Abstract
Objective Computer-aided design and manufacturing (CAD/CAM) implants are fabricated based on volumetric analysis of computed tomography (CT) scans and are routinely used for the reconstruction of orbital fractures. We present three cases of patients with sphenoorbital meningiomas that underwent tumor resection, orbital decompression, and orbital reconstruction with patient specific porous titanium or acrylic implants in a single procedure.
Methods The extent of bone resection of the sphenoorbital meningiomas was planned in a virtual three-dimensional (3D) environment using preoperative thin-layer CT data. The anatomy of the orbital wall in the resection area was reconstructed by superimposing the contralateral unaffected orbit and by using the information of the neighboring bony structures. The customized implants and a corresponding craniotomy template were designed in the desired size and shape by the manufacturer.
Results All patients presented with a sphenoorbital meningioma and exophthalmos. After osteoclastic craniotomy with the drilling template, orbital decompression was performed. Implant fitting was tight in two cases and could be easily fixated with miniplates and screws. In the third patient, a reoperation was necessary for additional bone resection, as well as drilling and repositioning of the implant. The postoperative CT scans showed an accurate reconstruction of the orbital wall. After surgery, exophthalmos was substantially reduced and a satisfying cosmetic result could be finally achieved in all patients.
Conclusions The concept of preoperative 3D virtual treatment planning and single-step orbital reconstruction with CAD/CAM implants after tumor resection involving the orbit is well feasible and can lead to good cosmetic results.
Keywords: CAD/CAM implants, single-step, meningioma, orbital decompression, craniotomy
Introduction
Orbital lesions, such as sphenoorbital meningiomas exert a mass effect and can cause exophthalmos and visual disturbance by compression of the optic nerve. 1 Surgical therapy of sphenoorbital tumors consists of tumor resection and/or orbital decompression with subsequent reconstruction of the bony defects. 1 2 3 To achieve good functional and aesthetic results, restoration of the orbital walls with perfect symmetry is required. However, due to the complex anatomy of the orbital cavity and its surrounding structures, orbital reconstruction remains a challenge for craniofacial surgeons and neurosurgeons.
The conventional approach for reconstructive cranioplasty consists of using bone grafts, biomaterials (e.g., titanium) with a preformed shape, or bone cement. 4 These are established methods for reconstruction of bony defects and their use is timesaving and inexpensive. However, due to the complex geometry of the orbital cavity with several planes of curvature and different thickness, restoration of the original shape is particularly challenging for orbital lesions and a good functional and aesthetic outcome cannot be guaranteed. 5
Owing to the advances in computer-aided design (CAD) and computer-aided manufacturing (CAM), custom-made, and individually tailored implants are widely used for cranioplasty of a predefined defect. 6 7 CAD/CAM implants are manufactured based on volumetric analysis of computed tomography (CT) scans and are already routinely used for cranioplasty reconstruction of orbital fractures. 8 In contrast, single-step orbital decompression and reconstruction with prefabricated customized CAD/CAM implants as surgical strategy for treatment of sphenoorbital lesions represents a new concept and has not been well documented in the literature.
In the current article, we present three cases of patients that underwent orbital decompression for sphenoorbital meningiomas and orbital reconstruction with customized porous titanium or acrylic implants during the same operation. These implants were manufactured preoperatively based on a three-dimensional (3D) CT reconstruction and virtual surgical planning of the craniotomy and resection margins in a 3D CAD environment.
Methods
We report surgical details and clinical outcomes of three patients that underwent orbital decompression and cranioplasty with CAD/CAM implants in a single procedure. According to the institutional guidelines, an ethics committee approval was not required for this retrospective study
Fabrication of the CAD/CAM Implants
After clinical and radiological diagnosis of a sphenoorbital meningioma and decision toward single-step surgery, the patients received a preoperative thin-layer 64-slice multidetector cranial CT scan with 0.5 mm slice thickness (Philips iCT or Philips Brilliance 64, Philips, Best, The Netherlands) that allows 3D reconstruction of the bony structures. The respective DICOM data (Digital Imaging and Communications in Medicine) were provided to the manufacturing company of the CAD/CAM implants (Anatomics Pty Ltd, St Kilda, Australia). After a digital 3D reconstruction of the skull and tumor was performed by the company, the computerized model was sent to the surgeon. A simulated extent of resection and craniotomy was performed in a virtual 3D environment by the surgeon using commercially available software (AnatomicsRx, Anatomics Pty Ltd, St Kilda, Australia). The representative of the manufacturing company gave advice regarding the feasibility of the construction of the implant and assisted in planning the resection margins. Thereafter, the anatomy of the orbital wall in the resection area was virtually reconstructed by superimposing the contralateral unaffected orbit and by using the information of the neighboring bony structures to achieve a symmetrical shape. Finally, the neurosurgeon approved the extent of the craniotomy and the design of the implant.
The customized implants were fabricated in the desired size and shape using CAM. The implants were made of either polymethyl methacrylate (PMMA) or porous titanium. Both materials are frequently used for medical implants in neuro- and craniofacial surgery achieving good morphological and aesthetic results. 9 10 11 12 The advantages of these materials include a high biocompatibility, ability to ossify, light weight, and low-thermal conductivity. 9 13 The prosthesis has a chamfer to avoid sinking of the implant into the resection area and several holes for fixation with plates and miniscrews.
A corresponding drilling template is produced to help carrying out a precise craniotomy. The drilling template has the form of the frame and is fixed to the skull with miniscrews.
The customized CAD/CAM implant and the corresponding drilling template are delivered nonsterile within 3 weeks and need to undergo a standard autoclaving process for sterilization prior to their intraoperative use.
A photograph of a PMMA implant and the corresponding drilling template is provided in Fig. 1 .
Fig. 1.
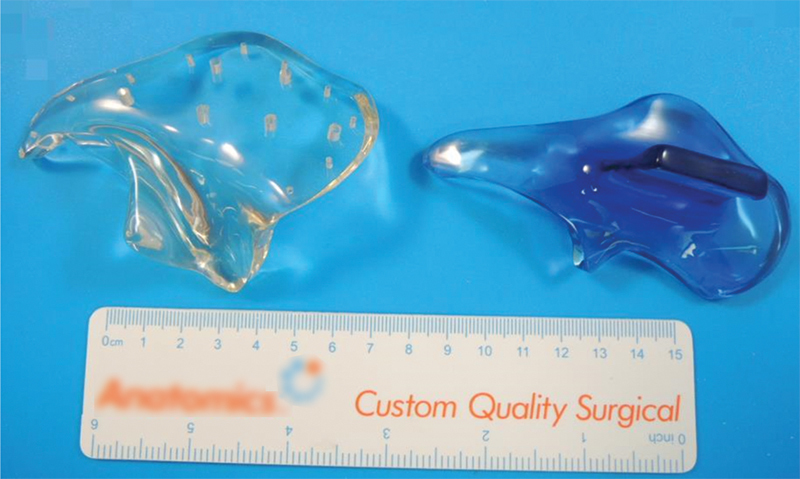
Photograph of a customized PMMA implant and the corresponding drilling template. PMMA, polymethyl methacrylate.
Surgical Procedure
At the beginning of the procedure, the thin-layer CT data were loaded into Brainlab navigation software (Brainlab Cranial, Brainlab, Munich, Germany) to allow neuronavigation guidance during surgery.
The patients were operated in supine position with the head fixed in a Mayfield holder and turned to the nonaffected side at an angle of roughly 30 degrees. A standard frontotemporal approach through a curvilinear incision was used for exposure. Upon identification of the affected region, the drilling template was applied and fixed to the skull with miniscrews. Osteoclastic craniotomy was performed as specified by the drilling template. Subsequently, a decompression of the orbit was performed through generous removal of the superior and lateral borders of the orbit, taking care not to alter the outer contour of the craniotomy. After sufficient bone removal, the customized implant was inserted within the resection area. In all three cases, the borders of the craniotomy had to be slightly enlargened with a Kerrison's punch or a diamond burr to achieve a tight fit of the prosthesis. Thereafter, the implants were fixed with plates and miniscrews to the skull.
Case Reports
Case 1
A 46-year-old female presented with blurred vision on the right eye, diplopia, and right-sided exophthalmos which developed over a 4-month period. Thin-sliced CT and magnetic resonance imaging (MRI) showed a contrast-enhancing intraosseous mass of the anterior skull base with infiltration into the right orbital cavity and compression of the right optical nerve ( Fig. 2A ). A single-step procedure with implantation of a custom-made acryl implant was planned. After osteoclastic frontotemporal craniotomy using the drilling template, the lateral orbital wall was decompressed and complete extradural anterior clinoidectomy was performed. The implant fitted tightly and was fixed using miniscrews. The surgical aim was to decompress the optic canal to prevent further deterioration of the vision and the exophthalmos. Since decompression could be sufficiently achieved by bone resection, the lesion itself was not removed. A postoperative plain CT scan demonstrated the correct adjustment of the implant ( Fig. 2B – D ). Postoperatively, the visual acuity remained unchanged but the exophthalmos and the diplopia improved. Subsequently, the meningioma was treated by definitive radiotherapy to a cumulative dose of 54 Gray in 30 fractions at 1.8 Gray ( Fig. 2E and F ), which was performed without occurrence of adverse events. At last available follow-up 17 months after surgery, there were no delayed implant-related complications.
Fig. 2.
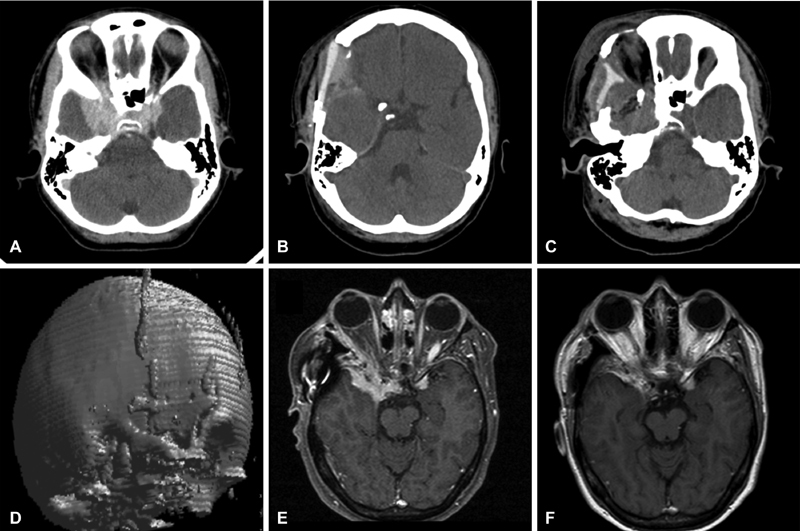
A 46-year-old female presented with right sided exophthalmus. Preoperative cranial CT showed a contrast-enhancing mass of the anterior skull base with infiltration into the right orbital cavity ( A ). Single-step decompression and reconstruction with a customized acryl implant was performed. Postoperative CT demonstrates correct adjustment of the implant with good reconstruction of the lateral orbital wall ( B – D ). Five months after surgery, the meningioma ( E ) was treated by definitive radiotherapy, achieving complete tumor regression ( F ). CT, computed tomography.
Case 2
A 63-year-old female patient presented with exophthalmos. The patient had undergone resection of an intraorbital meningioma 17 years before presentation. MRI showed a recurrent en plaque meningioma of the right sphenoid wing and the orbital cavity ( Fig. 3A – C ). After osteoclastic frontotemporal craniotomy using the drilling template, resection of the superior and lateral orbital wall was performed under neuronavigation guidance. The customized titanium implant fitted well into the defect, as documented by postoperative plain CT scan ( Fig. 3D – F ). Postoperatively, the exophthalmos improved and the patient did not have diplopia or visual impairment. In postoperative soft-tissue window CT, the titanium implant caused only minimal scatter artifacts which allows a radiologic follow-up of the orbital structures ( Fig. 3G ). However, the patient complained about prolonged headache 6 days after surgery. A plain CT scan showed an epidural fluid collection beneath the implant ( Fig. 3H ), which did not require surgery and resolved spontaneously. During a 26-month clinical follow-up duration, no delayed complications was observed.
Fig. 3.
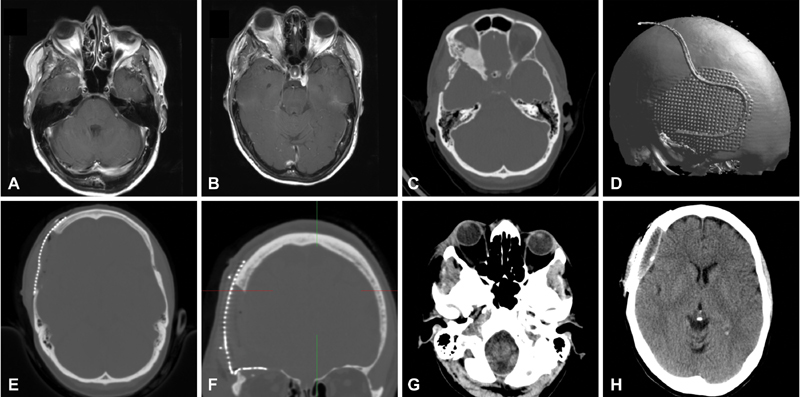
A 63-year-old female patient presented with exophthalmos ( A ). MRI and CT showed an en plaque meningioma of the right sphenoid wing with osseus infiltration into the orbital cavity ( B , C ). Surgery consisted of single-step osteoclastic resection of the superior and laterial orbital wall and implantation of a customized titan implant. Postoperative CT scan shows a proper fit of the implant with adequate reconstruction of the orbital walls ( D – F ) and the exophthalmos improved clinically. Postoperative soft-tissue window CT shows low scatter artifacts in the ocular apex region ( G ). Six days after surgery, a control CT scan shows epidural hygroma beneath the implant which resolved spontaneously ( H ). CT, computed tomography; MRI, magnetic resonance imaging.
Case 3
A 54-year-old female patient presented with right sided exophthalmos and intermittent headaches. CT and MRI showed an intraosseous contrast enhancing lesion, with infiltration of sphenoid and frontal bones, particularly the sphenoid wing and temporal fossa and extending to the orbital rim, consistent with an enplaque meningioma. A single-step procedure with subtotal tumor resection, orbital decompression and acryl CAD/CAM implant reconstruction was performed ( Fig. 4A and B ). After the swelling subsided, the patient presented with a persistent depression of the right orbit leading to a facial dysmorphia. CT and MRI revealed misalignment of the CAD/CAM implant ( Fig. 4C and D ), so that a second procedure was necessary to correct the orbital congestion. Revision surgery consisted of additional bone removal and repositioning of the implant. Thereafter, an acceptable anatomic and functional outcome was achieved. There were no delayed implant-related complications during a 25-month follow-up period.
Fig. 4.
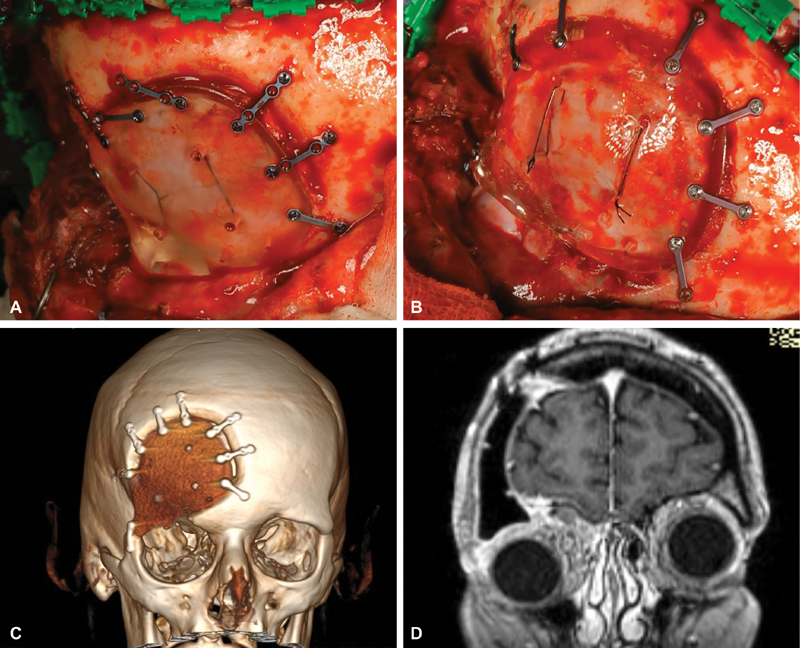
A 54-year-old female patient presented with right sided exophthalmos. CT and MRI showed an enplaque meningioma of the sphenoid wing and temporal fossa extending to the orbital rim (data not available). A single-step procedure with subtotal tumor resection, orbital decompression, and acryl CAD/CAM implant reconstruction was performed. Intraoperative photographs show a suboptimal fit of the implant after craniectomy with the drilling template ( A ) with an elevation of the orbital rim ( B ). After the swelling subsided, the patient presented with a persistent depression of the right orbit leading to a facial dysmorphia. Postoperative three-dimensional CT reconstruction revealed suboptimal placement of the implant, with a gap between frontal bone, implant and low lying orbital rim ( C ). Postoperative coronal MRI showing excessive pressure of the contents of the right orbit through the misaligned implant ( D ). Repositioning of the implant in a second procedure was necessary to correct the orbital congestion. CT, computed tomography; MRI, magnetic resonance imaging.
Results
All patients presented with a sphenoorbital meningioma and consecutive exophthalmos. After osteoclastic craniotomy with the drilling template, the resection margins were further trimmed to achieve adequate orbital decompression. In all cases, the lateral and superior walls of the orbital cavity were removed. In two cases, the implants could be placed satisfactorily within the resection area. The cranioplasty implants fitted tightly and could be easily fixed with miniplates and screws. In the third case, implant fitting was suboptimal with a subsequent depression of the orbital rim. All patients underwent a postoperative native cranial CT scan to control for adequacy of the decompression and fitting of the implant. In the CT scan, the implants did not produce local artifacts and allowed a precise evaluation of the neighboring structures which may be of importance for follow-up examinations.
The exophthalmos improved in the two patients with correct fit of the implant whereas the third patient needed to undergo revision surgery due to excessive pressure of the contents of the right orbit through the misaligned implant. In one case, we observed postoperative seroma collections surrounding the implant, which resolved spontaneously. Rebleeding and cerebrospinal fluid fistulas did not occur. Wound healing was normal without any incidence of wound healing disorders. During midterm follow-up, implant-related complications, such as infection, extrusion, or malposition, did not occur.
Discussion
Sphenoorbital lesions exert a mass effect on the optical nerve and the ocular bulb, resulting in visual disturbance and exophthalmos, respectively. 1 Surgical decompression of the orbital cavity improves these symptoms; however, orbital reconstruction remains a particular challenge for the surgeons. To obtain an excellent aesthetic and functional outcome, accurate reconstruction of the original orbital geometry achieving perfect symmetry may be required. Reconstructive osteoplasty of the orbital cavity is more difficult than reconstructive cranioplasty of the skull due to the complex anatomy of the orbit with different planes of curvature and different thickness.
Orbital reconstruction with standardized preformed implants or bone grafts is relatively easy and inexpensive, but this technique only allows an approximate reconstruction of the orbital cavity and the functional and aesthetic results depend on the experience of the surgeon and the complexity of the defect. Therefore, a satisfactory cosmetic and functional outcome cannot be guaranteed.
Owing to the recent advances in CAD/CAM engineering technology, cranioplasty with customized implants has become an established neurosurgical procedure which helps to obtain good functional and aesthetic results. 14 In orbital reconstructive surgery, CAD/CAM implants have been predominantly used for reconstruction of orbital fractures. 8 15 16 Compared with standardized preformed implants, customized implants allow for a more accurate reconstruction of the original orbital geometry. Zimmerer et al performed a prospective study on 195 patients and compared standard preformed with individualized prostheses for posttraumatic reconstruction. The authors showed that customized implants provide a more precise reconstruction and an improved functional and aesthetic outcome than preformed implants. 5 In particular, accurate reconstruction of the orbital wall helps to reduce the incidence of postoperative enophthalmos and diplopia. 8
In the above cited articles, customized implants were fabricated on the basis of a pre-existing osseous defect. In contrast, there are only little data available on single-step tumor decompression and CAD/CAM cranioplasty.
In 2017, Carolus et al presented two patients with intraosseous skull base meningiomas that underwent tumor resection and one-step cranioplasty with a customized CAD/CAM titanium implant. 17 The authors reported a good fitting of the implants and satisfactory cosmetic results. Gerbino et al reported good morphological outcome using customized polyetheretherketone (PEEK) implants in three patients with fronto-orbito-pterional craniotomy for intracranial lesions. 18 Similarly, Jalbert et al reported on five cases with benign lesions in the frontoorbital region that underwent one-step reconstruction with PEEK implants. 19
An important aspect of one-step orbital reconstruction consists of careful preoperative virtual planning of craniotomy and the resection margins in a CAD environment based on volumetric analysis of 3D CT data. In case where complete tumor resection is possible, meticulous and accurate preoperative tracing of the margins of the bone infiltration is important, since intraoperative modification of the planned craniotomy (for example due to tumor-positive margins) is not possible and doing so would lead to suboptimal fitting of the implant. In our experience, it is not uncommon that the meningioma infiltrates the skull base extensively, rendering complete resection impossible, with an emphasis on the cosmetic outcome. Furthermore, although the planning process can be time-consuming, this approach does not require more elaborate techniques, such as a stereolithographic model.
In two of the three cases, there was tumor infiltration of the superior and/or lateral orbital rim. The anatomy of the orbital rim is complex and can be best reconstructed with the usage of CAD/CAM implants. In the third case, the CAD/CAM implant was used to reconstruct the lateral and superior orbital wall. The reconstruction of the anterior temporal fossa helps to avoid postoperative asymmetry, particularly in cases of coexisting temporal muscle atrophy, although such a reconstruction is also possible with simple techniques, such as fitting a mesh or using a bone split-graft technique. Since admittedly the usage of the CAD/CAM implant comes with a higher cost (between €4,000 and 5,000 at our institution), we believe that customized implants should be used when reconstruction of the superolateral orbital rim is necessary.
In the current study, we report our technical experience with the use of a reproducible approach that combines orbital decompression and reconstruction with customized implants in one procedure. One-step surgery was feasible in all cases, and craniotomy could be performed as previously planned in the virtual CAD environment. However, good functional and aesthetic results could only be achieved in two of three patients. In the third patient, the implant did not fit tightly and modifications of the craniotomy led to new bone implant conflict points or to bigger gaps. During revision surgery, the height of the orbital rim could be improved but only at the cost of suboptimal fitting at the margins. We believe that the problem can be identified in the craniotomy itself. Although the implant and the drilling template are designed to fit perfectly, following the marked contours during craniotomy can be challenging, particularly in areas of tumor infiltration and thickening of the bone. Therefore, this accuracy cannot always be achieved, especially not in the orbital region which is characterized by a complex anatomy. For this reason, we had to slightly modify the craniotomy margins in all three cases to achieve a tight fit of the implant.
In our experience, although the decompression of the orbital wall should be generous, there is no need to reconstruct the orbital walls completely. For a good cosmetic result after orbital decompression, proper reconstruction of the superior and lateral orbital rim is sufficient. Designing the implant in a way that loyally reconstructs the anatomy of the orbit requires complex implant design and very precise performing of the craniotomy and can ultimately lead to failure, as in case 3.
Conclusion
The use of CAD/CAM implants for single-step decompression and reconstruction of the orbital cavity is feasible, and good anatomic and functional results can be achieved if the implants fit tightly. During surgery, a precise craniotomy is necessary for an accurate fit of the customized implants due to the complex orbital geometry. Although the necessary virtual surgical preplanning can be cumbersome, one single-step operation may be less time consuming in total if compared with the two-staged procedures.
Footnotes
Conflict of Interest None.
References
- 1.Scarone P, Leclerq D, Héran F, Robert G. Long-term results with exophthalmos in a surgical series of 30 sphenoorbital meningiomas. Clinical article. J Neurosurg. 2009;111(05):1069–1077. doi: 10.3171/2009.1.JNS081263. [DOI] [PubMed] [Google Scholar]
- 2.Ringel F, Cedzich C, Schramm J.Microsurgical technique and results of a series of 63 spheno-orbital meningiomas Neurosurgery 2007600402214–221., discussion 221–222 [DOI] [PubMed] [Google Scholar]
- 3.Cannon P S, Rutherford S A, Richardson P L, King A, Leatherbarrow B. The surgical management and outcomes for spheno-orbital meningiomas: a 7-year review of multi-disciplinary practice. Orbit. 2009;28(06):371–376. doi: 10.3109/01676830903104645. [DOI] [PubMed] [Google Scholar]
- 4.Sahoo N, Roy I D, Desai A P, Gupta V. Comparative evaluation of autogenous calvarial bone graft and alloplastic materials for secondary reconstruction of cranial defects. J Craniofac Surg. 2010;21(01):79–82. doi: 10.1097/SCS.0b013e3181c3ba58. [DOI] [PubMed] [Google Scholar]
- 5.Zimmerer R M, Ellis E, III, Aniceto G S et al. A prospective multicenter study to compare the precision of posttraumatic internal orbital reconstruction with standard preformed and individualized orbital implants. J Craniomaxillofac Surg. 2016;44(09):1485–1497. doi: 10.1016/j.jcms.2016.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Heissler E, Fischer F-S, Bolouri S et al. Custom-made cast titanium implants produced with CAD/CAM for the reconstruction of cranium defects. Int J Oral Maxillofac Surg. 1998;27(05):334–338. doi: 10.1016/s0901-5027(98)80060-x. [DOI] [PubMed] [Google Scholar]
- 7.Saringer W, Nöbauer-Huhmann I, Knosp E. Cranioplasty with individual carbon fibre reinforced polymere (CFRP) medical grade implants based on CAD/CAM technique. Acta Neurochir (Wien) 2002;144(11):1193–1203. doi: 10.1007/s00701-002-0995-5. [DOI] [PubMed] [Google Scholar]
- 8.Klein M, Glatzer C. Individual CAD/CAM fabricated glass-bioceramic implants in reconstructive surgery of the bony orbital floor. Plast Reconstr Surg. 2006;117(02):565–570. doi: 10.1097/01.prs.0000200770.83864.bc. [DOI] [PubMed] [Google Scholar]
- 9.Groth M J, Bhatnagar A, Clearihue W J, Goldberg R A, Douglas R S. Long-term efficacy of biomodeled polymethyl methacrylate implants for orbitofacial defects. Arch Facial Plast Surg. 2006;8(06):381–389. doi: 10.1001/archfaci.8.6.381. [DOI] [PubMed] [Google Scholar]
- 10.Wehmöller M, Weihe S, Rasche C, Scherer P, Eufinger H. CAD/CAM-prefabricated titanium implants for large skull defects—clinical experience with 166 patients from 1994 to 2000. Int Congr Ser. 2004;1268:667–672. [Google Scholar]
- 11.Eufinger H, Wehmöller M. Individual prefabricated titanium implants in reconstructive craniofacial surgery: clinical and technical aspects of the first 22 cases. Plast Reconstr Surg. 1998;102(02):300–308. doi: 10.1097/00006534-199808000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Huang G J, Zhong S, Susarla S M, Swanson E W, Huang J, Gordon C R. Craniofacial reconstruction with poly(methyl methacrylate) customized cranial implants. J Craniofac Surg. 2015;26(01):64–70. doi: 10.1097/SCS.0000000000001315. [DOI] [PubMed] [Google Scholar]
- 13.Özcan M, Hämmerle C. Titanium as a reconstruction and implant material in dentistry: advantages and pitfalls. Materials (Basel) 2012;5(09):1528–1545. [Google Scholar]
- 14.Choudhry O J, Christiano L D, Arnaout O, Adel J G, Liu J K. Reconstruction of pterional defects after frontotemporal and orbitozygomatic craniotomy using Medpor Titan implant: cosmetic results in 98 patients. Clin Neurol Neurosurg. 2013;115(09):1716–1720. doi: 10.1016/j.clineuro.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 15.Lieger O, Richards R, Liu M, Lloyd T. Computer-assisted design and manufacture of implants in the late reconstruction of extensive orbital fractures. Arch Facial Plast Surg. 2010;12(03):186–191. doi: 10.1001/archfacial.2010.26. [DOI] [PubMed] [Google Scholar]
- 16.Fan X, Zhou H, Lin M, Fu Y, Li J. Late reconstruction of the complex orbital fractures with computer-aided design and computer-aided manufacturing technique. J Craniofac Surg. 2007;18(03):665–673. doi: 10.1097/scs.0b013e31803ffaaa. [DOI] [PubMed] [Google Scholar]
- 17.Carolus A, Weihe S, Schmieder K, Brenke C. One-step CAD/CAM titanium cranioplasty after drilling template-assisted resection of intraosseous skull base meningioma: technical note. Acta Neurochir (Wien) 2017;159(03):447–452. doi: 10.1007/s00701-016-3053-4. [DOI] [PubMed] [Google Scholar]
- 18.Gerbino G, Bianchi F A, Zavattero E, Tartara F, Garbossa D, Ducati A. Single-step resection and reconstruction using patient-specific implants in the treatment of benign cranio-orbital tumors. J Oral Maxillofac Surg. 2013;71(11):1969–1982. doi: 10.1016/j.joms.2013.03.021. [DOI] [PubMed] [Google Scholar]
- 19.Jalbert F, Boetto S, Nadon F, Lauwers F, Schmidt E, Lopez R. One-step primary reconstruction for complex craniofacial resection with PEEK custom-made implants. J Craniomaxillofac Surg. 2014;42(02):141–148. doi: 10.1016/j.jcms.2013.04.001. [DOI] [PubMed] [Google Scholar]


