Abstract
Background:
Surgical management may be indicated for patients with insertional Achilles tendinopathy (IAT) after failure of nonoperative management, and various surgical techniques have been described.
Hypothesis:
We present the technique and results of modified dorsal closing wedge calcaneal osteotomy, performed in a cohort of 28 consecutive patients. We hypothesized that this will be a safe procedure that can improve hindfoot pain and function for most patients who will return to preoperative daily life and sports activities.
Study Design:
Case series; Level of evidence, 4.
Methods:
A modified dorsal closing wedge osteotomy was performed in 28 patients (mean age, 54.7 years) from November 2015 to December 2016. All patients were followed for at least 2 years postoperatively.
Results:
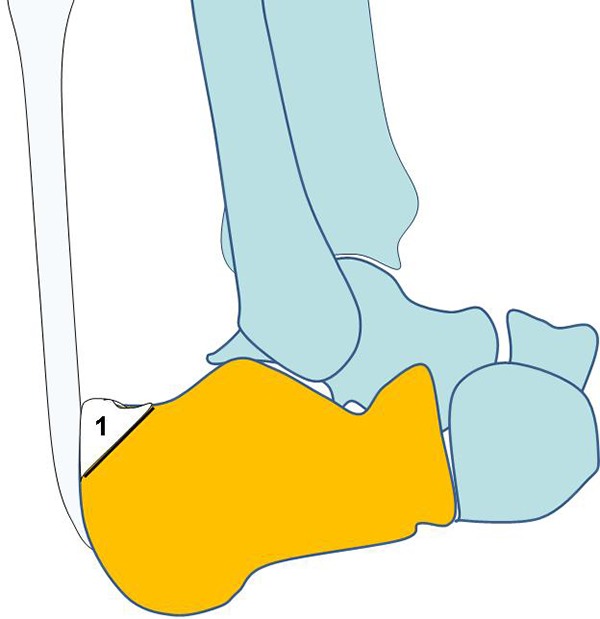
All osteotomies united at a mean of 5 weeks. The mean anatomic change in calcaneal length was 4 mm (range, 3-6 mm). The overall complication rate was 10.7%. There were 2 superficial wound infections (7.1%) and 1 instance of sural nerve–related paresthesia (3.5%) reported. All patients returned to their presurgical level of activities at a mean of 23 ± 8.0 weeks. Further, 3 of 4 patients who participated in recreational sports activities returned to their preinjury level. Visual analog scale and Victorian Institute of Sports of Australia–Achilles scores significantly improved postoperatively (P < .001) and continued to improve for 24 months.
Conclusion:
The modified dorsal closing wedge calcaneal osteotomy is a safe procedure and significantly improved pain and function in patients with IAT at 2 years after surgery.
Keywords: Achilles tendon, insertional tendinopathy, calcaneal osteotomy, dorsal closing wedge
Insertional Achilles tendinopathy (IAT) is distinct from midportion/noninsertional Achilles tendinopathy or retrocalcaneal bursitis.8,14,21,22 In general, posterior heel pain syndrome is a combination of 3 conditions, the so-called Haglund triad, which is characterized by IAT, retrocalcaneal bursitis, and Haglund deformity. Considering the anatomic location, symptoms, clinical findings, and histopathological results, the Achilles Tendon Study Group proposed the term insertional Achilles tendinopathy.13,21 The distal portion of the Achilles tendon (AT) is affected in 24% of patients presenting with pain at or around the AT.2 The management of IAT varies substantially; several surgical and nonsurgical treatment modalities have been described, but no consensus has been reached regarding the most effective management.2,19,22 Nonoperative modalities for IAT include rest, ice, nonsteroidal anti-inflammatory drugs, careful footwear selection, and activity avoidance.2,13 Eccentric exercises of the gastrocnemius-soleus complex, although beneficial for midportion tendinopathy, are not as effective for insertional tendinopathy, helping only 32% of patients.2,5 Extracorporeal shock wave therapy may play a role in chronic cases,19 and surgery is indicated in patients unresponsive to nonoperative therapy for at least 6 months.2,6 However, no consensus has been reached regarding the most appropriate surgical procedure to perform.7 Traditionally, IAT is treated surgically through a lateral approach to the insertion zone, removal of the retrocalcaneal bursa, excision of the posterior prominence of the calcaneal bone, and debridement of the insertion zone.13,16 Other open approaches include medial and midline longitudinal incisions as well as curvilinear incision.13 A transverse (Cincinnati) incision allows wide exposure of the insertion, debridement, and calcaneal osteotomy of the posterosuperior corner of the calcaneus2 with excellent outcomes.15 In calcific IAT, debridement of the calcific deposits can be so extensive as to dictate disinsertion of the AT and its reinsertion in the calcaneus with suture anchors.11,14 A dorsal closing wedge calcaneal osteotomy for the management of IAT was first described by Zadek in 193924 and later popularized by Keck and Kelly.9 It is considered a safe procedure with excellent results and a low rate of complications such as shortening of the os calcis and creation of a plantar beak on the apex of the osteotomy.6,7,9,24 The rationale for performing such calcaneal osteotomy to improve IAT-associated pain is to alter the mechanics of the insertion of the AT and avoid friction between the calcaneus and AT.13,20
We present the 2-year outcomes of a longitudinal investigation on the clinical and radiographic outcome of a modified dorsal closing wedge technique in patients with IAT.
Methods
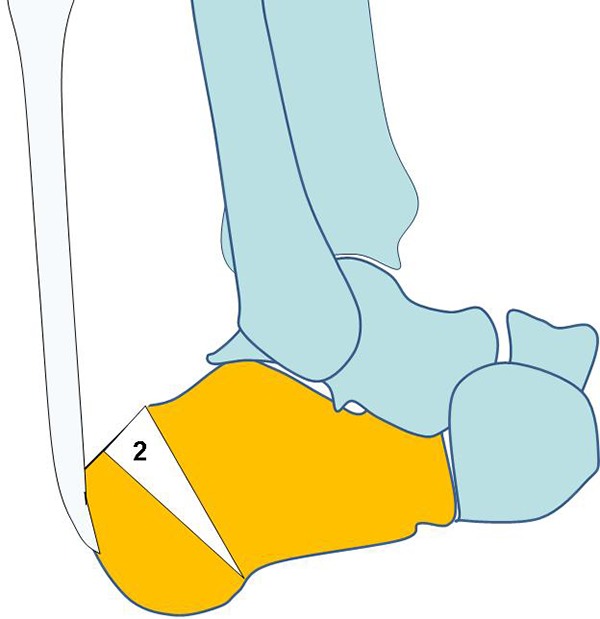
This study was approved by the local ethics committee of the University of Salerno. For the purposes of this study, we prospectively enrolled 28 patients from November 2015 to December 2016. All underwent the index procedure (modified dorsal closing wedge osteotomy of the calcaneus) for IAT. All patients were tertiary referrals to the senior author (N.M.), and in all of the patients, nonoperative treatments of at least 6 months had not resulted in amelioration of their symptoms. Complete or modified rest from recreational activities, nonsteroidal anti-inflammatory medication, physiotherapy, ultrasound therapy, intrabursal or peritendinous injection with prolotherapy, corticosteroids, or platelet-rich plasma had not produced significant pain relief. Patients were not entered in the present study if they were smokers or had diabetes, hypothyroid, gout, or autoimmune disease. Patients were excluded if previous surgery to the involved foot and ankle had been performed. All patients underwent clinical assessment by the senior author, who confirmed the diagnosis of IAT. Patients were examined while prone: Pain was elicited at palpation of the posterior aspect of the calcaneus at the insertion of the AT. The Royal London Hospital test was positive: The tenderness and pain at palpation of the insertion of the AT with the ankle plantar flexed were relieved when palpation was performed with the ankle dorsiflexed.12 A weightbearing lateral radiograph of the involved hindfoot excluded calcific insertional tendinopathy and showed evidence of a prominent posterior calcaneal tuberosity (Haglund prominence).
Degenerative tendinopathy affecting less than 50% of the insertion of the AT into the calcaneus was confirmed on preoperative magnetic resonance imaging scans.
Surgical Technique
Patients had surgery under spinal anesthesia, with a calf tourniquet 3 cm distal to the head of the fibula, while positioned in the lateral position. Preoperatively, 2 g of cefazolin was injected through an intravenous cannula into a dorsal vein of the foot of the leg to be operated on, after exsanguination of the limb was performed with an Esmarch bandage and inflation of the tourniquet to 250 mm Hg.3,4,10,23 A short lateral incision was made just anterior to the AT and progressing in a proximal to distal direction at a 45° angle to the long axis of the calcaneus. A full-thickness flap was elevated, and the lateral wall of the calcaneus was exposed. The incision always lay well posterior in relation to the course of the sural nerve. The posterosuperior corner of the calcaneus was removed by use of a sagittal saw (Figure 1).
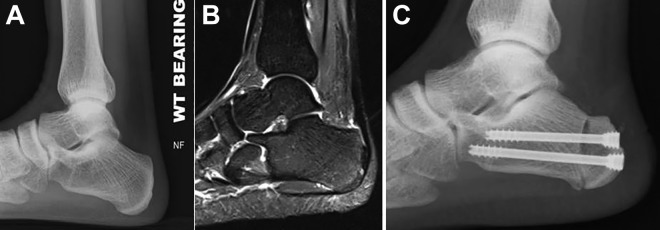
Figure 1.
The posterosuperior corner of the calcaneus (1) is excised.
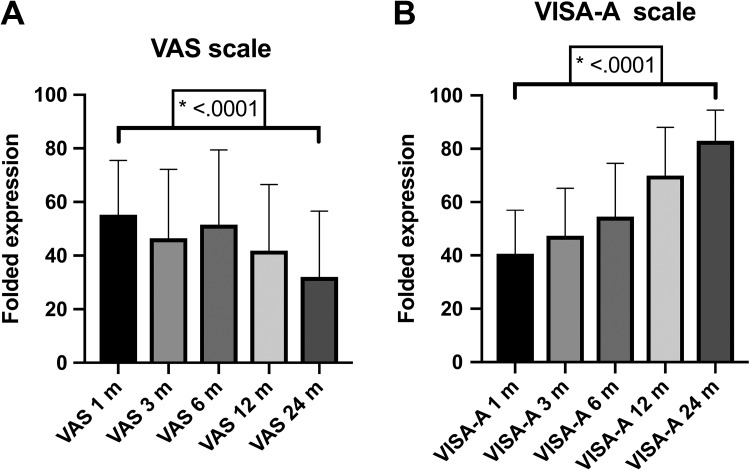
The osteotomy was initiated just superior to the calcaneal insertion of the Achilles fibers and was carried out at approximately a 45° angle to the long axis of the tendon up to the posterosuperior surface of the calcaneus. The surgeon made a 2.5-cm vertical incision at the center of the posterior aspect of the calcaneus, taking care to place the incision distal to the insertion of the AT on the calcaneus. The dorsally based wedge calcaneal osteotomy was then performed through the lateral incision (Figure 2). The first cut of the osteotomy was performed 1.5 cm anterior to the AT, tilted at about a 40° angle to the major axis of the calcaneus. The second cut was made 1 to 1.2 cm anterior to the first osteotomy, performed at a convergent angle so as to meet the first cut at the plantar apex, taking care to preserve a bone hinge at the apex of the wedge close to the plantar surface of the calcaneus. In this way, the dorsal base of the wedge was about 1 cm. The wedge was removed, and the osteotomy was gently closed (Figure 3).
Figure 2.
The dorsal closing wedge osteotomy (2) is schematically shown.
Figure 3.

Intraoperative view. The posterosuperior bony prominence has been removed, the osteotomy has been completed, and the bone wedge has been removed from the calcaneus.
Next, 2 parallel Kirschner wires, 1 superior and 1 inferior approximately 1.2 cm apart from each other, were advanced from the posterior aspect of the calcaneus in the desired direction of the cannulated screws that would be used for fixation. Once the optimal direction had been ascertained, the Kirschner wires were advanced for 1 cm in the calcaneus. Once the osteotomy surfaces were juxtaposed, the 2 Kirschner wires were advanced to a suitable position and checked with image intensification; then, routine fixation was undertaken with 2 partially threaded cancellous screws of appropriate length (Figures 4 and 5).
Figure 4.
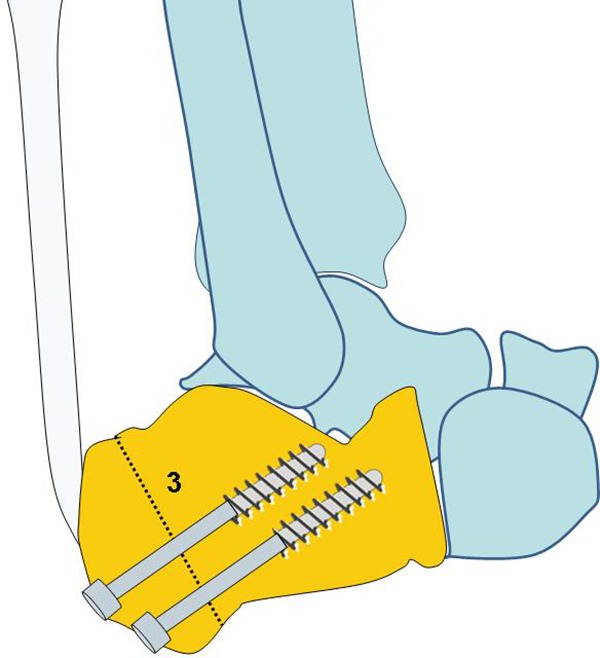
After the bone wedge has been removed, the opposing osteotomy surfaces (dotted line) are brought together and fixed with 2 screws. Note the proximal and anterior translation of the Achilles tendon insertion compared with Figure 2.
Figure 5.
Preoperative (A) radiograph and (B) magnetic resonance image and (C) postoperative radiograph of a patient undergoing surgical management for insertional Achilles tendinopathy.
A No. 2 Vicryl continuous suture (Polyglactin 910 braided absorbable suture; Johnson & Johnson) was used for the deeper tissues, and the skin was closed with staples or with continuous subcuticular suture using Monocryl No. 3-0 (Ethicon). The operated limb was then immobilized in a below-knee cast with the foot plantarflexed for 4 weeks.
Postoperative Protocol
Patients were administered 100 mg of aspirin daily until full mobility was achieved. Patients were allowed to bear weight in the cast as tolerated, as soon as possible, with crutches and were instructed to undertake mobilization exercises of the toes, knee, and hip every waking hour. After 4 weeks, the cast was removed and an Aircast walker (DJO) was applied, with the foot plantarflexed. After 2 months, mobilization exercises were encouraged and patients were allowed to bear weight fully in the walker. Proprioception exercises were initiated, and ankle and subtalar joint mobilization was undertaken. Isometric contraction of the gastrocnemius-soleus complex, stationary cycling, and swimming were encouraged. Gradual progression to recreational activities at 3 months was planned according to each patient’s progress. At 3 months from the index procedure, the walker was removed, and patients gradually returned to their normal activities thereafter.
Follow-up
All patients were followed up with at 1, 3, 6, 12, and 24 months after surgery. A visual analog scale (VAS) pain score (range, 0-100) and the Victorian Institute of Sports of Australia–Achilles (VISA-A) score18 (Appendix) were recorded preoperatively and then postoperatively at each patient’s follow-up appointments (3, 6, 12, and 24 months). Outcome assessment was performed by an orthopaedic fellow who had not participated in the management of the patients (A.D.A.), assessing patients independently of the treating surgeon.
Radiographic assessment, consisting of lateral hindfoot and axial calcaneal radiographs, included union of the osteotomy and measurement of calcaneal length before and after surgery. On the lateral hindfoot radiograph, a line was drawn parallel to the calcaneocuboid joint to connect the most superior and inferior points on the anterior calcaneus. From the midpoint of this line, the line to the most posterior aspect of the calcaneus revealed the length of the calcaneus. All measurements were performed at follow-up visits by an orthopaedic fellow who was fully conversant with such measurement techniques and who made the measurements independently from the treating surgeon. The researcher measured each radiograph on 2 separate occasions, 2 weeks apart from one another. If the 2 measurements were more than 5% discordant, the measurements were performed again. The mean of the 2 measurements was used for statistical purposes.
Statistical Analysis
Statistical analysis was performed with repeated-measures 1-way analysis of variance. The Geisser-Greenhouse correction was used for categorical variables, and the Student t test for paired data was used to compare VAS and VISA-A scores at 1 and 24 months. Data were entered in an Excel spreadsheet (Microsoft Corporation) and analyzed by use of GraphPad Prism 8.0 Statistical Software (GraphPad Software). A P value less than .05 was considered significant.
Results
The study enrolled 28 patients (13 men, 15 women; mean age, 54.7 years; range, 37-75 years). Of the women, 10 were postmenopausal. All patients were followed up with for at least 2 years (range, 2-2.5 years). The overall complication rate was 10.7%. There were 2 cases (7.1%) of superficial wound infection, which were treated successfully with oral antibiotics. Further, 1 patient (3.5%) reported paresthesia in the distribution area of the sural nerve. The patient was managed expectantly, and the symptoms resolved with time. No major complications (eg, deep venous thrombosis, deep infection, malunion or nonunion of the osteotomy) were recorded. All patients returned to their presurgery level of activities. Of 4 patients who practiced recreational sport activity, 3 returned to their preinjury level. Return to previous activities ranged from 4 months to more than 8 months, with a mean ± SD time of 23 ± 8.0 weeks.
The median ± SD VAS score at 1 month was 55.3 ± 20.2 (range, 20-90), and the median VAS score at 24 months was 32 ± 24.6 (range, 10-90) (P < .0001) (Figure 6A). The median VISA-A score at 1 month was 40.6 ± 16.3 (range, 12-75), and the median VISA-A score after 2-year follow-up was 83 ± 11.4 (range, 60-100) (P < .0001) (Figure 6B).
Figure 6.
A statistically significant difference (P < .0001) was found on comparison of (A) visual analog scale (VAS) and (B) Victorian Institute of Sports of Australia–Achilles (VISA-A) scores at 1 and 24 months.
Radiographic examination revealed healing of the calcaneal osteotomy at a mean of 5 weeks (range, 4-10 weeks). The calcaneal length was a mean of 83 mm (range, 73-95 mm) before the osteotomy and 79 mm (range, 72-92 mm) after surgery. The mean anatomic change in calcaneal length was 4 mm (range, 3-6 mm).
Discussion
The most important finding of the present study is that the dorsal closing wedge osteotomy associated with an osteotomy of the posterosuperior corner of the calcaneus is safe and effective and can be reliably used to aid in the resolution of symptoms after failure of nonoperative management of IAT. The VAS and VISA-A scores showed improvement of symptoms, especially pain, during daily activities, with significant differences between preoperative assessment and the final clinical review for both VAS and VISA-A scores (P < .0001).
Controversy remains regarding the optimal surgical treatment of IAT when nonoperative management fails.13,16,17 In the current study, a modified dorsal closing wedge osteotomy produced encouraging results at 2-year follow-up. A dorsally based closing wedge osteotomy was first described by Zadek24 and popularized by Keck and Kelly.9 The original Zadek osteotomy did not include removal of the so-called Haglund calcaneal bony prominence. Given that in theory, IAT pathomechanics identify friction between bone and tendon as a causative factor, we believed that resection of the bony (Haglund) deformity was necessary (always present in our cohort of patients). Removal of the Haglund bony prominence eliminates friction and impingement between the AT and calcaneus, therefore maximizing the “off-loading” effect with the presented technique compared with the conventional Zadek osteotomy.13,20 Furthermore, choosing the location of the osteotomy (see Figures 1 and 2) allows anterior and proximal translation of the insertion of the AT, thus possibly decreasing the Fowler-Philip angle (angle between the inferior calcaneus and the posterior surface of the calcaneus). We did not differentiate our management strategy based on measurement of Fowler-Phillip angle, as the same surgical technique was applied to all patients with IAT for whom nonoperative management had failed. We adopted the rationale of performing a dorsal closing wedge (Zadek-type) osteotomy to change the mechanical environment of the AT insertion in all patients, irrespective of the sagittal alignment of the calcaneus (eg, assessing Fowler-Phillip angle). We believe that one should also consider the direct impingement of tendon against the Haglund prominence, which can contribute to symptoms. Thus, our rationale was to change the loading axis of the AT by performing an osteotomy, not to neglect the Haglund prominence when it was present. Nevertheless, resecting the Haglund prominence and performing the osteotomy were easily feasible through the lateral surgical approach and were unlikely to add morbidity or prolong recovery. Boffeli et al1 used a similar technique to surgically manage IAT, but the location of their osteotomy was more posterior than the one described in the present investigation.
Georgiannos et al,7 in a case series of 52 patients, reported a complication rate (10.9%) that was very similar to ours, with good clinical results (VISA-A score), although their patients were younger, and most were athletes. Georgiannos et al7 used a technique that was quite different from ours, producing a more anterior first osteotomy cut and using a single cannulated screw or staples to stabilize the osteotomy. We preferred to perform the more posterior cut first, preventing instability of the fragment. Recently, Georgiannos et al6 published a modification of their technique using temporary Kirschner wire fixation to avoid instability of the osteotomy.
The senior author previously reported the surgical management of IAT using a Cincinnati approach with debridement of the insertional portion of AT. Although successful, allowing return to activities of daily living including sport, this approach required approximately 9 months of rehabilitation.14 With the current technique, debridement of AT was not performed. It remains debatable, however, whether tendon debridement is required once the insertion of the AT has been off-loaded, changing its mechanics through the closing wedge osteotomy, which could be useful to manage failure of previous surgery in patients with IAT.
Comparative studies may enlighten the debate regarding what type of calcaneal osteotomy yields better results and whether additional procedures (eg, debridement of AT insertion) are required. In our cohort, we chose not to debride the tendon itself, despite preoperative imaging findings of tendinopathy, and good results were nevertheless obtained.
A common cause of failure of technically well-performed surgery seems to be attempting to return to sport too early. Because IAT seems to result from abnormal stress-shielding rather than simple overuse, it is important to respect the postoperative protocol and let the tendon adapt to the changed loads, particularly in high-level athletes.20
Limitations
This study has some limitations. The study sample was relatively small. We also acknowledge that functional measurements could have been undertaken, including, for example, formal testing of the force exerted by the gastrocnemius-soleus complex before the procedure and at the latest follow-up.
The procedures reported in the present investigation have been performed by an experienced fellowship-trained orthopaedic surgeon with a special interest in the field. In this particular instance, the surgeon was well beyond his learning curve, as he had been using this technique for nearly 10 years before initiating this particular study. We caution, therefore, that meticulous attention to detail, and especially to a slow postoperative rehabilitation, should be undertaken.
Our sample included only relatively low-demand individuals, and in this respect, further investigations have to ascertain whether this approach would be beneficial in a different population of patients—for example, athletic patients.
Finally, our series did not include a control group. A randomized controlled trial comparing 2 or more techniques could be planned to demonstrate which one offers superior outcomes. One has to emphasize, however, the difficulties such a study design would face, given the variety of conditions (eg, Haglund calcaneal bony prominence, retrocalcaneal bursa, intratendinous calcification) that can result in posterior heel pain, often occurring in combination, and also the different pathomechanics associated with foot deformity.
Conclusion
The modified dorsal closing wedge osteotomy reported in the present investigation is a safe surgical technique for the management of IAT, with good medium-term results. It produces a predictable, significant improvement in pain relief at a minimum 2-year follow-up.
Appendix
The Victorian Institute of Sports of Australia–Achilles (VISA-A) Questionnaire: An Index of the Severity of Achilles Tendinopathy
In this questionnaire, the term pain refers specifically to pain in the Achilles tendon region.
-
For how many minutes do you have stiffness in the Achilles region on first getting up?
-
Once you are warmed up for the day, do you have pain when stretching the Achilles tendon fully over the edge of a step (keeping the knee straight)?

-
After walking on flat ground for 30 minutes, do you have pain within the next 2 hours? (If unable to walk on flat ground for 30 minutes because of pain, score 0 for this question).

-
Do you have pain walking downstairs with a normal gait cycle?

-
Do you have pain during or immediately after doing 10 single-leg heel raises from a flat surface?

-
How many single-leg hops can you do without pain?

-
Are you currently undertaking sport or other physical activity?
- Please complete either A, B, or C in this question.
- If you have no pain while undertaking Achilles tendon loading sports, please complete question 8A only.
- If you have pain while undertaking Achilles tendon loading sports but it does not stop you from completing the activity, please complete question 8B only.
- If you have pain that stops you from completing Achilles tendon loading sports, please complete question 8C only.
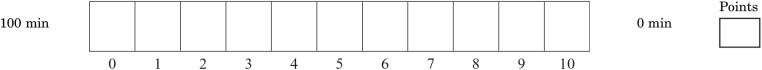
-
If you have no pain while undertaking Achilles tendon loading sports, for how long can you train or practice?

-
If you have some pain while undertaking an Achilles tendon loading sport, but it does not stop you from completing your training or practice, how long can you train or practice?

-
If you have pain that stops you from completing your training or practice in an Achilles tendon loading sport, how long can you train or practice?
Footnotes
Final revision submitted November 2, 2019; accepted December 3, 2019.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the ethics committee of the University of Salerno.
References
- 1. Boffeli TJ, Peterson MC. The Keck and Kelly wedge calcaneal osteotomy for Haglund’s deformity: a technique for reproducible results. J Foot Ankle Surg. 2012;51(3):398–401. [DOI] [PubMed] [Google Scholar]
- 2. Carmont MR, Maffulli N. Management of insertional Achilles tendinopathy through a Cincinnati incision. BMC Musculoskelet Disord. 2007;8:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. de Lalla F. Antibiotic prophylaxis in orthopedic prosthetic surgery. J Chemother. 2001;13(1):48–53. [DOI] [PubMed] [Google Scholar]
- 4. de Lalla F, Viola R, Pellizzer G, Lazzarini L, Tramarin A, Fabris P. Regional prophylaxis with teicoplanin in monolateral or bilateral total knee replacement: an open study. Antimicrob Agents Chemother. 2000;44:316–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fahlstrom M, Jonsson P, Lorentzon R, Alfredson H. Chronic Achilles pain treated with eccentric calf muscle training. Knee Sports Surg Traumatol Arthrosc. 2003;11(5):327–333. [DOI] [PubMed] [Google Scholar]
- 6. Georgiannos D, Kitridis D, Bisbinas I. Dorsal closing wedge calcaneal osteotomy for the treatment of insertional Achilles tendinopathy: a technical tip to optimize its results and reduce complications. Foot Ankle Surg. 2018;24(2):115–118. [DOI] [PubMed] [Google Scholar]
- 7. Georgiannos D, Lampridis V, Vasiliadis A, Bisbinas I. Treatment of insertional Achilles pathology with dorsal wedge calcaneal osteotomy in athletes. Foot Ankle Int. 2017;38(4):381–387. [DOI] [PubMed] [Google Scholar]
- 8. Kearney R, Costa ML. Insertional Achilles tendinopathy management: a systematic review. Foot Ankle Int. 2010;31(8):689–694. [DOI] [PubMed] [Google Scholar]
- 9. Keck S, Kelly P. Bursitis of the posterior part of the heel, evaluation of surgical treatment of eighteen patients. J Bone Joint Surg. 1965;47:267–273. [PubMed] [Google Scholar]
- 10. Lazzarini L, Novelli A, Marzano N, et al. Regional and systemic prophylaxis with teicoplanin in total knee arthroplasty: a tissue penetration study. J Arthroplasty. 2003;18:342–346. [DOI] [PubMed] [Google Scholar]
- 11. Maffulli N, Del Buono A, Testa V, Capasso G, Oliva F, Denaro V. Safety and outcome of surgical debridement of insertional Achilles tendinopathy using a transverse (Cincinnati) incision. J Bone Joint Surg Br. 2011;93-B:1503–1507. [DOI] [PubMed] [Google Scholar]
- 12. Maffulli N, Kenward MG, Testa V, Capasso G, Regine R, King JB. Clinical diagnosis of Achilles tendinopathy with tendinosis. Clin J Sport Med. 2003;13(1):11–15. [DOI] [PubMed] [Google Scholar]
- 13. Maffulli N, Saxena A, Wagner E, Torre G. Achilles insertional tendinopathy: state of the art. J ISAKOS. 2019;4:48–57. [Google Scholar]
- 14. Maffulli N, Wong J, Almekinder LC. Types and epidemiology of tendinopathy. Clin Sports Med. 2003;22:675–672. [DOI] [PubMed] [Google Scholar]
- 15. Maffulli N, Testa V, Capasso G, Sullo A. Calcific insertional Achilles tendinopathy: reattachment with bone anchors. Am J Sports Med. 2004;32:174–182. [DOI] [PubMed] [Google Scholar]
- 16. Oshri Y, Palmanovich E, Brin YS, et al. Chronic insertional Achilles tendinopathy: surgical outcomes. Muscles Ligaments Tendons J. 2012;2(2):91–95. [PMC free article] [PubMed] [Google Scholar]
- 17. Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006;45(5):508–521. [DOI] [PubMed] [Google Scholar]
- 18. Robinson JM, Cook JL, Purdam C, et al. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med. 2001;35(5):335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rompe JD, Furia J, Maffulli N. Eccentric loading compared with shock wave treatment for chronic insertional Achilles tendinopathy: a randomized, controlled trial. J Bone Joint Surg Am. 2008;90(1):52–61. [DOI] [PubMed] [Google Scholar]
- 20. Sayana MK, Maffulli N. Insertional Achilles tendinopathy. Foot Ankle Clin N Am. 2005;10:309–320. [DOI] [PubMed] [Google Scholar]
- 21. van Dijk CN, van Sterkenburg MN, Wiegerinck JI, Karlsson J, Maffulli N. Terminology for Achilles tendon related disorders. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):835–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wiegerinck JI, Kerkhoffs GM, van Sterkenburg MN, Sierevelt IN, van Dijk CN. Treatment for insertional Achilles tendinopathy: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:1345–1355. [DOI] [PubMed] [Google Scholar]
- 23. Young SW, Zhang M, Freeman JT, Vince KG, Coleman B. Higher cefazolin concentrations with intraosseous regional prophylaxis in TKA. Clin Orthop Relat Res. 2013;471(1):244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zadek I. An operation for the cure of achillobursitis. Am J Surg. 1939;43:542–546. [Google Scholar]