Abstract
Marijuana is seeing increased use both globally and domestically. Yet, the scientific community has not fully reached consensus about what negative health effects and to what extent marijuana smoking may cause. In this study, we evaluated the associations between the body burden of polycyclic aromatic hydrocarbons (PAHs) among marijuana smokers and the smoking heaviness. We observed a clear, increasing trend of PAH body burdens as marijuana smoking increased. The findings highlight the importance of capturing the heaviness of marijuana smoking in future studies, and support the need for well-designed toxicological and epidemiological studies for understanding the health effects of marijuana use in a changing environment.
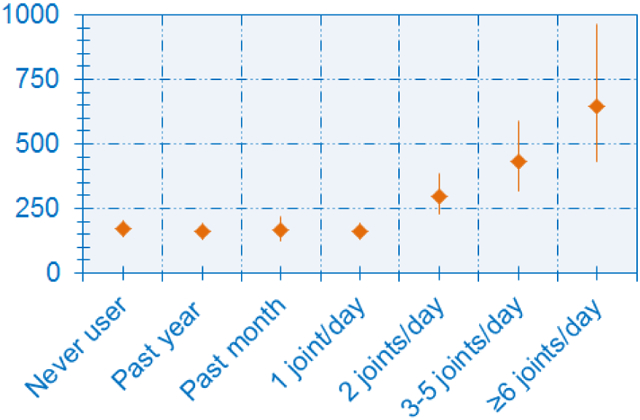
Graphical Abstract
Marijuana use is increasing, and is now the world’s third most-popular recreational drug following alcohol and tobacco.1 This trend will likely continue with the increasing legalization of medicinal and recreational marijuana. Widespread use raises concerns about adverse health effects as many toxic chemicals identified in tobacco smoke are also present in marijuana smoke.2, 3 Use of marijuana has been found to be associated with many adverse health consequences, including anxiety and panic in naive users,4 impaired lung function,5 chronic bronchitis,6 increased heart rate7 and myocardial infarction.8 Long-term marijuana use is also associated with impaired cognitive abilities,9 and abnormal brain function.10 Yet, the scientific community has not fully reached consensus about what negative health effects and to what extent marijuana smoking may cause. For instance, while some studies indicated plausible associations between marijuana smoking and lung cancer,11 other reports have concluded that “smoking marijuana does not increase the risk for certain cancer”, 12 including lung cancer in adults. To further explore potential dose-response relationships between marijuana smoking and exposures, in the present study, we examined the associations between the body burdens of polycyclic aromatic hydrocarbons (PAHs), a group of carcinogens present in marijuana smoke,2, 3 and the heaviness of marijuana smoking.
We analyzed the data collected from the National Health and Nutrition Examination Surveys (NHANES) (2005–2014), a series of cross-sectional health examination surveys representative of the U.S. civilian noninstitutionalized population that are conducted by the National Center for Health Statistics (NCHS) of the U.S. Centers for Disease Control and Prevention. Participants included in this analysis were ≥ 18 years old.
PAH metabolite levels in urine samples during NHANES 2005–2012 were measured using isotope-dilution gas chromatography (GC) coupled with tandem mass spectrometry (MS/MS) with limits of detection (LOD) in the range of 7–19 pg/mL.13 In NHANES 2013–2014, an isotope dilution-high performance liquid chromatography (HPLC)– MS/MS method with LODs ranging from 7–90 pg/mL was used to quantify the urinary levels of PAH metabolites.14 Urinary creatinine concentration was measured using a colorimetric method based on Jaffé rate reaction.
We merged the survey data according to NCHS recommendations,15 and we grouped participants into never users and exclusive ever marijuana smokers. Participants were categorized as never users if they (1) had serum cotinine levels ≤ 10 ng/mL; (2) self-reported never used marijuana or hashish and never smoked at least 100 cigarettes in life and never smoked any tobacco products within the last five days prior to their NHANES physical examination. Participants were considered as exclusive ever marijuana smokers if they: (1) self-reported ever smoked marijuana or hashish in life time; (2) had serum cotinine levels ≤ 10 ng/mL; (3) never smoked at least 100 cigarettes in life and never smoked any tobacco products within the last five days of the survey. Exclusive ever marijuana smokers were further categorized into exclusive daily, past-month and past-year marijuana smokers. Sample sizes and characteristics for demographic and socioeconomic covariates are given in Table 1.
Table 1 –
Demographic Characteristics of nonusers and exclusive marijuana users in NHANES 2005-2014
| Exclusive daily marijuana smokers (per day) a | Exclusive ever marijuana smokers b | ||||||
|---|---|---|---|---|---|---|---|
| 1-joint | 2 joints | 3-5 joints | ≥ 6 joints | Last-month | Last-year | Never user c | |
| Total, N | 25 | 27 | 16 | 5 | 32 | 100 | 1819 |
| Gender, No. (%) | |||||||
| Male | 18 (72) | 19 (68) | 11 (69) | 3 (60) | 13 (41) | 57 (57) | 711 (39) |
| Female | 7 (28) | 8 (32) | 5 (31) | 2 (40) | 19 (59) | 43 (43) | 1108 (61) |
| Age, mean (SD), year | 34 (3.1) | 36 (2.8) | 33 (3.5) | 27 (2.6) | 29 (1.7) | 30 (1.3) | 39 (0.4) |
| Race/ethnicity, No. (%) | |||||||
| Non-Hispanic White | 8 (32) | 16 (57) | 5 (31) | 3 (60) | 11 (34) | 45 (45) | 495 (27) |
| Non-Hispanic Black | 5 (20) | 4 (18) | 4 (25) | 2 (40) | 14 (44) | 25 (25) | 371 (20) |
| Mexican American | 3 (12) | 5 (18) | 2 (13) | - | 4 (13) | 16 (16) | 443 (25) |
| Other race | 9 (36) | 2 (7) | 5 (31) | - | 3 (9) | 14 (14) | 510 (28) |
Participants who self-reported smoked marijuana or hashish daily within the last five days of the survey, but had serum cotinine levels were ≤ 10 ng/mL and never smoked at least 100 cigarettes in life & never smoked any tobacco products within the last five days of the survey.
Participants who self-reported ever smoked marijuana or hashish during last month and last year from the time of the survey, but had serum cotinine levels were ≤ 10 ng/mL and never smoked at least 100 cigarettes in life & never smoked any tobacco products within the last five days of the survey.
Participants whose serum cotinine levels were ≤ 10 ng/mL and self-reported never used marijuana or hashish & never smoked at least 100 cigarettes in life & never smoked any tobacco products within the last five days of the survey.
Using SAS (version 9.4; SAS Institute Inc.), we performed multiple regression analyses to calculate the least square geometric means (hereafter called – adjusted GM) and 95% confidence intervals (95% CI) from natural log-transformed urinary PAH metabolite concentrations, adjusted for age, race/ethnicity and gender. Models also adjusted for natural log-transformed serum cotinine and urinary creatinine concentrations to account for potential variation from secondhand tobacco smoke exposure and urine dilutions among spot samples, respectively.2, 16 Concentrations < the LOD were substituted with the LOD divided by the square root of 2, using the same method used by the CDC (2018).17 Differences with p < .05 were considered statistically significant.
Among 2,024 participants who had valid laboratory measurements and questionnaire data, we identified 1,819 never users and 205 exclusive ever marijuana users Among exclusive ever marijuana users, 25 smoked 1 joint of marijuana daily (mean age [SD], 34 [3.1] years), 27 smoked 2 joints daily (36 [2.8] years), 16 smoked 3–5 joints daily (33 [3.5] years), and 5 smoked ≥ 6 joints daily (27 [2.6] years). We identified 32 (29 [1.7] years) and 100 (30 [1.3] years) exclusive marijuana users who smoked marijuana in the last month and last year, respectively.
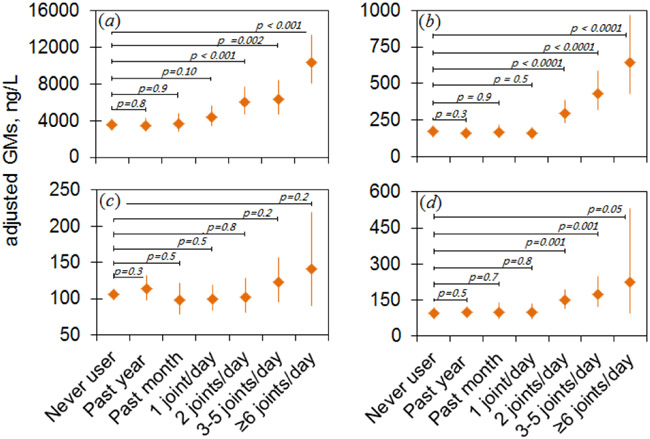
PAH metabolites were detected in all urine samples from the participants in this analysis. Adjusted GMs of PAH metabolites, except for 1-hydroxyphenanthrene, were significantly higher in exclusive daily marijuana users who smoked at least 2 joints per day than in nonusers, last month and last year users (p<0.05) (Figure 1). No statistically significant difference in metabolite levels were identified among never users, exclusive 1-joint daily, past-month and past-year marijuana users.
Figure 1.
Adjusted geometric means of urinary concentrations of PAH metabolites (ng/L). (a) 2-Hydroxynaphthalene. (b) 2-Hydroxyfluorene. (c) 1-Hydroxyphenanthrene. (d) 1-Hydroxypyrene. Categories refer to Table. Error bars indicate 95% confidence intervals.
We observed that the metabolite of phenanthrene, 1-hydroxyphenanthrene, was not as a sensitive marker of marijuana smoke as other PAH metabolites (Figure 1). It is highly likely that differences exist in the absorption, distribution, metabolism and excretion mechanisms of PAHs in human body. Nevertheless, we identified a clear, increasing trend of PAH body burden as marijuana smoking increased. This observation provides evidence supporting the plausible association between marijuana smoking and adverse health effects, including lung cancer.
We did not observe a significant difference in PAH exposure among nonusers, exclusive marijuana past year, past month, or 1 joint/day users. This finding suggests that low level marijuana use does not contribute significantly beyond background exposure levels in the general population resulting from other sources, such as gas/oil/coal, vehicle exhaust, wood smoke and diets, which could “dilute” the contributions to the body burdens from marijuana smoke exposure. Given that marijuana is often used infrequently, our findings highlight the importance of capturing the heaviness of marijuana smoking (frequency and quantity) in future epidemiological studies.
In addition, although participants included in this study were from a representative sample of the general US population, sample sizes for exclusive marijuana ever smokers were small. This was mainly because the drug relevant questions had received low responding rates. Identifying and obtaining a sufficient sample of heavy marijuana users is a common challenging issue in exposure and epidemiological studies due to personal, social and legal considerations. For instance, in nearly all studies reviewed in the latest report by National Academies of Sciences, Engineering, and Medicine (NASEM),12 sample sizes were small for cancer patients who consumed high amounts of marijuana. Small sample unavoidably result in broad variability in measurements. In epidemiological studies, small sample size is often a major source of bias. Overall, this study supports the need for well-designed toxicological and epidemiological studies for understanding the health effects of marijuana use in a changing environment.
Acknowledgments
Funding Sources
This study was supported by Roswell Park Comprehensive Cancer Center.
ABBREVIATIONS
- NHANES
National Health and Nutrition Examination Surveys
- PAHs
polycyclic aromatic hydrocarbons
- GC
gas chromatography
- HPLC
high performance liquid chromatography
- MS/MS
tandem mass spectrometry
- LOD
limit of detection
- GM
geometric mean
Footnotes
The authors declare no competing financial interest.
REFERENCES
- (1).UNODC (2014). World Drug Report. United Nations Office on Drugs and Crime, http://www.unodc.org/documents/wdr2014/World_Drug_Report_2014_web.pdf (accessed on May 7, 2018). [Google Scholar]
- (2).Wei B, Alwis KU, Li Z, Wang L, Valentin-Blasini L, Sosnoff CS, Xia Y, Conway KP, and Blount BC (2016). Urinary concentrations of PAH and VOC metabolites in marijuana users. Environ. Int 88, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Moir D, Rickert WS, Levasseur G, Larose Y, Maertens R, White P, and Desjardins S (2007). A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem. Res. Toxicol 21, 494–502. [DOI] [PubMed] [Google Scholar]
- (4).Hall W, and Degenhardt L (2009). Adverse health effects of non-medical cannabis use. The Lancet 374, 1383–1391. [DOI] [PubMed] [Google Scholar]
- (5).Taylor DR, Fergusson DM, Milne BJ, Horwood LJ, Moffitt TE, Sears MR, and Poulton R (2002). A longitudinal study of the effects of tobacco and cannabis exposure on lung function in young adults. Addiction 97, 1055–1061. [DOI] [PubMed] [Google Scholar]
- (6).Tetrault JM, Crothers K, Moore BA, Mehra R, Concato J, and Fiellin DA (2007). Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch. Inter. Med 167, 221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Jones RT (2002). Cardiovascular system effects of marijuana. J. Clin. Pharmacol 42. [DOI] [PubMed] [Google Scholar]
- (8).Mittleman MA, Lewis RA, Maclure M, Sherwood JB, and Muller JE (2001). Triggering myocardial infarction by marijuana. Circulation 103, 2805–2809. [DOI] [PubMed] [Google Scholar]
- (9).Solowij N, Stephens RS, Roffman RA, Babor T, Kadden R, Miller M, Christiansen K, McRee B, and Vendeti J (2002). Cognitive functioning of long-term heavy cannabis users seeking treatment. JAMA. 287, 1123–1131. [DOI] [PubMed] [Google Scholar]
- (10).Block RI, O'leary DS, Ehrhardt JC, Augustinack JC, Ghoneim MM, Arndt S, and Hall JA (2000). Effects of frequent marijuana use on brain tissue volume and composition. Neuroreport 11, 491–496. [DOI] [PubMed] [Google Scholar]
- (11).Mehra R, Moore BA, Crothers K, Tetrault J, and Fiellin DA (2006). The association between marijuana smoking and lung cancer: a systematic review. Arch. Inter. Med 166, 1359–1367. [DOI] [PubMed] [Google Scholar]
- (12).NASEM (2017). National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research, http://nationalacademies.org/hmd/reports/2017/health-effects-of-cannabis-and-cannabinoids.aspx (accessed on May 7, 2018). [PubMed]
- (13).Li Z, Romanoff LC, Trinidad DA, Pittman EN, Hilton D, Hubbard K, Carmichael H, Parker J, Calafat AM, and Sjödin A (2014). Quantification of 21 metabolites of methylnaphthalenes and polycyclic aromatic hydrocarbons in human urine. Anal. Bioanal. Chem 406, 3119–3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (14).Wang Y, Meng L, Pittman EN, Etheredge A, Hubbard K, Trinidad DA, Kato K, Ye X, and Calafat AM (2017). Quantification of urinary mono-hydroxylated metabolites of polycyclic aromatic hydro-carbons by on-line solid phase extraction-high performance liquid chromatography-tandem mass spectrometry. Anal. Bioanal. Chem 409, 931–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).US-CDC (2013). Centers for Disease Control and Prevention. The National Health and Nutrition Examination Survey (NHANES) Analytic and Reporting Guidelines, https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx (accessed on January 11, 2018).
- (16).Barr DB, Wilder LC, Caudill SP, Gonzalez AJ, Needham LL, and Pirkle JL (2005). Urinary creatinine concentrations in the US population: implications for urinary biologic monitoring measurements. Environ. Health Perspect 113, 192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).US-CDC (2018). CDC, Centers for Disease Control and Prevention Fourth National Report on Human Exposure to Environmental Chemicals: Updated Tables. Atlanta, GA, https://www.cdc.gov/exposurereport/index.html (accessed on July 23, 2018). [Google Scholar]