Abstract
Disturbances in sleep and circadian rhythms may be important, albeit underappreciated, risk factors for the initiation of alcohol use and the escalation of alcohol problems. In this review, we first describe sleep and circadian changes during adolescence and young adulthood. Second, we explain how these sleep/circadian changes intersect with onset and escalation of alcohol use. Third, we briefly note how alcohol use (whether acute or chronic) affects sleep and circadian rhythms. Finally, we articulate a conceptual model containing two mechanistic pathways—broadly positive and negative reinforcement—linking sleep/circadian factors to alcohol involvement before listing key areas we believe are ripe for further inquiry.
Keywords: sleep, circadian rhythms, alcohol, positive reinforcement, negative reinforcement
INTRODUCTION
Accumulating evidence indicates that disturbances in sleep and circadian rhythms may be important, albeit underappreciated, risk factors for the initiation of alcohol use and the escalation of alcohol problems. In this review, we (1) briefly review relevant changes in sleep and circadian rhythms during adolescence into young adulthood, when alcohol use is onsetting and peaking. (2) describe burgeoning evidence that sleep/circadian disturbances often precede and/or predict alcohol involvement, (3) briefly note alcohol’s effects on subsequent sleep/circadian rhythms, and (4) articulate some putative mechanisms linking sleep/circadian factors to alcohol involvement that we identify as areas deserving further inquiry.
SLEEP AND CIRCADIAN CHANGES DURING ADOLESCENCE AND YOUNG ADULTHOOD
Marked changes in sleep and circadian rhythms begin with the onset of puberty and continue into the early 20’s, corresponding with increased heavy alcohol use [1]. Sleep timing shifts later over this timespan, as evident via both studies of actual sleep timing, as well as studies of morningness/eveningness preference [2, 3]. Along with sociocultural influences, these timing shifts appear to be driven by two biological processes: (1) increasingly later circadian timing (e.g.,, per salivary melatonin) [2]; and (2) a slower accumulation of homeostatic sleep pressure (i.e., per electroencephalographic (EEG) measures of slow-wave activity) [4]. Based on studies of chronotype, the shift towards later timing appears to peak around age 20, then reverses course towards earlier timing over the rest of the lifespan [3]. The tendency towards later timing is mismatched with early school start times, resulting in difficulty falling asleep (insomnia), insufficient sleep, and daytime sleepiness on weekdays, as well as large swings in sleep timing and duration on weekends, when adolescents tend to stay up later and sleep in in order to make up for lost sleep (i.e., ‘social jet lag’ [5]). Current recommendations are for 8-10 hours of sleep per night on average [6], but large survey studies suggest that ~ 1/3 of adolescents achieve the recommended sleep duration [7]. The prevalence of insomnia is also elevated during adolescence and young adulthood [8].
SLEEP AND CIRCADIAN CHARACTERISTICS AS CORRELATES OF AND RISK FACTORS FOR ALCOHOL INVOLVEMENT
Concurrent associations between sleep disturbances and heavier alcohol use and/or more problems during adolescence and young adulthood are well-recognized [9]. Furthermore, worse or insufficient sleep appears to be related to engagement in alcohol use [10] and more severe consequences of alcohol use [11], particularly when coupled with higher alcohol coping motives (e.g., drinking to reduce anxiety) [12]. Perhaps the most consistent finding is that greater eveningness (a preference for relatively later activity and sleep) is associated with greater alcohol involvement [13–16]. Eveningness is also associated with greater endorsement of a range of reasons for drinking that are associated with elevated alcohol use [17]. Evening-types are more likely to experience larger weekday-weekend changes in sleep timing (i.e., social jet lag) [5], which have also been linked to higher alcohol use in adolescents and young adults [18*, 19].
Studies employing objective circadian measures (e.g., salivary melatonin) are much scarcer, but generally align with the subjective sleep literature. In a sample of high-school aged adolescents with a history of substance use disorders (SUD), later circadian timing and greater circadian misalignment were both associated with higher current SUD symptoms [20]. Circadian misalignment was operationalized as a shorter interval between the onset of melatonin secretion (typically 2-3 hours before bedtime) and the midpoint of the sleep period, consistent with sleeping at an earlier time relative to one’s circadian clock. This finding was extended recently to 18-22 year-olds using the same operationalization of circadian misalignment [18*]. Greater circadian misalignment prior to the weekend was associated with greater alcohol use over the weekend. These findings suggest that it’s not simply later timing that matters, but the relative timing between one’s sleep schedule and one’s internal circadian clock.
Importantly, an increasing number of longitudinal studies of sleep and alcohol involvement have been published in the last decade. Almost without exception, these studies have consistently reported that poor sleep, short sleep, and later and/or more variable sleep timing predict the onset and/or escalation of alcohol use and alcohol-related problems [21–25]. One limitation of some of these studies has been the necessary reliance on convenience measures of sleep, often based on single items from larger questionnaires (e.g., Child Behavior Check List). However, more recent publications have begun to address this limitation. For example, a recent paper from the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) study assessed a wider range of sleep/circadian characteristics using full questionnaires and/or abbreviated versions of validated questionnaires [26*]. In that study, greater eveningness, later bedtimes (weekday and weekend), and shorter weekday sleep duration at baseline were all predictive of an increase in heavy drinking a year later, accounting for baseline drinking.
EFFECTS OF ALCOHOL USE ON SLEEP AND CIRCADIAN RHYTHMS
While a detailed review of alcohol effects on sleep and circadian rhythms is beyond the scope of the present paper (see [27, 28] for more thorough discussion), we offer a concise review of the most pertinent findings here. Acute use of alcohol in healthy adults tends to speed the onset of sleep and improve sleep consolidation in the first half of the night, including increasing slow wave sleep, while disrupting sleep in the second half of the night, including reducing rapid eye movement (REM) sleep [27]. These acute effects may depend on both time-of-day and developmental stage. Evening use of alcohol may be relatively more stimulating for adolescents and emerging adults than at other times of day [29], and alcohol is generally less sedating during adolescence [30], which together may explain findings suggesting that alcohol use does not reduce the time to fall asleep in adolescents [31]. In laboratory studies of chronic alcohol use (repeated alcohol administration), any short-term benefits for sleep in the first half of the night disappear [32]. Sleep disorders are common (36-91%) among people with an alcohol use disorder (AUD) [33], consistent with long-term heavy alcohol use disrupting sleep. Although relatively less studied in adolescents, one longitudinal study suggests that adolescents with an AUD at baseline have persistent sleep disturbances at least 5 years later [22]. Alcohol use is also associated with altered circadian rhythms in humans [28] and animal models, with the latter suggesting that alcohol disrupts light’s phase-shifting effects on circadian timing [34], although a study in humans failed to replicate this effect [35].
The effects of alcohol on sleep may be moderated by sleep/circadian factors. A few laboratory-based alcohol administration studies suggest that adults with insomnia differentially benefit from alcohol use in the short-term, with relatively larger increases in slow wave sleep and reductions in anxiety compared to adults without insomnia [32]. However, these benefits diminish quickly with consecutive nights of alcohol use [36]. Although similar studies have not been conducted in adolescents with insomnia, data suggests that adolescents with insomnia are more likely to self-medicate with alcohol, particularly among males [37].
POSSIBLE MECHANISMS LINKING SLEEP/CIRCADIAN FACTORS TO RISK FOR ALCOHOL INVOLVEMENT
We put forth a conceptual model (see Figure 1) that integrates existing literature with future directions to further our understanding of how sleep and circadian disturbances increase risk for alcohol problems. Based on the extant evidence, we contend that putative mechanisms linking sleep/circadian factors to increased risk for alcohol involvement fall into two categories that can be broadly labeled positive and negative reinforcement, respectively.
Figure 1.
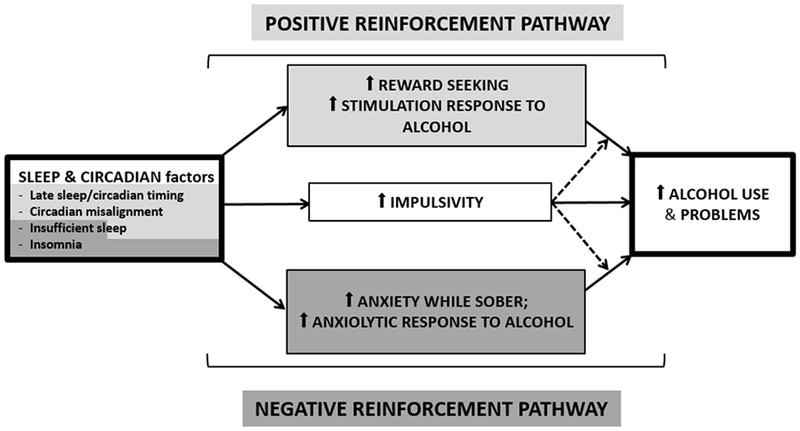
Conceptual model of how sleep and circadian disturbances may increase risk for alcohol problems via positive and negative reinforcement pathways. Furthermore, impulsivity could play an exacerbating role in both positive and negative reinforcement pathways. Shading is used to distinguish the two separate pathways, including indicating potentially distinct pathways from specific sleep/circadian characteristics, such as circadian misalignment influencing alcohol use via positive reinforcement processes, while insomnia influencing alcohol use via negative reinforcement processes. The bi-color shading of insufficient sleep is intended to indicate that it may influence risk via both positive and negative reinforcement pathways.
As reviewed in more detail elsewhere [38, 39], a burgeoning literature implicates reward-related processes (i.e., positive reinforcement) in the link between sleep/circadian disturbance and adolescent alcohol involvement. Robust evidence supports sleep/circadian modulation of reward-related behavior (e.g., alcohol use and drug-seeking behavior) and its underlying physiology [40–45]. In adolescent and young adult samples, increased eveningness is associated with greater self-reported sensation- and novelty-seeking, reward dependence, and impulsivity [46–49]. Furthermore, we have shown in late adolescence that greater eveningness is associated with altered neural reactivity to reward and in turn correlated with greater alcohol use and AUD symptoms [50], including prospectively [51]. Although these studies have generally employed monetary reward tasks, preliminary evidence from a alcohol administration study we conducted suggests that later sleep timing may be associated with increased sensitivity to alcohol-related reward [52*]. Specifically, we found that later sleep timing in an adult, moderate-drinking sample was associated with greater self-reported stimulation following alcohol consumption (relative to drinking a non-alcohol beverage). Notably, this appeared to be only true in White, not Black participants (see below for further discussion).
Evidence for the negative reinforcement pathway linking sleep/circadian factors to alcohol involvement comes from evidence that alcohol is often used to improve sleep and reduce anxiety (which may, in turn, ease the transition to sleep). Alcohol is a commonly reported “sleep aid” in individuals with poor sleep [53], with prevalence estimates up to ~30% in the general US population [54]. Although, as described above, the evidence clearly indicates that alcohol use is detrimental to sleep overall, at least one national survey reported that ~67% of individuals with insomnia view alcohol as effective for improving sleep [54]. Notably, anxiety is commonly comorbid with insomnia [55] and alcohol problems [56]. Higher anxiety predicts drinking to cope with negative mood [57] and greater reduction in tension/anxiety following alcohol consumption [58]. This may explain in part the aforementioned finding that individuals with insomnia exhibit relatively greater sleep benefits after alcohol use [59*]. The insomnia group (n=11) in that study also reported a greater post-alcohol decrease in anxiety relative to the control group (n=9), suggesting that alcohol may be more reinforcing to individuals with insomnia due to a larger reduction in anxiety. Insomnia and related sleep disturbances appear to increase the risk of relapse in alcohol-dependent individuals during abstinence [60], suggesting that insomnia may engage negative reinforcement processes at multiple stages of the AUD course.
Impulsivity could play an exacerbating role in both positive and negative reinforcement pathways, given evidence of its sensitivity to sleep/circadian factors (e.g., [61*]) and relevance to alcohol problems [62]. Specifically, impulse control appears to be diminished in the context of late sleep timing, sleep disturbance and/or sleep loss, making affected individuals more likely to engage in heavy alcohol use during periods of worsened mood (i.e., negative urgency) or when feeling more stimulated from alcohol.
FUTURE DIRECTIONS
Although we believe the existing evidence makes a compelling case for the value of understanding the role of sleep and circadian characteristics in risk for later alcohol involvement and alcohol use disorder, a number of important questions remain.
In particular, research is needed to articulate which specific sleep (e.g., timing, duration, continuity) and circadian (e.g., chronotype, time of alcohol use) factors are mechanistically related to responses to alcohol, mood (positive and/or negatively-valenced), impulsivity, and their interaction (e.g., negative urgency: acting rashly while in a strong negative mood). Identification of biobehavioral mechanisms by which sleep/circadian factors influence alcohol involvement will directly contribute to the optimization of prevention and intervention approaches. Examination of the dynamic transaction between sleep, impulsivity, mood and alcohol response is needed to further understanding of for whom sleep/circadian factors are likely to increase problematic alcohol use.
Such work will require moving beyond the cross-sectional study designs that have dominated the extant literature to prospective and experimental designs. Although longitudinal papers in this area are accumulating, many are limited by use of single items rather than well-validated full self-report measures or objective alternatives (e.g, wrist actigraphy). We assert the need for more intensive, prospective studies using ecological momentary assessment (EMA) methods and robust sleep measures to investigate more proximal relationships between sleep/circadian factors, putative mechanisms, and alcohol use. A few such studies are emerging, including a recent one in college students that reported complex, bidirectional day-to-day relationships between sleep and drinking. Specifically, Fucito and colleagues [63*] reported that heavy drinking predicted delayed timing and shorter sleep that night, while short sleep, early wake times, and greater sleep quality predicted heavier drinking the following day. And, of course, to properly assess causality and directionality, we need more experimental studies, including both sleep/circadian manipulation protocols and alcohol administration protocols, both of which can be combined with EMA.
As in other areas of the literature, there has been insufficient consideration to date of the role of sex and/or race in sleep/circadian-alcohol associations. Sleep/circadian characteristics vary by sex and race [64–66], as does alcohol use behavior and risk for alcohol problems [67, 68]. For example, male individuals tend to exhibit later sleep timing [65], while female individuals report more insomnia [66]. Black individuals tend to experience both shorter and worse sleep than White individuals [69] but may be less subject to apparent effects of sleep timing on alcohol response [52]. Given that all of these sleep/circadian characteristics have been linked in turn to alcohol involvement, it is plausible that they may contribute to relative risk differences across sex and race. Indeed, a handful of studies suggest that sex moderates the respective relationships between sleep/circadian characteristics and sensation-seeking, reward dependence, depression, and nicotine use [70*–73], and two recent studies suggest that men may be particularly vulnerable to sleep-related risk for alcohol problems [37, 74*].
Finally, while the literature to-date suggests that sleep-focused treatments benefit sleep in heavy-drinking individuals or those with AUD, no studies have yet shown a differential benefit for alcohol-related outcomes [75, 76]. We are excited about the prospect that as our understanding of mechanisms improves, the possibility for enhancing current treatment approaches will likely increase, perhaps by incorporating chronotherapeutic approaches (e.g., bright light) that have not yet been employed in AUD patients. This holds great promise considering sleep-focused treatment carries less stigma than alcohol-focused interventions [77*, 78], which could motivate relevant individuals to seek help for sleep while paving the way for eventual focus on their alcohol involvement.
Acknowledgments
FUNDING: This work was supported by the National Institutes of Health including R01AA025626 (Hasler), R01AA025617 (Pedersen), and R01AA026249 (Hasler/Pedersen)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES CITED
- 1.Tucker JS, et al. , Substance use trajectories from early adolescence to emerging adulthood: A comparison of smoking, binge drinking, and marijuana use. Journal of Drug Issues, 2005. 35(2): p. 307–332. [Google Scholar]
- 2.Crowley SJ, et al. , A longitudinal assessment of sleep timing, circadian phase, and phase angle of entrainment across human adolescence. PLoS One, 2014. 9(11): p. e112199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roenneberg T, et al. , A marker for the end of adolescence. Current Biology, 2004. 14(24): p. R1038–9. [DOI] [PubMed] [Google Scholar]
- 4.Jenni OG and Carskadon MA, Sleep Behavior and Sleep Regulation from Infancy through Adolescence: Normative Aspects. Sleep Medicine Clinics, 2007. 2(3): p. 321–329. [Google Scholar]
- 5.Wittmann M, et al. , Social jetlag: Misalignment of biological and social time. Chronobiology International, 2006. 23(1&2): p. 497–509. [DOI] [PubMed] [Google Scholar]
- 6.Paruthi S, et al. , Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med, 2016. 12(6): p. 785–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basch CE, Prevalence of sleep duration on an average school night among 4 nationally representative successive samples of American high school students, 2007–2013. Preventing chronic disease, 2014. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson E, et al. , Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics, 2006. 117(2): p. 247–256. [DOI] [PubMed] [Google Scholar]
- 9.Johnson EO and Breslau N, Sleep problems and substance use in adolescence. Drug and Alcohol Dependence, 2001. 64(1): p. 1–7. [DOI] [PubMed] [Google Scholar]
- 10.McKnight-Eily LR, et al. , Relationships between hours of sleep and health-risk behaviors in US adolescent students. Preventive Medicine, 2011. 53(4): p. 271–273. [DOI] [PubMed] [Google Scholar]
- 11.Kenney SR, et al. , Global sleep quality as a moderator of alcohol consumption and consequences in college students. Addictive Behaviors, 2012. 37(4): p. 507–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kenney SR, et al. , Mental health, sleep quality, drinking motives, and alcohol-related consequences: A path-analytic model. Journal of Studies on Alcohol and Drugs, 2013. 74(6): p. 841–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tavernier R and Willoughby T, Are all evening-types doomed? Latent class analyses of perceived morningness-eveningness, sleep and psychosocial functioning among emerging adults. Chronobiology International, 2013(0): p. 1–11. [DOI] [PubMed] [Google Scholar]
- 14.Pieters S, et al. , Puberty-dependent sleep regulation and alcohol use in early adolescents. Alcoholism: Clinical and Experimental Research, 2010. 34(9): p. 1512–8. [DOI] [PubMed] [Google Scholar]
- 15.Saxvig IW, et al. , Prevalence and correlates of delayed sleep phase in high school students. Sleep medicine, 2012. 13(2): p. 193–9. [DOI] [PubMed] [Google Scholar]
- 16.Urban R, Magyarodi T, and Rigo A, Morningness-eveningness, chronotypes and health-impairing behaviors in adolescents. Chronobiology International, 2011. 28(3): p. 238–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Digdon N and Landry K, University students’ motives for drinking alcohol are related to evening preference, poor sleep, and ways of coping with stress. Biological Rhythm Research, 2013. 44(1): p. 1–11. [Google Scholar]
- *18.Hasler BP, et al. , Circadian misalignment and weekend alcohol use in late adolescent drinkers: Preliminary evidence. Chronobiology International, 2019: p. 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper reports that greater weekday circadian misalignment, as measured by the interval between the onset of melatonin secretion and the midpoint of sleep, is associated with greater alcohol use on the weekend. Besides extending a prior finding that a similar measure of circadian misalignment correlated with symptoms of substance abuse and dependence in a sample of adolescents, the study is notable for its use of and objective measure of circadian misalignment and ecological momentary assessment approach to measuring sleep and alcohol use.
- 19.O’Brien EM and Mindell JA, Sleep and risk-taking behavior in adolescents. Behavioral Sleep Medicine, 2005. 3(3): p. 113–33. [DOI] [PubMed] [Google Scholar]
- 20.Hasler BP, et al. , Circadian phase in sleep-disturbed adolescents with a history of substance abuse: A pilot study. Behavioral Sleep Medicine, 2008. 6(1): p. 55–73. [DOI] [PubMed] [Google Scholar]
- 21.Hasler BP, Kirisci L, and Clark DB, Restless sleep and variable sleep timing during late childhood accelerate the onset of alcohol and drug involvement. Journal of Studies on Alcohol and Drugs, 2016. 77(4): p. 649–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasler BP, et al. , A longitudinal study of insomnia and other sleep complaints in adolescents with and without alcohol use disorders. Alcoholism: Clinical and Experimental Research, 2014. 38(8): p. 2225–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mike T, et al. , The hazards of bad sleep: Sleep duration and quality as predictors of adolescent alcohol and cannabis use. Drug and Alcohol Dependence, 2016. 168: p. 335–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong MM, et al. , Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcoholism: Clinical and Experimental Research, 2004. 28(4): p. 578–87. [DOI] [PubMed] [Google Scholar]
- 25.Wong MM, et al. , Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcoholism: Clinical and Experimental Research, 2010. 34(6): p. 1033–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *26.Hasler BP, et al. , Eveningness and later sleep timing are associated with greater risk for alcohol and marijuana use in adolescence: Initial findings from the National Consortium on Alcohol and Neurodevelopment in Adolescence. Alcoholism: Clinical and Experimental Research, 2017. 41(6): p. 1154–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]; A longitudinal study in adolescents suggesting that eveningness and sleep timing are risk factors for alcohol and marijuana involvement. This study is notable for including a comprehensive battery of self-reported sleep assessments, and importantly, the sleep analyses were a priori rather than post hoc secondary analyses.
- 27.Ebrahim IO, et al. , Alcohol and sleep I: Effects on normal sleep. Alcoholism: Clinical and Experimental Research, 2013. 37(4): p. 539–49. [DOI] [PubMed] [Google Scholar]
- 28.Hasler BP, et al. , Circadian rhythms, sleep, and substance abuse. Sleep Medicine Reviews, 2012. 16(1): p. 67–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Reen E, et al. , Biphasic effects of alcohol as a function of circadian phase. Sleep, 2013. 36(1): p. 137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spear LP and Varlinskaya EI, Adolescence, in Recent developments in alcoholism. 2005, Springer, p. 143–159. [PubMed] [Google Scholar]
- 31.Chan JK, et al. , The acute effects of alcohol on sleep architecture in late adolescence. Alcoholism: Clinical and Experimental Research, 2013. 37(10): p. 1720–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roehrs T and Roth T, Sleep, sleepiness, and alcohol use. Alcohol Res Health, 2001. 25(2): p. 101–9. [PMC free article] [PubMed] [Google Scholar]
- 33.Chakravorty S, Chaudhary NS, and Brower KJ, Alcohol Dependence and Its Relationship With Insomnia and Other Sleep Disorders. Alcoholism: Clinical and Experimental Research, 2016. 40(11): p. 2271–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Damaggio AS and Gorman MR, The circadian timing system in ethanol consumption and dependence. Behavioral Neuroscience, 2014. 128(3): p. 371–386. [DOI] [PubMed] [Google Scholar]
- 35.Burgess HJ, et al. , A single dose of alcohol does not meaningfully alter circadian phase advances and phase delays to light in humans. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 2016. 310(8): p. R759–R765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roehrs T and Roth T, Insomnia as a path to alcoholism: tolerance development and dose escalation. Sleep, 2018. 41(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang J, et al. , Emergence of Sex Differences in Insomnia Symptoms in Adolescents: A Large-Scale School-Based Study. Sleep, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hasler BP and Clark DB, Circadian misalignment, reward-related brain function, and adolescent alcohol involvement. Alcoholism: Clinical and Experimental Research, 2013. 37(4): p. 558–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Logan RW, et al. , Impact of sleep and circadian rhythms on addiction vulnerability in adolescents. Biological Psychiatry, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murray G, et al. , Nature’s clocks and human mood: the circadian system modidates reward motivation. Emotion, 2009. 9(5): p. 705–16. [DOI] [PubMed] [Google Scholar]
- 41.Sleipness EP, Sorg BA, and Jansen HT, Diurnal differences in dopamine transporter and tyrosine hydroxylase levels in rat brain: dependence on the suprachiasmatic nucleus. Brain Research, 2007. 1129(1): p. 34–42. [DOI] [PubMed] [Google Scholar]
- 42.Webb IC, et al. , Diurnal variations in natural and drug reward, mesolimbic tyrosine hydroxylase, and clock gene expression in the male rat. Journal of Biological Rhythms, 2009. 24(6): p. 465–76. [DOI] [PubMed] [Google Scholar]
- 43.Hampp G and Albrecht U, The circadian clock and mood-related behavior. Communicative & Integrative Biology, 2008. 1(1): p. 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spanagel R, et al. , The clock gene Per2 influences the glutamatergic system and modidates alcohol consumption. Nature Medicine, 2005. 11(1): p. 35–42. [DOI] [PubMed] [Google Scholar]
- 45.Ozburn AR, et al. , The role of Clock in ethanol-related behaviors. Neuropsychopharmacology, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tonetti L, et al. , Morningness-eveningness preference and sensation seeking. European Psychiatry, 2010. 25(2): p. 111–5. [DOI] [PubMed] [Google Scholar]
- 47.Killgore WD, Effects of sleep deprivation and morningness-eveningness traits on risk-taking. Psychological Reports, 2007. 100(2): p. 613–26. [DOI] [PubMed] [Google Scholar]
- 48.Hasler BP, et al. , Morningness-eveningness and depression: Preliminary evidence for the role of BAS and positive affect. Psychiatry Research, 2010. 176(2-3): p. 166–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Adan A, et al. , Relationship between circadian typology and functional and dysfunctional impulsivity. Chronobiology International, 2011. 27(3): p. 606–19. [DOI] [PubMed] [Google Scholar]
- 50.Hasler BP, et al. , Weekend-weekday advances in sleep timing are associated with altered reward-related brain function in healthy adolescents. Biological Psychology, 2012. 91(3): p. 334–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hasler BP, et al. , Eveningness among late adolescent males predicts neural reactivity to reward and alcohol dependence two years later. Behavioural Brain Research, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *52.Hasler BP, et al. , Preliminary evidence that real world sleep timing and duration are associated with laboratory-assessed alcohol response. Alcoholism: Clinical and Experimental Research, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]; Our paper was the first to examine the relationship between sleep timing and response to alcohol. Although the study was not primarily designed to test hypotheses regarding sleep, strengths of the study include laboratory-based alcohol administration and assessment of sleep timing over multiple days under naturalistic conditions
- 53.Johnson EO, et al. , Epidemiology of alcohol and medication as aids to sleep in early adulthood. Sleep, 1998. 21(2): p. 178–86. [DOI] [PubMed] [Google Scholar]
- 54.Ancoli-Israel S and Roth T, Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep, 1999. 22: p. S347–53. [PubMed] [Google Scholar]
- 55.Alvaro PK, Roberts RM, and Harris JK, A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep, 2013. 36(7): p. 1059–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kushner MG, Abrams K, and Borchardt C, The relationship between anxiety disorders and alcohol use disorders: a review of major perspectives and findings. Clinical psychology review, 2000. 20(2): p. 149–171. [DOI] [PubMed] [Google Scholar]
- 57.Kushner MG, et al. , Anxiety mediates the association between anxiety sensitivity and coping-related drinking motives in alcoholism treatment patients. Addictive Behaviors, 2001. 26(6): p. 869–885. [DOI] [PubMed] [Google Scholar]
- 58.Zack M, et al. , Effects of Drink-Stress Sequence and Gender on Alcohol Stress Response Dampening in High and Low Anxiety Sensitive Drinkers. Alcoholism: Clinical and Experimental Research, 2007. 31(3): p. 411–422. [DOI] [PubMed] [Google Scholar]
- *59.Roehrs T, et al. , Ethanol as a hypnotic in insomniacs: self administration and effects on sleep and mood. Neuropsychopharmacology, 1999. 20(3): p. 279–286. [DOI] [PubMed] [Google Scholar]; Insomnia may be an important moderator of alcohol response, with some evidence that individuals with insomnia benefit more from the sleep-promoting and anxiolytic properties of alcohol. Still, this rigorous lab-based study suggests that alcohol remains a poor choice for a sleep aid even among individuals with insomnia, reporting that they develop increasing tolerance to alcohol’s sleep promoting effects over subsequent days of alcohol use, while simultaneously pursuing larger doses of alcohol.
- 60.Brower KJ, Insomnia, alcoholism and relapse. Sleep medicine reviews, 2003. 7(6): p. 523–539. [DOI] [PubMed] [Google Scholar]
- *61.McGowan NM and Coogan AN, Sleep and circadian rhythm function and trait impidsivity: An actigraphy study. Psychiatry research, 2018. 268: p. 251–256. [DOI] [PubMed] [Google Scholar]; This study used wrist actigraphy to obtain an objective assesmsent of sleep-wake patterns and also employed a well-established nonparametric approach to calculate circadian parameters of the rest-activity data. After dividing the adults sample into low and high impulsivity based on the Barrett Impulsiveness Scale, they found that the high impulsivity group exhibited later sleep timing, less sleep, worse sleep efficiency, and disturbances on the circadian measures, all consistent with the sleep/circadian risk phenotype discussed in the present review paper.
- 62.Dick DM, et al. , Understanding the construct of impidsivity and its relationship to alcohol use disorders. Addiction biology, 2010. 15(2): p. 217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63*.Fucito LM, et al. , Reciprocal variations in sleep and drinking over time among heavy-drinking young adults. J Abnorm Psychol, 2018. 127(1): p. 92–103. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper is notable for its intensive monitoring of sleep (via actigraphy) and alcohol use in 42 heavy-drinking young adults over seven days. More such ecological momentary assessment designs are needed in this area to understand the proximal, and apparently bidirectional associations, between sleep and alcohol use.
- 64.Malone SK, et al. , Differences in morning-evening type and sleep duration between Black and White adults: Results from a propensity-matched UK Biobank sample. Chronobiology International, 2017: p. 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Roenneberg T, et al. , Epidemiology of the human circadian clock. Sleep Medicine Reviews, 2007. 11(6): p. 429–438. [DOI] [PubMed] [Google Scholar]
- 66.Zhang B and Wing Y, Sex differences in insomnia: a meta-analysis. SLEEP, 2006. 29(1): p. 85–93. [DOI] [PubMed] [Google Scholar]
- 67.Nolen-Hoeksema S, Gender differences in risk factors and consequences for alcohol use and problems. Clinical psychology review, 2004. 24(8): p. 981–1010. [DOI] [PubMed] [Google Scholar]
- 68.Zapolski TC, et al. , Less drinking, yet more problems: understanding African American drinking and related problems. Psychological bulletin, 2014. 140(1): p. 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Petrov ME and Lichstein KL, Differences in sleep between black and white adults: an update and future directions. Sleep medicine, 2016. 18: p. 74–81. [DOI] [PubMed] [Google Scholar]
- 70*.Mathew GM, Hale L, and Chang A-M, Sex Moderates Relationships Among School Night Sleep Duration, Social Jetlag, and Depressive Symptoms in Adolescents. Journal of biological rhythms, 2019: p. 0748730419828102. [DOI] [PMC free article] [PubMed] [Google Scholar]; Although sex as a moderating factor linking sleep and circadian disturbance with adverse health outcomes has been understudied, this paper underscores its importance, suggesting that females may be relatively more vulnerable to sleep/circadian-related risk for depression.
- 71.Antúnez JM, Navarro JF, and Adan A, Morningness–eveningness and personality characteristics of young healthy adults. Personality and Individual Differences, 2014. 68: p. 136–142. [Google Scholar]
- 72.Broms U, et al. , Evening types are more often current smokers and nicotine-dependent-a study of Finnish adult twins. Addiction, 2011. 106(1): p. 170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hsu C-Y, et al. , Associations between chronotypes, psychopathology, and personality among incoming college students. Chronobiology International, 2012. 29(4): p. 491–501. [DOI] [PubMed] [Google Scholar]
- 74*.Rognmo K, et al. , Gender differences in the bidirectional relationship between alcohol consumption and sleeplessness: the Tromso study. BMC public health, 2019. 19(1): p. 444. [DOI] [PMC free article] [PubMed] [Google Scholar]; Based on a longitudinal (>10 years) dataset, this paper reports that only males show bidirectional associations between disturbed sleep and alcohol use: higher alcohol use at T1 and/or increasing alcohol use from T1 to T2 predicted worse sleep at T2, and worse sleep at T1 or worsening sleep from T1 to T2 predicted higher alcohol use at T2. No sleep-alchool associations were observed among the female participants.
- 75.Arnedt JT, et al. , Cognitive-behavioral therapy for insomnia in alcohol dependent patients: a randomized controlled pilot trial. Behav Res Ther, 2011. 49(4): p. 227–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Currie SR, et al. , Randomized controlled trial of brief cognitive-behavioural interventions for insomnia in recovering alcoholics. Addiction, 2004. 99(9): p. 1121–1132. [DOI] [PubMed] [Google Scholar]
- 77*.Fucito LM, et al. , Using sleep interventions to engage and treat heavy-drinking college students: A randomized pilot study. Alcoholism: Clinical and Experimental Research, 2017. 41(4): p. 798–809. [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper reports the effectiveness of sleep-focused treatment as a strategy to engage heavy drinking adolescents/young adults, who otherwise might not pursue treatment. This study also suggests that sleep treatments are effective in improving sleep and alcohol-related outcomes in younger drinkers.
- 78.Fucito LM, et al. , Perceptions of heavy-drinking college students about a sleep and alcohol health intervention. Behavioral sleep medicine, 2015. 13(5): p. 395–411. [DOI] [PMC free article] [PubMed] [Google Scholar]


