this preparation is still vulnerable to other extraction techniques. The implementation of a “Patch‐for‐Patch” policy, introduced in Ontario, Canada,37 where patients must return used patches in exchange for new ones, saw a reduction in overall fentanyl prescribing, but not in opioid‐related deaths,38 and there have been reports of counterfeit fentanyl patches being returned.39
4.3. A rise in the availability of NPFDs
NPFDs are sourced from two principal routes: diversion of veterinary fentanyls (e.g. carfentanyl) and illicit production. Due to its extreme potency,14 a single vial of carfentanyl can be diluted down to produce thousands of doses,21 which when coupled with diversion from veterinary sources39 facilitates the availability of carfentanyl on the illicit drug market. Indeed, carfentanyl was found in a majority of NPFD cases reported to NPSAD. Instructions for the synthesis of carfentanyl40 and other NPFDs41, 42 are easily accessible via the internet, and production is relatively straightforward. This has led to an increase in the number of available NPFDs in recent years,15, 22 and is evidenced by their detection in cases reported to NPSAD. Their manufacture is not controlled under the drug control conventions of the United Nations, and can therefore be produced and traded with less risk than other substances.15 Again, due to high potencies where a few grams can make thousands of doses, they are easier to conceal and smuggle than other illicit drugs,15 but also by the same means represent a serious risk to law enforcement workers taking part in drug seizure operations. According to figures published by the United States Drug Enforcement Agency, importing and selling fentanyl has the potential to generate approximately 20 times more profit for drug trafficking organisations than heroin.43 When extrapolating these economics to the much more potent NPFDs, the profit margins are even greater.22 An additional driver for the recent increase in NPFD availability is a possible long‐term decline in heroin availability in Europe.22 Heroin shortages have previously paved the way for synthetic opioids, including NPFDs, to act as replacement products.22
The European Monitoring Centre for Drugs and Drug Addiction reports that in Europe fentanyl derivatives—mainly in the form of powders, tablets and liquids—are being seized in much larger quantities than ever before. There were 738 seizures in 2016 alone, with 4.6 litres of synthetic opioids seized, up from the 1.8 litres reported in the previous year.31 As yet, there is no evidence that illicit laboratories are producing NPFDs within the UK,22 with their source likely originating from China.15
4.4. NPFD use is inextricably linked with polydrug use
NPFDs are most commonly available in powder form whereupon they can be dissolved and injected, smoked or inhaled. On occasion they present in the form of tablets and small paper squares for ingestion, or liquids for injection.22, 32 They can be found in pure form, but are more often diluted by adulterants such as non‐opioid analgesics (e.g. paracetamol, ibuprofen) and caffeine, or added to heroin to act as fortification.15 NPFD cases reported to NPSAD have a high correlation with non‐opioid analgesic intake, heroin and cocaine, indicating their use as adulterants and reinforcing the notion that NPFD use is intricately linked with these markets.15 In Canada, the proportion of seized heroin samples found to include a fentanyl derivative has risen from less than 0.4% in 2012 to 40% in 2016 and 60% in 2017, with a fentanyl derivative being found at post‐mortem in 74% of opioid‐overdose cases in 2016.22 Marketed to consumers as heroin, oxycodone and hydrocodone pills,43 and even cocaine,15 it is unclear whether NPFDs are sold knowingly from the perspective of both vendors and customers.22 Unwitting NPFD consumption carries extreme risks, with no precautionary information available for consumers, and appropriate doses impossible to calculate, even for chronic opioid misusers. Polydrug use with alcohol, other illicit substances, and pharmaceutical medications (specifically CNS depressants such as benzodiazepines and Z‐drugs) has also been identified frequently in NPFD post‐mortem cases from across Europe,15 and is reflected in the NPSAD case reports presented here.
The marked number of NPFD cases reported to NPSAD where multiple fentanyl derivatives in combination with other opioids were found at post‐mortem adds weight to the already considerable argument for increasing access to the opioid antagonist naloxone.32 By widening naloxone availability, in combination with providing training in opioid overdose recognition and response, it is possible to prevent opioid‐related deaths from occurring. The development of new non‐injectable formulations, such as nasal sprays,44 has facilitated naloxone use in a wider range of settings where it can be administered by first responders, law enforcement, and friends and relatives of known opioid users. However, due to the higher potencies and longer duration of action of NPFDs,19, 20 even if naloxone is effectively administered, it may be followed by a relapse as naloxone is relatively short acting,45 and thus NPFD overdose cases would require repeat naloxone administrations.
4.5. Limitations
Due to the low tissue concentrations, high potencies and wide range of possible fentanyl derivatives, their post‐mortem detection has proved challenging.22 Fentanyls have previously not been included as part of the standard toxicology screen in suspected overdoses, with a number of retrospective toxicology reports recently performed resulting in reclassification of heroin overdose deaths to include fentanyls.22 Furthermore, standard gas chromatography–mass spectrometry screening methods are not able to detect highly potent NPFDs,46 requiring the more sensitive liquid chromatography tandem mass spectrometry instrumentation for detection, which is less readily available. Historically, fentanyl‐associated deaths are therefore under‐reported,39 with part of the increase seen in recent NPSAD reporting potentially an artefact of fentanyls now being tested for more routinely. However, as NPSAD is reported to voluntarily, and post‐mortems with fully comprehensive toxicology tests are not carried out for all deaths, the figures presented here likely under‐represent the true number of fentanyl‐associated deaths occurring in England. Testing for NPFDs will likely become more commonplace, as has occurred for the synthetic cannabinoids.47
5. CONCLUSIONS
The increasing availability of pharmaceutical fentanyls and NPFDs represents a serious risk to both public health and individuals, particularly males and those with established opioid misuse. Unintentional misuse of these compounds in England is contributing to the substantial increase in fentanyl‐associated deaths that is being observed at a global level. Of particular concern are the extreme potencies possessed by the NPFDs and the risks of unintentional death through the unsupervised consumption of pharmaceutical fentanyl, whether prescribed or obtained illicitly. More needs to be done to increase consumers' awareness of these risks, with improvements made to reduce diversion of prescribed fentanyls.
COMPETING INTERESTS
There are no competing interests to declare.
CONTRIBUTORS
H.C. conceived and designed the research, collected, analysed and interpreted the data, revised the article critically for important intellectual content, and approved the final version to be submitted. B.W. analysed and interpreted the data, revised the article critically for important intellectual content, and approved the final version to be submitted. C.C. conceived and designed the research, collected, analysed and interpreted the data, drafted the article, and approved the final version to be submitted.
ACKNOWLEDGEMENTS
The authors wish to thank Coroners for their assistance in providing data to NPSAD, and to Christine Goodair for aiding with case report data entry. The authors confirm that the Principal Investigator for the paper is Caroline S. Copeland.
Claridge H, Williams BD, Copeland CS. A deadly trend in fentanyl fatalities (England, 1998–2017). Br J Clin Pharmacol. 2020;86:437–444. 10.1111/bcp.14135
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Brownstein MJ. A brief history of opiates, opioid peptides, and opioid receptors. PNAS. 1993;90(12):5391‐5393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Waldhoer M, Barlett SE, Whistler JL. Opioid receptors. Annu Rev Biochem. 2004;73:953‐990. [DOI] [PubMed] [Google Scholar]
- 3. Katzung BG. Basic and Clinical Pharmacology. 14th ed. New York: McGraw‐Hill; 2017. [Google Scholar]
- 4. Stanley TH. The fentanyl story. J Pain. 2014;15(12):1215‐1226. [DOI] [PubMed] [Google Scholar]
- 5. Raffa RB, Pergolizzi JV Jr, Le Quang JA, et al. The fentanyl family: a distinguished medical history tainted by abuse. J Clin Pharmacol Ther. 2018;43:154‐158. [DOI] [PubMed] [Google Scholar]
- 6. Davis PJ, Cook DR. Clinical pharmacokinetics of the newer intravenous anaesthetic agents. Clin Pharmacokinet. 1986;11(1):18‐35. [DOI] [PubMed] [Google Scholar]
- 7. Ehieli E, Yalamuri S, Brudney CS, Pyati S. Analgesia in the surgical intensive care unit. Postgrad Med J. 2017;93(1095):38‐45. [DOI] [PubMed] [Google Scholar]
- 8. Bawden J, Villa‐Roel C, Singh M, et al. Procedural sedation and analgesia in a Canadian ED: a time‐in‐motion study. Am J Emerg Med. 2011;29(9):1083‐1088. [DOI] [PubMed] [Google Scholar]
- 9. Nelson L, Schwaner R. Transdermal fentanyl: pharmacology and toxicology. J Med Toxicol. 2009;5(4):230‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Taylor DR. Fentanyl buccal tablet: rapid relief from breakthrough pain. Expert Opin Pharmacother. 2007;8(17):3043‐3051. [DOI] [PubMed] [Google Scholar]
- 11. Mystakidou K, Panagiotou I, Gouliamos A. Fentanyl nasal spray for the treatment of cancer pain. Expert Opin Pharmacother. 2011;12(10):1653‐1659. [DOI] [PubMed] [Google Scholar]
- 12. Harris DG. Management of pain in advanced disease. Br Med Bull. 2014;110(1):117‐128. [DOI] [PubMed] [Google Scholar]
- 13. Aldington D, Jagdish S. The fentanyl “lozenge” story: from books to battlefield. J R Army Med Corps. 2014;160(2):102‐104. [DOI] [PubMed] [Google Scholar]
- 14. Leen JLS, Juurlink DN. Carfentanil: a narrative review of its pharmacology and public health concerns. Can J Anaesth. 2019;66(4):414‐421. [DOI] [PubMed] [Google Scholar]
- 15. European Monitoring Centre for Drugs and Drug Addiction . (2018) Fentanils and synthetic cannabinoids: driving greater complexity into the drug situation. Retrieved from: http://www.emcdda.europa.eu/system/files/publications/8870/2018-2489-td0118414enn.pdf. Accessed June 2019.
- 16. Fentanyl prescribing in England. https://openprescribing.net. Accessed April 2019.
- 17. Suh YG, Cho KH, Shin DY. Total synthesis of fentanyl. Arch Pharm Res. 1998;21(1):70‐72. [DOI] [PubMed] [Google Scholar]
- 18. Killgore JK, Jacob M. Methods for the synthesis of alfentanil, sufentanil and remifentanil. Patent ID: US7208604. 2007.
- 19. Armenian P, Vo KT, Barr‐Walker J, Lynch KL. Fentanyl, fentanyl analogs and novel synthetic opioids: a comprehensive review. Neuropharmacology. 2018;134(Pt A):121‐132. [DOI] [PubMed] [Google Scholar]
- 20. Mounteney J, Giraudon I, Denissov G, Griffiths P. Fentanyls: are we missing the signs? Highly potent and on the rise in Europe. Int J Drug Policy. 2015;26(7):626‐631. [DOI] [PubMed] [Google Scholar]
- 21. European Monitoring Centre for Drugs and Drug Addiction . European drug report 2014: Trends and developments. 2014. Retrieved from: http://www.emcdda.europa.eu/attachements.cfm/att_228272_EN_TDAT14001ENN.pdf. Accessed June 2019.
- 22. European Monitoring Centre for Drugs and Drug Addiction . Fentanyl in Europe EMCDDA trendspotter study. 2012. Retrieved from: http://www.emcdda.europa.eu/attachements.cfm/att_191974_EN_TD3112230ENN_Fentanyl.pdf. Accessed June 2019.
- 23. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid involved overdose deaths—United States, 2010–2015. Morb Mortal Wkly Rep. 2016;65(50‐51):1445‐1452. [DOI] [PubMed] [Google Scholar]
- 24. Peterson AB, Gladden RM, Delcher C, et al. Increases in fentanyl‐related overdose deaths—Florida and Ohio, 2013–2015. MMWR Morb Mort Wkly Rep. 2016;65:844‐849. [DOI] [PubMed] [Google Scholar]
- 25. Special Advisory Committee on the Epidemic of Opioid Overdoses . National report: Apparent opioid‐related deaths in Canada (Released March 2018). Web‐based Report. Ottawa: Public Health Agency Canada; 2017. Retrieved from: https://www.canada.ca/en/public-health/services/publications/healthy-living/national-report-apparent-opioid-related-deaths-released-march-2018.html. Accessed June 2019. [Google Scholar]
- 26. Corkery JM, Loi B, Claridge H, Goodair C, Schifano F. Deaths in the lesbian, gay, bisexual and transgender United Kingdom communities associated with GHB and precursors. Curr Drug Metab. 2018;19(13):1086‐1099. [DOI] [PubMed] [Google Scholar]
- 27. When a death is reported to a Coroner. Retrieved from: https://www.gov.uk/after-a-death/when-a-death-is-reported-to-a-coroner. Accessed August 2019.
- 28. United Nations Office on Drugs and Crime . Recommended Methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens. United Nations Office on Drugs and Crime; 2017. Retrieved from: https://www.unodc.org/documents/scientific/Recommended_methods_for_the_identification_and_analysis_of_Fentanyl.pdf. Accessed August 2019. [Google Scholar]
- 29. Harding SD, Sharman JL, Faccenda E, et al. The IUPHAR/BPS Guide to PHARMACOLOGY in 2018: updates and expansion to encompass the new guide to IMMUNOPHARMACOLOGY. Nucleic Acids Res. 2018; 46:D1091‐D1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alexander SPH, Kelly E, Marrion NV, et al. THE CONCISE GUIDE TO PHARMACOLOGY 2017/18: Overview. Br J Pharmacol. 2017; 174(S1):S1‐S16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. European Monitoring Centre for Drugs and Drug Addiction (2018). European Drug Report: Trends and Developments. Retrieved from: http://www.emcdda.europa.eu/system/files/publications/8585/20181816_TDAT18001ENN_PDF.pdf. Accessed June 2019.
- 32. Sury MRJ, Palmer JHMG, Cook TM, Pandit JJ, Mahajan RP. The state of UK anaesthesia: a survey of National Health Service activity in 2013. Br J Anaesth. 2014;113:575‐584. [DOI] [PubMed] [Google Scholar]
- 33. Royal College of Anaesthetists (2014). Nationwide survey of all UK hospitals shows anaesthetic care is consultant delivered and very safe. Retrieved from: https://www.rcoa.ac.uk/news-and-bulletin/rcoa-news-and-statements/nationwide-survey-of-all-uk-hospitals-shows-anaesthetic. Accessed June 2019.
- 34. Mather LE. Opioid pharmacokinetics in relation to their effects. Anaesth Intensive Care. 1987;15(1):15‐22. [DOI] [PubMed] [Google Scholar]
- 35. Lötsch J, Walter C, Parnham MJ, Oertel BG, Geisslinger G. Pharmacokinetics of non‐intravenous formulations of fentanyl. Clin Pharmacokinet. 2013;52(1):23‐36. [DOI] [PubMed] [Google Scholar]
- 36. Van Nimmen NF, Veulemans HA. Validated GC‐MS analysis for the determination of residual fentanyl in applied Durogesic reservoir and Durogesic D‐trans matrix transdermal fentanyl patches. J Chromatogr B Analyt Technol Biomed Life Sci. 2007;846(1‐2):264‐272. [DOI] [PubMed] [Google Scholar]
- 37. Safeguarding our Communities Act (Patch for Patch Return Policy). 2015. Retrieved from: https://www.ontario.ca/laws/statute/15s33. Accessed June 2019.
- 38. Public Safety Canada (2018). Assessment of the Impact of the Ontario Fentanyl Patch‐for‐Patch Return Program. Retrieved from: https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/2017-s023/2017-s023-en.pdf. Accessed June 2019.
- 39. Pharmacy Connection (2018). Identifying Counterfeit or Tampered Fentanyl Patches. Retrieved from: https://pharmacyconnection.ca/counterfeit-fentanyl-patches-spring-2018/. Accessed June 2019.
- 40. World Health Organisation Expert Committee on Drug Dependence (2017). Carfentanil Critical Review Report. Retrieved from: https://www.who.int/medicines/access/controlled-substances/Critical_Review_Carfentanil.pdf. Accessed June 2019.
- 41. Huang B‐S, Deutsche K, Terrell RC, Kudzma LV. N‐aryl‐N‐(4‐piperidinyl)amides and pharmaceutical compositions and method employing such compounds. Patent ID: US4584303. 1985.
- 42. Janssen PA. N‐(1‐alkyl‐4‐piperidyl)‐Narylalkanoamides. Patent ID: FR1517671(A). 1968.
- 43. US Department of Justice Drug Enforcement Administration (2017). National Drug Threat Assessment. Retrieved from: https://www.dea.gov/sites/default/files/docs/DIR-040-17_2017-NDTA.pdf. Accessed June 2019.
- 44. Wermeling DP. A response to the opioid overdose epidemic: naloxone nasal spray. Drug Deliv Transl Res. 2013;3(1):63‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ryan SA, Dunne RB. Pharmacokinetic properties of intranasal and injectable formulations of naloxone for community use: a systematic review. Pain Manag. 2018;8(3):231‐245. [DOI] [PubMed] [Google Scholar]
- 46. Swanson DM, Hair LS, Strauch Rivers SR, et al. Fatalities involving carfentanil and furanyl fentanyl: two case reports. J Anal Toxicol. 2017;41(6):498‐502. [DOI] [PubMed] [Google Scholar]
- 47. Ford LT, Berg JD. Analytical evidence to show letters impregnated with novel psychoactive substances are a means of getting drugs to inmates within the UK prison service. Ann Clin Biochem. 2018;55(6):673‐678. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


