Abstract
Individuals with attention-deficit/hyperactivity disorder (ADHD) frequently have sleep disturbances, daytime sleepiness, and/or circadian rhythm abnormalities. This article reviews recent advancements and key future directions: examining group differences across the life span, advancing a developmental psychopathology perspective, moving from correlation to causation, conceptualizing ADHD as a 24-hour disorder, understanding sleep in relation to other health behaviors, and evaluating sleep in interventions for individuals with ADHD. This is an exciting time in the empirical study and clinical care of sleep disturbances and circadian rhythm alterations in individuals with ADHD. As research continues to advance, studies are increasingly using large samples and longitudinal/experimental research designs to test hypotheses that will ultimately allow for a more robust and sophisticated understanding of sleep and ADHD.
Keywords: attention-deficit/hyperactivity disorder, chronobiology, chronotype, circadian rhythm, daytime sleepiness, developmental psychopathology, intraindividual variability, sleep
Introduction
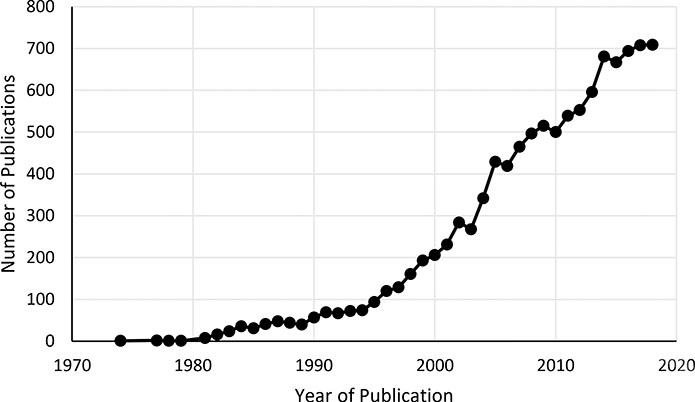
Despite long-standing interest in the co-occurrence of attention-deficit/hyperactivity disorder (ADHD) and sleep disturbances, empirical investigation of these two topics has only intensified in recent years. A simple literature search indicates that the research on ADHD and sleep has grown – and continues to grow – at a rapid pace. As shown in Figure 1, the literature on ADHD and sleep steadily grew from the mid-1970s through the mid-1990s (“restless sleep” was a symptom for diagnosing ADHD in the DSM-III, though removed when the DSM-III-R was published in 1987), and then started to accumulate at an increasingly fast rate. Of the 10,632 total publications from 1970–2018, a third (3,459) were published in just the last five years alone. The size and scope of this literature has led to a recent book devoted entirely to ADHD and sleep [1]. Needless to say, this is an exciting time for research in this area, yet it is also difficult (nay, impossible) to stay informed of the many advancements across this diverse field. In this article I prioritize research conducted in the past two years to highlight select key issues and future directions to advance the empirical understanding and clinical care of ADHD and sleep.
Figure 1. Number of publications between 1970 and 2018 that include sleep and attention-deficit/hyperactivity disorder (ADHD) in the title.
Note. Search conducted in PubMed on May 31, 2019. Search set to identify any publication with sleep and ADHD (or related terms such as attention-deficit/hyperactivity disorder, attention deficit disorder, hyperkinetic disorder, or hyperkinetic reaction of childhood) in the publication title (total publication N = 10,632).
Establishing Group Differences across the Life Span
As with most areas of ADHD research, early research on ADHD and sleep focused almost entirely on school-aged children. A decade ago, a seminal meta-analysis of this research documented that children with ADHD have significantly more impaired sleep compared to their healthy peers across most subjective sleep domains (e.g., bedtime resistance, sleep onset, night and morning wakings, daytime sleepiness) and some objective sleep parameters (e.g., actigraphy-measured sleep onset latency and sleep time; polysomnography-measured sleep efficiency; sleepiness based on average time to fall asleep for the Multiple Sleep Latency Test [MSLT]) [2]. However, until recently, the extent to which adolescents and adults with ADHD had more sleep disturbances than their same-age counterparts was largely unknown. Substantial progress has been made in this regard in recent years, allowing for a better understanding of sleep and ADHD across the life span.
Adolescence is a time of rapid neurobiological, developmental, and socio-contextual changes known to impact and be impacted by sleep [3]. Shortened sleep and sleep disturbances become increasingly common in adolescence, and it is important to know if adolescents with ADHD continue to have poorer sleep compared to their peers during this developmental stage. A systematic review concluded that sleep disturbances are associated with ADHD (and ADHD symptoms) in adolescence, though studies reported mixed findings and were generally limited by small or non-representative samples, non-standardized sleep and/or ADHD measures, and cross-sectional designs [4]. Recent studies have begun to advance the knowledge base regarding sleep in adolescents with ADHD. We examined sleep in a large sample of eighth-grade adolescents with (n=162) and without (n=140) ADHD [5•]. Adolescents with ADHD were more likely than comparison adolescents to obtain insufficient sleep on school days (per sleep diary) and on weekends (per both diary and actigraphy), and to report staying up all night in the previous two weeks (14% and 5%, respectively). Further, we found that even after controlling for a number of variables known to impact sleep (e.g., sex, pubertal development, other psychiatric disorders, medication use), ADHD was associated with shorter school night sleep duration, greater daytime sleepiness, and more sleep disturbance [5•]. These findings indicate that even during a developmental stage when sleep problems and daytime sleepiness are elevated across the population, individuals with ADHD are still more likely than their peers to have poor sleep and increased sleepiness. Recent cross-sectional studies point to the possible roles of nighttime media use [6], general technology use [7], and sleep hygiene [8] as possible factors that may contribute to sleep problems in adolescents with ADHD. Other factors that will be important to investigate include academic and organization/homework problems, comorbid psychopathologies and emotion dysregulation, caffeine and substance use, and family and peer difficulties. These factors have received surprisingly little research attention in samples of individuals carefully diagnosed with ADHD [1], and studies are needed to test both independent and joint effects. It will likewise be important to examine sleep as a predictor of adjustment in adolescents with ADHD, including consideration of domains that typically emerge in adolescence (e.g., driving, substance use) or increase in adolescence (e.g., depression, suicidality). One longitudinal study found sleep problems to predict increases in depressive and oppositional defiant symptoms, but not anxiety symptoms, one year later in adolescents with ADHD [9]. Given the complexities and possible transactional processes, longitudinal studies with multiple timepoints are especially needed to examine predictors, consequences, and bi-directional pathways involving sleep and sleepiness in adolescents with ADHD. As just one example, organization problems may lead to sleep being displaced by other tasks, and poor or insufficient sleep may in turn lead to poorer attention in class and greater academic difficulties.
Growing attention has also been devoted to sleep in adults with ADHD, and the first meta-analysis of sleep in adults with ADHD was recently conducted [10••]. Findings were largely consistent with meta-analytic findings in children, with adults with ADHD having poorer sleep than adults without ADHD across most subjective sleep domains but few group differences in objective sleep parameters. Adults with ADHD differed from adults without ADHD on two actigraphy-derived parameters: sleep onset latency and sleep efficiency. Although the meta-analysis found no group differences on any of the polysomnography-derived parameters examined, the authors noted that few studies were available to examine certain parameters (e.g., apnea-hypopnea index; time to tall asleep during the MSLT). Studies are also needed to examine sleep microarchitecture (e.g., slow waves, sleep spindles), medication and comorbidity effects, and other factors that may underlie subjective sleep problems in adults with ADHD [10••]. In considering rates of subjective sleep disturbances, it is clear that insomnia is more prevalent in adults with ADHD than adults without ADHD [11]. For instance, a large study recently conducted in Norway found 66.8% of adults with ADHD met established cutoff criteria for insomnia, compared to 28.8% of adults without ADHD [12]. Another study of adults with clinically-elevated ADHD symptoms found 43% to report significant insomnia symptoms, 41% to report short sleep duration, and 6% to report long sleep duration [13]. These studies found current inattentive symptoms [12] or both inattentive and hyperactive-impulsive symptoms [13] to be associated with insomnia. These findings appear to be consistent with a longitudinal study that found children with ADHD to have poorer sleep quality in young adulthood, but only among those whose ADHD persisted into adulthood [14•].
Advancing a Developmental Psychopathology Perspective
There is growing evidence that ADHD is associated with poor sleep, especially via subjective reports, across the lifespan. A crucial next step is for longitudinal research that uses a developmental psychopathology framework to understand the interplay of ADHD, sleep, and adjustment [15,16]. Understanding group differences is certainly valuable, but it will be increasingly important for researchers to move beyond group comparisons to examine why individuals with ADHD are at heightened risk for sleep problems, how sleep problems emerge and change over time for individuals with ADHD, who with ADHD is most at risk for developing and having persistent sleep problems, and which functional outcomes are most impacted by disturbed sleep in individuals with ADHD. For example, attention, mood, and emotion regulation may be particularly impacted by inadequate or poor sleep among individuals with ADHD, whereas the impact on anxiety or social functioning may be less pronounced. In addition, there may be certain subgroups of individuals with ADHD who are more susceptible than other subgroups to the impact of insufficient/poor sleep (e.g., individuals with executive function deficits) or more likely to develop sleep problems (e.g., individuals with co-occurring internalizing psychopathology). Toward this end, both person-centered and variable-centered approaches will be important to develop a more complete understanding of sleep and ADHD across development.
A developmental psychopathology framework is especially important to understand sleep disturbances in ADHD within the context of normative sleep development. For example, seven-week-old boys at familial risk for ADHD have less stable sleep patterns (i.e., greater inconsistency from day-to-day in the amount of quiet sleep and number of awakenings) during the daytime sleep stability than comparison infants [17]. Of note, group differences were specific to daytime sleep patterns (as opposed to 24-hour periods or nighttime sleep), which the authors hypothesized may point to the role of parenting behaviors, perhaps via a disorganized environment and ways in which the sleep-wake cycle is handled [17]. More studies are needed that examine sleep and ADHD risk in early childhood, including environmental contributions, which may shed light on developmental pathways to disturbed sleep in children at risk for ADHD who do and do not go on to have the disorder. Studies using a developmental psychopathology framework are also well-suited to examine both biological and environmental contributions to sleep problems in individuals with or at risk for ADHD [14•]. Relatedly, it will be important for studies to examine not only individuals with ADHD who experience sleep disturbances, but also individuals with ADHD who do not experience sleep problems. A risk and resilience framework can be used to test mechanisms and moderators that are crucial to building theoretical models of the co-occurrence and differentiation of ADHD and sleep disturbances.
Moving from Correlation to Causation
Most studies examining ADHD and sleep have been correlational, even as it has long been noted that ADHD and sleep disturbances are intricately intertwined [18–20]. Three studies have used experimental sleep protocols to examine whether shortened sleep duration is a causal contributor to functioning in youth diagnosed with ADHD. First, Gruber et al. [21] found moderate sleep restriction led to poorer performance on a Continuous Performance Test (CPT) in both children (ages 7–11 years) with (n = 11) and without (n = 32) ADHD, such that children with ADHD had deterioration that reached clinical levels of CPT-assessed inattention. The other two studies were both published within the last year. Cremone-Caira et al. [22] examined the impact of sleep duration on inhibitory control using a Go/No-Go task in children (ages 6–9 years) with (n = 11) and without (n = 15) ADHD. Findings indicated that inhibitory control improved by more than 13% from baseline when children with ADHD extended their overnight sleep duration [22].
We recently conducted an experimental sleep study examining a broader array of functioning domains, and also focused on adolescents with ADHD [23••]. Forty-eight adolescents successfully completed the three-week sleep protocol which consisted of a phase stabilization week, followed in randomized counterbalanced order by one week of sleep restriction (6.5 hours in bed) and one week of sleep extension (9.5 hours in bed). Compared to the extended sleep week, parents reported more inattentive and oppositional behaviors and both adolescents and parents reported more sluggish cognitive tempo symptoms and greater daytime sleepiness during the restricted sleep week. In contrast to Gruber et al. [21], no effects were found for CPT performance. Nevertheless, this study provides the first evidence that shortened sleep duration is causally linked to poorer daytime functioning in adolescents with ADHD [23••]. Additional experimental studies are certainly needed, with attention to the possible impact of cumulative restricted sleep and measures that can be kept masked to sleep conditions (e.g., teacher ratings).
Conceptualizing ADHD as a 24-Hour Disorder
Given the scope of daytime and nighttime difficulties linked to ADHD, and their interrelations, it is increasingly clear that ADHD should be conceptualized as a 24-hour disorder. ADHD is characterized by substantial variability, and despite mixed findings there is also evidence that ADHD is associated with high intraindividual variability of sleep/wake patterns [24]. For instance, in the same sample of eighth-grade adolescents described above [5•], we found adolescents with ADHD to have more variable sleep/wake patterns than their peers without ADHD using both actigraphy and daily sleep diaries [25]. An important next step is to evaluate predictors and consequences of sleep/wake variability in youth and adults with ADHD.
In addition, there is appreciable attention being devoted to investigating possible circadian rhythm alterations in individuals with ADHD. Although more studies are needed across development, individuals with ADHD may be more likely to have an evening circadian preference and later chronotype [26, 27, 28••]. Further, adults with ADHD with co-occurring sleep-onset insomnia have a delayed melatonin onset assessed using dim light melatonin onset (DLMO, a marker for the circadian pacemaker) compared to either healthy controls or adults with ADHD without insomnia [29]. Similar DLMO findings have been reported in children with ADHD [30]. Advancing our understanding of the interplay of genetic, neural, homeostatic, and circadian systems in relation to ADHD is a key research priority [19]. For instance, it has been hypothesized that a delayed circadian rhythm phase may be one cause of ‘late-onset’ ADHD in adolescence [31•], an intriguing possibility in need of empirical investigation.
Understanding Sleep in Relation to Other Health Behaviors
An important direction for research is to examine sleep in the context of other health behaviors in individuals with ADHD. ADHD is associated with a range of health behaviors, including more dangerous driving, less physical activity, poorer nutrition and increased obesity, greater alcohol/substance use, and risky sexual behaviors [32–35]. Although the data are more conclusive in some of these areas compared to others, there is a pressing need to develop integrated models of health-related behaviors in ADHD. Sleep should certainly be included in such work, as many health behaviors are themselves interrelated either directly, bidirectionally, or in a spillover and cascading fashion. An important direction for new research is to examine the interplay of sleep and other health behaviors among individuals with ADHD.
Evaluating Sleep in Existing and Novel Interventions
A recent meta-analysis confirms that methylphenidate treatment is associated with sleep problems and several types of insomnia [36]. However, the degree to which medication impacts sleep in individuals with ADHD is a complex issue with key considerations including whether there were pre-existing sleep disturbances, dose and formulation of the medication, and length of treatment [37]. Further, recent studies conducted in children [38] and adults [12] with ADHD have called into question the notion that stimulant treatment invariably worsens sleep, underscoring the need for studies that aim to delineate which individuals with ADHD are most likely to develop sleep problems following medication initiation and/or have sleep problems persist following medication titration. There is growing evidence that melatonin reduces sleep onset delay and lengthens total sleep time in youth with ADHD [39,40]. Still, the evidence base remains small, and existing studies have a high degree of heterogeneity and/or limited sample sizes.
Behavioral interventions are recommended as the first-line treatment of insomnia, but until quite recently trials of behavioral sleep interventions in ADHD samples had not been conducted [39]. Studies have begun to address this gap, at least in school-aged children with ADHD [41–46]. Specifically a team of researchers in Australia have conducted a series of randomized controlled trials (RCTs) examining brief behavioral interventions for children with ADHD and co-occurring sleep problems [41–43, 44••]. The initial pilot RCT demonstrated feasibility and acceptability, as well as improvements in sleep and, for participants who received 2–3 sessions (as opposed to 1 session), improvements in children’s quality of life and daily functioning in addition to parent anxiety [41]. The investigators then conducted a large-scale efficacy trial with three-month, six-month [42], and 12-month [43] outcome assessments. The brief sleep hygiene + behavioral strategies intervention had a modest improvement on ADHD symptoms and also improved children’s sleep, behavior, and quality and life, with most effects sustained at the six-month follow-up [42]. Compared to usual clinical care, children who received the intervention were less likely to have moderate/severe sleep problems and had better daytime functioning at the 12-month follow-up [43]. However, sustained effects were small and the intervention was less effective for children who were not taking ADHD medication and for children who had parents experiencing depressive symptoms [43]. A recent cluster-randomized translational trial found that a brief, low-cost sleep intervention can be delivered by community clinicians and improve sleep in children with ADHD, though effects unfortunately did not extend to other domains of child and parent functioning [44••]. Together, these studies indicate that brief, behavioral-focused sleep interventions can be provided to families of children with ADHD with relatively low burden and cost. Nevertheless, additional work is needed to extend and optimize effects. For example, it is possible that a brief intervention will be sufficient for some families, whereas other families may need a more intensive intervention [47]. Similarly, which sleep disturbances remit following non-sleep-focused evidence-based treatments, and which are most likely to persist? Questions such as these may be optimally addressed using a sequential, multiple assignment, randomized trial (SMART). To be sure, there has been substantial progress in beginning to evaluate behavioral sleep interventions for children with ADHD, though there is still much work to do, including evaluating cognitive-behavioral sleep interventions in adolescents and adults with ADHD.
Conclusions
This is an exciting time in the empirical study and clinical care of sleep disturbances and circadian rhythm alterations in children, adolescents, and adults with ADHD. As research continues to advance, studies are increasingly using large samples and longitudinal/experimental designs to test hypotheses that will ultimately allow for a more robust and sophisticated understanding of sleep and ADHD. Still, far more work is needed, including in many areas not discussed herein given space limitations. This is thus an opportune time for investigators and clinicians interested in sleep and ADHD, including junior and senior investigators alike. If you haven’t already, I invite you to join in studying this area of major theoretical and clinical importance. You don’t have to decide now, feel free to sleep on it.
Acknowledgments
Funding: Stephen Becker is currently supported by grant number K23MH108603 from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health (NIH).
Footnotes
Conflict of interest statement: None declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References and recommended reading
Papers of particular interest, published within the period of review, have been highlighted as:
• of special interest
•• of outstanding interest
- 1.Hiscock H, Sciberras E (Ed): Sleep and ADHD: An evidence-based guide to assessment and treatment San Diego, CA: Elsevier/Academic Press; 2019. [Google Scholar]
- 2.Cortese S, Faraone SV, Konofal E, Lecendreux M: Sleep in children with attention-deficit/hyperactivity disorder: Meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry 2009, 48:894–908. [DOI] [PubMed] [Google Scholar]
- 3.Crowley SJ, Wolfson AR, Tarokh L, Carskadon MA: An update on adolescent sleep: New evidence informing the perfect storm model. J Adolesc 2018, 67:55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lunsford-Avery JR, Krystal AD, Kollins SH: Sleep disturbances in adolescents with ADHD: A systematic review and framework for future research. Clin Psychol Rev 2016, 50:159–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Becker SP, Langberg JM, Eadeh HM, Isaacson PA, Bourchtein E: Sleep and daytime sleepiness in adolescents with and without ADHD: Differences across ratings, daily diary, and actigraphy. J Child Psychol Psychiatry 2019.• This is the largest study to date to examine sleep and sleepiness in adolescents with and without ADHD, using multiple informants and sleep measures. The sample was comprised of eighth-grade adolescents (mean age = 13 years) with (n = 162) and without (n = 140) ADHD recruited from two sites in the United States. Ratings were collected from adolescents, parents, and teachers, and adolescents wore an actigraph and completed a daily sleep diary for approximately two weeks. Comapred to adolescents without ADHD, adolescents with ADHD were more likely to report falling asleep in class and to have stayed up all night at least twice in the previous two weeks. When controlling for several variables known to impact sleep, ADHD remained associated with shorter diary and actigraphy school night sleep duration, adolescent- and parent-reported daytime sleepiness, and parent-reported difficulties initiating and maintaining sleep and total sleep disturbance. Controlling for other variables, the odds of being classified with clinically elevated parent-reported sleep disturbance were 6.20 times greater for adolescents with ADHD.
- 6.Becker SP, Lienesch JA: Nighttime media use in adolescents with ADHD: links to sleep problems and internalizing symptoms. Sleep Medicine 2018, 51:171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bourchtein E, Langberg JM, Cusick CN, Breaux RP, Smith ZR, Becker SP: Technology use and sleep in adolescents with and without attention-deficit/hyperactivity disorder. J Pediatr Psychol 2019, 44:517–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martin CA, Hiscock H, Rinehart N, Heussler HS, Hyde C, Fuller-Tyszkiewicz M, McGillivray J, Austin DW, Chalmers A, Sciberras E: Associations between sleep hygiene and sleep problems in adolescents with ADHD: A cross-sectional study. J Atten Disord 2018:1087054718762513. [DOI] [PubMed] [Google Scholar]
- 9.Becker SP, Langberg JM, Evans SW: Sleep problems predict comorbid externalizing behaviors and depression in young adolescents with attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry 2015, 24:897–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Díaz-Román A, Mitchell R, Cortese S: Sleep in adults with ADHD: Systematic review and meta-analysis of subjective and objective studies. Neurosci Biobehav Rev 2018, 89:61–71.•• This is the first systematic review and meta-analysis of studies examining subjective and objective sleep parameters in adults diagnosed with ADHD. To be included, participants had to have an ADHD diagnosis established according to ICD or DSM criteria, and studies had to also include a comparison group of adults without ADHD. Thirteen studies were included. Compared to adults without ADHD, adults with ADHD significantly differed in seven out of nine subjective parameters: night awakenings, daytime sleepiness, sleep onset latency, psychosomatic symptoms during sleep onset, sleep quality, sleep efficiency, and general sleep problems (no differences in sleep duration or restorative value of sleep). The groups differered on two out of five actigraphic parameters: sleep onset latency and sleep efficiency (no differences in true sleep, assumed sleep time, or actual wake time). No group differences were found on any of the nine polysomnography parameters. The authors concluded that ADHD in adulthood is associated with subjectively reported sleep problems but more research is needed to examine if these subjective problems are underpinned by objective sleep alterations. No more than four studies were available for all objective parameters and most subjective parameters, underscoring the need for additional studies of sleep in adults carefully diagnosed with ADHD.
- 11.Wynchank D, Bijlenga D, Beekman AT, Kooij JJS, Penninx BW: Adult attention-deficit/hyperactivity disorder (ADHD) and insomnia: An update of the literature. Curr Psychiatry Rep 2017, 19:98. [DOI] [PubMed] [Google Scholar]
- 12.Brevik EJ, Lundervold AJ, Halmoy A, Posserud MB, Instanes JT, Bjorvatn B, Haavik J: Prevalence and clinical correlates of insomnia in adults with attention-deficit hyperactivity disorder. Acta Psychiatr Scand 2017, 136:220–227. [DOI] [PubMed] [Google Scholar]
- 13.Wynchank D, Ten Have M, Bijlenga D, Penninx BW, Beekman AT, Lamers F, de Graaf R, Kooij JJS: The association between insomnia and sleep duration in adults with attention-deficit hyperactivity disorder: Results from a general population study. J Clin Sleep Med 2018, 14:349–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gregory AM, Agnew-Blais JC, Matthews T, Moffitt TE, Arseneault L: ADHD and sleep quality: Longitudinal analyses from childhood to early adulthood in a twin cohort. J Clin Child Adolesc Psychol 2017, 46:284–294.• This study included 2,232 twin children in the Environmental Risk Longitudinal Twin Study in the United Kingdom. ADHD was assessed at ages 5, 7, 10, 12, and 18 years, and subjectively-reported sleep quality was assessed at age 18. Children with ADHD had poorer sleep quality in early adulthood, but only if there ADHD persisted. Adults with remitted ADHD did not differ from adults without ADHD in sleep quality. ADHD and poorer sleep quality in early adulthood were associated because of genetic (55%) and nonshared environmental (45%) influences. Additional longitudinal studies are needed that include additional sleep measures.
- 15.Becker SP, Langberg JM, Byars KC: Advancing a biopsychosocial and contextual model of sleep in adolescence: a review and introduction to the special issue. J Youth Adolesc 2015, 44:239–270. [DOI] [PubMed] [Google Scholar]
- 16.Meltzer LJ: Future directions in sleep and developmental psychopathology. J Clin Child Adolesc Psychol 2017, 46:295–301. [DOI] [PubMed] [Google Scholar]
- 17.Landau R, Sadeh A, Vassoly P, Berger A, Atzaba-Poria N, Auerbach JG: Sleep patterns of 7-week-old infants at familial risk for attention deficit hyperactivity disorder. Infant Mental Health Journal 2010, 31:630–646. [DOI] [PubMed] [Google Scholar]
- 18.Dahl RE: The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology 1996, 8:3–27. [Google Scholar]
- 19.Owens JA, Gruber R, Brown T, Corkum P, Cortese S, O’Brien L, Stein M, Weiss M: Future research directions in sleep and ADHD: report of a consensus working group. J Atten Disord 2013, 17:550–564. [DOI] [PubMed] [Google Scholar]
- 20.Lundahl A, Kidwell KM, Van Dyk TR, Nelson TD: A meta-analysis of the effect of experimental sleep restriction on youth’s attention and hyperactivity. Developmental Neuropsychology 2015, 40:104–121. [DOI] [PubMed] [Google Scholar]
- 21.Gruber R, Wiebe S, Montecalvo L, Brunetti B, Amsel R, Carrier J: Impact of sleep restriction on neurobehavioral functioning of children with attention deficit hyperactivity disorder. Sleep 2011, 34:315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cremone-Caira A, Root H, Harvey EA, McDermott JM, Spencer RMC: Effects of sleep extension on inhibitory control in children with ADHD: A pilot study. J Atten Disord 2019:1087054719851575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Becker SP, Epstein JN, Tamm L, Tilford AA, Tischner CM, Isaacson PA, Simon JO, Beebe DW: Shortened sleep duration causes sleepiness, inattention, and oppositionality in adolescents with attention-deficit/hyperactivity disorder: Findings from a crossover sleep restriction/extension study. J Am Acad Child Adolesc Psychiatry 2019, 58:433–442.•• This study used an experimental sleep restriction/extension protocol to investigate whether shortened sleep duration is causally linked to sleepiness, inattention, and behavioral functioning in adolescents diagnosed with ADHD. Seventy-two adolescents (ages 14–17 years) entered a three-week sleep protocol using an experimental crossover design. The protocol included a phase stabilization week, followed in randomized counterbalanced order by one week of sleep restriction (6.5 hours in bed) and one week of sleep extension (9.5 hours in bed). Sleep was monitored with actigraphy and daily sleep diaries, with laboratory visits at the end of each week. Analyses included 48 adolescents who had complete actigraphy data and successfully completed the sleep protocol (defined a priori as obtaining ≥1 hour actigraphy-measured sleep duration during extension compared to restriction). Compared to the extended sleep week, parents reported more inattentive and oppositional symptoms during the restricted sleep week, and both parents and adolescents reported more sluggish cognitive tempo symptoms and greater daytime sleepiness. No effects were found for parent-reported hyperactivity-impulsivity, adolescent-reported ADHD inattention, or Continuous Performance Test parameters. This study provides the first evidence that sleep duration is a causal contributor to daytime behaviors in adolescents with ADHD and suggests that sleep may be an important target for intervention in adolescents with ADHD.
- 24.Becker SP, Sidol CA, Van Dyk TR, Epstein JN, Beebe DW: Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep Med Rev 2017, 34:94–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Langberg JM, Breaux RP, Cusick CN, Green CD, Smith ZR, Molitor SJ, Becker SP: Intraindividual variability of sleep/wake patterns in adolescents with and without attention-deficit/hyperactivity disorder. Journal of Child Psychology & Psychiatry 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Snitselaar MA, Smits MG, van der Heijden KB, Spijker J: Sleep and circadian rhythmicity in adult ADHD and the effect of stimulants: A review of the current literature. J Atten Disord 2017, 21:14–26. [DOI] [PubMed] [Google Scholar]
- 27.Gruber R, Fontil L, Bergmame L, Wiebe ST, Amsel R, Frenette S, Carrier J: Contributions of circadian tendencies and behavioral problems to sleep onset problems of children with ADHD. BMC Psychiatry 2012, 12:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coogan AN, McGowan NM: A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. Attention Deficit and Hyperactivity Disorders 2017, 07:07.•• This systematic review provides a thorough overview of research examining the role of circadian dysfucntion in the sleep problems associated with ADHD, as well as how circadian processes and dysfunction may contribute to etioloy and/or symptomatology of ADHD. Sixty-two studies were included in this review, including 25 studies in adults and 37 studies in children/adolescents. Consistent findings were found between delayed circadian phase and later chronotype/evening preference in relation to ADHD/ADHD symptoms. The authors highlight the importance of examining chronotherapeutic approaches to “correct” underlying phase alterations and, ultimately, reducing ADHD symptoms. Also, most studies have used melatonin as a somnolent and studies are needed to test melatonin to advance circadian phase in individuals with ADHD and circadian dysfunction. Finally, there is a specific need for longitudinal studies and more studies examining polymorphisms in circadian clock genes and ADHD.
- 29.Van Veen MM, Kooij JJ, Boonstra AM, Gordijn MC, Van Someren EJ: Delayed circadian rhythm in adults with attention-deficit/hyperactivity disorder and chronic sleep-onset insomnia. Biol Psychiatry 2010, 67:1091–1096. [DOI] [PubMed] [Google Scholar]
- 30.Van der Heijden KB, Smits MG, Van Someren EJ, Gunning WB: Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: a circadian rhythm sleep disorder. Chronobiol Int 2005, 22:559–570. [DOI] [PubMed] [Google Scholar]
- 31.Lunsford-Avery JR, Kollins SH: Editorial Perspective: Delayed circadian rhythm phase: A cause of late-onset attention-deficit/hyperactivity disorder among adolescents? J Child Psychol Psychiatry 2018, 59:1248–1251.• There is substantial interest and debate related to recent claims of a “late-onset” ADHD that differs from the childhood-onset neurodevelopmental disorder. In this editorial perspective, the authors put forth the intriguing hypothesis that delayed circadian rhythm phase may explain ADHD symptom onset in adolescence. The authors draw upon developmental, behavioral, neurocognitive, and genetic evidence to build their hypothesis. They further describe both direct and indirect mechanisms by which circadian rhythm misalignment in adolescence may contribute to late-onset ADHD symptoms. There are many important lines of inquiry to test the fascinating hypotheses detailed in this editorial perspective.
- 32.Holton KF, Nigg JT: The association of lifestyle factors and ADHD in children. J Atten Disord 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barkley RA, Murphy KR, Fischer M: ADHD in adults : What the science says. New York: Guilford Press; 2008. [Google Scholar]
- 34.Davis C: Attention-deficit/hyperactivity disorder: Associations with overeating and obesity. Curr Psychiatry Rep 2010, 12:389–395. [DOI] [PubMed] [Google Scholar]
- 35.Pollak Y, Dekkers TJ, Shoham R, Huizenga HM: Risk-taking behavior in attention deficit/hyperactivity disorder (ADHD): A review of potential underlying mechanisms and of interventions. Curr Psychiatry Rep 2019, 21:33. [DOI] [PubMed] [Google Scholar]
- 36.Faraone SV, Po MD, Komolova M, Cortese S: Sleep-associated adverse events during methylphenidate treatment of attention-deficit/hyperactivity disorder: A meta-analysis. J Clin Psychiatry 2019, 80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stein MA, Weiss M, Hlavaty L: ADHD treatments, sleep, and sleep problems: complex associations. Neurotherapeutics 2012, 9:509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Becker SP, Froehlich TE, Epstein JN: Effects of methylphenidate on sleep functioning in children with attention-deficit/hyperactivity disorder. J Dev Behav Pediatr 2016, 37:395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cortese S, Brown TE, Corkum P, Gruber R, O’Brien LM, Stein M, Weiss M, Owens J: Assessment and management of sleep problems in youths with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2013, 52:784–796. [DOI] [PubMed] [Google Scholar]
- 40.Abdelgadir IS, Gordon MA, Akobeng AK: Melatonin for the management of sleep problems in children with neurodevelopmental disorders: a systematic review and meta-analysis. Arch Dis Child 2018, 103:1155–1162. [DOI] [PubMed] [Google Scholar]
- 41.Sciberras E, Fulton M, Efron D, Oberklaid F, Hiscock H: Managing sleep problems in school aged children with ADHD: a pilot randomised controlled trial. Sleep Med 2011, 12:932–935. [DOI] [PubMed] [Google Scholar]
- 42.Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D, Khano S, Oberklaid F: Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: randomised controlled trial. BMJ 2015, 350:h68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sciberras E, Mulraney M, Mensah F, Oberklaid F, Efron D, Hiscock H: Sustained impact of a sleep intervention and moderators of treatment outcome for children with ADHD: a randomised controlled trial. Psychol Med 2019:1–10. [DOI] [PubMed] [Google Scholar]
- 44.Hiscock H, Mulraney M, Heussler H, Rinehart N, Schuster T, Grobler AC, Gold L, Mudiyanselage SB, Hayes N, Sciberras E: Impact of a behavioral intervention, delivered by pediatricians or psychologists, on sleep problems in children with ADHD: A cluster-randomized, translational trial. Journal of Child Psychology & Psychiatry 2019.•• This study builds upon the previous randomized clinical trials examining brief behavioral sleep interventions in children with ADHD conducted by the same research team in Australia. Those studies are also noteworthy, but this recent study is especially unique and important as it presents a rare translational trial in the study of interventions for ADHD. The researchers tested the intervention showing efficacy in their previous work to examine whether it would be effective and cost-effective when delivered in community settings by psychologists or pediatricians. Participants were 361 children (ages 5–13 years) with ADHD and parent-reported sleep problems who were randomized at the pediatrician level to usual care or the intervention which consisted of two consultations with a pediatrician or a psychologist coverering sleep hygiene and tailored behavioral strategies. Compared to children in the control condition, children in the intervention condition had fewer moderate/severe sleep problems at three months and six months, with no statistically significant difference in reduced sleep problems between chidlren treated by a psychologist or pediatrician. Children in the intervention condition also had improved sleep on a validated parent-report sleep questionnaire, though no differences were found using child- or teacher-reported sleep measures. There was also no evidence that the intervention impacted ADHD symptoms, behavior, quality of life, autism spectrum disorder symptoms, or parenting.
- 45.Corkum P, Lingley-Pottie P, Davidson F, McGrath P, Chambers CT, Mullane J, Laredo S, Woodford K,Weiss SK: Better Nights/Better Days - Distance intervention for insomnia in school-aged children with/without ADHD: A randomized controlled trial. J Pediatr Psychol 2016, 41:701–713. [DOI] [PubMed] [Google Scholar]
- 46.Keshavarzi Z, Bajoghli H, Mohamadi MR, Salmanian M, Kirov R, Gerber M, Holsboer-Trachsler E,Brand S: In a randomized case-control trial with 10-years olds suffering from attention deficit/hyperactivity disorder (ADHD) sleep and psychological functioning improved during a 12-week sleep-training program. World Journal of Biological Psychiatry 2014, 15:609–619. [DOI] [PubMed] [Google Scholar]
- 47.Becker SP: The triple threat of sleep, adolescence, and ADHD In Sleep and ADHD: An evidence-based guide to assessment and treatment. Edited by Hiscock H, Sciberras E: Elsevier/Academic Press; 2019:257–294. [Google Scholar]