Summary
Background
Elevated risk of psychotic disorders in migrant groups is a public mental health priority. We investigated whether living in areas of high own-region migrant density was associated with reduced risk of psychotic disorders among migrants and their children, and whether generation status, probable visible minority status, or region-of-origin affected this relationship.
Methods
We used the Swedish registers to identify migrants and their children born between Jan 1, 1982, and Dec 31, 1996, and living in Sweden on or after their 15th birthday. We tracked all included participants from age 15 years or date of migration until emigration, death, or study end (Dec 31, 2016). The outcome was an ICD-10 diagnosis of non-affective psychosis (F20–29). We calculated own-region and generation-specific own-region density within the 9208 small areas for market statistics neighbourhoods in Sweden, and estimated the relationship between density and diagnosis of non-affective psychotic disorders using multilevel Cox proportional hazards models, adjusting for individual confounders (generation status, age, sex, calendar year, lone dwelling, and time since migration [migrants only]), family confounders (family income, family unemployment, and social welfare), and neighbourhood confounders (deprivation index, population density, and proportion of lone dwellings), and using the Akaike information criterion (AIC) to compare model fit.
Findings
Of 468 223 individuals included in the final cohort, 4582 (1·0%) had non-affective psychotic disorder. Lower own-region migrant density was associated with increased risk of psychotic disorders among migrants (hazard ratio [HR] 1·05, 95% CI 1·02–1·07 per 5% decrease) and children of migrants (1·03, 1·01–1·06), after adjustment. These effects were stronger for probable visible minority migrants (1·07, 1·04–1·11), including migrants from Asia (1·42, 1·15–1·76) and sub-Saharan Africa (1·28, 1·15–1·44), but not migrants from probable non-visible minority backgrounds (0·99, 0·94–1·04). Among migrants, adding generation status to the measure of own-region density provided a better fit to the data than overall own-region migrant density (AIC 36 103 vs 36 106, respectively), with a 5% decrease in generation-specific migrant density corresponding to a HR of 1·07 (1·04–1·11).
Interpretation
Migrant density was associated with non-affective psychosis risk in migrants and their children. Stronger protective effects of migrant density were found for probable visible minority migrants and migrants from Asia and sub-Saharan Africa. For migrants, this risk intersected with generation status. Together, these results suggest that this health inequality is socially constructed.
Funding
Wellcome Trust, Royal Society, Mental Health Research UK, University College London, National Institute for Health Research, Swedish Research Council, and FORTE.
Introduction
Elevated psychosis risk in migrants and their children has been well established in European2, 3, 4, 5, 6 and North American studies,7, 8, 9 yet adequate explanations for this phenomenon have not been elucidated.10 The persistence of increased risk for children of migrants implicates factors in the post-migratory environment, including so-called ethnic density, in the development of psychotic disorders.4 The ethnic density hypothesis posits that minority ethnic individuals living in areas with higher proportions of people from their own ethnic group have better health outcomes than those living in areas with lower ethnic density.11 Some have theorised that this might be due to the protective effect of increased social support or fewer experiences of discrimination, although other explanations are possible.12, 13
Studies have observed an association between low ethnic density and elevated psychosis risk,14, 15, 16, 17, 18, 19, 20 yet the relationship between the two appears more nuanced than a simple association.15 For example, a study in the Netherlands found the difference between incidence rates in populations of low and high ethnic density was most pronounced for Moroccan migrants.15 A study in London (UK) found the highest schizophrenia risk among black and minority ethnic individuals who lived in areas with low ethnic density.17 These contextually specific effects might reflect the different migration patterns, attitudes to migrant reception, and meaning attached to ethnic identities in different contexts.21 Fewer studies have looked at migrant density. One study found a surprising association between migrant density and later risk of non-affective psychotic disorders among children of migrants but not among migrants.1 These findings indicate that the effect of migrant density on psychosis risk might vary by region of origin, ethnicity, probable visible minority status, or generation status; it is not yet clear what is underlying the observed patterns.
Research in context.
Evidence before this study
Ethnic density—ie, the proportion of people from one's own ethnic group living in the immediate neighbourhood—has been proposed as a protective factor for psychotic disorders, but longitudinal evidence on this issue is sparse. We searched PubMed for studies published up to July 1, 2019, that measured the impact of ethnic density on psychotic disorders, using the terms “psychotic disorder*”, “schizophrenia”, “migrant density”, “ethnic density.” We identified 11 studies mostly published from cross-sectional studies in the UK or the Netherlands. While several studies suggested an overall association between greater ethnic density and reduced risk of psychotic disorders, this has not been shown for all ethnic groups. Only one set of studies from Denmark have considered whether ethnic density is longitudinally associated with non-affective psychotic disorders, finding an association for children of migrants but not migrants. Large, longitudinal, nationwide studies are required to determine whether these effects differ by generation status (ie, migrants versus their children), region of origin, visible minority status, or type of migrant density (ie, overall own-region migrant density or generation-specific own-region density).
Added value of this study
To our knowledge, this is the largest study to date investigating this issue, incorporating multilevel survival analysis to precisely model small area effects on psychosis risk. We show consistently increased risks of later psychotic disorders for migrants and children of migrants in neighbourhoods with lower own-region migrant density at age 15 years. This effect was particularly pronounced among probable visible minority migrant groups, including migrants from Asia and sub-Saharan Africa. We found no evidence for a migrant density effect for migrants or their children from other regions. Generation-specific migrant density was more strongly associated with psychosis risk in migrants, overall.
Implications of all the available evidence
Our longitudinal study strengthens earlier cross-sectional research by showing that own-group migrant density has stronger protective effects on non-affective psychosis risk for probable visible minority migrants. These effects were present for both migrants and their children, but were more pronounced by generation-specific density among migrants. Previous research has highlighted that ethnic density might be less important for some groups—eg, the black Caribbean population in the UK—than ethnic integration with respect to psychosis risk. This new evidence suggests that ethnic and migrant density might have intersectional effects with other factors involved in shaping psychosis risk. This research can be used to elucidate the pathways by which inequalities in mental health might be socially constructed, and creates an opportunity for public mental health intervention.
While it is likely that a broad range of factors underlie the migrant density effect, a plausible pathway by which migrant density affects psychotic disorder rates in migrants and their children could be through visible minority status. Those living in areas of low own-region migrant density might perceive themselves as different from others in their social environment, contributing to a sense of social exclusion, higher levels of social stress, and more frequent experiences of discrimination.21, 22 On the basis of these theories, we hypothesised that the migrant density effect would be more pronounced in probable visible minority than non-visible minority migrants.
While both migrants and their children might share visible minority status and could be subject to discriminatory experiences in the host country, it is probable that children of migrants have higher linguistic and cultural fluency in the host country. By contrast, first-generation migrants might rely on networks of individuals from the same region of origin who share language or cultural practices for social support, information, and connection to resources. Furthermore, neighbourhoods with high migrant density might be more likely to have culturally sensitive health and social services and access to religious facilities, ethnic foods, and cultural programmes. Thus, we hypothesised that the risk of psychotic disorders would be elevated for both migrants and their children living in areas of low migrant density, but that this effect would be more pronounced for migrants.
Here, we used prospectively collected registry data on a nationwide cohort in Sweden to examine how neighbourhood migrant density might influence subsequent risk of psychotic disorders, with consideration for the impact of generation status, probable visible minority status, and region of origin on the strength of this relationship.
Methods
Study design and population
This cohort study used data from Psychiatry Sweden, a comprehensive register linkage developed for mental health research23 that provides nationwide data on the entire population living in Sweden since 1920. It links together several registers, including those of most relevance here: the Register of the Total Population, the immigration and emigration register (known as STATIV), the Multi-Generation register, and the National Patient Register. The registers include all people living in Sweden, including immigrants from the time they are granted permanent residency rights. We identified all migrants (ie, individuals born outside of Sweden) and children of migrants (ie, individuals born in Sweden with at least one migrant parent) born between Jan 1, 1982, and Dec 31, 1996, and living in Sweden on or after their 15th birthday. Individuals were tracked from their 15th birthday or immigration to Sweden after age 15 years (earliest possible date: Jan 1, 1997) until emigration, death, or the end of the study period (Dec 31, 2016). We excluded temporary visitors and those without a residency permit, including asylum seekers and undocumented migrants; participants missing parental information, family income, and employment status; participants missing neighbourhood information at cohort entry or in the following year (to allow for register data to be updated by Statistics Sweden); and participants with an ICD-10 diagnosis of non-affective psychosis (F20–29) before their 15th birthday.
Outcomes
Our outcome was an ICD-10 diagnosis of non-affective psychosis (F20–29) recorded in the National Patient Register. Date of cohort exit was defined as the date of first diagnosis from age 15 years or older, as this corresponds with the age of onset for psychotic disorders after which psychotic disorders can be reliably captured by diagnostic criteria in the Swedish health-care system.24
Exposures
We estimated own-region migrant density for migrants and their children by using the 9208 small areas for market statistics (SAMS) neighbourhoods maintained by Statistics Sweden; the median population size of a SAMS neighbourhood in 2011 was 726 people (IQR 312–1378). We determined the total population in each neighbourhood by migrant status and region of origin, and estimated SAMS area-level characteristics including our migrant density exposures. We considered the SAMS neighbourhoods in which migrants lived at age 15 years or after immigration to Sweden, if later. Full details on how we derived our migrant density variables are given in the appendix (p 2).
We considered eight regions of origin: Nordic, Europe (excluding Nordic countries), Asia, Oceania, Middle East and north Africa, sub-Saharan Africa, North America (including Mexico), and South America. We included two additional categories—mixed migrant or Swedish migrant—for children of migrants where patients were from different regions: children of migrants were classified as Swedish migrant if they had one Swedish parent and one migrant parent, or were classified as mixed migrant if they had two migrant parents from different regions.
We estimated two migrant density exposures: overall own-region migrant density and generation-specific own-region migrant density. Overall own-region migrant density was estimated as the percentage of the neighbourhood total population from the same region of origin as the migrants in question, including both migrants and children of migrants. For example, for a migrant (or child of migrant) from Asia, this would be the proportion of the neighbourhood population who were either migrants or children of migrants from Asia. Generation-specific migrant density was restricted to the proportion of people from each participant's own region and generation status (ie, migrant or children of migrant). For example, for a migrant from Asia, this would be the proportion of the neighbourhood population who were also migrants from Asia; for children of migrants from Asia, this would be the proportion of the neighbourhood population who were also children of migrants from Asia. For both exposures, we calculated quintiles of migrant density and a continuous measure (5% change).
Probable visible minority density combined those from Asia, the Middle East and north Africa, sub-Saharan Africa, and South America, and probable non-visible minorities were individuals from Nordic countries, Europe, Oceania, and North America. Our classification of participants according to this definition of probable visible minority status was based on our understanding of the majority ethnicities in each participant's region of origin. We expressed this as 5% change in the proportion of the neighbourhood population who were probable visible minorities.
Covariates
We included several individual and family covariates: sex, age, calendar year, generation status, lone dwelling, time since migration (migrants only), family disposable income quintile, receipt of social welfare, and family unemployment (of all family members in the same household). Age was modelled as a time-varying covariate because risk of psychotic disorders varies substantially by age,25 and all other covariates were included as fixed covariates. Any household with only one individual registered at cohort entry was considered a lone dwelling household. Disposable family income quintiles were calculated on the basis of the total population in each year, and families were categorised from quintile 1 (lowest) to quintile 5 (highest). Each individual was assigned their familial income quintile in the year of their cohort entry. Familial receipt of social welfare and unemployment status were defined as binary variables (receiving social welfare benefits vs not receiving and any family member unemployed vs employed, respectively).
For each neighbourhood, for each year, we calculated population density (people per km2), proportion of lone dwelling households, and a deprivation index score. The deprivation score was generated by calculating the proportion of each neighbourhood which was low income, unemployed, receiving social welfare, or convicted of a criminal offence. These proportions were standardised and summed to create quintiles of deprivation from quintile 1 (least deprived) to quintile 5 (most deprived). Participants were assigned values of these neighbourhood covariates in their year of cohort entry, as for the migrant density variables above.
Statistical analysis
We inspected the level of missingness in the data, which was low (6·0%) overall and therefore conducted a complete-case analysis, as it was expected to produce unbiased results.29 We used multilevel Cox proportional hazards regression, accounting for the hierarchical structure of the data (participants were nested within neighbourhoods). We used Mestreg in Stata to fit a random-effects Weibull model with normally distributed random effects, which allowed the baseline hazard to vary across neighbourhoods.
The null model, without fixed effects, was fitted to quantify the variation in the baseline hazard for psychosis attributable to the neighbourhood level, assessed via Wald χ2 tests. Next, we fitted an unadjusted model including each migrant density exposure separately as a predictor of psychosis incidence. We then adjusted for individual confounders (generation status, age, sex, calendar year, lone dwelling, and time since migration [migrants only]), family confounders (family income, family unemployment, and social welfare), and neighbourhood confounders (deprivation index, population density, and proportion of lone dwellings) in separate models, before fitting a fully adjusted model. To investigate whether overall own-region migrant density or generation-specific migrant density fitted the data better for migrants and children of migrants, we estimated stratified fully adjusted models for migrants and children of migrants separately. The Akaike information criterion (AIC) was calculated to compare model fit, where better fit was indicated by lower scores. We then investigated whether own-region migrant density had a different effect on psychosis risk by probable visible minority status. Finally, we accounted for region of origin to ensure our density measures were not merely a proxy for region. We adjusted our models for region and calculated region-specific migrant density effects in a supplemental analysis.
We present descriptive statistics of the cohort, including percentages and median (IQR), and the Pearson correlation coefficient to compare correlation between migrant density measures. We also report unadjusted and adjusted hazard ratios (HRs) with 95% CIs. We used Stata (version 15.1) for all analyses.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
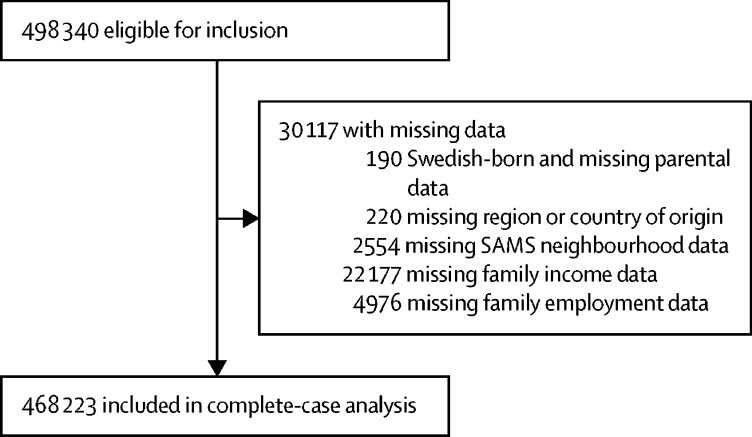
498 340 participants were eligible for inclusion, of whom 30 117 had missing data. Most missing data regarded family income, with 4·5% of participants missing family income information (figure; appendix p 3).
Figure.
Study profile
468 223 individuals were included in the final cohort for our complete-case analysis (figure): 268 686 (57·4%) were migrants and 199 537 (42·6%) were children of migrants. The cohort included 4582 cases (1·0%) of non-affective psychotic disorder with 5·0 million person-years of follow-up. The largest group of migrants were from Europe, excluding Nordic countries, whereas the largest proportion of children of migrants were of Nordic origin (table 1).
Table 1.
Individual-level and neighbourhood-level sociodemographic characteristics
|
Migrants (n=268 686) |
Children of migrants (n=199 537) |
|||||
|---|---|---|---|---|---|---|
| Percentage of migrants | Cases* | Person-years in dataset | Percentage of children of migrants | Cases* | Person-years in dataset | |
| Non-affective psychosis | ||||||
| Yes | 0·9% | 2468 | 17 902 | 1·1% | 2114 | 17 374 |
| No | 99·1% | 266 218 | 2 585 051 | 98·9% | 197 423 | 2 398 031 |
| Sex | ||||||
| Female | 49·2% | 845 (34·2%) | 1 281 490 | 48·6% | 752 (35·6%) | 1 170 667 |
| Male | 50·8% | 1623 (65·8%) | 1 321 463 | 51·4% | 1362 (64·4%) | 1 244 738 |
| Date of birth | ||||||
| 1982–86 | 52·6% | 1358 (55%) | 1 450 168 | 25·8% | 776 (36·7%) | 881 907 |
| 1987–92 | 31·2% | 790 (32%) | 823 312 | 34·0% | 801 (37·9%) | 861 980 |
| 1993–96 | 16·3% | 320 (13%) | 329 473 | 40·2% | 537 (25·4%) | 671 518 |
| Region† | ||||||
| Nordic‡ | 7·7% | 103 (4·2%) | 131 882 | 28·7% | 644 (30·5%) | 766 149 |
| Europe | 31·8% | 693 (28·1%) | 880 211 | 13·5% | 270 (12·8%) | 310 934 |
| Asia | 16·4% | 297 (12%) | 365 971 | 4·1% | 61 (2·9%) | 92 699 |
| Oceania | 0·4% | 3 (0·1%) | 7648 | 0·0% | 0 | 62 |
| Middle East and north Africa | 27·3% | 693 (28·1%) | 796 928 | 20·9% | 349 (16·5%) | 471 962 |
| Sub-Saharan Africa | 10·5% | 550 (22·3%) | 261 899 | 3·8% | 127 (6%) | 72 516 |
| North America | 2·5% | 50 (2%) | 55 558 | 0·3% | 6 (0·3%) | 6338 |
| South America | 3·4% | 79 (3·2%) | 102 857 | 3·5% | 66 (3·1%) | 84 025 |
| Swedish migrant | .. | .. | .. | 18·9% | 390 (18·4%) | 456 995 |
| Mixed migrant | .. | .. | .. | 6·4% | 201 (9·5%) | 153 726 |
| Family income | ||||||
| Quintile 1 (lowest) | 49·1% | 848 (34·4%) | 958 143 | 4·1% | 99 (4·7%) | 80 303 |
| Quintile 2 | 15·1% | 422 (17·1%) | 432 327 | 13·6% | 388 (18·4%) | 315 374 |
| Quintile 3 | 19·2% | 650 (26·3%) | 640 135 | 25·6% | 671 (31·7%) | 685 210 |
| Quintile 4 | 11·3% | 386 (15·6%) | 398 985 | 29·8% | 582 (27·5%) | 727 617 |
| Quintile 5 (highest) | 5·3% | 162 (6·6%) | 173 363 | 24·0% | 374 (17·7%) | 606 902 |
| Family receiving social welfare | ||||||
| Yes | 34·4% | 1299 (52·6%) | 1 090 802 | 16·9% | 573 (27·1%) | 405 858 |
| No | 65·6% | 1169 (47·4%) | 1 512 152 | 83·1% | 1541 (72·9%) | 2 009 547 |
| Family unemployment | ||||||
| Yes | 10·4% | 365 (14·8%) | 393 276 | 24·8% | 608 (28·8%) | 624 504 |
| No | 89·6% | 2103 (85·2%) | 2 209 677 | 75·2% | 1506 (71·2%) | 1 790 901 |
| Own-region migrant density | ||||||
| Quintile 1 (lowest) | 19·2% | 604 (24·5%) | 510 823 | 15·5% | 391 (18·5%) | 374 540 |
| Quintile 2 | 18·8% | 474 (19·2%) | 494 666 | 22·4% | 462 (21·9%) | 544 363 |
| Quintile 3 | 19·4% | 409 (16·6%) | 472 935 | 22·2% | 447 (21·1%) | 531 915 |
| Quintile 4 | 20·7% | 464 (18·8%) | 522 679 | 20·8% | 420 (19·9%) | 515 082 |
| Quintile 5 (highest) | 21·9% | 517 (20·9%) | 601 851 | 19·1% | 394 (18·6%) | 449 505 |
| Generation-specific migrant density§ | ||||||
| Quintile 1 (lowest) | 16·2% | 524 (21·2%) | 431 697 | 20·0% | 477 (22·6%) | 469 565 |
| Quintile 2 | 20·3% | 498 (20·2%) | 507 747 | 20·0% | 399 (18·9%) | 480 988 |
| Quintile 3 | 20·9% | 478 (19·4%) | 533 552 | 20·0% | 404 (19·1%) | 491 161 |
| Quintile 4 | 21·3% | 460 (18·6%) | 550 091 | 20·0% | 415 (19·6%) | 491 463 |
| Quintile 5 (highest) | 21·3% | 508 (20·6%) | 579 867 | 20·0% | 419 (19·8%) | 482 228 |
Percentages are given on number of cases.
Region of birth for migrants and region of parental birth for children of migrants.
Includes children of migrants with one Nordic-born parent and one Swedish-born parent.
Migrants from same region or children of migrants from same parental region.
Levels of neighbourhood migrant density varied by neighbourhood, participant region of origin, and generation status. Overall, median own-region migrant density was 6·4% (IQR 3·0–13·0; range 0·0–80·0; appendix p 4). The range of possible values of own-region density varied by region of origin. For migrants and children of migrants from Oceania, the maximum neighbourhood own-region density was 1·8%, whereas those from the Middle East and north Africa could live in a neighbourhood with up to 80·0% of the neighbourhood from the same region of origin.
Separated by generation status, median neighbourhood own-region migrant density was 4·9% (IQR 2·2–10·6; range 0·0–58·7) for migrants and 3·4% (1·5–5·6; 0·0–35·5) for children of migrants (appendix p 4).
A null multilevel Cox regression model showed that some of the variance in psychosis rates was explained by neighbourhood-level clustering (Wald χ2 p=0·0001; appendix p 4), justifying use of a multilevel approach for this analysis. The unadjusted estimates showed that each 5% decrease in own-region migrant density was accompanied by a 3% increase in risk of developing psychotic disorders (HR 1·03, 95% CI 1·02–1·05; table 2). After adjustment for individual, family, and neighbourhood confounders, the effect remained, such that a 5% decrease in own-region migrant density corresponded to a 5% increase in psychosis risk (1·05, 1·03–1·06; table 2). When investigated by quintiles of migrant density, both unadjusted and adjusted estimates showed an increase in risk of psychotic disorders as own-region migrant density decreased (table 2).
Table 2.
Hazard ratios of non-affective psychosis by quintiles of own-region migrant density
| Hazard ratio (95% CI) | AIC | ||
|---|---|---|---|
| Unadjusted | .. | 72 817 | |
| Quintile 1 (lowest) | 1·35 (1·23–1·48)* | .. | |
| Quintile 2 | 1·07 (0·97–1·18) | .. | |
| Quintile 3 | 1·01 (0·92–1·12) | .. | |
| Quintile 4 | 1·00 (0·91–1·11) | .. | |
| Quintile 5 (highest) | 1 (ref) | .. | |
| Individual-adjusted and family-adjusted | .. | 72 767 | |
| Quintile 1 (lowest) | 1·35 (1·23–1·48)* | .. | |
| Quintile 2 | 1·13 (1·03–1·24)* | .. | |
| Quintile 3 | 1·10 (0·99–1·21) | .. | |
| Quintile 4 | 1·05 (0·96–1·16) | .. | |
| Quintile 5 (highest) | 1 (ref) | .. | |
| Neighbourhood-adjusted only | .. | 72 715 | |
| Quintile 1 (lowest) | 1·60 (1·44–1·77)* | .. | |
| Quintile 2 | 1·26 (1·13–1·40)* | .. | |
| Quintile 3 | 1·17 (1·05–1·30)* | .. | |
| Quintile 4 | 1·12 (1·01–1·24)* | .. | |
| Quintile 5 (highest) | 1 (ref) | .. | |
| Fully adjusted | .. | 69 952 | |
| Quintile 1 (lowest) | 1·36 (1·22–1·52)* | .. | |
| Quintile 2 | 1·14 (1·03–1·27)* | .. | |
| Quintile 3 | 1·11 (1·00–1·23) | .. | |
| Quintile 4 | 1·07 (0·96–1·18) | .. | |
| Quintile 5 (highest) | 1 (ref) | .. | |
| Per 5% decrease in density | |||
| Unadjusted | 1·03 (1·02–1·05)* | 72 799 | |
| Individual-adjusted only | 1·02 (1·01–1·04)* | 69 964 | |
| Neighbourhood-adjusted only | 1·07 (1·05–1·09)* | 72 741 | |
| Fully adjusted† | 1·05 (1·03–1·06)* | 69 957 | |
Models were adjusted for individual and family confounders (generation status, age, sex, calendar year, lone dwelling, family income, social welfare, family unemployment, and time since migration [migrants only]) or neighbourhood confounders (deprivation index, population density, and proportion of lone dwellings). Fully adjusted estimates include individual, family, and neighbourhood confounders. AIC=Akaike information criterion.
p<0·05.
The correlation between own-region migrant density and generation-specific migrant density was high (correlation 0·90), and there was a similar pattern of risk for migrants regardless of the measure used (table 3). A 5% decrease in own-region density corresponded to a 5% elevation in risk of non-affective psychosis in migrants (HR 1·05, 95% CI 1·02–1·07) whereas a 5% decrease in generation-specific density corresponded to a 7% elevation (1·07, 1·04–1·11; table 3). Among children of migrants, a 5% decrease in own-region density corresponded to a 3% increase in risk (1·03, 1·01–1·06). When comparing the model fit for these two measures of migrant density, we found that the generation-specific measure described the data better for migrants, with a lower AIC, but that the own-region measure performed better for children of migrants (table 3).
Table 3.
Fully adjusted hazard ratios of non-affective psychotic disorders and migrant density, by generation status
|
Migrants |
Children of migrants |
||||
|---|---|---|---|---|---|
| Adjusted hazard ratio (95% CI) | AIC | Adjusted hazard ratio (95% CI) | AIC | ||
| Own-region migrant density | .. | 36 110 | .. | 33 307 | |
| Quintile 1 (lowest) | 1·37 (1·17–1·59)* | .. | 1·28 (1·10–1·49)* | .. | |
| Quintile 2 | 1·17 (1·00–1·36) | .. | 1·10 (0·95–1·28) | .. | |
| Quintile 3 | 1·12 (0·97–1·30) | .. | 1·08 (0·93–1·25) | .. | |
| Quintile 4 | 1·13 (0·99–1·30) | .. | 1·01 (0·87–1·17) | .. | |
| Quintile 5 (highest) | 1 (ref) | .. | 1 (ref) | .. | |
| Per 5% decrease | 1·05 (1·02–1·07)* | 36 106 | 1·03 (1·01–1·06)* | 33 307 | |
| Generation-specific own-region migrant density | .. | 36 102 | .. | 33 311 | |
| Quintile 1 (lowest) | 1·42 (1·21–1·67)* | .. | 1·16 (1·01–1·34)* | .. | |
| Quintile 2 | 1·17 (1·01–1·37)* | .. | 0·96 (0·84–1·11) | .. | |
| Quintile 3 | 1·12 (0·96–1·29) | .. | 1·00 (0·87–1·15) | .. | |
| Quintile 4 | 1·04 (0·90–1·20) | .. | 1·02 (0·89–1·18) | .. | |
| Quintile 5 (highest) | 1 (ref) | .. | 1 (ref) | .. | |
| Per 5% decrease | 1·07 (1·04–1·11)* | 36 103 | 1·03 (0·97–1·09) | 33 313 | |
| Own-region migrant density by visible minority status (per 5% decrease) | |||||
| Probable visible minorities | 1·07 (1·04–1·11)* | .. | 1·04 (1·00–1·08) | .. | |
| Probable non-visible minorities | 0·99 (0·94–1·04) | .. | 0·99 (0·96–1·03) | .. | |
Hazard ratios are adjusted for individual and family confounders (age, sex, lone dwelling, family income, social welfare, family unemployment, and time since migration [migrants only]) and neighbourhood confounders (deprivation index, population density, and proportion of lone dwellings). AIC=Akaike information criterion.
p<0·05.
Among probable visible minority individuals, the risk of psychosis increased by 7% per 5% decrease in own-region migrant density (HR 1·07, 95% CI 1·04–1·09) for migrants and children of migrants combined. There was no evidence of an increase in risk of psychosis diagnosis among non-visible minority migrants (1·00, 0·97–1·02). The increased risk for probable visible minority individuals was slightly stronger among migrants than children of migrants (table 3).
When region was added to the fully adjusted analysis, the point estimates for migrant density effect followed a similar pattern, but precision was lower and 95% CIs overlapped unity (appendix p 5). In the region-adjusted model, there was evidence of a null effect among children of migrants (HR 1·00, 95% CI 0·97–1·03).
We observed differences in the migrant density effect by region of origin. We found increased risk of non-affective psychosis for migrants from Asia and sub-Saharan Africa in areas of lower migrant density (table 4), but no evidence of a migrant density effect for other migrant groups or for children of migrants from any specific region; however, we cannot exclude uncertainty due to low power in some subgroups.
Table 4.
Region-specific migrant density effects, by generation status
|
Migrants |
Children of migrants |
|||||
|---|---|---|---|---|---|---|
| Cases | Person-years | Adjusted hazard ratio (95% CI) | Cases | Person-years | Adjusted hazard ratio (95% CI) | |
| Nordic* | 103 | 131 882 | 1·01 (0·90–1·13) | 644 | 766 149 | 0·97 (0·93–1·00) |
| Europe | 693 | 880 211 | 0·98 (0·92–1·04) | 270 | 310 934 | 1·06 (0·96–1·17) |
| Asia | 297 | 365 971 | 1·42 (1·15–1·76)† | 61 | 92 699 | 1·15 (0·73–1·79) |
| Middle East and north Africa | 693 | 796 928 | 1·03 (0·98–1·08) | 349 | 471 962 | 1·00 (0·94–1·06) |
| Sub-Saharan Africa | 550 | 261 899 | 1·28 (1·15–1·44)† | 127 | 72 516 | 0·94 (0·80–1·11) |
| North America | 50 | 55 558 | 1·77 (0·21–14·77) | 6 | 6338 | 0·89 (0·00–162·16) |
| South America | 79 | 102 857 | 0·67 (0·43–1·05) | 66 | 84 025 | 1·15 (0·69–1·93) |
| Swedish migrant | .. | .. | .. | 390 | 456 995 | 0·83 (0·59–1·18) |
| Mixed migrant | .. | .. | .. | 201 | 153 726 | 1·17 (0·33–4·10) |
Numbers were too low in the Oceania group for the model to converge, so excluded from this analysis. Hazard ratios were adjusted for individual and family confounders (age, sex, lone dwelling, family income, social welfare, family unemployment, and time since migration [migrants only]) and neighbourhood confounders (deprivation index, population density, and proportion of lone dwellings) and are calculated per 5% decrease in density.
Includes children of migrants with one Nordic-born parent and one Swedish-born parent.
p<0·05.
Discussion
In this national, longitudinal cohort study, we showed that risk of non-affective psychotic disorder among migrants in Sweden increased as neighbourhood own-region migrant density decreased. We found this effect for both migrants and children of migrants. The impact of own-region migrant density was more pronounced for probable visible minority individuals than probable non-visible minority migrants. Additionally, we showed that consideration of generational migrant density status (ie, migrants or children of migrants) was important for migrants, but overall own-region migrant density described the data better for children of migrants.
Our findings should be considered in the context of several limitations. First, we had no information on ethnicity, which is not routinely collected in Swedish registers. We used region of origin to estimate migrant density, which might not align with an individual's self-reported ethnicity.26, 27, 28 Furthermore, our definition of probable visible minority status was based on our knowledge of the majority ethnicity in each region of origin, which might have led to measurement error without direct information on participants' ethnicity. In all likelihood, a small proportion of individuals were misclassified according to probable visible minority status. It is possible that factors other than visible minority status align with our classification of migrants by this measure, including level of economic development in their region of origin, cultural factors, or other reasons hitherto unknown.
Second, there were some missing data on exposures and covariates. We did a complete-case analysis, as it was expected to produce unbiased results with these modest levels of missing data.29
Third, differential use of the health-care system by migrant density might have biased the results of this study. Previous research has shown that migrants use psychiatric care at lower rates than Swedish-born individuals.30 It is plausible that in neighbourhoods with high migrant density, psychiatric services are underused and thus diagnoses are less common. Underuse in areas of high migrant density could be due to lower health literacy, lack of culturally sensitive services, reduced familiarity with the health-care system, or higher levels of mental health stigma and corresponding hesitation to access care.31, 32 Neighbourhood stratification of public infrastructure could result in areas with fewer health-care options, reduced access to specialised psychiatric services, and lower quality of care in more deprived neighbourhoods,33 which might differentially affect migrants or minority ethnic populations.
Finally, there were limitations of the spatially referenced data used in this study, including issues of scale and multiple addresses. Previous research has used a range of geographical regions to determine spatial boundaries, but there is little evidence showing at which scale geographical factors have salience.34 Furthermore, although the registered address could be where a migrant resides, they might spend substantial portions of time in different neighbourhood environments; as we do not have a measure of time spent in other spaces, we also do not know their exposure to migrant density in those spaces.34 Neighbourhood factors were measured at a single point in time and thus do not capture the cumulative exposures over time or differing exposure levels for those who have moved.35 Our multilevel analysis accounting for neighbourhood clustering represents an advance over previous research; however, further research using spatial modelling techniques would enhance our understanding of how individuals experience spatial exposures.
This study has several strengths, including nearly complete coverage in Sweden for 19 years of follow-up, including migrants arriving between 1982 and 2011. This ensured we included several important waves of immigration to Sweden of both labour migrants and refugees from diverse settings, such as Iraq, Iran, Afghanistan, and eastern Africa.36 Our long follow-up period, until December, 2016, allowed us to investigate migrant density throughout Sweden. The choice of a multilevel approach correctly modelled dependencies within the data in a survival context for the first time, to our knowledge, which is a notable advance on previous research. A wide range of confounders were considered and both own-region and generation-specific migrant density were investigated, which were measured prospectively in relation to the outcome.
Previous research has shown an overall migrant density effect for psychotic disorders14, 15, 16, 17, 18, 19, 20 and psychotic experiences,37 but that the effect was concentrated in certain migrant groups, including black African and black Caribbean groups.37, 38, 39 Consistent with these studies, we found an overall migrant density effect, with stronger evidence for migrants from Asia and sub-Saharan Africa than other groups.
Our finding that the migrant density effect was similar in migrants and children of migrants contradicts a Danish study that found stronger neighbourhood ethnic density effects for children of migrants than migrants.1 There were methodological differences between the studies that might explain these disparate results. The Danish study was based on a smaller cohort of 90 476 migrants and their children, compared with the 468 223 included in our study. The Danish study used parish areas (3500 residents) whereas our study used smaller neighbourhoods (median of 726 residents). There were some differences in how we classified regions and calculated migrant density. The Danish study did not account for the multilevel nature of these data in the analysis. These divergent results could be partially explained by different national approaches to migration and integration in Sweden and Denmark; however, these countries are similar in other ways, so this is unlikely to fully account for the observed differences. Considering these contrasting results by generation status, more research is needed to reach a consensus.
There are many aspects of the neighbourhood that could explain elevated risk of psychotic disorders in some migrant groups. Previous research has highlighted the importance of population density and neighbourhood deprivation as explanatory factors for elevated psychotic disorders in migrant groups. As migrants are more likely to reside in urban areas, and urbanicity has been linked to increased rates of psychotic disorders,40 we controlled for population density. Neighbourhood deprivation could also play a role in the patterning of psychosis risk, as residential segregation by socioeconomic status and ethnicity is persistent in many cities,13 and migrants and minority ethnic groups are more likely to live in deprived neighbourhoods owing to limited socioeconomic resources and structural racism.41, 42, 43 Thus, we controlled for neighbourhood deprivation to ensure the propensity for migrant groups to reside in more deprived neighbourhoods did not account for our findings.
It is plausible that the observed migrant density effect is due to aspects of the neighbourhood social environment, including the impact of social support, social stress, experiences of inclusion or exclusion, and experiences of discrimination and racism. Migrant density might work through psychosocial pathways12 to provide increased social support, enhance feelings of inclusion, and buffer individuals from experiences of racism and discrimination. While family members comprise an important source of social support and social capital,44 relationships with friends and neighbours can contribute to a wider sense of inclusion and belonging. Migrants moving to areas with a high concentration of individuals from the same region could experience a greater sense of belonging, feel connected to others, and have access to emotional and practical support.45 Furthermore, living in areas of low ethnicity density could lead to the perception of being different from one's social environment, contributing to higher levels of social stress, and more frequent experiences of discrimination.21, 22 Previous research has shown lower rates of reported discrimination and low social support among minority ethnic individuals living in areas of high migrant density.38 The direct experience of discrimination has been shown to affect health, but also the fear of racisim46 and perceived discrimination47 can have detrimental effects on mental health. Our findings of a protective migrant density effect among probable visible minority migrants could be due to reduced exposure to racism, discrimination, or feelings of isolation and otherness, although this was not found for children of migrants.22, 48
Our results align with a proposed neurobiological pathway to psychotic disorders via alterations to threat perception.47, 49, 50, 51 Using functional MRI, McCutcheon and colleagues52 showed increased amygdala responses to outgroup faces for both black and white ethnic groups, with evidence that this was more pronounced for those from residential areas with low own-region ethnicity. Minority ethnic groups, particularly those living in areas of low own-region migrant density, might have more frequent exposure to outgroup faces, corresponding to heightened amygdala responses.53 The greater outgroup contact in day-to-day life for visible minority individuals and the neurobiological response to threat experiences are consistent with our observation of highest risk among probable visible minority living in areas of low migrant density.
In conclusion, we found evidence that migrant density reduced the risk of psychotic disorders for migrants and children of migrants. Generation-specific density was more strongly associated with reduced risk of psychotic disorder for migrants, for whom having neighbours with a shared migration experience, language, or culture could be important. For children of migrants who were born in Sweden and thus face fewer linguistic and cultural barriers to integration than their parents, generation-specific density was less important than overall migrant density. The protective effect of migrant density was pronounced for probable visible minority migrants and children of migrants but not for probable non-visible minority individuals. While these findings largely align with previous studies, this study shows unique patterns of risk by generation status; further research is warranted to understand the underlying mechanisms of the migrant density effect.
Acknowledgments
Acknowledgments
This work was supported by a Sir Henry Dale Fellowship jointly funded by the Wellcome Trust and the Royal Society (grant number: 101272/Z/13/Z to JBK), by Mental Health Research UK (to JD), and by a UCL Overseas Research Scholarship (to JD). JD, GL, and JBK are also supported by the National Institute for Health Research, University College London Hospital, Biomedical Research Centre. This research was also supported by the Swedish Research Council (grant number: 523-2010-1052 to CD) and FORTE (grant number 2014-1430; 2014-2678 to A-CH).
Contributors
JD, JBK, GL, A-CH, and CD were involved in study conception and design. JD extracted the data and completed the data analysis. JD, JBK, GL, A-CH, and CD contributed to data interpretation. JD wrote the first draft and all authors commented on the manuscript and provided input on the final manuscript.
Declaration of interests
JBK reports grants from the Wellcome Trust and Royal Society and GL reports grants from University College London, during the conduct of the study. The remaining authors declare no competing interests.
Supplementary Material
References
- 1.Schofield P, Thygesen M, Das-munshi J. Neighbourhood ethnic ww. Schizophr Res. 2018;195:501–505. doi: 10.1016/j.schres.2017.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dykxhoorn J, Hollander A-C, Lewis G, Magnusson C, Dalman C, Kirkbride JB. Risk of schizophrenia, schizoaffective, and bipolar disorders by migrant status, region of origin, and age-at-migration: a national cohort study of 1·8 million people. Psychol Med. 2019;49:2354–2363. doi: 10.1017/S0033291718003227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cantor-Graae E, Selten J-P. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162:12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- 4.Bourque F, Van Der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med. 2011;41:897–910. doi: 10.1017/S0033291710001406. [DOI] [PubMed] [Google Scholar]
- 5.Pedersen CB, Cantor-Graae E. Age at migration and risk of schizophrenia among immigrants in Denmark: a 25-year incidence study. Am J Psychiatry. 2012;169:1117–1118. doi: 10.1176/appi.ajp.2012.12050614. [DOI] [PubMed] [Google Scholar]
- 6.Veling W. Ethnic minority position and risk for psychotic disorders. Curr Opin Psychiatry. 2013;26:166–171. doi: 10.1097/YCO.0b013e32835d9e43. [DOI] [PubMed] [Google Scholar]
- 7.Kirkbride JB, Hollander A-C, Anderson KK. Migration and risk of psychosis in the Canadian context. CMAJ. 2015;187:637–638. doi: 10.1503/cmaj.150494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith GN, Boydell J, Murray RM. The incidence of schizophrenia in European immigrants to Canada. Schizophr Res. 2006;87:205–211. doi: 10.1016/j.schres.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 9.Bresnahan M, Begg MD, Brown A. Race and risk of schizophrenia in a US birth cohort: another example of health disparity? Int J Epidemiol. 2007;36:751–758. doi: 10.1093/ije/dym041. [DOI] [PubMed] [Google Scholar]
- 10.Morgan C, Knowles G, Hutchinson G. Migration, ethnicity and psychoses: evidence, models and future directions. World Psychiatry. 2019;18:247–258. doi: 10.1002/wps.20655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bécares L, Shaw R, Nazroo J. Ethnic density effects on physical morbidity, mortality, and health behaviors: a systematic review of the literature. Am J Public Health. 2012;102:33–66. doi: 10.2105/AJPH.2012.300832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaw RJ, Atkin K, Bécares L. Impact of ethnic density on adult mental disorders: narrative review. Br J Psychiatry. 2012;201:11–19. doi: 10.1192/bjp.bp.110.083675. [DOI] [PubMed] [Google Scholar]
- 13.Pickett KE, Wilkinson RG. People like us: ethnic group density effects on health. Ethn Health. 2008;13:321–334. doi: 10.1080/13557850701882928. [DOI] [PubMed] [Google Scholar]
- 14.Termorshuizen F, Smeets HM, Braam AW, Veling W. Neighborhood ethnic density and psychotic disorders among ethnic minority groups in Utrecht City. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1093–1102. doi: 10.1007/s00127-014-0842-z. [DOI] [PubMed] [Google Scholar]
- 15.Veling W, Susser E, Van Os J, Mackenbach JP, Selten JP, Hoek HW. Ethnic density of neighborhoods and incidence of psychotic disorders among immigrants. Am J Psychiatry. 2008;165:66–73. doi: 10.1176/appi.ajp.2007.07030423. [DOI] [PubMed] [Google Scholar]
- 16.Boydell J, Van Os J, Mckenzie K. Incidence of schizophrenia in ethnic minorities in London: ecological study into interactions with environment. BMJ. 2001;323:1336–1338. doi: 10.1136/bmj.323.7325.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirkbride JB, Morgan C, Fearon P, Dazzan P, Murray RM, Jones PB. Neighbourhood-level effects on psychoses: re-examining the role of context. Psychol Med. 2007;37:1413–1425. doi: 10.1017/S0033291707000499. [DOI] [PubMed] [Google Scholar]
- 18.Kirkbride JB, Boydell J, Ploubidis G. Testing the association between the incidence of schizophrenia and social capital in an urban area. Psychol Med. 2008;38:1083–1094. doi: 10.1017/S0033291707002085. [DOI] [PubMed] [Google Scholar]
- 19.Schofield P, Ashworth M, Jones R. Ethnic isolation and psychosis: re-examining the ethnic density effect. Psychol Med. 2011;41:1263–1269. doi: 10.1017/S0033291710001649. [DOI] [PubMed] [Google Scholar]
- 20.Schofield P, Thygesen M, Das-Munshi J. Ethnic density, urbanicity and psychosis risk for migrant groups—a population cohort study. Schizophr Res. 2017;190:82–87. doi: 10.1016/j.schres.2017.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bécares L, Nazroo J, Jackson J, Heuvelman H. Ethnic density effects on health and experienced racism among Caribbean people in the US and England: a cross-national comparison. Soc Sci Med. 2012;75:2107–2115. doi: 10.1016/j.socscimed.2012.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health Place. 2009;15:670–678. doi: 10.1016/j.healthplace.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Rutström I, EPiCSS group Psychiatry Sweden—the register linkage. Karolinksa Institutet. 2019. https://ki.se/en/phs/psychiatry-sweden-the-register-linkage-epicss-group
- 24.Dalman C, Broms J, Cullberg J, Allebeck P. Young cases of schizophrenia identified in a national inpatient register. Soc Psychiatry Psychiatr Epidemiol. 2002;37:527–531. doi: 10.1007/s00127-002-0582-3. [DOI] [PubMed] [Google Scholar]
- 25.Hollander A-C, Dal H, Lewis G, Magnusson C, Kirkbride JB, Dalman C. Refugee migration and risk of schizophrenia and other non-affective psychoses: cohort study of 1·3 million people in Sweden. BMJ. 2016;352 doi: 10.1136/bmj.i1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gomez SL, Kelsey JL, Glaser SL, Lee MM, Sidney S. Inconsistencies between self-reported ethnicity and ethnicity recorded in a health maintenance organization. Ann Epidemiol. 2005;15:71–79. doi: 10.1016/j.annepidem.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 27.Porter M, Todd A, Zhang L. Ethnicity or cultural group identity of pregnant women in Sydney, Australia: is country of birth a reliable proxy measure? Women Birth. 2016;29:168–171. doi: 10.1016/j.wombi.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 28.Saunders CL, Abel GA, El Turabi A, Ahmed F, Lyratzopoulos G. Accuracy of routinely recorded ethnic group information compared with self-reported ethnicity: evidence from the English Cancer Patient Experience survey. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-002882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dong Y, Peng C-YJ. Principled missing data methods for researchers. Springerplus. 2013;2:222. doi: 10.1186/2193-1801-2-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hollander A-C, Dalman C. Utrikesfödda använder mindre psykiatrisk vård än svenskfödda de första åren i Sverige. Lakartidningen. Jan 14, 2020 http://lakartidningen.se/Klinik-och-vetenskap/Temaartikel/2020/01/Utrikesfodda-anvander-mindre-psykiatrisk-vard-an-svenskfodda-de-forsta-aren-i-Sverige/ [PubMed] [Google Scholar]
- 31.Whitley R, Kirmayer LJ, Groleau D. Understanding immigrants' reluctance to use mental health services: a qualitative study from Montreal. Can J Psychiatry. 2006;51:205–209. doi: 10.1177/070674370605100401. [DOI] [PubMed] [Google Scholar]
- 32.Derr AS. Mental health service use among immigrants in the United States: a systematic review. Psychiatr Serv. 2016;67:265–274. doi: 10.1176/appi.ps.201500004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hussein M, Diez Roux A V, Field RI. Neighborhood socioeconomic status and primary health care: usual points of access and temporal trends in a major US urban area. J Urban Health. 2016;93:1027–1045. doi: 10.1007/s11524-016-0085-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang Z, Manjourides J, Cohen T, Hu Y, Jiang Q. Spatial measurement errors in the field of spatial epidemiology. Int J Health Geogr. 2016;15:21. doi: 10.1186/s12942-016-0049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Price C, Dalman C, Zammit S, Kirkbride JB. Association of residential mobility over the life course with nonaffective psychosis in 1·4 million young people in Sweden. JAMA Psychiatry. 2018;75:1128–1136. doi: 10.1001/jamapsychiatry.2018.2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Migrationsverket Sweden and migration. 2018. https://sweden.se/migration
- 37.Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. Int J Soc Psychiatry. 2000;46:34–46. doi: 10.1177/002076400004600105. [DOI] [PubMed] [Google Scholar]
- 38.Das-Munshi J, Bécares L, Boydell JE. Ethnic density as a buffer for psychotic experiences: findings from a national survey (EMPIRIC) Br J Psychiatry. 2012;201:282–290. doi: 10.1192/bjp.bp.111.102376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bécares L. Ethnic density effects on psychological distress among Latino ethnic groups: an examination of hypothesized pathways. Health Place. 2014;30:177–186. doi: 10.1016/j.healthplace.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 40.March D, Hatch SL, Morgan C. Psychosis and place. Epidemiol Rev. 2008;30:84–100. doi: 10.1093/epirev/mxn006. [DOI] [PubMed] [Google Scholar]
- 41.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Musterd S. Social and ethnic segregation in Europe: levels, causes, and effects. J Urban Aff. 2005;27:331–348. [Google Scholar]
- 43.Quillian L. Segregation and poverty concentration: the role of three segregations. Am Sociol Rev. 2012;77:354–379. doi: 10.1177/0003122412447793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dykxhoorn J, Hollander A-C, Lewis G, Dalman C, Kirkbride JB. Family networks during migration and risk of non-affective psychosis: a population-based cohort study. Schizophr Res. 2019;208:268–275. doi: 10.1016/j.schres.2019.01.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Straiton ML, Ledesma HML, Donnelly TT. A qualitative study of Filipina immigrants' stress, distress and coping: the impact of their multiple, transnational roles as women. BMC Womens Health. 2017;17:72. doi: 10.1186/s12905-017-0429-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karlsen S, Nazroo JY. Fear of racism and health. J Epidemiol Community Health. 2004;58:1017–1018. doi: 10.1136/jech.2004.020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Veling W, Pot-Kolder R, Counotte J, van Os J, van der Gaag M. Environmental social stress, paranoia and psychosis liability: a virtual reality study. Schizophr Bull. 2016;42:1363–1371. doi: 10.1093/schbul/sbw031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Das-Munshi J, Becares L, Dewey ME, Stansfeld SA, Prince MJ. Understanding the effect of ethnic density on mental health: multi-level investigation of survey data from England. BMJ. 2010;341 doi: 10.1136/bmj.c5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chekroud AM, Everett JAC, Bridge H, Hewstone M. A review of neuroimaging studies of race-related prejudice: does amygdala response reflect threat? Front Hum Neurosci. 2014;8:179. doi: 10.3389/fnhum.2014.00179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pinkham AE, Liu P, Lu H, Kriegsman M, Simpson C, Tamminga C. Amygdala hyperactivity at rest in paranoid individuals with schizophrenia. Am J Psychiatry. 2015;172:784–792. doi: 10.1176/appi.ajp.2014.14081000. [DOI] [PubMed] [Google Scholar]
- 51.Reininghaus U, Kempton M, Valmaggia LR. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. 2016;42:712–722. doi: 10.1093/schbul/sbv190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCutcheon R, Bloomfield M, Dahoun T. Amygdala reactivity in ethnic minorities and its relationship to the social environment: an fMRI study. Psychol Med. 2018;48:1985–1992. doi: 10.1017/S0033291717003506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Veling W, Selten J-PP, Susser E, Laan W, Mackenbach JP, Hoek HW. Discrimination and the incidence of psychotic disorders among ethnic minorities in the Netherlands. Int J Epidemiol. 2007;36:761–768. doi: 10.1093/ije/dym085. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.