Abstract
Background:
Population-based planning tools are important for informing diabetes-prevention efforts in First Nations communities. We used the Diabetes Population Risk Tool (DPoRT) to predict 10-year diabetes risk and describe the factors that contribute to diabetes risk in First Nations adults living in Ontario First Nations communities.
Methods:
We examined population data from adult (≥ 20 yr) respondents to the First Nations Regional Health Survey (RHS) phase 3, a representative cohort of First Nations people living in Ontario First Nations communities. We applied the DPoRT to risk factor information in the survey to predict the distribution of 10-year type 2 diabetes incidence and number of new diabetes cases from 2015/16 to 2025/26.
Results:
There were 993 respondents to the RHS phase 3 adult survey, of whom 936 (708 without diabetes and 228 with a diagnosis of type 2 diabetes) were eligible for inclusion. The DPoRT predicted a type 2 diabetes risk of 9.6% (confidence interval [CI] 8.3–10.8) between 2015/16 and 2025/26, corresponding to 3501 (95% CI 2653–4348) new diabetes cases. Diabetes cases were predicted to occur disproportionately among those experiencing food insecurity, low income, overweight, obesity and physical inactivity. Reduced diabetes risk was predicted among those who reported connections to Indigenous culture, as measured by eating traditional vegetative foods a few times or often in the previous 12 months.
Interpretation:
Socioeconomic conditions and known risk factors for type 2 diabetes are important determinants of diabetes risk in First Nations communities. Culturally appropriate policies, programming and services that address socioeconomic disadvantage and other diabetes risk factors in First Nations communities likely have an important role for diabetes prevention in First Nations adults.
First Nations people experience a disproportionate risk of diabetes compared to other populations in Canada. 1,2 In addition to genetic susceptibility, socioeconomic determinants and risk behaviours that are common diabetes risk factors in all populations,3 First Nations people have unique experiences that contribute to diabetes risk, including intergenerational effects of colonization, loss of culture and language, epigenetic mechanisms, and disproportionate experiences of low income, food insecurity and risky behaviours compared to other populations in Canada. 4–7 First Nations people also experience important protective effects against diabetes that are tied with connections to Indigenous traditions and cultural continuity.8
There is considerable diversity between and within Indigenous groups relative to risk factors and health experiences. 7 Understanding how the risk factors for type 2 diabetes are distributed in First Nations people living in First Nations communities and how these factors contribute to diabetes risk is critical for informing diabetes-prevention strategies that are culturally appropriate and address the health gaps, needs and challenges that are unique to First Nations communities.9
The objective of this study was to apply a validated population-based risk-prediction tool for diabetes to data relevant for First Nations communities to estimate the number of new diabetes cases over 10 years and examine the social determinants and other factors that are driving diabetes risk in the First Nations population living in First Nations communities in Ontario.
Methods
Setting
This study was conducted in Ontario in partnership with the Chiefs of Ontario. It focused on the First Nations population living in First Nations communities. There are 133 First Nations communities in Ontario, the majority of which are located in northern Ontario.
Data source and study population
We used data from phase 3 (2015/16) of the adult Regional Health Survey (RHS), a cross-sectional survey of First Nations people living on reserve and northern First Nations communities across Canada.10,11 It is the only source of national health-related data for First Nations communities that is fully under First Nations ownership and control. Data are available for phase 1 (2002–2003), phase 2 (2008–2010) and phase 3 (2015–2017); data collection for phase 4 is planned for 2020. At the national level, the First Nations Information Governance Centre coordinates the development and implementation of the RHS. The centre and its regional partners (in Ontario, the Chiefs of Ontario), which serve as data stewards, govern access to the RHS in ways that respect First Nations principles of ownership, control, access and possession.12
Guided by a cultural framework that conceptualizes health from First Nations perspectives, the RHS collects information based on Western and traditional understandings of health and well-being.13 The adult survey included questions about diabetes, demographic characteristics, health and chronic conditions, food security, other social determinants, and First Nations language and culture.
The RHS phase 3 sampling design used complex sampling that incorporated a 2-stage sampling strategy. The first stage involved the selection of communities to participate in the survey. First Nations communities were stratified by region, subregion and community size (small [< 300 people], medium [300–1500 people] and large [> 1500 people]). Large communities were automatically included in the sample; medium-sized and small communities were selected randomly with equal probability within their respective strata.
The second stage pertained to the selection of people within each community sampled. Community members were identified through band membership lists. Data were gathered to represent 10 categories of the community population (5 age groups by gender). The sampling rate within each community was determined as a function of the overall subregion probability (within regions) and the probability of community selection (within a subregion). In total, 5.5% of the target population was sampled, and the response rate was 76.1%.11,14
The study sample was drawn from the respondents to the RHS phase 3 adult survey administered in Ontario. We applied population exclusions that were required to estimate diabetes risk validly with the Diabetes Population Risk Tool (DPoRT).15,16 We selected the DPoRT in collaboration with the Chiefs of Ontario after considering its relevance for use with self-reported risk factor information in the RHS and its ability to generate population-level risk estimates, and after testing its model performance (methodologic details and the algorithm are described elsewhere15–17 and in Appendix 1, available at www.cmajopen.ca/content/8/1/E178/suppl/DC1). Specifically, we excluded people who were less than 20 years old at the interview date, those who reported being diagnosed with type 1 or gestational diabetes, and women who reported being pregnant at interview.
Estimating type 2 diabetes risk
We applied the DPoRT to information on risk factors for type 2 diabetes from the RHS to estimate 10-year type 2 diabetes incidence and future diabetes cases in the First Nations population living in First Nation communities.
Diabetes risk factors
We examined the distribution of type 2 diabetes risk across important risk factor variables that are known to contribute to diabetes risk.9 Demographic and socioeconomic risk factors included sex, age group (20–44 yr, 45–64 yr, ≥ 65 yr), household food security (food secure, moderately/severely food insecure) and household income category (annual income ≤ $24 999, $25 000–$49 999, $50 000–$69 999, $70 000–$99 999, ≥ $100 000). In the DPoRT algorithm, income is included as a binary variable (highest income [quintile 5] v. lowest income [quintiles 1–4]). For the purposes of estimating diabetes risk with the DPoRT, we assigned people who reported having a household income of $70 000 or more to the highest income quintile, which corresponds to the income distribution for the Ontario general population.18
Risk factors related to health included consumption of traditional vegetation (e.g., berries, wild vegetation and wild rice) in the previous 12 months (not at all, a few times/often), knowledge of a First Nations language, even if only a few words (yes, no), self-reported diagnosis of hypertension, smoking status (current smoker, former smoker, never smoked), body mass index and physical activity. Body mass index was classified according to the international standard: normal weight (18.5–24.9), overweight (25.0–29.9) and obese (≥ 30).19 Physical activity level was measured by means of the physical activity index in the RHS, which calculates total energy expenditure by multiplying the number of times the person engaged in each activity in the previous 3 months, the average duration of participation in minutes and the metabolic equivalent value assigned to each activity.20 Respondents were categorized as being inactive (0–1.4 kcal/kg per day), moderately inactive (1.5–2.9 kcal/kg per day) or active (≥ 3.0 kcal/kg per day).
Statistical analysis
We calculated means to describe the distribution of risk factors for type 2 diabetes in the First Nations population by type 2 diabetes status. We restricted DPoRT diabetes risk estimates to respondents who did not report having type 2 diabetes at baseline and who had valid risk factor information required for the DPoRT algorithm (n = 670). Respondents who had missing values on income were assigned to the lowest income quintile groups (quintiles 1–4), which corresponded to the most frequently reported income groups for this population.
We averaged diabetes risk estimates across all respondents to determine the 10-year population risk of diabetes between 2015/16 and 2025/26. We reported DPoRT risk estimates by important subgroups defined by diabetes risk factors. We estimated the number of new cases of type 2 diabetes by multiplying the average risk by the population size. We weighted individual responses using sampling weights provided by the First Nations Information Governance Centre, based on 2014 registry counts from Indigenous and Northern Affairs Canada, to accurately represent the population. We calculated estimates and 95% confidence intervals (CIs) using the SPSS Complex Samples Module (IBM Corp.), which produced estimates based on the weights and specifications of the RHS’s complex sampling design. All analyses were conducted at the Chiefs of Ontario office in Toronto with SPSS Version 23.
Ethics approval
Access to RHS data for this study was approved by the data governance process at the Chiefs of Ontario.
Results
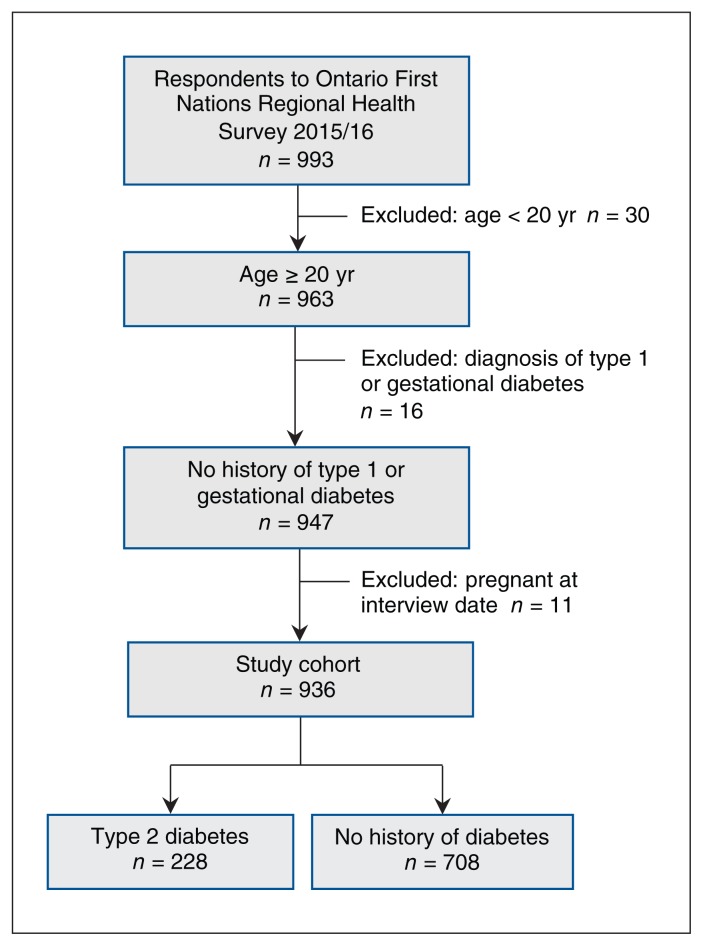
There were 993 respondents to the RHS phase 3 adult survey administered in Ontario. After exclusions, the data for 936 respondents were retained for analysis, of whom 708 reported no diabetes and 228 reported having a diagnosis of type 2 diabetes at the interview date (Figure 1).
Figure 1:
Flow diagram showing participant selection.
The weighted distribution of baseline characteristics of the cohort is summarized in Table 1. At interview, First Nations adults with diabetes were older, more likely to be classified with obesity and more likely to report hypertension compared to First Nations adults without diabetes. Overall, First Nations adults were observed to experience a high prevalence of low household income and food insecurity. The most prevalent risk factors among both those with and without diabetes were physical inactivity, overweight, obesity and current smoking. The majority of First Nations adults reported consuming different types of traditional vegetation in the year before the survey and had knowledge of a First Nations language.
Table 1:
Weighted distribution of baseline characteristics of adult First Nations respondents to the Regional Health Survey10,11 with and without diabetes in Ontario, 2015/16, and estimated 10-year (2015/16–2025/26) risk of type 2 diabetes and new diabetes cases expected
| Characteristic | % of people (95% CI) | 10-yr type 2 diabetes risk (95% CI) | ||
|---|---|---|---|---|
|
|
|
|||
| Type 2 diabetes n = 228 Weighted = 11 209* |
No history of diabetes n = 708 Weighted = 39 494* |
10-yr diabetes risk, %† | No. of new diabetes cases‡ | |
| Overall | – | – | 9.6 (8.3–10.8) | 3501 (2653–4348) |
|
| ||||
| Sex | ||||
|
| ||||
| Male | 44.7 (41.1–48.4) | 51.5 (48.7–54.3) | 11.3 (9.3–13.4) | 2013 (1507–2518) |
|
| ||||
| Female | 55.3 (51.6–58.9) | 48.5 (45.7–51.3) | 7.9 (7.1–8.8) | 1488 (1106–1870) |
|
| ||||
| Age at interview, yr | ||||
|
| ||||
| 20–44 | 25.9 (16.3–38.6) | 61.4 (54.5–67.9) | 5.6 (4.6–6.6) | 1237 (893–1582) |
|
| ||||
| 45–64 | 44.9 (34.7–55.7) | 28.5 (22.8–35.0) | 15.8 (14.0–17.6) | 1658 (1176–2141) |
|
| ||||
| ≥ 65 | 29.2 (24.1–34.8) | 10.0 (7.7–13.1) | 15.7 (13.7–17.8) | 605 (372–839) |
|
| ||||
| Household income | ||||
|
| ||||
| ≤ 24 999 | 26.9 (20.4–34.6) | 22.2 (18.1–26.9) | 10.3 (8.4–12.3) | 863 (597–1129) |
|
| ||||
| 25 000–49 999 | 19.1 (13.1–26.9) | 22.9 (17.5–29.4) | 10.4 (8.7–12.1) | 836 (607–1167) |
|
| ||||
| 50 000–69 999 | 12.2 (8.5–17.3) | 4.1 (2.6–6.4) | 12.6 (9.7–15.5) | 204 (89–319) |
|
| ||||
| 70 000–99 999 | 6.6 (4.7–9.0) | 5.1 (3.4–7.5) | 8.9 (5.9–11.7) | 177 (94–261) |
|
| ||||
| ≥ 100 000 | 7.7 (4.1–14.0) | 3.1 (1.4–6.7) | 8.0 (5.4–10.5) | 93 (15–171) |
|
| ||||
| Missing | 27.5 (21.8–34.1) | 42.6 (34.3–51.3) | 8.7 (6.4–10.9) | 1326 (799–1854) |
|
| ||||
| Food security | ||||
|
| ||||
| Food secure | 57.3 (50.2–64.1) | 52.0 (47.0–56.9) | 9.5 (8.0–11.1) | 1869 (1336–2402) |
|
| ||||
| Food insecure | 41.3 (34.5–48.4) | 44.8 (39.9–49.8) | 9.6 (8.2–11.1) | 1595 (1213–1976) |
|
| ||||
| Body mass index | ||||
|
| ||||
| Normal weight | 8.4 (4.7–14.5) | 23.0 (16.0–31.9) | 2.7 (2.0–3.5) | 244 (182–308) |
|
| ||||
| Overweight | 33.8 (27.7–40.3) | 36.0 (31.4–40.9) | 7.4 (6.4–8.4) | 929 (734–1125) |
|
| ||||
| Obese | 53.0 (46.0–59.8) | 38.8 (31.6–46.5) | 15.8 (14.8–16.9) | 2270 (1527–3013) |
|
| ||||
| Physical activity level | ||||
|
| ||||
| Active | 22.9 (17.6–29.1) | 29.0 (23.9–34.5) | 7.5 (5.7–9.2) | 845 (536–2339) |
|
| ||||
| Moderately active | 12.6 (7.8–19.5) | 13.9 (10.6–18.0) | 10.6 (7.4–13.8) | 565 (300–830) |
|
| ||||
| Inactive | 58.4 (51.6–64.8) | 50.5 (45.3–55.5) | 10.6 (9.3–11.9) | 1960 (1581–2339) |
|
| ||||
| Smoking status | ||||
|
| ||||
| Never smoked | 21.1 (15.5–28.0) | 24.9 (18.1–33.0) | 10.5 (9.3–11.8) | 1024 (595–1451) |
|
| ||||
| Former smoker | 35.8 (28.6–43.7) | 21.3 (16.8–26.6) | 11.2 (9.8–12.7) | 907 (663–1151) |
|
| ||||
| Current smoker | 41.5 (32.6–50.9) | 51.1 (42.6–59.5) | 8.4 (6.5–10.4) | 1569 (1177–1961) |
|
| ||||
| Hypertension | ||||
|
| ||||
| Yes | 53.6 (43.7–63.3) | 14.0 (11.6–16.9) | 21.1 (18.8–23.4) | 1118 (792–1445) |
|
| ||||
| No | 45.4 (35.7–55.3) | 83.2 (80.3–85.6) | 7.6 (6.3–8.9) | 2382 (1754–3010) |
|
| ||||
| Consumption of traditional vegetation in previous 12 mo | ||||
|
| ||||
| A few times/often | 90.8 (84.8–94.5) | 84.0 (77.5–88.6) | 9.5 (8.1–10.9) | 3007 (2230–3783) |
|
| ||||
| Not at all | 12.6 (8.0–19.0) | 7.3 (4.1–12.7) | 10.4 (7.8–12.9) | 367 (251–668) |
|
| ||||
| Knowledge of a First Nations language | ||||
|
| ||||
| Yes | 89.8 (84.9–93.2) | 92.1 (88.8–94.5) | 9.8 (8.7–10.9) | 3093 (2308–3877) |
|
| ||||
| No | 10.2 (6.8–15.1) | 7.9 (5.5–11.2) | 10.1 (7.7–12.5) | 369 (183–555) |
Note: CI = confidence interval.
Represented population estimated with the use of Regional Health Survey10,11 sampling weights. Column percentages do not total 100% where missing values are not reported.
Estimated among respondents who reported not having a diabetes diagnosis at baseline.
Column totals do not add to 3501 owing to rounding. Also, we do not report those with missing information on food security, body mass index, physical activity, consumption of traditional foods or knowledge of a First Nations language.
Using DPoRT, we estimated that the 10-year incidence of type 2 diabetes among First Nations adults living in First Nations communities was 9.6% (95% CI 8.3–10.8), corresponding to 3501 new type 2 diabetes cases between 2015/16 and 2025/26. Given that diabetes incidence is influenced by the level of risk associated with the factors that contribute to diabetes and the prevalence of those risk factors within the population, Table 1 presents results for both 10-year diabetes risk and number of new cases by important subgroups. About one-third (1237) of new diabetes cases were predicted to occur in First Nations adults aged 20–44, and about half (1658) were predicted among those aged 45–64.
Socioeconomic factors were major contributors to diabetes risk in these communities. The 2 lowest income groups (≤ $24 999 and $25 000–$49 999) were predicted to account for almost half (1699) of new diabetes cases. Furthermore, almost half (1595) of new cases were predicted to occur among First Nations adults who reported experiencing food insecurity.
Other risk factors were observed to contribute to the predicted type 2 diabetes cases. The 10-year risk for diabetes was predicted to be 15.8% (95% CI 14.8–16.9) among those with obesity and 10.6% (95% CI 9.3–11.9) among those that were physically inactive, compared to 2.7% (95% CI 2.0–3.5) among those with normal weight and 7.5% (95% CI 5.7–9.2) among physically active people. Diabetes risk was found to be lower among those who reported eating traditional vegetation a few times or often in the previous year than among those who reported not eating it at all (9.5% [95% CI 8.1–10.9] v. 10.4% [95% CI 7.8–12.9]).
Of the new diabetes cases, about two-thirds (2270) were predicted to occur among those with obesity, about half (1960) among physically inactive people and about one-fifth among those who were overweight (929). Although diabetes risk was elevated among those with hypertension (21.1%, 95% CI 18.8–23.4), more new diabetes cases were predicted to occur among adults with no hypertension than among those with hypertension (2382 v. 1118 cases), which reflects the distribution of hypertension in the community.
Interpretation
We have shown that key socioeconomic and additional risk factors that contribute to type 2 diabetes are prevalent in First Nations adults living in First Nations communities in Ontario. Furthermore, using a validated tool to estimate diabetes risk, we predicted that, between 2015/16 and 2025/26, the type 2 diabetes risk will be 9.6% in this population, which aligns with the annual diabetes incidence of 0.80% observed in 2014 for First Nations people in Ontario.17 A large proportion of new cases were predicted to occur among younger people, in agreement with previous research showing a younger age at onset of diabetes for First Nations people.21
We estimated that many new diabetes cases will occur among First Nations adults experiencing socioeconomic disadvantage, as well as among those with well-established diabetes risk factors including overweight, obesity and physical inactivity. It is widely recognized that the process of colonization has affected the health and well-being of Indigenous people through dislocation from traditional lands and lifestyles, cultural suppression and forced assimilation, among other effects.22,23
Remote northern First Nations communities in particular experience unique challenges in accessing healthy and inexpensive foods,10,24 and changes from traditional lifestyles and diets have contributed to the high prevalence of obesity and physical inactivity among First Nations people.22,25 Our study also showed lower diabetes risk among adults who reported eating traditional vegetative foods in the previous 12 months than among those who reported not eating such foods, which suggests a role for cultural continuity in diabetes-prevention efforts for First Nations people.
Our study has shown the application of a population risk prediction tool in understanding the distribution of diabetes risk in First Nations on-reserve communities. Future applications of the DPoRT can involve modelling scenarios that integrate information on baseline trends in diabetes risk and risk factors to inform culturally relevant diabetes-prevention strategies in First Nations communities.
Limitations
The findings of this study should be interpreted in context with several considerations. It is important to recognize that the DPoRT algorithm was originally developed and validated in a cohort of people from the Ontario general population, which included First Nations people living off reserve.15 Although the DPoRT was determined to have appropriate predictive accuracy for the First Nations population in that most First Nations people with self-reported diabetes were correctly classified as being at high risk, a small proportion were shown to be misclassified as being at low risk. Furthermore, the DPoRT was validated against physician-diagnosed diabetes as captured in the Ontario Diabetes Database, which does not capture people with diabetes not recognized by themselves or their doctor. In addition, an inherent limitation of ascertaining chronic diseases through self-reported data is the potential for reporting biases. A previous study that examined agreement between survey and administrative data showed that the weighted prevalence with self-reported data was lower than the prevalence with administrative data; however, a good level of agreement was found for diabetes and hypertension.26 Given these considerations, it is possible that the DPoRT estimates may underestimate the true diabetes risk and new cases in First Nations people.
Our study included only proxy measures of Indigenous culture, namely, traditional foods and language, which do not capture all aspects of First Nations culture and traditional activities.
Finally, with the use of self-reported data, there is the potential for reporting biases, such as recall, social desirability and overreporting of healthier behaviours.
Conclusion
We found that low income and food insecurity, along with overweight, obesity and physical inactivity, were associated with a large proportion of the predicted diabetes cases in First Nations people living in First Nations communities in Ontario. We also found important protective effects of Indigenous cultural connections on diabetes risk in this population. Our findings underscore that policies, programming and services that address socioeconomic disadvantage and known risk factors for type 2 diabetes, as well as incorporate traditional and cultural approaches, may have tangible impacts on preventing type 2 diabetes in First Nations people.
Supplementary Material
Acknowledgements
The authors’ partner through the early design, implementation and final dissemination of this project was the Chiefs of Ontario. Their many contributions were key to the content and quality of the project. The authors acknowledge the members of the project Patient Advisory Committee for providing insightful and thoughtful input; their advice made a substantial contribution in shaping the work. The authors also acknowledge the First Nations people from Big Grassy River First Nation, Alderville First Nation, Caldwell First Nation, Six Nations of the Grand River and Moose Cree First Nation with diabetes who shared their personal experiences. Finally, the authors thank Graham Mecredy for his contributions in running and vetting the statistical program applied to the Regional Health Survey data.
See related research article at www.cmajopen.ca/lookup/doi/10.9778/cmajo.20190096
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
Contributors: Laura Rosella and Carmen Jones conceived the study. Laura Rosella, Kathy Kornas and Carmen Jones analyzed and interpreted the data. All of the authors contributed to the study design and drafting of the manuscript, revised the manuscript critically for important intellectual content, approved the final version to be published and agreed to be accountable for all aspects of the work.
Funding: This study received funding from an IMPACT Award from the Ontario SPOR SUPPORT Unit, the Brian Hennen Chair held by Michael Green and Operating Grant FRN-142498 from the Canadian Institutes of Health Research. Laura Rosella is supported by a Canada Research Chair in Population Health Analytics (950-230702).
Disclaimer: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/8/1/E178/suppl/DC1.
References
- 1.Diabetes Canada Clinical Practice Guidelines Expert Committee. Crowshoe L, Dannenbaum D, Green M, et al. Type 2 diabetes and Indigenous peoples. Can J Diabetes. 2018;42(Suppl 1):S296–306. doi: 10.1016/j.jcjd.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 2.Dyck R, Osgood N, Lin TH, et al. Epidemiology of diabetes mellitus among First Nations and non-First Nations adults. CMAJ. 2010;182:249–56. doi: 10.1503/cmaj.090846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellou V, Belbasis L, Tzoulaki I, et al. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One. 2018;13:e0194127. doi: 10.1371/journal.pone.0194127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Setting the context: an overview of Aboriginal health in Canada. Prince George (BC): National Collaborating Centre For Aboriginal Health; 2013. [Google Scholar]
- 5.Mazereeuw MV, Yurkiewich A, Jamal SJ, et al. Cancer risk factors and screening in First Nations in Ontario. Health Promot Chronic Dis Prev Can. 2017;37:186–93. doi: 10.24095/hpcdp.37.6.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner NJ, Turner KL. Traditional food systems, erosion and renewal in northwestern North America. Indian J Tradit Knowl. 2007;6:57–68. [Google Scholar]
- 7.Diabetes in Canada: facts and figures from a public health perspective. Ottawa: Public Health Agency of Canada; 2011. Diabetes among First Nations, Inuit, and Métis populations; pp. 89–105. [Google Scholar]
- 8.Oster RT, Grier A, Lightning R, et al. Cultural continuity, traditional Indigenous language, and diabetes in Alberta First Nations: a mixed methods study. Int J Equity Health. 2014;13:92. doi: 10.1186/s12939-014-0092-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young TK, Reading J, Elias B. Type 2 diabetes mellitus in Canada’s First Nations: status of an epidemic in progress [published erratum in CMAJ 2000;163:1132] CMAJ. 2000;163:561–6. [PMC free article] [PubMed] [Google Scholar]
- 10.National Report of the First Nations Regional Health Survey Phase 3: Volume Two. Ottawa: First Nations Information Governance Centre; 2018. [Google Scholar]
- 11.National Report of the First Nations Regional Health Survey Phase 3: Volume One. Ottawa: First Nations Information Governance Centre; 2018. [Google Scholar]
- 12.First Nations Regional Health Survey (RHS): best practice tools for OCAP compliant research. Ottawa: First Nations Information Governance Centre; 2011. [accessed 2020 Mar. 3]. Available: https://fnigc.ca/sites/default/files/RHSBestPracticeBooklet.pdf. [Google Scholar]
- 13.Dumont J. First Nations Regional Longitudinal Health Survey (RHS) cultural framework. Ottawa: First Nations Information Governance Centre; 2005. [Google Scholar]
- 14.First Nations Regional Health Survey Phase 3 (RHS): supporting community engagement to advance the well-being of First Nations. Ottawa: First Nations Information Governance Centre; 2012. [Google Scholar]
- 15.Rosella LC, Manuel DG, Burchill C, et al. PHIAT-DM team. A population-based risk algorithm for the development of diabetes: development and validation of the Diabetes Population Risk Tool (DPoRT) J Epidemiol Community Health. 2011;65:613–20. doi: 10.1136/jech.2009.102244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosella LC, Lebenbaum M, Li Y, et al. Risk distribution and its influence on the population targets for diabetes prevention. Prev Med. 2014;58:17–21. doi: 10.1016/j.ypmed.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Green ME, Jones CR, Walker JD, et al. First Nations and diabetes in Ontario. Toronto: ICES; 2019. [Google Scholar]
- 18.Statistics Canada. Tax filers and dependents with income by total income, sex and age. [accessed 2020 Mar. 5]. Table 11-10-0008-01. Available: www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1110000801.
- 19.Obesity: preventing and managing the global epidemic — report of a WHO Consultation. Geneva: World Health Organization; 2000. (WHO Technical Report series 894). [PubMed] [Google Scholar]
- 20.RHS Phase 3 data dictionary adult survey. Ottawa: First Nations Information Governance Centre; 2018. [Google Scholar]
- 21.Turin TC, Saad N, Jun M, et al. Lifetime risk of diabetes among First Nations and non-First Nations people. CMAJ. 2016;188:1147–53. doi: 10.1503/cmaj.150787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haman F, Fontaine-Bisson B, Batal M, et al. Obesity and type 2 diabetes in northern Canada’s remote First Nations communities: the dietary dilemma. Int J Obes (Lond) 2010;34(Suppl 2):S24–31. doi: 10.1038/ijo.2010.236. [DOI] [PubMed] [Google Scholar]
- 23.Wilk P, Maltby A, Cooke M. Residential schools and the effects on Indigenous health and well-being in Canada — a scoping review. Public Health Rev. 2017;38:8. doi: 10.1186/s40985-017-0055-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson D, Macdonald D. The income gap between Aboriginal peoples and the rest of Canada. Ottawa: Canadian Centre for Policy Alternatives; 2010. [Google Scholar]
- 25.Socha T, Zahaf M, Chambers L, et al. Food security in a northern First Nations community: an exploratory study on food availability and accessibility. J Aborig Health. 2012;8:5–14. [Google Scholar]
- 26.Muggah E, Garve E, Bennett C, et al. Ascertainment of chronic diseases using population health data: a comparison of health administrative data and patient self-report. BMC Public Health. 2013;13:16. doi: 10.1186/1471-2458-13-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.