Abstract
Background
Technology-assisted total hip arthroplasty (TA-THA) using either computer-assisted navigation or robotic assistance has become increasingly more popular. The purpose of this study was to examine the trends and patient factors associated with TA-THA.
Methods
This is a retrospective review utilizing the National Inpatient Sample, a large national database incorporating inpatient hospitalization information. International Classification of Diseases, 9th Revision codes were used to identify patients with hip osteoarthritis who underwent primary total hip arthroplasty (THA). Patients were then separated into those who underwent TA-THA or conventional THA. Outcomes of interest included annual TA-THA utilization; patient and hospital characteristics associated with TA-THA; and trends for length of stay (LOS), cost, and discharge to home.
Results
From 2005 to 2014, a total of 2,588,304 patients with hip osteoarthritis who underwent THA were identified in the National Inpatient Sample database. Of those, 39,700 (1.5%) underwent TA-THA. The number of TA-THA procedures increased from 178 (0.1% of all THA) in 2005 to 10,045 (3.0% of all THA) in 2014, which represented a 30-fold increase in incidence (P-trend <.0001). TA-THA was associated with Hispanic race, higher patient income, and the Western region of the United States. During the study period, there was a trend toward decreased LOS and increased discharge to home for both TA-THA and conventional THA. TA-THA was associated with higher inpatient cost.
Conclusion
TA-THA is being increasingly used in the United States and is associated with specific patient factors. However, the value of TA-THA compared to conventional THA remains unclear and should be assessed with future research.
Level of Evidence
III (retrospective cohort study).
Keywords: Total hip arthroplasty, Computer-assisted navigation, Robotic assistance, Clinical epidemiology, Database study
Introduction
Total hip arthroplasty (THA) is a highly efficacious treatment for patients with hip osteoarthritis (HOA) [[1], [2], [3]]. Despite the success of THA, mechanical complications such as instability and aseptic loosening still occur and are often the result of implant malpositioning or sizing mismatch [[4], [5], [6], [7], [8]]. These complications may ultimately require revision surgeries which not only increase patient morbidity and disability but also increase health care costs [[8], [9], [10], [11]].
Technology-assisted THA (TA-THA), which includes both computer-assisted navigation and robotic assistance, aims to minimize these mechanical complications by improving surgeon precision and accuracy with respect to implant positioning based on criteria defined by Lewinnek et al [[12], [13], [14]]. Multiple studies have demonstrated that TA-THA improves acetabular component position compared to conventional THA [[15], [16], [17], [18], [19], [20], [21]]. However, whether TA-THA results in meaningful improvement in clinical outcomes compared to conventional THA remains unclear. Bohl et al [22] recently showed decreased dislocation and acetabular component revision rates in their retrospective study of 14,540 patients who underwent THA with computer-assisted navigation. Conversely, other studies, including 2 randomized trials by Lass et al and Parratte et al, have found no clinically significant differences in patient-reported outcomes or revision surgery rates between TA-THA and conventional THA [[19], [20], [21],[23], [24], [25]]. Despite these findings, it appears that TA-THA is becoming increasingly more popular. A retrospective study by Boylan et al [26] using a statewide database found that rates of TA-THA increased from 0.5% in 2008 to 5.2% in 2015. Whether the same trend exists nationally in the United States is unclear as the current literature lacks studies that examine the national utilization of TA-THA.
The purpose of this study was to use a large, national database to examine the utilization of TA-THA; to identify any patient and/or hospital factors associated with TA-THA use; and to compare trends in health care resource utilization, specifically hospital length of stay (LOS), hospital cost, and patient discharge to home for TA-THA vs conventional THA. We hypothesize that a majority of TA-THA procedures are done in younger, healthier patients at large, academic centers.
Material and methods
Our study cohort was identified using the National Inpatient Sample (NIS) over a 10-year period (2005-2014). The NIS is a nationally representative database developed from all hospitals participating in the Healthcare Cost and Utilization Project (HCUP) and validated through a federal–state–industry partnership sponsored by the Agency for Healthcare Research and Quality (AHRQ) [26]. It is based on inpatient data from over 40 states derived from billing and discharge information, covering approximately 96% of the U.S. population using an estimate of 20% stratified sample of discharges from U.S. community hospitals [27]. A stratified formula based on discharge weights reported by participating HCUP institutions was designed to allow an estimation of nationally representative statistics. Available variables include demographic data, diagnoses, procedures, LOS, cost, and hospital characteristics [27]. Since the NIS database has been sufficiently deidentified of any personal health information or identifiers, this study was deemed exempt by the Institutional Review Board at our institution.
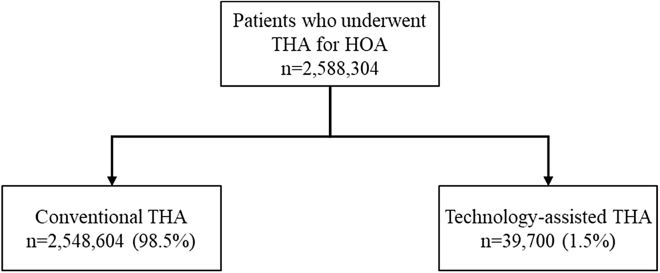
Patients older than 18 years of age with a history of HOA who were admitted and underwent primary THA from 2005 to 2014 were considered for this study. Patients were identified using the International Classification of Diseases, 9th Revision (ICD-9) diagnosis codes for HOA (715.15, 715.25, 715.35, 715.95) and ICD-9 procedure code for primary THA (81.51). We chose to combine ICD-9 codes for computer-assisted surgery (00.31, 00.32, 00.33, 00.34, 00.35, and 00.39) and robotic-assisted surgery (17.41 and 17.49) to identify our TA-THA cohort (Fig. 1 and Table 1). Baseline comorbidity was quantified using the Elixhauser Comorbidity Index (ECI), a composite score of 31 comorbid conditions. Higher scores corresponded to greater burden of comorbid conditions [28].
Figure 1.
Patients who underwent THA for HOA were separated based on whether they had conventional THA vs technology-assisted THA using ICD-9 codes.
Table 1.
ICD-9 codes used for identifying patients of interest.
| Diagnosis | ICD-9 codes |
|---|---|
| Hip osteoarthritis | 715.15, 715.25, 715.35, 715.95 |
| Procedure | ICD-9 codes |
| Total hip arthroplasty | 81.51 |
| Computer-assisted surgery | 00.31, 00.32, 00.33, 00.34, 00.35, 00.39 |
| Robotic-assisted surgery | 17.41, 17.49 |
Patient demographics and hospital characteristics as well as hospital LOS, cost, and discharge to home for TA-THA patients were analyzed and compared with those of conventional THA patients. Patient demographics included age (years), sex (male and female), race (white, black, Hispanic, Asian, Native American, and other), and insurance (Medicare, Medicaid, private, and self-pay). Hospital characteristics included hospital type (urban nonteaching, urban teaching, and rural), hospital size based on number of beds (large, medium, and small), and region (Northeast, Midwest, South, and West). Of note, the number of beds used to classify hospital size as well as states included in each region are based off NIS definitions and can be found in Appendix 1, Appendix 2, respectively [29,30]. Individual hospitalization cost was calculated using diagnosis-related group codes multiplied by hospital-specific cost-to-charge ratios provided by the AHRQ. HCUP indices of the diagnosis-related group were then used to account for differences in hospitalization severity [31]. The cost was subsequently standardized for inflation using the yearly gross domestic product.
All result sample sizes represented national annual estimates, accounting for individual discharge-level weights from the NIS's stratified 2-stage cluster design, using Stata's survey data commands. Descriptive statistics were used to describe both baseline characteristics and outcome parameters within each comparison group. The annual incidence of TA-THA was calculated for each available year, and trend probability analysis was done using the Cochran-Armitage method, with a significance level set at P < .05. Within each demographic section, the first demographic category listed by the AHRQ served as the reference value for comparisons using a survey weighted regression. Logistic regression analysis was used to calculate odds ratios (OR) without multivariate adjustment. Continuous variables were reported using mean, 95% confidence interval (CI), and P-value. Analysis was done using a 2-tailed Student's t-test after ensuring normal distributions. For skewed, nonparametric distributions, continuous variables are presented as median (interquartile range) and analyzed using the Wilcoxon rank-sum test. Trends for hospital LOS, cost, and patient discharge to home were generated by plotting annual means for both conventional THA and TA-THA. All statistical analysis was performed by comparing TA-THA patients to conventional THA patients for each outcome of interest. Data were analyzed using Stata 15.1 (College Station, TX). All tests were unpaired and significance level was defined at P < .05.
Results
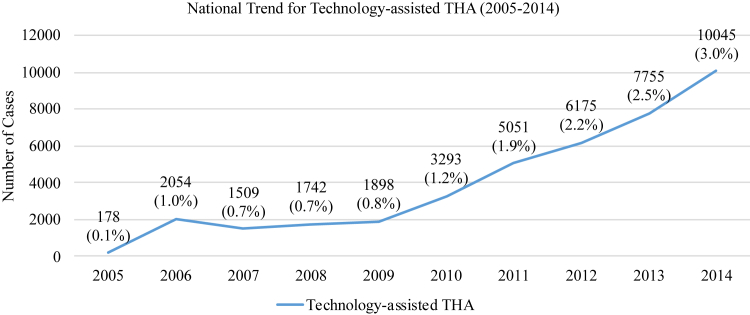
During our 10-year study period, there were 2,588,304 patients with HOA who underwent primary THA identified in the NIS database. Among these patients, 2,548,604 (98.5%) underwent conventional THA and 39,700 (1.5%) underwent TA-THA (Fig. 1). There were 178 TA-THA procedures performed in 2005 and 10,045 TA-THA procedures performed in 2014, which represented a 30-fold increase in annual incidence from 0.1% to 3.0% of all THA procedures over the study period (P-trend <.0001) (Fig. 2).
Figure 2.
National trends for technology-assisted THA from 2005 to 2014. The number of technology-assisted THA cases increased from 178 (0.1% of all THA) in 2005 to 10,045 (3.0% of all THA) in 2014 (P-trend <.0001).
Patient demographics
There was no difference in patient age, sex, insurance type, or ECI scores between TA-THA patients and conventional THA patients (Table 2, Table 3). Of note, out of the 39,700 patients who underwent TA-THA, 20,909 (52.7%) patients had Medicare and 16,573 (41.7%) patients had private insurance. Black patients were less likely to undergo TA-THA (OR = 0.65, 95% CI: 0.54-0.79, P < .0001) compared to white patients. On the other hand, Hispanic patients were more likely to undergo TA-THA (OR = 1.33, 95% CI: 1.02-1.74, P = .033) compared to white patients. Patients from the 25-50th and 50-75th percentile income brackets were more likely to undergo TA-THA (OR = 1.21, 95% CI: 1.06-1.39, P = .005 and OR = 1.18, 95% CI: 1.01-1.38, P = .042, respectively) compared to patients from the 0-25th percentile income bracket.
Table 2.
Patient demographics.
| Age (y) |
Elixhauser Comorbidity Index |
|||||
|---|---|---|---|---|---|---|
| Mean | 95% CI | P-valuea | Mean | 95% CI | P-valuea | |
| Conventional THA | 65.5 | 65.3-65.6 | – | 1.76 | 1.75-1.78 | – |
| Technology-assisted THA | 65.4 | 64.9-65.9 | .8824 | 1.77 | 1.71-1.83 | .6874 |
P-value when compared to conventional THA group.
Table 3.
Patient demographics and hospital characteristics.
| Conventional THA % (N) | TA-THA % (N) | OR | 95% CI | P-valuea | |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 98.4 (1,117,096) | 1.5 (17,478) | 1.00 | (Reference) | |
| Female | 98.5 (1,425,474) | 1.5 (22,136) | 0.99 | 0.95-1.04 | .765 |
| Race | |||||
| White | 98.4 (1,865,733) | 1.6 (31,011) | 1.00 | (Reference) | |
| Black | 98.9 (146,006) | 1.1 (1573) | 0.65 | 0.54-0.79 | <.0001 |
| Hispanic | 97.8 (64,684) | 2.2 (1434) | 1.33 | 1.02-1.74 | .033 |
| Asian | 98.0 (17,377) | 2.0 (359) | 1.24 | 0.84-1.85 | .282 |
| Native American | 97.1 (6532) | 2.9 (194) | 1.78 | 0.90-3.53 | .096 |
| Other | 98.7 (42,899) | 1.3 (571) | 0.80 | 0.57-1.12 | .191 |
| Insurance | |||||
| Medicare | 98.5 (1,342,901) | 1.5 (20,909) | 1.00 | (Reference) | |
| Medicaid | 98.7 (80,178) | 1.3 (1020) | 0.82 | 0.64-1.05 | .111 |
| Private | 98.4 (1,042,331) | 1.6 (16,573) | 1.02 | 0.93-1.12 | .668 |
| Self | 98.7 (17,068) | 1.3 (230) | 0.87 | 0.62-1.21 | .396 |
| Income | |||||
| 0-25th percentile | 98.6 (469,046) | 1.4 (6490) | 1.00 | (Reference) | |
| 25-50th percentile | 98.3 (628,124) | 1.7 (10,542) | 1.21 | 1.06-1.39 | .005 |
| 50-75th percentile | 98.4 (672,650) | 1.6 (10,951) | 1.18 | 1.01-1.38 | .042 |
| 75-100th percentile | 95.5 (733,295) | 1.5 (10,861) | 1.07 | 0.84-1.37 | .584 |
| Hospital type | |||||
| Rural | 98.9 (254,466) | 1.1 (2776) | 1.00 | (Reference) | |
| Urban teaching | 98.4 (1,211,882) | 1.6 (19,806) | 1.49 | 0.95-2.36 | .080 |
| Urban nonteaching | 98.4 (1,074,356) | 1.6 (17,084) | 1.46 | 0.96-2.23 | .081 |
| Hospital size | |||||
| Small | 98.3 (470,994) | 1.7 (8064) | 1.00 | (Reference) | |
| Medium | 98.6 (646,679) | 1.4 (9043) | 0.81 | 0.58-1.16 | .255 |
| Large | 98.4 (1,423,031) | 1.6 (22,560) | 0.93 | 0.63-1.37 | .701 |
| Region | |||||
| Northeast | 98.9 (527,727) | 1.1 (5683) | 1.00 | (Reference) | |
| Midwest | 99.0 (686,206) | 1.0 (6709) | 0.91 | 0.52-1.58 | .733 |
| South | 98.3 (809,961) | 1.7 (13,688) | 1.57 | 0.94-2.63 | .088 |
| West | 97.5 (524,745) | 2.5 (13,586) | 2.40 | 1.61-3.59 | <.0001 |
P-value when compared to reference category.
Hospital characteristics
There was no difference in hospital type or hospital size between TA-THA patients and conventional THA patients (Table 3). However, patients from the Western region of the United States were more likely to undergo TA-THA (OR = 2.40, 95% CI: 1.61-3.59, P < .0001) compared to patients from the Northeast region (Table 3).
Health care resource utilization trends
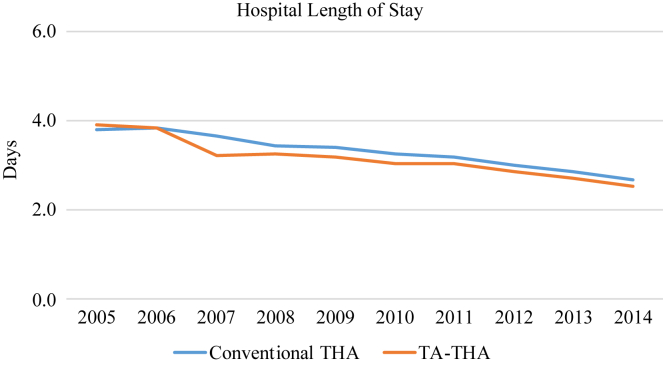
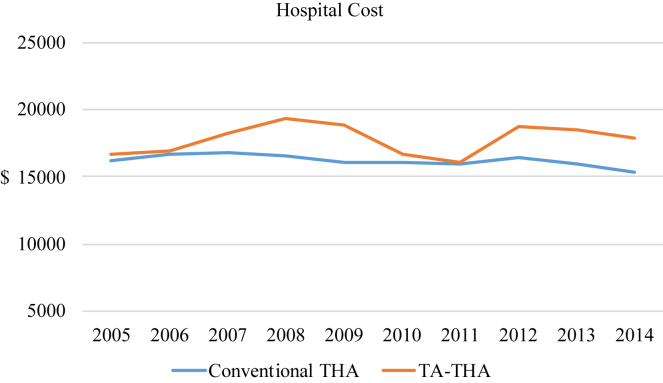
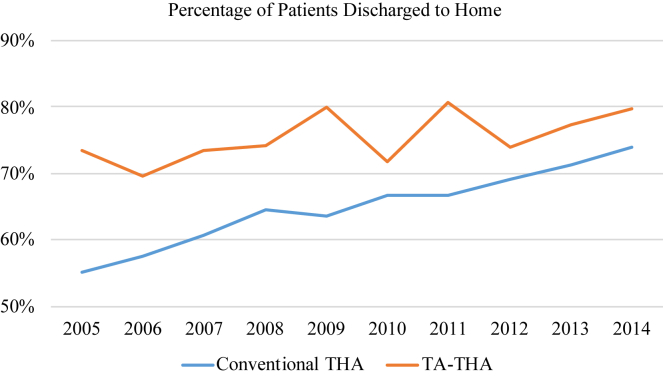
Hospital LOS decreased over the study period for both conventional THA and TA-THA. The average LOS decreased from 3.8 days in 2005 to 2.7 days in 2014 for conventional THA patients, whereas the average LOS decreased from 3.9 days in 2005 to 2.5 days in 2014 for TA-THA patients (Fig. 3). Hospital cost decreased over the study period for conventional THA and increased for TA-THA. The average cost decreased from $16,237.42 in 2005 to $15,327.01 in 2014 for conventional THA, whereas the average cost increased from $16,694.07 in 2005 to $17,846.10 in 2014 for TA-THA (Fig. 4). The percentage of patients discharge to home increased over the study period for both cohorts. Specifically, the percentage of patients discharged to home increased from 55% in 2005 to 74% in 2014 for conventional THA, whereas the percentage of patients discharged to home increased from 74% in 2005 to 80% in 2014 for TA-THA (Fig. 5).
Figure 3.
Hospital length of stay decreased over the study period for both conventional THA and TA-THA. Specifically, the average length of stay decreased from 3.8 d in 2005 to 2.7 d in 2014 for patients who underwent conventional THA, whereas the average length of stay decreased from 3.9 d in 2005 to 2.5 d in 2014 for TA-THA.
Figure 4.
The average hospital cost decreased over the study period for conventional THA and increased for TA-THA. Specifically, average cost decreased from $16,237.42 in 2005 to $15,327.01 in 2014 for conventional THA, whereas the average cost increased from $16,694.07 in 2005 to $17,846.10 in 2014 for TA-THA.
Figure 5.
The percentage of patients discharged to home increased over the study period for both conventional THA and TA-THA. Specifically, the percentage of patients discharged to home increased from 55% in 2005 to 74% in 2014 for conventional THA, whereas the percentage of patients discharged to home increased from 74% in 2005 to 80% in 2014 for TA-THA. Patients who underwent TA-THA had a higher percentage of discharges to home compared to those who underwent conventional THA throughout the study period.
Discussion
Previous studies have demonstrated that TA-THA improves the precision and accuracy of acetabular component positioning compared to conventional THA [[15], [16], [17], [18], [19], [20], [21]]. However, it is unclear whether the use of TA-THA results in improved long-term clinical outcomes and decreased postoperative complications compared to conventional THA [[19], [20], [21], [22], [23], [24], [25]]. Furthermore, purchasing any computer-assisted navigation or robotic-assistance systems requires not only a significant initial financial investment but also a routine maintenance fee and disposable instrument cost [12,14,26]. In addition, use of technology assistance has been shown to increase operative times and potentially increase patient radiation exposure because of the need for a preoperative CT scan with certain systems [19,32,33]. Despite these shortcomings, our retrospective cohort study found that utilization of TA-THA increased from 2005 to 2014 in the United States. To the best of our knowledge, our study is the first to use a large, national database to evaluate the utilization of TA-THA in the United States.
Using a statewide database, Boylan et al [26] found that TA-THA use increased from 2008 to 2015. We showed a similar increase from 2005 to 2014, but our study was done using the NIS, a national database. Antonios et al used the NIS to evaluate the national trend of technology-assisted total knee arthroplasty (TA-TKA) and found an increase from 1.2% in 2005 to 7.0% in 2014 [34]. Thus, it is clear that the increasing use of technology assistance is not just limited to THA but also present in other common orthopaedic procedures such as TKA.
In our study, patients who underwent TA-THA had no differences in age or medical comorbidities, as measured by ECI, compared to those who underwent conventional THA. Our findings differ from what Bohl et al [22] showed, which was that patients who underwent THA with computer-assisted navigation tended to be younger and with fewer medical comorbidities. We attribute these differences to the fact that Bohl et al used the Medicare Part A claims data set and included only Medicare patients ≥65 years old, whereas we included all insurance payers for patients of all ages. We believe that the broader scope of our study allows for a more accurate representation of the national landscape of TA-THA utilization.
We also found that socioeconomic factors such as race and patient income were associated with use of TA-THA. Specifically, when compared to white patients, black patients were less likely to undergo TA-THA, whereas Hispanic patients were more likely to undergo TA-THA. In addition, patients from higher income quartiles were found to have an increased likelihood of undergoing TA-THA. These findings are similar to what Bohl et al [22] found in their study and suggest a potential disparity in the utilization of TA-THA based on socioeconomic factors. Although large, prospective randomized controlled trials are needed to determine if TA-THA results in improved clinical outcome measures, the socioeconomic differences presented here warrant further investigation to eliminate any inequitable distribution of a new surgical technology.
We found no differences in the likelihood of undergoing TA-THA based on hospital size or type. These findings are similar to what Antonios et al showed in their analysis of TA-TKA but differ from Bohl et al in their retrospective study of THA with computer-assisted navigation [22,34]. Specifically, Bohl et al [22] showed that large, teaching medical centers had increased utilization of computer-assisted navigation. We again attribute these findings to the fact that their study was done using the Medicare Part A claims database, whereas our study was done using the NIS database which contains all insurance payers. In our study, nearly half of the patients who underwent TA-THA had private insurance. Thus, privately insured patients constitute a large proportion of patients in our study and their inclusion may influence the association of hospital type and size with TA-THA.
Our analysis revealed regional differences associated with the use of TA-THA. Specifically, we found that TA-THA was more likely to be done in the Western region compared to the Northeast region. This finding is similar to what numerous other studies have shown which is that use of technology assistance in arthroplasty surgery, whether it is computer-assisted navigation or robotic assistance, is more prevalent in the Western region of the United States [22,34].
During our study period, the average LOS for both TA-THA and conventional THA decreased from approximately 4 days to 2 days. These findings are similar to what other studies have shown. Specifically, Bohl et al [22] showed that a majority of the patients who underwent THA with computer-assisted navigation stayed 2-3 days in the hospital. Furthermore, we found an increase in the percentage of patients discharged to home for both TA-THA and conventional THA. We attribute the similarity in trends for LOS and discharge to home for both TA-THA and conventional THA to the growing emphasis on early discharge from the hospital after THA regardless of whether technology assistance was used.
We found that average hospital costs decreased for conventional THA but increased for TA-THA during our study period. More importantly, with the exception of 2 time points at 2010 and 2011, the general trend of average hospital cost demonstrated a consistently increased cost for TA-THA compared to conventional THA. Unfortunately, the NIS does not provide specific details regarding hospital cost so we are unable to identify the exact contributors to the increased cost. Furthermore, our data set does not account for costs of preoperative CT scans or cost of purchase and/or maintenance of the devices used in TA-THA. These limitations impede our ability to assess the true cost of TA-THA, which is potentially even greater than what our study demonstrated. However, our findings echo what others have shown which is that TA-THA is generally more costly than conventional THA [17,26].
We recognize that our retrospective cohort study has several limitations. First, there are inherent weaknesses in a large database study including potential for errors in coding and data entry. To minimize these errors, we chose to combine the ICD-9 codes for computer-assisted surgical procedures and robot-assisted surgical procedures into one group. Unfortunately, this process prevents us from stratifying our results based on computer-assisted navigation or robot assistance. However, we believe that for the purposes of our study, a combined TA-THA group is sufficient for answering our study questions. Another important limitation to point out is that the NIS does not provide any information regarding hospital or surgeon volume of surgical cases. This prevented us from analyzing whether TA-THA use was associated with the number of THAs that a particular institution or surgeon performed. The NIS also does not contain any operative details such as duration of surgery, blood loss, surgeon experience, types of components used, or intraoperative fracture. Furthermore, our study did not compare clinical outcomes associated with TA-THA to those of conventional THA. Specifically, owing to the configuration of the NIS, we were unable to assess patient-reported outcomes or postoperative complications such as postoperative dislocation, periprosthetic fracture, or component failure. Finally, we recognize that our analysis of health care resource utilization is limited to trends for LOS, cost, and patient discharge location. These observations are meant only to illustrate changes in these variables over time for TA-THA and conventional THA and are not meant to prove any association or causation.
Despite the aforementioned limitations, our study has several strengths. First, to the best of our knowledge, we not only report on the largest number of TA-THA patients to date but also provide the first national utilization analysis over a 10-year period (2005-2014). Furthermore, the NIS captures patients of all ages and insurance types across the United States, which allows us to provide a more accurate analysis of patient and hospital factors associated with TA-THA.
Conclusions
Our retrospective cohort study showed that the utilization of TA-THA increased during a 10-year period (2005-2014) in the United States. There were no differences in patient age and overall health, as measured by ECI, associated with TA-THA procedures. Instead, TA-THA procedures were associated with specific socioeconomic factors, including race and income, and were more prevalent in the Western region of the United States. Despite the increased utilization of TA-THA during our study period, it remains unclear whether TA-THA improves patient-reported outcomes and minimizes postoperative complications compared to conventional THA. Therefore, additional high-quality prospective studies focusing on outcomes should be conducted before the widespread adoption of this new surgical technology.
Footnotes
All authors declared no conflicts of interest.
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2019.12.009.
Appendix A. Supplementary data
Appendix
Appendix 1.
NIS definitions of hospital size based on number of beds.a
| Location and teaching status | Hospital bedsize |
||
|---|---|---|---|
| Small | Medium | Large | |
| Northeast region | |||
| Rural | 1-49 | 50-99 | 100+ |
| Urban, Non-teaching | 1-124 | 125-199 | 200+ |
| Urban, Teaching | 1-249 | 250-424 | 425+ |
| Midwest region | |||
| Rural | 1-29 | 30-49 | 50+ |
| Urban, Non-teaching | 1-74 | 75-174 | 175+ |
| Urban, Teaching | 1-249 | 250-374 | 375+ |
| Southern region | |||
| Rural | 1-39 | 40-74 | 75+ |
| Urban, Non-teaching | 1-99 | 100-199 | 200+ |
| Urban, Teaching | 1-249 | 250-449 | 450+ |
| Western region | |||
| Rural | 1-24 | 25-44 | 45+ |
| Urban, Non-teaching | 1-99 | 100-174 | 175+ |
| Urban, Teaching | 1-199 | 200-324 | 325+ |
Appendix 2.
NIS breakdown of United States regions by state.a
| Region | States |
|---|---|
| Northeast | Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont |
| Midwest | Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, Ohio, South Dakota, Wisconsin |
| South | Arkansas, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia |
| West | Alaska, Arizona, California, Colorado, Hawaii, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming |
References
- 1.NIH consensus conference: total hip replacement. NIH consensus development panel on total hip replacement. JAMA. 1995;273(24):1950. [PubMed] [Google Scholar]
- 2.Felson D.T., Lawrence R.C., Hochberg M.C. Osteoarthritis: new insights. Part 2: treatment approaches. Ann Intern Med. 2000;133(9):726. doi: 10.7326/0003-4819-133-9-200011070-00015. [DOI] [PubMed] [Google Scholar]
- 3.Elmallah R.K., Chughtai M., Khlopas A. Determining cost-effectiveness of total hip and knee arthroplasty using the short form-6D utility measure. J Arthroplasty. 2017;32(2):351. doi: 10.1016/j.arth.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Lewinnek G.E., Lewis J.L., Tarr R., Compere C.L., Zimmerman J.R. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217. [PubMed] [Google Scholar]
- 5.Kennedy J.G., Rogers W.B., Soffe K.E., Sullivan R.J., Griffen D.G., Sheehan L.J. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13(5):530. doi: 10.1016/s0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 6.Ulrich S.D., Seyler T.M., Bennett D. Total hip arthroplasties: what are the reasons for revision? Int Ortho. 2008;32(5):597. doi: 10.1007/s00264-007-0364-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gallo J., Havranek V., Zapletalova J. Risk factors for accelerated polyethylene wear and osteolysis in ABG I total hip arthroplasty. Int Orthop. 2010;34(1):19. doi: 10.1007/s00264-009-0731-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gwam C.U., Mistry J.B., Mohamed N.S. Current epidemiology of revision total hip arthroplasty in the United States: national inpatient sample 2009 to 2013. J Arthroplasty. 2017;32(7):2088. doi: 10.1016/j.arth.2017.02.046. [DOI] [PubMed] [Google Scholar]
- 9.Ong K.L., Mowat F.S., Chan N., Lau E., Halpern M.T., Kurtz S.M. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop Relat Res. 2006;446(22) doi: 10.1097/01.blo.0000214439.95268.59. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 11.Bozic K.J., Kurtz S.M., Lau E., Ong K., Vail T.P., Berry D.J. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1):128. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 12.Banerjee S., Cherian J.J., Elmallah R.K., Pierce T.P., Jauregui J.J., Mont M.A. Robot-assisted total hip arthroplasty. Expert Rev Med Devices. 2016;13(1):47. doi: 10.1586/17434440.2016.1124018. [DOI] [PubMed] [Google Scholar]
- 13.Jacofsky D.J., Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31(10):2353. doi: 10.1016/j.arth.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 14.Wasterlain A.S., Buza J.A., 3rd, Thakkar S.C., Schwarzkopf R., Vigdorchik J. Navigation and robotics in total hip arthroplasty. JBJS Rev. 2017;5(3) doi: 10.2106/JBJS.RVW.16.00046. [DOI] [PubMed] [Google Scholar]
- 15.Kalteis T., Handel M., Herold T., Perlick L., Baethis H., Grifka J. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. Int Orthop. 2005;29(5):272. doi: 10.1007/s00264-005-0671-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dorr L.D., Malik A., Wan Z., Long W.T., Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 17.Brown M.L., Reed J.D., Drinkwater C.J. Imageless computer-assisted versus conventional total hip arthroplasty: one surgeon's initial experience. J Arthroplasty. 2014;29(5):1015. doi: 10.1016/j.arth.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Domb B.G., El Bitar Y.F., Sadik A.Y., Stake C.E., Botser I.B. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472(1):329. doi: 10.1007/s11999-013-3253-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lass R., Kubista B., Olischar B., Frantal S., Windhager R., Giurea A. Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty. 2014;29(4):786. doi: 10.1016/j.arth.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 20.Snijders T., van Gaalen S.M., de Gast A. Precision and accuracy of imageless navigation versus freehand implantation of total hip arthroplasty: a systematic review and meta-analysis. Int J Med Robot. 2017;13(4) doi: 10.1002/rcs.1843. [DOI] [PubMed] [Google Scholar]
- 21.Rajpaul J., Rasool M.N. Leg length correction in computer assisted primary total hip arthroplasty: a collective review of the literature. J Orthop. 2018;15(2):442. doi: 10.1016/j.jor.2018.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bohl D.D., Nolte M.T., Ong K., Lau E., Calkins T.E., Della Valle C.J. Computer-assisted navigation is associated with reductions in the rates of dislocation and acetabular component revision following primary total hip arthroplasty. J Bone Joint Surg Am. 2019;101(3):250. doi: 10.2106/JBJS.18.00108. [DOI] [PubMed] [Google Scholar]
- 23.Ellapparadja P., Mahajan V., Deakin A.H., Deep K. Reproduction of hip offset and leg length in navigated total hip arthroplasty: how accurate are we? J Arthroplasty. 2015;30(6):1002. doi: 10.1016/j.arth.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 24.Keshmiri A., Schroter C., Weber M., Craiovan B., Grifka J., Renkawitz T. No difference in clinical outcome, bone density and polyethylene wear 5-7 years after standard navigated vs. conventional cementfree total hip arthroplasty. Arch Orthop Trauma Surg. 2015;135(5):723. doi: 10.1007/s00402-015-2201-2. [DOI] [PubMed] [Google Scholar]
- 25.Parratte S., Ollivier M., Lunebourg A., Flecher X., Argenson J.N. No benefit after THA performed with computer-assisted cup placement: 10-year results of a randomized controlled study. Clin Orthop Relat Res. 2016;474(10):2085. doi: 10.1007/s11999-016-4863-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boylan M., Suchman K., Vigdorchik J., Slover J., Bosco J. Technology-assisted hip and knee arthroplasties: an analysis of utilization trends. J Arthroplasty. 2018;33(4):1019. doi: 10.1016/j.arth.2017.11.033. [DOI] [PubMed] [Google Scholar]
- 27.Agency for Healthcare Research and Quality . Healthcare cost and utilization project (hcup) 2014. Introduction to the hcup national inpatient sample (nis)https://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2014.jsp [Google Scholar]
- 28.Austin S.R., Wong Y.N., Uzzo R.G., Beck J.R., Egleston B.L. Why summary comorbidity measures such as the Charlson comorbidity Index and Elixhauser score work. Med Care. 2015;53(9):e65. doi: 10.1097/MLR.0b013e318297429c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agency for Healthcare Research and Quality Bedsize of hospital. In: Healthcare cost and utilization project (hcup) https://www.hcup-us.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp [PubMed]
- 30.Agency for Healthcare Research and Quality NIS states, by region. In: Healthcare cost and utilization project (hcup) https://www.hcup-us.ahrq.gov/figures/nis_figure2_2012.jsp [PubMed]
- 31.Agency for Healthcare Research and Quality Cost-to-charge ratio files. In: Healthcare cost and utilization project (hcup) https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp [PubMed]
- 32.Weber M., Woerner M., Springorum R. Fluoroscopy and imageless navigation enable an equivalent reconstruction of leg length and global and femoral offset in THA. Clin Orthop Relat Res. 2014;472(10):3150. doi: 10.1007/s11999-014-3740-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Manzotti A., Cerveri P., De Momi E., Pullen C., Confalonieri N. Does computer-assisted surgery benefit leg length restoration in total hip replacement? Navigation versus conventional freehand. Int Orthop. 2011;35(1):19. doi: 10.1007/s00264-009-0903-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Antonios J.K., Korber S., Sivasundaram L. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: an analysis of patient and hospital factors. Arthroplasty Today. 2019;5(1):88. doi: 10.1016/j.artd.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.