Abstract
Background
The length of in-hospital stay (LOS) is an important measure of efficiency in the use of hospital resources and care quality outcomes after orthopaedic surgery. This study investigated the influence of patients' characteristics including demographic factors and the presence of comorbid preoperative depression on LOS after primary total knee arthroplasty (TKA).
Methods
Data were extracted from the California Healthcare Cost and Utilization Project database for hospital discharges after primary TKA for adults aged 50 years and older from 2007 to 2010 (n = 133,603). LOS was defined as the difference in days between the date of admission and the date of discharge. We included demographic data (age, sex, race), comorbidity of depression, and years of admission as covariates in the multivariable model. Negative binomial regression was used to model the effect(s) of covariates on the LOS. As a secondary analysis, the association of covariates with the extended LOS (>9 days) was also investigated using logistic regression.
Results
Our study showed that female sex, age, Medicaid insurance, and race were associated with a longer LOS. Most importantly, a diagnosis of depression was associated with a significantly longer LOS (1.05 times longer: 95% CI: 1.04-1.06) and was independently associated with 1.83 times higher odds (95% CI: 1.50-2.23) of belonging to the extended LOS group. Compared to 2007, significant reductions of both LOS and a longer LOS were noted throughout all later years from 2008 to 2010.
Conclusions
Our study revealed that a diagnosis of depression and patient's characteristic such as age, female sex, Medicaid, nonwhite race resulted in a statistically significant increased LOS. These findings can be useful for planning and resource allocation for total knee replacement programs.
Keywords: Length of stay, Total knee arthroplasty (TKA), Depression
Introduction
Total knee arthroplasty (TKA) remains one of the most successful surgeries in terms of cost-effectiveness, pain reduction, and improvement in quality of life for patients with knee osteoarthritis. The number of TKAs being performed each year is increasing and is expected to reach 3.48 million by the year 2030 [1]. As a result, efforts to decrease reimbursement have been undertaken by payors to conserve health care resources. The result is an increased demand on hospital resources to provide adequate care to TKA patients and maintain a positive margin. The length of hospital stay (LOS) is one representation of the amount of resources used. It reflects several aspects of hospital care including the complexity of the case, the efficiency of hospital care, and the nature of hospital policies on admission and discharge.
There is increasing evidence that psychosocial factors have a significant impact on the outcomes of TKA. Depression is among the most commonly diagnosed psychiatric illnesses [2] and is one factor that may have a significant impact on patient recovery and outcome. The incidence of depression has increased over time in the United States [[3], [4], [5]], decreasing quality of life and placing a burden on the health care system. The purpose of this study was to apply appropriate statistical models to analyze a large population-based database to determine what variables affected inpatient LOS after primary TKA and explore whether an increase in hospital LOS might be associated with the presence of comorbid depression. Therefore, our findings may be useful for preoperative discussions or interventions, surgical decision making, and perioperative or postoperative planning for TKA patients with depression.
Material and methods
Data source
The data were extracted from the California Healthcare Cost and Utilization Project (HCUP) database [6] for hospital discharges after primary total knee (TKA, n = 133,603) performed from 2007 to 2011 on subjects aged 50 years and older. We included subjects with osteoarthritis (ICD-9-CM diagnosis 63 codes: 715.0 [0, 4, 9], 715.1 [0-8], 715.2 [0-8], 715.3 [0-8], 715.8 [0, 9], 715.9 [0-8]), and all repeat admissions within a year were treated as independent cases. At the time of analysis, the 2010 HCUP was the most current database available. The HCUP data include all-payer, encounter-level data for admissions for all hospitals in California.
Outcome variables
The patient's hospital LOS is commonly used as an outcome variable indicative of hospital performance. The LOS is the difference in days between the date of admission and the date of discharge. In addition to the original metric (days) of LOS, we defined a dummy variable that indicated an extended LOS as the excessive days beyond an outlier limit (Fig. 1). Based on observed inpatient LOS days, 95% of LOS (<9 days) was as expected or regular. The remaining 5% of stays over this cutoff were defined as irregular, prolonged stays or outliers. This outlier categorization was proposed as a better measure for studying inpatient care inefficiency [7]. Both measures were used in the analysis to evaluate the impact of covariates on LOS.
Figure 1.
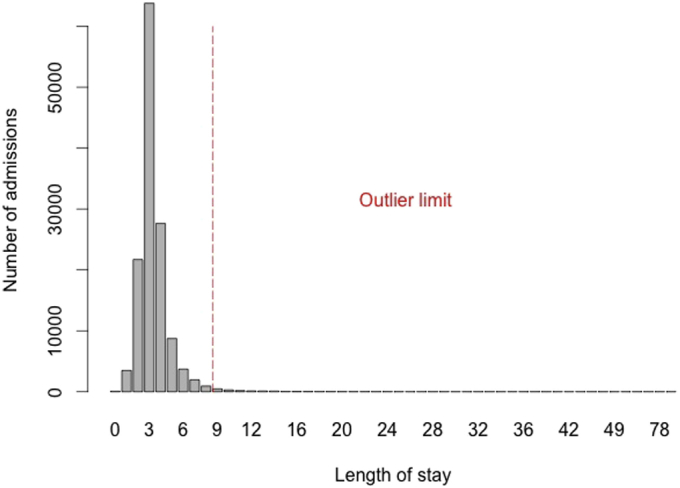
LOS distribution-primary total knee arthroplasties.
Study covariates
The explanatory variables included in the analysis are patients' demographics (age, sex, race), clinical characteristics (comorbidity of depression), and a temporal variable (year of admission). Age was categorized in 5-year age groups: 50-54, 55-59, 60-64, 65-69, 70-74, 75-79, 80 or older. The reference age group is the youngest, 50-54 years. Race was represented by 5 categories of white, black, Hispanic, Asian, and others. Comorbid depression present on the index admission was identified using the algorithm described in Elixhauser et al. [8] according to the International Classification of Diseases, version 9 (ICD9-CM diagnosis code) at the time of surgery.
Statistical analyses
Initial descriptive and univariate analyses were first conducted. We then fitted multivariate regression models for predicting LOS to test for associations of patient characteristics with LOS. In fitting a multivariate regression model on an original scale of LOS, we used a negative binomial model (NBM). The NBM is preferred over a Poisson model for skewed count data when there is overdispersion, that is, when the mean and the variance are not equal, which was in our case. Statistical results are in the form of log-ratios, the incident rate ratios (IRRs). A positive coefficient in the regression output indicates that a variable will increase the LOS relative to its reference category, and conversely, a negative coefficient will decrease the LOS relative to its reference category. We reported the ratio, the exponent of the coefficient, which can be interpreted, all other things being fixed, as the ratio of the LOS at one level of the covariate to the LOS expected for one level less. The residuals were analyzed to validate the fit of the negative binomial model to the data.
We also conducted a secondary analysis to determine the impact of different covariates on the odds of being in the outlier LOS group. A multivariate logistic regression model was fit on the dichotomous outcome of “regular” vs “outlier” LOS. Adjusted odds ratios were calculated to estimate the associated relative risk of belonging to the longer stay subgroup whose LOS was considered an outlier. A P-value ≤ .05 was considered to be significant and all tests were 2 sided. All statistical analyses were performed using R statistical software version 3.1.3 (www.R-project.org) [9].
Results
The median LOS after admission was 3 days (interquartile range, 3-4 days) with a mean of 3.4 days (SD = 1.7 days). The maximum LOS was 158 days. The distribution of LOS was strongly positively skewed, with a small minority of patients having very long postoperative lengths of stay as shown in Figure 1.
Table 1 shows the summary of descriptive statistics of admissions (n = 133,603) across the key explanatory variables. In the cohort, females (62.3%) had more admissions than males (37.7%). 74.8% of patients were white, 4.6% were black, 13.7% were Hispanic, 3.8% were Asian, and 3% were categorized as other race. About 7.3% of admissions were diagnosed with depression at the time of surgery. Most admissions were by private insurance or Medicare coverage (97.4%) compared to Medicaid (2.6%). The number of admissions steadily increased over time, 13% over a 4-year period.
Table 1.
Summary of descriptive statistics for subjects receiving total knee arthroplasty, HCUP-California, 2007-2010 (N = 133,603).
| Characteristics | Frequency (%) |
|---|---|
| Year of admission | |
| 2007 | 31,615 (23.7%) |
| 2008 | 32,535 (24.3%) |
| 2009 | 33,746 (25.3%) |
| 2010 | 35,707 (26.7%) |
| Age (y) | |
| 50-54 | 9113 (6.8%) |
| 55-59 | 15,667 (11.7%) |
| 60-64 | 20,717 (15.5%) |
| 65-69 | 24,539 (18.4%) |
| 70-74 | 23,437 (17.5%) |
| 75-79 | 21,222 (15.9%) |
| Over 80 | 18,908 (14.2%) |
| Insurance type | |
| Medicaid | 3498 (2.6%) |
| All other insurance | 130,099 (97.4%) |
| Sex | |
| Female | 81,951 (62.3%) |
| Male | 49,683 (37.7%) |
| Ethnic group | |
| White | 95,715 (74.8%) |
| Hispanic | 17,565 (13.7%) |
| Black | 5950 (4.6%) |
| Asian | 4923 (3.8%) |
| All others | 3805 (3.1%) |
| Comorbidity depression | |
| Yes | 9786 (7.3%) |
| No | 123,817 (92.7%) |
In the multivariate analysis, a full model predicting LOS that included all explanatory variables was first developed (Table 2) by fitting the negative binomial model. The results in Table 2 are in terms of the IRR. Holding all other variables constant, we found that a diagnosis of depression was associated with a significantly longer LOS (IRR 1.05 95% CI [1.04 1.06]). Females had significantly longer LOS than males (IRR 1.03 95% CI [1.03-1.04]). The association with age and LOS increased monotonically, with age categories older than 65 years having a significantly longer LOS than 50-54 year olds, from 1.03 (95% CI [1.01 1.04]) times longer for 65-69 year olds up to 1.15 (95% CI [1.14 1.17]) times longer for those over age 80. Furthermore, there was a significantly longer LOS associated with being all nonwhite groups compared to whites (IRR 1.06 95% CI [1.05, 1.07] for Hispanic, IRR 1.11 95% CI [1.10, 1.13] for black, IRR 1.12 95% CI [1.10, 1.14] for Asian) and being insured with Medicaid compared to other insurance (IRR 1.22 95% CI [1.19-1.24]). All other variables being equal, patients admitted in 2011 had an LOS 0.860 times shorter (95% CI [0.85 0.87]) than those admitted in 2007.
Table 2.
Multivariable models for length of stay after total knee arthroplasty in California, 2007-2010 (N = 133,603).
| Characteristics | Negative binomial model on LOS, indicating relative LOS |
Logistic regression model for probability of having outlier LOS (>9 d) |
||||
|---|---|---|---|---|---|---|
| aRatio | [95% CI] | Odds ratio | [95% CI] | |||
| Sex | ||||||
| Male# | 1.00 | 1.000 | ||||
| Female | 1.031d | 1.025 | 1.037 | 0.635d | 0.561 | 0.718 |
| Age (y) | ||||||
| 50-54# | 1.000 | 1.000 | ||||
| 55-59 | 1.004 | 0.989 | 1.019 | 0.889 | 0.629 | 1.258 |
| 60-64 | 1.006 | 0.992 | 1.021 | 1.040 | 0.753 | 1.437 |
| 65-69 | 1.028d | 1.014 | 1.042 | 1.217 | 0.889 | 1.666 |
| 70-74 | 1.051d | 1.037 | 1.066 | 1.557c | 1.145 | 2.117 |
| 75-79 | 1.093d | 1.078 | 1.108 | 1.973d | 1.454 | 2.677 |
| Over 80 | 1.154d | 1.138 | 1.171 | 2.932d | 2.176 | 3.951 |
| Ethnic group | ||||||
| White# | 1.000 | 1.000 | ||||
| Hispanic | 1.063d | 1.054 | 1.072 | 1.214b | 1.019 | 1.447 |
| Black | 1.111d | 1.096 | 1.126 | 1.917d | 1.503 | 2.445 |
| Asian | 1.118d | 1.102 | 1.135 | 2.045d | 1.615 | 2.590 |
| All others | 1.045d | 1.026 | 1.064 | 1.096 | 0.760 | 1.581 |
| Insurance type | ||||||
| All other insurance# | 1.000 | 1.000 | ||||
| Medicaid | 1.216d | 1.195 | 1.238 | 3.721d | 2.932 | 4.724 |
| Depression comorbidity | ||||||
| No# | 1.000 | 1.000 | ||||
| Yes | 1.052d | 1.041 | 1.064 | 1.826d | 1.496 | 2.229 |
| Year of admission | ||||||
| 2007# | 1.000 | 1.050 | 0.906 | 1.218 | ||
| 2008 | 0.958d | 0.950 | 0.966 | 0.800c | 0.681 | 0.940 |
| 2009 | 0.918d | 0.910 | 0.925 | 0.634d | 0.535 | 0.751 |
| 2010 | 0.888d | 0.881 | 0.895 | 0.607d | 0.513 | 0.718 |
Exponent of the coefficient, which is the expected change in log count for a one-unit increase in a “Characteristic,” interpreted as a ratio to the #Reference category.
P < .05.
P < .01.
P < .001.
Table 2 also reports adjusted odds ratios (ORs) for factors predicting an extended (outlier) LOS (>9 days) based on a logistic regression model. Similarly to factors affecting LOS, the comorbidity of depression was independently associated with 1.83 times higher odds (95% CI [1.50 2.23]) of belonging to the extended LOS group. Those over 80 years older had 2.4 times higher odds (95% CI [1.89 3.06]) of belonging to the extended LOS subgroup than the reference group, 50-54 year olds. Relative to other insured groups, the odds of belonging to the extended LOS subgroup increased about 4-fold (OR 3.72 95% CI [2.93 4.72]) for the Medicaid insured. The odds decreased over time and significantly decreased by 39% (OR 0.61 95% CI [0.51 0.72]) in 2010 compared with the reference year 2007. The likelihood of being in the extended LOS subgroup was significantly higher in patients who were black (OR 1.92 95% CI [1.50 2.44]), Hispanic (OR 1.21 95% CI [1.02 1.45]), or Asian (OR 2.05 95% CI [1.62 2.59]), compared to white. Being a woman, however, yielded odds 40% lower of being in the outlier LOS group compared to men (OR 0.64 95% CI [0.56 0.72]), which is in contrast with the LOS analysis.
Discussion
As the demand for TKA increases due to its well-proven clinical success, hospital admissions place a substantial burden on the health system. Therefore, decreased reimbursement and alternative payment models, such as bundled payment, have emerged. This requires that providers develop ways to provide care in an efficient cost-effective manner to maintain a positive margin. Decreasing length of stay is one way to impact the cost of the procedure. Therefore, it is important to recognize all the factors that affect hospital LOS to try to optimize the use of medical resources and ultimately optimize the care and outcomes of patients.
In this study, we used multivariate analyses to identify patient-related factors associated with LOS and extremely longer LOS. We found that a comorbid diagnosis of depression was associated with higher odds of longer in-hospital length of stay after TKA. Subjects who were female or black race tended to stay in the hospital longer after TKA in patients of all ages. LOS has demonstrated a general decline over time. One of the interesting findings is that although females overall have a longer in-hospital LOS than male counterparts, they tend to have lower risk of having an extremely extended LOS. In summary, patient-related factors, including older age, higher levels of depression, were associated with increased risk of lengthy LOS. Although both outcomes of the analysis would assist clinicians and managers in the preparation of prescriptive policies for a better utilization of resources by comparing and contrasting the significant factors, our finding that patients with depression are at high risk of prolonged LOS is particularly important in that it will allow physicians to treat those patients more aggressively.
Most studies of LOS have not been subjected to well-designed modeling. The distribution of LOS data is frequently positively skewed. Much of the LOS research either analyzed mean LOS using linear regression where the models must assume unskewed data [10,11] or used logistic regression on a binomial split of the LOS data, which may assume a simple process for finding optimal and clinically relevant cut points. The Poisson and negative binomial modeling techniques are often used for modeling count data, such as the number of days. A negative binomial model is preferred when there is overdispersion; that is, when the mean and the variance are not equal. In the context of LOS, this can occur if there are more 0 days of admission than anticipated under a Poisson model. In this study, we used an NBM to test the association of patient characteristics with LOS. As a secondary analysis, an extended LOS was defined as a binary outcome variable that was positive when the postoperative LOS exceeds the 99th percentile of LOS [12]. The 99th percentile LOS was chosen as a cutoff to account for normal variations and differing practices of surgeons and hospitals while still capturing patients with abnormally extended LOS. The logistic regression model was then applied for the development of the model on this outcome. The use of this methodology is the strength of this study.
Although this retrospective study provides novel data regarding an impact of depression on length of stay after TKA, this study has some limitations. Study limitations include nonresponse bias and the use of diagnostic codes, which may be associated with underdiagnosis of conditions. Because depression was captured based on presence of a diagnostic code, psychological comorbidities and its underlying severity may be underrecognized and underdiagnosed; it is likely that we missed some cases. This might have biased our estimates toward null. Unfortunately, a retrospective study design did not allow us to have confirmation of depression diagnosis by examination by a psychologist or psychiatrist. Therefore, the direction of impact of this bias on our study findings overall is unclear. To validate diagnosis of depression, some gold standard such as a chart review may be desirable, which unfortunately was not feasible due to the limited resources available to us. In our future study, we will endeavor to direct our focus to a more granular examination of the specifics of ICD-9 coding and its potential flaws. A misclassification biases due to the temporal change of diagnostic codes should be also assessed in our future studies. Another limitation of this study includes those inherent in any analysis of data from large administrative databases. They are not collected for research purposes; thus, data elements may vary in accuracy, and key clinical variables such as ICU-specific physiologic and laboratory data are usually lacking. Specific efforts should be made to validate the data elements used, as has been done in several world regions. As with any other research question, it is imperative that the analysis plan should be carefully defined in advance and that appropriate attention be paid to potential sources of bias and confounding. For example, because ICD-9-CM codes were used to retrieve the diagnoses, procedures, and adverse events, there is a possibility of misclassification error. However, prior studies suggest that misclassifications are likely distributed evenly among groups, preventing them from affecting our statistical analysis [13].
Conclusions
Our analysis of population-based data from one large state provides important information to understand the drivers of cost and longer LOS after TKA. Our study showed that female sex, advanced age, Medicaid insurance, and black race were associated with a longer LOS. Our study additionally revealed that a diagnosis of depression during the hospital stay resulted in a statistically significant increased LOS. A prediction model using easily and routinely obtained preoperative measures based on our findings could be developed to predict absolute LOS in patients after knee replacement and help to better manage these patients. Further work is needed to develop strategies to address depression to improve length of stay after TKA.
Our study highlights the need for attention to patients with this potentially modifiable condition. This could inform preoperative discussions, surgical decision making, and postoperative planning for TKA patients. These findings can be useful for planning and resource allocation for total knee replacement programs.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2019.11.010.
Appendix A. Supplementary data
References
- 1.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Kessler R.C., Chiu W.T., Demler O., Walters E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Compton W.M., Conway K.P., Stinson F.S. Changes in the prevalence of major de- pression and comorbid substance use disorders in the United States between 1991- 1992 and 2001-2002. Am J Psychiatry. 2006;163:2141. doi: 10.1176/ajp.2006.163.12.2141. [DOI] [PubMed] [Google Scholar]
- 4.Murray C.J., Lopez A.D. Alternative projections of mortality and disability by cause 1990-2020: global burden of disease study. Lancet. 1997;349:1498. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 5.Somers J.M., Goldner E.M., Waraich P. Prevalence and incidence studies of anxiety disorders: a systematic review of the literature. Can J Psychiatry. 2006;51:100. doi: 10.1177/070674370605100206. [DOI] [PubMed] [Google Scholar]
- 6.Agency for Healthcare Research and Quality. H-CUPnet 2012 National Statistics. 2012 https://hcupnet.ahrq.gov/ [Google Scholar]
- 7.Silber J.H., Rosenbaum P.R., Koiziol L.F., Sutaria N., M R.R., Even-Shoshan O. Conditional length of stay. Health Serv Res. 1999;34(1 pt 2):349. [PMC free article] [PubMed] [Google Scholar]
- 8.Elixhauser A., Steiner C., Harris D.R., Coffey R.M. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 9.R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/. [Accessed 1 December 2019].
- 10.Zheng F., Cammisa F.P., Sandhu H.S., Girardi F.P., Khan S.N. Factors predicting hospital stay, operative time, blood loss, and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion, and segmental instrumentation. Spine. 2002;27:818. doi: 10.1097/00007632-200204150-00008. [DOI] [PubMed] [Google Scholar]
- 11.Mahadevan D., Challand C., Keenan J. Revision total hip replacement: predictors of blood loss, transfusion requirements, and length of hospitalisation. J Orthop Traumatol. 2010;11:159. doi: 10.1007/s10195-010-0105-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lilleeng S. Norsk institutt for sykehusforskning; Trondheim: 1992. Trimpunkt, kostnadsvekter og enhetspriser for HCFA versjon 3 og 8 [Outliers, cost-weights and index- prices for HCFA version 3 and 8] [Google Scholar]
- 13.Buller L.T., Best M.J., Klika A.K., Barsoum W.K. The influence of psychiatric comorbidity on perioperative outcomes following primary total hip and knee arthroplasty; a 17-year analysis of the National Hospital Discharge Survey database. J Arthroplasty. 2015;30(2):165. doi: 10.1016/j.arth.2014.08.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


