Abstract
BACKGROUND AND OBJECTIVE:
To determine the ultra–wide-field fundus autofluorescence (UWFFAF) and optical coherence tomography (OCT) features of syphilitic outer retinopathy (SOR).
PATIENTS AND METHODS:
Retrospective chart review.
RESULTS:
Three patients with SOR were investigated. Treatment with parenteral penicillin led to improvement of outer retinopathy, visual acuity, and symptoms. UWFFAF showed speckled hyperautofluorescence, hypoautofluorescence, and normal autofluorescence, similar to what has been described as a trizonal pattern in acute zonal occult outer retinopathy (AZOOR) in the chronic case of SOR, but with hyperautofluorescent areas in the two acute cases. OCT showed disruption of the photoreceptor outer segment ellipsoid zone and external limiting membrane, which improved after penicillin treatment, and corresponded to normalization of the hyperautofluorescent areas on UWFFAF. There was irregularity and nodular thickening of retinal pigment epithelium on OCT in areas of mottled hyperautofluorescence.
CONCLUSION:
SOR can present similarly to AZOOR on UWFFAF and should be highly suspected in cases presenting like AZOOR.
INTRODUCTION
Acquired syphilis is a potentially chronic multisystem disease caused by the spirochete Treponema pallidum. Ophthalmic involvement in syphilis can occur at any stage in the disease, potentially affecting the anterior and the posterior segments with uveitis; however, in primary syphilis, involvement can include the eyelids or conjunctiva, and occasionally the sclera in secondary and tertiary syphilis. The most common ocular manifestation of syphilis is uveitis. Ocular syphilis is a masquerade condition because of the variety of its manifestations traditionally without pathognomonic signs.1
Syphilitic chorioretinitis can present in two main forms: as punctate inner retinitis associated with retinal hemorrhages, perivasculitis, and overlying vitritis, or, less commonly, as an outer retinitis, which can vary from a placoid appearance to a syphilitic outer retinitis (SOR) resembling acute zonal occult outer retinopathy (AZOOR).2–6 The placoid form was first described by de Souza et al.2 and was given the name acute syphilitic posterior placoid chorioretinitis (ASPPC) by Gass.3 HIV infection has been reported to be associated with this presentation.3,7,8 The angiographic, autofluorescence, and optical coherence tomography (OCT) features of SOR are quite distinctive and can provide useful information regarding the pathologic processes in this condition.9 Recently, two separate reports described three cases of SOR presenting similarly to AZOOR.4,5
The utility of ultra–wide-field fundus autofluorescence (UWFFAF) has become increasingly apparent for the evaluation and monitoring of patients with posterior uveitis. Autofluorescence imaging of the fundus can show the metabolic activity of the retinal pigment epithelium (RPE), which reflects the activity of diseases involving the outer retina. UWFFAF enables noninvasive imaging of the retinal periphery with enhanced ability to detect changes that would be missed by traditional fundus cameras as well as standard wide-field cameras.10,11 UWFFAF has been shown to be superior to color fundus photography in delineating the extent of RPE alterations in cases of uveitis.12 Spectral-domain OCT (SD-OCT) is another important imaging tool that shows changes at different levels of the retina and choroid, increasing our understanding of localization of inflammation in various uveitic entities, as well as enhancing our ability to monitor response to treatment.13 This case series describes the UWFFAF and SD-OCT features of SOR presenting like AZOOR, before and after treatment.
PATIENTS AND METHODS
This is a retrospective chart review of three cases of SOR seen at Casey Eye Institute, Oregon Health & Science University, Portland, OR. Demographic and clinical data were collected by reviewing the medical records of the study subjects. The preservation of data confidentiality was addressed properly during this study, and it was conducted with the approval of the institutional review board.
Ophthalmic Imaging
All patients underwent both UWFFAF imaging and pseudo-color (red and green only) imaging using the Optos ultra–wide-field imaging device (Optos, Dunfermline, United Kingdom). The UWFFAF images were acquired using a scanning laser ophthalmoscope technology with a green laser of 532 nm as the excitation light and with signal emitted from the retina detected from a raster scan after passing through an emission filter with a bandpass of 570 nm to 780 nm. OCT scans of the retina were obtained using the Spectralis SD-OCT (Heidelberg Engineering, Heidelberg, Germany).
RESULTS
Case 1
A 57-year-old white male patient presented with a 3-week history of blurred and distorted vision, impaired color perception, and redness of both eyes following a flu-like illness that occurred 10 weeks prior to presentation and lasted 6 weeks. He denied photopsias or photophobia. Best-corrected visual acuity (BCVA) was 20/40 in the right eye (OD) and hand motions (HM) in the left eye (OS) at initial presentation. Intraocular pressure (IOP) was 14 mm Hg in both eyes. Slit-lamp examination revealed no cells or flare in the anterior chamber (AC) nor in the anterior vitreous of either eye. A relative afferent pupillary defect in the left eye was noted. Fundus examination showed bilateral RPE mottling in the macula and RPE atrophy in the posterior pole centered around the optic disc (Figure 1A, only left eye shown; right eye was similar but subtler in appearance). UWFFAF imaging demonstrated a large peripapillary area of hypoautofluorescence and diffuse hyperautofluorescence throughout the fovea/perifovea, with UWFFAF showing the entire extent of abnormal autofluorescence, whereas a standard widefield 50° FAF would not have shown the entire extent of involvement (Figure 1B, only left eye shown). The normal foveal relative hypoautofluorescence due to increased luteal pigment in the fovea appeared to be blunted on the FAF image (Figure 1C), with surrounding hyperautofluorescence; the fovea itself had a relative hyperautofluorescence compared to normal FAF images. On the other hand, the area of frank hypoautofluorescence by the optic nerve on Figure 1C corresponded to the area of RPE atrophy on the SD-OCT (white dotted bracket; Figures 1C and 1D). In addition, SD-OCTs of the maculae in both eyes (OU) revealed diffuse loss of the photoreceptor inner segment ellipsoid zone (EZ) and external limiting membrane (ELM) reflectivity, including in the foveal center (Figure 1D and 1E), corresponding to the relative hyperautofluorescence in this area (white dotted bracket; Figures 1C and 1D). Serologic tests for hepatitis C virus, HIV were negative. A T. pallidum antibody test was positive, rapid plasma reagin (RPR) titer was 1:128, and a cerebrospinal fluid venereal disease research laboratory test (CSF VDRL) was positive with a titer of 1:2.
Figure 1.
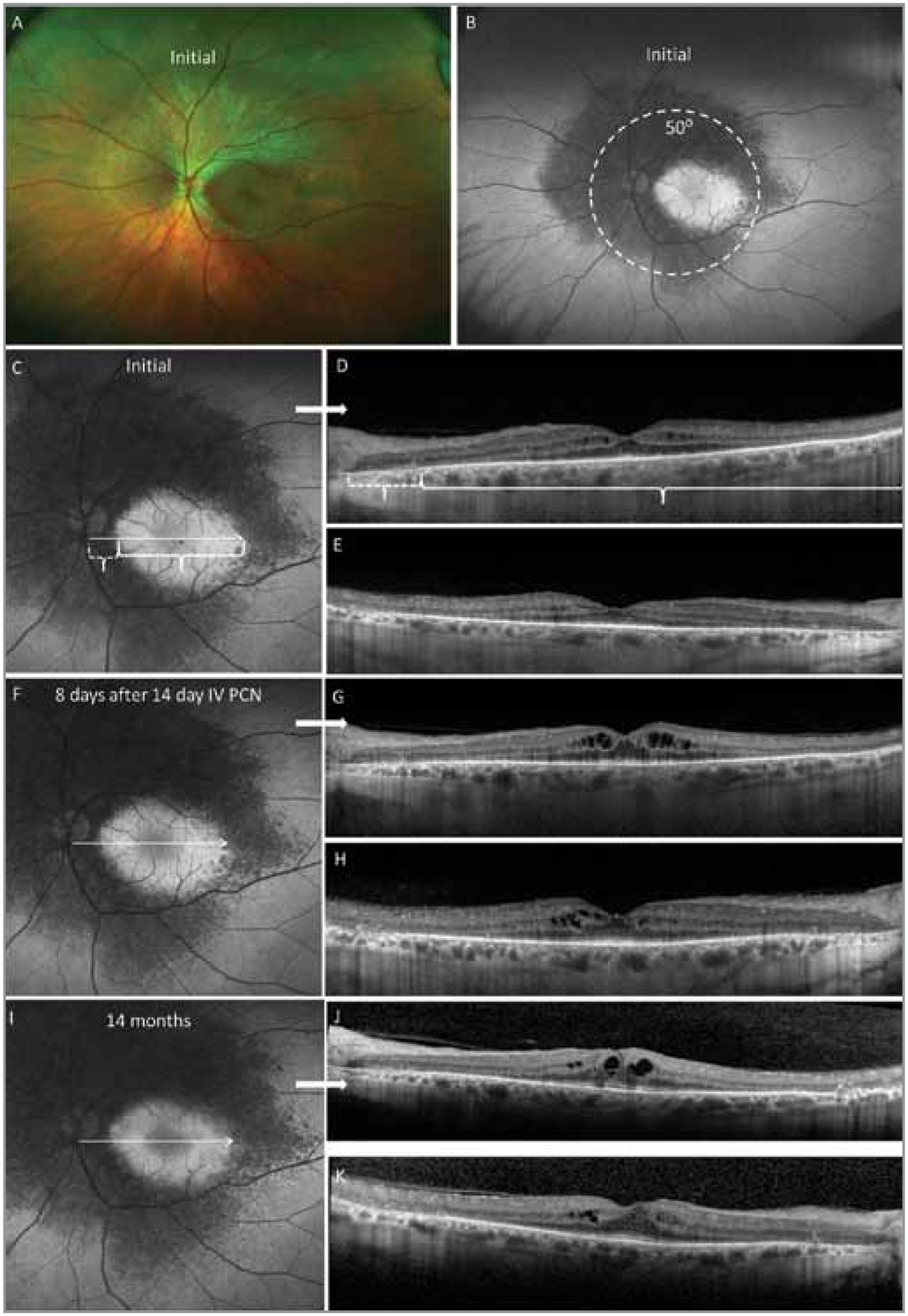
Case 1: Acute on chronic syphilitic outer retinopathy. (A) Ultra–wide-field fundus pseudocolor image demonstrating retinal pigment epithelial (RPE) mottling and atrophy. (B) Ultra–wide-field fundus autofluorescence (UWFFAF) image showing larger extent of autofluorescence abnormalities than can be seen on standard widefield 50° FAF (white dotted circle). (C, D) Initial high-magnification UWFFAF of left eye showing correlation of hyperautofluorescent areas to areas of ellipsoid zone (EZ) disruption on spectral-domain optical coherence tomography (SD-OCT), and hypoautofluorescent areas correlating with RPE and outer retinal atrophy (white dotted bracket). (E) Initial SD-OCT of right eye demonstrating diffuse macular EZ disruption. (F) High-magnification UWFFAF of left eye at follow-up after penicillin treatment showing partial recovery to normal fundus autofluorescence correlating with partial recovery of EZ reflectivity on SD-OCT of the left eye (G). There is increased cystoid macular edema (CME) in both eyes (right eye SD-OCT shown in H). (I) UWFFAF of left eye at 14 months after initial presentation showing stable recovery to normal foveal autofluorescence. (J-K) SD-OCTs demonstrating improvement of foveal EZ reflectivity with persistent cystoid macular edema in both eyes at 14 months. White arrows denote location of SD-OCTs obtained.
Based on the above findings, the patient was diagnosed with syphilitic outer retinopathy and started on a 2-week course of intravenous (IV) aqueous penicillin G, 4 million units every 4 hours. Follow-up during and after the IV penicillin course showed improvement of BCVA from HM to 20/50 OS and a partial return to normal in the foveal autofluorescence pattern (Figure 1F, only left eye shown), corresponding to a partial recovery of EZ and ELM reflectivity in the fovea on OCT (Figures 1G and 1H). BCVA OD remained 20/40 initially. Conversely, cystoid macular edema (CME) worsened OU after completion of IV penicillin, from central macular thicknesses (CMTs) of 310 μm OD and 321 μm OS at baseline to 373 μm OD and 382 μm OS after treatment (Figures 1D, 1E, 1G, and 1H). This was thought to be due to an inflammatory reaction to treponemal antigens released after antibiotic treatment such as occurs during a Jarisch-Herxheimer reaction,14 and oral prednisone was started at a dose of 50 mg per day and tapered at 10 mg per week decrements. At this point, the CSF VDRL had turned negative, and the RPR improved to 1:8. Addition of oral prednisone led to dramatic improvement of CME and improvement of visual acuity to 20/30 OD and 20/30 OS; CMT improved to 320 μm OD and 363 μm OS after initiating oral prednisone. One year after initial treatment, this patient underwent a second course of IV penicillin for 4 weeks due to persistently positive RPR, after which recurrent CME improved without oral prednisone. At last follow-up 14 months after presentation, visual acuity was 20/40 OD and 20/30 OS with 1+ posterior subcapsular cataracts in both eyes. Macular autofluorescence appeared to return to a more normal foveal and parafoveal pattern (Figure 1I), whereas EZ and ELM visibility in the fovea remained improved despite persistent CME (Figures 1J and 1K). Peripapillary hypoautofluorescence remained the same throughout follow-up, reflecting the chronicity of the latter changes. Selected case details are found in Table 1.
TABLE.
Case Summaries of Syphilitic Outer Retinopathy
| Case | 1 | 2 | 3 |
| Age | 57 | 45 | 51 |
| Gender | M | M | M |
| SUN Category Uveitis | Posterior uveitis | Panuveitis | Posterior uveitis |
| Bilateral | Yes | No | No |
| OD: 20/40 | OD: 20/20 | OD: 20/20 | |
| OS: HM | OS: CF | OS: 20/200 | |
| 1st: IV PCN G × 2 weeks | IV PCN G × 3 weeks | IV PCN G × 2 weeks | |
| 2nd: IV PCN G × 4 weeks | |||
| OD: 20/40 | OD: 20/20 | OD: 20/15 | |
| OS: 20/30 | OS: 20/30 | OS: 20/20 | |
| Duration of follow-up | 14 months | 3.5 months | 3 months |
| HIV status | Negative | Negative | Positive |
| CSF VDRL | Positive | Negative | Not done |
| Treponema IgG | Positive | Positive | Positive |
| RPR Titer | 1:128 | 1:128 | 1:512 |
SUN = standardization of uveitis nomenclature; BCVA = best-corrected visual acuity; IV = intravenous; HM = hand motions; CF = count fingers; OD = right eye; OS = left eye; PCN = penicillin; HIV = human immunodeficiency virus; CSF = cerebral spinal fluid; VDRL = venereal disease research laboratory test; IgG = immunoglobulin G; RPR = rapid plasma regain
Case 2
A 45-year-old white man noticed redness and irritation of the left eye during the previous 10 days, which improved slightly with allergy eye drops. Two days after symptoms started, the central vision in the left eye declined. He denied other health problems and was not taking any medications. He did report unprotected sex with multiple partners. Visual acuity was 20/20 OD and counting fingers at 5 inches OS upon presentation. IOP was 13 mm Hg OD and 14 mm Hg OS. Slit-lamp examination demonstrated left conjunctival injection, inferior small keratic precipitates, 0.5+ cells in the AC, and 1+ cells in the anterior vitreous. Fundus examination OS revealed mild optic disc edema and a large zonal area of flat, outer retinal whitish yellow discoloration with a well-delineated border extending throughout the macula, inferior, and inferonasal retinal periphery (Figure 2A). Examination of the right eye revealed a flat, temporal macular choroidal nevus but was otherwise normal. UWFFAF OS showed diffuse speckled hyperautofluorescence in the macula as well as slightly speckled hyperautofluorescence in a continuous sector of inferior and inferonasal retina extending out to the periphery (Figure 2B), showing a much larger extent of retinal involvement than what would have been appreciated on a standard 50° wide-field FAF image.
Figure 2.
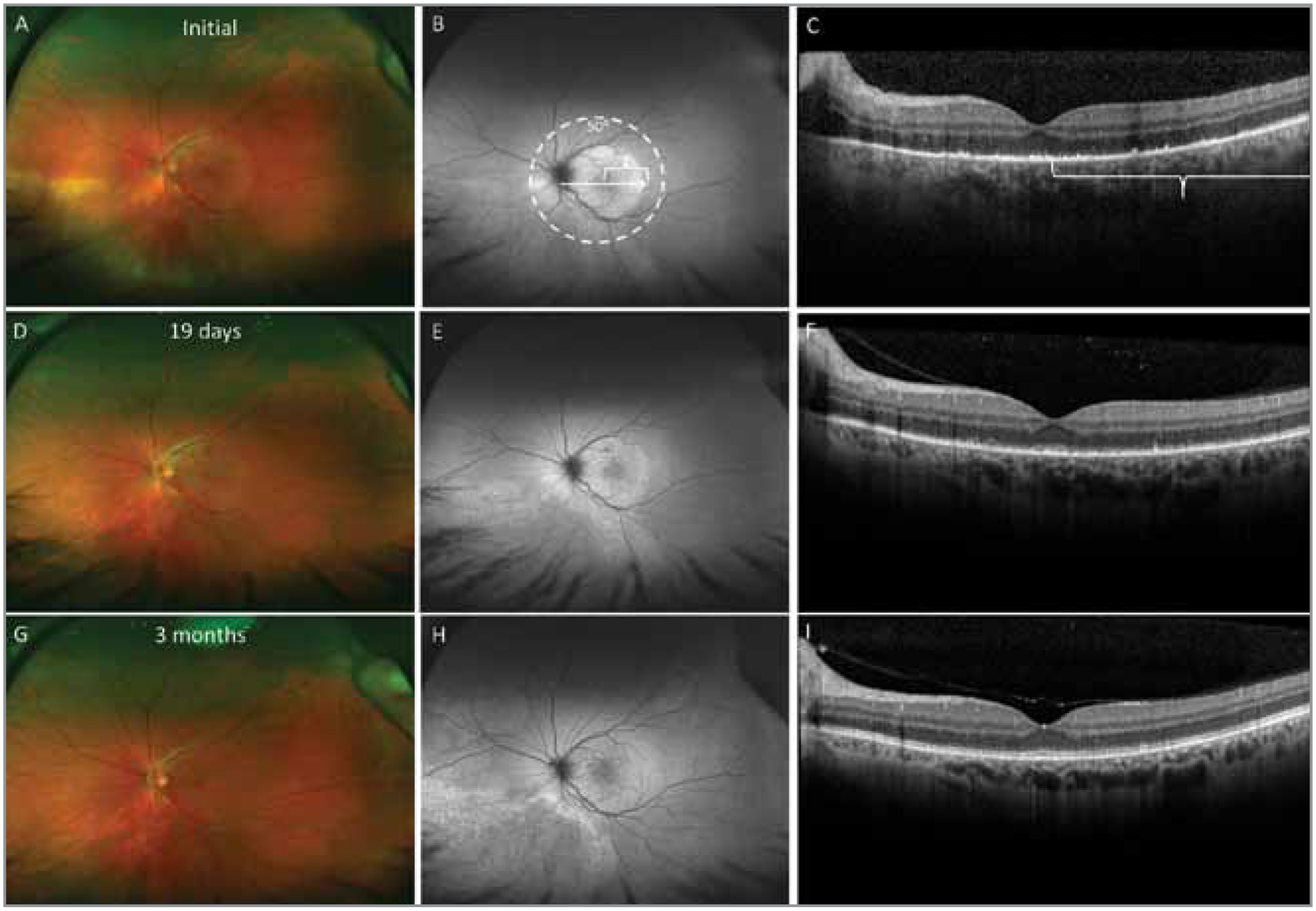
Case 2: Macular and inferonasal zonal syphilitic outer retinopathy. (A, B) Ultra–wide-field fundus and autofluorescence (UWFFAF) images demonstrating yellowish outer retinitis and hyperautofluorescent areas corresponding with ellipsoid zone (EZ) loss on spectral-domain optical coherence tomography (SD-OCT) (C) at initial presentation. (D, E) Normalization of fundus appearance and reduction in intensity of hyperautofluorescence on UWFFAF after treatment, with partial recovery of EZ on SD-OCT (F). (G, H) Continued improvement of fundus appearance and hyperautofluorescence intensity in macula with conversion to mottled hypoautofluorescence with hyperautofluorescent border in the inferonasal quadrant. (I) Return to nearly normal EZ reflectivity on SD-OCT of the left eye 3 months after presentation (after penicillin treatment). White arrow denotes location of SD-OCT obtained.
SD-OCT revealed diffuse EZ and ELM disruption in the macula involving the fovea, as well as RPE level excrescences throughout the macula (Figure 2C) corresponding to areas of hyperautofluorescence on the UWFFAF image. An area showing transition from diminished to normal EZ/ELM reflectivity in the temporal SD-OCT scan (white bracket) corresponded to the abrupt transition from hyperautofluorescence to normal autofluorescence (Figures 2B and 2C) on UWFFAF. The T. pallidum immunoglobulin G was positive, RPR titer was 1:128, HIV testing was negative, and quantiferon was negative. His CSF VDRL was also negative. The patient was placed on IV penicillin G 1 million units per hour continuously via a peripherally inserted central catheter line on an out-patient basis for 3 weeks and prednisolone eye drops four times per day OS with a tapering course. He also tested positive for chlamydia and was simultaneously treated with a one-time dose of oral azithromycin 1g. One week after initiating IV penicillin, visual acuity had improved to 20/150 OS. By 19 days after initiating therapy, visual acuity improved to 20/40 OS, with improvement of the outer retinitis (Figure 2D); less prominent hyperautofluorescence, especially in the inferonasal sector (Figure 2E) of the UWFFAF image; and improved EZ reflectivity in the fovea on SD-OCT (Figure 2F). By 3 months, visual acuity was 20/30 OS, with improved fundus appearance (Figure 2G); residual RPE changes in the fovea, superior macula, and inferonasal retins; without thickening or whitening of the retina; and with complete resolution of optic disc edema. There was normalization of autofluorescence on UWFFAF in the macula except for several hyperautofluorescent foci corresponding to residual RPE changes (Figure 2H), and restoration of ELM and EZ reflectivity throughout most of the macula (Figure 2I). The inferonasal periphery converted to mottled hypoautofluorescence with a hyperautofluorescent posterior border reminiscent of the pattern seen in AZOOR cases (Figure 2H).
Case 3
A 51-year-old white male with a history of HIV, chronic myelogenous leukemia, and deep venous thrombosis presented with photopsias and sudden vision loss in the left eye for the past 10 days. The patient was diagnosed with HIV 15 years ago, which was well-controlled on highly active antiretroviral therapy. He had a remote history of treatment for syphilis. The BCVA was 20/20 OD and 20/200 OS. IOP was 17 OD and 14 OS. Slit lamp examination of the left eye showed a quiet AC with 1+ anterior vitreous cells and pigment. Fundus examination of the left eye showed hyperemia of the optic disc, fine mottled RPE changes in the macula and superonasal peripheral retina. Examination of the right eye was normal. UWFFAF OS showed hyperautofluorescence in the macula and superonasal retina extending from the optic nerve with a much larger area of retina involved than what would have been demonstrated on a standard 50° widefield FAF image (Figure 3A). Although an ultra-widefield fundus picture was not obtained, a 50° fundus photo demonstrated the subtle examination appearance with mild RPE changes in the macula and superonasal to the optic nerve (Figure 3B). Although the fluorescent treponemal antibody was positive and RPR was 1:512, a quantiferon and chest X-ray were negative. The patient was treated with 2 weeks of IV penicillin G. By day 10 of treatment, vision improved to 20/40 OS. Figure 3C shows reduced hyperautofluorescence on UWFFAF 3 months afterwards (post-treatment). On initial presentation, a higher magnification UWFFAF image OS revealed hyperautofluorescent areas corresponding to EZ and ELM disruption on SD-OCT (Figures 3D and 3E), sparing the temporal macula. The abrupt transition from hyperautofluorescence to normal autofluorescence on the initial UWFFAF corresponded to the transition from decreased EZ/ELM reflectivity to normal EZ/ELM reflectivity on SD-OCT (white bracket; Figures 3D and 3E). By 3 months, visual acuity OS returned to 20/20. The follow-up high magnification UWFFAF revealed near normalization of fundus autofluorescence (FAF) in the macula with mild hyperautofluorescence in the parafovea (Figure 3F), corresponding to near normalization of EZ/ELM reflectivity on SD-OCT but with slight attenuation of EZ/ELM reflectivity in the parafovea (white bracket and white dotted bracket; Figures 3F and 3G). Hyperautofluorescence in the periphery had also returned to near normal autofluorescence by 3 months (Figure 3C).
Figure 3.
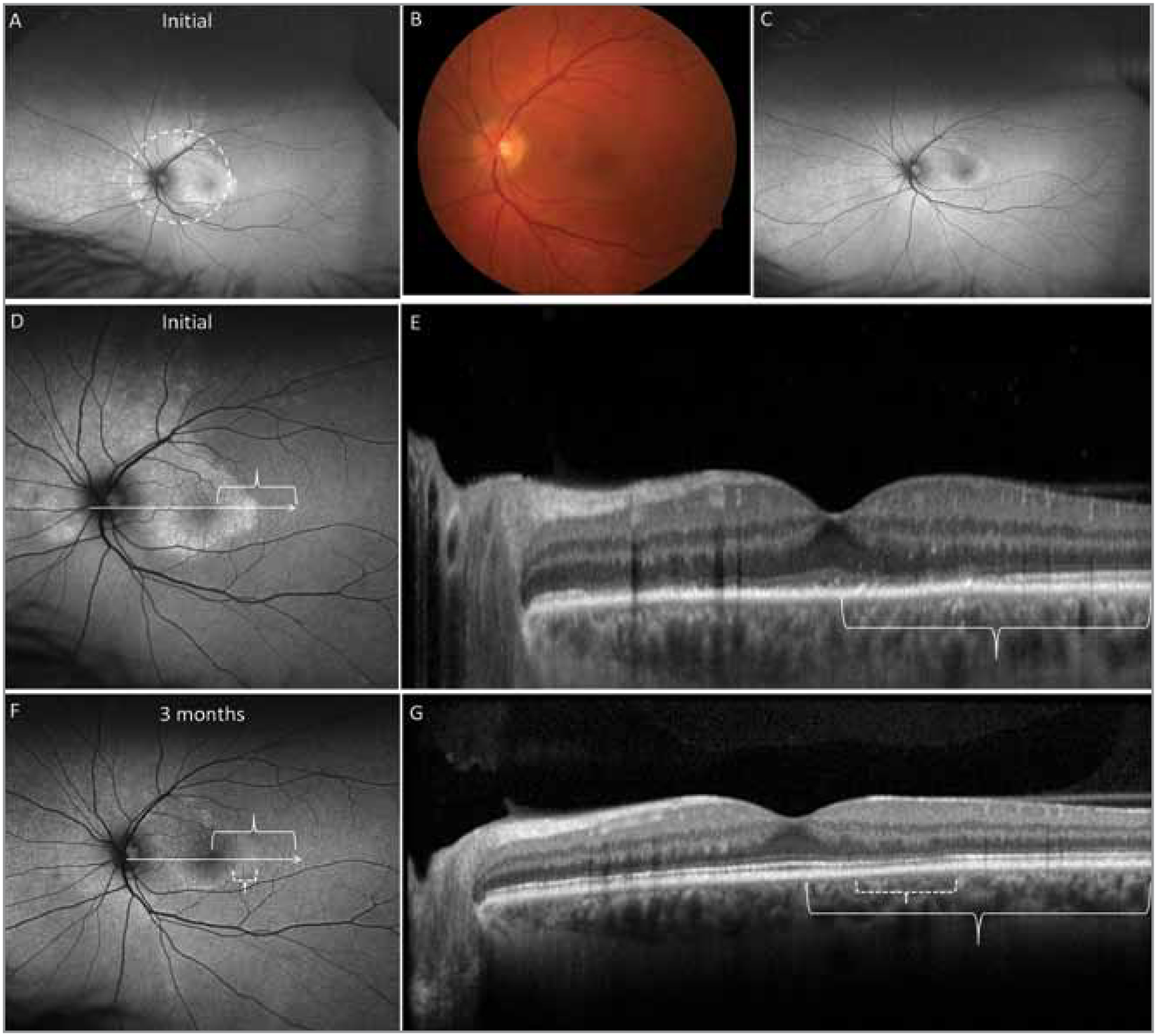
Case 3: Macular and superonasal zonal syphilitic outer retinopathy. (A) Ultra–wide-field fundus autofluorescence (UWFFAF) at initial presentation showing hyperautofluorescent zones in macula and superonasal periphery (much larger extent noted on UWFFAF than 50° fundus autofluorescence, white dotted circle). (B) Mild optic nerve edema and fine retinal pigment epithelial mottling in the fovea is seen on fundus photo of the left eye at initial presentation. (C) Reduction in intensity of hyperautofluorescence is noted in this UWFFAF image obtained 3 months after presentation (after penicillin treatment). (D, E) Correlation between hyperautofluorescent areas on high-magnification UWFFAF and ellipsoid zone (EZ) disruption on spectral-domain optical coherence tomography (SD-OCT), as well as normal autofluorescence with normal reflectivity of EZ (white bracket). (F, G) Correlation between reduction in intensity of hyperautofluorescence on high magnification UWFFAF and return of EZ reflectivity on SD-OCT (white bracket) at 3 months after presentation. Persistent area of slightly abnormal parafoveal hyperautofluorescence corresponds to mildly diminished EZ reflectivity in parafovea on SD-OCT (white dotted bracket). White arrows denote location of SD-OCTs obtained.
DISCUSSION
Although syphilis was nearly eradicated from the United States in 2000, the Centers for Disease Control and Prevention report increased incidence between the years 2005 and 2013 (www.cdc.gov). Therefore, even today, one must maintain a low threshold for diagnosing syphilis.15 Recognition of syphilitic uveitis is important because it is a curable cause of uveitis, but when left untreated, is associated with a high incidence of permanent severe vision loss, with particularly devastating consequences if treated with immunosuppression because of a lack of recognition of the infectious etiology.16,17
Overall, we found that UWFFAF showed a greater extent of retinal involvement in SOR compared to what would have been shown by standard widefield 50° FAF in all three of our cases, as well as good (nearly point-by-point) correlation between autofluorescence abnormalities and SD-OCT changes where the latter could be obtained (in the macula). The exact mechanism of hyperautofluorescence in acutely affected areas during SOR is not entirely clear. It is possible for instance, that photoreceptor inflammation results in loss of photopigment, and a subsequent relative increase in emission of autofluorescence from the underlying RPE. This loss of photopigment could change the reflectivity of the EZ on SD-OCT, which we found corresponded to areas of acute hyperautofluorescence on UWFFAF. The subjects who demonstrated return to normal autofluorescence appear to support this hypothesis rather than a primary RPE process resulting in increased RPE accumulation of lipofuscin. Alternatively, increased production of autofluorophores by inflamed photoreceptors or infiltrating leukocytes could potentially contribute to hyperautofluorescence. Finally, we cannot rule out that increased lipofuscin accumulation in abnormal RPE is not progressing toward normal autofluorescence as it transitions toward atrophy prior to exhibiting hypoautofluorescence, although normalization of autofluorescence even after longer follow-up argues against the latter.18 Hypoautofluorescent areas in our chronic refractory case (Case 1) were generally thought to be due to RPE atrophy.
All three SOR cases presented here had similar posterior ocular features at differing levels of chronicity with outer retinal disruption causing increased autofluorescence on UWFFAF and loss of EZ and ELM on SD-OCT upon acute presentation. Acute on chronic cases such as Case 1 have a similar UWFFAF appearance to AZOOR in that there is a trizonal pattern described as normal autofluorescence outside of a delineating line (zone 1) surrounding a speckled hyperautofluorescent zone (zone 2) and a hypoautofluorescent zone (zone 3).18,19 One possible distinction between AZOOR and SOR is that the zone 1 delineating line usually has greater intensity hyperautofluorescence and is much more distinctly demarcated in AZOOR compared with SOR.
Although not robustly present in our patients, the presence of other signs of intraocular inflammation (AC or vitreous cell) with an AZOOR-like fundus appearance might be more highly associated with syphilis rather than AZOOR. Similar to AZOOR, SOR can also present with sudden onset visual field defect associated with photopsias and other symptoms of photoreceptor dysfunction such as impaired color vision and blurring of central vision.20 Additionally, Case 1 was similar to AZOOR in the presence of a prodromal viral illness, which can occur in 20% of AZOOR cases.21 Fundus examination findings in SOR can also be similar to AZOOR in that there may be well-defined areas of pigment mottling in the posterior pole or a well-defined yellowish circular outer retinal process through the macula with clear demarcation from the surrounding retina and extending in a contiguous zone to the ora serrata. The addition of UWFFAF to the imaging protocol for SOR illustrates this similarity to AZOOR.
The current standard treatment for ocular syphilis is with parenteral penicillin, since it is considered neurosyphilis, although it is not known how often ocular syphilis is associated with documented neurosyphilis. One study showed CSF abnormalities in 57% of syphilitic uveitis patients.22 It also unclear whether syphilitic anterior uveitis alone can be treated as secondary syphilis with intramuscular penicillin alone, and there remains no gold standard for duration of parenteral penicillin treatment. HIV coinfection should always be investigated given its association with syphilitic progression and increased rate of relapse.23
We report three cases of SOR that presented similarly to AZOOR, with minimal intraocular inflammation. Two-thirds of cases had posterior uveitis alone (one with minimal anterior vitreous cell), and one case presented with mild AC inflammation. SD-OCT revealed EZ and ELM disruption in all three cases, with irregularity and nodular thickening of the RPE in two cases, and CME in one case, which was attributed to an immunological reaction to dead organisms after penicillin initiation. Interestingly, the outer retinal disruptions on OCT were reversible after penicillin treatment in acutely presenting cases, which reflects the importance of early recognition and prompt management with parenteral antibiotics to restore vision. Hyperautofluorescent areas on UWFFAF also improved with treatment whereas hypoautofluorescent areas remained stable, which reflects irreversible damage to the outer retina and RPE. Finally, despite poor initial visual acuities in affected eyes, prompt treatment with parenteral penicillin resulted in excellent visual acuity outcomes.
CONCLUSION
This series emphasizes the importance of maintaining a high suspicion for ocular syphilis even in cases of posterior uveitis with minimal other signs of intraocular inflammation. Patients suspected of having AZOOR should be tested for syphilis because it is a potentially treatable cause. Multimodal imaging, especially SD-OCT and UWFFAF, can show the pathological changes at the level of the outer retina and RPE in SOR, and both imaging modalities can facilitate monitoring response to treatment.
Acknowledgments
Supported by National Institutes of Health grant K08EY022948 (PL) and Career Development Awards from Research to Prevent Blindness (PL). The Casey Eye Institute has received an unrestricted grant from Research to Prevent Blindness.
Dr. Lin has received grants from the National Institutes of Health, as well as other financial support from Abbvie, CavtheRx, Prothena, and pSivida outside the submitted work. The remaining authors report no relevant financial disclosures.
REFERENCES
- 1.Moradi A, Salek S, Daniel E, et al. Clinical features and incidence rates of ocular complications in patients with ocular syphilis. Am J Ophthalmol. 2015;159(2):334–343. [DOI] [PubMed] [Google Scholar]
- 2.de Souza EC, Jalkh AE, Trempe CL, Cunha S, Schepens CL. Unusual central chorioretinitis as the first manifestation of early secondary syphilis. Am J Ophthalmol. 1988;105(3):271–276. [DOI] [PubMed] [Google Scholar]
- 3.Gass JD, Braunstein RA, Chenoweth RG. Acute syphilitic posterior placoid chorioretinitis. Ophthalmology. 1990;97(10):1288–1297. [DOI] [PubMed] [Google Scholar]
- 4.Kim JA, Park KH, Woo SJ. A case of syphilitic outer retinitis mimicking acute zonal occult outer retinopathy. Korean J Ophthalmol. 2014;28(6):497–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lima BR, Mandelcorn ED, Bakshi N, Nussenblatt RB, Sen HN. Syphilitic outer retinopathy. Ocul Immunol Inflamm. 2014;22(1):4–8. [DOI] [PubMed] [Google Scholar]
- 6.Zamani M, Garfinkel RA. Corticosteroid-induced modulation of acute syphilitic posterior placoid chorioretinitis. Am J Ophthalmol. 2003;135(6):891–894. [DOI] [PubMed] [Google Scholar]
- 7.Chao JR, Khurana RN, Fawzi AA, Reddy HS, Rao NA. Syphilis: Reemergence of an old adversary. Ophthalmology. 2006;113(11):2074–2079. [DOI] [PubMed] [Google Scholar]
- 8.Tran TH, Cassoux N, Bodaghi B, Fardeau C, Caumes E, Lehoang P. Syphilitic uveitis in patients infected with human immunodeficiency virus. Graefes Arch Clin Exp Ophthalmol. 2005;243(9):863–869. [DOI] [PubMed] [Google Scholar]
- 9.Matsumoto Y, Spaide RF. Autofluorescence imaging of acute syphilitic posterior placoid chorioretinitis. Retin Cases Brief Rep. 2007;1(3):123–127. [DOI] [PubMed] [Google Scholar]
- 10.Gupta V, Al-Dhibi HA, Arevalo JF. Retinal imaging in uveitis. Saudi J Ophthalmol. 2014;28(2):95–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Witmer MT, Kiss S. Wide-field imaging of the retina. Surv Ophthalmol. 2013;58(2):143–154. [DOI] [PubMed] [Google Scholar]
- 12.Reznicek L, Seidensticker F, Stumpf C, et al. Systematic analysis of wide-field fundus autofluorescence (FAF) imaging in posterior uveitis. Curr Eye Res. 2014;39(2):164–171. [DOI] [PubMed] [Google Scholar]
- 13.Pichi F, Ciardella AP, Cunningham ET Jr., et al. Spectral domain optical coherence tomography findings in patients with acute syphilitic posterior placoid chorioretinopathy. Retina. 2014;34(2):373–384. [DOI] [PubMed] [Google Scholar]
- 14.Fathilah J, Choo MM. The Jarisch-Herxheimer reaction in ocular syphilis. Med J Malaysia. 2003;58(3):437–439. [PubMed] [Google Scholar]
- 15.Patton ME, Su JR, Nelson R, Weinstock H, Centers for Disease Control and Prevention (CDC). Primary and secondary syphilis – United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(18):402–406. [PMC free article] [PubMed] [Google Scholar]
- 16.Curi AL, Sarraf D, Cunningham ET Jr. Multimodal imaging of syphilitic multifocal retinitis. Retin Cases Brief Rep. 2015;9(4):277–280. [DOI] [PubMed] [Google Scholar]
- 17.Hong MC, Sheu SJ, Wu TT, Chuang CT. Ocular uveitis as the initial presentation of syphilis. J Chin Med Assoc. 2007;70(7):274–280. [DOI] [PubMed] [Google Scholar]
- 18.Shifera AS, Pennesi ME, Yang P, Lin P. Ultra-wide-field fundus autofluorescence findings in patients with acute zonal occult outer retinopathy. Retina. 2016. October 17 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mrejen S, Khan S, Gallego-Pinazo R, Jampol LM, Yannuzzi LA. Acute zonal occult outer retinopathy: A classification based on multi-modal imaging. JAMA Ophthalmol. 2014;132(9):1089–1098. [DOI] [PubMed] [Google Scholar]
- 20.Monson DM, Smith JR. Acute zonal occult outer retinopathy. Surv Ophthalmol. 2011;56(1):23–35. [DOI] [PubMed] [Google Scholar]
- 21.Gass JD, Agarwal A, Scott IU. Acute zonal occult outer retinopathy: A long-term follow-up study. Am J Ophthalmol. 2002;134(3):329–339. [DOI] [PubMed] [Google Scholar]
- 22.Amaratunge BC, Camuglia JE, Hall AJ. Syphilitic uveitis: A review of clinical manifestations and treatment outcomes of syphilitic uveitis in human immunodeficiency virus-positive and negative patients. Clin Exp Ophthalmol. 2010;38(1):68–74. [DOI] [PubMed] [Google Scholar]
- 23.Becerra LI, Ksiazek SM, Savino PJ, et al. Syphilitic uveitis in human immunodeficiency virus-infected and noninfected patients. Ophthalmology. 1989;96(12):1727–1730. [DOI] [PubMed] [Google Scholar]


