Abstract
The Anatomical Society has developed a series of learning outcomes in consultation with dentists, dental educators and anatomists delivering anatomical content to undergraduate dental students. A modified Delphi methodology was adopted to select experts within the field that would recommend core anatomical content in undergraduate dental programmes throughout the UK. Utilising the extensive learning outcomes from two UK Dental Schools, and neuroanatomy learning outcomes that remained outside the Anatomical Society's Core Gross Anatomy Syllabus for Medical Students, a modified Delphi technique was utilised to develop dental anatomical learning outcomes relevant to dental graduates. The Delphi panel consisted of 62 individuals (n = 62) from a wide pool of educators associated with the majority of undergraduate dental schools in the UK, representing a broad spectrum of UK Higher Education Institutions. The output from this study was 147 anatomical learning outcomes deemed to be applicable to all dental undergraduate programmes in the UK. The new recommended core anatomy syllabus for dental undergraduates, grouped into body regions, offers a comprehensive anatomical framework with which to scaffold clinical practice. The syllabus, presented as a set of learning outcomes, may be used in a variety of pedagogic situations, including where anatomy teaching exists within an integrated dental curriculum (both horizontally in the basic sciences part of the curriculum and vertically within the clinical years).
Keywords: anatomy, Bachelor of Dental Surgery, curriculum, dentistry, learning outcomes, undergraduate education
The new recommended core anatomy syllabus for dental undergraduates offers a comprehensive anatomical framework with which to scaffold clinical practice. Presented as a set of 147 learning outcomes, the syllabus may be used in a variety of pedagogic situations, including where anatomy teaching exists within an integrated dental curriculum.

Introduction
As for all health professions, the role of the dentist is ever evolving and, consequently, dental education is also evolving. Recently, there have been numerous changes to dental education to reflect this, with an increasing push towards integrated curricula. Within the UK, upon completion of undergraduate dental education, Dental Foundation Training (DFT) is a mandatory 1‐year training programme based within primary dental care for all graduates who wish to practice dentistry within the UK's National Health Service (NHS; Coleman & Finn, 2019a,b). Upon successful completion of DFT, entry to the NHS Dental Performers List is permitted, and many dentists then go on to work independently as a general dental practitioner. Other dental graduates opt for a longer training period after qualification as full‐time trainees. On completion of 1‐year DFT, some graduates apply to 12 months (or longer) of Dental Core Training; the majority of these posts are based within secondary care. Furthermore, there are 2‐year integrated training programmes based within both primary care and secondary care for graduates wishing to pursue this route (Coleman & Finn, 2019a,b). In the context of this study, an appreciation of the different routes a recent graduate can pursue is necessary, as all must be equally prepared to practise and have the same solid grounding within gross anatomy; dentistry is essentially a surgical science (McHanwell, 2015; McHanwell & Matthan, in press).
Given the surgical nature of the role of the dental practitioner, human morphology including gross anatomy must provide a strong focus throughout a dental degree, and should be woven seamlessly both horizontally and vertically throughout (McHanwell, 2015; McHanwell & Matthan, in press). Dental students, within two years from the commencement of their course, will often undertake irreversible surgical procedures on patients (McHanwell, 2015; McHanwell & Matthan, in press). In this context, the need to ensure students are equipped with sufficient anatomy to become safe, and effective, practitioners is paramount. What then are the limits of anatomical knowledge needed for safe practice? Gross anatomy currently occupies centre stage within dental curricula, most often being taught within the early years of the programme and alongside other basic sciences (e.g., microbiology, physiology, nutrition, immunology and metabolism). Numerous anatomical topics are taught within dentistry, and there is an expectation that competence is gained across the spectrum of these topics, from foundational gross anatomy to neuroanatomy relating to jaw movements and pain pathways, pre‐ and postnatal developmental head and neck anatomy, and both basic and specialised histology relating to dentistry; these anatomical themes feed into dental curricula vertically, where a firm grasp of the fundamentals aid in comprehension of complex dental surgical areas (McHanwell, 2015; McHanwell & Matthan, in press).
McHarg & Kay (2008) assert that ‘the goal of all dental schools is to develop competent, knowledgeable dentists who have excellent communication skills and a sense of social responsibility’. However, the statement that a key objective of a dental degree is to develop dental surgeons cannot be dismissed (McHanwell, 2015; McHanwell & Matthan, in press). The course structure of dental programmes in the UK is variable, with an external steer towards an outcomes‐based educational model (Harden et al. 1999a; Harden 1999b), primarily in response to the requirement for institutions to blueprint their curricula to the national regulator, i.e., the General Dental Council (GDC), in order to achieve institutional accreditation. The current consensus across educators and curriculum developers of dental degrees indicates a central ‐ and pivotal ‐ role for gross anatomy to the dental practitioner (Guttmann, 2003; Guttmann et al. 2003; Bergman et al. 2008; Drake et al. 2009; Louw et al. 2009; Craig et al. 2010), although it is acknowledged that there remain challenges when tailoring teaching through learning outcomes (Bateman et al. 2018). It was thus the aim of this study to produce a recommended anatomy syllabus for dental graduates that could be used as a framework upon which institutions could scaffold their own degrees, both horizontally and vertically, with gross anatomical content deemed crucial for laying the foundations of safe practice.
While educators and curriculum developers appear to agree about the role of gross anatomy within dental curricula, regulatory body guidance is sparse on specific anatomical content that should be included, as evidenced by the GDC Preparing for Practice (PfP) document (General Dental Council, 2015) and, prior to that, the First 5 Years document (General Dental Council, 2008), both of which outline basic sciences content in broad and non‐specific terms. Within the UK and Europe, no detailed guidance on recommended anatomical content for dental courses exists. There are, however, recommended core syllabuses developed by the Anatomical Society for several other healthcare disciplines (Smith et al. 2016a,b; Finn et al. 2018; Connelly et al. 2018; Holland et al. 2019). This is not to say that there is any evidence of a diminishing role for anatomy within dental curricula. Indeed, its importance has been underscored by the Education Committee of the British Association of Oral and Maxillofacial Surgeons (Macluskey et al. 2012, 2016). The GDC's learning outcome 1.1.6 in the PfP document outlines that practitioners upon registration are able to ‘identify relevant and appropriate dental, oral, craniofacial and general anatomy and explain their application to patient management’ (General Dental Council, 2015); this must be relevant to the practice of dentistry and patient care. The core anatomy syllabus for dental graduates builds on this overarching outcome and is a framework at a more granular level with which course designers and dental educators can be guided to include anatomical content into their respective curricula. This is of particular importance with the increasing drive towards more outcomes‐based curricula. Consequently, the recommended core anatomical syllabus devised here can support learners and educators alike in understanding the content and end‐points they need to hone in to what is truly essential, and achievable, within their taught dental programmes.
Through the auspices of the Anatomical Society, we present here a recommended core anatomy syllabus for dental graduates that is presented systematically to facilitate mapping and blueprinting within individual higher education institution curricula.
Materials and methods
This study employed a modified Delphi approach, as described in the Anatomical Society's previously published syllabuses (Smith et al. 2016a,b; Finn et al. 2018; Connelly et al. 2018; Holland et al. 2019) and methodology paper (Smith et al. 2016a,b). The modified Delphi utilised existing learning outcomes as a starting point, rather than a blank page approach as per a traditional Delphi approach (Moxham et al. 2014). The study was conducted in four stages: (i) selection of currently used outcomes for review; (ii) Delphi Round 1; (iii) Delphi Round 2; and (iv) post‐Delphi final screening (Fig. 1). Ethical approval for this work was granted by the Hull York Medical School Ethics Committee (reference 17 08).
Figure 1.
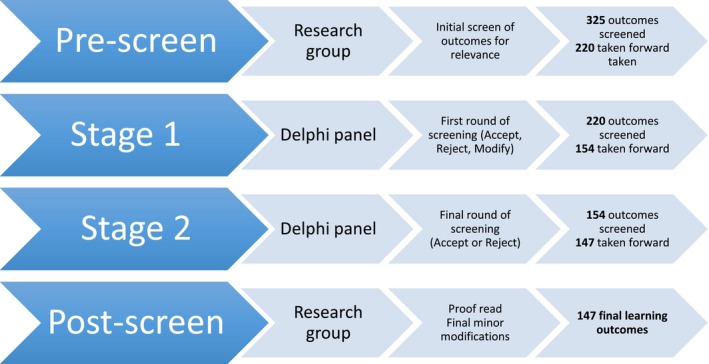
Key stages of the modified Delphi process for dental anatomy outcomes (adapted from Finn et al. 2018).
The research group
The research group, who coordinated the project, consisted of three of the contributing authors (GF, JM, MC). All authors have experience in teaching anatomy to undergraduate dental students, and GF, BM and SM have expertise in Delphi methodologies for developing anatomical syllabuses (McHanwell et al. 2007; Moxham et al. 2014; Smith et al. 2016a,b; Connelly et al. 2018; Finn et al. 2018; Holland et al. 2019). MC and BM have dental qualifications, and BM has written textbooks on head and neck anatomy for dentistry and is a member of the international committee dealing with anatomical and oroanatomical terminologies. SM has written a textbook on head and neck anatomy for speech students. SM and JM have written a chapter on teaching anatomy to undergraduate dental students.
Identification of the Delphi panel
The aim was to assemble a panel with expertise in embryology, anatomy, education and the clinical practice of dentistry. Potential panel members were identified from across UK Dental Schools. An invitation to participate in the study was circulated detailing the project and the three inclusion criteria. This stated the nominees must be one or more of the following: (i) a practising dental surgeon (either with, or without, a role in the teaching of dental undergraduates); (ii) an anatomist involved in teaching dental undergraduates; or (iii) an academic involved in either the teaching of, or organisation of, undergraduate dental curricula (i.e., a clinical lecturer or a professorial role). This resulted in a total of 33 panellists contributing to Round 1 and 62 panellists contributing to Round 2.
Stages of the Delphi study
Pre‐screening to select outcomes
The authors were unable to identify any pre‐existing published anatomy outcomes for dental undergraduate degrees in the UK. In order to gain an appreciation of current teaching, the anatomical outcomes were initially obtained from two UK institutions with established undergraduate dental programmes (139 outcomes were utilised in one institution and 131 in the second institution). In addition to this, outcomes relating to clinical anatomical correlations (in this paper termed Applied Anatomy) were obtained from one institution and neuroanatomy outcomes obtained from the Anatomical Society's Education Committee (McHanwell et al. 2007). The combination of the two curricula and the additional outcomes resulted in a total of 325 outcomes. Each outcome was then reviewed by the authors. This was to reduce duplication, to ensure consistent formatting, identify any gaps and ensure phrasing was in line with best practice (Kennedy et al. 2007; Holland et al. 2019). The pre‐screening of the combined outcomes resulted in 220 outcomes. The extensive work prior to the compilation of learning outcomes sent out to review by the Delphi panel was primarily to ensure that they were as accurate as possible in order to help maximise participation across as many institutions as possible. It was also thought that it would encourage participation with minimal effort from the panellists, in terms of stylistic and semantic modifications of individual learning outcomes.
Survey generation
All 220 outcomes were entered into Qualtrics survey software, version XM of Qualtrics, using the University of York account (Copyright © 2018 Qualtrics; Qualtrics, Provo, UT, USA). The survey was piloted to ensure accuracy and user‐friendliness. The survey began with instructions for completion, a statement of consent and contact information for the research team. Participants remained anonymous but were asked to complete basic demographic information including: (i) their institution; (ii) their principal role; (iii) whether or not their institution specifically teaches dentistry; and (iv) the manner by which anatomy for dentistry is taught at their institution. This information was recorded in order to describe the range of expertise within the panel.
Learning outcomes were presented in sections, each representing a concept (e.g., terminology) or region (e.g., nasal cavity). Each of the learning outcomes had a check‐box for the panellists to record his/her decisions at each of the two stages. Text boxes were also presented with each outcome to enable panel members to record their suggested modifications. Panellists could additionally record the reasons for their decisions or provide comments relating to the outcomes being reviewed within a free‐text box that followed each section. Prior to the survey becoming live, the data collection form was checked and piloted by the research team.
Setting consensus
Previous papers have contested the level at which consensus should be set for Delphi studies (Keeney et al. 2011). Figures within the literature range from 70% to 100% (Latif et al. 2016; Finn et al. 2018), with similar projects for different undergraduate programmes using 80% (McHanwell et al. 2007; Moxham et al. 2014; Smith et al. 2016a,b; Connelly et al. 2018; Finn et al. 2018; Holland et al. 2019). There are 16 institutions teaching dentistry in the UK, each using their own curricula. Consequently, considerable variability was predicted and, therefore, the consensus for this process was set at 80% (Finn et al. 2018; McBride & Drake, 2018).
Round 1 Delphi
Participants who had been identified as potential panellists were sent an e‐mail invitation to contribute to the project, an information sheet and a link to the online survey. The consent form was built into the survey and completion of the Delphi process was taken as implied consent. The Delphi survey was open for 8 weeks in order to maximise participation, with e‐mail reminders sent at 2, 4 and 6 weeks. Delphi panel members were asked to consider each learning outcome within the survey in terms of whether it should be regarded as: (i) acceptable (without modification); (ii) rejected; or (iii) accepted with modifications. Where modifications were proposed, panellists were able to provide their suggested modifications in the adjacent free‐text box or within the free‐text box at the end of each section. Indeed, in the free‐text boxes at the end of the section, panellists could propose additional learning outcomes for consideration. Thirty‐three panellists responded, providing 453 free‐text comments (Table 1).
Table 1.
Examples of panellists’ comments utilised to modify individual learning outcomes.
| Comment classification | Delphi Round 1 | Delphi Round 2 | ||
|---|---|---|---|---|
| n | Example(s) | n | Example(s) | |
| Supportive (S) | 3 | We cover this but could give it greater emphasis | 0 | |
| Contextual (C) | 140 | Some answers not relevant to dental or OMFS anatomy | 18 | Need to link this to common conditions |
| Modify (M) | 287 | Anatomical position of structures and their significance in understanding relationships between each other in the body | 18 | Describe the role of the neural crest, with emphasis on how this influences head and neck development (including oro‐dental structures) |
| Negative/not important (N) | 23 | I think we don't need to do brain as an undergraduate | 8 | This is poorly worded someone could − this knowledge as 'important'. It should be 'rationalise how the development ...' |
Analysis and decisions were undertaken using the protocol reported within existing anatomy syllabuses from the Anatomical Society (Smith et al. 2016a; Connelly et al. 2018; Finn et al. 2018; Holland et al. 2019). All submitted free‐text comments were reviewed and assigned to one of the following categories (Table 1): Supportive (S); Contextual (C); Modify (M); and Negative/not important (N). All learning outcomes achieving a consensus level of over 90% were accepted outright. Learning outcomes achieving a consensus level of between 81% and 90% were accepted, but modified if there were suggestions that might increase the level of agreement. All suggested modifications were reviewed using the rules developed by Smith et al. for the Core Anatomy Syllabus (Smith et al. 2016c), and discussed (following collation and anonymisation) among the research team (Table 2).
Table 2.
Rules developed by Smith et al. (2016c) for the core anatomy syllabus
| 1 | If all, or the majority of, comments suggest a particular change, then the learning outcome will be modified accordingly |
| 2 | If contradictory comments are being made, then discussion between the research team members will be used to decide which changes should be adopted and which rejected. The basis of these decisions should be to ensure clarity and to reduce repetition |
| 3 | In situations where one comment is felt by the research team to be especially apt, even if no other panel members’ comments match, then this single comment could be used to modify a learning outcome |
| 4 | Where a panel member makes a comment regarding inconsistency in terminology relating to a small number of learning outcomes, then the research team will discuss whether this inconsistency should be addressed across the whole syllabus and changes made |
| 5 | Anatomical terminology follows the guidelines laid out in Terminologia Anatomica (1998) |
| 6 | All decisions are recorded |
| 7 | These rules are applied, recognising that all changes will receive further scrutiny at Stage 3. Where any change results in lower levels of consensus being achieved, then the research team will restore the original learning outcome |
Round 2 Delphi
A second survey was created in Qualtrics, which consisted of the revised syllabus. This was circulated to the panellists as per Round 1. The survey was again active for 8 weeks, and e‐mail reminders were circulated after 2, 4 and 6 weeks (Fig. 1). Members were asked to review new learning outcome statements that had not yet reached consensus, and to either ‘accept’ these learning outcomes without modification or ‘reject’ outright. The learning outcomes that achieved consensus during Round 1 were included in the survey, so that panel members were reminded of their inclusion within the syllabus and to aid identification of potential gaps or duplication. However, no further input was sought regarding their inclusion (Smith et al. 2016c). Free‐text comments were still permissible for all learning outcome statements, and 44 comments were received (Table 1) from 62 panellists. Free‐text suggestions for minor amendments (other than accept/reject) considered at this stage included removal of any duplicate content, and correction of grammatical or typographical errors.
Post‐screen: final proofing post‐Delphi
The final step in this process was a review by the research group of the final list of learning outcome statements in order to ensure that no typographical or grammatical errors existed in the final draft.
Results
Panel demographics, anatomy curriculum breakdown
For Round 1, the Delphi panel was composed of 33 panellists (Table 3). These represented different stakeholders: dentists (27%); educators (24%); anatomists (15%); and maxillofacial specialists (9%) (24% other). For Round 2, the Delphi panel (sent out to the same distribution list) was composed of 62 panellists. The majority of the panellists for this round were dentists (48%). The remaining panellists were educators (19%), maxillofacial specialists (11%) and anatomists (5%) (16% other).
Table 3.
Demographics of the Delphi panel.
| Demographic data collected | Percent of panel | Number | Percent of panel | Number |
|---|---|---|---|---|
| Round 1 | Round 2 | |||
| Institution teaches anatomy as part of curriculum | ||||
| Yes | 87.88% | 29 | 88.71% | 55 |
| No | 12.12% | 4 | 11.29% | 7 |
| Total | 33 | 62 | ||
| Mode of anatomy teaching at institution | ||||
| Within an integrated (systems‐based) curriculum | 27.59% | 8 | 43.64% | 24 |
| As a stand‐alone course | 27.59% | 8 | 16.36% | 9 |
| A mixture of the above | 34.48% | 10 | 38.18% | 21 |
| Other (please specify) | 10.34% | 3 | 1.82% | 1 |
| Total | 29 | 55 | ||
| Specialty of panellist | ||||
| Dentist | 27.27% | 9 | 48.39% | 30 |
| Maxillofacial specialist | 9.09% | 3 | 11.29% | 7 |
| Anatomist | 15.15% | 5 | 4.84% | 3 |
| Educator | 24.24% | 8 | 19.35% | 12 |
| Other | 24.24% | 8 | 16.13% | 10 |
| Total | 33 | 62 | ||
Anatomy was taught in 88% (Round 1) and 89% (Round 2) of panellists’ institutions (Table 3). For 28% of the panellists’ institutions in Round 1, anatomy was taught either within a systems‐based curriculum (28%) or as a stand‐alone course (28%), or as a mix of the two (34%; Table 3). Ten percent of panellists in Round 1 put down Other as the mode of anatomy delivery at their institution. For panellists in Round 2, 44% delivered anatomy in a systems‐based delivery, and 38% delivered the subject as a mix of a systems‐based and stand‐alone curriculum. Sixteen percent of panellists in Round 2 came from institutions with stand‐alone anatomy courses, with 2% responding Other.
Core items identified in Round 1 of the Delphi process
The first stage of the two‐part Delphi process began with 220 learning outcomes. The acceptance threshold (panel consensus) was set at 80% by the research panel because of the wide variability in experience of the panellists and the wide variation in dental school curricula within the UK. The panel rejected 66 outcomes (equivalent to 30% of the original learning outcome list circulated to the panel). The highest number of outcomes rejected were related to the anatomy of the head and neck, where, of a total of 92 learning outcomes concerning the head and neck, 27 were rejected by the panel. This amounted to a 29% rejection rate. The greatest change in outcomes were for the ear (with a 75% rejection), the vertebral column (71% rejection), the upper limb (67% rejection), thoracic anatomy (54% rejection) and abdominal anatomy (40% rejection). Forty‐five learning outcomes in total were subsumed into other outcomes as a result of overlap noted by the panel. Eighty‐eight learning outcomes were accepted outright by the panel, and 66 outcomes were modified and went to Round 2 of the Delphi process for re‐review. Panellists were in agreement in only one area surveyed, namely basic anatomical terminology, where no learning outcomes were rejected.
Core items identified in Round 2 of the Delphi process
Round 2 of the Delphi panel listed all the learning outcomes, including those that had been accepted outright in Round 1. These were highlighted and included for completion sake to ensure that the panellists were able to form a full picture of the outcomes for re‐review, but with no opportunity offered of rejection or modification (Table 4). Round 2 thus included 154 outcomes, with 88 previously accepted. Of the 66 outcomes that were offered to the panellists for re‐review, 57 outcomes (86 percent) were accepted outright or with very minor textual changes (eight outcomes had minor changes suggested). Seven learning outcomes were rejected (one on the axial skeleton from the anatomical region relating to the vertebral column and one on development of foregut/midgut/hindgut). Two further outcomes were discussed by the research team, and modified and included into the final Delphi list with changes recommended by the panel. Some minor, and insightful, comments to the already accepted outcomes were suggested. These were discussed by the research team, and minor modifications to the wording were accepted. Some typographical errors that were previously unnoticed were corrected.
Table 4.
Anatomical regions and pattern of outcome change.
| Region | Delphi Round 1 | End of Delphi Round 1 | Difference | Delphi Round 2 | Final | Difference | Percentage difference from Delphi Round 1 |
|---|---|---|---|---|---|---|---|
| Anatomical terms | 8 | 8 | 0 (−) | 8 | 8 | 0 (−) | None |
| Embryology | 14 | 11 | −3 (−21%) | 11 | 10 | −1 (−9) | −29% |
| Neuroanatomy | 29 | 22 | −7 (−24%) | 22 | 17 | −5 (−23 %) | −41 % |
| Head and neck* | 92 | 65 | −27 (−29 %) | 65 | 65 | 0 (−) | −29 % |
| Ear* | 8 | 2 | −6 (−75 %) | 2 | 2 | 0 (−) | −75 % |
| Vertebral column* | 7 | 2 | −5 (−71 %) | 2 | 1 | −1 (−50%) | −85% |
| Thorax | 24 | 13 | −11 (−54%) | 13 | 13 | 0 (−) | −54% |
| Abdomen | 5 | 3 | −2 (−40%) | 3 | 3 | 0 (−) | −40% |
| Upper limb | 3 | 1 | −2 (−67%) | 1 | 1 | 0 (−) | −67% |
| Applied anatomy** | 30 | 27 | −3 (−10%) | 27 | 27 | 0 (−) | −10% |
| Total | 220 | 154 | −66 (−30) | 154 | 147 | −7 (−4.5%) | −33% |
Combined under head and neck in the final syllabus.
Collated from clinical applications spanning multiple body systems.
One‐hundred and forty‐seven (147) is the final number of learning outcomes accepted by the Delphi panel as being recommended/core. The percentage change from Round 1 stands at a 33% reduction of outcomes. Twenty percent of learning outcomes were subsumed into already existing outcomes. The final anatomical regions from the two rounds and research panel modifications are: (i) anatomical terms; (ii) embryology; (iii) neuroanatomy; (iv) head and neck; (v) ear; (vi) vertebral column; (vii) thorax; (viii) abdomen; (ix) upper limb; and (x) applied anatomy. As a result of there being low numbers of learning outcomes for the ear and vertebral column, they were subsumed in the final list within the Head and Neck section.
Discussion
Selection of outcomes, and exclusion and inclusion criteria
During pre‐screening, 325 learning outcomes were generated from the anatomy syllabuses of the curricula of two dental schools, neuroanatomical learning outcomes were included from a previous Delphi survey (McHanwell et al. 2007), and clinical correlations relating to dentistry as a surgical science were added by the authors. Histological and specialised oral biological outcomes were excluded from the list presented to the Delphi panel, based on agreement that they fell outside the remit of a syllabus targeting gross anatomy. The inclusion of clinical anatomical correlations within the survey was also discussed, and a consensus was reached not to highlight these in order to avoid steering the Delphi panel. This approach is in line with the approaches adopted by other core anatomical curriculum papers (Smith et al. 2016a; Connelly et al. 2018; Finn et al. 2018; Holland et al. 2019), where the principle has been to arrive at a consensus to be able to guide a range of curricula in the UK and beyond, many of which retain a clear demarcation between preclinical and clinical course content. To adopt an alternative approach and single out anatomy in the dental curriculum, by highlighting those learning outcomes with clinical correlations, would be inconsistent. This weighed heavily in the decision made by the panel to refrain from guiding the panel by highlighting those learning outcomes that contained clinical correlations, despite wide acknowledgement by the panel on the utility of clinical correlations in guiding teaching content. By arriving at a consensus for ‘core’ anatomical content, the panel aims to indicate what is particularly important for the dental course; clinical correlations for all of these core outcomes can be provided within individual course curricula to meet the needs of the curriculum design and course delivery method best suited to them. It was felt that to highlight the inclusion of clinical correlations for some learning outcomes and not for others, for example, by providing a clinical correlation relating to dental local anaesthesia but not one for procedures or conditions pertaining to the posterior triangle of the neck, there would be the possibility for misinterpretation by the readership, where the innervation of the teeth and the trigeminal nerve could be seen as core but the latter as not core. This level of steerage was felt to be inappropriate for a core syllabus intended to be utilised across a wide variety of dental curricula, and it was not within the scope of this paper to advise dental schools on recommended pedagogic methods to deliver core anatomical content.
From the initial 325 learning outcomes, 220 outcomes were provided for scrutiny by the expert Delphi panel. After two rounds of consideration by the panellists, the final list of learning outcomes comprised 147 outcomes, indicating an overall 33% reduction in the initial list of learning outcomes. The panel accepted 70% of outcomes outright in Round 1, and 86% in Round 2. Learning outcomes that received strong acceptance in Round 1 tended to be those related to the day‐to‐day clinical practice of dentistry, including osteology and the course of pertinent nerves, the trigeminal and facial nerves. The outcome ‘Describe the craniofacial skeleton, including the mandible, and the bones which make up the skull’, for instance, received 100% acceptance in Round 1 and remained unchanged throughout the process. As mentioned previously, neurological learning outcomes were those obtained during the collation of the anatomy syllabus for medical undergraduates and added to the final list of outcomes submitted for the opinion of the Delphi panel. Five of the seven outcomes rejected outright in Round 2 were related to neuroanatomy, perhaps because the outcomes were considered to be too specific for undergraduate dental teaching or because there is a trend towards focussing on clinically relevant anatomy to the general dental practitioner. Table 4 highlights where there were significant rejections in learning outcomes.
Analysis of the final list of learning outcomes revealed that, of the 30 anatomy outcomes presented to the panel that contained clinical correlations, only three were rejected. This represents merely a 10% reduction of these outcomes, the lowest reduction in outcomes overall. Consequently, these outcomes are presented as a separate section in the final syllabus (‘Applied Anatomy’) as the majority probably relate to material taught in the later stages of the dental curriculum. Clinical learning outcomes, or outcomes where there was clarification of the clinical relevance, appeared to be favoured, despite the decision by the research panel not to steer the Delphi panellists, and it is noteworthy that, during the compilation process in pre‐screening, most of these anatomical outcomes were taken from modules taught in the third year of the dental course.
Panel membership, demographics and research panel membership
A previous criticism of the modified Delphi methodology in compiling anatomical syllabuses has been that the learning outcomes are generated by a relatively small group of anatomists, only some of whom were clinically qualified (Smith et al. 2016a). To counter this, and also to ensure the panel had representation from multiple expert stakeholders with an interest in anatomical knowledge in dentistry, a wide group of dental educators was invited to partake in the Delphi panel. The panel was larger for Round 2, although the same panellist distribution list was contacted. The increase in numbers of panellists is perhaps a reflection of the ease of reviewing outcomes that are more relevant/familiar and for which a large proportion have already been accepted (although panellists still commented on several of them). This high level of engagement within the dental community might reflect the eagerness of dental educators to be involved in the process as, in contrast, a review of other Delphi syllabuses reveals a trend of attrition in Round 2 of the process.
Themes and pattern of rejection
Analysis of the rejected learning outcomes shows a shift towards minimal teaching of the upper limb, abdominal and thoracic anatomy outcomes within the syllabus. Medical and dental students have, on occasions, been taught anatomy with the same learning outcomes. It is instructive therefore to compare learning outcomes for these two healthcare professions. A comparison with the Anatomical Society's core syllabus for medical undergraduates (Smith et al. 2016a) reveals a striking reduction of outcomes for the dental syllabus in all regions apart from the head and neck (and the embryology and applied anatomical outcomes which relate directly to head and neck anatomy). This finding might be related to time constraints within the dental curriculum. Indeed, all but one learning outcome relating to the vertebral column (and that also considerably modified by the panel) was rejected in the final list (Table 4). A reduction of 85% of outcomes relating to the axial skeleton, even after modification, highlights the point that the basic framework of the human body is not necessarily considered particularly relevant to dentistry, the focus according to the Delphi panellists being on the head and neck. Even within the head and neck anatomy region, a 75% reduction of learning outcomes occurred for the anatomy relating to the ear. Other regions with considerable rejection of learning outcomes were the upper limb (67% reduction of outcomes), thorax (54% reduction), neuroanatomy (41% reduction) and abdomen (40% reduction).
The initial list did not have many learning outcomes relating to radiology. Furthermore, panellists showed a propensity to reject radiology and imaging outcomes, as these were deemed to not be within the remit of gross anatomy. Radiology is usually studied as a separate specialised dental discipline. Consequently, there is little radiology taught within the gross anatomy component of dental programmes. It has been suggested that students struggle conceptually when interpreting two‐dimensional radiographic images in terms of three‐dimensional anatomy, and therefore it may be advantageous to study radiology alongside gross anatomy (McHanwell, 2015; McHanwell & Matthan, in press). Moreover, the GDC stance on radiology teaching and interpretation of images is limited, although all‐encompassing, outcome 1.2.4 of PfP stating that dentists, as part of a comprehensive patient assessment, must be able to ‘undertake relevant special investigations and diagnostic procedures, including radiography’ (General Dental Council, 2015). We therefore are of the opinion that, even though few outcomes refer to radiological anatomy in the present syllabus, this should be further reviewed as we examine the impact of this recommended (core) syllabus for anatomy within dentistry in a subsequent study.
We also have some issues relating to the lack of inclusion of some neuroanatomy learning outcomes. It appears that neuroanatomy was a challenging area in which to reach consensus. This was evidenced in both Rounds 1 and 2, where neuroanatomy outcomes were heavily pruned. This occurred despite some neuroanatomy outcomes (e.g., trigeminal pathways) being related directly to the face and dentition. Moreover, neuroanatomy has been identified as a key area for understanding pain and control of jaw movements. It also has significance for understanding other somatic sensations, as well as for the central connections of the cranial nerves and the relationships of the brain to the internal cranium (McHanwell, 2015; McHanwell & Matthan, in press).
Many embryological learning outcomes were rejected by the panel. These are outcomes that the research panel were reluctant to discard, as head and neck anatomy is more readily understood by students if the embryological trends (e.g., the development of pharyngeal arches) are known (McHanwell, 2015; McHanwell & Matthan, in press). The advantages potentially gained by teaching embryology alongside relevant gross anatomy may thus be numerous, although it has been suggested that it may be best taught as part of a craniofacial development course to allow the learner to make appropriate clinical linkages (McHanwell, 2015; McHanwell & Matthan, in press).
It should be recognised that core syllabuses are also being devised by the International Federation of Associations of Anatomists (IFAA; Tubbs et al. 2014; Moxham et al. 2015, 2018; Tubbs & Paulk, 2015; Fakoya et al. 2017; Webb et al. 2019). These do not use learning outcomes but, rather, are presented as lists of topics. Both the Anatomical Society's and IFAA's approaches have advantages and disadvantages but, as more of the syllabuses appear, it will be instructive to compare them in order to see where similarities and differences exist. Once these different curricula are completed, it would be possible to reconcile the perceived differences on the basis of having clear indications about what topics and learning outcomes are universally considered core, in order to recommend suitable clinical correlations for all learning outcomes that may be utilised to steer foundational anatomy content. The panel recognises the challenges involved in this decision‐making process and that this could only be satisfactorily accomplished in the clinical context if the clinicians teaching on dental courses were actively involved in establishing suitable clinical correlations, including advising where in the 4‐ and 5‐year dental courses such clinical cases are best considered by the students.
Presently, the use of learning outcomes may appear more conducive to some educators for the development of dental courses. One finding from the present project that came as a surprise was that over 10 percent of panellists claimed that their dental courses did not teach anatomy. Whether this relates to anatomy being ‘hidden’ within the curriculum is unknown. As suggested by McHanwell (2015) and McHanwell & Matthan (in press), dentistry is a surgical profession and it seems to us that, consequently, anatomy is an essential component of a dental course. It is hoped that this recommended syllabus will encourage those dental schools that look carefully at the mission of their education and training to comply with the core material identified in this survey.
This recommended core syllabus, as for other syllabuses devised by the Anatomical Society and the IFAA, provides the minimum level of knowledge expected of a recently qualified graduate in dentistry in order to carry out clinical procedures safely and effectively. In applying the term core to this syllabus, the authors are mindful of the need to define what the term core should be taken to mean in this context. At one level, it could be taken to mean a syllabus that students would be expected to demonstrate mastery of virtually in its entirety. In turn, this would imply any assessment based upon this syllabus and taken by students might require a pass mark to be set at 85% or higher. The authors consider this unrealistic. Instead, the authors take the term core in this context to mean content that a student might be expected to master over the length of an undergraduate programme perhaps with the content reviewed, revisited and elaborated on at the later stages of a course, depending on the structure of that course as outlined below. In this guise, a core syllabus is very much an educator‐facing, rather than a learning‐facing, document. Indeed, depending on the course philosophy and objectives, it would be expected that some material would be taught beyond core. It can be argued that a university education requires that, in some areas, students should be brought to the frontiers of knowledge. The aim of developing core syllabuses is therefore to set standards, not impose them. Furthermore, the core syllabus does not dictate how or when the syllabus is delivered. Thus, it remains appropriate and relevant to stand‐alone anatomy courses, integrated courses and spiral courses where anatomy is taught at various stages throughout dental education and training. Indeed, course and curriculum developers are cautioned that this core syllabus requires implementation with due consideration to other elements of the basic sciences components within the early years of a dental degree, as well as in consideration with clinical aspects of the curriculum in the later years; an isolated core anatomy syllabus is meaningless in the context of a dental degree with its strong surgical focus. Thus, there is no one‐size‐fits‐all solution on the question of this anatomy syllabus; varying stakeholder perspectives have influenced the final list of learning outcomes. Rather than attempting to deliver anatomy education purely to the list of outcomes generated by the expert panel, the core syllabus must be considered as guidance for course and curriculum developers within institutions of the key anatomical content requiring consideration and implementation within the dental degree to supplement the overarching anatomical ambitions articulated by national regulatory bodies. Finally, the anatomy syllabus relevant to dentistry listed here cannot be considered an exhaustive list of the anatomy required over the course of a career within the profession, and dental practitioners will continue to be required to acquire knowledge in their postgraduate careers. This postgraduate knowledge will, however, hinge on the foundational undergraduate knowledge presented here, despite its speciality‐dependent nature.
Limitations
One potential limitation is that the panel was not homogeneous for both rounds, which means views may not be consistent. The panel was also large; this can be both a strength and a limitation. Larger panels mean more institutions are represented but, the more panel members, the less likely consensus will be achieved. However, the diversity of the panel ensured a wide range of comments from which the research panel was able to glean insights. When the panel was largely in agreement, the outcomes were likely to be those that were valued across the specialisms and disciplines, spanning preclinical educators as well as clinicians.
Sampling to construct the panel is often a limitation with Delphi studies. While all institutions were not represented, the researchers used a purposive sampling strategy with participant snowballing. It should also be acknowledged that the panellists were all from schools in the UK delivering undergraduate dentistry courses. However, we have no reason to believe that dental education in the UK is significantly different from other countries with an established tradition of dental education.
The Anatomical Society core anatomy syllabus for undergraduate dentistry
The Anatomical Society and the expert Delphi panel of anatomy and dental educators recommend that the following learning outcomes should be achieved by all students upon graduation, to demonstrate a basic level of competence in anatomy.
Anatomical Terms
Overview
Dental graduates require anatomical terminology to effectively communicate with their colleagues. General anatomical terminology is a prerequisite for learning anatomy and the foundation on which further anatomy knowledge is built on.
-
1
Describe the anatomical position and its significance in understanding relationships between structures in the body.
-
2
Define the basic anatomical terms medial, median, lateral, proximal, distal, superior, inferior, deep, superficial, anterior/ventral, posterior/dorsal, cephalic/cranial, rostral, caudal.
-
3
Describe the basic anatomical planes axial/transverse/horizontal, sagittal and coronal.
-
4
Define the basic terms used to describe movement: protraction, retraction, elevation, depression, flexion, extension, lateral flexion, pronation, supination, abduction, adduction, medial and lateral rotation.
-
5
Describe and contrast different types of joints (synovial, fibrous and cartilaginous) and their associated structures (cartilage, tendons, ligaments, bursa) in relation to movement, stability and function, with a specific focus on the head and neck region.
-
6
Explain why knowledge of a muscle's attachments, innervation and blood supply is important in understanding its functions.
-
7
Describe the organisation of the vascular system of the body. Name and describe the function of the major arteries, veins and lymph vessels of the body.
-
8
Identify and describe the main regions of the head and neck.
Embryology
Overview
Dental graduates should have a grounding in head and neck embryology relating to developmental disorders of the craniofacial region.
-
9
Describe early embryogenesis (fertilisation to the establishment of the three germ layers). Explain the cellular derivatives of the three germ layers.
-
10
Describe the process of neurulation and the development of the neural crest, with emphasis on how this influences head and neck development (including oro‐dental structures).
-
11
Describe prenatal and postnatal (up to the last growth spurt) skull and craniofacial bone development, including the skull base. Explain the development of the mandible and temporomandibular joint.
-
12
Define the component parts of the skull and explain its corresponding embryological origin.
-
13
Describe and explain the formation of the pharyngeal arches and pharyngeal pouches.
-
14
List the derivatives of the pharyngeal arches and pouches, and the branchial clefts. Explain the relationships between their embryonic structures and adult derivatives.
-
15
Describe prenatal development of the face, palate, mandible, oral cavity and tongue. Describe their postnatal function.
-
16
Describe tooth development (crown, roots, enamel, dentine, pulp; including dentinogenesis, amelogenesis).
-
17
Describe the development and structure of dental tissues and tooth attachment tissues (cementum, periodontal ligament, alveolar bone, gingiva and oral mucosa).
-
18
Describe the effects of ageing on oro‐dental structures.
-
19
Explain the embryological development of the tongue and the thyroid gland, and list the clinical consequences of developmental anomalies.
Neuroanatomy
Overview
Dental graduates require a grounding in neuroanatomy, particularly with regard to the pathways involved in pain and paraesthesia.
-
20
Define the different categories of nervous system: central, peripheral, autonomic, sympathetic and parasympathetic.
-
21
Describe the structural features of spinal nerves and cranial nerves. Compare their main structural and functional differences.
-
22
Describe and compare the structure and organisation of the somatic and autonomic nervous systems.
-
23
Define the characteristics of a reflex. Explain the mechanism of a basic reflex circuit.
-
24
Define the terms grey and white matter, fasciculus, tract, commissure, pathway, chiasm, decussation, nucleus, ganglion and cortex.
-
25
Identify the major functional features and divisions of the brain.
-
26
Describe the areas of cerebral cortex subserving major special functions: motor, sensory, visual, auditory, memory and emotion, and decision‐making and social behaviour. Explain the manifestations of related disorders.
-
27
Summarise the position of the corpus callosum and ascending and descending tracts, with particular emphasis on the trigeminal sensory system.
-
28
Describe the blood supply to the brain and explain the functional deficits occurring after ‘stroke’ involving individual cerebral arteries.
-
29
Describe the origins, courses and functions of the cranial nerves.
-
30
Describe the neural pathways subserving the special senses.
-
31
Describe the anatomy and major functions (endocrine, autonomic) of the hypothalamus and pituitary gland. Explain the manifestations of related disorders.
-
32
Discuss the position and major functions of the ascending aminergic systems (noradrenaline, dopamine and serotonin) and cholinergic systems.
-
33
Explain the anatomical basis of cranial nerve assessment.
-
34
Identify the major features of the brain on coronal, axial and sagittal sections on computed tomography images.
-
35
Describe the course that each cranial nerve takes from its intracranial origin to the foramina by which it enters or leaves the skull.
-
36
Explain the mechanisms that exist to protect the brain from mechanical injury.
Head and neck
Overview
Dental graduates require a sound grounding in all aspects of head and neck anatomy. They should be able to describe structures and relationships, including the innervation and blood supply of areas relating to: (i) the skull, mandible and teeth; (ii) the face and facial skeleton; (iii) the temporomandibular joint; infratemporal fossa and pterygomandibular fossa; (iv) the nasal cavity; (v) the oral cavity; (vi) the ear; (vii) the orbital cavity; (viii) the neck structures; and (ix) the structures relating to the larynx, pharynx and soft palate. They should be able to demonstrate the position of the palpable and imaging landmarks of the major bones of the skull as well as the key clinically relevant landmarks in the neck that form the foundation of being able to perform a clinical examination of the neck.
-
37
Identify the basic anatomical and structural features of the skull (internal and external).
-
38
Identify the individual bones of the skull. Describe the main features of the individual bones of the skull.
-
39
Describe the craniofacial skeleton, including the mandible, and the bones that make up the skull.
-
40
Describe the boundaries of the three cranial fossae within the skull. Identify their main component parts, foramina and contents.
-
41
Describe the course of cranial nerves exiting from the interior of the skull into the head and neck region.
-
42
List the major arteries supplying the interior of the cranium and the brain.
-
43
Describe the osteology and function of the mandible, and identify its osteological features.
-
44
Describe the innervation of the maxillary and mandibular teeth, and their supporting structures.
-
45
Describe the anatomical basis of common variations in sensory innervation of the teeth.
-
46
Describe the anatomical features of the periodontal ligament and the gingiva, and their relationships of the individual teeth.
-
47
Describe the relationships of the mandible and maxilla to surrounding structures.
-
48
Describe the main bony features of the craniofacial skeleton.
-
49
Describe and identify the major foramina of the craniofacial skeleton. List the structures passing through them.
-
50
Describe the organisation and function of the muscles of facial expression, and their main attachments.
-
51
Describe the main branches of the facial nerve. Explain the causes and clinical consequences of damage to these nerves.
-
52
List the main divisions of the trigeminal nerve. Explain the pattern of sensory innervation of the face and the clinical significance relating to this pattern of distribution.
-
53
Explain the significance of the motor and sensory innervation within the face, and its relevance to dental anaesthesia.
-
54
Describe the organisation of the blood supply to the face and scalp. Explain the importance of knowledge of retrograde venous flow and the clinical consequences of connections between the facial drainage system and those within the skull.
-
55
Describe the anatomy, function and innervation of parotid gland. Explain its clinical significance.
-
56
Describe the major venous drainage systems from the interior of the cranium.
-
57
Describe the anatomy of the temporomandibular joint, including its ligaments, capsule and articular disc. Explain movement at the temporomandibular joint. Explain how the translation and hinge movements in the two compartments of the joint enable mandibular elevation and depression.
-
58
Describe the attachments, actions and innervations of the muscles involved in mastication. List their attachments and their actions on the mandible and their innervation.
-
59
Explain the sequence of actions of the muscles of mastication during a chewing cycle.
-
60
Describe the infratemporal fossa and its contents. Define the boundaries of the infratemporal fossa and its osteology.
-
61
Describe the main branches of the maxillary artery. List the major structures they supply.
-
62
Describe the major branches of the mandibular division of the trigeminal nerve. List the structures they innervate, in particular with relation to dental anaesthesia.
-
63
Describe the major branches of the maxillary division of the trigeminal nerve. Define their functions with regard to dental anaesthesia.
-
64
Describe the parasympathetic autonomic ganglia of the head and their functions, with particular relevance to dental practice.
-
65
Describe the pterygopalatine fossa and list its contents.
-
66
Describe the bones of the nasal cavity, in particular the major features of the lateral wall and septum. List its main nerve and blood supply.
-
67
Describe the anatomy of the paranasal sinuses. Identify the drainage points of the paranasal air sinuses within the nasal cavity. Explain the clinical consequences of their location, in particular that of the maxillary sinus.
-
68
Describe the autonomic nervous supply relevant to the nose with regard to dentistry.
-
69
Identify the structures of the paranasal sinuses on plain radiograph film.
-
70
Describe the anatomy of the oral cavity. Define its boundaries and identify the main anatomical features.
-
71
Describe the functional anatomy of the tongue. Describe its muscles, and sensory and motor innervation.
-
72
Describe the course and distribution of the hypoglossal nerve.
-
73
Describe the anatomy of the palate. Explain the clinical consequences of embryological developmental anomalies.
-
74
Define the boundaries and contents of the submandibular region. Define the anatomical relationships of the structures within it.
-
75
Describe the contents of the floor of the mouth. Define the anatomical relationships of these structures.
-
76
Describe the relationships of structures entering or exiting the floor of the mouth, particularly in relation to the hyoglossus muscle.
-
77
Describe the submandibular and sublingual salivary glands, and explain their function.
-
78
List the sensory innervation of the teeth and supporting structures. Explain the relevant nerve blocks for surgical intervention on a tooth.
-
79
List the three parts of the ear and structures located within each part (including the ossicles), and explain its links to the nasopharynx, and functions in relation to the transmission of sound.
-
80
Describe the course and functions of the facial nerve and its branches in the petrous part of the temporal bone. Explain the clinical consequences of damage to the facial nerve in its intrapetrous course.
-
81
Describe the boundaries of the orbit and the associated osteology of the orbital cavity. List the openings in the orbit and the structures travelling through them.
-
82
Describe the extraocular muscles. Explain their function.
-
83
Describe the courses of nerves within the orbit. Explain the clinical consequences of injury to these nerves.
-
84
Describe the course, branches and functions of the ophthalmic division of the trigeminal nerve.
-
85
Describe the structure of the eyeball. List the structures that support the eyeball within the orbit.
-
86
Describe the basic anatomical organisation of the neck with regard to its boundaries and functional compartments. Explain the clinical anatomy of the neck in relation to its clinical examination.
-
87
Describe the organisation of the main fascial compartments of the neck. List the functions of fascia.
-
88
Identify and describe the course of the anterior and external jugular veins in the neck.
-
89
Identify and describe the main features of the cervical spine, cervical vertebrae and first rib.
-
90
Describe the contents of the anterior and posterior triangles, and define their boundaries.
-
91
Describe the anatomy of the thyroid gland (and associated structures) and its clinical significance.
-
92
Identify the structures in the root of the neck (thoracocervical region), at the thoracic inlet.
-
93
Describe the structures within the carotid sheath.
-
94
Describe the organisation of the lymphatic drainage of the head and neck, with an emphasis on the deep cervical chain.
-
95
Describe the tissue spaces anatomically connected to the upper and lower jaws.
-
96
Define the relationships between the neck and adjacent regions in the head, neck and thorax, with particular reference to the spread of infection.
-
97
Describe the osteology of the hard palate.
-
98
Describe the relationships of the soft palate. List the attachments, actions and innervation of the muscles of the soft palate.
-
99
Describe the clinical anatomy of the pharynx. Identify the anatomical features of the pharynx (including the musculature and innervation of the pharyngeal wall), and its division into the nasopharynx, oropharynx and laryngopharynx.
-
100
Describe the anatomy of the interior of the pharynx. Explain the functions of the pharynx and soft palate in swallowing and speech.
-
101
Describe the main anatomical features of the larynx, including its skeletal and cartilaginous framework, musculature, sensory and motor nerve supply, and mucosal lining. Explain its functional anatomy.
-
102
Describe the relationship of the thyroid gland to the larynx and pharynx. Explain the course of the recurrent laryngeal nerve, and its clinical significance in laryngeal dysfunction.
-
103
Describe the general organisation of the muscles on the posterior aspect of the neck.
Thorax
Overview
Dental graduates should be familiar with the bony arrangement of the thoracic cavity, the clavicle, sternum and ribs. They should be able to appreciate the divisions and contents of the mediastinum. They should be familiar with the anatomy of the respiratory and cardiovascular system in the thorax (heart, lungs and great vessels) and the structure of the diaphragm.
-
104
Describe the basic functional anatomy of the thorax and respiratory system. Identify the bony features and major surface landmarks of the chest wall.
-
105
Describe the main anatomical features of the trachea and lungs, including an understanding of the locations associated with inhaled foreign bodies.
-
106
Explain the movements of the diaphragm. List the muscles involved in normal, vigorous and forced ventilation.
-
107
Describe the major divisions of the mediastinum with regard to the spread of oro‐facial infection.
-
108
List the main component parts of the bronchial tree and the bronchopulmonary segments. Explain their functional and clinical significance.
-
109
Describe the coronary circulation.
-
110
Identify the major anatomical features of each chamber of the heart and explain their functional significance.
-
111
Describe the structure and position of the atrioventricular, pulmonary and aortic valves, and their function in the prevention of reflux of blood during the cardiac cycle.
-
112
Describe the anatomical course of the spread of electrical excitation through the chambers of the heart.
-
113
Describe the course of the ascending aorta, the arch of the aorta and the descending thoracic aorta. Name their major branches and the structures they supply.
-
114
Identify the brachiocephalic veins, inferior and superior venae cavae, and the azygos venous system.
-
115
Describe the origin, course and distribution of the vagus and phrenic nerves, with special consideration to clinical manifestations of head and neck pathology.
-
116
Describe the course and location of the oesophagus in the cervical and thoracic regions.
Upper limb
Overview
Dental graduates should be able to provide an overview of the general organisation of the upper limb, and have a working knowledge of the origin and course of the nerves innervating the structures therein as well as of the vasculature relevant to procedures.
-
117
Provide a general account of the organisation of structures in the upper limb, with emphasis on the vasculature and how it relates to venepuncture and measurement of blood pressure.
Abdomen
Overview
Dental graduates should understand the general organisation of the abdominal wall, and the abdomen and its contents, and their relationships with the other systems of the body. They should be familiar with the anatomy of the gastrointestinal tract in the abdomen (stomach, duodenum, jejunum, ileum, caecum and colon) and the hepatobiliary system (liver, gallbladder), endocrine system (suprarenal glands and the endocrine components of the pancreas), and the urinary system (kidneys and ureters) and haematopoietic organs (spleen).
-
118
Describe the general organisation of the digestive system.
-
119
Describe the position and functional anatomy of the stomach, duodenum, jejunum, ileum, caecum, ascending, transverse and descending colon, sigmoid colon and rectum.
-
120
Identify the liver, gallbladder, pancreas, spleen, kidneys, stomach, duodenum, jejunum, ileum. Explain their key relations to other abdominal organs.
Applied anatomy
Overview
Dental graduates require targeted applied clinical anatomy relating to structures associated with common or emergency procedures. They should be able to describe the underlying anatomy relating to procedures and clinical investigations.
-
121
Describe the clinically relevant anatomy of the nose and paranasal sinuses, in particular with regard to epistaxis, maxillary and nasal fractures, and spread of odontogenic infection.
-
122
Describe the applied anatomy associated with disorders of the temporomandibular joint and their implications for clinical dental practice.
-
123
Explain the clinical significance of the muscles of facial expression in relation to clinical dentistry, in particular with regard to spread of infection and prosthetics.
-
124
Describe the clinical anatomy relevant to performing an inferior alveolar nerve block. Explain the anatomical basis of the more common techniques of dental anaesthesia.
-
125
Explain the clinical significance of hard and soft palate features relevant to dentistry.
-
126
Describe fractures of the mandible and how, depending on the fracture line, muscles attached to the mandible can either displace or bring together bony fragments.
-
127
Describe the routes by which infections may spread from teeth to adjacent structures.
-
128
Describe the consequences of fracture of the zygomatic complex in terms of the surrounding anatomical structures, including the maxillary air sinus.
-
129
Describe the anatomy of the skull in terms of the Le Fort classification for facial fractures.
-
130
Describe anatomically how an object hitting the region of the eye can result in 'blowout' fracture of the orbit. Explain the consequences of fractures around the orbit.
-
131
Describe how development of the face, palate, neck and thyroid gland can explain the appearance of a variety of cysts around the lower mouth, face and neck regions.
-
132
Describe the anatomical features that should be taken into consideration in an emergency airway situation.
-
133
Outline the possible anatomical reasons for a patient suffering from dysphagia.
-
134
Outline the effects and reasons for a patient developing facial palsy.
-
135
Describe the possible routes by which infection can spread intracranially from infected sites in the face and from within the infratemporal fossa.
-
136
Describe anatomically and neurologically the condition of trigeminal neuralgia.
-
137
Locate where on the head and neck arterial pulses may be discerned.
-
138
Describe both anatomically and neurologically how ptosis (drooping of the upper eyelid) can occur.
-
139
Describe the attachment of muscles and fascia to the mandible and hyoid bone that is associated with Ludwig's angina.
-
140
Describe the anatomy of the region around the mandibular third molar in terms of possible damage that can result during the tooth's surgical extraction.
-
141
Describe the anatomical structures that can be involved in trismus (difficulty in opening the lower jaw).
-
142
Describe the neurological basis for fainting.
-
143
Describe how patterns of lymphatic spread helps understand the spread of infection and metastasis of cancers.
-
144
Describe the routes of intracerebral spread of infection from the face and explain the significance of this to clinical dentistry.
-
145
Describe the main types of skull and mandibular fractures, and explain their functional and clinical consequences.
-
146
Explain the significance of lymphatic drainage with regard to metastatic spread of carcinoma of the head and neck.
-
147
Explain the role of the tissue spaces within the upper and lower jaws in the spread of infection in the head and neck.
Author contributions
All authors were responsible for contributions to concept, design, critical revision and approval of the manuscript. JM, GF and MC were responsible for acquisition of data, data analysis and data interpretation. GF also obtained ethical approval for the study.
Acknowledgements
This project was undertaken and supported by the Anatomical Society. The authors wish to express their gratitude to everyone involved, primarily to the dentists, educators, anatomists, maxillofacial specialists and any others who gave their time to participate in the Delphi panel. The authors also wish to thank the dental schools across the UK that participated in this exercise. The authors gratefully acknowledge Dr Hannah Shaw's contribution in the sharing of dental anatomy learning outcomes utilised at her institution.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- Bateman HL, McCracken GI, Thomason JM, et al. (2018) Learning outcomes: exploring implications of adopting a different level of detail. Eur J Dent Educ 22, 86–91. [DOI] [PubMed] [Google Scholar]
- Bergman EM, Prince KJ, Drukker J, et al. (2008) How much anatomy is enough? Anat Sci Ed 1, 184–188. [DOI] [PubMed] [Google Scholar]
- Coleman A, Finn GM (2019a) Post qualification dental training. Part 1: perceptions of different dental foundation & dental core training pathways. Br Dent J 227, 915–921. [DOI] [PubMed] [Google Scholar]
- Coleman A, Finn G (2019b) Post‐qualification dental training. Part 2: is there value of training within different clinical settings? Br Dent J 227, 989–995. [DOI] [PubMed] [Google Scholar]
- Connelly SA, Gillingwater TH, Chandler C, et al. (2018) The anatomical society's core anatomy syllabus for undergraduate nursing. J Anat 232, 721–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig S, Tait N, Boers D, et al. (2010) Review of anatomy education in Australian and New Zealand medical schools. ANZ J Surg 80, 212–216. [DOI] [PubMed] [Google Scholar]
- Drake RL, McBride JM, Lachman N, et al. (2009) Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ 2, 253–259. [DOI] [PubMed] [Google Scholar]
- Fakoya FA, Emmanouil‐Nikoloussi E, Sharma D, et al. (2017) A core syllabus for the teaching of embryology and teratology to medical students. Clin Anat 30, 159–167. [DOI] [PubMed] [Google Scholar]
- Finn GM, Hitch G, Apampa B, et al. (2018) The anatomical society core anatomy syllabus for pharmacists: outcomes to create a foundation for practice. J Anat 232, 729–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- General Dental Council (UK) (2008) The First Five Years: The Undergraduate Dental Curriculum. London: General Dental Council. [Google Scholar]
- General Dental Council (UK) (2015) Preparing for Practice: Dental Team Learning Outcomes for Registration. London: General Dental Council. [Google Scholar]
- Guttmann GD (2003) The current status of the anatomical sciences curriculum in US and Canadian dental schools. J Dent Educ 67, 375–379. [PubMed] [Google Scholar]
- Guttmann GD, Ma TP, MacPherson BR (2003) Making gross anatomy relevant to dental students. J Dent Educ 67, 355–358. [PubMed] [Google Scholar]
- Harden RM (1999b) AMEE guide no. 14: outcome‐based education: part 1‐an introduction to outcome‐based education. Med Teach 21, 7–14. [DOI] [PubMed] [Google Scholar]
- Harden RM, Crosby JR, Davis MH, et al. (1999a) AMEE guide no. 14: outcome‐based education: part 5‐from competency to meta‐competency: a model for the specification of learning outcomes. Med Teach 21, 546–552. [DOI] [PubMed] [Google Scholar]
- Holland JC, Smith C, O'Shea M, et al. (2019) The anatomical society core embryology syllabus for undergraduate medicine. J Anat 235, 847–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeney S, McKenna H, Hasson F (2011) The Delphi Technique in Nursing and Health Research. John Wiley & Sons. [Google Scholar]
- Kennedy D, Hyland A, Ryan N (2007) Writing and Using Learning Outcomes: A Practical Guide. Cork: University College Cork. [Google Scholar]
- Latif RA, Mohamed R, Dahlan AH, et al. (2016) Using delphi technique: making sense of consensus in concept mapping structure and multiple choice questions (MCQ). Edu Med J 8. [Google Scholar]
- Louw G, Eizenberg N, Carmichael SW (2009) The place of anatomy in medical education: AMEE guide no 41. Med Teach 31, 373–386. [DOI] [PubMed] [Google Scholar]
- Macluskey M, Durham J, Bell A, et al. (2012) A national survey of UK final year students’ opinion of undergraduate oral surgery teaching. Eur J Dent Educ 16, e205–e212. [DOI] [PubMed] [Google Scholar]
- Macluskey M, Shepherd S, Carter E, et al. (2016) A national follow‐up survey of UK graduates opinion of undergraduate oral surgery teaching. Eur J Dent Educ 20, 174–179. [DOI] [PubMed] [Google Scholar]
- McBride JM, Drake RL (2018) National survey on anatomical sciences in medical education. Anat Sci Educ 11, 7–14. [DOI] [PubMed] [Google Scholar]
- McHanwell S (2015) Teaching anatomical sciences to dental students In: Chan LK. and Pawlina W. (Eds.) Teaching Anatomy, pp. 353–361. Cham: Springer International Publishing. [Google Scholar]
- McHanwell S, Matthan J (in press) Teaching anatomical sciences to dental students In: Chan LK. and Pawlina W. (Eds.) Teaching Anatomy. Cham: Springer International Publishing. [Google Scholar]
- McHanwell S, Atkinson M, Davies DC, et al. (2007) A core syllabus in anatomy for medical students: adding common sense to need to know. Eur J Anat 11, 3–18. [Google Scholar]
- McHanwell S, Davies DC, Morris J, et al. (2019) A core syllabus in anatomy for medical students‐adding common sense to need to know. Eur J Anat 11, 3–18. [Google Scholar]
- McHarg J, Kay EJ (2008) The anatomy of a new dental curriculum. Br Dent J 204, 635–638. [DOI] [PubMed] [Google Scholar]
- Moxham BJ, Plaisant O, Smith CF, et al. (2014) An approach toward the development of core syllabuses for the anatomical sciences. Anat Sci Educ 7, 302–311. [DOI] [PubMed] [Google Scholar]
- Moxham B, McHanwell S, Plaisant O, et al. (2015) A core syllabus for the teaching of neuroanatomy to medical students. Clin Anat 28, 706–716. [DOI] [PubMed] [Google Scholar]
- Moxham BJ, McHanwell S, Berkovitz B (2018) The development of a core syllabus for the teaching of oral anatomy, histology, and embryology to dental students via an international ‘Delphi Panel’. Clin Anat 31, 231–249. [DOI] [PubMed] [Google Scholar]
- Smith CF, Finn GM, Stewart J, et al. (2016a) The Anatomical Society core regional anatomy syllabus for undergraduate medicine. J Anat 228, 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CF, Finn GM, Stewart J, et al. (2016b) Letter to editor: a new core gross anatomy syllabus for medicine. Anat Sci Educ 9(2), 209–210. [DOI] [PubMed] [Google Scholar]
- Smith CF, Finn GM, Stewart J, et al. (2016c) Anatomical Society core regional anatomy syllabus for undergraduate medicine: the Delphi process. J Anat 228, 2–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubbs RS, Paulk PB (2015) Essential anatomy of the head and neck: the complete Delphi panel list. Clin Anat 28, 423–423. [DOI] [PubMed] [Google Scholar]
- Tubbs RS, Sorenson EP, Sharma A, et al. (2014) The development of a core syllabus for the teaching of head and neck anatomy to medical students. Clin Anat 27, 321–330. [DOI] [PubMed] [Google Scholar]
- Webb AL, Green RA, Woodley SJ (2019) The development of a core syllabus for teaching musculoskeletal anatomy of the vertebral column and limbs to medical students. Clin Anat 32, 974–1007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


