Highlights
-
•
To our knowledge, it is the first documented case of a liver abscess caused by Raoultella ornithinolytica.
-
•
Liver abscess can have subtle presentation including chronic cough.
Keywords: Raoultella ornithinolytica, Pyogenic liver abscess, Cough
Abstract
Raoultella ornithinolytica is a Gram-negative rod belonging to the Enterobacteriaceae family and closely related to Klebsiella spp. It is commonly present in aquatic environments. Human infections caused by R. ornithinolytica are being increasingly recognized. It has been documented to cause various hospital-acquired infections including but not limited to gastrointestinal, skin, and genitourinary infections. The organism has been particularly associated with invasive procedures and is commonly seen in patients with malignancy, diabetes, chronic kidney disease and immunodeficiency. To our knowledge, we report the first case of pyogenic liver abscess caused by this organism. The patient presented subtly with a chronic, nonresolving cough and was managed successfully by surgical drainage and appropriate antimicrobials.
Introduction
Liver abscess is a relatively uncommon potentially life-threatening disease. With an annual incidence rate of 2.3–3.6 cases per 100,000, it accounts for approximately 8–20 cases of every 100,000 hospital admissions yearly; more commonly in men than women (3.3 vs 1.3 per 100,000, relative risk of 2.6) [1,2]. Of the three main categories of liver abscesses (pyogenic, amebic and fungal), pyogenic liver abscess (PLA) constitutes the vast majority, accounting for 48 % of visceral abdominal abscesses and 13 % of intra-abdominal abscesses overall [3]. Although patients most commonly present with fevers, chills and abdominal pain [4], subtle and atypical presentations including cough, hiccups and referred shoulder pain can also occur, which pose a diagnostic challenge for physicians. The etiology of PLA is often polymicrobial with E. coli being the most frequently reported organism in the United States [4]. Recently, Klebsiella spp. has been increasingly reported as a cause of monomicrobial liver abscess [5]. Nonetheless, the microbiological causes of PLA continue to expand.
Raoultella ornithinolytica is an encapsulated, Gram-negative, nonmotile rod belonging to the Enterobacteriaceae family [6]. It is closely related to Klebsiella spp. and easily misidentified as Klebsiella pneumonia or Klebsiella oxytoca [7]. Human infections related to R. ornithinolytica are being more frequently recognized [8]. However, to our knowledge, no case of R. ornithinolytica pyogenic liver abscess has ever been reported.
We present the case of an 84-year-old male with history of liver cyst, who was found to have pyogenic liver abscess caused by R. ornithinolytica and K. oxytoca, after presenting with chronic, nonresolving cough.
Case report
An 84-year-old male with a history of prostate cancer (following prostatectomy), coronary artery disease, chronic kidney disease and a segment-4 hepatic cyst for the past 15 years, initially presented to his primary-care physician with a chronic dry cough which improved in the recumbent position. He was found to have an unremarkable x-ray and computed tomography (CT) of the chest with a stable cyst in the liver and was referred to an otorhinolaryngologist who placed the patient on a ten-day course of prednisone, after which the patient noted partial improvement. Alleviation of symptoms was attempted with over-the-counter benzonatate (cough suppressant), and omeprazole, again without complete relief.
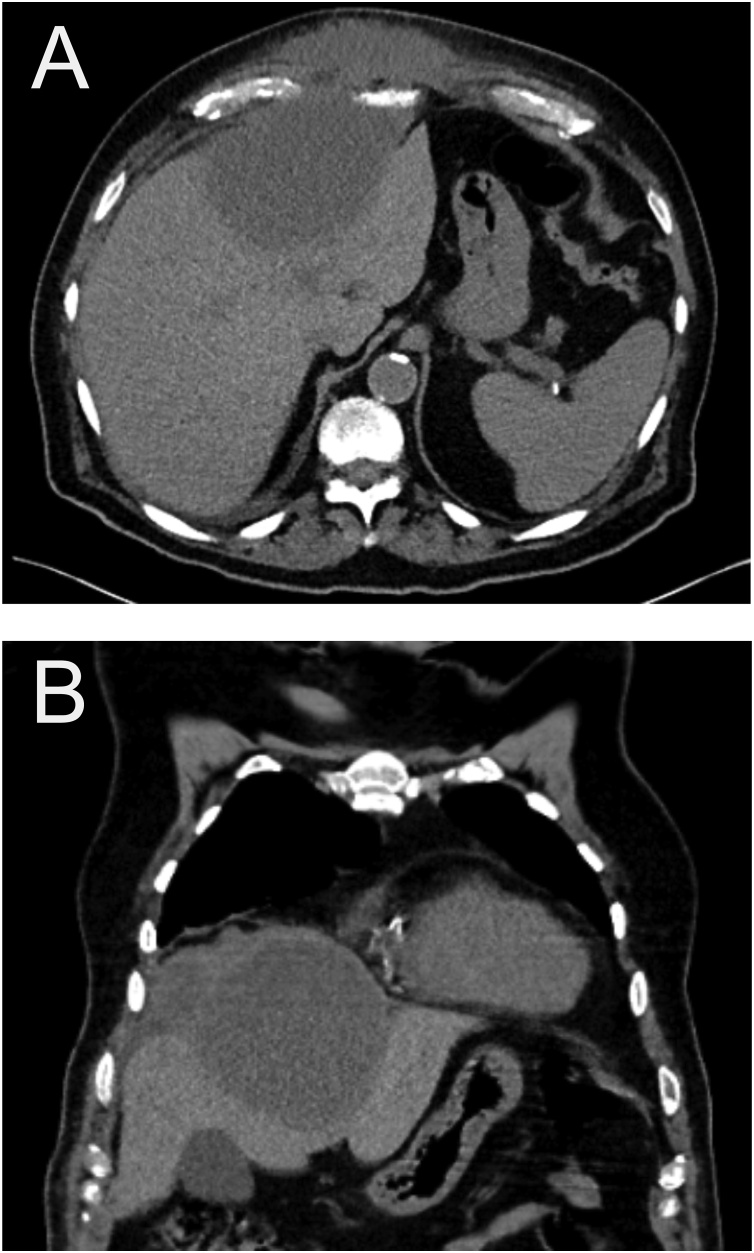
Six months after his initial presentation, the patient was seen in the emergency department for new-onset right-sided chest pain, in addition to the persistent dry cough. At that time, he denied fever, chills, upper respiratory symptoms, dyspnea, or abdominal pain. White blood cell count was 13,240/μL, creatinine 2.1 mg/dL, and electrocardiogram demonstrated normal sinus rhythm. He was discharged home with instructions to follow up with his pulmonologist if his symptoms persisted. Eight days later, he presented back to the emergency department not only with his persistent cough but also now with new onset epigastric pain. He also complained of intermittent fevers, chills, and a temperature to 99.6 °F. His labs revealed slight leukocytosis (12,370/μL), and anemia (8.8 gm/dL). Physical exam demonstrated an anterior thoracoabdominal-wall mass that was approximately 8 cm, firm, warm, nonfluctuant and erythematous. A CT of the chest, abdomen, and pelvis was obtained and demonstrated a complex fluid collection measuring 12.7 × 8.2 cm, consistent with a liver abscess in segment 4 of the liver with extension into and through the abdominal wall with an inflammatory subcutaneous collection, right perihepatic adenopathy, and trace amounts of right-sided pleural effusion (Fig. 1).
Fig. 1.
A) Axial and B) coronal CT images showing a 13-cm hypodense lesion in segments 4, 3, and 2, which appears to extend through the anterior abdominal wall.
The patient subsequently underwent CT-guided placement of an 8-Fr catheter. Over the initial 24 h there were 940 mL of purulent drainage. The patient reported complete resolution of his chronic cough within an hour of the procedure. He was started on broad-spectrum antimicrobials, including vancomycin and pipercillin-tazobactam which were later narrowed to ciprofloxacin after cultures of the fluid grew K. oxytoca and R. ornithinolytica. Both isolates were susceptible to all antimicrobials (covering Gram-negative bacteria) except ampicillin. In addition, K. oxytoca was also resistant to cefazolin.
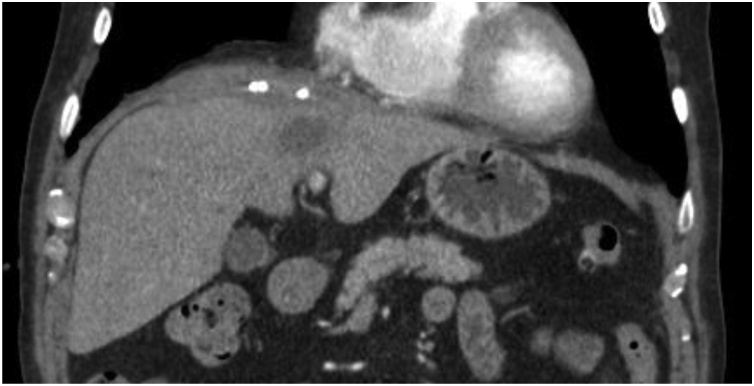
The patient underwent a repeat CT 48 h after drain placement which demonstrated improvement in the abscess, at that time consisting of two smaller components, one measuring 4.5 × 3.3 × 0.9 cm between the right hemidiaphragm and liver and the other 3.3 × 2.3 cm in segment 4 of the liver. Two days later the patient was discharged home with continuation of oral ciprofloxacin 500 mg twice a day. Two weeks after discharge, repeat imaging demonstrated decreased size of the abscess to 3.0 × 2.8 × 0.5 cm, again located between the right hemidiaphragm and liver, adjacent reactive lymph nodes, and stable simple cyst of left medial hepatic lobe (Fig. 2). The patient was seen in the office for a follow-up visit 10 days later, when the drain output was noted to be negligible and was removed. The patient has remained asymptomatic until at least the last follow-up at 4 months following drainage.
Fig. 2.
Interval decrease in size of perihepatic abscess down to approximate baseline size of the segment-4 liver cyst that became infected and developed into the liver abscess.
Discussion
We report the case of an 84-year-old male with a history of liver cyst presenting with atypical symptom of a choric cough like secondary to R. ornithinolytica and K. oxytoca pyogenic liver abscess presumably due to super infection of the liver cyst. Although other cases R. ornithinolytica infection have been reported, our is, to the best of our knowledge, the first case of a R. ornithinolytica PLA reported in the literature.
Indeed, human infections caused by R. ornithinolytica have been on the rise. For example, Seng et al. [8] recently reported a case series and literature review identifying 86 reported cases of R. ornithinolytica. Interestingly, half of these cases were published after 2015, including urinary tract infection, pneumonia, skin and breast abscesses, bacteremia, catheter infection, meningitis, and gastrointestinal infections including cholangitis, pancreatitis, and peritonitis.
Risk factors for R. ornithinolytica infections are invasive procedures (urinary catheters, mechanical ventilation, central-venous catheters) [8], cancer [8,9], immunodeficiency [8], diabetes [8,10], alcoholism [8], and chronic kidney disease (CKD) [11]. Our patient was a relatively healthy male with no recent procedures, hospitalization, diabetes mellitus, nor immunodeficiency. His only pertinent risk factor was CKD. He had a history of prostate cancer treated by prostatectomy in January 2000 without residual disease. Although R. ornithinolytica has been documented to be commonly found in fish, in aquatic environments, and soil, leading to scombroid poisoning [12], our patient reported no such exposure or symptoms.
Of note, our patient had a history of a liver cyst for at least 15 years and he presented with liver abscess at the same site, presumably due to a superinfection of the pre-existing liver cyst. Similarly, Vos and Laureys reported a case of a giant renal cyst causing colonic obstruction with fluid culture revealing R. ornithinolytica [13]. We suspect a transient bacteremia leading to inoculation of liver cyst and formation of abscess in our case as well. Though the majority of R. ornithinolytica infections are monomicrobial, polymicrobial infections with various Gram-positive and Gram-negative bacteria have been described [8]. In our case, there was a polymicrobial infection with K. oxytoca. Pyogenic liver abscess caused by K. oxytoca has been reported infrequently in the literature [14].
Regarding clinical features, our patient initially presented with chronic cough with essentially negative work-up, and subacute duration of epigastric pain. Cough as a symptom of liver abscess has been described and reported in the literature, but is clearly an uncommon presentation of an already very rare PLA subtype. Diaphragmatic irritation from abscess is thought to be responsible for such presentations. Indeed, our patient had complete resolution of his cough immediately after the drainage of his abscess. Fortunately, the isolate of R. ornithinolytica in this case was susceptible to nearly all antibiotics tested (except ampicillin). Most isolates reported in the literature have been resistant to amoxicillin [8].
In conclusion, we report a novel case of a liver abscess caused by R. ornithinolytica and K. oxytoca. R. ornithinolytica has been increasingly recognized as a cause of human infection, but not, until now, as a cause of PLA. This case therefore adds to the spectrum of disease caused by R. ornithinolytica. In addition, it also highlights the rare historical finding of chronic cough which can be seen in patients with PLA.
Author contributions
Asif Surani, Eliza Slama, Samantha Thomas: Writing original draft.
Steve Cunningham and Robert Ross: Writing- review and editing.
Funding disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Consent
Informed consent was obtained from the patient for publication of this case report and accompanying images.
Declaration of Competing Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Contributor Information
Asif Surani, Email: asurani@mcw.edu.
Eliza M. Slama, Email: eliza.slama@ascension.org.
Samantha Thomas, Email: samantha.thomas@ascension.org.
Robert W. Ross, Email: rross@asccension.org.
Steven C. Cunningham, Email: steven.cunningham@asccension.org.
References
- 1.Meddings L., Myers R.P., Hubbard J., Shaheen A.A., Laupland K.B., Dixon E. A population-based study of pyogenic liver abscesses in the United States: incidence, mortality, and temporal trends. Am J Gastroenterol. 2010;105(1):117–124. doi: 10.1038/ajg.2009.614. [DOI] [PubMed] [Google Scholar]
- 2.Mohsen A.H., Green S.T., Read R.C., McKendrick M.W. Liver abscess in adults: ten years experience in a UK centre. QJM. 2002;95(12):797–802. doi: 10.1093/qjmed/95.12.797. [DOI] [PubMed] [Google Scholar]
- 3.Altemeier W.A., Culbertson W.R., Fullen W.D. Intra-abdominal sepsis. Adv Surg. 1971;5:281–333. [PubMed] [Google Scholar]
- 4.Rahimian J., Wilson T., Oram V., Holzman R.S. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis. 2004;39(11):1654–1659. doi: 10.1086/425616. [DOI] [PubMed] [Google Scholar]
- 5.Ali A.H., Smalligan R.D., Ahmed M., Khasawneh F.A. Pyogenic liver abscess and the emergence of Klebsiella as an etiology: a retrospective study. Int J Gen Med. 2013;7:37–42. doi: 10.2147/IJGM.S54448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Drancourt M., Bollet C., Carta A., Rousselier P. Phylogenetic analyses of Klebsiella species delineate Klebsiella and Raoultella gen. nov., with description of Raoultella ornithinolytica comb. nov., Raoultella terrigena comb. nov. and Raoultella planticola comb. nov. Int J Syst Evol Microbiol. 2001;51(Pt 3):925–932. doi: 10.1099/00207713-51-3-925. [DOI] [PubMed] [Google Scholar]
- 7.Sitaula S., Shahrrava A., Al Zoubi M., Malow J. The first case report of Raoultella planticola liver abscess. IDCases. 2016;5:69–71. doi: 10.1016/j.idcr.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seng P., Boushab B.M., Romain F., Gouriet F., Bruder N., Martin C. Emerging role of Raoultella ornithinolytica in human infections: a series of cases and review of the literature. Int J Infect Dis. 2016;45:65–71. doi: 10.1016/j.ijid.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 9.Hadano Y., Tsukahara M., Ito K., Suzuki J., Kawamura I., Kurai H. Raoultella ornithinolytica bacteremia in cancer patients: report of three cases. Intern Med. 2012;51(22):3193–3195. doi: 10.2169/internalmedicine.51.8349. [DOI] [PubMed] [Google Scholar]
- 10.Solak Y., Gul E.E., Atalay H., Genc N., Tonbul H.Z. A rare human infection of Raoultella ornithinolytica in a diabetic foot lesion. Ann Saudi Med. 2011;31(1):93–94. doi: 10.4103/0256-4947.75794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hajjar R., Schwenter F., Su S.H., Gasse M.C., Sebajang H. Community-acquired infection to Raoultella ornithinolytica presenting as appendicitis and shock in a healthy individual. J Surg Case Rep. 2018;2018(5) doi: 10.1093/jscr/rjy097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kanki M., Yoda T., Tsukamoto T., Shibata T. Klebsiella pneumoniae produces no histamine: raoultella planticola and Raoultella ornithinolytica strains are histamine producers. Appl Environ Microbiol. 2002;68(7):3462–3466. doi: 10.1128/AEM.68.7.3462-3466.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vos B., Laureys M. Giant renal cyst as cause of colic obstruction. Rev Med Brux. 2009;30(2):107–109. [PubMed] [Google Scholar]
- 14.Paasch C., Wilczek S., Strik M.W. Liver abscess and sepsis caused by Clostridium perfringens and Klebsiella oxytoca. Int J Surg Case Rep. 2017;41:180–183. doi: 10.1016/j.ijscr.2017.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]