Abstract
Objective: Mindfulness-Based Cognitive Therapy (MBCT) is a promising psychosocial intervention for adult ADHD. The feasibility and effectiveness of an adapted MBCT program is explored, together with the possible process of change. Method: Mixed-method study with 31 ADHD patients participating in an adapted MBCT program. Self-report questionnaires on ADHD symptoms, executive functioning, mindfulness skills, self-compassion, patient functioning, and health status were administered before and after MBCT. Semi-structured interviews were conducted with 24 patients. Results: A modest drop-out of n = 5 (16%) was found. MBCT resulted in a significant reduction of ADHD symptoms and improvements of executive functioning, self-compassion, and mental health. Qualitative analysis provided insight in facilitators and barriers participants experienced, and their process of change. Conclusion: The adapted MBCT program seemed to be feasible for adults with ADHD and preliminary evidence for the effectiveness is shown. An adequately powered Randomized Controlled Trial (RCT) is needed to further examine the effectiveness of MBCT for ADHD.
Keywords: MBCT, adult ADHD, adult ADHD treatment, mindfulness, qualitative research
Introduction
ADHD is a neurodevelopmental disorder with a high persistence of core symptoms such as inattention, hyperactivity, and impulsivity into adulthood (Biederman, Petty, Clarke, Lomedico, & Faraone, 2011). A meta-analysis demonstrated a pooled prevalence of ADHD in adults of 2.5% (Simon, Czobor, Balint, Meszaros, & Bitter, 2009). Core symptoms are often associated with significant impairments in psychosocial, educational, and occupational functioning (Biederman et al., 2006; Gjervan, Torgersen, Nordahl, & Rasmussen, 2012). Moreover, adults with ADHD have higher rates of substance use, traffic violations, arrests, decreased quality of life, and sexual problems than those without ADHD (Biederman et al., 2006).
Although the National Institute for Health and Clinical Excellence (NICE) guideline on adults with ADHD (NICE, 2009) recommends pharmacological treatment with stimulants as part of a comprehensive treatment program, little is known about the effectiveness of nonpharmacological treatments for this population. Despite the demonstrated efficacy of stimulants (Mészáros et al., 2009), there is an urgent need for psychosocial interventions. First of all, not all patients respond adequately to stimulants (Wigal et al., 2010). Second, some patients experience adverse effects which can lead to discontinuation (Gajria et al., 2014). And finally, not all patients are willing to take medication, for instance because they wish to cope without medication (Matheson et al., 2013). A qualitative study in adult patients with ADHD showed that although medication was perceived as necessary by most, many of them felt that medication by itself was insufficient and would wish for additional psychosocial therapy (Matheson et al., 2013). Consequently, evidence-based psychosocial treatments focusing on alleviating ADHD symptoms and learning how to cope with residual symptoms and functional impairments are necessary in addition to or as an alternative for pharmacological treatment.
Promising psychosocial interventions for ADHD are Mindfulness-Based Interventions (MBIs). A well-known definition of mindfulness is intentionally paying attention moment by moment, in a non-judgmental way (Kabat-Zinn, 1990). Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT) are widely applied for patients with both physical and psychiatric conditions (Khoury et al., 2013). While the MBSR program is often applied to patients with chronic medical conditions, MBCT is the most commonly used MBI for patients with chronic psychiatric disorders (Segal, Williams, & Teasdale, 2012). MBCT was originally developed as a preventative intervention for patients with recurrent depression and has shown to be effective in patients with three or more prior depressive episodes (Chiesa & Serretti, 2011; Warren et al., 2016). A range of studies demonstrated preliminary evidence for the effectiveness of MBCT in other chronic psychiatric disorders, for instance in bipolar disorder (Strauss, Cavanagh, Oliver, & Pettman, 2014) and generalized anxiety disorder (Wong et al., 2016).
As research demonstrates that mindfulness meditation strengthens attention regulation (Fox et al., 2014; Malinowski, 2013; Tang, Holzel, & Posner, 2015) and improves executive functions (Chiesa, Calati, & Serretti, 2011), MBIs seem particularly promising for adults with ADHD (Bachmann, Lam, & Philipsen, 2016). Although offering MBIs for adult ADHD is relatively new (Cairncross & Miller, 2016), a few different MBIs have already been developed and examined for this patient group: Mindful Awareness Practices (Zylowska et al., 2008), Mindfulness-Based Group Training (Edel, Hölter, Wassink, & Juckel, 2014), and an adapted and extended MBCT program (Hepark et al., 2015). Preliminary evidence was found for the effect of MBIs in reducing core ADHD symptoms, improving executive functioning, and emotion regulation (Cairncross & Miller, 2016; Hepark et al., 2015; Mitchell, Zylowska, & Kollins, 2015), but further, well-designed studies are needed to investigate this. The treatment protocols of the abovementioned MBIs for adult ADHD were based on clinical assumptions about necessary modifications of standard mindfulness programs, like the MBSR or MBCT. However, it is not clear how ADHD patients perceive MBCT, and particularly what are considered the barriers and facilitators of such a protocol. Qualitative research is a valuable methodology to study this, as it can provide an elaborate reflection of persons’ personal experiences. Hence, the aim of this study was to examine the following research questions: (1) Is MBCT a feasible intervention for adults with ADHD?; (2) Is MBCT potentially effective in alleviating ADHD symptoms and improving executive functioning?; (3) What barriers and facilitators do patients with ADHD experience while participating in the MBCT? and (4) What do patients with ADHD learn from participating in MBCT?
Methods/Design
Study Design
A mixed-method pilot study (including quantitative and qualitative methodology) was conducted, following the guidelines for Good Reporting of a Mixed Method Study (GRAMMS; O’Cathain, Murphy, & Nicholl, 2008). The quantitative part of the study concerned the possible effectiveness of the intervention. In the qualitative part of this study the barriers and facilitators of an adapted MBCT program for adult ADHD patients were explored together with the process of change of the participants during and after the intervention. A multimethod approach was chosen with focus groups as primary method and individual interviews as secondary method, as focus groups are particularly suited for research questions focused on attitudes and experiences (Pope & Mays, 1999).
Participants
Patients were referred to the MBCT group by their general practitioner or by clinicians of the Radboudumc department of psychiatry, a specialist tertiary care center for the diagnosis and treatment of adult ADHD. We included patients with a primary diagnosis of ADHD, according to the criteria of Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR; American Psychiatric Association, 2000). Due to the exploratory character of the study, we only used a few exclusion criteria: (a) psychotic symptoms or suicidality, (b) current manic episode, and (c) learning difficulties or other cognitive impairments hampering participation in the MBCT.
Procedure
Interested patients were invited for a research interview, during which they were provided with extensive information about participation in the pilot study. Patients did not receive any payment for their participation. As the intervention was already applied as part of the regular care program for adults with ADHD, formal approval of the local medical ethics committee was not necessary. Patients were assessed with the psychiatric structured diagnostic interview MINI-Plus (Van Vliet & De Beurs, 2007) as part of the clinical routine at the Radboudumc department of psychiatry. The period between assessment and start of the intervention varied between 0 and 18 months in our population with a mean of 5 months.
All participants received online self-report questionnaires before and after MBCT. Three months after the start of the MBCT, they were invited to take part in a 2-hr focus group interview. Patients who were not able to participate in a focus group were invited for an individual semi-structured interview of 30 to 45 min by phone or face-to-face.
The first three focus group interviews were conducted by a psychiatrist and qualified mindfulness teacher (A.S.), the fourth by a psychologist and qualified mindfulness teacher (L.J.). The individual interviews were partly conducted by the same psychologist (L.J.) and partly by a research master student (A.V.). All interviewers were independent and had not been involved in the clinical care of the patients. A topic list of core questions was used that defined the areas to be covered during the interview (see Table 1). Focus group interviews were video-taped and individual interviews audio-taped. The participants gave written permission for the recording of the interviews. We did a member-check by sending a summary of the interviews to the patients to check whether their answers were interpreted in a correct way. Evaluation forms of a different sample of adult ADHD patients were used for triangulation to strengthen confidence in the validity of the findings. These forms were filled-out by 24 patients after having participated in the adapted MBCT training developed for adult ADHD.
Table 1.
Topic list of semi-structured interviews.
| 1. Feasibility of MBCT: |
| • Barriers of participation in general and due to ADHD symptoms |
| • Facilitators of participation |
| 2. Process of change: |
| • General functioning |
| • Coping with ADHD symptoms and functional impairments |
| • View of self |
Note. MBCT = Mindfulness-Based Cognitive Therapy.
Intervention
The training was primarily based on the MBCT (Segal et al., 2012), which consists of eight-weekly sessions of 2.5 hr each and a silent day between Sessions 6 and 7. Participants were instructed to practice at home for about 30 min per day with guided mindfulness exercises on CD’s and to complete home assignments in a workbook. Some modifications in the original MBCT program were made to make the intervention more suitable for adults with ADHD. These modifications were based on the Mindful Awareness Practices (MAPs) for ADHD program (Mitchell et al., 2015; Zylowska et al., 2008) and the extended and adapted MBCT program used in our previous study (Hepark et al., 2015). The content of the program in this pilot study was very similar to the MBCT program described in the protocol paper of our subsequent and ongoing randomized controlled trial (Janssen et al., 2015), see Table 2. The MBCT was taught by three qualified mindfulness teachers who met the advanced criteria of the Association of Mindfulness-Based Teachers in the Netherlands and Flanders and the internationally agreed good practice guidelines of the UK Network for Mindfulness-Based Teachers (http://mindfulnessteachersuk.org.uk/pdf/teacher-guidelines-2015.pdf).
Table 2.
Content of MBCT Program for ADHD Per Session.
| Theme of the session | Mindfulness exercises | (Psycho)education | Homework |
|---|---|---|---|
| 1. Automatic pilot | • 3-min breathing space • Raisin exercise • Bodyscan |
• Rationale of mindfulness for ADHD • Introduction in methods to integrate mindfulness in daily life: Support, Structure, and Strategy (3 Ss) |
• Breathing space • Attention for a routine activity • Mindful eating • Optional instead of compulsory: Short or long bodyscan |
| 2. Dealing with barriers | • Bodyscan • Sitting meditation with focus on breath • 3-min breathing space |
• Imagery exercise to demonstrate relationship between thoughts and feelings • Exploration of application of the 3 Ss |
• Optional instead of compulsory: Breathing space • Attention for a routine activity • Bodyscan • Awareness of pleasant events |
| 3. Mindfulness of the breath | • Sitting meditation with focus on breath, body • 3-min breathing space • Floor yoga practices • Walking meditation |
• Seeing exercise (a) to demonstrate the difference between observation and interpretation, (b) to discuss dealing with sensory input • Exploration of pleasant events |
• Daily instead of 3 times a day: breathing space • Floor yoga or sitting meditation • Awareness of unpleasant events |
| 4. Staying present | • Sitting meditation with focus on breath, body, sounds • 3-min breathing space • Walking meditation instead of floor yoga practices |
• Exploration of unpleasant events with attention for the interrelatedness of feelings, thoughts, and bodily sensations • Exercise focused on recognition and dealing with ADHD core symptoms |
• Daily instead of 3 times a day: breathing space • Sitting meditation • Awareness of top 3 ADHD symptoms |
| 5. Allowing and letting be | • Sitting meditation with focus on breath, body, sounds, thoughts, and feelings • 3-min breathing space “coping” • Standing yoga practices |
• Reflection on intention of participating • Psychoeducation about reacting versus responding in stressful situations and when ADHD symptoms are severe |
• Daily instead of 3 times a day: breathing space • Sitting meditation or standing yoga • Awareness of communication difficulties |
| 6. Mindful communication | • Standing yoga practices • 3-min breathing space |
• Exercise in mindful listening and speaking • Nonverbal communication exercise |
• Daily instead of 3 times a day: breathing space • Sitting meditation or standing yoga • Mindful listening and speaking |
| Silent day | • Varying meditation exercises • Silent lunch and tea break |
||
| 7. Taking care of yourself | • Sitting meditation with focus on breath, body, sounds, thoughts, emotions, and choiceless awareness • 3-min breathing space |
• Exercise on taking care of yourself by examining how to improve balance in life | • Breathing space • Practice without CDs • Reflect on training • Making an action plan |
| 8. The rest of your life | • Bodyscan • 3-min breathing space |
• Reflection on the training • Maintaining practice |
Note. Training components in bold indicate modifications we made in the original protocol based on this pilot study. MBCT = Mindfulness-Based Cognitive Therapy.
Outcome Measures
ADHD symptoms
The Conners’ Adult ADHD Rating Scale (CAARS-S; Conners, Erhardt, & Sparrow, 1999) is a 30-item self-report questionnaire. A Total Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994) ADHD Symptom score, an Inattention score, and a Hyperactivity-Impulsivity score are calculated. All subscales have shown good internal consistency and interrater reliability, as well as sensitivity to treatment outcome. Cronbach’s α coefficients varied from .76 to .95 at different time points (Adler et al., 2007).
Executive functioning
The adult version of the Behavior Rating Inventory of Executive Function (BRIEF-A; Roth & Gioia, 2005) is a 75-item self-report questionnaire yielding an overall score composed of two index scores: the Behavioral Regulation Index and the Metacognition Index. The Behavioral Regulation Index consists of four scales (Inhibit, Shift, Emotional Control, and Self-Monitor) and the Metacognition Index of five scales (Initiate, Working Memory, Plan/Organize, Task Monitor, and Organization of Materials). For the Dutch version of this questionnaire, Cronbach’s α coefficients ranged from .70 to .89 and test-retest reliability was .70 or higher (Scholte & Noens, 2011).
Mindfulness skills
The short form of the Five Facet Mindfulness Questionnaire (FFMQ-SF; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006; Bohlmeijer, Peter, Fledderus, Veehof, & Baer, 2011) is a 24-item self-report questionnaire which distinguishes five facets of mindfulness: Observing, Describing, Acting With Awareness, Non-judging, and Non-reactivity. The Dutch version of this questionnaire showed to be a reliable instrument which is sensitive to change in a population with depressive and anxiety symptoms. Cronbach’s α coefficients varied between .75 and .87 (Bohlmeijer et al., 2011).
Self-compassion
The short form of the Self-Compassion Scale (SCS-SF; Neff, 2003; Raes, Pommier, Neff, & Van Gucht, 2011) is a 12-item self-report questionnaire which measures six components of self-compassion: Self-Kindness, Self-Judgment, Common Humanity, Isolation, Mindfulness, and Over-identification. The shortened scale showed a near-perfect correlation with the original Self-Compassion Scale. In a Dutch population, the Cronbach’s α coefficient for the full scale is .87 and the coefficients for the subscales varied from .55 to .81. The internal consistency of the subscale Self-Kindness was relatively low (Raes et al., 2011).
General functioning
The Outcome Questionnaire (OQ 45.2; Lambert et al., 1996) is a 45-item self-report questionnaire. The Dutch version of the OQ showed Cronbach’s α coefficients between .69 and .93 and Pearsons’ r varied from .70 to .83 in a clinical population (de Jong et al., 2007).
Health status
The shortened version of the Health Survey (SF-12; Ware, Kosinski, & Keller, 1996) is a 12-item self-reported questionnaire based on the SF-36 (McHorney, Ware, & Raczek, 1993). The questionnaire divides eight domains in two main components: a physical component summary (physical functioning, role limitations due to physical problems, bodily pain, and general health) and a mental component summary (role limitations due to emotional problems, mental health, social functioning, and vitality). Internal consistency was acceptable, with a Cronbach’s α coefficient of .84 for the physical component and .81 for the mental component (Lim & Fisher, 1999). Found test-retest reliability coefficients were .89 for the physical component and .76 for the mental component measured in a population in the United States (Ware et al., 1996).
Statistical Analyses
Quantitative analysis
Baseline sociodemographic and clinical characteristics were compared for completers and non-completers (attended <4 sessions) of the MBCT with a t-test or chi-square test. Within-group differences between scores at baseline and at the end of the MBCT were computed with paired t-tests on an intention-to-treat basis. A Cohen’s d effect size was calculated for the within-group difference at the end of treatment based on the standard deviation at baseline. In addition, we calculated the number of patients who showed a clinical relevant improvement or deterioration in ADHD symptoms, as defined by a decrease or increase of ≥30% on the total DSM-IV score of the CAARS.
Qualitative analysis
The video/audio-tapes of the focus group and individual interviews were transcribed and analyzed based on the thematic analysis approach (Braun & Clarke, 2006). A qualitative software package (Atlas.ti) was used to assist in the coding of the transcribed verbatim. To ensure reliability, the transcripts were coded independently by two researchers (L.J. and A.V.). After each focus group interview, the found codes were compared and discussed until agreement was reached. The modified list of codes was used during the analyses of the following focus group interviews. The codes were grouped into categories and (sub)themes during a research team meeting with the involved researchers (A.S., L.J., and A.V.) and a psychiatrist (S.H.) with expertise in diagnosing and treating adult ADHD. Filled-out evaluation forms of a different sample of 24 adults with ADHD were used for triangulation.
Results
Study Population
A total of 31 patients participated in three pilot groups. Sixteen (52%) of the patients were referred by the specialist outpatient clinic of the Radboudumc and 15 (48%) by their general practitioner. Most patients were diagnosed with the inattentive subtype (n = 14, 45%) or the combined subtype (n = 14, 45%; see Table 3). A total of 14 patients (45%) did not use medication for ADHD at the start of the MBCT group. The majority of the patients (n = 16, 52%) had one or more comorbid Axis 1 disorders. Twelve patients (39%) were diagnosed with a current depressive and/or anxiety disorder. Other diagnoses were a somatoform disorder (n = 2, 6%), substance dependence (n = 2, 6%), and an autism spectrum disorder (n = 2, 6%). In nine patients, a comorbid Axis 2 disorder was diagnosed in the past. Two of these patients (7%) were diagnosed with a borderline personality disorder.
Table 3.
Baseline Characteristics in Completers and Non-completers of the MBCT.
| MBCT (n = 31) | Completers MBCT (n = 26) | Non-completers MBCT (n = 5) | p value | |
|---|---|---|---|---|
| Demographic and clinical characteristics; n (%) | ||||
| Female gender | 16 (52) | 12 (46) | 4 (80) | .33a |
| Age; M (SD) | 38 (12.4) | 36 (11.9) | 51 (4.5) | <.01** |
| ADHD medication | 17 (55) | 15 (58) | 2 (40) | .64a |
| Level of education | 1.0a | |||
| Low | 3 (12) | 3 (13) | - | |
| Middle | 9 (35) | 8 (35) | 1 (33) | |
| High | 14 (54) | 12 (52) | 2 (67) | |
| Subtype of ADHD | .28a | |||
| Inattentive type | 14 (45) | 13 (50) | 1 (20) | |
| Hyperactive-impulsive type | - | - | - | |
| Combined type | 14 (45) | 10 (39) | 4 (80) | |
| Not otherwise specified type | 3 (10) | 3 (12) | - | |
| Years since ADHD diagnosis; M (SD) | 3 (3.7) | 3 (3.1) | 5 (6.3) | .49 |
| Comorbidity Axis 1 DSM-IV | 16 (52) | 12 (46) | 4 (80) | .33a |
| Comorbidity Axis 2 DSM-IV | 9 (29) | 7 (27) | 2 (40) | .61a |
| Outcome measures; M (SD) | ||||
| ADHD symptoms, CAARS self-report | ||||
| Inattention | 15.7 (3.5) | 16.0 (3.6) | 14.0 (2.2) | .30 |
| Hyperactive-impulsive | 12.5 (3.0) | 12.4 (2.9) | 13.3 (3.5) | .61 |
| Executive functioning, BRIEF-ASR | 150.4 (17.8) | 148.1 (17.9) | 165.5 (6.8) | <.01** |
| Mindfulness skills, FFMQ-SF | 73.6 (8.3) | 74.2 (8.2) | 69.3 (9.2) | .27 |
| Self-compassion, SCS-SF | 42.9 (12.2) | 43.8 (11.8) | 36.5 (14.4) | .27 |
| Patient functioning, OQ 45.2 | 73.2 (20.1) | 69.5 (18.2) | 97.3 (16.5) | <.01** |
| Health status, SF-12 | ||||
| Physical health | 38.1 (7.2) | 39.2 (7.0) | 30.6 (3.2) | .02* |
| Mental health | 35.4 (10.0) | 37.2 (9.2) | 24.2 (8.2) | .01* |
Note. Improvement is indicated by a decrease in scores on the CAARS, BRIEF-ASR, and OQ 45.2 and an increase in scores on the FFMQ-SF, SCS-SF, and SF-12. MBCT = Mindfulness-Based Cognitive Therapy; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; CAARS = Conners’ Adult ADHD Rating Scale; BRIEF-ASR = Behavior Rating Inventory of Executive Function–Adult Self-Report Version; FFMQ-SF = Five Facet Mindfulness Questionnaire Short Form; SCS-SF = Self-Compassion Scale Short Form; OQ = Outcome Questionnaire; SF-12 = Short Form of the Health Survey. aChi-Square. * Statistical significant difference for <.05. ** Statistical significant difference for <.01.
Attendance of MBCT
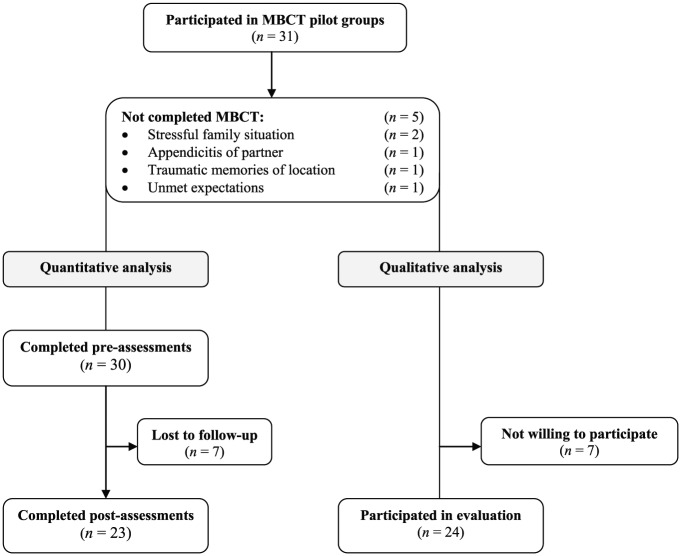
Of the 31 patients with ADHD who started with the MBCT group, five patients (16%) attended less than four sessions and were considered as non-completers (see Figure 1). Reasons for drop-out were stressful family situations (n = 2), appendicitis of partner, traumatic memories of the location the MBCT took place, and unmet expectations. Non-completers were significantly older, and reported higher levels of executive and general dysfunctioning and a lower physical and mental health status than the completers.
Figure 1.
Flowchart.
Note. MBCT = Mindfulness-Based Cognitive Therapy.
Preliminary Effectiveness of MBCT
The baseline assessment was completed by 30 patients, the post-treatment assessment by 23 patients (77%), see Figure 1. Four of the non-completers (n = 5) of the MBCT did not complete the post-treatment assessment. Study drop-outs were significantly older than study completers. Based on the intention-to-treat analysis, MBCT resulted in a significant reduction of total ADHD symptoms, and inattention and hyperactive-impulsive symptoms and an improvement of total executive functioning, the Metacognition Index and the subscales Self-Monitor, Working Memory, Plan/Organize, Task Monitor and Organization of Materials (see Table 4). Regarding ADHD symptom reduction, six patients showed a clinical relevant decrease in ADHD symptoms (26%), whereas no patients showed an increase in ADHD symptoms from pre- to post-MBCT treatment. In addition, there was a significant improvement of total self-compassion skills, the subscales Self-Kindness and Common Humanity, and mental health according to the SF-12, although physical health did not change. Finally, no substantial improvements were found in mindfulness skills, except for a trend for increasing “Acting with Awareness.”
Table 4.
Differences Within Group at the End of the MBCT Training.
| Pre-MBCT | Post-MBCT | Group difference [95% CI] | Cohen’s d | |
|---|---|---|---|---|
| ADHD symptoms, CAARS n = 23 | ||||
| Inattention | 15.8 (3.7) | 13.4 (3.2) | −2.4 [–4.0, –0.8]** | 0.65 |
| Hyperactive-impulsive | 12.3 (3.1) | 9.6 (2.7) | −2.8 [–4.1, –1.4]** | 0.90 |
| Total DSM-IV score | 28.1 (5.0) | 23.0 (3.8) | −5.2 [–7.8, –2.6]** | 1.04 |
| EF, BRIEF-ASR n = 22 | ||||
| Inhibit | 16.1 (2.4) | 15.0 (3.1) | −1.0 [–2.2, 0.1] | 0.42 |
| Shift | 11.9 (2.9) | 11.7 (2.6) | −0.2 [–1.0, 0.6] | 0.07 |
| Emotional control | 18.5 (5.7) | 17.9 (5.4) | −0.6 [–1.8, 0.6] | 0.11 |
| Self-monitor | 10.5 (2.8) | 9.5 (2.3) | −1.0 [–1.7, –0.3]* | 0.36 |
| Behavioral regulation index | 57.0 (10.4) | 54.1 (9.3) | −2.8 [–5.8, 0.2] | 0.27 |
| Initiate | 17.8 (3.5) | 17.1 (3.7) | −0.7 [–1.5, 0] | 0.20 |
| Working memory | 19.5 (2.1) | 18.5 (2.8) | −1.0 [–2.0, –0.1]* | 0.48 |
| Plan/organize | 22.5 (4.0) | 21.4 (3.9) | −1.1 [–2.2, –0.1]* | 0.28 |
| Task monitor | 13.0 (2.2) | 12.2 (2.5) | −0.7 [–1.7, 0.3] | 0.32 |
| Organization of materials | 17.3 (3.8) | 15.5 (4.0) | −1.8 [–3.0, –0.5]** | 0.47 |
| Metacognition index | 90.0 (12.7) | 84.6 (14.2) | −5.4 [–8.9, –1.9]** | 0.43 |
| Total score | 147.0 (19.0) | 138.8 (20.0) | −8.2 [–14.0, –2.4]** | 0.43 |
| Mindfulness skills, FFMQ-SF n = 22 | ||||
| Observe | 14.0 (2.9) | 14.0 (2.6) | 0.5 [–0.8, 0.9] | 0.17 |
| Describe | 16.2 (2.7) | 16.5 (3.4) | 0.4 [–0.7, 1.4] | 0.15 |
| Acting with awareness | 14.8 (3.8) | 13.4 (2.5) | −1.4 [–3.0, 0.2] | 0.37 |
| Non-judging | 14.8 (4.1) | 15.2 (3.5) | 0.4 [–1.0, 1.7] | 0.10 |
| Non-reactivity | 14.8 (3.8) | 15.2 (3.2) | 0.5 [–0.6, 1.5] | 0.13 |
| Total score | 74.5 (8.9) | 74.4 (8.2) | −0.2 [–3.1, 2.7] | 0.02 |
| Self-compassion, SCS-SF n = 22 | ||||
| Overidentification | 7.1 (4.0) | 8.0 (3.4) | 0.9 [–0.2, 2.1] | 0.23 |
| Self-kindness | 6.4 (2.1) | 8.0 (2.9) | 1.7 [0.6, 2.8]** | 0.81 |
| Mindfulness | 8.8 (3.1) | 9.5 (2.8) | 0.6 [–0.4, 1.6] | 0.19 |
| Isolation | 6.5 (3.3) | 7.6 (3.3) | 1.1 [–0.1, 2.3] | 0.33 |
| Common humanity | 7.4 (3.4) | 8.6 (2.6) | 1.3 [0, 2.5]* | 0.38 |
| Self-judgment | 6.7 (3.7) | 8.3 (3.2) | 1.5 [0, 3.1] | 0.41 |
| Total score | 42.9 (13.4) | 50.0 (14.5) | 7.1 [2.6, 11.6]** | 0.53 |
| Patient functioning, OQ 45.2 n = 22 | 69.2 (19.2) | 68.9 (17.6) | −0.3 [–6.8, 6.2] | 0.02 |
| Health status, SF-12 n = 22 | ||||
| Physical component summary | 38.8 (7.2) | 39.6 (7.2) | 0.7 [–1.8, 3.3] | 0.10 |
| Mental component summary | 37.0 (9.4) | 40.0 (11.5) | 3.1 [0.2, 6.0]* | 0.33 |
Note. Improvement is indicated by a decrease in scores on the CAARS, BRIEF-ASR, and OQ 45.2 and an increase in scores on the FFMQ-SF, SCS-SF, and SF-12. MBCT = Mindfulness-Based Cognitive Therapy; CI = confidence interval; CAARS = Conners’ Adult ADHD Rating Scale; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, 4th Edition; BRIEF-ASR = Behavior Rating Inventory of Executive Function–Adult Self-Report Version; FFMQ-SF = Five Facet Mindfulness Questionnaire Short Form; SCS-SF = Self-Compassion Scale Short Form; OQ = Outcome Questionnaire; SF-12 = Short Form of the Health Survey.
Statistical significant difference for <.05. **Statistical significant difference for <.01.
Qualitative Analysis
Of the 31 participants, 24 (77%) were willing to take part in the qualitative evaluation, see Figure 1. Fourteen of the patients participated in one of the four focus group interviews and ten were interviewed individually, seven by phone and three face-to-face. All members agreed in the member-check that the interpretation of their answers was accurate. Saturation was reached as no new codes emerged from the last few interviews. The qualitative analysis was focused on exploring the barriers and facilitators of our adapted MBCT program for adult ADHD and the process of change of the participants.
Feasibility
Analysis of the data revealed three broad categories of perceived facilitators and barriers during the MBCT: environmental factors, the training itself, and participant characteristics (see Table 5). Characteristics related to the training were further subdivided in five themes and characteristics related to the participant in four themes. Many (sub)themes could act as a facilitator as well as a barrier. A few acted only as a facilitator or barrier. Within each theme, we discussed the facilitators and barriers consecutively.
Table 5.
Themes and Subthemes of Facilitators and Barriers During the MBCT and Corresponding Quotations.
| Facilitators | Barriers | |
|---|---|---|
| Environmental factors | Support from family: And if they say “go take a three-minute break,” then I take a three-minute break. | Experiencing life stressors: It was really personal circumstances that made it harder. That made it impossible for me to concentrate and extra difficult for me to go there. |
| Training | ||
| Training program | Weekly sessions: When you come here, you’re here for two and a half hours and you force yourself to do things you’d be less likely to do at home. | Lack of repetition: That you don’t get something new every week while you feel the last thing hasn’t really sunk in yet, because it’s not in your system. |
| Content of the training | Silent day: You’re just silent for a day so you consciously don’t do things and you very consciously avoid social contact. That takes getting used to. But it’s also wonderful. ( . . . ) I’m not allowed to contact anyone, ( . . . ) so then you need to take a different direction and yes, that creates opportunities. | Long silence during meditations: In the long version ( . . . ), there’s two minutes in between and I really couldn’t concentrate on that. Because they say nothing for two minutes and I’m thinking, “is it over, is it over? Oh no darn, there’s another thirty minutes.” And then you’ve immediately lost your focus. |
| Mindfulness teacher | ||
| • Didactic approach | Directiveness: That she also briefly interrupted people, told them to take a moment. Stop ranting and raving, for example. | Homework presented as compulsory: If you set it as a task, for me it immediately becomes this big mountain, that ( . . . ) yeah I have to get over. Then I just give up. |
| • Attitude | Non-judgmental: Maybe also that it came up throughout the whole training: things are not right or wrong or it is what it is. Maybe that’s also what gave me a little push, to let things go a little more. | Not feeling accepted: I brought it up as a problem that I was struggling with, but [name teacher] was sort of like ( . . . ) that it was totally normal. Yes, I felt disappointed for a bit ( . . . ) that I didn’t really feel it was accepted that I had a problem. |
| Other participants | Contact with fellow ADHD patients: So that your own discomfort is suddenly shared by someone else and “oh yeah, okay, so it’s not me,” and that puts it into perspective. | Arriving too late: What I thought was a pity, ( . . . ) was people arriving late. I can’t recall a single session where everyone was on time. |
| Material | Folder: If you read the folder, I think it’s written really well. [ . . . ] It doesn’t tell me what to do, it doesn’t say what that person’s going through but I think it’s also written in the “we” form. | Space: Yes, lots of noise. That you heard people walking and that people also just came in, the door opening and closing during the exercises. That was a bit disturbing. |
| Participant | ||
| ADHD symptoms | Feeling restless inside: Either I felt hugely restless, or my head was somewhere else entirely. | |
| Additional symptoms | Physical complaints: At a certain point I was really ( . . . ) bothered by the pain. I just couldn’t do certain exercises any more. Suddenly I had to resort to the lying-down things ( . . . ). I even did the sitting meditation lying down. So that restricted me. | |
| Personality traits | Perseverance: I’m not a quitter ( . . . ). Yes, if you shy away from the hard stuff, that’s nice and easy but you don’t really achieve anything. ( . . . ) And I thought that now too: “I can stop, but then I don’t know if it’ll work.” | High expectations of self: Well, for me ( . . . ) that’s the expectation, because for me I think, “I’m going to do this properly again, every day straight away, I have to” and then you don’t manage to do that. |
| Coping strategies | Self-talk: Yes, just by saying to myself, “focus on your breathing, try to get into it.” | Procrastination: The will to do it is in there somewhere, but you put it off ( . . . ) postpone, postpone, postpone, avoid: “yes, soon,” or thinking vaguely again, “oh, I have to do that too.” |
Note. MBCT = Mindfulness-Based Cognitive Therapy.
Environmental factors
Several situational aspects appeared to be a facilitator or barrier. Support by a partner or relative was perceived as helpful during MBCT, whereas experiencing life stressors, and having a lack of time or a lack of structure at home were reported as barriers. Some patients considered the use of medication for ADHD as a facilitator, while others mentioned that switching medication impeded their functioning throughout the training.
Training characteristics
This category was divided in five themes: training program, content of training, mindfulness teacher, other participants, and material. Some aspects of the training program were perceived as facilitating. The diversity of the exercises and themes and the weekly sessions were for example mentioned as helpful. However, the lack of repetition of exercises, the short length of the training, and the large amount of homework were frequently considered as barriers. To create more room for repetition, some patients suggested to extend the length of the training or to offer booster sessions.
Within the content of the training some helpful training components could be distinguished: the silent day, the movement exercises, and the emphasis on informal practice. Other components of the training were considered as barriers: like the long silence in meditations, the posture during sitting meditation, and the slow pace during the exercises. About some components there was disagreement among the participants: like the long versions of meditations, the lack of social interaction during the silent day, and the amount of background theory about ADHD and mindfulness.
Most patients felt supported by their mindfulness teacher. Helpful aspects of the didactic approach of the teacher were clear communication and directiveness, while a lack of directiveness as well as an excess of directiveness were considered as barriers. Consequently, a proper amount of directiveness by the teacher seemed to be of importance. Facilitating aspects of the teachers’ attitude were for example openness, embodiment of mindfulness, and a non-judgmental and caring attitude toward the participants. On the other hand, not feeling accepted by the teacher was reported as a barrier by one patient.
Furthermore, taking part in the training with other participants was repeatedly mentioned as helpful. Especially the contact with fellow ADHD patients and the shared goal of learning mindfulness were considered as useful. Some behaviors of the other participants were perceived as barriers, like excessive talking, coming in too late, or complaining during the sessions.
Some of the participants experienced the material, especially the folder and the introduction of the CDs, as facilitating. Most of the mentioned limitations had to do with too much background noise (in the training location and on the CDs).
Characteristics of the participant
Within this category four themes emerged: ADHD symptoms, additional symptoms, personality traits, and strategies. Experiencing ADHD symptoms was often mentioned as a barrier during MBCT and at home. Throughout the training a lack of concentration, inner restlessness, and hyperactivity made it sometimes hard for participants to stay focused during the exercises and the inquiry. Furthermore, a few patients told that ADHD symptoms, like passivity and forgetfulness, had an adverse effect on their practice of mindfulness exercises at home.
Experiencing additional symptoms, like depression, anxiety, and physical symptoms, was also reported as a barrier. Some patients found it hard to be confronted with these symptoms during the training, especially when these limitations impaired their participation throughout the training, for instance in the movement exercises.
Various personality traits facilitated participation in MBCT, such as perseverance, sense of perspective, and openness to experiences. Other traits, like having high expectations and self-criticism, were considered as barriers.
Several coping strategies supported the patients during the training, for example, internal self-talk and adapting an exercise to one’s own needs. In contrast with this, procrastination was mentioned as an unhelpful coping strategy during the training, because it impeded the practice at home.
Process of Change
The qualitative data regarding the process of change revealed eight separate stages shared by most patients (see Table 6). Change typically started at the first stage and then gradually shifted to the subsequent ones. However, it is important to bear in mind that this was not an entirely linear process and all kinds of variations took place. Moreover, not all patients described all of these stages.
Table 6.
Themes and Subthemes of the Process of Change During MBCT and Corresponding Quotations.
| Examples | |
|---|---|
| 1. Stopping | Since we’re talking about stressful moments, that you can actually sort of stop, reflect on things. |
| 2. Noticing | If it’s quiet and I do the exercises, sometimes seven things are going on at once, as though they’re all happening at the same time. I almost always hear music; for example, I’ll be thinking about things from my daughter’s school, or that I still have to do this or that, or all sorts of things stacked on top of one another. |
| 3. Allowing | I think that in part I dare to allow that fear more. I don’t need, I’m just less afraid. I was like, I was always afraid, my whole life . . . and I’m now less afraid of that fear, as it were. |
| 4. Insight | It’s very enlightening to realize, ( . . . ) this is how it is. When I first heard I had ADD, I thought, that’s just having a bit of trouble concentrating and planning and things like that. But it’s everywhere, it’s in every fiber of your whole life. |
| 5. Changing perspective | So now the discovery process is starting for me, the process of “yes, so what do I really want then?” And I think I now have more headspace for that, but that causes a certain sense of unrest again. |
| 6. Self-regulation | |
| • Attention | I can spend the whole day in a haze, but when we focus consciously on our breathing, I’m able to turn it around. I also have that during meetings or discussions. If I’ve had enough at a certain point and I notice my mind wandering off, I think about the breathing and I’m able to be more present again. |
| • Impulsivity | I really feel it’s given me a sort of foothold, you learn how you can bring yourself back and pull yourself back from that impulsive behavior, and that’s really important. |
| • Hyperactivity | But also because my thoughts are somewhat calmer, I’m also calmer myself. I mean, I still need a sport to release my energy, because otherwise I’d go crazy. But ( . . . ) I was always happy to have my life dictated to me because I used to get bored very quickly, I always wanted to have something to do. And now I don’t have that as much. |
| • Working memory | Well, I invent stories and ( . . . ) I work with clay, so I’m always collecting ideas. And what I always noticed is that if I put my ideas aside, I sometimes forgot them ( . . . ). And I found that really frustrating. But now that I’m calmer I can put them to one side without accidentally losing them. So I can get them back again. |
| • Emotion regulation | Normally I would have lost my keys and then gone tearing through the house looking for them. ( . . . ) And then ( . . . ) completely losing yourself in that. And these days that just doesn’t happen anymore. When I lose something now it’s more like, “okay, then let’s just look for it,” and I go and stand calmly in my room and then at some point I find it. |
| • Goal-directed behavior | Yes, I feel much stronger. So normally when I’d walk through the department, I’d wander about and go in all directions. Now I walk in a steady, purposeful way. I know, “okay, I’m going to do this now” and I actually go and do it. |
| 7. Changing behavior | But it’s made it easier for me to ask for help. I think, “That’s going to trip me up.” My talents lie elsewhere, not in planning and organization. |
| 8. Experiencing effect | |
| • Well-being | I used to wake up every hour and a half by default. ( . . . ) I could set my watch by it, so to speak. And that happened a number of times. I don’t have that any more. I don’t know exactly when that changed, but I assume that this helped. |
| • Self-compassion | I’ve always had the tendency to get really mad at myself, like, “be careful for once” or “just be normal for once” ( . . . ). That’s changing a bit now, instead I think more like, “yeah, there I go again, this isn’t a matter of just trying harder.” ( . . . ) Yes, how would you say that … taking a slightly milder view of things. |
| • Connectedness | I’m subconsciously wired to go with the flow ( . . . ). I don’t always need to any more. ( . . . ) Because what it brings is the peace and the love that flourishes again, and well, that’s worth so much to me. |
Note. MBCT = Mindfulness-Based Cognitive Therapy.
Stopping
The first identified stage was stopping. Patients mentioned that they learned to take a break during the day and to shift their focus of attention from daily routine activities (doing mode) to their experience in the current moment (being mode).
Noticing
Throughout the MBCT, participants started to notice different aspects of their inner experience in the present moment, such as thoughts, emotions, bodily sensations. Various patients mentioned that they noticed signs of stress in an earlier stage. Sometimes patients became more aware of their tiredness when standing still.
Allowing
Noticing was regularly followed by allowing and accepting the experience as it arose. Several patients told that they learned to allow and accept their emotions, bodily sensations, inner restlessness, and pain, regardless of whether these experiences were pleasant or unpleasant. A patient described that this specific skill resulted in a more bearable experience of her situation.
Insight
Throughout the MBCT, many participants mentioned that they recognized and gained insight in their behavioral patterns. Moreover, several patients described that they better recognized their ADHD symptoms and their consequences, which resulted in an increased self-knowledge and a more realistic view of their impairments, without over- and underestimation. For some patients this led to the recognition of one’s own ability to influence certain aspects of their life. On the other hand, a few other patients mentioned that the gained insight in the impact of ADHD resulted in a sense of helplessness.
Changing perspective
These newly gained insights sometimes led to a change of perspective toward the inner experience and toward themselves. Several participants described that they developed the ability to observe their inner experience, such as thoughts and emotions, from “outside” (Shapiro, Carlson, Astin, & Freedman, 2006) instead of identifying with it. A change of self-image was also mentioned by some patients. For example, a patient revealed that he started to reflect on his values: “What do I like? What do I want?,” which was new for him.
Self-regulation
A substantial number of patients described that they were better able to regulate one’s own attention, thoughts, emotions, and actions to reach goals. Six distinctive self-regulation skills were identified.
Attention
Various participants told that their attentional control improved throughout the MBCT and that they were better able to maintain their focus on one task.
Impulsivity
An improvement of impulse control was often mentioned. Several patients learned to act less reactive toward internal and external stimuli. This sometimes resulted in a slower pace of acting and in more time for reflection.
Hyperactivity
For some participants, MBCT led to a decrease of hyperactivity. They experienced less inner restlessness, which expressed itself in a reduction of physical tension and a slower speed of the thought stream.
Working memory
A few times, patients mentioned that their forgetfulness decreased and that they tended to recall information or past events more easily. A patient revealed that he started to recall that he had already done a routine activity in an earlier stage, which prevented him from doing it again.
Emotion regulation
Several participants told that they were better able to modulate their emotional responses appropriately, which resulted in a reduction of irritability by unpleasant stimuli and a greater sense of emotional stability.
Goal-directed behavior
Many patients described an improvement of goal-directed and task-oriented behavior, which resulted in greater productivity and less chaos. Several patients mentioned that they were better able to oversee their tasks of the day and to prioritize. One patient told that he was better able to recognize the moments in which he unconsciously switched to another task than intended.
Changing behavior
Recognition and insight in one’s own behavioral patterns combined with a changed perspective and/or improved self-regulation skills sometimes led to the conscious choice to replace habitual behavior by more helpful behavior. Some participants started to take better care of themselves, for example, by setting proper limits or by asking others for help if necessary. A few participants mentioned that they felt a reduced willingness to restrain oneself. For example, one patient revealed that he always suppressed his hyperactivity, but started to experiment with allowing this active behavior in suitable situations.
Experiencing effects
Finally, many patients mentioned that they experienced effects on their well-being, their attitude toward themselves, and their relationship with others. Three subthemes were identified.
Well-being
Some patients explicitly described positive effects on their general well-being, like an increase in happiness and positivity, greater appreciation for life, and a reduction of sleep problems.
Self-compassion
Certain effects were related to a more self-compassionate attitude toward oneself. Several participants mentioned that they developed more self-kindness and self-acceptance when they encountered personal shortcomings or general suffering, instead of hurting themselves with self-criticism.
Connectedness
The changed behavior sometimes influenced the relationships with others. A few patients mentioned that they noticed that others responded differently to them. This could either result in an increased sense of connectedness with others or for one patient in a decreased sense of connectedness with her partner and incomprehension.
Triangulation
The gathered qualitative information about the feasibility and process of change was, in general, supported by the written evaluation forms. However, some additional topics emerged with regard to barriers of the schedule and the content of the training: too little time for formal practice in the training, the lack of variation in the exercises, and the lack of attention for the positive aspects of ADHD.
Discussion
Summary
This pilot study is the first mixed-method study exploring the feasibility, effectiveness, and process of change of adapted MBCT for ADHD. It was found that MBCT was feasible for most adults with ADHD, evidenced by a modest drop-out rate during MBCT of 16%, despite their inattention, hyperactivity, and/or impulsivity symptoms. Drop-out seemed to be related with an older age, higher levels of executive and general dysfunctioning, and a lower physical and mental health status. The qualitative part of our study gave insight in a broad variety of facilitators and barriers concerning environmental factors, the training itself, and characteristics of the participants. A process of change appeared to be initiated culminating in an improvement in self-regulation skills. This qualitative information was largely consistent with the quantitative results. Significant improvements were found of ADHD symptoms, executive functioning, self-compassion, and mental health. However, no improvements in mindfulness skills were found. A possible explanation might be that mindfulness skills need more time than 8 weeks to develop in ADHD patients. Therefore, future studies might include 3- and 6-month post-treatment measures to examine the long-term effects of MBCT on mindfulness skills and other important outcome measures.
Limitations
One of the limitations of the current study was the relatively high study drop-out of 23%, resulting in a relatively small sample size of patients completing both the pre- and post-treatment assessment. This limited the power of the analyses, heightening the chance of a type II error and making the estimated effect sizes less reliable. To reduce study drop-out in future research, increasing the number of exclusion criteria or shortening the length of the questionnaires is suggested. In addition, most of the drop-outs of the MBCT were not willing to fill-out the questionnaires after 3 months, which could have resulted in an overestimation of the treatment outcome. To reduce the drop-out during MBCT, exclusion of patients with the highest levels of executive and general dysfunctioning is recommended, for example by excluding patients with comorbid psychiatric disorders characterized by diminished executive functioning like the borderline personality disorder (Unoka & Richman, 2016), and autism spectrum disorder (Russo et al., 2007). An alternative recommendation is to develop a more adapted program that is also suitable for these patients.
Implications for Clinical Practice and Research
The qualitative analysis yielded meaningful insight in the facilitators and barriers of MBCT for ADHD. Importantly, patients found the majority of MBCT components acceptable and helpful in alleviating ADHD symptoms. Based on these results, we decided to make minor modifications in our MBCT program for adult ADHD (see Janssen et al., 2015 and Table 2). At first, in Sessions 3 and 4, walking meditation was included in the program, because many patients experienced the movement exercises as facilitating due to their physical restlessness. Second, the amount of homework exercises and assignments was reduced, as this was frequently considered as a barrier. Eventually, the teachers were instructed to emphasize the voluntary nature of the home exercises and assignments, for example, by using the term “guidelines for at home practice” instead of homework, accompanied by encouraging the participants to practice at home. This modification was based on the need for an appropriate amount of directiveness by the teacher.
At the beginning of our pilot study we had some doubts about whether or not certain components in the training would be feasible for adults with ADHD, such as the silent day and the substantial amount of formal practices in the training sessions. By carefully analyzing the gained information concerning the facilitators and barriers, we concluded that these components of the training were feasible for most of the patients in our study and that there were no well-founded reasons to adapt these components.
Conclusion
This pilot study showed that adapted MBCT, in which we stayed close to the regular MBCT program and merely made some minor modifications, is a feasible intervention for adults with ADHD. The richness of the qualitative data provided useful information to make well-founded decisions about whether to modify the program or adhere to the standard format of MBIs for mental health problems. The quantitative data showed preliminary evidence for the effectiveness of this intervention for adult ADHD. These results are mainly in line with previous studies (Cairncross & Miller, 2016; Hepark et al., 2015; Mitchell et al., 2015) and add to the increasing amount of empirical evidence for the effectiveness of other third-wave psychotherapies in clinical populations, such as acceptance and commitment therapy and dialectical behavior therapy (Hayes, 2004; Linehan et al., 2006). Based on this pilot study, a larger randomized controlled trial with follow-up assessments is currently being conducted (Janssen et al., 2015) to investigate the clinical and cost-effectiveness of MBCT for adults with ADHD.
Acknowledgments
We would like to thank Else Bisseling and Renée Metzemaekers for their willingness to cooperate in this pilot study as a mindfulness teacher. We also would like to thank the participants for their participation in this pilot study and for sharing their experiences.
Author Biographies
Lotte Janssen, MSc, is a psychologist, PhD student, and coordinator of the project “Aandacht voor ADHD” [Attention for ADHD], aimed at examining the (cost)effectiveness of MBCT versus treatment as usual in adults with ADHD at the Radboudumc Center for Mindfulness.
Alicia M. de Vries, MSc, is a psychologist and PhD student at the Department of Health Sciences of the University Medical Center Groningen.
Sevket Hepark, MD, is a psychiatrist at the outpatient clinic of the Radboud University Medical Center Nijmegen, specialized in care for adult patients with developmental disorders and personality disorders.
Anne E. M. Speckens, MD, PhD, is a professor of psychiatry at the Radboud University Medical Center Nijmegen. She is the founder and clinical director of the Radboudumc Center for Mindfulness. The center provides mindfulness courses for clinical populations with somatic and psychological conditions, health care professionals, and the general public.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Adler L. A., Faraone S. V., Spencer T. J., Michelson D., Reimherr F. W., Glatt S. J., . . . Biederman J. (2007). The reliability and validity of self- and investigator ratings of ADHD in adults. Journal of Attention Disorders, 11, 711-719. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual-text revision (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- Bachmann K., Lam A. P., Philipsen A. (2016). Mindfulness-Based Cognitive Therapy and the adult ADHD brain: A neuropsychotherapeutic perspective. Frontiers in Psychiatry, 7, Article 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer R. A., Smith G. T., Hopkins J., Krietemeyer J., Toney L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27-45. [DOI] [PubMed] [Google Scholar]
- Biederman J., Faraone S. V., Spencer T. J., Mick E., Monuteaux M. C., Aleardi M. (2006). Functional impairments in adults with self-reports of diagnosed ADHD: A controlled study of 1001 adults in the community. The Journal of Clinical Psychiatry, 67, 1478-1540. [DOI] [PubMed] [Google Scholar]
- Biederman J., Petty C. R., Clarke A., Lomedico A., Faraone S. V. (2011). Predictors of persistent ADHD: An 11-year follow-up study. Journal of Psychiatric Research, 45, 150-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohlmeijer E., Peter M., Fledderus M., Veehof M., Baer R. (2011). Psychometric properties of the Five Facet Mindfulness Questionnaire in depressed adults and development of a short form. Assessment, 8, 308-320. [DOI] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77-101. [Google Scholar]
- Cairncross M., Miller C. (2016). The effectiveness of mindfulness-based therapies for ADHD: A meta-analytic review. Journal of Attention Disorders, 1-17. Advance online publication. doi: 10.1177/1087054715625301 [DOI] [PubMed] [Google Scholar]
- Chiesa A., Calati R., Serretti A. (2011). Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clinical Psychology Review, 31, 449-464. [DOI] [PubMed] [Google Scholar]
- Chiesa A., Serretti A. (2011). Mindfulness based cognitive therapy for psychiatric disorders: A systematic review and meta-analysis. Psychiatry Research, 187, 441-453. [DOI] [PubMed] [Google Scholar]
- Conners C. K., Erhardt D., Sparrow E. P. (1999). Conners’ Adult ADHD Rating Scales (CAARS): Technical manual. North Tonawanda, NY: Multi-Health Systems Inc. (MHS) [Google Scholar]
- de Jong K., Nugter M. A., Polak M. G., Wagenborg J. E., Spinhoven P., Heiser W. J. (2007). The Outcome Questionnaire (OQ-45) in a Dutch population: A cross-cultural validation. Clinical Psychology & Psychotherapy, 14, 288-301. [Google Scholar]
- Edel M.-A., Hölter T., Wassink K., Juckel G. (2014). A comparison of mindfulness-based group training and skills group training in adults with ADHD: An open study. Journal of Attention Disorders, 21, 533-539. [DOI] [PubMed] [Google Scholar]
- Fox K. C., Nijeboer S., Dixon M. L., Floman J. L., Ellamil M., Rumak S. P., . . . Christoff K. (2014). Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neuroscience & Biobehavioral Reviews, 43, 48-73. [DOI] [PubMed] [Google Scholar]
- Gajria K., Lu M., Sikirica V., Greven P., Zhong Y., Qin P., . . . Xie J. (2014). Adherence, persistence, and medication discontinuation in patients with attention-deficit/hyperactivity disorder: A systematic literature review. Neuropsychiatric Disease and Treatment, 10, 1543-1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjervan B., Torgersen T., Nordahl H. M., Rasmussen K. (2012). Functional impairment and occupational outcome in adults with ADHD. Journal of Attention Disorders, 16, 544-552. doi: 10.1177/1087054711413074 [DOI] [PubMed] [Google Scholar]
- Hayes S. C. (2004). Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy, 35, 639-665. doi: 10.1016/S0005789404800133 [DOI] [PubMed] [Google Scholar]
- Hepark S., Janssen L., de Vries A., Schoenberg P. L., Donders R., Kan C. C., Speckens A. E. (2015). The efficacy of adapted MBCT on core symptoms and executive functioning in adults with ADHD: A preliminary randomized controlled trial. Journal of Attention Disorders, 1-12. Advance online publication. doi: 10.1177/1087054715613587 [DOI] [PubMed] [Google Scholar]
- Janssen L., Kan C. C., Carpentier P. J., Sizoo B., Hepark S., Grutters J., . . . Speckens A. E. (2015). Mindfulness based cognitive therapy versus treatment as usual in adults with attention deficit hyperactivity disorder (ADHD). BMC Psychiatry, 15(1), Article 216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York, NY: Delta. [Google Scholar]
- Khoury B., Lecomte T., Fortin G., Masse M., Therien P., Bouchard V., . . . Hofmann S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33, 763-771. doi: 10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
- Lambert M. J., Burlingame G. M., Umphress V., Hansen N. B., Vermeersch D. A., Clouse G. C., Yanchar S. C. (1996). The reliability and validity of the Outcome Questionnaire. Clinical Psychology & Psychotherapy, 3, 249-258. [Google Scholar]
- Lim L.-Y., Fisher J. (1999). Use of the 12-item short-form (SF-12) Health Survey in an Australian heart and stroke population. Quality of Life Research, 8, 1-8. [DOI] [PubMed] [Google Scholar]
- Linehan M. M., Comtois K. A., Murray A. M., Brown M. Z., Gallop R. J., Heard H. L., . . . Lindenboim M. S. (2006). Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of General Psychiatry, 63, 757-766. doi: 10.1001/archpsyc.63.7.757 [DOI] [PubMed] [Google Scholar]
- Malinowski P. (2013). Neural mechanisms of attentional control in mindfulness meditation. Frontiers in Neuroscience, 7, Article 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson L., Asherson P., Wong I. C. K., Hodgkins P., Setyawan J., Sasane R., Clifford S. (2013). Adult ADHD patient experiences of impairment, service provision and clinical management in England: A qualitative study. BMC Health Services Research, 13(1), Article 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHorney C. A., Ware J. E., Jr., Raczek A. E. (1993). The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care, 31, 247-263. [DOI] [PubMed] [Google Scholar]
- Mészáros Á., Czobor P., Bálint S., Komlósi S., Simon V., Bitter I. (2009). Pharmacotherapy of adult attention deficit hyperactivity disorder (ADHD): A meta-analysis. The International Journal of Neuropsychopharmacology, 12(8), 1137-1147. [DOI] [PubMed] [Google Scholar]
- Mitchell J. T., Zylowska L., Kollins S. H. (2015). Mindfulness meditation training for attention-deficit/hyperactivity disorder in adulthood: Current empirical support, treatment overview, and future directions. Cognitive and Behavioral Practice, 22, 172-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. (2009). Attention deficit hyperactivity disorder: The NICE guideline on diagnosis and management of ADHD in children, young people and adults. London, England: The British Psychological Society and the Royal College of Psychiatrists. [PubMed] [Google Scholar]
- Neff K. D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2, 223-250. [Google Scholar]
- O’Cathain A., Murphy E., Nicholl J. (2008). The quality of mixed methods studies in health services research. Journal of Health Services Research & Policy, 13(2), 92-98. [DOI] [PubMed] [Google Scholar]
- Pope C., Mays M. (1999). Qualitative research in health care (2nd ed.). London, England: BMJ Publishing. [Google Scholar]
- Raes F., Pommier E., Neff K. D., Van Gucht D. (2011). Construction and factorial validation of a short form of the Self-Compassion Scale. Clinical Psychology & Psychotherapy, 18, 250-255. [DOI] [PubMed] [Google Scholar]
- Roth R. M., Gioia G. A. (2005). Behavior Rating Inventory of Executive Function—Adult version (BRIEF-A). Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Russo N., Flanagan T., Iarocci G., Berringer D., Zelazo P. D., Burack J. A. (2007). Deconstructing executive deficits among persons with autism: Implications for cognitive neuroscience. Brain and Cognition, 65, 77-86. doi: 10.1016/j.bandc.2006.04.007 [DOI] [PubMed] [Google Scholar]
- Scholte E., Noens I. (2011). BRIEF-A: Vragenlijst over executief functioneren bij volwassenen [BRIEF-A: Inventory of executive function in adults]. Amsterdam, The Netherlands: Hogrefe. [Google Scholar]
- Segal Z. V., Williams J. M. G., Teasdale J. D. (2012). Mindfulness-based cognitive therapy for depression. New York, NY: The Guilford Press. [Google Scholar]
- Shapiro S. L., Carlson L. E., Astin J. A., Freedman B. (2006). Mechanisms of mindfulness. Journal of Clinical Psychology, 62, 373-386. [DOI] [PubMed] [Google Scholar]
- Simon V., Czobor P., Balint S., Meszaros A., Bitter I. (2009). Prevalence and correlates of adult attention-deficit hyperactivity disorder: Meta-analysis. British Journal of Psychiatry, 194, 204-211. doi: 10.1192/bjp.bp.107.048827 [DOI] [PubMed] [Google Scholar]
- Strauss C., Cavanagh K., Oliver A., Pettman D. (2014). Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: A meta-analysis of randomised controlled trials. PLoS ONE, 9(4), Article 13. doi: 10.1371/journal.pone.0096110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y.-Y., Holzel B. K., Posner M. I. (2015). The neuroscience of mindfulness meditation. Nature Reviews Neuroscience, 16, 213-225. doi: 10.1038/nrn3916 [DOI] [PubMed] [Google Scholar]
- Unoka Z. J., Richman M. (2016). Neuropsychological deficits in BPD patients and the moderator effects of co-occurring mental disorders: A meta-analysis. Clinical Psychology Review, 44, 1-12. doi: 10.1016/j.cpr.2015.11.009 [DOI] [PubMed] [Google Scholar]
- Van Vliet I., De Beurs E. (2007). Het Mini Internationaal Neuropsychiatrisch Interview (MINI). Een kort gestructureerd diagnostisch psychiatrisch interview voor DSM-IV en ICD-10 stoornissen [The Mini International Neuropsychiatric Interview (MINI). A short structured diagnostic psychiatric interview for DSM-IV and ICD-10 disorders]. Tijdschrift Voor Psychiatrie, 49, 393-397. [PubMed] [Google Scholar]
- Ware J. E., Jr., Kosinski M., Keller S. D. (1996). A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220-233. [DOI] [PubMed] [Google Scholar]
- Warren F., Kuyken W., Taylor R., Whalley B., Crane C., Bondolfi G., . . . Schwelzer S. (2016). Efficacy and moderators of mindfulness-based cognitive therapy (MBCT) in prevention of depressive relapse: An individual patient data meta-analysis from randomized trials. JAMA Psychiatry,73(6), 565-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wigal T., Brams M., Gasior M., Gao J., Squires L., Giblin J. (2010). Randomized, double-blind, placebo-controlled, crossover study of the efficacy and safety of lisdexamfetamine dimesylate in adults with attention-deficit/hyperactivity disorder: Novel findings using a simulated adult workplace environment design. Behavioral and Brain Functions, 6(1), Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S. Y. S., Yip B. H. K., Mak W. W. S., Mercer S., Cheung E. Y. L., Ling C. Y. M., . . . Wu J. C. Y. (2016). Mindfulness-based cognitive therapy v. group psychoeducation for people with generalised anxiety disorder: Randomised controlled trial. The British Journal of Psychiatry, 209, 68-75. [DOI] [PubMed] [Google Scholar]
- Zylowska L., Ackerman D. L., Yang M. H., Futrell J. L., Horton N. L., Hale T. S., . . . Smalley S. L. (2008). Mindfulness meditation training in adults and adolescents with ADHD a feasibility study. Journal of Attention Disorders, 11, 737-746. [DOI] [PubMed] [Google Scholar]