Abstract
Objectives:
Among US-born children of Latina US (USB) and Latina foreign-born mothers (FBM), to determine whether 1) household and child characteristics differ; 2) child health outcomes differ; 3) these differences diminish for children of FBM with longer duration of residence (DOR) in the US; and 4) these differences can be explained by food insecurity (FI) or by Supplemental Nutrition Assistance Program (SNAP) participation.
Methods:
Cross-sectional survey of 2,145 Latina mothers of publicly insured US born children 0–48 months old in a Boston emergency department (ED) 2004–2013. Predictors were FBM vs USBM and duration of residence in the US. Outcomes were mothers’ report of child health, history of hospitalization, developmental risk, hospital admission on the day of ED visit. Multivariable logistic regression adjusted for potential confounders and effect modification.
Results:
FBM versus USBM households had more household (31% vs 26%) and child (19% vs 11%) FI and lower SNAP participation (44% vs 67%). Children of FBM versus USBM were more likely to be reported in fair/poor vs good/excellent health (AOR 1.9, 95% CI [1.4, 2.6]), with highest odds for children of FBM with shortest DOR, and to be admitted to the hospital on the day of the ED visit (AOR 1.7, 95% CI [1.3, 2.2]). SNAP and FI did not fully explain these outcomes.
Conclusion:
When providing care and creating public policies, clinicians and policymakers should consider higher rates of food insecurity, lower SNAP participation, and risk for poor health outcomes in Latinx children of FBM.
Keywords: Child health, immigrant, Latinx, food insecurity, Supplemental Nutrition Assistance Program (SNAP)
INTRODUCTION
The United States Latinx (a gender-neutral alternative to Latino or Latina) population increased from 35 to 57.5 million from the year 2000 to 2016. Approximately 35% of the Latinx population are foreign-born (FB), with the greatest proportion of Mexican origin but an increasing number from Central American countries.1 Nearly half of US-born Latinx are younger than 18 years of age, and the majority of US citizen Latinx children have at least one foreign-born parent.2 The increasing population of US citizen children of FB Latinx parents may face increased hardships, combined with decreased access to public assistance programs and health care, which may override the perceived “healthy immigrant effect.”
Although Latinx people are typically treated as a single demographic group in health outcomes research, child health status is likely to differ by parental immigrant status and duration of residence (DOR), which influence economic opportunities, language proficiency, and access to public assistance programs and health care.3 Although their US-born children may still be eligible for the Supplemental Nutrition Assistance Program (SNAP), by current federal regulation, most foreign-born adults cannot participate in SNAP or Medicaid for the first five years of authorized US residence.4
Compared with children of US-born parents, children of immigrant and refugee parents face heightened risk of economic hardships that may have a negative impact on health. US-born children of Latinx immigrants are at high risk for experiencing food insecurity,5–7 an established risk factor for poor health.8 This risk was recently shown to have increased significantly between 1998 and 2011 for Latinx kindergarten-aged children of foreign- vs. U.S.-born mothers.9 Families with immigrant parents participate less frequently in SNAP, a program that can mitigate effects of food insecurity and poverty on health and development.10,11 Compared with children of citizens, children of non-citizens have been shown to have higher levels of food insecurity, lower participation in SNAP, and lower SNAP benefit amounts per household member even when they do participate.12
Despite poverty-related risk factors, studies supporting a “healthy immigrant paradox” - and more specifically to Latinx populations, the “Hispanic health paradox” - describe better health outcomes in immigrants and successive generations than would be predicted by socioeconomic status, with the strongest data for children of Mexican origin.13,14 Multiple hypotheses have been proposed to explain these paradoxes, and the effects of immigration on health outcomes usually diminish with successive generations. In some epidemiological studies, Latinx immigrants and their children compared with non-Latinx controls experienced fewer adverse outcomes in domains such as preterm birth, infant mortality, and asthma.15 Nevertheless, some data have demonstrated that children of foreign-born mothers (FBM) have higher odds of fair/poor child health.5 These findings have not been consistently shown in children and are not generalizable across various demographic groups,13,16 The strongest, yet still inconsistent, data are in the perinatal period with fewer studies regarding early childhood health or developmental outcomes. 13,17
Understanding differences in demographics and health and development outcomes between Latinx children of foreign- versus US-born parents – extending beyond infancy into early childhood – can inform targeted interventions to improve child and population health. Moreover, few data elucidate the health and developmental status of Latinx children of non-Mexican heritage nor the impact of mother’s DOR in the US.
Goals of this study were to determine whether: 1) household and child characteristics differ between US-born children of Latina USBM and FBM, 2) child health and development outcomes differ between children of Latina USBM and FBM, 3) these differences diminish for children of FBM with longer DOR in the US, and 4) differences in health outcomes can be partially attributed to food insecurity or to SNAP participation.
METHODS
Data collection
Children’s HealthWatch is an ongoing five-city repeat cross-sectional survey study investigating associations between economic hardships, public assistance programs, and health of children less than 48 months old and their caregivers. 5 The Boston site is Boston Medical Center, an urban hospital (the largest in New England) serving a predominantly low income population; data are collected in the pediatric emergency department (ED). The survey was translated from English to Spanish by native Spanish speakers from diverse Hispanophone regions and then back-translated before being certified by the Boston University School of Medicine Institutional Review Board (IRB). After obtaining informed consent, bilingual research assistants conducted face-to-face interviews in private settings using caregivers’ preferred language (English or Spanish), entering verbal responses onto laptop computers for secure transmission to a data analysis center.
Children’s HealthWatch survey participant eligibility criteria included the following: English or Spanish speaking, primary caregiver, knowledgeable about the child’s household, and self-reported Massachusetts state residency. Caregivers of critically ill or injured children, and those previously interviewed were excluded. IRB approval was obtained prior to data collection and renewed annually. Caregivers reported their place of birth but not their immigration or citizenship status.
Study population
For this study, additional eligibility criteria were children born in the US by maternal report aged 0–48 months whose birth mothers self-identified as Latina using the standard US Census question.18 To ensure comparable household incomes across all exposure groups, we restricted the sample to caregivers with public or no health insurance.11
Between January 2004 and June 2013, 7,793 caregivers completed the Children’s HealthWatch study interview. Of these participants, the 2,259 who self-identified as Latina and were also biological mothers were eligible for analysis. Excluding 114 mothers with private insurance yielded a final sample of 2,145 US-born children of Latina mothers, of whom 1,071 (49.9%) were born in the mainland US or Puerto Rico (USBM) and 1,074 (50.1%) were foreign born (FBM). Interviews were conducted in Spanish for 9% of USBM and 65% of FBM.
Predictors
Main exposure variables were mothers’ self-reported birthplace (foreign versus US), and for FBM, duration of residence (DOR) ascertained by self-reported year of arrival in the US. DOR was stratified into <5 years, 5–10 years, and >10 years to reflect adult eligibility for certain means-tested public assistance programs.5,19
Outcomes
Outcome variables included (1) mother’s rating of child health, (2) hospital admission from the ED at the time of interview determined by medical record review (3) history of prior hospitalization not including hospitalization at birth, determined by mother’s report, and (4) developmental risk, measured by one or more concerns expressed on the Parents’ Evaluation of Developmental Status (PEDS).20 Mothers rated their children’s health status as fair, poor, good, or excellent, a response adapted from the single, validated question from the Third National Health and Nutrition Examination Survey.21 The PEDS is a developmental screening test, validated in English and Spanish, recommended by the American Academy of Pediatrics for use from birth through age 7.20 Children with one or more significant concerns identified on the PEDS are considered at moderate risk for developmental disabilities and in need of additional screening, monitoring and intervention. For this outcome, we limited our sample to children ≥4 months old because of better PEDS sensitivity and specificity above that age.22
Covariates and Mediators
Potential confounders included mother’s report of child age and sex, mother’s education and employment, child’s birth weight (<2500 grams vs ≥2500 gram), gestational age, whether the child had ever been breastfed, and mother’s depressive symptoms. Mothers’ depressive symptoms were measured with the Kemper scale, a three-item screen shown to be sensitive, specific, and with a positive predictive value of 66 percent compared with the 8-item Rand screening instrument.23 Language of interview was not evaluated because of collinearity with mothers’ place of birth.
Food insecurity was assessed using the US Household Food Security Survey Module (HFSSM), an assessment of household food security standardized in English and Spanish that includes ten household-focused and eight child-specific questions.24 The US Department of Agriculture Economic Research Service classifies households as food insecure if they report they could not consistently afford enough food for active, healthy lives for all household members in the past 12 months because of constrained resources.4 We categorized participants as (1) household food insecure (HFI) if three or more household questions were endorsed as sometimes or often true vs. never true, (2) household and child food insecure (CFI) if two or more of the eight child-specific questions were also endorsed, and (3)all others as food secure.4
Mothers also answered questions about current participation in SNAP and WIC for themselves and their children. We examined food insecurity and lack of access to SNAP as potential mediators of the associations between maternal place of birth and child health, as suggested by a previous study.5
Statistical Analysis
We examined bivariate relationships between mother’s place of birth (US born vs foreign-born) and maternal and child characteristics, and further examined relationships stratified by FBM’s DOR in the US. To develop multivariable models, we examined these bivariate relationships between exposures and outcomes, and performed logistic regression adding child and maternal variables sequentially to the models to explore their influence on the primary relationship. After running five models, our final multivariable model controlled for child’s age and sex, gestational age, whether the child had ever breastfed, mother’s depressive symptoms and her education. We additionally performed a sensitivity analysis excluding mothers born in Puerto Rico (n = 270) to ensure that there was no effect modification as this group is US-Born but may have other demographic differences. We examined interview year as both a confounder and an effect modifier in the multivariable models. Food insecurity and SNAP participation were examined as mediators of the relationship between child health and mother’s place of birth. We employed the approach described by Baron and Kenny and Sobel’s test to examine mediation.25
RESULTS
Family Characteristics
Most mothers were born in mainland United States, Puerto Rico, El Salvador, and the Dominican Republic, with less than a quarter born in Honduras, Guatemala, Colombia, Mexico, and other countries. [Figure 1]
Figure 1.
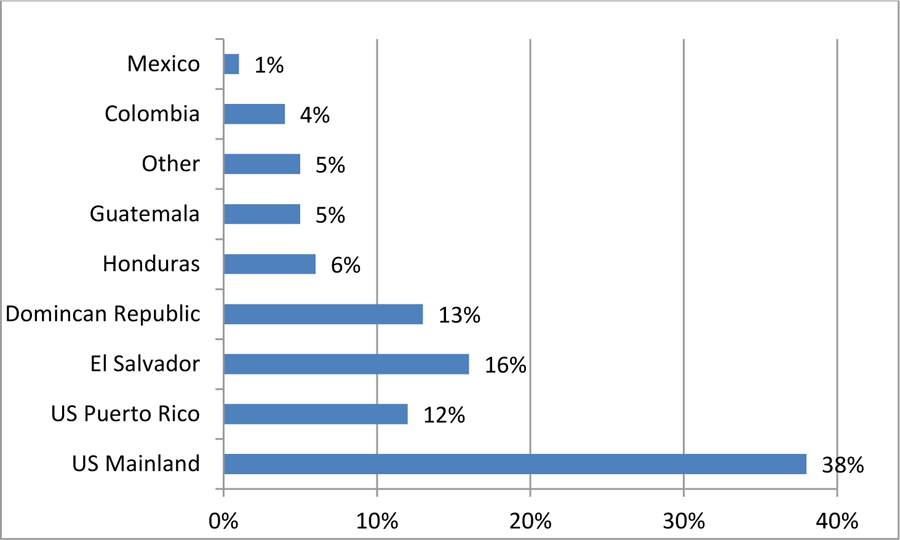
Mother’s Place of Birth
Source: Children’s HealthWatch - Boston data, 2004–2013
Mother, child and household characteristics differed by mother’s place of birth (USBM vs. FBM) and, among FBM, by duration of US residence. [Table 1] Among children of FBM, preterm birth was less common than among children of USBM (9.5% vs. 13.9%, respectively; p=0.002), and more children of FBM vs. USBM had ever been breastfed (88.9% vs 64.3%; p<0.001). FBM were less likely to screen positive for depression, had lower educational attainment, but were more likely to be married or partnered, and employed. FBM reported lower rates of SNAP participation than USBM (43.8% vs 67.1%, p<.001), as well as lower SNAP benefit amount per person per month in households that did participate in SNAP (mean of $79.0 vs $93.5 dollars per person per month, p<.001). More FBM than USBM participated in WIC (90.9 vs. 83.9%, p<.001).
Table 1:
Child and Maternal Characteristics of 2145 US-born Latinx children
| Characteristics | US-Born Latina Mother N=1071 |
Foreign-Born Latina Mother N=1074 |
p-value |
|---|---|---|---|
| Child Characteristics | N (%) | ||
| Child Sex - Female | 500 (46.7%) | 524 (48.8%) | 0.33 |
| Child Age, Months (Mean, SD) | 13.5 (11.4) | 13.9 (10.6) | 0.39 |
| Low Birthweight (<2500 grams) | 141 (13.3%) | 102 (9.8%) | 0.011 |
| Preterm Birth - Gestational Age < 37 weeks | 149 (13.9%) | 102 (9.5%) | 0.002 |
| Child Ever Breastfed | 688 (64.3%) | 954 (88.9%) | <0.001 |
| Child’s Insurance Type | 0.09 | ||
| Public | 1031 (96.5%) | 1016 (95.0%) | |
| None | 37 (3.5%) | 53 (5.0%) | |
| Maternal Characteristics | |||
| Age, Years (Mean, SD) | 28.2 (5.9) | 25.2 (5.9) | <.001 |
| Depressive Symptoms | 359 (33.5%) | 303 (28.2%) | 0.008 |
| Marital Status | <0.001 | ||
| Married/Partnered | 272 (25.5%) | 450 (41.9%) | |
| Not Married/Partnered | 796 (74.5%) | 623 (58.1%) | |
| Educational Attainment | 0.004 | ||
| Never/Elementary/Some High School | 411 (38.5%) | 487 (45.6%) | |
| Completed High School | 388 (36.3%) | 348 (32.6%) | |
| Tech School/College Grad or higher | 269 (25.2%) | 234 (21.9%) | |
| Employed | 323 (30.2%) | 404 (37.7%) | <0.001 |
| Language of Interview | <0.001 | ||
| Spanish | 100 (9.3%) | 701 (65.3%) | |
| English | 971 (90.7%) | 373 (34.7%) | |
| Household Characteristics | |||
| Number of children in Household (Mean,SD) | 2.2 (1.2) | 2.1 (1.1) | 0.003 |
| SNAP participation1 | 719 (67.1%) | 470 (43.8%) | <0.001 |
| SNAP Benefit Amount per person per month in dollars (Mean, SD) | 93.5 (48.3) | 79.0 (42.0) | <0.001 |
| WIC participation2 | 898 (83.9%) | 972 (90.9%) | <0.001 |
| Household Food Insecurity | 281 (26.2%) | 335 (31.3%) | 0.010 |
| Child Food Insecurity | 116 (10.8%) | 203 (18.9%) | <0.001 |
SNAP – Supplemental Nutrition Assistance Program,
WIC – Special Supplemental Nutrition Program for Women, Infants, and Children
Child Outcomes by Mother’s Place of Birth
In bivariate analyses compared to USBM, FBM more frequently rated their child’s health as fair/poor vs. excellent/good (15.7% vs 9.4%, respectively, p<0.001), and FBM’s children were more frequently admitted to the hospital from the ED (21.9% vs 12.7%, p<0.001). FBM reported higher rates of both HFI (31.3% vs 26.2%, p=0.01) and CFI (18.9% vs 10.8%, p<0.001) [Table 2]
Table 2:
Child Health Outcomes among Children of Foreign-Born versus US-Born Latina Mothers
| Outcomes | US-Born Latina Mother N=1071 |
Foreign-Born Latina Mother N=1074 |
p-value |
|---|---|---|---|
| N (%) | |||
| Maternal Rating of Child Health Fair or Poor | 100 (9.4%) | 168 (15.7%) | <0.001 |
| Admission from the Emergency Department on the Day of Interview | 136 (12.7%) | 235 (21.9%) | <0.001 |
| History of Prior Hospitalization | 245 (23.1%) | 243 (22.8%) | 0.85 |
| Developmental Risk (Ages ≥4 mo, n = 1572) | 169 (20.5%) | 128 (17.1%) | 0.09 |
Adjusted odds ratios (AOR) were consistent with unadjusted outcomes. [Table 3] Controlling for covariates, FBM had two-fold higher odds of reporting fair or poor child health (AOR 2.1 [95% CI 1.6, 2.8]) and nearly twice the odds of having their children admitted to the hospital from the ED (AOR 1.8 [95% CI 1.4, 2.3]). History of prior hospitalizations or developmental risk did not significantly differ between groups. Sensitivity analyses excluding mothers born in Puerto Rico did not change the results. Including interview year in the multivariable model did not meaningfully change the results, and adjusted effects of mother’s place of birth did not significantly change across study years (i.e., no significant interaction between place of birth and study year).
Table 3:
Unadjusted and Adjusted Odds of Child Health Outcomes among Children of Latina Foreign-Born vs. U.S. Born Mothers
| Child Outcomes | US Born Latina Mother |
FB Latina Mother Unadjusted OR |
FB Latina Mother Adjusted OR* |
|---|---|---|---|
|
Maternal rating of child health fair or poor |
1.00 |
1.80 (1.39, 2.35) p<0.001 |
2.07 (1.55, 2.75) p<0.001 |
| Admission from the Emergency Department on the Day of Interview | 1.00 |
1.92 (1.52, 2.42) p<0.001 |
1.80 (1.41, 2.30) p<0.001 |
| History of prior hospitalization | 1.00 | 0.98 (0.80, 1.20) p=0.85 |
1.09 (0.88, 1.35) p=0.44 |
| Developmental Risk | 1.00 | 0.80 (0.62, 1.03) p=0.09 |
0.93 (0.71, 1.23) p=0.62 |
Adjusted for child age, sex, gestational age, breastfed, maternal depression, maternal education. The reference group is US Born Latina Mothers.
Characteristics by Duration of Residence
As DOR in the US increased, mean maternal age and the proportion employed increased [Table 4]. For FBM with DOR <5, 5–10 and >10 years, the rates of SNAP participation were 33.7%, 45.3% and 51.5% respectively, and the mean (SD) dollar amount per household member increased significantly from $66.3 (36.2) and 74.0 (38.1), to 94.6 (46.0) respectively. DOR was not associated with rates of breastfeeding, maternal depressive symptoms, or low birth weight or prematurity. Spanish-language interviews were conducted for the majority of FBM with DOR <5 years, compared with less than half of FBM with DOR >10 years (p<.001).
Table 4:
Child and Maternal Characteristics among Latina Foreign-Born Mothers by Duration of Residence (DOR) in the US
| Characteristics | DOR <5 years N=302 |
DOR 5–10 years N=426 |
DOR >10 years N=309 |
p-value |
|---|---|---|---|---|
| Child Characteristics | N (%) | |||
| Child Sex - Female | 153 (50.7%) | 205 (48.1%) | 150 (48.5%) | 0.78 |
| Child’s Age, Months (Mean,SD) | 11.6 (10.5) | 13.5 (11.3) | 15.5 (11.9) | <.001 |
| Low Birthweight (<2500 grams) | 35 (11.9%) | 33 (8.0%) | 32 (10.5%) | 0.22 |
| Preterm Birth - Gestational Age < 37 weeks | 30 (10.0%) | 35 (8.3%) | 33 (10.7%) | 0.50 |
| Child Ever Breastfed | 271 (89.7%) | 386 (90.8%) | 267 (86.4%) | 0.15 |
| Child’s Insurance Type | 0.02 | |||
| Public | 276 (92.0%) | 407 (95.8%) | 297 (96.7%) | |
| None | 24 (8.0%) | 18 (4.2%) | 10 (3.3%) | |
| Maternal Characteristics | ||||
| Age, Years (Mean, SD) | 26.7 (5.7) | 28.0 (5.7) | 29.9 (6.0) | <.001 |
| Depressive Symptoms | 87 (28.8%) | 123 (28.9%) | 82 (26.5%) | 0.75 |
| Marital Status | 0.38 | |||
| Married/Partnered | 117 (38.7%) | 184 (43.2%) | 135 (43.7%) | |
| Not Married/Partnered | 185 (61.3%) | 242 (56.8%) | 174 (56.3%) | |
| Educational Attainment | <.001 | |||
| Never/Elementary/Some High School | 148 (49.2%) | 213 (50.1%) | 109 (35.6%) | |
| Completed High School | 84 (27.9%) | 139 (32.7%) | 109 (35.6%) | |
| Tech School/College Grad or higher | 69 (22.9%) | 73 (17.2%) | 88 (28.8%) | |
| Employed | 80 (26.6%) | 162 (38.2%) | 150 (48.5%) | <.001 |
| Language of Interview | <.001 | |||
| Spanish | 56 (18.5%) | 129 (30.3%) | 178 (57.6%) | |
| English | 246 (81.5%) | 297 (69.7%) | 131 (42.4%) | |
| Household Characteristics | ||||
| Number of Children in Household (Mean, SD) | 1.9 (1.0) | 2.0 (1.0) | 2.4 (1.2) | <.001 |
| SNAP participation1 | 101 (33.7%) | 193 (45.3%) | 159 (51.5%) | <.001 |
| SNAP Benefit Amount per person per month in dollars (Mean, SD) | 66.3 (36.2) | 74.0 (38.1) | 94.6 (46.0) | <.001 |
| WIC participation | 281 (94.0%) | 388 (91.3%) | 268 (86.7%) | 0.008 |
| Household food insecurity | 107 (35.5%) | 129 (30.3%) | 89 (28.9%) | 0.17 |
| Child food insecurity | 62 (20.6%) | 84 (19.7%) | 51 (16.6%) | 0.40 |
SNAP – Supplemental Nutrition Assistance Program
WIC – Special Supplemental Nutrition Program for Women, Infants, and Children
Child and Household Outcomes by Duration of Residence (DOR)
Outcomes were also examined in stratified analyses by mothers’ DOR. [Table 5] The only outcome that differed significantly by duration of residency was maternal rating of child’s fair/poor health, which decreased as DOR increased: from 18% (<5 years) to 17% (5–10 years), to 11% (>10 years), versus 9% for USBM (p=0.04 across DOR groups, and p<0.001 across groups including USBM).
Table 5:
Child Health Outcomes by Mothers’ Duration of Residence in the US
| Child Outcomes | US-Born Latina Mother N=1071 |
DOR < 5 years N=302 |
DOR 5–10 years N=426 |
DOR >10 years N=309 |
p-value2 |
|---|---|---|---|---|---|
| N (%) | |||||
| Maternal Rating of Child Health Fair or Poor | 100 (9.4%) | 55 (18.3%) | 72 (17.0%) | 35 (11.3%) | 0.04 <0.001 |
| Admission from the ED1 on the Day of Interview | 136 (12.7%) | 72 (23.8%) | 95 (22.3%) | 60 (19.4%) | 0.40 <0.001 |
| Developmental Risk (Ages >4 mo, n = 1546) | 169 (20.5%) | 33 (16.6%) | 46 (16.1%) | 47 (19.8%) | 0.52 0.31 |
| History of prior hospitalization | 245 (23.1%) | 70 (23.4%) | 100 (23.5%) | 65 (21.2%) | 0.74 0.89 |
ED - Emergency Department
the first p-value given compares percentages across the 3 DOR groups, excluding US Born mothers. The second p –value given compares percentages across 4 groups including US Born mothers.
Controlling for covariates, maternal rating of child health as fair/poor also differed significantly when comparing FBM with DOR<5 years to DOR>10 years (AOR 2.49 [1.70, 3.64] vs 1.48 [0.97, 2.27]; p=0.03). Admission from the ED in children of FBM vs USBM showed trends of decreased odds of each outcome with each incremental increase in DOR, but all odds remained elevated compared to children of USBM. [Table 6]
Table 6:
Adjusted Associations of Maternal Duration of Residence in the US with Child Health
| US-Born Latina Mother |
DOR<5 years AOR2 (95% CI) |
DOR 5–10 years AOR2 (95% CI) |
DOR >10 years AOR2 (95% CI) |
DOR>10 Vs DOR<5 p-value3 |
|
|---|---|---|---|---|---|
| Maternal Rating of Child Health Fair or Poor | 1.00 | 2.49 (1.70, 3.64) p<0.001 |
2.25 (1.58, 3.19) p<0.001 |
1.48 (0.97, 2.27) p=0.07 |
0.03 |
| Admission from the ED1 on the Day of Interview | 1.00 | 1.89 (1.35, 2.65) p<0.001 |
1.80 (1.33, 2.46) p<0.001 |
1.75 (1.24, 2.49) p=0.002 |
0.71 |
| Developmental Risk | 1.00 | 0.93 (0.61, 1.44) p=0.75 |
0.89 (0.61, 1.30) p=0.54 |
1.06 (0.72, 1.54) p=0.78 |
0.30 |
| History of Prior Hospitalization | 1.00 | 1.17 (0.85, 1.61) p=0.32 |
1.14 (0.86, 1.51) p=0.37 |
0.95 (0.69, 1.31) p=0.76 |
0.63 |
Adjusted for child age, sex, gestational age, breastfed, maternal depression, maternal education. The reference group is US Born Latina Mothers.
ED - Emergency Department
AOR and p-value are comparing DOR group to US-Born Latina mothers
p-value testing differences in AOR between DOR <5 years and DOR > 10 years
Mediation Analyses
Mediation analyses examined HFI and CFI as well as SNAP participation as potential mediators of the association between mother’s birthplace and the outcomes of child health and of admission to the hospital. Child but not household FI partially mediated fair/poor health and was statistically significant, but with small attenuation of the odds (AOR 2.07 decreased to 1.98, with Sobel p = 0.02). Child FI was borderline significant as a mediator for hospital admission from the ED (p=0.08 Sobel test), with little attenuation of mother’s place of birth OR from 1.80 to 1.75 (1.37, 2.25). Mediation was not significant for admission from the ED for either HFI or CFI. There was partial mediation by SNAP participation on admission from the ED, again with small attenuation of the AOR from 1.80 to 1.64 (Sobel p = 0.02), but not on reported child health.
DISCUSSION
In this study, we analyzed maternal and child characteristics as predictors of health outcomes beyond infancy to elucidate how the demographic and health risks for a growing, diverse group of US-born children of Latinx immigrant mothers differ from children of Latinx US-born mothers. US born children of FBM compared with children of USBM were more likely to have fair/poor child health, and to be admitted to the hospital from an ED visit. Odds of poor health and hospital admission from the ED were highest among children of FBM with shortest duration of residence in the US. Households with US born children of FBM were less likely to participate in SNAP and more likely to experience household and child food insecurity, but these characteristics only slightly attenuated the odds ratios of several of our examined outcomes.
Our study adds new information regarding how maternal immigrant status is related to health of young Latinx children, particularly those not of Mexican heritage. Our results extend data from a previous multicenter Children’s HealthWatch study that showed maternal rating of child health as fair or poor was more common among children of FBM than among children of USBM, and that FBM households were also at higher risk of food insecurity, particularly for those most recently arrived. That study, using data from 1998–2005, was not restricted to Latinx ethnicity and had quite variable immigrant populations by study site.5 We also added the other child health outcomes beyond maternal self-rated health; the finding of increased odds of hospital admission from the ED has implications for the health of children of Latinx mothers as well as health system costs. Other studies have shown similar effects of immigrant status on child and adult health; adult Latinx non-citizens may also have worse health than citizens.6,26
This study also adds to the literature in its focus on the largely non-Mexican population of Latinx children living in Boston. Prior health research on Latinx immigrants, including the Hispanic National Health and Nutrition Examination Survey, has primarily focused on Latinx populations with Mexican heritage.27 In our study, only 1% of FBM reported Mexico as their place of birth, while 27% were born in Honduras, Guatemala and El Salvador. From 2007 to 2015, the number of immigrants from these three countries rose by 25%.28 The current sample approximates the most recent Boston citywide data which found that half of Boston’s Latinx population is US-born (US Mainland or Puerto Rico) and the majority of those who are not US-born are from the Caribbean and Central America, with 6% from Mexico, compared to 32% nationally.29,30 Our sample is drawn from the Boston Medical Center ED, which provided 32% of emergency visits for Boston residents under 18 from 2004–2014 (all insurance types included).31 Given the increasing numbers of Latinx of Central American heritage in the US, health risks and outcomes specific to this population warrant separate investigation.32
Worse child health and increased odds of hospital admission among children of FBM were observed despite the presumed beneficial effects of the Hispanic health paradox. Although data supporting the Hispanic health paradox appears strongest in populations of Mexican heritage (only 1% of our study’s participants),13 this paradox may still have attenuated adverse effects of low-income and poverty and lack of access to health care on child health.33
Our finding of lower SNAP participation as well as lower household amounts received among FBM results from multiple factors, including difficulty experienced by immigrants and their caseworkers in understanding eligibility rules, complex application processes, language barriers, and transportation problems,34 as well as fears of negatively impacting their own or family members’ immigration status, even among documented immigrants.10,35 Although US-born and immigrant children with legal residence status who meet household income eligibility criteria are eligible for SNAP, most foreign-born parents who have resided in the US for less than five years are not eligible, leading to lower total household benefit amounts for SNAP even if children participate.36 In contrast, WIC eligibility is not restricted or proposed to be restricted by immigration status,34 which is one possible explanation for the higher participation of more recently arrived FBM in WIC. Many FBM with longer DOR arrived in the US as children or adolescents and thus likely have fewer language barriers; however, they may still experience barriers to participation in SNAP and other programs. This may help to explain why even children of FBM with DOR>10 years have higher odds of worse health and hospital admission.
Mediation analysis found that child food insecurity and SNAP participation only slightly attenuated the odds of diminished child health and increased odds of hospital admission, respectively. Prior literature has shown associations between food insecurity and poor health outcomes as well as protective effects of SNAP.37,38 The prior multi-site Children’s Health Watch study by Chilton et al, not restricted by ethnicity, did find that food insecurity mediated the association between immigrant status and child health for children of mothers with DOR <10 years.5 The sample size was larger in that study, and the change in AOR was also small. In our study, our findings of weak mediation by CFI and no mediation by HFI suggest that other unmeasured factors related to immigrant status may explain the relationship.39 These factors may include difficulty accessing multiple programs and services, beyond SNAP, as well as discrimination/bias and language barriers.
Language may explain in part the association of FBM with poor maternal rating of child health and higher odds of admission, as well as the lack of difference in developmental risk measurement. Language of interview (Spanish vs English) has been associated with worse maternal rating of child health, which may be culturally mediated in part by differing perceptions/translations of fair health that may change along with increased usage of English language.40 Language barriers may also result in worse access to and quality of medical care. 41 Among pediatric patients/families, limited English proficiency has also been associated with increased admission from the ED, after controlling for other variables including acuity of presentation.42 Conversely, children in Spanish- vs English-speaking households are less likely to be reported by their parents to be at risk for developmental and behavioral disorders.43 Thus, it is possible that effects of FBM on this outcome were attenuated by more interviews having been conducted in Spanish or by associated cultural or other factors.
This study’s strengths include its focus on a high-risk, diverse sample of Latinx families that is distinct from the most-studied Latinx populations of Mexican heritage and which is reflective of the national trend of increasing immigration from Central America. This “sentinel sampling” has strength in that it is designed to signal early trends in the highest risk populations before they may be widely generalizable.11 Limitations include lack of sufficient power to analyze whether outcomes differed by maternal country of origin; related analysis was done previously in a multi-site Children’s HealthWatch analysis and would be an important topic for future study.44 The concept of depression may differ cross-culturally, and the scale used in this study has not, to our knowledge, been specifically validated in Spanish. Finally, collinearity between mother’s place of birth and language of interview made it impossible to control for language in our analyses and the dataset lacked information about the level of language proficiency or increasing familiarity and comfort with US dominant culture.
Medical and public health practice systems should incorporate screening and intervention for social determinants of health, such as food insecurity as recommended by the American Academy of Pediatrics,45 and should be aware that regardless of legal status and eligibility, children of FBMs participate in SNAP less frequently and receive smaller amounts when they do participate. There are many unmeasured factors which may be mediating the association between immigrant status and child health outcomes, and further research is needed regarding remediable factors. This study provides a baseline which will be informative in interpreting future data and suggests a need for further research on the impact of current policies that may jeopardize the immigration status of FB parents of US-born children who participate in public nutrition-related and other programs.
What’s New:
Compared to children of Latina US-born mothers, US-born children of Latina foreign-born mothers were more likely to be food insecure, less likely to receive SNAP, had worse maternal rating of health, and more likely to be admitted to the hospital.
Acknowledgments
Funding Source: Margot Tang was supported by an institutional grant from NIH 2T32DK007477–31A1 and by the Harvard-wide Pediatric Health Services Research Fellowship Program. The work of Children’s HealthWatch is supported by private foundations and generous donors. Complete list of supporters is available at: www.childrenshealthwatch.org. Funders had no involvement in study design, in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Abbreviations:
- ED
Emergency Department
- CFI
Child Food Insecure
- FBM
Foreign-born mothers
- FI
Food Insecurity
- HFI
Household Food Insecure
- PEDS
Parents’ Evaluation of Developmental Status
- SNAP
Supplemental Nutrition Assistance Program
- US
United States
- USBM
United States-born mothers
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: Dr. Huh is employed as a Medical Director at Takeda Pharmaceuticals. This work was completed prior to Dr. Huh’s employment at Takeda Pharmaceuticals. The other authors have no financial relationships relevant to this article to disclose.
References
- 1.Stepler R, Brown A. Statistical Portrait of Hispanics in the United States [press release]. Pew Research Center, April 2016 2016. [Google Scholar]
- 2.Patten E. The Nation’s Latino Population is Defined by Its Youth. Pew Research Center;2016. [Google Scholar]
- 3.Huang ZJ, Yu SM, Ledsky R. Health status and health service access and use among children in U.S. immigrant families. Am J Public Health. 2006;96(4):634–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coleman-Jensen ARM, Gregory C, Singh A. Household Food Security in the United States in 2014. USDA;2015. [Google Scholar]
- 5.Chilton M, Black MM, Berkowitz C, et al. Food insecurity and risk of poor health among US-born children of immigrants. American journal of public health. 2009;99(3):556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalil A, Chen JH. Mothers’ citizenship status and household food insecurity among low-income children of immigrants. New Dir Child Adolesc Dev. 2008;2008(121):43–62. [DOI] [PubMed] [Google Scholar]
- 7.Rubio R, Grineski SE, Morales DX, Collins TW. The Role of Parents’ Nativity in Shaping Differential Risks of Food Insecurity Among US First Graders. Matern Child Health J. 2019;23(7):910–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook JT, Frank DA, Berkowitz C, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. The Journal of nutrition. 2004;134(6):1432–1438. [DOI] [PubMed] [Google Scholar]
- 9.Arteaga I, Potochnick S, Parsons S. Decomposing the Household Food Insecurity Gap for Children of U.S.-Born and Foreign-Born Hispanics: Evidence from 1998 to 2011. J Immigr Minor Health. 2017;19(5):1050–1058. [DOI] [PubMed] [Google Scholar]
- 10.Capps R, Fix M, Ost J, Reardon-Anderson J, Passel J. The Health and Well-Being of Young Children of Immigrants. Washington, D.C.: Urban Institute; Feb 8, 2005. [Google Scholar]
- 11.Ettinger de Cuba S, Chilton M, Bovell-Ammon A, et al. Loss Of SNAP Is Associated With Food Insecurity And Poor Health In Working Families With Young Children. Health Aff (Millwood). 2019;38(5):765–773. [DOI] [PubMed] [Google Scholar]
- 12.Van Hook J, Balistreri KS. Ineligible parents, eligible children: Food Stamps receipt, allotments, and food insecurity among children of immigrants. Social Science Research. 2006;35(1):228–251. [Google Scholar]
- 13.Teruya SA, Bazargan-Hejazi S. The Immigrant and Hispanic Paradoxes: A Systematic Review of Their Predictions and Effects. Hisp J Behav Sci. 2013;35(4):486–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Markides KS, Rote S. The Healthy Immigrant Effect and Aging in the United States and Other Western Countries. Gerontologist. 2019;59(2):205–214. [DOI] [PubMed] [Google Scholar]
- 15.Balcazar AJ, Grineski SE, Collins TW. The Hispanic health paradox across generations: the relationship of child generational status and citizenship with health outcomes. Public Health. 2015;129(6):691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic Paradox in Biological Risk Profiles. American Journal of Public Health. 2007;97(7):1305–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanchez-Vaznaugh EV, Braveman PA, Egerter S, Marchi KS, Heck K, Curtis M. Latina Birth Outcomes in California: Not so Paradoxical. Matern Child Health J. 2016;20(9):1849–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Humes K, Jones N, Ramirez R. Overview of Race and Hispanic Origin: 2010. U.S. Census Bureau;2011. [Google Scholar]
- 19.Teitler JO, Hutto N, Reichman NE. Birthweight of children of immigrants by maternal duration of residence in the United States. Soc Sci Med. 2012;75(3):459–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glascoe FP. Evidence-based approach to developmental and behavioural surveillance using parents’ concerns. Child Care Health Dev. 2000;26(2):137–149. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey III. In:1994.
- 22.Glascoe FP. Collaborating with parents : using parents’ evaluation of developmental status to detect and address developmental and behavioral problems. Nashville, TN: Ellsworth & Vandermeer; 1998. [Google Scholar]
- 23.Kemper KJ, Babonis TR. Screening for maternal depression in pediatric clinics. Am J Dis Child. 1992;146(7):876–878. [DOI] [PubMed] [Google Scholar]
- 24.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service;2000. [Google Scholar]
- 25.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. [DOI] [PubMed] [Google Scholar]
- 26.Rabbitt MP, Smith MD, Coleman-Jensen A. Food Security Among Hispanic Adults in the United States, 2011–2014. United States Department of Agriculture, Economic Research Service; May 2016 2016. [Google Scholar]
- 27.National Health and Nutrition Examination Survey; 2011–2012 Data Documentation, Codebook, and Frequencies; Demographic Variables & Sample Weights (DEMO_G). In:2013.
- 28.Cohn DPJ, Gonzalez-Barrera A. Rise in U.S. Immigrants From El Salvador, Guatemala and Honduras Outpaces Growth From Elsewhere. Washington, D.C.: Pew Research Center;2017. [Google Scholar]
- 29.Flores A. How the U.S. Hispanic population is changing. Pew Research Center; September 18, 2017. [Google Scholar]
- 30.Schuster L, et al. Powering Greater Boston’s Economy: Why the Latino Community is Critical to our Shared Future. Boston Indicators; June 7, 2017. [Google Scholar]
- 31.Murphy J. In: Deborah Frank M, ed. DATA SOURCE: Acute hospital case-mix databases, Massachusetts Center for Health Information and Analysis; DATA ANALYSIS: Research and Evaluation Office, Boston Public Health Commission ed. [Google Scholar]
- 32.Ataiants J, Cohen C, Riley AH, Tellez Lieberman J, Reidy MC, Chilton M. Unaccompanied Children at the United States Border, a Human Rights Crisis that can be Addressed with Policy Change. J Immigr Minor Health. 2018;20(4):1000–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flores G, Olson L, Tomany-Korman SC. Racial and Ethnic Disparities in Early Childhood Health and Health Care. Pediatrics. 2005;115(2):e183–e193. [DOI] [PubMed] [Google Scholar]
- 34.Pereira K, Crosnoe R, Fortuny K, et al. Barriers to Immigrants’ Access to Health and Human Services Programs. Washington, D.C.: US Department of Health and Human Services;2012. [Google Scholar]
- 35.Hacker K, Chu J, Leung C, et al. The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA. Social Science & Medicine. 2011;73(4):586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Broder T, Moussavian A, Blazer J. Overview of Immigrant Eligibility for Federal Programs. Los Angeles, CA: National Immigration Law Center;2015. [Google Scholar]
- 37.Kreider B, Pepper JV, Gundersen C, Jolliffe D. Identifying the Effects of SNAP (Food Stamps) on Child Health Outcomes When Participation Is Endogenous and Misreported. Journal of the American Statistical Association. 2012;107(499):958–975. [Google Scholar]
- 38.Black MM, Cutts DB, Frank DA, et al. Special Supplemental Nutrition Program for Women, Infants, and Children participation and infants’ growth and health: a multisite surveillance study. Pediatrics. 2004;114(1):169–176. [DOI] [PubMed] [Google Scholar]
- 39.Frank DA, Casey PH, Black MM, et al. Cumulative hardship and wellness of low-income, young children: multisite surveillance study. Pediatrics. 2010;125(5):e1115–1123. [DOI] [PubMed] [Google Scholar]
- 40.Jimenez M, You X, Padilla Y, et al. Language of Interview: Importance for Hispanic Mothers’ Self-Rated Health and Reports of Their Children’s Health Working Paper #2007–13-FF. In: Center for Research on Child Wellbeing; 2007. [Google Scholar]
- 41.Flores G. Families Facing Language Barriers in Healthcare: When Will Policy Catch Up with the Demographics and Evidence? J Pediatr. 2014;164(6):1261–1264. [DOI] [PubMed] [Google Scholar]
- 42.Rogers AJ, Delgado CA, Simon HK. The effect of limited English proficiency on admission rates from a pediatric ED: stratification by triage acuity. Am J Emerg Med. 2004;22(7):534–536. [DOI] [PubMed] [Google Scholar]
- 43.Zuckerman KE, Boudreau AA, Lipstein EA, Kuhlthau KA, Perrin JM. Household language, parent developmental concerns, and child risk for developmental disorder. Acad Pediatr. 2009;9(2):97–105. [DOI] [PubMed] [Google Scholar]
- 44.Chilton M, Ettinger de Cuba S, and Cutts DB et al. La alimentación y el bienestar de los ciudadanos estadounidenses más jóvenes de madres mexicanas, centroamericanas, y caribeñas. Cahiers Alhim de la Universidad de Paris 8 de Saint-Denis (May 2008.).
- 45.Promoting Food Security for All Children. Pediatrics. 2015;136(5):e1431–e1438. [DOI] [PubMed] [Google Scholar]


