Abstract
Aim
High-intensity binge drinking (HIBD), defined as two or more times the gender-specific binge threshold, is rapidly increasing in the USA; however, the underlying contributing factors are poorly understood. This study investigated the relationship of adverse childhood experiences (ACEs) and HIBD.
Methods
Two independent, cross-sectional samples were analysed: (a) past 12-month drinkers in the National Epidemiological Survey on Alcohol and Related Conditions-III (NESARC-III; n = 25,552) and (b) the National Institute on Alcohol Abuse and Alcoholism (NIAAA) clinical sample (n = 1303). Multinomial logistic regressions were utilized to estimate adjusted odds ratios (AORs) of ACEs on HIBD. Mediation analysis was performed to examine the relationship between the past 12-month psychiatric disorders, ACEs, and HIBD.
Results
In the NESARC-III sample, prevalence of ACEs increased across all binge levels with the highest prevalence in extreme HIBD; ACEs were associated with higher odds for HIBD (level II, odds ratio (OR) = 1.2–1.4; P = 0.03–0.001; level III, OR = 1.3–1.9; P < 0.001). Prevalence of DSM-5 diagnoses also increased across all binge levels. Substance use disorders (SUD), mood, personality and post-traumatic stress disorders (PTSD) conferred the highest odds with extreme HIBD (SUD: OR = 21.32; mood: 1.73; personality: 2.84; PTSD: 1.97; all Ps < 0.001). Mediation analyses showed that the association between ACEs and HIBD was fully mediated through SUD (proportion mediated: 70–90%) and partially through other psychiatric disorders (20–80%). In the NIAAA sample, ACEs were 2–5 times more prevalent in extreme HIBD with higher odds (ORs = 3–8, P < 0.001) compared with non-bingers.
Conclusion
ACEs were associated with significantly increased odds of HIBD and the relationship may be mediated by psychiatric disorders.
ACEs and comorbid psychiatric disorders are significant risk factors for HIBD, defined as two or more times the gender-specific binge threshold. Psychiatric disorders play a full or partial mediating role in the relationship between ACEs and HIBD.
INTRODUCTION
Heavy alcohol consumption is a leading cause of alcohol-associated diseases and premature deaths in the USA (Midanik et al., 2004; Mokdad et al., 2005; Lucey et al., 2009). Approximately 36% of all adults in the US ages 18 and older report episodes of binge drinking (BD) within the past year. BD is defined as reaching a blood alcohol concentration (BAC) ≥0.08%, which results in a gender-specific threshold of consuming five or more standard drinks (containing 14 g pure alcohol) on one occasion for men and four or more for women (Hingson et al., 2017). BD is a major risk factor for many acute and long-term health conditions (Charlet and Heinz, 2017) and has also been used as an indicator of dangerous alcohol consumption (Rehm et al., 2009; World Health Organization. Management of Substance Abuse Team, 2011). However, defining BD in a dichotomous way using gender-specific thresholds may obscure important information regarding heavier or more dangerous drinking behaviors and may suggest that all BD confers identical risk, regardless of how far it exceeds the threshold and how severe the consequences of the high-quantity levels are (Fish et al., 2018; Patrick and Azar, 2018).
Drinking two or more times the BD threshold is defined as high-intensity binge drinking (HIBD) which confers significant health risks. Individuals BD three times the threshold have BACs of 0.20–0.30% and often suffer from blackouts, memory loss, or overdoses. Individuals with HIBD have been shown to be at substantially increased risk of alcohol-related and other health-related consequences. While HIBD is prevalent among young adults, particularly college students (White et al., 2006), recent data indicate that the prevalence of HIBD has also increased among the general population in the last decade (Hingson et al., 2017). Although it is evident that individuals who engage in HIBD are predisposed to major public health problems, little is known about the underlying risk factors, pathophysiology and neurobiology of HIBD.
One well-studied risk factor for alcohol misuse is exposure to adverse childhood experiences (ACEs) (Brady and Back, 2012). Child abuse is common in the USA: the US Child Protective Services documented 700,000 cases of childhood sexual abuse, physical abuse and neglect in 2014 (Bynum et al., 2011). When expanding the ACE definition to include categories of household dysfunction, such as having mentally ill or incarcerated family members, or observing violence toward a mother or stepmother, approximately half of the children in the USA have experienced at least one type of trauma (Felitti et al., 1998). To date, most studies examining the association between ACEs and alcohol consumption have focused primarily on BD (Loudermilk et al., 2018), not on HIBD which might lead to more severe health consequences (Felitti et al., 1998; Bynum et al., 2011). Retrospective studies have linked ACEs with increased susceptibility to BD and alcohol use disorder (AUD) later in life (Kauhanen et al., 2011; Schwandt et al., 2013). Additionally, adolescents and young adults with ACEs report having their first drink earlier and are at a higher risk of developing psychiatric disorders compared with their peers without ACEs (Vallejos et al., 2017). Exposure to ACEs is also linked to higher odds of adulthood alcohol, opioid, and nicotine dependence, as well as depression, anxiety, suicidal behaviors, and schizophrenia (Rothman et al., 2008; Cheong et al., 2017; Cawthorpe et al., 2018; Rokita et al., 2018; Lew and Xian, 2019). However, associations between ACEs and heavy drinking that exceeds the binge threshold, associations between ACEs and comorbid psychiatric disorders among HIBD, as well as the role of psychiatric disorders in the relationship between ACEs and HIBD remain poorly understood (Regier et al., 1990; Kessler et al., 1996; Grant et al., 2004; Kessler et al., 2005; Nock et al., 2010).
In the present study, we aimed to investigate the relationship between ACEs and HIBD in a sample recruited in the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Defining HIBD as two or more times the BD threshold and extreme HIBD as three or more times the BD threshold, we estimated prevalence and odds ratio (OR) of each category of ACE among HIBD. Furthermore, we examined the association between past 12-month psychiatric diagnoses and HIBD, and explored psychiatric disorders as a mediator of the relationship between ACEs and HIBD. Our second goal was to confirm our findings in a clinical sample collected at the National Institute on Alcohol Abuse and Alcoholism (NIAAA) which was predominantly comprised of individuals with AUD.
METHODS
Sources of data
NESARC-III sample
The NESARC-III is a nationally representative survey of the non-institutionalized civilian US adult population 18 years and older. The cross-sectional samples were collected from 2012 to 2013. The detailed methodological information of sampling in NESARC-III are available elsewhere (https://www.niaaa.nih.gov/research/nesarc-iii/methodology). The final sample consisted of 25,552 respondents who reported at least one drink within the previous 12 months (Table 1). The NESARC-III survey protocol was approved by the institutional review boards of the National Institutes of Health (NIH) and Westat.
Table 1.
Frequency and prevalence of sociodemographic characteristics by alcohol binge levelsa
| Alcohol binge levelb | |||||
|---|---|---|---|---|---|
| Non-binge | Level I | Level II | Level III | P-value | |
| NESARC-III | N = 14,030 | N = 7,190 | N = 2,599 | N = 1,733 | |
| Weighted prevalence of N (%, SE) | 55.0 (0.56) | 27.6 (0.44) | 10.6 (0.29) | 6.8 (0.23) | |
| Age (years) (mean, SE) | 49.44 (0.25) | 40.54 (0.28) | 36.57 (0.38) | 33.85 (0.39) | <0.0001 |
| Age at first drink (mean, SE) | 20.93 (0.11) | 18.45 (0.08) | 17.68 (0.24) | 16.97 (0.13) | <0.0001 |
| Age at heaviest drinking (mean, SE) | 32.78 (0.23) | 28.33 (0.21) | 25.98 (0.34) | 24.80 (0.28) | <0.0001 |
| Gender: male (%, SE) | 45.1 (0.52) | 49.9 (0.71) | 69.4 (1.08) | 68.2 (1.23) | <0.0001 |
| Race | <0.0001 | ||||
| White, non-Hispanic | 68.2 (0.83) | 68.81 (0.90) | 68.97 (1.11) | 70.39 (1.38) | |
| Black, non-Hispanic | 11.9 (0.65) | 10.24 (0.64) | 7.40 (0.62) | 7.63 (0.89) | |
| American Indian | 1.30 (0.13) | 1.58 (0.20) | 2.17 (0.44) | 2.78 (0.56) | |
| Asian | 5.95 (0.46) | 3.75 (0.49) | 3.76 (0.54) | 2.86 (0.65) | |
| Hispanic | 12.63 (0.60) | 15.62 (0.77) | 17.70 (1.14) | 16.34 (1.06) | |
| Marital status (%, SE) | <0.0001 | ||||
| Married or cohabiting | 62.84 (0.70) | 56.01 (0.78) | 50.57 (1.13) | 42.51 (1.52) | |
| Widowed, separated or divorced | 20.26 (0.45) | 16.55 (0.53) | 13.22 (0.84) | 15.72 (1.12) | |
| Never married | 16.90 (0.48) | 27.44 (0.76) | 36.21 (1.17) | 41.76 (1.60) | |
| Educational attainment (%, SE) | <0.0001 | ||||
| Some high school | 9.20 (0.38) | 9.45 (0.46) | 11.18 (0.80) | 16.13 (1.19) | |
| High school graduate | 23.25 (0.67) | 22.52 (0.64) | 27.11 (1.18) | 31.94 (1.26) | |
| Some college or higher | 67.55 (0.84) | 68.03 (0.85) | 61.71 (1.37) | 51.93 (1.57) | |
| Family income, $ (%, SE) | <0.0001 | ||||
| 0–19,999 | 17.99 (0.54) | 19.79 (0.59) | 24.65 (1.20) | 30.14 (1.50) | |
| 20,000–34,999 | 17.96 (0.42) | 17.46 (0.57) | 17.00 (0.81) | 19.99 (1.18) | |
| 35,000–69,999 | 27.74 (0.53) | 26.68 (0.69) | 26.56 (0.91) | 29.18 (1.40) | |
| ≥70,000 | 36.31 (0.88) | 36.07 (0.97) | 31.80 (1.29) | 20.69 (1.32) | |
| NIAAA | N = 199 | N = 319 | N = 196 | N = 589 | |
| Frequency (%, SE) of N | 15.3 (1.0) | 24.5 (1.19) | 15.0 (0.99) | 45.2 (1.38) | |
| Age (years) (mean, SE) | 35.81 (0.91) | 33.81 (0.66) | 38.95 (0.91) | 41.99 (0.46) | <0.0001 |
| Gender: male (%, SE) | 55.28 (3.53) | 57.05 (2.78) | 64.29 (3.43) | 72.16 (1.85) | <0.0001 |
| Race | 0.01 | ||||
| White, non-Hispanic | 44.22 (3.53) | 54.86 (2.79) | 49.49 (3.58) | 47.20 (2.06) | |
| Black, non-Hispanic | 47.24 (3.55) | 34.80 (2.67) | 44.39 (3.56) | 47.20 (2.06) | |
| Asian | 5.03 (1.55) | 5.96(1.33) | 3.06 (1.23) | 2.86 (0.65) | |
| Hispanic | 1.51 (0.87) | 1.57 (0.70) | 1.53 (0.88) | 2.21 (0.61) | |
| Treatment-seeking AD (%, SE) | 2.51 (1.11) | 8.78 (1.59) | 38.27 (3.48) | 75.55 (1.77) | <0.0001 |
| Non-treatment-seeking AD (%, SE) | 1.01 (0.71) | 13.79 (1.93) | 28.06 (3.22) | 17.83 (1.58) | <0.0001 |
| Healthy volunteer (no AD) (%, SE) | 96.48(1.31) | 76.80 (2.37) | 33.67 (3.38) | 6.62 (1.03) | <0.0001 |
Abbreviation: AD, DSM-IV diagnosis of current alcohol dependence in NIAAA sample.
aFrequency or prevalence % and standard error (in parentheses) reported except where otherwise noted.
bAlcohol binge levels are gender-specific: for women, non-binge = 1–3; level I = 4–7; level II = 8–11; level III  12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III
12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III  15 drinks.
15 drinks.
NIAAA clinical sample
The NIAAA clinical sample consisted of 1,326 participants who were diagnosed using the Structured Clinical Interview for DSM-IV (First et al., 2002). Participants with alcohol dependence (AD) included both individuals seeking treatment for AD and non-treatment-seeking individuals. Detailed information is available in the Supplementary Material. All protocols were approved by the institutional review board. Informed consent was obtained in accordance with the Declaration of Helsinki.
Assessments
Adverse childhood experience
NESARC-III sample. NESARC-III used more comprehensive questions, namely ACEs, than the NIAAA clinical sample regarding childhood trauma experiences (CTEs). ACEs include categories for child abuse (sexual, physical, verbal abuse and physical and emotional neglect), as well as categories for household dysfunction consisting of witnessing a battered mother or stepmother, having a household member with a mental health or substance use disorder (SUD) or who was incarcerated, or who either attempted or committed suicide when respondents were younger than 18 years old. Detailed methodological description of ACEs and diagnoses of psychiatric disorders can be found in the Supplementary Material.
NIAAA clinical sample. The Childhood Trauma (CTQ) and Early Life Stress (ELSQ) Questionnaires were used to quantitatively assess CTEs in the NIAAA clinical sample. The CTQ is a 28-item, self-administered instrument for the retrospective assessment of childhood abuse and neglect (Bernstein et al., 2003). The five CTQ subscales comprise emotional abuse, physical abuse, sexual abuse, emotional neglect, and physical neglect. In the present study, average scores for each subscale were categorized into a binary outcome, such that a mean score of 2 or above indicates CTE exposure and a mean score below 2 indicates no exposure. The ELSQ is an 18-item assessment of exposure to specific traumatic events before age 18 (Sanders and Becker-Lausen, 1995). Subjects scoring above 2 on a CTQ subscale or endorsing the corresponding ELSQ item were considered to have a history of CTE. To be consistent with NESARC-III, CTEs were referred to as ACEs in the NIAAA clinical sample.
Alcohol binge levels
Alcohol consumption for the 90 days prior to screening or admission was assessed for the NIAAA clinical sample using the Timeline Followback (Sobell and Sobell, 1992). NESARC-III respondents reported the maximum number of drinks in a single day during the past 12 months. Consistent with current literature on high-intensity alcohol consumption (Hingson et al., 2017), four gender-specific binge levels were generated based on the maximum number of standard drinks (defined as 14 g alcohol) consumed on any single day in the survey-specified time period. For women, 4 categorized BD levels were defined as 1–3 drinks (non-binge), 4–7 drinks (level I), 8–11 drinks (level II), and 12 drinks or more (level III) in a single day. For men, the BD levels were categorized as 1–4 drinks (non-binge), 5–9 drinks (level I), 10–14 drinks (level II), and 15 drinks or more (level III). Levels I, II, and III thus correspond to one, two, and three or more times the gender-specific binary BD thresholds utilizing standard drinks ≥4 for women and ≥5 for men. HIBD was defined as two or more times the BD threshold, and extreme HIBD was defined as three or more times the BD threshold.
Statistical analysis
The NESARC-III and NIAAA samples were analysed separately due to differences in study design. The data analysis proceeded in two steps: first, the NESARC-III data was analysed to identify associations between each category of ACEs and binge levels. The NIAAA clinical data was then used to confirm the findings observed in the NESARC-III sample.
NESARC-III sample
Weighted cross-tabulations estimated the prevalence of sociodemographic characteristics and the 10 ACEs for each binge level. We also estimated the prevalence rates of past 12-month SUD and psychiatric disorders at the given binge level to describe prevalence of comorbidities. The weighted prevalence was compared across four binge groups using Rao-Scott Chi-Square Test and the weighted mean of age, age at onset of drinking, and age at the heaviest drinking across binge levels were also tested using a weighted regression model that was equivalent to a weighted analysis of variance. Adjusted odds ratios (AORs) were derived from multivariable multinomial logistic regression models that tested for associations between each ACE as an explanatory variable (e.g. sexual abuse) and BD levels as a response variable after controlling for age, gender, race, marital status, education attainment, and family income listed in Table 1. Consistent with the analyses for BD levels, multivariable logistic regression models were utilized for the relationship between each ACE and psychiatric disorders (e.g. AUD). The weights derived from the complex design of NESARC-III were incorporated into all analyses using SUDAAN, version 11.0.
Mediation analysis
As an exploratory analysis, mediation analysis was performed to test if an explanatory variable (X, e.g. sexual abuse) is associated with a response variable (Y, e.g. BD levels), indirectly through a third mediating variable (M, e.g. SUD). Based on a single mediator approach with three separate multinomial logistic regression models (Fig. 1), we defined a as an effect of an explanatory variable (X) on a mediating variable (M), b as an effect of a mediating variable (M) to a response variable (Y), c as a total effect of an explanatory variable X to a response variable Y, and c′ (cprime) as a direct effect of an explanatory variable (X) to a response variable Y adjusted for a mediating variable, M. First, we used Baron and Kenny’s four steps to identify the indirect effect of mediation analysis (1986). Detailed statistical procedures are described in the Supplementary Material. When all four conditions were met, a psychiatric diagnosis fully or partially mediated the relationship between ACE and binge levels. We then used the Sobel approach (MacKinnon et al., 2002) to test if the mediation effect (ab), quantified by the product of the a and b from the three models, was statistically significant. Furthermore, as another measure of mediation, a proportion of the mediated effect was calculated to quantify the magnitude of the indirect effect divided by the total effect of ACE on BD levels (MacKinnon et al., 2007). We explored SUD, mood disorder, anxiety disorder, post-traumatic stress disorders (PTSD), and personality disorder (PD) individually as a mediator and subsequently investigated three specific SUDs, AUD, nicotine use disorder (NUD), and drug use disorder (DUD). All mediation analyses incorporated weights using SUDAAN, version 11.0 and SAS (version 9.4; SAS Institute Inc., Cary, NC).
Fig. 1.
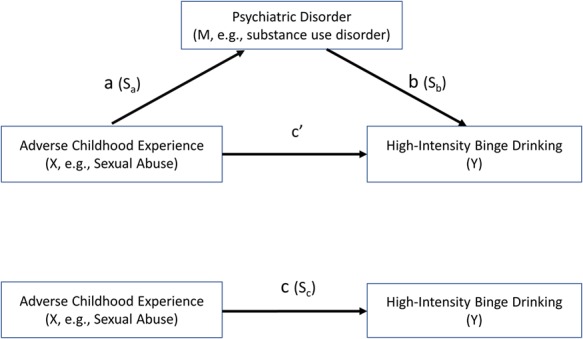
Standard tri-variate mediation: X = explanatory variable (ACE, e.g. sexual abuse), M = mediator (psychiatric disorder, e.g. SUD), Y = response variable (HIBD), Sa is the standard error of a, Sb is the standard error of b and Sc is the standard error of c.
NIAAA clinical sample
Frequencies of ACEs were estimated and compared for each binge level using chi-squared test for gender, race, and treatment-seeking AD. Mean differences of age across binge levels were tested by Kruskal–Wallis test due to non-normality. Multinomial logistic regression models controlling for age, gender, and race were employed to test the relationships between each ACE and each binge level. AORs were reported with the P-value to describe associations of each ACE on HIBD. All NIAAA analyses were performed using SAS (version 9.4; SAS Institute Inc., Cary, NC).
RESULTS
Sociodemographic characteristics across high-intensity binge levels
In the NESARC-III sample, 17.0% reported HIBD who were disproportionately white, younger overall, younger at age of the first drink, and younger at age of heaviest drinking (P < 0.0001). Prevalence of low to mid-level socioeconomic status increased across binge levels with P-values <0.0001 (Table 1).
Prevalence and association of ACEs with HIBD
In the NESARC-III sample, ACE prevalence increased across binge levels, ranging from 1.3 to 1.5 times among extreme HIBD compared with non-bingers (sexual abuse: 5.71–7.44%; physical abuse: 18.68–26.26%; verbal abuse: 26.57–38.59%; physical neglect: 18.87–29.04%; emotional neglect: 29.16–34.17%) (Table 2). Prevalence of household dysfunction also increased by 1.6–2.4 times across binge levels with the exception of family history of mental illness, which was not significantly different across any binge groups (P = 0.12). ACE prevalence of child abuse (sexual, physical, verbal abuse, and physical and emotional neglect) increased across binge levels (P < 0.001; Fig. 2) and ACE overall was the most prevalent at the extreme HIBD (P < 0.0001).
Table 2.
Weighted prevalence of ACEs by alcohol binge consumption levels in NIAAA and NESARC-III (%, SE)a
| Alcohol binge levelb | |||||
|---|---|---|---|---|---|
| Non-binge | Level I | Level II | Level III | P-value | |
| NESARC-III | N = 14,030 | N = 7,190 | N = 2,599 | N = 1,733 | |
| Child abuse and neglect | |||||
| Sexual abuse | 5.71 (0.25) | 5.86 (0.30) | 4.81 (0.53) | 7.44 (0.71) | 0.02 |
| Physical abuse | 18.68 (0.50) | 18.93 (0.63) | 19.48 (0.97) | 26.26 (1.48) | <0.0001 |
| Verbal abuse | 26.57 (0.61) | 28.03 (0.67) | 28.55 (1.14) | 38.59 (1.33) | <0.0001 |
| Physical neglect | 18.87(0.54) | 20.08 (0.58) | 22.07 (0.91) | 29.04 (1.39) | <0.0001 |
| Emotional neglect | 29.16 (0.58) | 29.89 (0.68) | 30.64 (1.09) | 34.17 (1.34) | 0.004 |
| Household dysfunction ACE | |||||
| Battered mother/stepmother | 10.10 (0.38) | 10.74 (0.47) | 12.12 (0.82) | 16.11 (1.22) | <0.0001 |
| Substance abuse | 22.93 (0.50) | 26.73 (0.71) | 29.04 (1.17) | 36.99 (1.54) | <0.0001 |
| Mental illness | 5.30 (0.20) | 6.01 (0.40) | 5.65 (0.45) | 6.71 (0.86) | 0.12 |
| Incarceration | 6.38 (0.28) | 8.87 (0.39) | 9.80 (0.68) | 15.41 (0.96) | <0.0001 |
| Suicide/suicide attempts | 2.84 (0.18) | 4.14 (0.28) | 4.26 (0.47) | 5.48 (0.68) | <0.0001 |
| NIAAA | N = 199 | N = 319 | N = 196 | N = 589 | |
| Child abuse and neglect | |||||
| Sexual abuse | 5.03 (1.55) | 6.58 (1.39) | 13.27 (2.43) | 19.19 (1.62) | <0.0001 |
| Physical abuse | 5.53 (1.62) | 9.72 (1.66) | 17.35 (2.71) | 28.69 (1.87) | <0.0001 |
| Emotional abuse | 16.08 (2.61) | 16.61 (2.09) | 26.53 (3.16) | 39.73 (2.02) | <0.0001 |
| Physical neglect | 3.54 (1.32) | 6.98 (1.44) | 8.81 (2.05) | 18.40 (1.60) | <0.0001 |
| Emotional neglect | 19.19 (2.81) | 24.13 (2.41) | 29.02 (3.28) | 42.69 (2.04) | <0.0001 |
aWeighted prevalence % (SE) reported.
bAlcohol binge levels are gender-specific: for women, non-binge = 1–3; level I = 4–7; level II = 8–11; level III  12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III
12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III  15 drinks.
15 drinks.
Fig. 2.
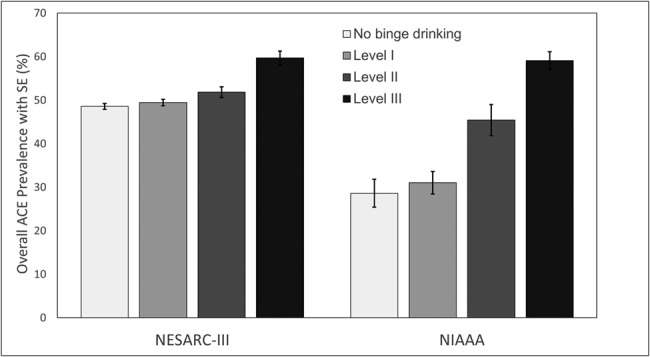
Prevalence of child abuse ACE by alcohol binge levels in the NESARC-III and NIAAA samples. Child abuse ACE includes five childhood abuse and neglect experiences: physical abuse, sexual abuse, emotional or verbal abuse, emotional neglect, and physical neglect. Prevalence difference P-values <0.001 for all levels in both NESARC-III (n = 25552) and NIAAA (n = 1303) samples.
Adjusted for sociodemographics but not psychiatric disorders, each ACE except family history of mental illness was associated with significantly higher odds of HIBD compared with non-binge drinkers, with the largest odds for level III (P < 0.001; Table 3). Among child abuse ACEs, verbal abuse conferred the highest ORs, and emotional neglect had the lowest ORs (verbal abuse for level III, 1.90, 95% CI, 1.65–2.18; level II, 1.23, 95% CI, 1.09–1.38; emotional neglect for level III, 1.27, 95% CI, 1.11–1.43; level II, 1.15, 95% CI, 1.02–1.29). Three of five household dysfunction ACEs, available only in NESARC-III, were significantly associated with HIBD and had increased odds across binge levels relative to the non-binging group. Having family members with substance abuse constituted the highest OR (level III: 1.90, 95% CI, 1.64–2.21; level II, 1.40, 95% CI, 1.23–1.58), and having a family member with suicide attempt or commission had the lowest ORs (level III, 1.58, 95% CI, 1.19–2.11; level II,1.35, 95% CI, 1.04–1.76).
Table 3.
AORs of ACEs on alcohol binge levels, adjusted for sociodemographic characteristicsa
| Alcohol binge levelb | ||||
|---|---|---|---|---|
| Non-binge | Level I | Level II | Level III | |
| NESARC-III | N = 14,030 | N = 7,190 | N = 2,599 | N = 1,733 |
| Sexual abuse | 1 (ref) | 1.10 (0.96–1.27) | 1.23 (0.94–1.62) | 1.86 (1.45–2.39) *** |
| Physical abuse | 1 (ref) | 1.10 (1.0–1.21) * | 1.23 (1.08–1.41) ** | 1.83 (1.54–2.18) *** |
| Verbal abuse | 1 (ref) | 1.11 (1.02–1.21) * | 1.23 (1.09–1.38) ** | 1.90 (1.65–2.18) *** |
| Physical neglect | 1 (ref) | 1.12 (1.02–1.24) * | 1.27 (1.10–1.47) ** | 1.80 (1.52–2.14) *** |
| Emotional neglect | 1(ref) | 1.09 (1.01–1.18) * | 1.15 (1.02–1.29) * | 1.27 (1.11–1.43) ** |
| Household dysfunction ACE | ||||
| Mother abused | 1(ref) | 1.09 (0.97–1.22) | 1.38 (1.18–1.61) *** | 1.77 (1.43–2.19) *** |
| Substance abuse | 1(ref) | 1.18 (1.08–1.28) ** | 1.40 (1.23–1.58) *** | 1.90 (1.64–2.21) *** |
| Mental Illness | 1(ref) | 1.10 (0.94–1.28) | 1.09 (0.91–1.29) | 1.23 (0.93–1.64) |
| Incarceration | 1(ref) | 1.16 (1.02–1.31) * | 1.19 (0.99–1.44) | 1.71 (1.45–2.03) *** |
| Suicide/suicide attempt | 1(ref) | 1.31 (1.06–1.61) * | 1.35 (1.04–1.76) * | 1.58 (1.19–2.11) ** |
| NIAAA | N = 199 | N = 319 | N = 196 | N = 589 |
| Child abuse and neglect | ||||
| Sexual abuse | 1 (ref) | 1.58 (0.71–3.50) | 3.32 (1.52–7.28) ** | 5.86 (2.92–11.75) *** |
| Physical abuse | 1 (ref) | 2.35 (1.11–4.93) * | 4.08 (1.94–8.59) ** | 7.95 (4.06–15.57) *** |
| Emotional abuse | 1 (ref) | 1.18 (0.72–1.93) | 1.97 (1.19–3.27) ** | 3.70 (2.41–5.69) *** |
| Physical neglect | 1 (ref) | 2.31 (0.96–5.56) | 2.49 (1.00–6.20) * | 5.48 (2.49–12.10) *** |
| Emotional neglect | 1 (ref) | 1.45 (0.93–2.26) | 1.64 (1.02–2.64) * | 2.90 (1.95–4.32) *** |
aAORs are reported with 95% CI in parentheses; AORs were generated from multinomial logistics regression adjusted for age, gender, race, marital status, education attainment, and family income for NESARC-III sample and age, gender, race for NIAAA sample; *P < 0.05 **P < 0.01 ***P < 0.001 (significant AORs in boldface).
bAlcohol binge levels are gender-specific: for women, non-binge = 1–3; level I = 4–7; level II = 8–11; level III  12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III
12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III  15 drinks.
15 drinks.
Prevalence and association of psychiatric disorders with HIBD
The prevalence of each psychiatric disorder in NESARC-III increased across binge levels, ranging from 1.3 to 5 times among individuals with extreme HIBD compared with non-bingers (SUD: 18.00–85.82%; any mood disorder: 12.18–22. 21%; any anxiety disorder: 12.54–16.39%; PTSD: 4.06–8.62%; any PD: 11.88–33.84%) (Table 4). Overall, the prevalence of psychiatric disorders was significantly different across binge levels (Ps < 0.0001) except that specific phobia and generalized anxiety disorder were not differently distributed at any binge levels (Ps > 0.05). The separate analysis for comorbid psychiatric disorders showed that, adjusted for sociodemographics, SUD was significantly associated with increasingly higher odds across all binging levels (level III OR, 21.32, 95% CI, 17.49–25.98), while at lesser magnitudes, mood, personality, and anxiety disorders were also significant (Table 5). Other subcategories of psychiatric disorders, with the exception of agoraphobia and social phobia, were also significantly associated with HIBD, especially extreme HIBD (Ps < 0.001).
Table 4.
Weighted prevalence of psychiatric disorders by alcohol binge consumption levels in NESARC-III (%, SE)a
| Alcohol binge levelb | |||||
|---|---|---|---|---|---|
| Non-binge (N = 14,030) | Level I (N = 7,190) | Level II (N = 2,599) | Level III (N = 1,733) | P-value | |
| Past-year psychiatric disorders | |||||
| SUD | 18.00 (0.50) | 42.01 (0.81) | 66.79 (1.16) | 85.82 (1.10) | <0.0001 |
| AUD | 3.36 (0.18) | 23.80 (0.68) | 50.72 (1.21) | 74.42 (1.33) | <0.0001 |
| NUD | 14.68 (0.47) | 24.62 (0.73) | 37.91 (1.31) | 53.46 (1.61) | <0.0001 |
| Any DUD | 2.11 (0.14) | 5.19 (0.35) | 9.39 (0.76) | 17.37 (1.09) | <0.0001 |
| Mood disorder | 12.18 (0.39) | 15.05 (0.53) | 16.25 (0.98) | 22.21 (1.20) | <0.0001 |
| Major depressive disorder | 9.91 (0.36) | 11.49 (0.49) | 11.79 (0.84) | 14.18 (1.05) | <0.0001 |
| Bipolar I disorder | 0.91 (0.10) | 1.83 (0.21) | 2.39 (0.41) | 5.19 (0.66) | <0.0001 |
| Anxiety disorder | 12.54 (0.40) | 14.52 (0.56) | 14.60 (0.92) | 16.39 (1.11) | 0.0003 |
| Agoraphobia | 1.18 (0.11) | 1.79 (0.21) | 2.16 (0.39) | 2.16 (0.41) | 0.0006 |
| Social phobia | 2.47 (0.18) | 3.28 (0.28) | 3.37 (0.43) | 3.90 (0.58) | 0.003 |
| Specific phobia | 5.51 (0.23) | 6.20 (0.40) | 5.83 (0.56) | 7.42 (0.79) | 0.06 |
| Generalized anxiety disorder | 5.21 (0.26) | 5.63 (0.34) | 6.13 (0.68) | 6.83 (0.67) | 0.09 |
| Panic disorder | 2.46 (0.16) | 3.77 (0.26) | 4.36 (0.53) | 5.21 (0.74) | <0.0001 |
| PTSD | 4.06 (0.22) | 5.23 (0.34) | 5.45 (0.57) | 8.62 (0.68) | <0.0001 |
| Personality disorder | 11.88 (0.43) | 16.97 (0.63) | 23.43 (1.23) | 33.84 (1.39) | <0.0001 |
| Schizotypal PD | 2.17 (0.30) | 6.77 (0.38) | 9.05 (0.73) | 13.62 (1.0) | <0.0001 |
| Borderline PD | 8.58 (0.34) | 12.77 (0.52) | 17.63 (1.04) | 25.81 (1.30) | <0.0001 |
| Antisocial (adult) | 16.49 (0.51) | 24.79 (0.63) | 33.37(1.37) | 43.72 (1.39) | <0.0001 |
Abbreviations: DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
aWeighted prevalence % (SE) reported.
bAlcohol binge levels are gender-specific: for women, non-binge = 1–3; level I = 4–7; level II = 8–11; level III  12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III
12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III  15 drinks.
15 drinks.
Table 5.
AORs of past-year substance use and other psychiatric disorders on alcohol binge levels, adjusted for sociodemographic characteristics in NESARC-IIIa
| OR, 95% CI | ||||
|---|---|---|---|---|
| Alcohol binge levelb | ||||
| Past-year psychiatric disorders | Non-binge (n = 14,030) | Level I (n = 7,190) | Level II (n = 2,599) | Level III (n = 1,733) |
| SUD | 1 (ref) | 3.05(2.80–3.33) *** | 7.99 (7.17–8.91) *** | 21.32(17.49–25.98) *** |
| AUD | 1 (ref) | 7.96 (6.94–9.11) *** | 25.25 (22.27–28.64) *** | 70.10(58.41–84.13) *** |
| NUD | 1 (ref) | 1.76 (1.60–1.95) *** | 3.11 (2.72–3.54) *** | 5.11 (4.41–5.91) *** |
| Any DUD | 1 (ref) | 1.92 (1.59–2.32) *** | 2.95 (2.33–3.75) *** | 5.15 (4.13–6.42) *** |
| Mood disorder | 1 (ref) | 1.14 (1.03–1.26) * | 1.32 (1.14–1.54) ** | 1.73 (1.46–2.04) *** |
| Major depressive disorder | 1 (ref) | 1.07 (0.95–1.21) | 1.21 (1.01–1.44) * | 1.33 (1.08–1.63) ** |
| Bipolar I disorder | 1 (ref) | 1.69 (1.31–2.19) *** | 2.04 (1.31–3.18) ** | 3.97 (2.67–5.91) *** |
| Anxiety disorder | 1 (ref) | 1.15 (1.02–1.30) * | 1.30 (1.10–1.53) ** | 1.37 (1.15–1.63) ** |
| Agoraphobia | 1 (ref) | 1.37 (1.01–1.84) * | 1.81 (1.20–2.74) ** | 1.54 (0.97–2.45) |
| Social phobia | 1 (ref) | 1.17 (0.94–1.46) | 1.18 (0.85–1.65) | 1.17 (0.83–1.64) |
| Specific phobia | 1 (ref) | 1.13 (0.96–1.32) | 1.20 (0.96–1.50) | 1.45 (1.14–1.84) ** |
| Generalized anxiety | 1 (ref) | 1.09 (0.92–1.28) | 1.31 (1.02–1.68) * | 1.38 (1.09–1.76) ** |
| Panic disorder | 1 (ref) | 1.35 (1.12–1.63) ** | 1.81 (1.35–2.42) *** | 1.97 (1.40–2.77) *** |
| PTSD | 1 (ref) | 1.16 (0.99–1.36) | 1.36 (1.08–1.71) * | 1.97 (1.56–2.47) *** |
| Personality disorder | 1 (ref) | 1.35 (1.21–1.51) *** | 1.91 (1.64–2.22) *** | 2.84 (2.48–3.26) *** |
| Schizotypal PD | 1 (ref) | 1.15 (0.98–1.35) | 1.42 (1.15–1.77) ** | 1.95 (1.54–2.45) *** |
| Borderline PD | 1 (ref) | 1.40 (1.24–1.57) *** | 2.02 (1.71–2.40) *** | 2.89 (2.44–3.42) *** |
| Antisocial (adult) personality | 1 (ref) | 1.51 (1.39–1.64) *** | 2.08 (1.80–2.39) *** | 3.00 (2.58–3.49) *** |
aAORs are reported with 95% CI in parentheses; AORs were generated from multinomial logistics regression adjusted for age, gender, race, marital status, education attainment, and family income for NESARC-III sample, and age, gender, race for NIAAA sample; P < 0.05 **P < 0.01 ***P < 0.001 (significant AORs in boldface).
bAlcohol binge levels are gender-specific: for women, non-binge = 1–3; level I = 4–7; level II = 8–11; level III  12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III
12 drinks; for men, non-binge = 1–4; level L = 5–9; level II = 10–14; level III  15 drinks.
15 drinks.
Mediation analysis of psychiatric disorders on the relationship between ACE and HIBD
As all four requirements of Baron and Kenny’s approach were satisfied with level III (the extreme HIBD), we found that each psychiatric disorder either fully or partially mediated the relationship between ACE and extreme HIBD. Table 6 shows the results of Sobel’s test statistics and the proportion mediated, which is the amount of reduction in the direct effect of ACE on HIBD due to each psychiatric disorder. SUD and any PD had the most significant mediating effect (P < 1.0E−10, Table 6), while any anxiety disorder had a significant, but weaker indirect effect (0.001 < P < 0.02). Mood disorder and PTSD also significantly mediated the association of ACE and HIBD (1.0E−10 < P < 1.0E−5). Consistent with the Sobel’s test, the proportion mediated by each psychiatric disorder varied across ACEs. We defined that over 80% of the proportion mediated was considered as full mediation. SUD, consisting of AUD, NUD, and DUD, accounted for 70–90% of the mediating effect on the relationship between ACEs and HIBD except family history of mental illness, which did not show significant associations with any binge levels (Supplementary Table S1). The proportions mediated by PD and PTSD were 60–80 and 30–50%, respectively, while mood and anxiety disorders had small mediating effects (mood, 20–30%; anxiety, <20%). Among categories of ACEs, the association of emotional neglect and HIBD was fully mediated by SUD or PD (proportion > 90%), which explained no direct association of emotional neglect on HIBD. The contribution of sexual abuse, family history of incarceration, and suicidal behavior to HIBD were also fully mediated through SUD and AUD (proportion > 80%, Supplementary Table S1). All detailed associated effects, a, b, c values, and Sobel’s t statistic were listed in Supplementary Table S2. The results of the mediation analyses suggested that SUD or AUD fully mediated the relationship between ACE and extreme HIBD, while other psychiatric disorders were partial mediators.
Table 6.
Mediation analyses of each psychiatric disorder in the relationship between ACE and level III (extreme HIBD) in NESARC-III
| Any SUD | Any mood disorder | Any anxiety disorder | PTSD | Any PD | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sobel testa | Proportion mediated | Sobel test | Proportion mediated | Sobel test | Proportion mediated | Sobel test | Proportion mediated | Sobel test | Proportion mediated | |
| Sexual abuse | 9.99*** | 0.86 | 5.80*** | 0.33 | 2.74** | 0.18 | 4.29*** | 0.49 | 11.31*** | 0.69 |
| Physical abuse | 13.11*** | 0.77 | 5.36*** | 0.27 | 2.87** | 0.14 | 4.49*** | 0.37 | 11.99*** | 0.62 |
| Verbal abuse | 15.16*** | 0.76 | 4.87*** | 0.26 | 2.34* | 0.13 | 4.05*** | 0.36 | 11.59*** | 0.62 |
| Physical neglect | 12.44*** | 0.72 | 5.41*** | 0.26 | 2.74** | 0.16 | 4.39*** | 0.39 | 12.59*** | 0.60 |
| Emotional neglect | 8.65*** | 0.92 | 6.00*** | 0.52 | 3.31** | 0.30 | 5.04*** | 0.63 | 12.51*** | 0.93 |
| Household dysfunction ACE | ||||||||||
| Mother abused | 11.02*** | 0.76 | 5.41*** | 0.27 | 3.02** | 0.16 | 4.65*** | 0.40 | 11.94*** | 0.60 |
| Substance abuse | 13.20*** | 0.74 | 5.16*** | 0.22 | 2.52* | 0.11 | 4.34*** | 0.29 | 11.47*** | 0.50 |
| Incarceration | 10.17*** | 0.82 | 5.44*** | 0.27 | 3.17** | 0.17 | 4.8*** | 0.41 | 11.77*** | 0.67 |
| Suicide/suicide attempt | 5.76*** | 0.82 | 5.37*** | 0.38 | 3.35** | 0.27 | 4.75*** | 0.49 | 10.14*** | 0.78 |
aSobel test statistics presented a mediation effect driven by three multinomial logistics regression adjusted for sociodemographic status; P value of the Sobel test statistic was calculated by a normal (Z) distribution with large sample size, *P < 0.05; **P < 0.01; ***P < 0.001).
Prevalence and association of ACEs with HIBD in the NIAAA sample
In the NIAAA sample, Table 1 shows that 60.2% reported HIBD, which combined level II (15%) and III (45.2%) by the definition. HIBD were predominantly male, generally older, and equally non-Hispanic whites and non-Hispanic black (P < 0.05). Unsurprisingly, HIBD was seen predominantly in treatment-seeking AD individuals due to clinically based sample recruitment (P < 0.0001). ACE frequencies similarly increased across binge levels, ranging from 2 to 5 times in extreme HIBD (sexual abuse: 5.03–19.19%; physical abuse: 5.53–28.69%; emotional abuse: 16.08–39.73%; physical neglect: 3.54–18.40%; emotional neglect: 19.19–42.69%) (P < 0.0001; Table 2, Fig. 2). Table 3 illustrates that physical abuse among extreme HIBD conferred the highest odds (OR, 7.95; 95% CI, 4.06–15.57) and emotional neglect had the lowest odds (2.90, 95% CI, 1.95–4.32) with all odds larger than those of the NESARC-III. The ORs of each ACE for HIBD were significant (P < 0.001).
DISCUSSION
Using two independent phenotypic samples, our study comprehensively investigated the relationship between ACEs, comorbid psychiatric disorders, and HIBD. Initial analyses examined a large nationally representative survey sample with individuals who had consumed alcohol in the past 12 months (NESARC-III, n = 22,552). Next, analyses were replicated in the NIAAA sample (n = 1,326) that contained a clinically severe alcohol -dependent phenotype. ACE prevalence overall (excluding household dysfunction ACEs) increased across binge levels in both samples. In the NESARC-III sample, among child abuse ACEs, verbal and sexual abuse showed the most significant associations with extreme HIBD. The effect sizes of household dysfunction ACEs were similar to child abuse ACEs, which supports the importance and utility of all types of ACEs as risk factors for HIBD. In addition, the prevalence of psychiatric diagnoses, with the exceptions of social anxiety and specific phobia, were higher in each BD level than estimates of the general US population (Kessler et al., 2005). For example, the past 12-month prevalence of major depressive disorder in each BD level (level I: 11.49%, level II: 11.79% and level III: 14.18%) was almost double the 6.7% 12-month prevalence reported in the 2016 National Survey on Drug Use and Health (Rebecca Ahrnsbrak et al., 2017). Similarly, PTSD was more than twice as prevalent in level III (8.62%) than estimates for US adults (3.6%). In general, AUD was the strongest risk factor across BD levels with increased odds of 70.1 for extreme HIBD among all psychiatric diagnoses. Given that these comorbid psychiatric disorders constitute risk factors for BD, the NESARC-III sample suggests that all psychiatric disorders may contribute directly or indirectly to the association between ACEs and HIBD with various magnitudes. Moreover, the full mediation effect of AUD on the relationship between ACEs and HIBD indicates that ACE may be associated with HIBD predominantly through AUD. We confirmed our findings in the NIAAA clinical sample with clinically severe phenotypes of ACEs and alcohol consumption that there were significant increases in all ACE prevalence rates across BD levels with the highest being a 2–5-fold increased ACE prevalence in the extreme HIBD group. Among individuals with extreme HIBD in the NIAAA sample, 95% were individuals with AD. The greater magnitude of odds of ACE on extreme HIBD in the NIAAA sample confirmed the results of the mediation analysis in NESARC-III, where ACEs were associated with extreme HIBD through AUD.
Our findings in the present study aligned with those in studies identifying a relationship between ACEs and alcohol consumption. A recent study conducted by Loudermilk et al. (2018) showed adults with household abuse had a 30% increased risk for BD and a 21% increased risk for AD compared with adults without household abuse. In addition to examining a mediating role of psychiatric disorders, our study differs from the previous studies which focused on only BD, not HIBD that has been shown to be associated with more severe alcohol-related health problems (Rosoff et al., 2019). Given the substantially more severe health consequences of heavy drinking that exceeds the binge threshold (i.e. HIBD), which might be missed in studies using binary BD as their main outcome, improving our ability to identify individuals at high risk for HIBD is crucial for improving public health outcomes. Our findings might have important implications for the identification and diagnostic assessment of individuals at risk for HIBD, as well as the development and implementation of treatment plans. Screening for recent HIBD is recommended, given the associations between binge level I, II, and III and broad health-related risks. The present study’s findings indicate that health-care providers should include questions about early childhood experiences of trauma and psychiatric disorders when assessing cases of HIBD behavior, regardless of AD diagnosis. At the public health level, there is evidence that BD rates respond to population level alcohol policies. As such, policy changes may reduce BD rates and prevent the consequences of harmful BD. Another recommendation at the public health level resulting from these findings is that the first stage that seems to contribute to HIBD and SUD, namely ACEs, should be minimized through adequate policies and child protection services.
There are several limitations to this study. First, the cross-sectional design does not allow to conclude any causality. Although our study provides potential evidence that psychiatric disorders may fully or partially mediate the relationship between ACE and HIBD, longitudinal research is needed to confirm the causal relationship. Moreover, mediation analyses with multiple mediators could be a more suitable approach to explain the underlying mechanism of the relationship due to comorbidity among psychiatric disorders. Second, recall bias for ACEs may lead to an underestimation of the impact of these events on HIBD (Kauhanen et al., 2011). Retrospective reports of ACEs, obtained in adulthood, may be biased regarding their severity compared with adolescent reports of ACEs (Femina et al., 1990; Williams, 1995). Further, previous research suggests that ACEs, in particular sexual abuse, are associated with an inability to remember details of the event(s) (Freyd et al., 2005). For BD outcomes, recall and social desirability biases may affect self-reported alcohol consumption, especially among HIBD (Hingson et al., 2017). The definition of HIBD was developed in previous studies, however, the categories preclude distinction between individuals consuming alcohol throughout the day and individuals’ binging that occurs rapidly enough for BAC to reach 0.08 g/dL within 2 hours, as is the NIAAA definition of BD. Third, certain populations were not covered in the NESARC-III, which may underestimate our findings. Similarly, AUDADIS interviews determining past 12-month substance, mood, anxiety, trauma-related and PDs were not conducted by clinicians, although NESARC-III psychiatric diagnoses have reported good accordance with clinical reappraisal procedure (Grant et al., 2017). Furthermore, it has been known that exposure or responses to ACEs differ by gender, and higher prevalences of AUD and more extreme alcohol consumption are associated with males compared with females (Erol and Karpyak, 2015; Liu et al., 2015). Future studies on a mediating role of specific psychiatric disorders (e.g. anxiety or eating disorders) on the relationship between ACEs and HIBD might consider focusing on gender differences.
In conclusion, our study shows that ACEs and comorbid psychiatric disorders are significant risk factors for HIBD in adulthood and that psychiatric disorders play a full or partial mediating role in the relationship between ACEs and HIBD. These findings suggest that health-care providers may consider including questions about early childhood experiences/trauma and psychiatric disorders when assessing cases of extreme BD behavior.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the National Institutes of Health (NIH) intramural funding [ZIA-AA000242 to F.W.L.]; Division of Intramural Clinical and Biological Research of the NIAAA. Dr. Charlet acknowledges funding from the German Research Foundation (DFG CH1936/1-1). We thank Melanie Schwandt (NIAAA/OCD) for statistical support.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Additional information
The original data set for the National Epidemiologic Survey on Alcohol and Related Conditions II (NESARC-III) is available from the NIAAA (http://www.niaaa.nih.gov).
References
- Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51:1173–82. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, et al. (2003) Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl 27:169–90. [DOI] [PubMed] [Google Scholar]
- Brady KT, Back SE (2012) Childhood trauma, posttraumatic stress disorder, and alcohol dependence. Alcohol Res 34:408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bynum L, Griffin T, Ridings DL, et al. (2011) Adverse childhood experiences reported by adults-five states, 2009 (reprinted from MMWR, vol 59, pg 1609-1613, 2010). JAMA 305:666–8. [PubMed] [Google Scholar]
- Cawthorpe D, Marriott B, Paget J, et al. (2018) Relationship between adverse childhood experience survey items and psychiatric disorders. Perm J 22:18–001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlet K, Heinz A (2017) Harm reduction-a systematic review on effects of alcohol reduction on physical and mental symptoms. Addict Biol 22:1119–59. [DOI] [PubMed] [Google Scholar]
- Cheong EV, Sinnott C, Dahly D, et al. (2017) Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open 7:e013228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erol A, Karpyak VM (2015) Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug Alcohol Depend 156:1–13. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, et al. (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med 14:245–58. [DOI] [PubMed] [Google Scholar]
- Femina DD, Yeager CA, Lewis DO (1990) Child abuse: adolescent records vs. adult recall. Child Abuse Negl 14:227–31. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, et al. (2002) User’s Guide for the Structured Clinical Interview for DSM-IV-TR Axis I Disorders—Research Version. New York, NY: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Fish JN, Hughes TL, Russell ST (2018) Sexual identity differences in high-intensity binge drinking: findings from a US national sample. Addiction 113:749–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freyd JJ, Putnam FW, Lyon TD, et al. (2005) The science of child sexual abuse. Science 308:501–1. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou S, Saha TD, et al. (2017) Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiat 74:911–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, et al. (2004) Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on alcohol and related conditions. Arch Gen Psychiatry 61:361–8. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Zha W, White AM (2017) Drinking beyond the binge threshold: predictors, consequences, and changes in the US. Am J Prev Med 52:717–27. [DOI] [PubMed] [Google Scholar]
- Kauhanen L, Leino J, Lakka HM, et al. (2011) Adverse childhood experiences and risk of binge drinking and drunkenness in middle-aged finnish men. Adv Prev Med 2011:478741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, et al. (2005) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. (vol 62, pg 617, 2005). Arch Gen Psychiatry 62:709–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, Mcgonagle KA, et al. (1996) The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am J Orthopsychiatry 66:17–31. [DOI] [PubMed] [Google Scholar]
- Lew D, Xian H (2019) Identifying distinct latent classes of adverse childhood experiences among US children and their relationship with childhood internalizing disorders. Child Psychiatry Hum Dev 50:668–80. [DOI] [PubMed] [Google Scholar]
- Liu Y, Sun Y, Tao F, et al. (2015) Associations between adverse childhood experiences with early puberty timing and possible gender difference. Zhonghua Liu Xing Bing Xue Za Zhi 36:314–7. [PubMed] [Google Scholar]
- Loudermilk E, Loudermilk K, Obenauer J, et al. (2018) Impact of adverse childhood experiences (ACEs) on adult alcohol consumption behaviors. Child Abuse Negl 86:368–74. [DOI] [PubMed] [Google Scholar]
- Lucey MR, Mathurin P, Morgan TR (2009) Alcoholic hepatitis. N Engl J Med 360:2758–69. [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, Fairchild AJ, Fritz MS (2007) Mediation analysis. Annu Rev Psychol 58:593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon DP, Lockwood CM, Hoffman JM, et al. (2002) A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 7:83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Chaloupka FJ, Saitz R, et al. (2004) Alcohol-attributable deaths and years of potential life lost—United States, 2001 (reprinted from MMWR, vol 53, pp. 866–870, 2004). JAMA 292:2831–2. [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, et al. (2005) Correction: actual causes of death in the United States, 2000. JAMA 293:293–4. [DOI] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, et al. (2010) Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry 15:868–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Azar B (2018) High-intensity drinking. Alcohol Res 39:49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebecca Ahrnsbrak JB, Hedden SL, Lipari RN, Park-Lee E. 2017. Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.htm (4 September 2018, date last accessed).
- Regier DA, Farmer ME, Rae DS, et al. (1990) Comorbidity of mental disorders with alcohol and other drug abuse. Results from the epidemiologic catchment area (ECA) study. JAMA 264:2511–8. [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, et al. (2009) Alcohol and Global Health 1 global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 373:2223–33. [DOI] [PubMed] [Google Scholar]
- Rokita KI, Dauvermann MR, Donohoe G (2018) Early life experiences and social cognition in major psychiatric disorders: a systematic review. Eur Psychiatry 53:123–33. [DOI] [PubMed] [Google Scholar]
- Rosoff DB, Charlet K, Jung J, et al. (2019) Association of high-intensity binge drinking with lipid and liver function enzyme levels. JAMA Netw Open 2:e195844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman EF, Edwards EM, Heeren T, et al. (2008) Adverse childhood experiences predict earlier age of drinking onset: results from a representative US sample of current or former drinkers. Pediatrics 122:e298–304. [DOI] [PubMed] [Google Scholar]
- Sanders B, Becker-Lausen E (1995) The measurement of psychological maltreatment: early data on the child abuse and trauma scale. Child Abuse Negl 19:315–23. [DOI] [PubMed] [Google Scholar]
- Schwandt ML, Heilig M, Hommer DW, et al. (2013) Childhood trauma exposure and alcohol dependence severity in adulthood: mediation by emotional abuse severity and neuroticism. Alcohol Clin Exp Res 37:984–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB (1992) Timeline follow-back—A technique for assessing self-reported alcohol-consumption. Measuring Alcohol Consumption: Psychosocial and Biological Methods. Totowa, NJ: Humana Press; 41–72. [Google Scholar]
- Vallejos M, Cesoni OM, Farinola R, et al. (2017) Adverse childhood experiences among men with schizophrenia. Psychiatry Q 88:665–73. [DOI] [PubMed] [Google Scholar]
- White AM, Kraus CL, Swartzwelder H (2006) Many college freshmen drink at levels far beyond the binge threshold. Alcohol Clin Exp Res 30:1006–10. [DOI] [PubMed] [Google Scholar]
- Williams LM. (1995) Recovered memories of abuse in women with documented child sexual victimization histories. J Trauma Stress 8:649–73. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Management of Substance Abuse Team (2011) Global Status Report on Alcohol and Health. Geneva, Switzerland:World Health Organization. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


