Abstract
Clinicians face many challenges when treating immature permanent teeth in young patients. Immediate blood clot induction can be a successful option as described by some case reports. No experimental studies or clinical trials have addressed this question. We have designed a clinical trial in which we hypothesized that there is no difference in success between immediate or delayed induction protocols. After confirmation of pulpal necrosis, patients were randomized. In the delayed group, 15 teeth were treated following the American Association of Endodontists guidelines, and calcium hydroxide was used as the intracanal medication. In the immediate group, 13 teeth had a blood clot inducted at the first appointment. The teeth were evaluated after 1, 3, and 12 months. Three independent evaluators assessed the periapical healing. The Pearson chi-square test or the Fisher exact test was used to compare the success rates between the 2 groups. Currently, of the 25 recruited patients (28 teeth), 19 have completed their 12-month follow-up. The group with delayed induction had a 71% success rate, and the group with immediate induction had a 33% success rate. In most cases (79%), trauma was the etiology. All successful cases started at stage 9 of root development (Nolla), and the majority showed healing type 2. Determination of the stage of root formation and etiology are possible critical factors for any therapeutic decision. In summary, it is early to conclude or suggest any of the protocols. Clearly, much more data are needed before sample size requirements can be met.
Keywords: Calcium hydroxide, immature necrotic teeth, regenerative endodontics, revascularization, single visit
For over a decade, the American Association of Endodontists (AAE) has promoted regenerative endodontic procedures (REP). This has been possible because of the collaborative work and research support by the Regenerative Endodontic Committee, the AAE Foundation, and the endodontic community. The number and impact of regenerative endodontic publications have increased rapidly in recent years. In recognition, the Journal of Endodontics has added a subheading of “Regenerative Endodontics” to its table of contents. Although the research in this area is looking for high levels of evidence, many clinicians have used published case reports to develop their regenerative procedures. Immature necrotic teeth can be successfully treated by REPs in the short-term, but the long-term outcome is still missing. Many questions remain unanswered. Can an REP be effectively applied in 1 appointment? Are interappointment intracanal medicaments needed? Are treated teeth more brittle? Can treated teeth be moved orthodontically? What kind of tissue is formed when pulps heal? What are the criteria for case selection? Higher levels of evidence are needed. Randomized clinical trials are required to provide plausible answers to these questions.
The AAE provides clinical recommendations for REPs, which are based on successful case reports and in vitro studies (1). Although several case series and pilot studies have been published, the protocol used varies on important factors such as the concentration and type of intracanal irrigation (sodium hypochlorite, calcium hydroxide [Ca(OH)2], or chlorhexidine), the type of interappointment medication (Ca[OH]2 or triple or double antibiotic paste), the capping material (gray or white mineral trioxide aggregate [MTA]), and the incorporation or lack of scaffold material (collagen or platelet-rich plasma) (2-9). Even the outcome expected varies as shown by prospective and retrospective case series studies. Outcomes were categorized as survival or success based on subjective evaluation of periapical healing and the increase in root width and root length (10, 11). Others have then categorized their outcome by the assessment of qualitative periapical healing and quantitative root width and length (12). For example, Chen et al (4) classified their outcome by 5 types of possible healing ranging from normal root continuation to severe calcification and hard tissue formation. This leads us to the conclusion that, despite several efforts to develop clinical guidelines, there are many variables to consider when we select a protocol and design a clinical study. Only a few clinical trials have been reported, and several are ongoing although no data have been published thus far (Table 1).
TABLE 1.
Randomized Clinical Trials (clinicaltrial.gov)
| Title | Sponsor | Sample | Time frame/status | Protocols |
|---|---|---|---|---|
| Comparison of Two Dental Techniques Used to Treat Teeth Which Have Become Infected of Painful Following Trauma Comparison | University of Liverpool, England | 30 | Completed February 2011–August 2015 | 1. Revitalization 2. MTA apexification |
| Regenerative Endodontic Procedure of Immature Permanent Teeth With L-PRF: a Pilot Controlled, Clinical Trial | Universitaire Ziekenhuizen Leuven Belgin | 20 | Collecting September 2014–September 2020 | 1. REP with L-PRF biological: stem and
progenitor cells 2. REP |
| Regenerative Endodontic Procedure of Immature Permanent Teeth With PRF: A Pilot Randomized Controlled Trial | Fujian Medical University, China | 50 | Collecting May 2013–February 2017 | 1. REP (TAP)/PRF-MTA 2. REP (TAP)/MTA |
| Revitalization of Immature Permanent Teeth With Necrotic Pulps Using SHED Cells | Fourth Military Medical University, China | 80 | Collecting February 2013–October 2017 | Scaffold-free SHED-deprived pellet single-group assignment |
| Regeneration of Pulp-Dentin Development in Teeth With Necrotic Pulps and Immature Roots | Loma Linda University University of North Carolina University of Texas Health Science Center at San Antonio | 120 | Collecting September 2014–November 2019 | 1. TAP/Emdogain (Institut Straumann AG,
Basel, Switzerland)/MTA 2. TAP/Collaplug (Calcitek, Carlsbad, CA)/MTA 3. MTA apexification |
L-PRF, leucocyte and platelet-rich fibrin; MTA, mineral trioxide aggregate; PRF, platelet-rich fibrin; REP, regenerative endodontic procedure; SHED,stem cells from human exfoliated deciduous teeth; TAP, triple antibiotic paste.
Clinicians face many challenges when treating immature permanent teeth in young patients. These include patient behavior and anatomic features such as the lack of apical constriction and short and thin roots. Besides these challenges, the primary target of the latest regenerative clinical guidelines by the AAE includes the preservation of vitality of the apical papilla and its stem cells (1). In 2008, Huang et al (13) hypothesized that partial survival of the dental apical papilla after pulpal necrosis in immature permanent teeth is responsible for the successful outcomes. Lovelace et al (14) found a significant number of stem cells coming from the apical bleeding during the induction of a blood clot in immature teeth compared with the number in circulating blood. The cytotoxicity of the intracanal irrigants used for REP has consistently shown that chlorhexidine and sodium hypochlorite inhibit stem cell attachment to dentinal walls. On the other hand, EDTA promotes stem cell attachment and differentiation and does so even after prior use of chlorhexidine and sodium hypochlorite (15-18). The use of full-strength intracanal antibiotics inhibits stem cell growth and leads to cell death. Other advocated intracanal medicaments at high concentrations have also been questioned. Calcium hydroxide supports the induction of stem cell growth and is much more easily removed from dentinal walls than tetracycline-containing pastes (19, 20).
One possible strategy that may favor maintenance of the vitality of the apical papilla is to complete the treatment in a single appointment with immediate blood clot induction. This might also enhance patient compliance (7,21-23). However, there is little experimental evidence to support a single-appointment protocol, except for a single in vivo study in beagle dogs (24). In this study, their protocol included the use of 2.5% sodium hypochlorite (Endovac; Kerr, Orange, CA), minimal instrumentation, and immediate blood clot induction. The study showed a comparable outcome with the group in which the traditional 2-visit protocol was used. This traditional protocol included triple antibiotic paste with blood clot induction at a subsequent appointment (24). Some case reports do describe successful outcomes after an immediate blood clot induction, but no experimental studies or clinical trials have addressed this question (21-25). With this knowledge gap in the literature identified, we have designed a clinical trial in which we have hypothesized that there is no difference between immediate or delayed induction in terms of the successful outcome of periapical healing and the increase in root width and root length. Here we describe the designed clinical trial along with the preliminary findings.
Materials and Methods
Randomized Clinical Trial Design
The Institutional Review Board of the University of Michigan, Ann Arbor, MI, approved the research protocol, and the study has been conducted since 2012 at the Graduate Endodontic Clinic, School of Dentistry, University of Michigan. Nonpregnant, healthy, American Society of Anesthesiologists (ASA) physical status classification 1 and 2, and cooperative 6- to 25-year-old patients were screened for the study. Patients diagnosed with pulp necrosis on an immature permanent tooth or patients with at least 1 open apex of 1 mm or more in diameter were recruited. Selected teeth needed to be restorable and not periodontally involved (no periodontal probing >4 mm). Teeth with evidence of internal or external resorption, ankylosis, or root fracture were excluded from the study.
All potential participants were evaluated clinically and radiographically. The evaluation included assessment of pain, swelling, and/or presence of a sinus tract. Percussion of the tooth, palpation of the periapical area, discoloration of the crown, mobility, and probing depths were also recorded. Vitality tests were conducted using a cold stimulus with Endo-Ice (Coltène/Whaledent Inc, Cuyahoga Falls, OH) and an electrical stimulus with a pulp tester (Analytic Technology, Redmond, WA). Radiographs were obtained with the use of prefabricated bite registration material using Blu-Bite and a parallel system (Fast Set Berry and XCP Film Holding System; Henry Schein, Inc, Melville, NY). All eligible patients or their guardians signed informed consent/assent forms.
Clinical Procedures
The treated teeth were anesthetized with mepivacaine HCl 3% under rubber dam isolation. Access was performed, and the diagnosis of pulp necrosis was confirmed. The working length was determined with the use of the Root ZX apex locator (J. Morita USA, Inc, Irvine, CA) and confirmed with a radiograph. To verify an open apex of at least 1.0 mm or more, size of the apical foramen was confirmed with 100/0.02 size gutta-percha material. Canals were irrigated with 20 mL 2.5% sodium hypochlorite. Minimal instrumentation was performed with nonbinding K-files. Afterward, the canal was irrigated with 3 mL saline followed by 3 mL 17% EDTA for no less than 2 minutes. All irrigation was performed 1–2 mm short of the working length, and the canal was dried with paper points. Case randomization was performed using a random number generated by an online calculator. Each case was assigned to 1 of the 2 treatment protocols: immediate or delayed induction.
Treatment Protocol 1: Immediate Induction
A size 20 K-file with a bent tip was placed 2–3 mm past the apex to induce bleeding into the canal. Fifteen minutes was allowed to obtain a blood clot that would reach the coronal third of the canal. If bleeding did not occur, patients were transferred into the rescue treatment protocol group. The rescue protocol follows the procedures described in the delayed induction protocol. After the blood clot formation was achieved, a small Collacote piece (Zimmer Dental, Carlsbad, CA) was placed on the blood clot followed by 2–3 mm of white MTA (ProRoot; Dentsply Tulsa Dental, Tulsa, OK). A radiograph was taken, and a small sponge was placed before temporization with glass ionomer (GC Fuji IX GP; GC America Inc, Alsip, IL). The occlusion was evaluated and adjusted. If a sinus tract was present, 0.12% chlorhexidine (21) (Peridex; 3M ESPE, St Paul, MN) was used to irrigate the sinus tract before patient dismissal.
Treatment Protocol 2: Delayed Induction
Ca(OH)2 (Multi-Cal; Pulpdent, Watertown, MA) was used as an interappointment medicament to fill the entire canal, and the pulp chamber access was closed with glass ionomer (GC Fuji IX GP). The occlusion was evaluated and adjusted. If a sinus tract was present, 0.12% chlorhexidine (Peridex) was used to irrigate. At the following appointment, patients were assessed, and if the resolution of signs and symptoms was noted, the teeth were reaccessed, and a blood clot was induced as described in the immediate protocol. In cases with persistent signs and symptoms of disease or if the bleeding was not induced, Ca(OH)2 was replaced in the canal. A maximum of 2 visits that included further irrigation and placement of intracanal Ca(OH)2 were allowed before the cases were categorized as failures and offered the rescue treatment implemented.
Follow-up
At 4 weeks after induction, patients were assessed for symptoms, but no radiographs were taken. Patients were advised to return for 3, 12, and 24 months for clinical and radiographic follow-ups. Radiographs were taken using previously recorded index bites. Monetary compensation was given at each of the follow-up visits.
Data Collection and Statistics
Evaluation of Success in Periapical Healing.
Pretreatment and 12-month follow-up radiographs were placed side by side at the same magnification with the crown of the tooth masked. Four blinded experienced and calibrated evaluators assessed the radiographs. The evaluators evaluated and classified the difference in periapical radiolucency as decreased, unchanged, or increased (26). Decreased lesions associated with an absence of signs or symptoms were recorded as successful cases. Cases with any increased or uncertain periapical lesions associated with any signs or symptoms were classified as failed cases, and rescue therapy was adopted. Intra- and interevaluator agreement was determined using Cohen κ statistics. When there was a discrepancy between evaluators, the final outcome was determined by a group discussion among the evaluators. The Pearson chi-square test or the Fisher exact test was used to compare the success rates between the 2 groups at the various time points. In a later step, after data collection gets completed, changes in root length, canal wall width, and radiographic root area will be considered as potential indicators of the treatment success.
In conjunction with the periapical score, a descriptive score of the apical root development adapted from Chen et al (4) was recorded: type 0, no changes; type 1, increased thickening of the canal walls and continued root maturation; type 2, there is no significant continuation of root development and the root apex has remained blunt and closed; type 3, there is continued root development and the apical foramen remained open; type 4, there is severe calcification (obliteration) of the canal space; and type 5, there is a hard tissue barrier formed in the canal space between the coronal MTA plug and the root apex.
Results
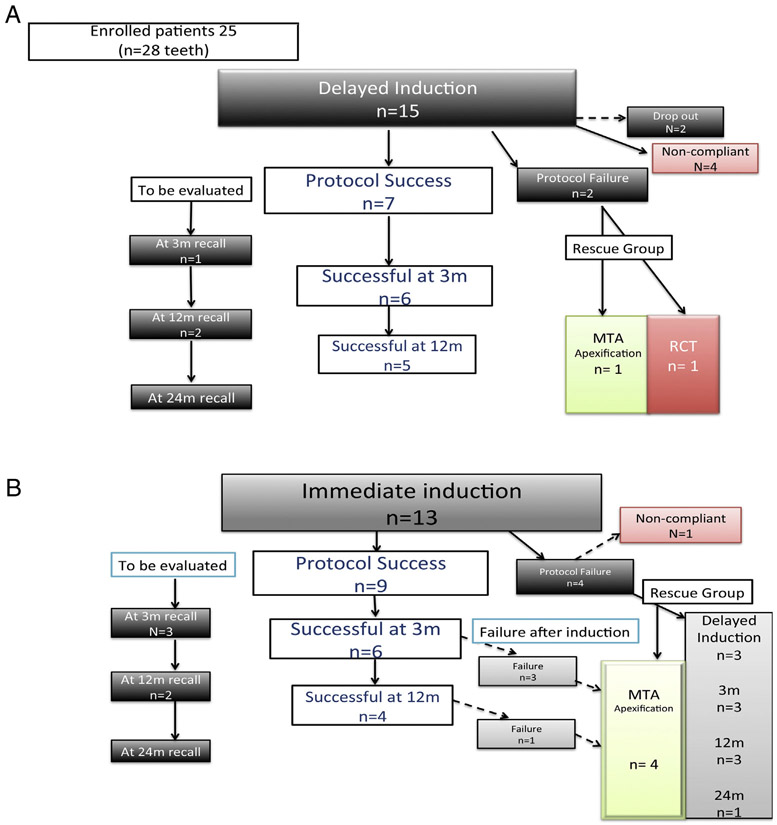
Because this study is currently in progress, only preliminary data of the 12-month recall cases are presented here. A total of 60 patients (63 teeth) have been screened, and 25 patients (28 teeth), 17 men and 8 women, were enrolled in the study. The main etiology found was trauma in 79% of cases (22/28 cases), and only 10% (3/28 cases) had caries or dental anomalies. Anterior teeth accounted for 79% (22/28 cases) of the cases, whereas 19% (5/28 cases) and 2% (1/28 cases) were premolars and molars, respectively. After randomization, 15 cases were assigned to the delayed group, 7 of which had a successful induction. No failures have been observed for these cases over the 3-month, 12-month, and 24-month recalls. Among the remaining 8 cases, 2 cases dropped out, 4 cases were noncompliant, and 2 cases did not follow the original protocol because they needed more than 2 visits with intracanal medication. The conclusion of protocol failure was drawn when the infection persisted or the blood clot was not induced (Fig. 1). Successful immediate induction of intracanal bleeding was achieved in 9 of 13 patients randomized to the immediate protocol. The remaining 4 cases did not meet the protocol requirements because the blood clot was not induced. Of these, 3 were treated, and 1 case was excluded from the trial because of poor compliance. Unlike the delayed protocol, 3 cases in this immediate group failed by the 3-month recall and 1 case failed by the 12-month recall. The main cause of failure for these cases was a persistent infection or a sinus tract present and/or an increase in the size of the periapical lesion, but all cases were asymptomatic. These 4 cases have been treated with MTA apexification (Fig. 1). In general, only mild and moderate adverse events such as tooth discoloration occurred in 46% of teeth (13/28). Persistent local infection was reported as failed cases. No severe adverse effects such as allergic reactions, systemic infections, or tooth loss were reported.
Figure 1.
Distribution of cases. (A) The delayed induction protocol group. (B) The immediate induction protocol group. Some cases in which the protocol could not be followed were transferred to the rescue group.
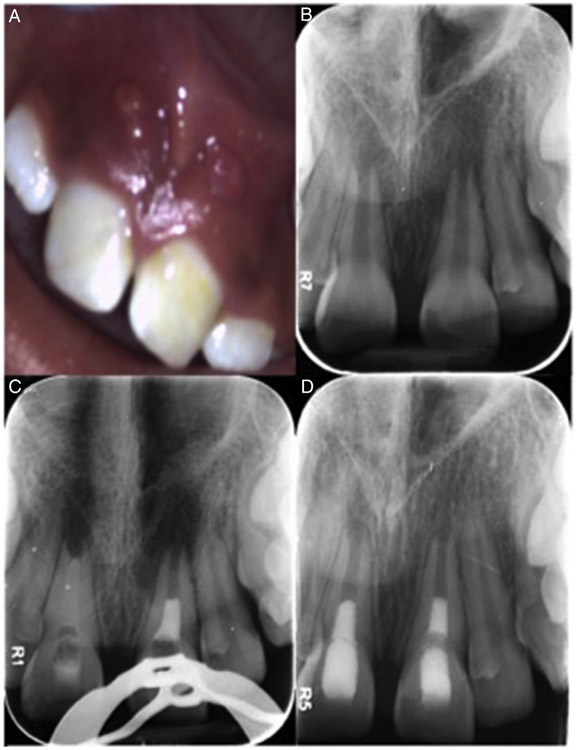
Overall, with the limitation of the small sample size collected up to date at the 12-month recall, there is a success rate of 71% for the delayed group and 33% for the immediate group with no statistically significant difference (relative risk calculation, P = .260) (Table 2). The analysis of the success rate for the successfully induced cases gives a higher success rate, 100% success for the delayed group and 50% success rate for the immediate group with no significant difference (Table 2.). Agreement between evaluators ranged from 0.67 to 0.85 according to the Cohen κ test. All successful cases started at stage 9 of root development (Nolla classification) (27), and the majority showed healing type 2 (4), especially in the delayed group in which the apex became closed and blunt (Tables 3 and 4 and Fig. 2). As the patients reach their 24-month follow-up, further analysis with ImageJ (National Institutes of Health, Bethesda, MD) and TurboReg software (Biomedical Imaging Group, Swiss Federal Institute of Technology, Lausanne, VD, Switzerland) will be performed for root length, root width, and root area quantification for comparison with the 12-month follow-up cases reported here (28, 29)
TABLE 2.
Data from Recalled Patients at the 12-month Follow-up: Success Rate
| Protocol | Recall successful | Recall failed | Success rate (including
failure induction), n (%) |
Success rate (including successful induction), n (%) |
|---|---|---|---|---|
| Immediate Induction (n = 12) | 4 | 8 | (4/12) 33 | (4/8) 50 |
| Delayed Induction (n = 7) | 5 | 2 | (5/7) 71 | (5/5) 100 |
TABLE 3.
Data from Recalled Patients at the 12-month Follow-up: Nolla Stage and Type of Healing
| Recalled successfully at 12 months |
Nolla stage (9) |
Type 0 |
Type 1 |
Type 2 |
Type 3 |
Type 4 |
Type 5 |
|---|---|---|---|---|---|---|---|
| n = 9 | 9 | 0 | 1 | 5 | 1 | 1 | 3 |
TABLE 4.
Data from Recalled Patients at the 12-month Follow-up: Demographics
| Recall successful |
Recall failured |
|||
|---|---|---|---|---|
| Demographics | Immediate induction |
Delayed induction |
Immediate induction |
Delayed induction |
| Trauma | 4 | 4 | 5 | 2 |
| Dental anomaly | 2 | |||
| Caries | 1 | 1 | ||
| Male | 3 | 2 | 5 | 2 |
| Female | 1 | 3 | 3 | |
| Sinus tract present (preoperatively) | 2 | 2 | 3 | 1 |
Figure 2.
A 10-year-old female patient with a history of trauma (noncomplicated crown fracture) diagnosed with pulp necrosis and asymptomatic apical periodontitis of teeth #8 and #9. (A) The clinical photograph at the initial visit. Teeth #8 and #9 presented mild swelling and a parulis in the buccal mucosa. (B) Periapical radiolucencies and stage of root formation (Nolla 9) for both apices. (C) The treatment for both was determined by random numbers. Tooth #8 was delayed, and tooth #9 was treated with the immediate induction protocol. (D) At the 12-month follow-up visit, the patient was asymptomatic and showed complete periapical healing and apical healing type 2 with a blunted apex and no evident changes in wall thickening.
Discussion
Currently, there are no clinical trials reporting on immediate induction for regenerative endodontics despite the need of randomized clinical trials in this field. Preliminary data from this randomized clinical trial comparing immediate induction versus delayed induction protocols showed so far a clinical success rate of 71% for delayed induction and a 33% success rate for immediate induction. There were more recalled failures for immediate induction and none for delayed induction. Failures (33%, 4/12 cases) occurred during induction when intracanal bleeding could not established, and 33% (4/12 cases) of the failures occurred after 3 months following the induction. The failed cases were then treated following the delayed induction protocol. However, for the delayed induction protocol group, the recalled failures were 29% (2/7 cases) and occurred just at the time of the induction. These cases have been treated by MTA apexification and conventional root canal therapy. The success rate of the cases after successful induction was 100% for delayed induction and 50% for immediate induction.
In a previous retrospective report (10), 20 selected cases were evaluated with a 100% survival rate for teeth treated with a revascularization protocol and a lower success rate of 80% for this group. The main etiology found for the revascularization cases was dental anomalies (60%), and only 35% came from trauma and 5% from caries. Interestingly, in the same study, when the authors evaluated 22 cases treated by conventional apexification using Ca(OH)2, the survival and success rate was 77% for survival and success with the main etiology found for this group being trauma (81% of the cases). This is very similar to our preliminary results. We found a recalled success rate of 71%. Trauma was the main etiology in 79% of cases. Alobaid et al (11) reported a pilot retrospective cohort study in which they showed a higher survival rate for cases treated with MTA apexification (100%) and a lower survival rate for the cases treated with revascularization (95%). However, when the clinical success rate was evaluated, the revascularization group had a 79% success rate compared with the MTA apexification group with a 100% success rate. In their study for the revascularization group, trauma was associated with 79% including severe trauma such as avulsion. The apexification group had fewer cases with severe trauma. Both of these studies have no randomization and are retrospective. However, the association between success rate and etiology are possible predictor factors. Kahler et al (12) published a prospective analysis of 16 consecutive cases in which qualitative assessment of periapical healing was used; 90.3% of the cases showed resolution of the lesion with only complete apical closure for 19.4% of the cases. The main etiology in their study was trauma (81.2%, 13/16 cases), and their protocol included revascularization after triple antibiotic paste with metronidazole, ciprofloxacin, and amoxicillin. In our study, having so far 79% of cases with trauma and using Ca(OH)2, the success rate has been 71%. Nonetheless, bigger sample sizes are imperative for any valid conclusion.
At the time that pulp necrosis is diagnosed, the stage of root development might be a relevant predictor factor for periapical and apical healing. The stage of root development differed significantly in a retrospective study in which revascularization cases were more immature compared with apexification cases (11). The authors found more complications associated with the more immature teeth. Here we report that all teeth treated and successfully recalled were categorized as type 8 to 9 Nolla (27) for stage of root development at their first visit. The majority of our successful cases at the 12-month recall showed apical healing type 2. In this healing, there is no significant continuation of the root development, with the root apex becoming blunt and closed as reported by Chen et al (4). Others have found that despite a high success rate for apical healing the apex maturity was incomplete for most of the cases, showing maturation for some cases even after 18 and 36 months (12). Unfortunately, there is no information of the stage of root development at the time of induction for most studies. Patients’ age and tooth type might be relevant predictor factors for periapical and apical healing. In our study, the majority of patients recruited were young males (average age = 10.5 years) with upper anterior teeth involved because of trauma. These are the common features reported by most of the case series and retrospective and prospective pilot clinical studies (4,10-12).
Complications such as tooth discoloration, no blood clot formation, and persistent infection can occur during regenerative endodontic protocols. Alobaid et al (11) classified these complications as mild, moderate, or severe depending on the therapy needed. Although triple antibiotic paste containing tetracycline was not used in our study, we reported discoloration in 46% of the cases. Others using triple paste without tetracycline have also found similar complications (7, 9, 11, 12, 30). The use of MTA, white or gray, seems to be the main cause. No blood clot formation is another common minor complication. For those cases, the induction can be postponed for a later visit. In our study, if the blood clot was not formed at the initial visit, the case was transferred to the rescue group. The treatment followed was similar to the one for the delayed protocol group. Persistent infection is a moderate complication as previously classified (11). For the immediate induction group, 4 cases, 3 at the 3-month recall and 1 at the 12-month recall, were classified as reinfected and transferred to the rescue group. No severe events such as allergic reactions, spread of infection, tooth retraumatized, or tooth loss have been reported.
Multiple clinical protocols for REPs have been reported as successful (31). This makes evaluation and correlation of the protocols with the outcome difficult although it is clear that the disinfection of the root canal system might be incomplete for the cases failing after immediate induction. More microbiological studies are needed to understand the etiology and the best protocol of disinfection for these cases (32). It is also possible that a more resistant biofilm is associated with the presence of a sinus tract in which the infection is well established (33). Determining the type of the stem cells contained in the apical papilla may reveal another possible predictor factor for further analysis (34, 35). Determination of the stage of root formation and etiology, as discussed previously, are possible critical factors for any therapeutic decision. In summary, it is early to conclude or suggest any of the protocols. Clearly, much more data are needed before sample size requirements can be met.
Significance.
Randomized clinical trials are fundamental studies to support evidence-based practice in regenerative endodontics. This report presents preliminary data from an ongoing clinical randomized trial to support if immediate induction is feasible for immature teeth.
Acknowledgments
The authors thank the students from the endodontic graduate clinic including Dr Anna DeGraft-Johnson, Dr Dmitry Vodopyanov, Dr Darya Dabiri, and Dr Faisal Almoghaisseebb; endodontic program director Dr Neville McDonald; of and department chair Dr Jacques E. Nör for their collaboration with this project.
Supported by the Cariology, Restorative Sciences and Endodontics Department; Delta Dental Foundation; and American Association of Endodontics Foundation.
Footnotes
The authors deny any conflict of interest related to this study.
References
- 1.American Association of Endodontists. AAE regenerative endodontics clinical considerations. Available at: http://www.aae.org/uploadedfiles/publications_and_research/research/currentregenerativeendodonticconsiderations.pdf. Accessed June 30, 2016.
- 2.Chueh LH, Ho YC, Kuo TC, et al. Regenerative endodontic treatment for necrotic immature permanent teeth. J Endod 2009;35:160–4. [DOI] [PubMed] [Google Scholar]
- 3.Shah N, Logani A, Bhaskar U, et al. Efficacy of revascularization to induce apexification/apexogensis in infected, nonvital, immature teeth: a pilot clinical study. J Endod 2008;34:919–25. [DOI] [PubMed] [Google Scholar]
- 4.Chen MY, Chen KL, Chen CA, et al. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures. Int Endod J 2012;45:294–305. [DOI] [PubMed] [Google Scholar]
- 5.Bezgin T, Yilmaz AD, Celik BN, et al. Efficacy of platelet-rich plasma as a scaffold in regenerative endodontic treatment. J Endod 2015;41:36–44. [DOI] [PubMed] [Google Scholar]
- 6.Nagata JY, Gomes BP, Rocha Lima TF, et al. Traumatized immature teeth treated with 2 protocols of pulp revascularization. J Endod 2014;40:606–12. [DOI] [PubMed] [Google Scholar]
- 7.McTigue DJ, Subramanian K, Kumar A. Case series: management of immature permanent teeth with pulpal necrosis: a case series. Pediatr Dent 2013;35:55–60. [PubMed] [Google Scholar]
- 8.Jadhav G, Shah N, Logani A. Revascularization with and without platelet-rich plasma in nonvital, immature, anterior teeth: a pilot clinical study. J Endod 2012;38: 1581–7. [DOI] [PubMed] [Google Scholar]
- 9.Dabbagh B, Alvaro E, Vu DD, et al. Clinical complications in the revascularization of immature necrotic permanent teeth. Pediatr Dent 2012;34:414–7. [PubMed] [Google Scholar]
- 10.Jeeruphan T, Jantarat J, Yanpiset K, et al. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods—a retrospective study. J Endod 2012;38: 1330–6. [DOI] [PubMed] [Google Scholar]
- 11.Alobaid AS, Cortes LM, Lo J, et al. Radiographic and clinical outcomes of the treatment of immature permanent teeth by revascularization or apexification: a pilot retrospective cohort study. J Endod 2014;40:1063–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kahler B, Mistry S, Moule A, et al. Revascularization outcomes: a prospective analysis of 16 consecutive cases. J Endod 2014;40:333–8. [DOI] [PubMed] [Google Scholar]
- 13.Huang GT, Sonoyama W, Liu Y, et al. The hidden treasure in apical papilla: the potential role in pulp/dentin regeneration and bioroot engineering. J Endod 2008;34: 645–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lovelace TW, Henry MA, Hargreaves KM, et al. Evaluation of the delivery of mesen-chymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. J Endod 2011;37:133–8. [DOI] [PubMed] [Google Scholar]
- 15.Casagrande L, Demarco FF, Zhang Z, et al. Dentin-derived BMP-2 and odontoblast differentiation. J Dent Res 2010;89:603–8. [DOI] [PubMed] [Google Scholar]
- 16.Trevino EG, Patwardhan AN, Henry MA, et al. Effect of irrigants on the survival of human stem cells of the apical papilla in a platelet-rich plasma scaffold in human root tips. J Endod 2011;37:1109–15. [DOI] [PubMed] [Google Scholar]
- 17.Galler KM, D’Souza RN, Federlin M, et al. Dentin conditioning codetermines cell fate in regenerative endodontics. J Endod 2011;37:1536–41. [DOI] [PubMed] [Google Scholar]
- 18.Martin DE, De Almeida JF, Henry MA, et al. Concentration-dependent effect of sodium hypochlorite on stem cells of apical papilla survival and differentiation. J Endod 2014;40:51–5. [DOI] [PubMed] [Google Scholar]
- 19.Ruparel NB, Teixeira FB, Ferraz CC, et al. Direct effect of intracanal medicaments on survival of stem cells of the apical papilla. J Endod 2012;38:1372–5. [DOI] [PubMed] [Google Scholar]
- 20.Berkhoff JA, Chen PB, Teixeira FB, Diogenes A. Evaluation of triple antibiotic paste removal by different irrigation procedures. J Endod 2014;40:1172–7. [DOI] [PubMed] [Google Scholar]
- 21.Shin SY, Albert JS, Mortman RE. One step pulp revascularization treatment of an immature permanent tooth with chronic apical abscess: a case report. Int Endod J 2009;42:1118–26. [DOI] [PubMed] [Google Scholar]
- 22.Chaniotis A The use of a single step regenerative approach for the treatment of a replanted mandibular central incisor with severe resorption. Int Endod J 2016; 49:802–12. [DOI] [PubMed] [Google Scholar]
- 23.McCabe P Revascularization of an immature tooth with apical periodontitis using a single visit protocol: a case report. Int Endod J 2015;48:484–97. [DOI] [PubMed] [Google Scholar]
- 24.da Silva LA, Nelson-Filho P, da Silva RA, et al. Revascularization and periapical repair after endodontic treatment using apical negative pressure irrigation versus conventional irrigation plus triantibiotic intracanal dressing in dogs’ teeth with apical periodontitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109:779–87. [DOI] [PubMed] [Google Scholar]
- 25.Topçuoğlu G, Topçuoğlu HS. Regenerative endodontic therapy in a single visit using platelet-rich plasma and Biodentine in necrotic and asymptomatic immature molar teeth: a report of 3 cases. J Endod 2016;42:1344–6. [DOI] [PubMed] [Google Scholar]
- 26.Orstavik D, Kerekes K, Eriksen HM. The periapical index: a scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol 1986;2: 20–34. [DOI] [PubMed] [Google Scholar]
- 27.Nolla CM. The development of the permanent teeth. J Dent Child 1960;27: 254–66. [Google Scholar]
- 28.Bose R, Nummikoski P, Hargreaves K. A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. J Endod 2009;35:1343–9. [DOI] [PubMed] [Google Scholar]
- 29.Flake NM, Gibbs JL, Diogenes A, et al. A standardized novel method to measure radiographic root changes after endodontic therapy in immature teeth. J Endod 2014;40:46–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim JH, Kim Y, Shin SJ, et al. Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod 2010;36:1086–91. [DOI] [PubMed] [Google Scholar]
- 31.Diogenes A, Henry MA, Teixeira FB, et al. An update on clinical regenerative endodontics. Endod Topics 2013;28:2–23. [Google Scholar]
- 32.Fouad AF, Verma P. Healing after regenerative procedures with and without pulpal infection. J Endod 2014;40(Suppl):S58–64. [DOI] [PubMed] [Google Scholar]
- 33.Ricucci D, Siqueira JF Jr. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod 2010;36: 1277–88. [DOI] [PubMed] [Google Scholar]
- 34.Kim SH, Kim S, Shin Y, et al. Comparative gene expression analysis of the coronal pulp and apical pulp complex in human immature teeth. J Endod 2016;42:752–9. [DOI] [PubMed] [Google Scholar]
- 35.Diogenes A, Ruparel NB, Shiloah Y, Hargreaves KM. Regenerative endodontics: a way forward. J Am Dent Assoc 2016;147:372–80. [DOI] [PubMed] [Google Scholar]