Summary
Background
A quarter of a century ago, two global events—the International Conference on Population and Development in Cairo, and the Fourth World Conference on Women in Beijing—placed gender equality and reproductive health and rights at the centre of the development agenda. Progress towards these goals has been slower than hoped. We used survey data and national-level indicators of social determinants from 74 countries to examine change in satisfaction of contraceptive need from a contextual perspective.
Methods
We searched for individual-level data from repeated nationally representative surveys that included information on sexual and reproductive health, and created a single dataset by harmonising data from each survey to a standard data specification. We described the relative timings of sexual initiation, first union (cohabitation or marriage), and first birth and used logistic regression to show the change in prevalence of sexual activity, demand for contraception, and modern contraceptive use. We used linear regression to examine country-level associations between the gender development index and the expected length of time in education for women and the three outcomes: sexual activity, demand for contraception, and modern contraceptive use. We used principal component analysis to describe countries using a combination of social-structural and behavioural indicators and assessed how well the components explained country-level variation in the proportion of women using contraception with fractional logistic regression.
Findings
In 34 of the 74 countries examined, proportions of all women who were sexually active, not wanting to conceive, and not using a modern contraceptive method decreased over time. Proportions of women who had been sexually active in the past year changed over time in 43 countries, with increases in 30 countries; demand for contraception increased in 42 countries, and use of a modern method of contraception increased in 37 countries. Increases over time in met need for contraception were correlated with increases in gender equality and with women's time in education. Regression analysis on the principal components showed that country-level variation in met contraceptive need was largely explained by a single component that combined behavioural and social-contextual variables.
Interpretation
Progress towards satisfying demand for contraception should take account of the changing context in which it is practised. To remove the remaining barriers, policy responses—and therefore research priorities—could require a stronger focus on social-structural determinants and broader aspects of sexual health.
Funding
UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction.
Introduction
The mid-1990s saw two landmark events in global efforts to advance gender equality and reproductive health and rights. In 1994, the UN International Conference on Population and Development in Cairo, Egypt, created a paradigm shift, taking contraception out of the context of population control and into the wider context of sexual and reproductive health and rights.1 The following year, the UN's Fourth World Conference on Women: Action for Equality, Development and Peace, held in Beijing,2 marked an important watershed in the advancement of gender equality, setting strategic objectives for the advancement of women and, crucially, emphasising the importance of social determinants in understanding women's health.
The Cairo and Beijing conferences fundamentally shifted thinking on development,3 leading to a global consensus that reproductive health and rights are essential, not only in improving reproductive health outcomes, but in achieving broader improvements in health, education, and economic outcomes,4, 5 and that women's equality is a precondition for securing the wellbeing and prosperity of all people: “The full and equal participation of women in civil, cultural, economic, political and social life, at the national, regional and international levels, and the eradication of all forms of discrimination on grounds of sex, are priority objectives of the international community.”6
Research in context.
Evidence before this study
Before undertaking the study, we searched PubMed and Google Scholar for studies published between Jan 1, 2000, and Sept 30, 2019, with no language restrictions using the search terms “timing of reproductive health events”, “timing of family life events”, “unmet contraception need”, “unmet need for family planning”, “ICPD”, “contraceptive use”, “non-contraceptive use“, “trends”, and “cross-national variation” to identify studies describing trends in contraceptive use and policy-related factors associated with change, globally. We examined quantitative, qualitative, and mixed methods studies. Several studies have described regional variation and trends in unmet need for contraception. They have, variously, assessed the extent to which targets are being met, whether the scale of progress is less or greater than might have been expected, and what the demographic impact and development benefits might be. Few have examined contraceptive use in the wider social-structural context or in relation to other sexual health-related behaviours.
Added value of this study
We use data from national and international surveys to describe change over time and differences between regions in met need for contraception in the context of demographic change, wider social-structural determinants, and other sexual health-related behaviours. We find wide cross-national variation in demand for and use of modern contraceptive methods, with modest increases over time. The length of time spent single and sexually active, and the interval between sexual initiation and first birth, has increased in many countries. Indicators of women's social position—ie, gender equality and expected years in education—account for some of the variability in country-level progress made in meeting contraceptive need, as do indicators measuring wider aspects of sexual behaviour.
Implications of all the available evidence
Previous research showing small gains in meeting need for contraception has been interpreted as evidence of slow progress towards goals relating to reproductive health and rights. A perspective on progress that takes account of increased demand for contraception, and the demographic and social contextual background in which it is practised, is important to adjust this perspective and guide programmatic action. Monitoring trends in contraceptive use in the broader context of sexual health and in the social context of women's lives is important to assess progress towards the goals of the International Conference on Population and Development and their legacy.
Recognition in the Cairo and Beijing conferences that reproductive health and women's empowerment are intertwined, and that each is necessary for the advancement of society, has had a catalytic effect on contraception provision and use7 and has underpinned successive global initiatives to advance their goals. The importance of contraceptive use to progress in all major Sustainable Development Goal (SDG) themes is reflected in SDG indicator 3.7.1: “The proportion of women of reproductive age (aged 15–49 years) who have their need for family planning satisfied with contraceptive use”.8 In operational terms, this describes the proportion of women who currently do not want to become pregnant and are using contraception.9 Policy makers have set a benchmark of meeting 75% of the demand for family planning in all countries by 2030; achieving this is expected to bring both demographic and development benefits.5
Monitoring trends in contraceptive use in the broader context of sexual health and in the social context of women's lives is important to examine progress towards goals related to gender equality, development, and reproductive rights, and 2020 is a pivotal year in which to do so. Not only does it mark a quarter of a century since the Cairo and Beijing conferences, it also represents a 5-year milestone towards achieving the 2030 SDGs. Considerable effort has been invested in documenting cross-national comparisons and trends in contraceptive use and unmet contraceptive need,10, 11, 12 assessing whether targets are being met,13 and estimating impact.5 Differences between countries and the trends over time also need to be set in the social and behavioural context in which they occur. We use data from national and international surveys to describe change over time in sexual activity, demand for and use of modern contraceptive methods, and link these with country-level social determinants and aspects of sexual lifestyles.
Methods
Data sources
We aimed to identify and obtain individual-level data from all repeated nationally representative surveys that included information on sexual and reproductive health. We gave preference to surveys that sampled men and women, irrespective of marital status, and those that covered a wide age range. However, we did not discard surveys with a more limited target population if those were the only data available in that country.
We began with a database of 98 surveys from 55 countries that we had initially constructed for our 2006 global review of sexual behaviour.14 We identified subsequent surveys in these countries via internet searches and personal contacts.
We identified and obtained individual-level data for all Demographic and Health Surveys (DHS),15 AIDS Indicator Surveys (AIS),15 and Multiple Indicator Cluster Surveys (MICS)16 from their respective repositories. We also searched other data repositories: UK Data Archive,17 Inter-university Consortium for Political and Social Research,18 DataFirst,19 South Africa's Human Sciences Research Council's Research Data Service,20 and Global Health Data Exchange.21 Additionally, we searched the literature using PubMed and Google Scholar for pre-existing studies and their data sources. We did internet searches and used Twitter to identify potential sources of data. Our searches were done in English but we did not include any language restrictions on the resulting articles or datasets. We identified geographical areas where we lacked data and contacted researchers in those countries to identify suitable data.
In addition to sexual health data, we obtained national-level social and economic indicators from the UN22 and included those with the most complete data (gross domestic product [GDP] per capita, gender development index, gender inequality index, female and male expected years of education). Where data were not available for a year, we carried them forwards from the previous estimate.
Most surveys were face-to-face interviews, done by experienced interviewers as part of large-scale national surveys. National sample frames were used; sample sizes varied depending on the nature of the survey: DHS typically aim to sample 1% of households to obtain estimates across a wide range of reproductive health indicators whereas national surveys typically calculate sample size on the basis of a focused set of measures, thus providing a smaller set of estimates with greater precision.
Data management
Individual-level data from each survey were harmonised to a standard data specification and compiled into a single dataset. DHS, AIS, and MICS each use their own standard instruments with local adaptations (set out in the report for each survey) but some national surveys obtained data differently. Where there were inconsistencies between surveys in question wording, response categories, or denominators, we coded a variable that was broadly comparable to the data available in the DHS, since this was the most common data source. Where differences between the surveys were too great to generate a comparable variable, we excluded that country's data from analyses using that variable or did not analyse trends over time for that variable. The data specification and information available for each survey are available on request. We retained all survey design information including the original weights.
Summary measures and indicators
We defined summary measures that allowed us to maximise the number of surveys included in the analysis while remaining comparable. We allocated the entire female survey sample to one of six categories: (1) never had sex; (2) had sex but not in the past 12 months; (3) had sex in the past 12 months and currently pregnant; (4) had sex in the past 12 months and wants to have a child; (5) had sex in the past 12 months, does not want to have a child, and is using a modern method of contraception; and (6) had sex in the past 12 months, does not want to have a child, and is not using a modern method of contraception. We additionally estimated demand for contraception as the proportion of sexually active women who did not want to conceive, and the met need as the proportion of women who were sexually active and did not want to conceive who were using a modern method of contraception.
We defined users of modern contraceptive methods as those using any of the following: female and male sterilisation, oral contraceptives, intrauterine contraceptive device, injectables, implants, female and male condoms, diaphragm, contraceptive foam and jelly, contraceptive ring, cervical cap, and contraceptive sponge.
We defined women who did not want to conceive as those who did not want a child in the year following the survey. Some surveys did not ask respondents when they would like to conceive and we had to infer this from other questions (appendix pp 6–11). We assumed that not wanting to conceive at the time of the survey was equivalent to not wanting to conceive in the next year. Questions on contraceptive use also varied across surveys (appendix pp 6–11). We assumed that current contraceptive use, queried in both the DHS and MICS, was similar to the use ascertained in other surveys with different phrasing (for example, method used at last intercourse).
We listed indicators that described key aspects of sexual health relevant to the holistic concept of reproductive and sexual health.10 In each survey, we estimated all indicators for both men and women, then narrowed our focus to measures that were widely available.
We identified three key transitions: first sexual intercourse, first union (cohabitation or marriage), and first birth. Age at first sexual intercourse is a key indicator as it marks entry into the period of exposure to sexual and reproductive health outcomes including unintended pregnancy and sexually transmitted infection. First union is likely to coincide with changes in fertility preferences and sexual activity and, in some circumstances, access to reproductive and sexual health services. Age at first union was defined as either age at first marriage or cohabitation; we assumed that surveys asked about the one that was most locally relevant and treated them as equivalent. For each event, we estimated the lifetable median age at event and IQR, by birth cohort. From the survival functions, we estimated the cumulative proportions of people born in the 1990s who had first sexual intercourse before the ages of 15, 17, and 19 years and the proportions of those born in the 1980s who entered their first cohabitation or marriage by ages 18, 23, and 28 years.
We estimated the proportion of people who had more than one partner in the year before the survey, and the proportion of people who reported sex in the 4 weeks before the survey. We could not include measures describing the types of partners (ie, spousal or cohabiting vs non-cohabiting) or condom use due to inconsistencies across surveys and lack of data.
Data on abortion and post-abortion care are scarce and, where they are available, reporting is known to be poor23 and a global comparison is not possible.
Statistical analysis
We summarised each indicator for men and women in each survey. Unless otherwise stated, estimates are for all women aged 15–49 years. Ages at first sexual intercourse and first union and the proportions reporting sex and multiple partners in the past year were also estimated for men aged 15–49 years. Surveys that included only ever-married women are identified in the results; in analysis of these surveys, we did not scale the survey estimates to be representative of all women and therefore estimates from these countries are representative of ever-married women only. The earliest MICS in Serbia and Montenegro restricted relevant questions to people younger than 25 years.
Binary variables were summarised as proportions with logit confidence intervals. Ages at events were summarised with lifetable medians.
We looked for variation and trends in sexual activity, demand for contraception, and met need for contraception. We quantified the change over time in each outcome using logistic regression and plotted the odds ratios (ORs) for each country and survey, comparing each survey with the earliest survey in that country. To assess whether changes were concentrated in certain age groups, we included interaction terms in the logistic models and, where interaction terms made an important contribution to the model, we present stratified ORs.
We did an ecological analysis to describe the country-level association between two measures of gender equality (the gender development index and expected years of education for females) and our three outcome measures: (1) the proportion of women who are sexually active, (2) the proportion of sexually active women who do not want to conceive, and (3) the proportion of women who are sexually active, not wanting to conceive, and using a modern method of contraception. For each exposure–outcome combination, we fitted a linear regression model from which we extracted the regression coefficient and the R2 statistic.
We used principal component analysis (PCA) to assess whether other aspects of sexual health and social-structural determinants were correlated with use of contraception. We summarised the key measures of sexual behaviour for men and women in the most recent survey for each country, combined these with relevant national indicators of social-structural determinants, and did a PCA based on the correlation matrix to identify which linear combinations of country-level variables captured a large fraction of the variation in the summary statistics. We included, for both men and women, the cumulative proportions who had first sexual intercourse by ages 15 years and 17 years and who had first union by ages 18 years and 23 years, and estimates from the most recent survey of the proportions who had more than one partner in the past year, who had sex in the past year, and who had sex in the past 4 weeks. We included recent national estimates of the gender development index, the number of years of education expected for men and women, and GDP per capita. We then assessed the relation between the principal components and the national estimate of contraceptive met need using fractional logistic regression and used linear regression to show the relationship between the scores on the individual principal components and met need.
We used Stata 15 for all data management and analysis.
Role of the funding source
This work was funded by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction as part of a larger review of global sexual health data. The funder had no role in the analysis or interpretation of these results. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
We identified 249 surveys from 86 countries. Data for two countries could not be included due to local data sharing regulations24 and late arrival.25 Data were obtained for 242 surveys done between 1995 and 2018 in 84 countries. The number of surveys included in the analysis of sexual activity, contraceptive use, and contraceptive demand and in the analysis of the intervals between first sex, union, and birth are shown in the appendix (p 2), alongside a summary of the number of surveys used for each country and the total number of male and female survey respondents aged 15–49 years and 15–24 years (appendix pp 3–4). 74 countries had sufficient information to be included in the analysis and 63 countries had data from more than one survey. Most data were available for sub-Saharan Africa, followed by Latin America and the Caribbean. The list of countries contributing data to each analysis is given in the appendix (ecological analysis: pp 17–18; PCA: pp 20–21).
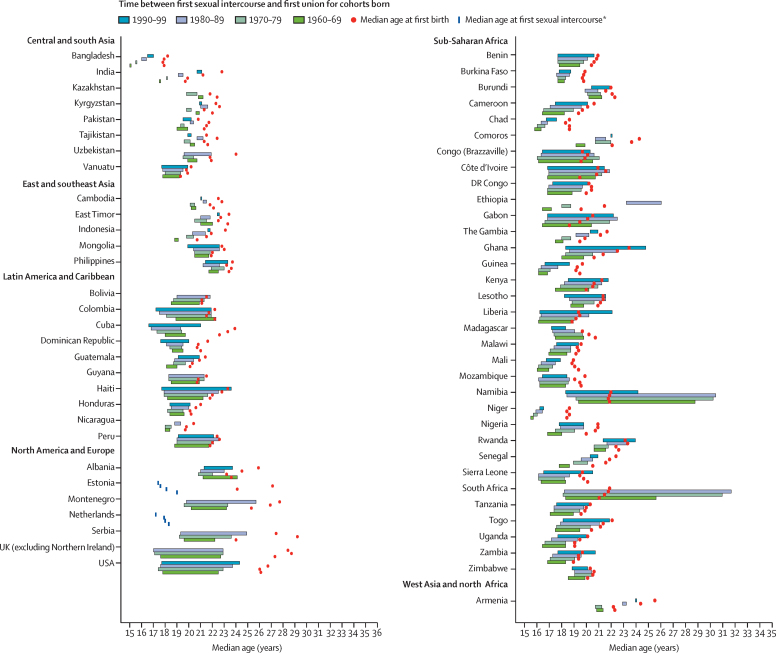
For 64 countries with sufficient data for logistic regression, we estimated ages at first sex, first union, and first birth (figure 1). Age at first sexual intercourse ranged from 15 to 24 years and, over time, has decreased in some countries (eg, Cuba, Columbia) and increased in others (eg, Uganda, Cameroon). Age at first union ranged between 15 and 31 years, and has increased over time in most countries. Age at first birth ranged from 18 to 31 years and has increased in most countries. There is considerable variation in the lengths of the intervals between first sexual intercourse and first union, and first sexual intercourse and first birth, indicating differing levels of demand for contraception and contraception use. In a substantial minority of countries, age at first birth precedes age at first union. The period spent sexually active before marriage or cohabitation has lengthened over time in many countries, due to changes in age at first sexual intercourse and first union, thus altering the age range of those who might be most in need of contraception.
Figure 1.
Length of the interval between the median ages at first sexual intercourse and first union, and the median age at first birth for women born between 1960 and 1999 by country and region
The interval between median ages at first sexual intercourse and first union (cohabitation or marriage) are shown as bars, whereas median age at first birth is shown as points. For each country, younger cohorts are presented first (blue and purple), followed by older cohorts (light and dark green). *Median age at first sexual intercourse is shown for countries without information on age at first union.
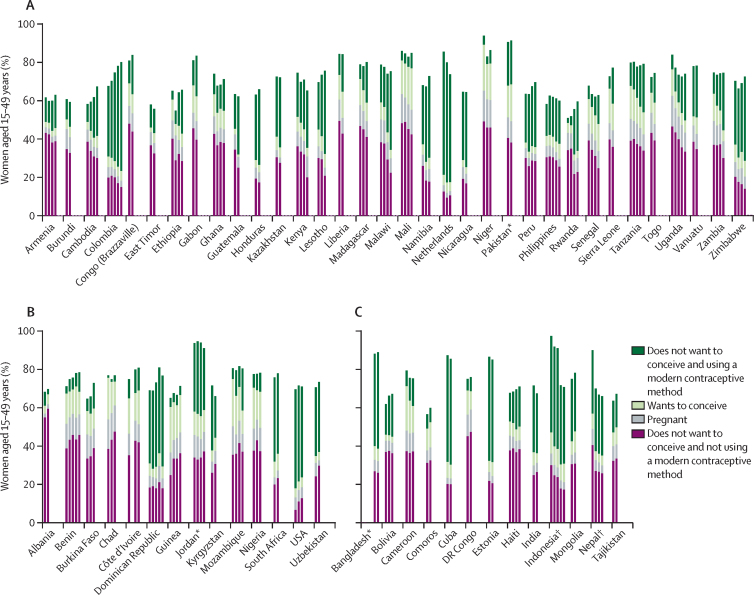
To understand satisfaction of contraceptive need, we considered trends over time in sexual activity, intention to conceive, and use of modern contraceptive methods. The proportion of contraceptive need satisfied is influenced by whether women are sexually active and whether they wish to conceive. These proportions vary substantially between countries and have changed over time (figure 2). The height of the bars in figure 2 show, for each survey, those who had sex in the past year as a proportion of all women. These sexually active women are subdivided into four groups: currently pregnant, wanting to conceive, not wanting to conceive and using a modern method of contraception, and not wanting to conceive and not using a modern method of contraception.
Figure 2.
Proportion of sexually active women according to desire to conceive, pregnancy status, and use of a modern contraceptive method
Countries are grouped according to the change over time in the proportion of sexually active women aged 15–49 years who do not want to conceive and are not using a modern contraceptive method and whether this proportion has A) decreased, B) increased, or C) remained the same. *Surveys of ever-married women only. †Surveys of ever-married women followed by surveys of all women; for India, only the all-women surveys are shown.
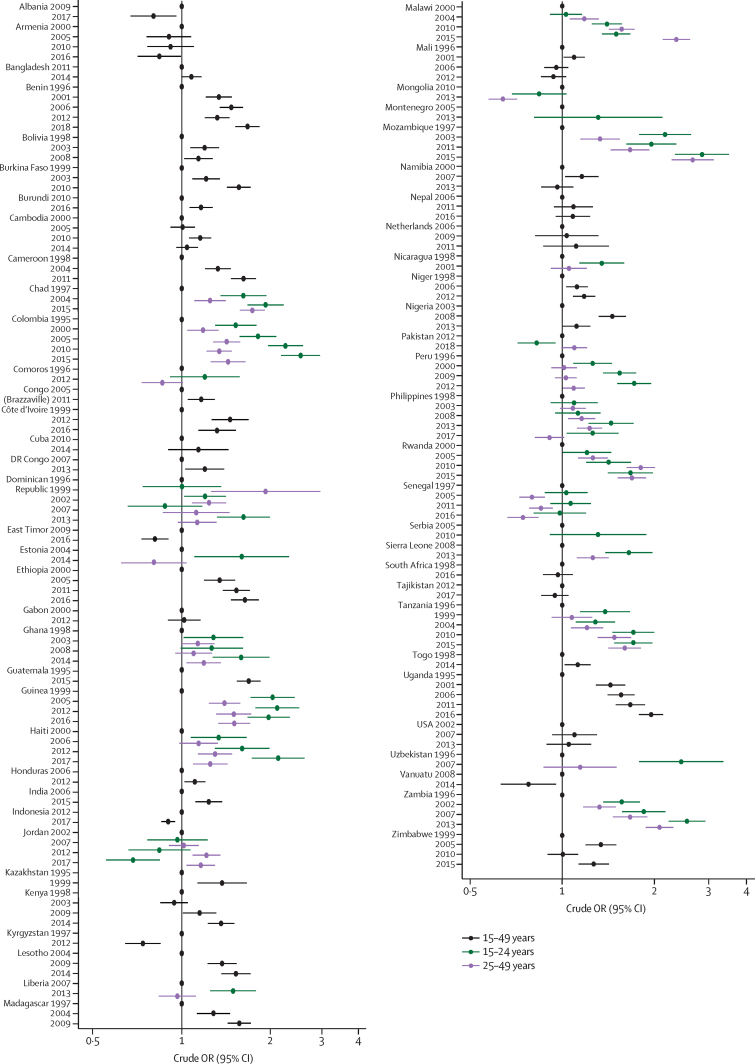
In 34 countries, the proportion of women who are sexually active and needing, but not using, modern methods of contraception has declined (figure 2A). In 32 countries in this group, the decline was accompanied by the expansion in use of modern contraceptive methods, although the changes were not simultaneous in all countries (figure 3). In eight countries (Cambodia, Colombia, Gabon, Lesotho, Namibia, Peru, Philippines, Sierra Leone), the decline occurred alongside an increase in the proportion of all women who were sexually active (figure 4) and in 24 countries, it also coincided with an increase in the proportion of women wanting to avoid conception (figure 5), with changes observed in all age groups.
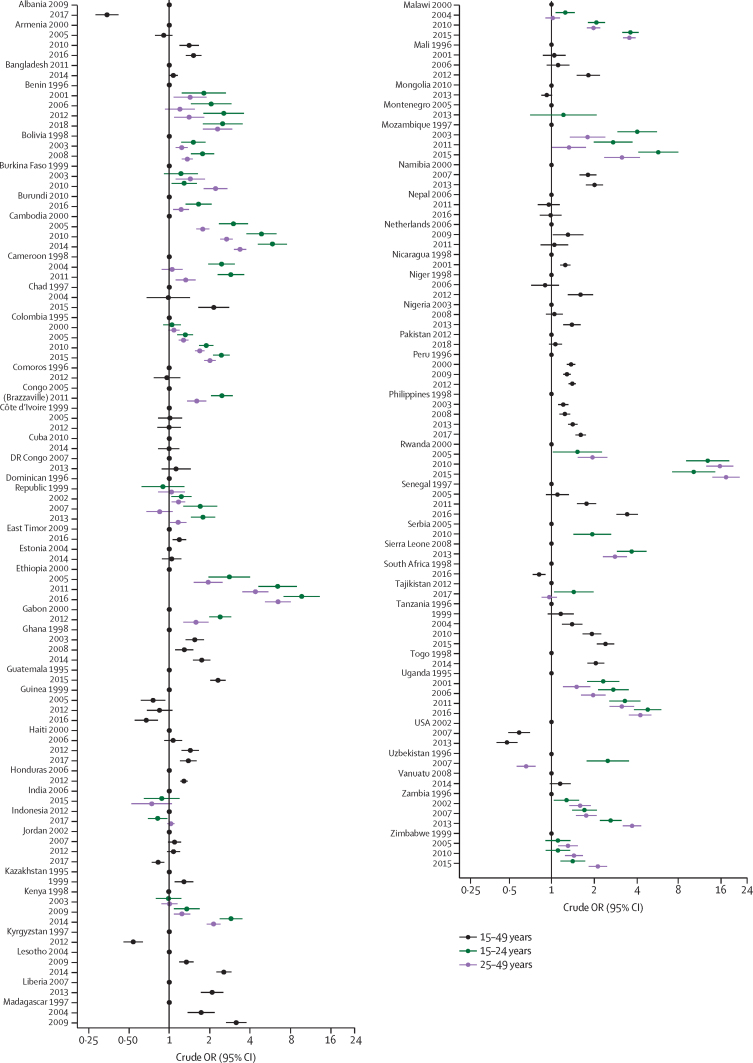
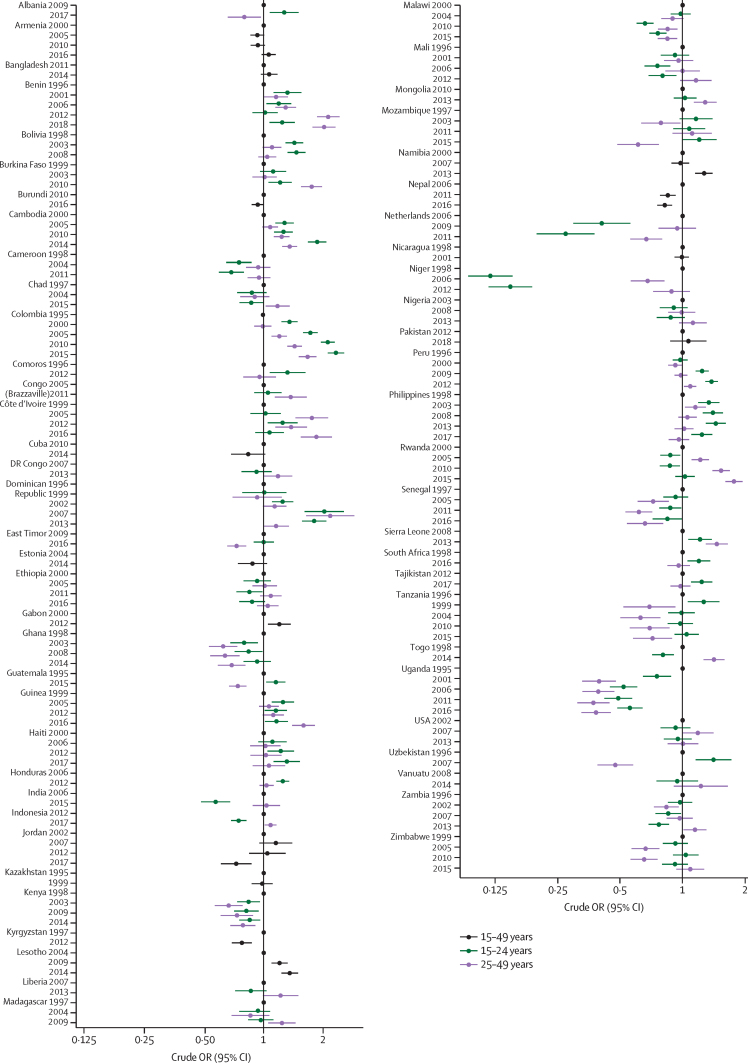
Figure 3.
Crude odds ratios, by country, for change over time in met need for modern contraceptive methods
Met need for modern contraceptive methods was estimated as the proportion of sexually active women aged 15–49 years who do not want to conceive and are using modern contraceptive methods. Where terms for interaction between age and year of survey made an important contribution to the model, we present stratified odds ratios.
Figure 4.
Crude odds ratios, by country, for change over time in the prevalence of sexually active women, as a proportion of all women aged 15–49 years
Women were defined as sexually active if they had had sex in the past year. Where terms for interaction between age and year of survey made an important contribution to the model, we present stratified odds ratios.
Figure 5.
Crude odds ratios, by country, for change over time in the demand for modern contraceptive methods
Demand for modern contraceptive methods was estimated as the proportion of sexually active women aged 15–49 years who do not want to conceive. Where terms for interaction between age and year of survey made an important contribution to the model, we present stratified odds ratios.
In 14 countries, the proportion of women who are sexually active and needing, but not using, a modern contraceptive method has increased (figure 2B). In five countries (Benin, Burkina Faso, Côte d'Ivoire, Dominican Republic, and Guinea), we see an overall increase in the proportion of women who were sexually active and an increase in the odds of sexual activity (figure 4), and in seven (Benin, Burkina Faso, Chad, Côte d'Ivoire, Guinea, Mozambique, and Nigeria), an increase in the proportion of those women not wanting to conceive (figure 5). In six countries (Benin, Burkina Faso, Chad, Dominican Republic, Mozambique, and Nigeria), the increase in unmet need for contraception occurred despite increases in modern contraceptive method use, including a substantial increase in Mozambique (figure 3). The odds of contraceptive method use declined in six countries (Albania, Guinea, Jordan, Kyrgyzstan, South Africa, and the USA; figure 3) and was accompanied by an increase in the proportion of the population needing contraception in three of these countries (South Africa, Guinea, and Albania; figure 2). In Benin and Burkina Faso, the increased use of modern contraceptive methods was not sufficient to reduce the proportion of women who had demand for contraception but were not using it, because of substantial growth in the proportion of women who were sexually active and who did not want to conceive.
In 13 countries, there was no overall change over time in the proportion of women who were sexually active, not wanting to conceive, and not using contraception (figure 2C). In three countries (Bolivia, Cameroon, and Haiti), this was because divergent trends over time for younger and older women cancelled each other out (appendix pp 12–16), and in Haiti and Bolivia, increases in use of modern contraceptive methods were not enough to meet increased demand and an increased proportion of sexually active young women (Figure 3, Figure 4).
43 countries have seen a change over time in the proportion of women who had sex in the year before the survey, 30 of which have seen increases (figure 4). In 37 countries, the change differed by age group, with differences in the direction and magnitude of effects and no overall pattern.
In 42 countries, the odds of sexually active women not wanting to conceive increased over time (figure 5). In four countries (Liberia, Nicaragua, Peru, and Uzbekistan), this increase occurred only in one age group, with no change in the other age group. In nine countries, demand for contraception declined over time in at least one age group.
In 37 countries, there was an increase over time in the odds of modern contraceptive method use among women who do not wish to conceive (figure 3). In 20 countries, this increase was different for women aged 15–24 years and those aged 25–49 years. There was no change in 12 countries and a decline in the remainder. In some countries, such as Ethiopia and Rwanda, there were some striking increases, and many saw the odds of modern contraceptive method use triple over a 15–20-year period.
In the 67 countries with data on sexual activity, demand for contraception, and use of contraception, the UN estimate of the gender development index for the year of the most recent survey data ranged from 0·61 to 1 (where 1 indicates complete gender parity and 0 complete gender inequality), with a median of 0·89 (IQR 0·84–0·95), and linear regression results (clustered by country) showed a strong positive association with demand for modern contraceptive method use (coefficient 66·7; p<0·0001; R2=0·46) and the proportion of women with a demand for contraception who are using a modern contraceptive method (134·7; p<0·0001; R2=0·34; appendix p 19).
The expected years of education for females ranged from 2 to 21 years with a median of 10 years (IQR 7·7–12·3) and also showed a strong positive correlation with demand for (coefficient 2·3; p<0·0001; R2=0·63) and use of (4·7; p<0·0001; R2=0·53) modern contraceptive methods in linear regression models.
As gender inequality declines at the country level, and expected years of female education increases, the proportion of women wanting to avoid conception increases, as does the proportion using a modern contraceptive method among those who have demand for contraception (appendix p 19).
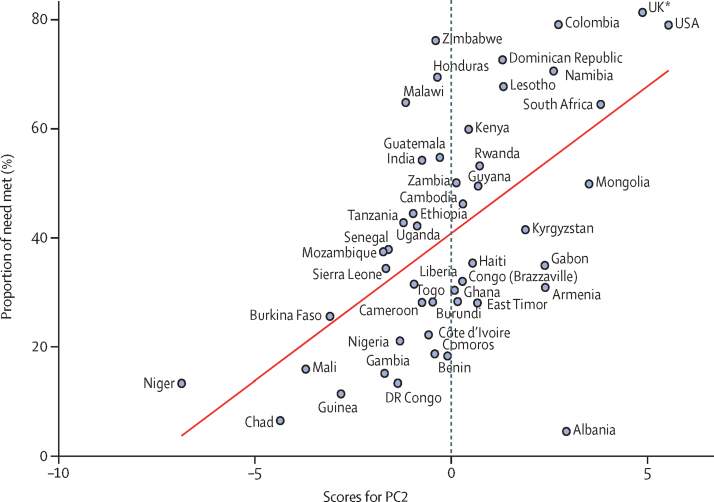
Full PCA results are given in the table, alongside results from fractional logistic regression and the correlation coefficients between each principal component and contraceptive met need. Four components had eigenvalues greater than 1 and collectively explained 84% of the total variation. Country-level fractional logistic regression showed that principal components 2 (PC2) and 4 (PC4) were positively associated with met need (table).
Table.
Principal component analysis
| Principal component 1 | Principal component 2 | Principal component 3 | Principal component 4 | ||
|---|---|---|---|---|---|
| Proportions and associations | |||||
| Proportion of variance explained | 0·35 | 0·30 | 0·11 | 0·09 | |
| Cumulative proportion | 0·35 | 0·64 | 0·75 | 0·84 | |
| Coefficient of regression of scores on contraceptive met need | 0·05; p=0·209 | 0·26; p<0·0001 | −0·06; p=0·444 | 0·20; p=0·013 | |
| Correlation coefficient for scores with contraceptive met need | 0·165 | 0·583 | −0·042 | 0·2177 | |
| Loadings on principal components | |||||
| Proportions of survey respondents | |||||
| Men | |||||
| Had first sexual intercourse by age 15 years | 0·2744 | 0·1260 | −0·3767 | 0·1792 | |
| Had first sexual intercourse by age 17 years | 0·3190 | 0·1453 | −0·3059 | 0·1417 | |
| Had first union by age 18 years | 0·2209 | −0·1360 | 0·0549 | 0·4509 | |
| Had first union by age 23 years | 0·1910 | −0·1360 | 0·2631 | 0·5115 | |
| Had >1 partner in the past year | 0·3299 | 0·0076 | −0·2963 | −0·0902 | |
| Had sex in the past year | 0·3273 | 0·1574 | 0·0266 | 0·1212 | |
| Had sex in the past 4 weeks | 0·2573 | 0·1393 | 0·3402 | 0·1611 | |
| Women | |||||
| Had first sexual intercourse by age 15 years | 0·3083 | −0·2239 | −0·0525 | −0·1687 | |
| Had first sexual intercourse by age 17 years | 0·3399 | −0·1521 | −0·1011 | −0·2121 | |
| Had first union by age 18 years | 0·1289 | −0·3883 | 0·0596 | −0·0090 | |
| Had first union by age 23 years | 0·0915 | −0·3401 | 0·1528 | 0·1505 | |
| Had >1 partner in the past year | 0·2544 | 0·2150 | −0·0317 | −0·2613 | |
| Had sex in the past year | 0·3277 | −0·0163 | 0·1211 | −0·3271 | |
| Had sex in the past 4 weeks | 0·1871 | 0·0459 | 0·5724 | −0·1406 | |
| Social-structural variables | |||||
| Expected years of education (female) | −0·0057 | 0·4039 | 0·1281 | 0·0920 | |
| Expected years of education (male) | 0·0224 | 0·3683 | 0·1292 | 0·0519 | |
| Gender development index | −0·0274 | 0·3258 | −0·1503 | 0·2844 | |
| GDP per capita | 0·1081 | 0·2976 | 0·2216 | −0·2254 | |
Table shows the proportion of the variance explained by each component, the associations between the component scores and the proportion of women who do not want to conceive who are currently using a modern method, and the loadings on the principal components of each variable. GDP=gross domestic product.
PC2 discriminates countries based on ages at first sexual intercourse and first union, multiple partnerships among women, sexual activity among men, and social and economic indicators. Countries with higher ages at first sexual intercourse for women, lower ages for men, and higher ages at first union for both sexes had a high score, as did countries with higher prevalence of multiple partnerships among women and more sexual activity among men. Countries with greater gender equality, longer time in education, and higher GDP also scored highly. Figure 6 shows contraceptive met need by score for PC2, and there is a clear positive correlation between the two estimates (correlation coefficient 0·58; table).
Figure 6.
Linear relationship of PC2 score with met need for modern contraceptive methods
Met need for modern contraceptive methods was estimated as the proportion of sexually active women aged 15–49 years who do not want to conceive and are using modern contraceptive methods, with the regression line from a linear regression of PC2 score and met need shown in red. The coefficients on PC2 for all included variables are shown in the table. PC2=principal component 2. *Excluding Northern Ireland.
PC4 distinguishes countries on gender development measures (gender development index and expected years of education for females and males) and men's age at first union, women's age at first sexual intercourse, and women's sexual activity in the past year. Countries with high scores have earlier ages at first union and first sexual intercourse for men, later age at first sexual intercourse for women, lower proportions of people with multiple partnerships, more recent sexual activity for men and less for women, and high gender development index combined with low GDP. The UK and the USA have low scores on PC4, whereas Honduras and Guatemala have high scores. Plotted against contraceptive met need (appendix p 22), the data are more dispersed than in figure 6 and the correlation between met need and PC4 is lower (0·22; table).
Discussion
Our results show that transitions to sexual initiation, entry into a cohabiting or marital relationship, and first parenthood vary widely between settings and over time. Age at first sexual intercourse has fallen in some countries and increased in others, the latter generally in tandem with increases in age at first union and first birth. There is considerable variation in the intervals between first sexual intercourse and first union, and first sexual intercourse and first birth, but generally they have widened, lengthening time spent sexually active and single or child-free, and thus increasing demand for contraception. The proportion of women who are sexually active has changed over time in most countries, and changes have not been confined to young women. Likewise, changes in the demand for and use of contraception are not solely seen among young women, no doubt reflecting diverse preferences in terms of postponing and limiting births. Use of modern contraceptive methods has increased in half of the countries in this analysis. Increases in demand for contraception were typically seen for women of all ages, whereas changes in sexual activity and modern contraceptive method use were age dependent in most of the countries where change occurred.
These trends have implications for the provision of services, especially where different patterns are seen for women at different ages. Some countries are faced with an expanding group of women who have a demand for contraception; however, even rapid increases in use of modern contraceptive methods might not be enough to immediately reduce the number of women who have a need for contraception but are not using a method. Where different changes occur for younger and older women, alterations might be needed to the provision of sexual and reproductive health services to ensure equitable coverage.
With regard to social determinants, our ecological analysis suggests that as gender inequality declines, and expected years of female education increase, demand for and the use of modern contraceptive methods increases. The regression results suggested that, for every 0·1-point increase in the gender development index, there was an increase of 6·7 percentage points in the proportion of women who were sexually active and did not want to conceive and an increase of 13·5 percentage points in the proportion of those women using modern methods of contraception. Each extra year of education expected for girls correlated with an increase of 2·3 percentage points in demand for modern contraceptive methods and an increase of 4·7 percentage points in use of modern contraceptive methods.
At a country level, PCA showed that a combination of variables describing wider aspects of sexual behaviour and social-structural determinants explained much of the variation in the met need for contraception. In the combination of variables most strongly associated with contraceptive met need (PC2), coefficients were higher for social-structural variables than for behavioural indicators (except for age at first union among women). That differences in met need for contraception can be explained using other aspects of sexual behaviour and social-structural determinants provides support for our hypothesis that demand for and use of contraception are embedded in a larger social context and should not be considered in isolation.
We have harmonised sexual behaviour data from countries with nationally representative survey data on sexual and reproductive health and social-structural determinants. This has permitted assessment of the role of sexual lifestyles and wider social context in met need for contraception. Harmonised data are inevitably a simplification and we made assumptions about the equivalence of data collected in different ways. These assumptions might have undermined our ecological analyses and PCA, but there are no outliers to suggest that our assumptions were incorrect and, since many of the surveys are from DHS and therefore directly comparable, we have confidence in the overall results. The harmonisation process highlighted the value of using a standard instrument to collect data on an agreed set of measures. As well as ensuring comparability of the data collected, the ease of use makes cross-country and trend analyses more feasible. Surveys from high-income countries typically covered sexual health topics in great detail but often did not collect items that have become the de-facto standard, through inclusion in DHS and other international efforts, which makes cross-national comparisons difficult. Furthermore, known individual-level determinants, such as wealth and place of residence, although commonly collected are not straightforward to harmonise and include in cross-country analyses because the meaning of, for example, urban residence varies widely. We lacked comparable global data on abortion and post-abortion care, which is an important omission in any assessment of the extent to which contraceptive need is met.
The generalisability of the results is weakened by a lack of data for some regions and for some aspects of sexual and reproductive health. Many countries had no surveys, and some surveys obtained very little information. The social-structural variables were not available for all countries and all timepoints. Countries in which data are available are likely to be different from those where they are not in ways that are important to the study objectives. This might have undermined the ecological analysis and the PCA, since countries with incomplete data were excluded, and precluded detailed analysis of regional differences. The surveys we have used were carried out over a long period and the interval between first and last survey ranges from 3 to 22 years. Thus, our comparisons are not directly comparable in calendar year terms, but we would not expect changes to be strongly linked to calendar time. The initial starting points of the countries were very different and there have not been coordinated changes in the determinants.
The relatively modest increases in the extent of met need for modern contraceptive methods shown in our analyses and those of others10, 12, 13, 26 have been interpreted as signalling a degree of failure in meeting reproductive health goals.1, 7, 26 Yet the picture is not wholly negative. Regions in which contraceptive use is lowest overall are also those in which individual countries have shown the most dramatic increase in the proportion of women needing, and using, modern methods of contraception—eg, Rwanda, Kenya, and Ethiopia. However, a recurring theme in our results is that increases in modern contraceptive method use might not keep up with increases in demand caused by changes in sexual activity and fertility intentions.
Trends need to be seen against a backcloth of rapid social and demographic change. Increases in the proportion of single women who are sexually active, the near-universal desire for smaller families, longer intervals between marriage or cohabitation and first parenthood, and the postponement of parenthood in many countries, shown both in our data and elsewhere, have created challenges that were less apparent a quarter of a century ago.
Evidence of an association, at the national level, between gender equality, education, and met need for modern contraceptive methods supports the International Conference on Population and Development's emphasis on the importance of the empowerment of women in reaching its goals. Gender equality is likely to affect contraceptive use through the degree to which women engage in sexual activity and are able to negotiate contraceptive use, the extent of freedom to access services, and power imbalances in personal relationships. While studies have highlighted problems of access, lack of knowledge, and fear of side-effects as barriers to use,27, 28, 29 they have also shown that negative perceptions among people close to potential users can be a barrier to the adoption of modern contraceptive methods.28, 30, 31 Societal attitudes to women and their reproductive health could be reflected, via the political process, in the provision, or otherwise, of effective family planning services that are shown to be associated with satisfying contraceptive need.32
Our finding of an association between contraceptive use and a combination of variables relating to sexual health vindicates recent efforts by WHO to adopt a broader, integrated concept of sexual and reproductive health and to translate it into a framework for policy and practice.33 Others have shown that non-use of contraception is associated with intimate partner violence and non-consensual sex34, 35, 36, 37 and sexual satisfaction.38, 39, 40 To date, emphasis in terms of efforts to improve contraceptive use has tended to be on access; however, progress contingent on further improvements to provision might be limited.28 The most promising interventions now could well be those focusing on social-structural changes to remove remaining barriers and on influences on ability to achieve fertility intentions at the social-contextual level.
The policy response might need to shift, and with it, the research agenda. Given the diversity seen in permutations of levels of sexual activity, demand for contraception, and use of contraception, there is clearly considerable variation in ways in which different countries are addressing and meeting their targets. A better understanding of the mechanisms by which social determinants and lifestyle factors affect ability to achieve fertility intentions in different contexts is crucial to programmatic efforts to increase contraceptive use.
Data sharing
The data used in this paper have been shared with the authors and ownership, and access to, the data rests with the original producers.
Acknowledgments
Acknowledgments
This work was funded by a grant from the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction. We are grateful to the researchers who shared their national survey data with us: Helle Karro, Kai Haldre, and Inge Ringmets (Estonia), for data from the Estonian Women's Health 2014 survey report (Department of Obstetrics and Gynaecology, University of Tartu; funded by the European Regional Development Fund through the Estonian Research Council project TerVe [grant number 3.2.1002.11–0002]; Research Ethics Committee of the University of Tartu [number 226/T-7; 17.06.2013]); and Hanneke de Graaf and Ciel Wijsen (Netherlands), for data from Rutgers International Sexual Health in the Netherlands surveys.
Contributors
ES, RHS, MJP, LP, and MM identified and harmonised the data and did all the analyses. KW reviewed the literature and ES, RHS, MJP, LP, MM, and KW planned the analyses. All authors interpreted results and contributed to drafting the paper.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Sippel S. ICPD beyond 2014: moving beyond missed opportunities and compromises in the fulfilment of sexual and reproductive health and rights. Glob Public Health. 2014;9:620–630. doi: 10.1080/17441692.2014.921828. [DOI] [PubMed] [Google Scholar]
- 2.United Nations Women Fourth World Conference on Women Platform for Action, Sec. C-91. New York, September 1995. https://www.un.org/womenwatch/daw/beijing/fwcwn.html (accessed Feb 19, 2020).
- 3.Haslegrave M. Sexual and reproductive health and rights in the Sustainable Development Goals and the post-2015 development agenda: less than a year to go. Reprod Health Matters. 2014;22:102–108. doi: 10.1016/S0968-8080(14)44812-2. [DOI] [PubMed] [Google Scholar]
- 4.Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012;380:165–171. doi: 10.1016/S0140-6736(12)60827-7. [DOI] [PubMed] [Google Scholar]
- 5.Goodkind D, Lollock L, Choi Y, McDevitt T, West L. The demographic impact and development benefits of meeting demand for family planning with modern contraceptive methods. Glob Health Action. 2018;11:1423861. doi: 10.1080/16549716.2018.1423861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations Population Fund International Conference on Population and Development (ICPD) https://www.unfpa.org/events/international-conference-population-and-development-icpd (accessed Feb 22, 2020).
- 7.Carr B, Gates MF, Mitchell A, Shah R. Giving women the power to plan their families. Lancet. 2012;380:80–82. doi: 10.1016/S0140-6736(12)60905-2. [DOI] [PubMed] [Google Scholar]
- 8.United Nations Population Division World contraceptive use 2019. 2019. https://www.un.org/en/development/desa/population/publications/dataset/contraception/wcu2019.asp (accessed Oct 15, 2019).
- 9.Bradley SEK, Croft TN, Fishel JD, Westoff CD. Revising unmet need for family planning. DHS Analytical Studies No. 25. ICF International; Calverton, MD: 2012. [Google Scholar]
- 10.Alkema L, Kantorova V, Menozzi C, Biddlecom A. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet. 2013;381:1642–1652. doi: 10.1016/S0140-6736(12)62204-1. [DOI] [PubMed] [Google Scholar]
- 11.Cleland J, Harbison S, Shah IH. Unmet need for contraception: issues and challenges. Stud Fam Plann. 2014;45:105–122. doi: 10.1111/j.1728-4465.2014.00380.x. [DOI] [PubMed] [Google Scholar]
- 12.Fabic MS, Choi Y, Bongaarts J. Meeting demand for family planning within a generation: the post-2015 agenda. Lancet. 2015;385:1928–1931. doi: 10.1016/S0140-6736(14)61055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cahill N, Sonneveldt E, Stover J. Modern contraceptive use, unmet need, and demand satisfied among women of reproductive age who are married or in a union in the focus countries of the Family Planning 2020 initiative: a systematic analysis using the Family Planning Estimation Tool. Lancet. 2018;391:870–882. doi: 10.1016/S0140-6736(17)33104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wellings K, Collumbien M, Slaymaker E. Sexual behaviour in context: a global perspective. Lancet. 2006;368:1706–1728. doi: 10.1016/S0140-6736(06)69479-8. [DOI] [PubMed] [Google Scholar]
- 15.The DHS Program, USAID Data. 2019. https://dhsprogram.com/Data/ (accessed Sept 18, 2019).
- 16.UNICEF Multiple indicator cluster surveys. 2019. https://mics.unicef.org/surveys (accessed Sept 18, 2019).
- 17.UK Data Archive Find data. https://www.data-archive.ac.uk/find (accessed Nov 25, 2019).
- 18.Inter-university Consortium for Political and Social Research Find & analyse data. https://www.icpsr.umich.edu/icpsrweb/ICPSR (accessed Sept 18, 2019). [DOI] [PMC free article] [PubMed]
- 19.DataFirst Our data services. https://www.datafirst.uct.ac.za/services (accessed Nov 25, 2019).
- 20.Human Sciences Research Council HSRC research data service. http://datacuration.hsrc.ac.za/ (accessed Sept 19, 2019).
- 21.GHDx Global Health Data Exchange. http://ghdx.healthdata.org (accessed Nov 25, 2019).
- 22.UN Human development data (1990–2017) http://hdr.undp.org/en/data (accessed Oct 17, 2019).
- 23.Lindberg L, Scott RH. Effect of ACASI on reporting of abortion and other pregnancy outcomes in the US National Survey of Family Growth. Stud Fam Plann. 2018;49:259–278. doi: 10.1111/sifp.12068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghaznavi C, Sakamoto H, Yoneoka D, Nomura S, Shibuya K, Ueda P. Trends in heterosexual inexperience among young adults in Japan: analysis of national surveys, 1987–2015. BMC Public Health. 2019;19:355. doi: 10.1186/s12889-019-6677-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barrense-Dias Y, Akré C, Berchtold A, Leeners B, Morselli D, Surís J-C. Sexual health and behavior of young people in Switzerland. Lausanne, I Institut universitaire de médecine sociale et préventive; 2018. (Raisons de santé 291). [DOI] [Google Scholar]
- 26.Darroch JE, Singh S. Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: an analysis of national surveys. Lancet. 2013;381:1756–1762. doi: 10.1016/S0140-6736(13)60597-8. [DOI] [PubMed] [Google Scholar]
- 27.Campbell M, Sahin-Hodoglugil NN, Potts M. Barriers to fertility regulation: a review of the literature. Stud Fam Plann. 2006;37:87–98. doi: 10.1111/j.1728-4465.2006.00088.x. [DOI] [PubMed] [Google Scholar]
- 28.Sedgh G, Hussain R. Reasons for contraceptive nonuse among women having unmet need for contraception in developing countries. Stud Fam Plann. 2014;45:151–169. doi: 10.1111/j.1728-4465.2014.00382.x. [DOI] [PubMed] [Google Scholar]
- 29.Williamson LM, Parkes A, Wight D, Petticrew M, Hart GJ. Limits to modern contraceptive use among young women in developing countries: a systematic review of qualitative research. Reprod Health. 2009;6:3. doi: 10.1186/1742-4755-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edietah EE, Njotang PN, Ajong AB, Essi MJ, Yakum MN, Mbu ER. Contraceptive use and determinants of unmet need for family planning; a cross sectional survey in the North West Region, Cameroon. BMC Womens Health. 2018;18:171. doi: 10.1186/s12905-018-0660-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taukobong HF, Kincaid MM, Levy JK. Does addressing gender inequalities and empowering women and girls improve health and development programme outcomes? Health Policy Plan. 2016;31:1492–1514. doi: 10.1093/heapol/czw074. [DOI] [PubMed] [Google Scholar]
- 32.Bongaarts J, Hardee K. The role of public-sector family planning programs in meeting the demand for contraception in sub-Saharan Africa. Int Perspect Sex Reprod Health. 2017;43:41–50. doi: 10.1363/43e3917. [DOI] [PubMed] [Google Scholar]
- 33.Stephenson R, Gonsalves L, Askew I, Say L. Detangling and detailing sexual health in the SDG era. Lancet. 2017;390:1014–1015. doi: 10.1016/S0140-6736(17)32294-8. [DOI] [PubMed] [Google Scholar]
- 34.Bergmann JN, Stockman JK. How does intimate partner violence affect condom and oral contraceptive use in the United States? A systematic review of the literature. Contraception. 2015;91:438–455. doi: 10.1016/j.contraception.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Emenike E, Lawoko S, Dalal K. Intimate partner violence and reproductive health of women in Kenya. Int Nurs Rev. 2008;55:97–102. doi: 10.1111/j.1466-7657.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- 36.Maxwell L, Devries K, Zionts D, Alhusen JL, Campbell J. Estimating the effect of intimate partner violence on women's use of contraception: a systematic review and meta-analysis. PLoS One. 2015;10:e0118234. doi: 10.1371/journal.pone.0118234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moore AM, Frohwirth L, Miller E. Male reproductive control of women who have experienced intimate partner violence in the United States. Soc Sci Med. 2010;70:1737–1744. doi: 10.1016/j.socscimed.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 38.Higgins JA, Smith NK. The sexual acceptability of contraception: reviewing the literature and building a new concept. J Sex Res. 2016;53:417–456. doi: 10.1080/00224499.2015.1134425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.John NA, Babalola S, Chipeta E. Sexual pleasure, partner dynamics and contraceptive use in Malawi. Int Perspect Sex Reprod Health. 2015;41:99–107. doi: 10.1363/4109915. [DOI] [PubMed] [Google Scholar]
- 40.Sanders JN, Higgins JA, Adkins DE, Stoddard GJ, Gawron LM, Turok DK. The impact of sexual satisfaction, functioning, and perceived contraceptive effects on sex life on IUD and implant continuation at 1 year. Womens Health Issues. 2018;28:401–407. doi: 10.1016/j.whi.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used in this paper have been shared with the authors and ownership, and access to, the data rests with the original producers.