INTRODUCTION
One out of 7 adults used marijuana in 2017.1 The concentration of tetrahydrocannabinol (THC), the primary psychoactive component of marijuana is increasing in commercially available products.2 However, there is little safety data available on the acute effects of cannabis outside of its psychoactive effects. One area of interest is the acute cardiovascular effects of marijuana given the ubiquitous presence of endocannabinoid receptors in the myocardium, coronary endothelium, and vascular endothelial and smooth muscle cells.3 We conducted a systematic review to examine the acute cardiovascular effects of marijuana use.
METHODS
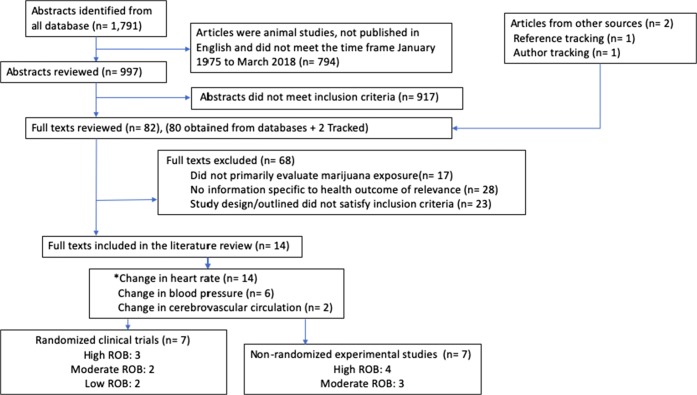
We searched PubMed, MEDLINE, EMBASE, PsychINFO, and Cochrane Library for all English-language experimental studies examining marijuana use and acute cardiovascular effects between January 1, 1975, and March 31, 2018. Our search using MeSH terms outlined in Figure 1 yielded 1791 articles. We exclude articles with less than 20 participants. Two reviewers (M.G. and D.R.) selected 997 abstracts for review of which 80 met inclusion criteria and were selected for full text review. Two papers were added via author and reference tracking. Inter-rater reliability for the abstract selection process and the concurrent decision to include the article was excellent (Cohen kappa 0.87). We discussed the overall strength of evidence as a group for each outcome and graded it as insufficient, low, moderate, or high risk of bias (ROB) using methods outlined by the AHRQ.4 The protocol was registered on Prospero at the start of our review (No. CRD42016051297).
Figure 1.
Flow of articles in the review. MeSH terms: (Marijuana OR Marihuana OR Tetrahydrocannabinol OR Cannabinoid) AND (Hypertension OR Hypotension OR Blood pressure OR Heart Rate OR Bradycardia OR Tachycardia OR Arrhythmia OR Hemodynamics OR Syncope OR Cerebrovascular Constriction). An asterisk indicates that some studies were assigned more than one outcome label and are counted twice.
RESULTS
Article Characteristics
Fourteen articles focused on change of heart rate (HR), 6 on blood pressure (BP), and 2 on cerebrovascular circulation in response to marijuana administration. Among these, 7 were randomized clinical trials (RCT) and 7 were non-randomized experimental studies. Twelve out of 14 studies employed inhalation/smoking as the route of exposure. THC content in smoke ranged from 1.5 to 3.6% per cigarette (equal to 14 to 35 mg). The highest dose of THC administered as edible or an injection was 17.5 and 5 mg, respectively. Half the articles were rated as high ROB (Table 1).
Table 1.
Summary of Experimental Studies that Examined Exposure to Marijuana and Acute Cardiovascular Changes
| Study year, citation, and design | Study population | Dose of MJ exposure | Outcome examined | Result in study | Risk of bias† |
|---|---|---|---|---|---|
| Klumpers LE, et al. 2012 “Novel Delta (9) THC formulation Namisol (R) has beneficial pharmacokinetics and promising pharmacodynamic effects.” Br J Clin Pharmacol. RCT | 21 healthy MJ users, age 18 to 55, mean age 21.6 | Panel I: 5 mg oral or sublingual THC. Panel II: 6.5 or 8 mg oral THC or matching placebo | 1.Tachycardia |
• Exposure to 5 mg oral THC showed no significant difference in HR (p = 0.9261) compared with 5 mg sublingual THC in pane I. • Exposure to 6.5 and 8 mg THC showed significant increase in HR (p = 0.0019 and p = 0.0014, respectively) compared with placebo control group. |
Low |
| Cooper, et al. 2009 “Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts.” Drug and alcohol dependence. RCT | 24 young healthy current MJ users, age 21 to 45, mean age 25.5 | MJ blunt: 1.8, 3.6% THC or MJ cigarette: 1.8, 3.6% THC or placebo | 1.Tachycardia |
• Subjects randomized to receive placebo, a MJ blunt, or MJ cigarette. • Exposure to highest dose of both joints and blunts MJ showed significant increase in HR (p ≤ 0.05) compared with inactive MJ (placebo). There was no difference in tachycardia between blunts and joints. |
High |
| D’souza, et al. 2008 “Blunted psychotomimetic and amnestic effects of Δ-9-tetrahydrocannabinol in frequent users of cannabis.” Neuropsychopharmacology. RCT | 30 frequent cannabis users and 22 healthy controls, age 18 to 55, mean age 26.9 | 2.5 mg or 5 mg THC per injection or placebo | 1.Tachycardia |
• Subjects randomized to receive placebo, 2.5 or 5 mg THC through injection. • Exposure to cannabis showed increase in HR in a dose-dependent manner (dose: F (1,427) = 65.5, p < 0.0001); dose*time (F (8,427) = 21.1, p < 0.0001) with no significant group differences, even at baseline compared with controls. |
Moderate |
| Mathew, et al. 2003 “Postural syncope after marijuana: a transcranial Doppler study of the hemodynamics.” Pharmacol Biochem Behav. RCT | 29 young healthy experienced MJ users, age 20–38, mean age 25.5 | 3.55% smoke THC or 0.2 mg/ml infusion THC in albumin (4 mg total) or placebo |
1.Increase in pulse rate 2.Decrease in BP 3.CBV |
• Subjects divided to 2 groups (MJ cigarette or placebo) and (THC injection and placebo). • Exposure to MJ showed increase in resting pulse rate (F = 87.46, df = 1,27, p < .001) in both groups with no group differences. • Exposure to MJ showed drop in systolic BP (t = 2.90, df = 27, p < 0.01) • Exposure to MJ showed greater drop in CBV (t = 2.92, df = 27, p < 0.007) in more DZ group. |
Low |
| Chait Perry, et al. 1994 “Acute and residual effects of alcohol and marijuana, alone and in combination, on mood and performance.” Psychopharmacology. RCT | 20 young healthy current MJ users, age 21 to 34, mean age 24.7 | 3.6% THC per cigarette | 1.Tachycardia |
• Subjects grouped as placebo alcohol, low and high alcohol conditions with average of 4.7 ± 0.4, 4.7 ± 0.3, and 5.1 ± 0.4 MJ cigarette exposure, respectively. • Exposure to MJ showed increase in HR with mean (± SE) of 17.1 ± 2.5, 17.8 ± 2.5, and 18.7 ± 2.2 for placebo alcohol, low and high alcohol conditions. It also showed HR increases was moderately correlated to number of MJ cigarette (r = 0.45). |
Moderate |
| Lex, et al. 1984 “Effects of acute marijuana smoking on pulse rate and mood states in women.” Psychopharmacolog. RCT | 28 young female MJ users, age 21 to 36, mean age 26.07 | 1.8% THC per cigarette or placebo | 1.Tachycardia |
• Pulse rate was recorded 30 min prior and at 15, 30, 90, and 180 min post-exposure. • Exposure to MJ showed differences in PR at 15 min (p < 0.01 for both regular and intermittent smokers) and 30 min (p < 0.01 for regular smokers, p < 0.001 for intermittent smokers) compared with placebo. |
High |
| Pihl, et al. 1978 “The effect of marihuana intoxication on blood pressure.” J Clin Psychol. RCT | 48 young male experienced MJ users, age 18 to 35, mean age 23 | Low does MJ: 0.005 g or 0.003 g THC per cigarette, high dose MJ: 0.006 g or 0.0045 g THC per cigarette |
1.Tachycardia 2.Increase/decrease in BP |
• Subjects randomized to receive coltsfoot, placebo, low dose MJ, and high dose MJ. • Exposure to MJ showed highly significant differences in PR (drug*time F = 4.62, df = 1/44, p < 0.01) between the groups. • Exposure to MJ showed no significant differences in SBP and DBP between the groups. However, it showed significant differences between pre-post-exposure and decrease in SBP (F = 5.34, df = 1/44, p < 0.05). |
High |
| Ponto, et al. 2004 “Effect of acute marijuana on cardiovascular function and central nervous system pharmacokinetics of [15O] water: effect in occasional and chronic users.” J Clin Pharmacol. Experimental study | 12 occasional and 12 chronic MJ users, age 20 to 36, mean age 22.1 | 20 mg THC per cigarette or placebo |
1.Tachycardia 2.Increase/decrease in BP 3.Cerebral blood flow |
• Subjects randomized to receive placebo or active MJ cigarette. • Exposure to MJ showed significant relation between change in HR and MJ use status (p < 0.0001) with the repeated-measures ANOVA. • Exposure to MJ showed no difference between MJ use (occasional and chronic) status and change in SBP or DBP. • Exposure to MJ showed no change in global cerebral blood flow (evaluated via PET scans) between MJ and placebo groups. |
High |
| Mathew, et al. 1993 “Depersonalization after marijuana smoking.” Biol Psychiatry. Experimental study | 35 young healthy MJ users, mean age 27.1 | 1.75%, 3.55% THC per cigarette or placebo |
1.Tachycardia 2.Increase/decrease in BP |
• Subjects randomized to receive placebo, 1.75% or 3.55% THC cigarette. • Exposure to MJ showed significant linear association between MJ dose and PR [drug*time interaction (F) = 14.79, p < 0.001]. • Exposure to MJ showed slight but significant linear association between MJ dose and decrease in systolic BP [F = 3.08, p < 0.02]. |
Moderate |
| Mendelson, et al. 1984 “Reinforcing properties of oral Δ 9-tetrahydrocannabinol, smoked marijuana, and nabilone: Influence of previous marijuana use.” Psychopharmacology. *Experimental study | 23 young healthy male MJ users, age 22 to 30, mean age 25.5 | 2 mg oral nabilone or 1 g MJ cigarette (1.83% THC) or 17.5 mg oral THC or placebo | 1.Tachycardia |
• Exposure to MJ showed significant increase in PR (p < 0.01) among intermittent and occasional users following MJ smoking. • Exposure to MJ showed a small but significant increase in PR (p < 0.05) among regular and intermittent users following oral THC administration. However, it showed a greater increase in PR among occasional users (p < 0.01). • Exposure to MJ showed a small but statistically significant elevation in PR (p < 0.05) among all subjects following nabilone administration (no tachycardia observed). |
Moderate |
| Ashton, et al. 1981 “The seed and the soil: effect of dosage, personality and starting state on the response to delta 9 tetrahydrocannabinol in man.” Br J Clin Pharmacol. Experimental study | 32 young healthy MJ users, mean age 23.4 |
Exp1: 2.5 mg or 10 mg THC per cigarette. Exp2: 8 mg THC per cigarette or placebo |
1.Tachycardia |
• Exposure to 2.5 mg THC showed 14.5% increase in HR 1 min after smoking compared with the mean pre-smoking rate in experiment 1. It also showed 34.8% increase in HR 15 min after smoking of 10 mg THC. • Exposure to 8 mg THC showed increase in HR by mean rise of 12.6 bpm 13 min after smoking compared with placebo. |
High |
| Miller, et al. 1977 “Marijuana: Dose-response effects on pulse rate, subjective estimates of potency, pleasantness, and recognition memory.” Pharmacology. Experimental study | 32 healthy male moderate MJ users, age 21 to 28 | 5, 10, 15 mg THC per cigarette or placebo | 1.Tachycardia |
• Exposure to MJ showed linear association between MJ dose (F = 4.97, df = 3, 28; p < 0.007), time effect (F-43.37, df = 3.84, p < 0.0001) and dose*time interaction (F = 8.03, df = 9.84, p < 0.0001). • Exposure to MJ showed increase in PR with dose up to 10 mg with mild reversal at 15 mg dose. |
Moderate |
| Bernstein, et al. 1976 “Medical implications of marijuana use.” Am J Drug Alcohol Abuse. Experimental study | 27 young healthy male MJ users, mean age 23.4 | 2.1% THC per cigarette |
1.Tachycardia 2.Increase/decrease in BP |
•Exposure to MJ showed increase in PR following MJ smoking. It also showed tachycardia was more prominent when the pulse was counted with the subject in the standing position following MJ smoking. • No significant association between MJ smoking and change in BP. |
High |
| Steadward, et al. 1975 “The effects of smoking marihuana on physical performance.” Med Sci Sports. Experimental study | 20 young healthy male MJ users, age 21 to 27, mean age 23.1 | 18.2 mg THC per cigarette or 1.4 mg placebo |
1.Tachycardia 2.Increase in BP |
• Subjects randomized to receive placebo or active MJ cigarette. • Exposure to MJ showed a significant increase in HR (p < 0.05) from control to MJ and from placebo to MJ. • Exposure to MJ showed a significant increase in SBP and DBP (p < 0.05) compared with controls and placebo. |
High |
BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure; HR, heart rate; MG, milligram; MJ, marijuana; PR, pulse rate; RCT, randomized control trial; RR, relative risk; THC, tetrahydrocannabinol; CBV, cerebral blood velocity; ANOVA, analysis of variance
*All studies examined the plant form of MJ except *study which also examined the synthetic form
†We used the Cochrane Risk of Bias Tool for Clinical Trials, and NIH Quality Assessment Tool for Controlled Intervention Studies to assess risk of bias (ROB)
Heart Rate
All 14 studies (7 RCTs and 7 non-randomized experimental) rated as low to high ROB reported marijuana use was associated with tachycardia. The 2 low ROB RCT studies reported increase in HR after exposure to 3.55% smoke, 8 mg oral, or 4 mg injection THC. Two moderate ROB RCTs found an increase in HR in a dose-dependent manner. Two non-randomized studies (moderate ROB) found a linear association between use and tachycardia. The last moderate ROB (non-randomized experimental) study reported all forms of marijuana (1.83% smoked, 17.5 mg oral THC, and 2 mg synthetic nabilone) increased HR.
Blood Pressure
Six studies examined BP as an outcome (2 RCTs, and 4 non-randomized experimental studies). Findings were mixed. In one study (RCT, low ROB) exposure to 3.55% THC per cigarette or 4 mg THC per injection showed a drop in systolic BP (p < 0.01). The non-randomized study (moderate ROB) reported a linear association between marijuana dose (1.75 to 3.55%) and decreasing systolic BP. The remaining 4 high ROB studies had mixed findings with 3 studies showing no effect and one study reporting an increase in BP.
Cerebrovascular Circulation
Exposure to 3.55% THC per cigarette or 4 mg THC injection (RCT, low ROB) showed drop in cerebral blood velocity (p < 0.007) while administration of 20 mg THC per cigarette (equal to 2.08% THC) in a second study (non-randomized study, high ROB) showed no association with change in global cerebral blood flow (Table 1).
DISCUSSION
Low strength evidence suggests that marijuana use is associated with tachycardia. There was insufficient evidence on the relationship between marijuana use and acute changes in blood pressure and cerebrovascular circulation.
While the psychoactive effects of THC are well known,5 our review suggests that low concentrations of THC can cause tachycardia which may have health implications for older adults with vascular disease. The studies included this review had lower concentration of THC compared with products currently on the market. The highest dose of THC used in experimental studies in our review was 3.6% per cigarette. Pre-rolled cannabis cigarettes available for purchase in cannabis dispensaries contain THC concentrations often exceeding 18% and reaching as high as 35%.2, 6 This is particularly concerning in older population with existing cardiovascular disease where acute hemodynamic changes may precipitate adverse outcomes.
Our study has several limitations. We may have overlooked relevant studies published outside of our predefined timeline. In addition, studies were conducted in young health populations limiting generalizability.
In conclusion, low concentrations of THC are associated with tachycardia among largely healthy and young populations. More safety data on use of high concentrations of THC and in clinically diverse populations are needed.
Authors’ Contribution
SK had the idea for the study. SK, MG, DR, DK, and TC created the study design. MG and DR collected the data. SK verified the data. MG, DR, DK, and SK analyzed and interpreted the data. SK and MG wrote and revised the manuscript. All authors critically revised the manuscript and approved the final version for submission. SK is the guarantor.
Compliance with Ethical Standards
Conflict of Interest
All authors declare that they have no conflict of interest.
Ethical Approval
Not needed.
Data Sharing
Data set available from corresponding author on request.
Transparency
The manuscript’s guarantor (SK) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned have been explained.
Footnotes
Prior Presentations
SGIM meeting Washington DC, April 19–22, 2017 presented.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Steigerwald S, Wong PO, Cohen BE, Ishida JH, Vali M, Madden E, et al. Smoking, vaping, and use of edibles and other forms of marijuana among US adults. Ann Intern Med. 2018;169(12):890–892. doi: 10.7326/M18-1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Steigerwald S, Wong PO, Khorasani A, Keyhani S. The form and content of cannabis products in the United States. J Gen Intern Med. 2018. 10.1007/s11606-018-4480-0. [DOI] [PMC free article] [PubMed]
- 3.Pacher P, Bátkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58:389–462. doi: 10.1124/pr.58.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkman ND, Lohr KN, Ansari M, McDonagh M, Balk E, Whitlock E, et al. Grading the Strength of a Body of Evidence When Assessing Health Care Interventions for the Effective Health Care Program of the Agency for Healthcare Research and Quality: An Update. Methods Guide for Comparative Effectiveness Reviews. (Prepared by the RTI-UNC Evidence-based Practice Center under contract no. 290-2007-10056-I.) AHRQ publication no. 13(14)-EHC130-EF. Rockville: Agency for Healthcare Research and Quality; November 2013. Accessed at https://ahrq-ehc-application.s3.amazonaws.com/media/pdf/methods-guidance-grading-evidence_methods.pdf on 12 October 2017.
- 5.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–27. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LaFrate A. Colorado Marijuana Study Finds Legal Weed Contains Potent THC Levels. NBCNews.com, Accessed at https://marijuanaharmlessthinkagain.org/wp-content/uploads/2014/04/Colorado-Marijuana-Study-Finds-Legal-Weed-Contains-Potent-THC-Levels.pdf on 23 March 2015.